Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 10, Issue 1
- A study of the nature and level of trust between patients and healthcare providers, its dimensions and determinants: a scoping review protocol
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-3451-5024 Supathiratheavy Rasiah 1 ,
- Safurah Jaafar 1 ,
- Safiah Yusof 2 ,
- Gnanajothy Ponnudurai 3 ,
- Katrina Pooi Yin Chung 4 ,
- Sasikala Devi Amirthalingam 5
- 1 Community Medicine , International Medical University, Bukit Jalil , Kuala Lumpur , Malaysia
- 2 Nutrition and Dietetics , International Medical University, Bukit Jalil , Kuala Lumpur , Malaysia
- 3 Human Biology , International Medical University , Bukit Jalil , Kuala Lumpur , Malaysia
- 4 Pathology , International Medical University , Bukit Jalil , Kuala Lumpur , Malaysia
- 5 Family Medicine , International Medical University , Bukit Jalil , Kuala Lumpur , Malaysia
- Correspondence to Dr Supathiratheavy Rasiah; supathiratheavy{at}imu.edu.my
Introduction The aim of this scoping review is to systematically search the literature to identify the nature and or level of trust between the patient, the users of health services (eg, clients seeking health promotion and preventive healthcare services) and the individual healthcare providers (doctors, nurses and physiotherapists/ occupational therapists), across public and private healthcare sectors, at all levels of care from primary through secondary to tertiary care. It also aims to identify the factors that influence trust between patients, users of health services (clients) and providers of healthcare at all levels of care from primary care to tertiary care, and across all health sectors (public and private). The study will also identify the tools used to measure trust in the healthcare provider.
Methods and analysis The scoping review will be conducted based on the methodology developed by Arksey and O’Malley’s scoping review methodology, and Levac et al ’s methodological enhancement. An experienced information specialist (HM) searched the following databases MEDLINE, EMBASE, the Cochrane Library, Cumulative Index to Nursing and Allied Health Literature. The search terms were both keywords in the title and/or abstract and subject headings (eg, MeSH, EMTREE) as appropriate. Search results were downloaded, imported and stored into a ‘Refworks’ folder specifically created for reference management. The preliminary search was conducted between 7 December 2017 and 14 December 2017. Quantitative methods using content analysis will be used to categorise study findings on factors associated with trust between patients, clients and healthcare providers. The collection of studies will be also examined for heterogeneity. Qualitative analysis on peer reviewed articles of qualitative interviews and focus group discussion will be conducted; it allows clear identification of themes arising from the data, facilitating prioritisation, higher order abstraction and theory development. A consultation exercise with stakeholders may be incorporated as a knowledge translation component of the scoping study methodology.
Ethics and dissemination Ethical approval will be obtained for the research project from the Institutional Review Board. The International Medical University will use the findings of this scoping review research to improve the understanding of trust in healthcare, in its endeavour to improve health services delivery in its healthcare clinics and hospitals, and in its teaching and learning curriculum. The findings will also help faculty make evidence based decisions to focus resources and research as well as help to advance the science in this area. Dissemination of the results of the scoping review will be made through peer-reviewed publications, research reports and presentations at conferences and seminars.
- level of Trust in healthcare
- scoping review protocol
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2018-028061
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
This study seeks to identify the level and nature of trust in healthcare between patients, users of health services and specific individual healthcare providers, for example, physicians, surgeons, nurses, community health workers, physiotherapists and occupational therapists, and pharmacists.
It will review the literature across all levels of care from primary care to tertiary care, and in the private and public sector.
It also seeks to identify the factors that influence trust and the tools used to measure trust in healthcare providers.
The study reviews articles published only in English and over a period of 10 years between January 2007 and December 2017.
The scoping review will not include trust in the provision of health services by dentists, allied health professionals such as phlebotomists, medical laboratory scientists, dietitians and social workers, and in the area of mental health, and trust at the macro level or health systems level, so as to be focused in the scope covered.
Introduction
Context of healthcare provision.
The provision of healthcare occurs in a setting characterised by uncertainty and an element of risk as to the competence and intentions of the healthcare providers. 1 Traditionally, it has been widely accepted that the users or consumers of the service (ie, the patients, and the clients who come for health promotion and preventive healthcare services) trust the judgement, knowledge and expertise of the health professional to provide a competent service. 2 The effective delivery of healthcare requires both the supply of healthcare as well as the acceptance and use of services by the patient and clients. Patient-provider interaction is at the heart of healthcare provision. 2 The nature and environment of healthcare provision occurs on a relational basis—relationships between the providers and users of the service which consequentially impact on health outcomes and wellness.
Trust and its importance in healthcare
Trust is a relational notion between people, people and organisations, and people and events. 3 Patient’s trust in the physician can be defined as a collection of expectations that the patients have from their doctor. 4 It can also be defined as a feeling of reassurance or confidence in the doctor. 5 It is an unwritten agreement between two or more parties for each party to perform a set of agreed upon activities without ‘fear of change from any party’. 6 This is especially true in relationships that result from a lack of choice or occur in a context of asymmetry, such as that between the healthcare provider and patient. Thus, trust is a set of expectations that the healthcare provider will do the best for the patient, and with good will, recognising the patient’s vulnerability. Trust facilitates cooperation between people (known to each other and/or strangers) that is catalysed, facilitated and sustained by trust. 7 Trust is fundamental to effective interpersonal relations and community living. 7 It forms a fundamental basis in the provision of healthcare.
Trust between the patient and the healthcare provider ( doctors, nurses, physiotherapists/occupational therapists ) is important in provider–patient interaction and rapport. It influences patient management outcomes, especially in the treatment of long term illness, as well as influences outcomes of health promotion and prevention initiatives. A trusting relationship between healthcare provider and patient can have a direct therapeutic effect. 8 Trust relations can be distinguished at the micro and macro levels. At the micro level, Trust can be interpersonal trust which is that trust between the individual patient or individual client and the individual clinician, or between two clinicians; organisational or institutional trust is that between the clinician and the manager of the organisation. Trust at the macro level includes trust between patients, the public and the organisation or institution. This study will focus on interpersonal trust between the patient or client and the individual healthcare provider.
Trust is typically associated with high quality communication and interaction, which facilitates disclosure by the patient, enables the practitioner to encourage necessary behaviour changes and may permit the patient greater autonomy in decision-making about treatment. 9
Understanding the issues that influence a person’s trust in the healthcare provider will assist in drawing up suitable operational policies in the delivery of healthcare, as well as influence healthcare practices and behaviours among providers. Transferring this knowledge to medical education will create an emerging practitioner who will be more aligned to the patients’ needs.
Erosion of trust in health care
Critical incidents and sentinel events have contributed to erosion of the patients’ trust in healthcare, the institutions and health systems. 10 The changing sociopolitical environment in healthcare, the impact of the era of information technology and the fact that patients have become increasingly empowered to make informed decisions, have influenced the nature of trust in the healthcare provider. 11
The aim of this scoping review is
To systematically search the literature to identify the nature and or level of trust between the patient, the users of health services and the individual healthcare providers, across public and private healthcare sectors, at all levels of care from primary through secondary to tertiary care.
To identify the factors that influence trust between patients and healthcare providers, at all levels of care from primary through to tertiary level of care, and across all sectors—public and private.
To identify the tools used to measure trust in healthcare between patients, clients and providers of healthcare.
Conceptual framework
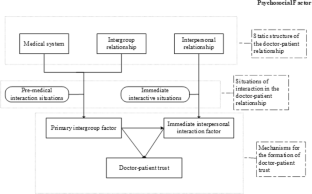
Figure 1 depicts the conceptual framework for trust in healthcare. The study will explore the nature and or the level of trust at the micro-level between patients and users of health services and the individual healthcare provider. The study will also explore the factors that influence trustbetween patients and healthcare providers.
- Download figure
- Open in new tab
- Download powerpoint
Conceptual framework of trust in healthcare.
Commissioning agency
This study is commissioned by the International Medical University, Kuala Lumpur Malaysia. The university has identified research on ‘Trust in Healthcare’ as one of its research thrust areas in its journey towards becoming the centre for research on trust in healthcare.
Study design
The scoping review will be conducted based on the methodology developed by Arksey and O’Malley’s 12 scoping review methodology, and Levac et al ’s 13 methodological enhancement. This framework identifies six stages in undertaking a scoping review: (1) identifying the research question, (2) identifying relevant studies, (3) selecting studies, (4) charting the data, (5) collating, summarising and reporting the results. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist and the PRISMA 2009 flow diagram will be used as a checklist in designing, reviewing and reporting this scoping review.
Stage 1: identifying the research question
The research questions are:
What is the nature and or level of trust between the patient, the users of health services (clients) and the individual healthcare providers (interpersonal trust) across public and private healthcare sectors, at all levels of care from primary through secondary to tertiary care?
What are the factors that influence trust between patients, users of health services and providers of healthcare?
What are the tools used to measure trust in healthcare at the interpersonal level?
Stage 2: identifying relevant studies
The scoping review will be as comprehensive as possible in identifying primary studies and reviews answering the research questions. The research will be restricted to publications in English between the time period of January 2007 and December 2017 and adhere to the eligibility criteria. A preliminary search was conducted between 7 December 2017 and 14 December 2017.
Information sources and search strategy
An experienced information specialist (HM) searched the following databases MEDLINE, EMBASE, the Cochrane Library, Cumulative Index to Nursing and Allied Health Literature. The search terms were both keywords in the title and or abstract and subject headings (eg, MeSH, EMTREE) as appropriate. Search results were downloaded and imported and stored into a ‘Refworks’ folder specifically created for reference management. The preliminary search was conducted between 7 December 2017 and 14 December 2017.
A variety of grey literature will also be searched through the websites of relevant agencies such as the National Institutes of Health, National Institute for Health and Care Excellence and Agency for Healthcare Research and Quality, to identify studies, reports and conference abstracts of relevance to the research questions of this review. We will also conduct a targeted search of the grey literature in local, provincial, national and international organisations’ websites and related health or scientific organisations. Supplementary articles may be obtained by contacting field experts and searching references of relevant articles.
Stage 3: study selection
Study selection process.
First step: Study selection will be initiated using screening procedures to pull together only potentially eligible studies for the scoping review. It involves two steps of screening. The first step will be to go through all the collected titles and abstracts by two independent reviewers. All retrieved citations are subjected to a set of minimum inclusion criteria. These criteria were tested a priori on a sample of abstracts to ensure that they are robust to capture articles that may relate to ‘Nature and Levels of Trust in Healthcare providers’. Any discrepancies will be resolved either through consensus or, if needed, involvement of a third reviewer. Finally, articles that are selected as deemed relevant by either or both of the reviewers will be included in the full-text review in the second step screening. The online or e-learning articles are not included in the study selection for inclusion .
In the second step, both the reviewers will be assigned to the same articles and assess them in full text. Any disagreement between the reviewers will be resolved through discussion with a third reviewer, and thus facilitating consensus for final inclusion. An inter-rater reliability calculation may be done if needed.
Eligibility criteria
Titles and abstracts of articles which directly matched the identified keywords from year 2007 to 2017 will be filtered for relevance to nature and level of trust between healthcare providers and patients or users of health services. We will include studies that fulfil the following criteria:
The study reported qualitative and or quantitative data on the nature of trust or levels of trust between healthcare providers and patients or users of health services.
The study took place in a healthcare setting.
The study was published or reported in the English language.
The study was published in journals, reports or in conference proceedings as literature.
The study measured interpersonal trust (eg, trust in the nurse, physician, healthcare provider) with a valid, reliable instrument and used an established trust questionnaire (ie, included a reference to a published article which used the respective trust questionnaire) or used a validated questionnaire.
The study looked at factors affecting trust in healthcare between patients, clients and the healthcare provider.
Studies using unvalidated instruments, single item questionnaires or those measuring trust in non-health related environment will be excluded.
Stage 4: data collection
Data items and data abstraction process.
A data extraction form will be created by the research team. This form will be reviewed and pretested by all reviewers before implementation to ensure that it captures the information accurately. All reviewers will be trained and be given an exercise using a random sample of articles to be included in the study. The data extraction form will also be piloted on a sample of five articles by the reviewers involved in the scoping study. The aim is to assess for completeness and ease of use. The percentage of agreement between reviewers will also be measured with a target of at least 80 percent agreement.
To ensure study relevance, the various study characteristics are listed below and, this includes but is not limited to the following:
Publication year.
Source origin/country of origin.
Aims/purpose of the study.
Research/study design.
Methodology.
Population characteristics (eg, number of participants, country, physician specialty).
Nature of Healthcare settings—hospital, clinic types, unit/department, primary care/secondary care/tertiary care, public or private sector.
Description of quality indicators including definition, numerator, dominator, psychometrics of the indicators (face validity, reliability, construct validity, risk adjustment).
Intervention characteristics (eg, concept, duration, engagement strategy, timing, required resources).
Tools used to measure level of trust, physician engagement, intervention results (eg, barriers, facilitators, outcomes).
Any factors reported to be associated with hospital physician engagement:
Demographics.
Characteristics of the work environment (eg, organisational support, quality of work-life and perceptions of safety).
Work attitudes (eg, physician work engagement, job satisfaction, commitment and empowerment).
Work outcomes (eg, patient experience, safety, quality of care, individual and organisational performance).
Key findings that relate to the review questions.
The information extracted will then be summarised and tabulated in an Excel file. Each article will be assigned to two reviewers. The reviewers will work independently to extract the data; the data extracted by the pair of reviewers will be compared, and any discrepancies will be further discussed to ensure consistency between the reviewers. Conflicts will be discussed between the reviewers and consensus obtained. If there is difficulty in reaching a consensus, a third reviewer’s opinion will be obtained. This process is undertaken so as to ensure accurate and reliable data collection.
Stage 5: data summary and synthesis of results
Quantitative methods using content analysis will be used to categorise study findings on factors associated with trust between patients, clients and healthcare providers. The collection of studies will be also examined for heterogeneity. Qualitative analysis on peer reviewed articles of qualitative interviews and focus group discussion will be conducted; it allows clear identification of themes arising from the data, facilitating prioritisation, higher order abstraction and theory development. The findings will be analysed (including descriptive numerical summary analysis and qualitative thematic analysis), discussed and reported.
In reviewing the instruments used to measure trust, they will be evaluated for validity and reliability, as well as to understand the domains which are measured, and how the domains are measured.
Stage 6: consultation
A consultation exercise with stakeholders will be incorporated as a knowledge translation component of the scoping study methodology.
Patient and public involvement
Patients and public were not involved in the development of this scoping review protocol.
Data management
All data will be kept confidential and a master index of all studies reviewed will be maintained.
Implications
The findings will be discussed as they relate to the study purpose and implications for future research, practice and policy. The International Medical University will use the findings of this scoping review research to improve the understanding of trust in healthcare, in its endeavour to improve health services delivery by its faculty in its healthcare clinics and hospitals, and in its teaching and learning curriculum. The findings will also help faculty make evidence-based decisions to focus resources and research as well as help to advance the science in this area.
Ethics and dissemination
Ethical approval will be obtained for the research project from the Institutional Review Board of the International Medical University. Dissemination of the scoping review findings will be done through peer-reviewed publications, research reports and conference/seminar presentations.
Acknowledgments
The team would like to acknowledge the following: (1) Mohammad Hisyamuddin (Librarian, International Medical University, Kuala Lumpur, Malaysia) who assisted in the initial search for the journal articles and developed the database of articles in the 'Ref works folder'. (2) Dr Teguh Haryo Sasongko Associate Professor Human Biology, School of Medicine International Medical University, Kuala Lumpur, Malaysia who assisted in the final review of the paper.
- Pellegrini CA
- Anderson LA ,
- Caterinicchio RP
- Mechanic D ,
- Chipidza FE ,
- Wallwork RS ,
- Corrigan JM ,
- Donaldson MS
- Blendon RJ ,
- Benson JM ,
- Colquhoun H ,
Contributors SR: main author, conceived the project, developed the conceptual framework for the study, analysed the preliminary data and wrote the manuscript, and also independent reviewer in the preliminary review. SJ: contributed in writing the manuscript and was one of the independent reviewers in the preliminary review. SY: contributed in performing the search working with the librarian to search for and compile the list of relevant journal articles and store in the specific 'Refworks' folder. GP: contributed in writing the manuscript. CPYK: contributed in writing the manuscript. SDA: contributed in writing the manuscript. All authors read and approved the final version of the manuscript.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
Advertisement
The Formation Mechanism of Trust in Patient from Healthcare Professional’s Perspective: A Conditional Process Model
- Published: 20 January 2022
- Volume 29 , pages 760–772, ( 2022 )
Cite this article
- Yao Wang 1 , 2 ,
- Qing Wu 1 ,
- Yanjiao Wang 1 &
- Pei Wang ORCID: orcid.org/0000-0002-6309-2366 1
853 Accesses
6 Citations
Explore all metrics
Based on an integrated model of doctor–patient psychological mechanisms, the formation mechanism of doctor-–patient trust was systematically demonstrated from the healthcare professional (HCP)’s perspective integrating intergroup relations (expectations), interpersonal relations (communication), and psychosocial (stereotypes). The results of a survey of 3000 doctors and nurses from 14 provinces in eastern, central, and western China support the rationality of an integrated model of doctor–patient psychological mechanisms. The establishment of doctor–patient trust is influenced by the direct role of primary intergroup factors, the indirect role of immediate interpersonal interactions, and the moderating role of social psychology. Specifically, (1) doctor–patient trust is directly predicted by HCP’s expectation and indirectly influenced by communication; (2) stereotypes regulate the relationship between HCP’s expectation, communication, and doctor–patient trust: the activation of positive stereotypes enhances the positive relationship among the three; Negative stereotypes only positively contribute to mediated pathway-communication behaviors and have a weaker facilitation effect compared to positive stereotypes.
This is a preview of subscription content, log in via an institution to check access.
Access this article
We’re sorry, something doesn't seem to be working properly.
Please try refreshing the page. If that doesn't work, please contact support so we can address the problem.
Institutional subscriptions
Similar content being viewed by others
Social trust, interpersonal trust and self-rated health in china: a multi-level study.
Zhixin Feng, Athina Vlachantoni, … Kelvyn Jones
The Relationship Between the Physician-Patient Relationship, Physician Empathy Query ID="Q1" Text=" Please check if the captured title is correct." , and Patient Trust
Qing Wu, Zheyu Jin & Pei Wang

Trust and Its Role in the Medical Encounter
Stephen Holland & David Stocks
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Agliata, A. K., & Renk, K. (2009). College students’ affective distress: The role of expectation discrepancies and communication. Journal of Child and Family Studies, 18 (4), 396.
Article Google Scholar
Atkinson, J. W. (1957). Motivational determinants of risk-taking behavior. Psychological Review, 64 (6p1), 359.
Article PubMed Google Scholar
Bandura, A. (1986). Social foundations of thought and action. Englewood Cliffs, NJ, 1986(23–28)
Barber, B. (1983). The logic and limits of trust . New Brunswick, NJ: Rutgers University Press.
Baviskar, K. (2015). Doctor-patient relation a study of communication. Asian Journal of Research in Social Sciences and Humanities, 5 (9), 1–8.
Birkhäuer, J., Gaab, J., & Calnan, M. (2017). Is having a trusting doctor-patient relationship better for patients’ health? European Journal for Person Centered Healthcare, 5 (1), 145–147.
Bostan, S., Acuner, T., & Yilmaz, G. (2007). Patient (customer) expectations in hospitals. Health Policy, 82 (1), 62–70.
Cegala, D. J., Coleman, M. T., & Turner, J. W. (1998). The development and partial assessment of the medical communication competence scale. Health Communication, 10 (3), 261–288.
Article CAS PubMed Google Scholar
Chai, M. Q., & Wang., J., (2016). An exploration of formation mechanism of doctor-patient trust crisis: From the perspective of intergroup relationship. Journal of Nanjing Normal University (Social Science Edition) , 02
Chang, P.-C., Wu, T., & Du, J. (2020). Psychological contract violation and patient’s antisocial behaviour. International Journal of Conflict Management, 31 (4), 647–664. https://doi.org/10.1108/ijcma-07-2019-0119
Chrisler, J. C., Barney, A., & Palatino, B. (2016). Ageism can be hazardous to women’s health: Ageism, sexism, and stereotypes of older women in the healthcare system. Journal of Social Issues, 72 (1), 86–104.
Cook, K. S., Kramer, R. M., Thom, D. H., Stepanikova, I., Mollborn, S. B., & Cooper, R. M. (2004). Trust and distrust in patient-physician relationships: Perceived determinants of high-and low-trust relationships in managed-care settings . Russell Sage Foundation.
Google Scholar
Crisp, R. J., & Turner, R. N. (2009). Can imagined interactions produce positive perceptions?: Reducing prejudice through simulated social contact. American Psychologist, 64 (4), 231–240.
Cuddy, A. J., Fiske, S. T., & Glick, P. (2007). The BIAS map: Behaviors from intergroup affect and stereotypes. Journal of Personality and Social Psychology, 92 (4), 631–648.
Dhingra, C., Anand, R., & Prasad, S. (2014). Reflection over doctor patient relationship: A promise of trust. Journal of Oral Health & Community Dentistry , 8 (2)
Dong, X. (2020). New interpretation of trust from the holistic perspective. Journal of China University of Mining & Technology(Social Sciences) , (1009–105X), 1–10.
Dong, Z., & Chen, C. (2016). A preliminary study of validity and reliability of the Chinese version of the Physician Trust in Patient Scale. Chinese Mental Health Journal , 30(7), 481–485.
Douglass, T., & Calnan, M. (2016). Trust matters for doctors? Towards an agenda for research. Social Theory & Health, 14 (4), 393–413.
Du, L., Xu, J., Chen, X., Zhu, X., Zhang, Y., Wu, R., Ji, H., & Zhou, L. (2020). Rebuild doctor–patient trust in medical service delivery in China. Scientific Reports, 10 (1), 1–11. https://doi.org/10.1038/s41598-020-78921-y
Article CAS Google Scholar
Gabay, G. (2019). Patient self-worth and communication barriers to trust of Israeli patients in acute-care physicians at public general hospitals. Qualitative Health Research, 29 (13), 1954–1966.
Glasman, L. R., & Albarracín, D. (2006). Forming attitudes that predict future behavior: A meta-analysis of the attitude-behavior relation. Psychological Bulletin, 132 (5), 778.
Article PubMed PubMed Central Google Scholar
Greene, J., & Ramos, C. (2021). A mixed methods examination of health care provider behaviors that build patients’ trust. Patient Education and Counseling, 104 (5), 1222–1228.
Grob, R., Darien, G., & Meyers, D. (2019). Why physicians should trust in patients. JAMA, 321 (14), 1347.
Guo, A., & Wang, P. (2020). The current state of doctors’ communication skills in Mainland China from the perspective of doctors’ self-evaluation and patients’ evaluation: A cross-sectional study. Patient Education and Counseling, 104 , 1–7.
Hao, J., Yang, J., Peng, Y., & Ma, X. (2016). Factor analysis of patients’ trust of township health centers in suburbs, Beijing. Medicine and Society, 29(4), 17–19.
Hauer, K. E., Fernandez, A., Teherani, A., Boscardin, C. K., & Saba, G. W. (2011). Assessment of medical students’ shared decision-making in standardized patient encounters. Journal of General Internal Medicine, 26 (4), 367–372.
Hayes, A. F. (2012). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling . University of Kansas.
Higgins, E. T., Idson, L. C., Freitas, A. L., Spiegel, S., & Molden, D. C. (2003). Transfer of value from fit. Journal of Personality and Social Psychology, 84 (6), 1140.
Hillen, M., De Haes, H., Stalpers, L., Klinkenbijl, J., Eddes, E., Butow, P., van der Vloodt, J., van Laarhoven, H. W., & Smets, E. (2014). How can communication by oncologists enhance patients’ trust? An experimental study. Annals of Oncology, 25 (4), 896–901.
Koirala, N. (2019). Trust and communication in a doctor patient relationship. Birat Journal of Health Sciences, 4 (3), 770–770.
Kuzla, A. (2017). A review of acceptant responses to stereotype threat: Performance expectations and self-handicapping strategies. DTCF Dergisi, 57 (2), 1223–1248.
Li, Y., & Wang, P. (2018). The social psychological mechanism of the construction of doctor-patient trust. Chinese Social Psychological Review, 14 , 4–15.
Liu, J., Yu, C., Li, C., & Han, J. (2020). Cooperation or conflict in doctor-patient relationship? An analysis from the perspective of evolutionary game. IEEE Access, 8 , 42898–42908.
Luhmann, N. (2018). Trust and power . Wiley.
Makoul, G. (2001). The SEGUE framework for teaching and assessing communication skills. Patient Education and Counseling, 45 (1), 23–34.
Marx, D. M., & Stapel, D. A. (2006). Understanding stereotype lift: On the role of the social self. Social Cognition, 24 (6), 776–792.
Nie, J. B., Cheng, Y., Zou, X., Gong, N., Tucker, J. D., Wong, B., & Kleinman, A. (2018). The vicious circle of patient–physician mistrust in China: Health professionals’ perspectives, institutional conflict of interest, and building trust through medical professionalism. Developing World Bioethics, 18 (1), 26–36.
Oettingen, G., & Mayer, D. (2002). The motivating function of thinking about the future: Expectations versus fantasies. Journal of Personality and Social Psychology, 83 (5), 1198.
Perna, G., Varriale, L., & Ferrara, M. (2019). The role of communication in stereotypes, prejudices and professional identity: The case of nurses. Organizing for digital innovation (pp. 79–95). Springer International Publishing.
Chapter Google Scholar
Petrocchi, S., Iannello, P., Lecciso, F., Levante, A., Antonietti, A., & Schulz, P. (2019a). Interpersonal trust in doctor-patient relation: Evidence from dyadic analysis and association with quality of dyadic communication. Social Science & Medicine, 235 , 112391.
Petrocchi, S., Iannello, P., Lecciso, F., Levante, A., Antonietti, A., & Schulz, P. J. (2019b). Interpersonal trust in doctor-patient relation: Evidence from dyadic analysis and association with quality of dyadic communication. Social Science & Medicine . https://doi.org/10.1016/j.socscimed.2019.112391
Prizer, L. P., Gay, J. L., Perkins, M. M., Wilson, M. G., Emerson, K. G., Glass, A. P., & Miyasaki, J. M. (2017). Using social exchange theory to understand non-terminal palliative care referral practices for Parkinson’s disease patients. Palliative Medicine, 31 (9), 861–867.
Qu, X. P., & Ye, X. C. (2014). Development and evaluation research of measurement tools for stereotypes of doctor role perception. Chinese Hospital Management, 34 (2), 48–50.
Riva, S., & Pravettoni, G. (2014). How to define trust in medical consultation? A new perspective with the game theory approach. Global Journal for Research Analysis, 3 (8), 76–79.
Rosenthal, R. (2003). Covert communication in laboratories, classrooms, and the truly real world. Current Directions in Psychological Science, 12 (5), 151–154.
Ruan, X., & Xiao, X. (2017). Correlation analysis on trusted patient assessment and occupational well-being of pediatricians in Wuhan City. Occup and Health, 33 (12), 1661–1664.
Ruscher, J. B. (1998). Prejudice and stereotyping in everyday communication. Advances in Experimental Social Psychology, 30 , 241–307.
Scheid, T. L., & Smith, G. H. (2017). Is physician-patient concordance associated with greater trust for women of low socioeconomic status? Women & Health, 57 (6), 631–649.
Schneider, D. J. (2005). The psychology of stereotyping . Guilford Press.
Shah, R., & Ogden, J. (2006). ‘What’s in a face?’The role of doctor ethnicity, age and gender in the formation of patients’ judgements: An experimental study. Patient Education and Counseling, 60 (2), 136–141.
Sherlock, R. (1986). Reasonable men and sick human beings. The American Journal of Medicine, 80 (1), 2–4.
Shih, M., Ambady, N., Richeson, J. A., Fujita, K., & Gray, H. M. (2002). Stereotype performance boosts: The impact of self-relevance and the manner of stereotype activation. Journal of Personality and Social Psychology, 83 (3), 638.
Skirbekk, H., Middelthon, A.-L., Hjortdahl, P., & Finset, A. (2011). Mandates of trust in the doctor–patient relationship. Qualitative Health Research, 21 (9), 1182–1190.
Street, R. L., Jr. (2002). Gender differences in health care provider–patient communication: Are they due to style, stereotypes, or accommodation? Patient Education and Counseling, 48 (3), 201–206.
Sun, L., & Wang, P. (2019a). Theoretical system of the harmonious doctor-patient relationship evaluation. Journal of Shanghai Normal University(Philosophy & Social Sciences Edition), 48 (05), 88–98.
Sun, L., & Wang, P. (2019b). Theory construction on the psychological mechanism of the harmonious doctor-patient relationship and its promoting technology. Advances in Psychological Science, 27 (6), 951–964.
Thom, D. H., & Campbell, B. (1997). foTlG INALRESEARCH patient-physician trust: An exploratory study. The Journal of Family Practice, 44 (2), 169.
CAS PubMed Google Scholar
Thom, D. H., Wong, S. T., Guzman, D., Wu, A., Penko, J., Miaskowski, C., & Kushel, M. (2011). Physician trust in the patient: Development and validation of a new measure. The Annals of Family Medicine, 9 (2), 148–154.
Thorne, S. E., & Robinson, C. A. (1988). Reciprocal trust in health care relationships. Journal of Advanced Nursing, 13 (6), 782–789.
Tyler, R., & Pugh, L. C. (2009). Application of the theory of unpleasant symptoms in bariatric surgery. Bariatric Nursing and Surgical Patient Care, 4 (4), 271–276.
Wang, P. (1999). A review of social cognitive research on stereotypes. Journal of Psychological Science, 22 (4), 342–345.
Wang, X. J., & Wang, C. (2016). Doctor-patient trust in contemporary China: Characteristics, current situation and research prospects. Journal of Nanjing Normal University (Social Science Edition), 2 , 102–109.
Wang, P., Yin, Z., Luo, X., Ye, X., & Bai, Y. (2018). The impact of doctor-patient communication frequency on the stereotype of the doctor. Studies of Psychology and Behavior, 16 (1), 119.
Ward, P. (2018). Trust and communication in a doctor-patient relationship: A literature review. Arch Med, 3 (3), 36.
Xu, L. L., Sun, L. N., Li, J. Q., Zhao, H. H., & He, W. (2021). Metastereotypes impairing doctor–patient relations: The roles of intergroup anxiety and patient trust. PsyCh Journal, 10 (2), 275–282.
Yao, Q., Ma, H. W., & Yue, G. A. (2010). Success expectations and performance: Regulatory focus as a moderator. Acta Psychologica Sinica, 42 (06), 704.
Yoshihisa, K., & Victoria, W.-L.Y. (2010). Serial reproduction: An experimental simulation of cultural dynamics. Acta Psychologica Sinica, 42 (01), 56–71.
Zhang, B., Yuan, F., & Xu, L. (2014). Reducing the effects of stereotype threat: intervention strategies and future directions. Journal of Psychological Science, 37 (1), 197–204.
Zhang, N., & Zhao, J. (2014). Research on credibility crisis in doctor-patient relationship based on expectation disconfirmation theory. Chinese Medical Ethics, 27 (3), 391–393.
Download references
Acknowledgements
We thank the staff of our partner hospitals for their help in collecting data.
This research was supported by Major bidding projects for National Social Sciences Fund of China (17ZDA327).
Author information
Authors and affiliations.
Faculty of Education, East China Normal University, Shanghai, China, No. 3663 North Zhongshan Road, 200062
Yao Wang, Qing Wu, Yanjiao Wang & Pei Wang
College of Education, Lanzhou City University, Lanzhou, China
You can also search for this author in PubMed Google Scholar
Contributions
YW and QW contributed equally to this article. YW and QW: design of the work; analysis, interpretation of data for the work, drafting the work and revising it critically for important intellectual content. YW: proofreading manuscript. PW: validation, investigation, resources, writing—review and editing, supervision, project administration, funding acquisition, and final approval of the version to be published.
Corresponding author
Correspondence to Pei Wang .
Ethics declarations
Conflict of interest.
Yao Wang, Qing Wu, Yanjiao Wang, and Pei Wang declare that they have no conflict of interest.
Ethical Approval
This study was approved by the local ethics committee of Shanghai Normal University and was conducted in accordance with the Declaration of Helsinki (2013).
Consent to Participate
All participants were informed before the investigation began. All methods were carried out in accordance with relevant guidelines and regulations.
Human and Animal Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the ethics committee of Shanghai Normal University.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Wang, Y., Wu, Q., Wang, Y. et al. The Formation Mechanism of Trust in Patient from Healthcare Professional’s Perspective: A Conditional Process Model. J Clin Psychol Med Settings 29 , 760–772 (2022). https://doi.org/10.1007/s10880-021-09834-9
Download citation
Accepted : 01 December 2021
Published : 20 January 2022
Issue Date : December 2022
DOI : https://doi.org/10.1007/s10880-021-09834-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Integrated model of doctor–patient psychological mechanisms
- Healthcare professional’s expectations
- Doctor–patient trust
- Communication
- Conditional process model
- Find a journal
- Publish with us
- Track your research
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Analyzing patient trust through the lens of hospitals managers—The other side of the coin
Contributed equally to this work with: Aviad Tur-Sinai, Royi Barnea
Roles Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Software, Validation, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations Department of Health Systems Management, The Max Stern Yezreel Valley College, Yezreel Valley, Israel, School of Nursing, University of Rochester Medical Center, Rochester, NY, United States of America
Roles Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing
Affiliation Assuta Health Services Research Institute, Tel Aviv, Israel
Roles Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing
Affiliations Shamir Medical Center (Assaf Harofeh), Be’er Ya’akov, Israel, Israeli Center for Emerging Technologies (ICET), Tel Aviv, Israel, Department of Management, Bar Ilan University, Ramat Gan, Israel
- Aviad Tur-Sinai,
- Royi Barnea,

- Published: April 26, 2021
- https://doi.org/10.1371/journal.pone.0250626
- Reader Comments
Trust is an essential element in patient-physician relationships, yet trust is perceived differently among providers and customers exist. During January-February 2020 we examined the standpoints of medical managers and administrative directors from the private and public health hospitals on patient-physician trust, using a structured questionnaire. Thirty-six managers in public and private hospitals (24 from the public sector and 12 from the private sector) responded to the survey. Managers in the private sector rated trust higher in comparison to managers in the public sector, including trust related to patient satisfaction, professionalism and accountability. Managers from public hospitals gave higher scores to the need for patient education and shared responsibility prior to medical procedures. Administrative directors gave higher scores to various dimensions of trust and autonomy while medical managers gave higher scores to economic considerations. Trust is a fundamental component of the healthcare system and may be used to improve the provision and quality of care by analyzing standpoints and comparable continuous monitoring. Differences in position, education and training influence the perception of trust among managers in the health system. This survey may allow policy makers and opinion leaders to continue building and maintaining trust between patients and care providers.
Citation: Tur-Sinai A, Barnea R, Tal O (2021) Analyzing patient trust through the lens of hospitals managers—The other side of the coin. PLoS ONE 16(4): e0250626. https://doi.org/10.1371/journal.pone.0250626
Editor: Anat Gesser-Edelsburg, University of Haifa, ISRAEL
Received: January 20, 2021; Accepted: April 10, 2021; Published: April 26, 2021
Copyright: © 2021 Tur-Sinai et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The data used in this study contains sensitive information about the study participants and they did not provide consent for public data sharing. The current approvals by the Ethical Committees of Assuta Medical Center and Shamir Medical Center (reference numbers 0108-19-ASF and 0034-19-ASMC) do not include data sharing. A minimal data set could be shared by request from a qualified academic investigator for the sole purpose of replicating the present study, provided the data transfer is in agreement with IL legislation on the general data protection regulation and approval by the Israeli Ethical Review Authority. Contact information: Mrs. Michal Yannay, Research Ethics Committee, Assuta Medical Center: [email protected] , Israel; Prof. Matityahu Berkovitch, Research Ethics Committee, Shamir Medical Center: [email protected] , Israel.
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Patient trust is a fundamental cornerstone in patient-physician encounters [ 1 ], yielding improvement in health outcomes, continuity of care and satisfaction [ 2 , 3 ]. Although the definition of "trust" is still vague, it contains components of loyalty, personal care, consistent longitudinal care [ 4 ], regular good experiences, increasing knowledge [ 5 ], contentment [ 6 ], sometimes acknowledged as "personal doctoring" [ 7 ].
Although all partners involved in patient care; i physicians, patients and their families and medical managers, believe that trust has become one of the foundations of modern healthcare, these relationships are often unbalanced. Individuals who seek healthcare services may perceive the medical environment as precarious due to the risk of medical errors [ 8 ] Complete trust in the physician may be fragile, and requires to increase physicians’ awareness, compassion [ 9 ] and training [ 10 ]. Moreover, in the overloaded work environment of physicians, patient expectations are not always fully understood or accepted by the treating physician.
Within the medical world, surgical procedures emphasize the patient-physician relationship. The informed consent procedure prior to surgery is a unique opportunity to achieve patients’ trust by using medical knowledge in order to help patients overcome their fear [ 11 ], improve satisfaction and enhance patients’ experience.
Achieving patient trust in a hospital setting requires more than a simple person to person encounter. Patients’ experience is often associated with waiting times for hospital appointments, and threatening events such as a treatment or surgery. Sometimes the experience reflects the weakness of the individual patient by highlighting socioeconomic gaps in accessibility to care [ 12 ].
Lack of resources and poor leadership may impact the health system, described as "key factors leading to providers’ inadequate trust, contributed to poor quality services, driving a perverse cycle of negative patient–provider relations" [ 13 ]. A factor analysis of patient perception of trust showed that the contribution of empathy and assurance was relatively low and explained 8% and 5.6% of trust respectively, in comparison to comfortable facilities and appearance (21%), confidentiality (18.7%) and staff responsiveness (16%) [ 14 ]. The type of provider (public/private), hospital experience, the format of insurance coverage, freedom of choice also affect trust and distrust, alongside the configuration of the healthcare system [ 15 ].
A cross-sectional analysis in 23 countries [ 16 ] revealed that trust in physicians differs among health systems and may correlate to health strategy and policy, and to the nature of the health system itself. Trust in physicians was significantly higher in decommodified countries that highlight health as a basic human right (e.g., the United Kingdom, Japan, Norway and the Netherlands) than in commodified countries such as United States (3.8 vs. 3.4; P = 0.0035). The net support of family members, representing high "social trust" [ 17 ], can play a role in the physician-patient-family trust triangle.
The Israeli healthcare system is publicly funded, relying on governmental accountability. Provision of care is available through four health maintenance organizations (HMOs) to any citizen needing medical attention regardless of the ability to pay. Three tiers of coverage are provided: Tier 1 is universal coverage under the National Health Insurance Law (1995) to all residents in accordance with a standard positive list (“basket”) including surgery, acute and rehabilitative inpatient care, medications, and community care. For medications, tests, and treatments in the community, however, copays are charged. Tier 2 comprises supplemental insurance arrangements delivered by the HMOs, including a list of treatments, services, and medications, but only a few palliative medications, and no life-saving ones. Furthermore, the HMOs’ supplemental policies differ in terms, types and extent of oncological coverage. Tier 3 contains various private health insurance policies (personal and group). People who lack private coverage are, of course, susceptible to pay for care not included in the basic basket.
Due to dwindling resources in the Israeli public healthcare system [ 18 ], surgical waiting times may be prolonged, causing many patients to seek treatment in private healthcare. Although the proportion of surgical positions in private hospitals is only 11% of all surgery positions in Israel, approximately a quarter of all surgeries are conducted in the private healthcare system [ 19 ], where patients use their private (commercial) insurance or HMO’s supplementary insurance. Notably, only elective procedures are performed in private hospitals [ 20 ].
The researchers decided to regard patient-physician trust from two opposite directions: a "top-down" approach centered on the patient and excellency in care, and a "bottom-up" approach that involves medium-level managers, medical executives and heads of clinical departments in patient-physician dialogues. Although trust is currently well-established in patient-physician interactions, its vague definition may lead to differences in perceptions, standpoints and behavior among various stakeholders–service providers as well as customers/patients. To understand and improve the patient-physician dialogue, this study was aimed to understand health managers’ perceptions of trust. Specifically, (1) to examine the standpoints of the medical leadership (comprising leading clinical experts who stance as medical managers and administrative executives) on patient-physician trust; and (2) to identify trends and compare similarities and gaps between the private and public health sectors.
This cross-sectional study was conducted during January-February 2020 among physicians in managerial positions (clinical and department managers and hospital medical executives) and administrative managers working in general hospitals in the public and private sectors in Israel. Altogether the 24 public and the 4 private general hospitals in the country were approached, thus reflecting leaders from the entire healthcare system.
Sampling technique
37 managers were approached and 36 agreed to participate: 24 in public and 12 in the private hospitals in Israel. Potential participants were chosen by their involvement in policy decision-making discussion groups and relevance to the study’s aim. The proportion of participants from each sector was determined by the ratio of private to public general hospitals in Israel (5:11). All participants were approached personally with a request to participate in the study and all of them agreed to participate. None of the managers refused to participate in the survey.
Prior to administering the questionnaire, the purpose and procedure of the survey were explained in a telephone call.
Ethical issues
The study was formally approved by the Ethical Committees of Assuta Medical Center and Shamir Medical Center. Each medical center’s Helsinki committees approved the study ethics, the procedure, and the survey questionnaire (reference numbers 0108-19-ASF and 0034-19-ASMC). The participants were informed in writing that their answers would be kept secret for the purposes of the study and they were required to declare their consent to this. All the participants were provided with information regarding the research purpose, confidentiality of information, and right to revoke the participation without prior justification.
Questionnaire and data collection
A structured questionnaire was used to collect opinions via personal interviews. The questionnaire included 61 items in 4 parts, based on a grounded theory [ 21 ], with a Cronbach’s alpha of 0.9172: (A) Components of trust in caregivers and providers (3 questions), values and ideological principles, such as autonomy, satisfaction, accountability freedom of choice and economic implication of care utilization (8 questions); (B) Potential implications of surveys as tools to assess patients as customers (8 questions), personal values of the participating manager (4 questions); (C) Perceived understanding and trust of patients in ten selected operative procedures (30 questions), the effect of low patient trust on caregivers (one question); (D) participant demographics (7 questions). The participants rated each item on a scale of 1 (fully disagree) to 10 (fully agree).
The operative procedures discussed in Section C of the questionnaire were chosen by an expert committee to represent highly prevalent procedures (with significant activity in private and public hospitals) in a variety of clinical fields and populations. These included: adenoidectomy, appendectomy, cholecystectomy, hysterectomy, mastectomy, repair of inguinal hernia, repair of undiscerning testicle, rhinoplasty, total hip replacement and total knee replacement.
Statistical analysis
For each of the questionnaire items, means and Standard Deviations were calculated in accordance with the various reference groups—type of provider (public sector or private) and position of manager/director (director or administrative). The mean and the S.D. of each of the various dimensions were calculated the same way, including, as stated, references to several questions for each.
To check statistical variance among the reference groups in regard to each the dimension and research question, an independent t-test was performed. Also, a 95% CI was calculated in order to examine the difference in the mean for each of the dimensions, in accordance with the various reference groups, as well as the Cohen’s d effect size.
A total of 36 managers participated in the study: 24 participants (17 men and 9 women) from 5 public hospitals, and 12 participants (9 men and 3 women) from 4 private hospitals. Nineteen participants were physicians in clinical managerial positions and 17 were clinicians in executive managerial positions that also had medical management training.
Service provider (private vs. public)
Managers working in the private sector (PRsM) rated core variables related to patient satisfaction and aspects of trust in physicians, the hospital and the healthcare system as a whole, higher compared to the average rating of managers working in the public sector (PBsM) (8.61 vs. 7.89, p = 0.04). They also rated variables related to autonomy and economic considerations higher than PBsM (while despite having observed a difference, it is not possible to draw a statistically supported conclusion) (7.43 vs. 6.85, p = 0.40 and 7.59 vs. 6.38, p = 0.23, respectively) ( Table 1 ). PRsM also gave higher ratings, compared to PBsM, to variables relating to professionalism and accountability, such as physician accountability for best practice (9.17 vs. 6.96, p = 0.01), the hospital’s accountability to supply good care (while despite having observed a difference, it is not possible to draw a statistically supported conclusion) (8.42 vs. 7.50, p = 0.21), the freedom to choose a specific surgeon (while despite having observed a difference, it is not possible to draw a statistically supported conclusion) (8.36 vs. 7.75, p = 0.48), and payment as a factor in care provision from the perspective of the caregiver and the hospital (while despite having observed a difference, it is not possible to draw a statistically supported conclusion) (7.89 vs. 6.25, p = 0.17; 7.30 vs. 5.89, p = 0.49, respectively) ( S1 Appendix ). PRsM also gave higher scores to the opportunity to use surveys as potential tools for assessing the patient as a customer. In contrast, PBsM gave higher ratings to two perceived beneficial implications of such a survey: being a tool for strategic planning (7.29 vs 6.69, p = 0.04), and the need to educate medical students to listen to their patients, and to integrate patients values and wishes in a shared decision making approach (while despite having observed a difference, it is not possible to draw a statistically supported conclusion) (9.28 vs 8.92 p = 0.23). PRsM gave higher scores to patients’ preliminary knowledge regarding the procedures (while despite having observed a difference, it is not possible to draw a statistically supported conclusion) (7.34 vs. 7.05, p = 0.49). On the other hand, PBsM gave higher scores to the need for patient’s education prior to medical procedures (while despite having observed a difference, it is not possible to draw a statistically supported conclusion) (7.95 vs. 7.49 p = 0.26) as well as to shared responsibility in decision making (8.70 vs. 7.28 p<0.01) ( Table 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0250626.t001
An elaboration of the dimensions and a one-by-one examination of the ten specific operative procedures included in the survey revealed a consistent trend of higher average trust scores by PBsM compared to PRsM in eight of the ten operative procedures: appendectomy (9.00 vs. 6.55 respectively, p<0.01), gallbladder removal (8.63 vs, 7.18, p = 0.02), inguinal hernia (8.92 vs. 7.67, p = 0.01), hysterectomy (8.71 vs. 7.42, p = 0.01), mastectomy (9.08 vs. 8.36, p = 0.08) (an observed difference with proximity to p = 0.05 limit), rhinoplasty (8.38 vs. 7.42, p = 0.06) (an observed difference with proximity to p = 0.05 limit), undescended testicle repair (8.58 vs. 7.10, p = 0.04) and tonsillectomy (8.83 vs. 7.58, p = 0.01) ( S2 Appendix ).
Comparative scoring of the consequence of knowledge transfer from physicians to patients revealed dissimilarities among the participants; for example, PBsM rated the importance of providing knowledge or the added value of explanation/education significantly higher in hysterectomy (8.17 vs.7.00, p = 0.03) and tonsillectomy (8.50 vs 7.58 respectively, p = 0.06) (an observed difference with proximity to p = 0.05 limit) compared with PRsM ( S2 Appendix ). In other cases the opposite picture was revealed: PRsM rated the importance of providing knowledge on knee replacement and inguinal hernia significantly higher compared to PBsM (8.08 vs. 6.42, p = 0.01 and 9.00 vs. 7.46 p<0.01, respectively).
The role and position of the participating managers (Medical Managers vs. Administrative Directors)
Administrative Directors (AD) had rated dimensions of trust and autonomy higher than medical managers (MM) (while despite having observed a difference, it is not possible to draw a statistically supported conclusion) (8.65 vs. 7.67, p<0.01 and 7.29 vs. 6.82, p = 0.47, respectively). AD also rated patients’ preliminary knowledge regarding the procedures and the need for patient education prior to medical procedures higher than MM (while despite having observed a difference, it is not possible to draw a statistically supported conclusion) (7.98 vs. 7.63, p = 0.36 and 7.29 vs. 7.01 p = 0.48, respectively). MM rated economic considerations and sharing responsibility regarding treatment decisions higher than AD (while despite having observed a difference, it is not possible to draw a statistically supported conclusion) (7.11 vs. 6.34, p = 0.42, and 8.41 vs. 8.02 p = 0.42, respectively) ( Table 2 ).
https://doi.org/10.1371/journal.pone.0250626.t002
Dimensions related to the perception of patient surveys as a managerial or planning tool or as a barometer to partnership in care showed even smaller difference between MM and AD (while despite having observed a difference, it is not possible to draw a statistically supported conclusion) (7.12 vs 7.08, p = 0.96 and 9.19 vs 9.12, p = 0.79, respectively).
MM rated trust within the scope of particular operative procedures consistently higher than AD, as demonstrated for appendectomy (8.79 vs. 7.56 respectively, p = 0.06) (an observed difference with proximity to p = 0.05 limit). In contrast, AD rated the importance of knowledge transfer to the patient or the added value of explanation/education significantly higher than MM in procedures such as mastectomy (8.19 vs. 7.26, p = 0.05), knee replacement (8.24 vs. 7.16, p = 0.02) and hip replacement (8.06 vs. 7.11, p = 0.04) ( S2 Appendix ).
A qualitative analysis of free text remarks added to the questionnaire revealed PRsM mentioned that the major forces leading to patient-physician trust are cohesiveness within the multidisciplinary team members, while PBsM emphasized professionalism as a leading vector. PRsM refere to economic incentives as obstacles to the perception of full trust; such as fair pricing, charges or mode of payment. In comparison, PBsM mentioned socioeconomic gaps or disparities in accessibility to care as barriers to full trust.
"Trust" is a complex entity, composed of sharing of knowledge, responsibility and satisfaction, and increases safety behavior and perception [ 22 ] when both sides rely on each other and have an incentive to join forces to keep a "contract". Traditionally surveys refer to either the patient’s standpoint or less frequently to physicians values, yet rarely introduce the perspective of the medical leadership. Our unique contribution focuses on the standpoints on medical managers, presenting differences according to their expertise, position and provider sector. The analysis revealed several trends, however we primarily focus on the most significant finding., The importance of trust as a general value was ranked higher by administrative managers compared to clinical managers and by managers in the private sector compared to managers in the public sector. On the contrary the value of patient- doctor partnership or "shared responsibility" was ranked higher by public sector managers in comparison with private sector managers, while position (medical vs administrative) showed no significant differences. A profound observation reveals administrative managers deeply appreciate trust among all stakeholders- the general practitioner, the surgeon and the entire healthcare. They also emphasized the caregiver’s responsibility as a key professional principle. Analysis by the type of provider showed private sector managers unsurprisingly highlighted the responsibility of the physician regarding the patient-doctor equation, moreover they suggest such surveys may be used as managerial tool for further planning and improvement.
Other topics investigated in our questionnaire revealed no significant differences among the groups of participants, although clues to trends were traced; for example PBsM gave ranked higher freedom of choice and considering patients’ preferences, alongside the added value of residents’ education and the opportunity of data sharing.
The same trend exists across almost all types of operative procedures examined, PRsM attributed greater importance of professionalism and accountability, probably due to the frequent attention drawn to these elements by their board of directors. This may be explained by the characteristics of the targeted encounter between the patient and the physician in the public health sector, shortly before the surgical procedure. In contrast, in the private healthcare system the patient-physician relationship starts in a consultation meeting prior to the surgery, and the patient has several opportunities to create trust with the care provider and to consider options for care before the operative procedure take place.
Our findings, which indicate higher trust levels among managers in the private health sector compared to the public setting are in line with Niv-Yagoda’s work, which showed an association between low levels of trust in the public healthcare system and the public’s perception regarding the importance of patient’s autonomy (e.g., selecting a surgeon) [ 23 ].
We believe that the executive managers rated trust higher than their counterparts due to their experience and holistic approach emphasizing the current focus on patient empowerment and the MoH strategic guidance to implement patient-centered policy. Interestingly, clinical professional experts highlighted economic issues, which are considered a barrier to consumption of health services, in particular, elective surgeries. Clinical managers may also consider the economic burden as a bigger threat to avoid maximal beneficial treatment to socially deprived populations.
The qualitative analysis of participants’ remarks added to the questionnaire, revealed differences in the major themes about factors influencing trust as well a spectrum of positive and negative sentiments: PRsM regard effective multidisciplinary teamwork as a leading force to trust, while economic barriers may reduce trust. PBsM believe professionalism is the foremost vector to gain trust, while socioeconomic gaps decrease trust.
As every Israeli resident is entitled by law to receive surgery in the public healthcare system, regardless of his/her financial resources, it is possible that PBsM expressed pointed to the importance of equity while PRsM highlighted economic incentives.
The sentiment in both sectors was positive "Trust exists and is a crucial element is healthcare, an essential need". Surprisingly PRsM described trust as a comprehensive, ongoing encounter, while PBsM referred to it as an acute episode or a "snapshot", explained by the episode of informed consent prior to surgery.
Study limitations
Although we approached managers from various medical centers in the public and the private sector, the convenience sampling method may have limited our ability to generalize our findings, and the small sample may have influenced the statistical strength. Additionally, as the managers were approached personally, a social desirability may have affected their answers. Further research may clarify trends that are emerging yet non significantly, we suggest a to compare our findings with another health system.
Conclusions
Trust is an essential component of healthcare systems and as such should be further nourished and maintained by both patients and care providers. By focusing on manager perspectives, we were able to provide a complementary view to that of patients, yet far from completion. This survey may allow policy makers and opinion leaders to continue building and maintaining trust between patients and care providers. Moreover, it would be interesting to explore whether the Covid-19 breakout that appeared after our survey was already completed, would have an influence on this fragile patient-physician relationship.
Supporting information
S1 appendix. overall perception of trust by service provider or type of expertise (mean)..
https://doi.org/10.1371/journal.pone.0250626.s001
S2 Appendix. Perceived understanding and trust of patients in selected operative procedures (mean).
https://doi.org/10.1371/journal.pone.0250626.s002
- View Article
- Google Scholar
- PubMed/NCBI
- Open access
- Published: 20 July 2023
Indicators of the dimensions of trust (and mistrust) in early primary care practice: a qualitative study
- Allen F. Shaughnessy 1 ,
- Andrea Vicini, SJ 2 ,
- Mary Zgurzynski 4 ,
- Monica O’Reilly-Jacob 3 &
- Ashley P. Duggan 1 , 5
BMC Primary Care volume 24 , Article number: 150 ( 2023 ) Cite this article
1524 Accesses
5 Altmetric
Metrics details
Trust occurs when persons feel they can be vulnerable to others because of the sincerity, benevolence, truthfulness and sometimes the competence they perceive. This project examines the various types of trust expressed in written reflections of developing healthcare clinicians. Our goal is to understand the roles trust plays in residents’ self-examination and to offer insight from relationship science to inform the teaching and clinical work for better trust in healthcare.
We analyzed 767 reflective writings of 33 residents submitted anonymously, to identify explicit or implicit indicators attention to trust or relationship development. Two authors independently coded the entries based on inductively identified dimensions. Three authors developed a final coding structure that was checked against the entries. These codes were sorted into final dimensions.
We identified 114 written reflections that contained one or more indicators of trust. These codes were compiled into five code categories: Trust of self/trust as the basis for confidence in decision making ; Trust of others in the medical community ; Trust of the patient and its effect on clinician ; Assessment of the trust of them exhibited by the patient ; and Assessment of the effect of the patient’s trust on the patient’s behavior .
Broadly, trust is both relationship-centered and institutionally situated. Trust is a process, built on reciprocity. There is tacit acknowledgement of the interplay among what the residents do is good for the patient, good for themselves, and good for the medical institution. An exclusive focus on moments in which trust is experienced or missed, as well as only on selected types of trust, misses this complexity.
A greater awareness of how trust is present or absent could lead to a greater understanding and healthcare education for beneficial effects on clinicians’ performance, personal and professional satisfaction, and improved quality in patients’ interactions.
Peer Review reports
Where is the wisdom we have lost in knowledge?
Where is the knowledge we have lost in information?
-- From The Rock , T.S. Eliot
In healthcare, the yearning to be seen as an individual is particularly poignant because the relationship between clinician and patient is in many ways so intimate—and, at the same time, the learning and practice of relationships in clinical care can feel so distant. The vulnerability of sharing, with the resulting generation of wisdom, can get lost in biomedical measures, in knowledge, and information. In this project, we explore written reflections from developing healthcare clinicians to offer insight into the teaching and clinical practice of trust. Our project and data offer practical insight for teaching and improving trust in healthcare, including intrapersonal trust (trusting oneself) and interpersonal/relational trust (trusting colleagues and patients) and organizational trust (trusting healthcare systems and structures). We address implications of trust from relationship science and human communication research as well as practical implications of trust.
Across disciplines, trust is conceptualized as entailing some level of risk, uncertainty, or willingness to be vulnerable, and trust creates an expectancy about future behavior since a person must assume that a person, group, or organization will behave in a particular way [ 1 ]. Trust, at its core, is when a person feels they can be vulnerable to others because of the sincerity, benevolence, truthfulness and sometimes the competence they perceive of others [ 2 ]. People may extend trust to individuals, organizations, or societal structures that could act to further our interests or protect what we see as vulnerable. Trust often involves a transfer of power to a person or to a system [ 3 ]. Trust in organizations involves not only competence, but also openness and honesty, concern for stakeholders, reliability, and a sense of attachment or values that are aligned with our desires [ 4 ]. Healthcare professionals and patients know well when they experience trust in a healthcare interaction and system; they can rely on their healthcare team to be at their service and committed to promoting well-being [ 5 ].
Trust is usually bidirectional and relationship-based, built over time and across a series of interactions. Patients who experience high trust are less likely to second guess what healthcare professionals suggest as diagnostic follow-up, therapy, or lifestyle advice; an additional expert opinion might still be needed, but even that is an expression of a trust-based relationship [ 6 ]. Trust is usually vigilant and includes critical discernment, not implying dependence or surrendering independence [ 2 ]. Clinicians who feel they can trust and are trusted by patients feel recognized and appreciated for their clinical knowledge and competence and are confirmed in their ability to promote health, well-being, and flourishing in patients and within society [ 7 ]. Trust is a commodity that cannot be presupposed, but can be examined and promoted [ 8 ]. Trust also involves systemic and structural dimensions such that increasing trust in healthcare contexts can be beneficial in multiple ways—subjective and objective, relational and social, financial and organizational [ 9 ].Trust is a value in itself, and trust facilitates deeper relational interactions, continuity of care, quality of services provided, and facilitates opportunities for containing healthcare costs; on the other hand, when trust is lacking, dissatisfaction, disappointments, and frustrations appear to dominate and compromise healthcare experiences [ 2 ].
The effect of trust on the provision and receipt of healthcare is well documented. Better trust of physicians by patients lowers their perception of risk of treatment [ 10 ]. Patients with diabetes who trust their physician are more likely to follow suggested self-care guidelines [ 11 ]. Trust is also both a critical ingredient to and result of effective shared decision-making [ 12 , 13 ]. Patients who do not trust their physicians are more inclined to make their own decisions rather than using a shared decision approach [ 14 ].
This article focuses on trust in an inductive way by examining various types and dimensions of trust identified in reflective writings from developing healthcare clinicians attending to their experiences interacting with patients, colleagues, and staff. Written reflections offer insights into their understanding of trust and how trust impacted them. Our goal is to understand the various roles trust play in residents’ self-examination and to offer implications for teaching and improving trust in healthcare.
This project began as an effort to introduce reflective writing and to improve reflective writing skills of family medicine residents in a single residency in the United States. The 33 residents were given regularly scheduled time to write these reflections into an internet-based database. They were not required to write the reflection at this time but could access the database at any time. They were not given a prompt but were asked to give each entry a title and link to clinical topic where appropriate. The reflections were not graded or evaluated in any way and were available only to the resident. Most (94%) of the residents participating in this project were women and were at all levels of residency education. This percentage is consistent with 94% of the Family Medicine residents being women. A total of 767 reflections were written over 18 months and were collected for this project.
IRB approval and ethical protections for participants
We obtained Institutional Review Board approval from two institutions where the researchers are affiliated. First, the project was approved as exempt and with waiver of written informed consent by the Cambridge Health Alliance Institutional Review Board (first author’s affiliation) and then by Boston College (other authors’ affiliation) under the classification of education research. All methods were carried out in accordance with regulations that apply to exempted research. Reflection entries were de-identified by a researcher not involved with participants (AD) before the analysis, other than being categorized by year of training. This analysis was performed after all participants graduated from the training program. In addition, examples from the reflections in this paper are aggregated or paraphrased in a way to disguise identification with a specific residency or medical resident.
Analysis of the reflections began with a research assistant identifying explicit uses of the word “trust” in the writings. One author read through all reflective entries. Using an inductive method to develop a framework of the underlying structure of experiences in the data [ 15 ], this author identified entries with explicit or implicit indicators of reporting or reflecting on issues of trust. These entries served as the basis for analysis. A second author read through all these entries to further identify meaning units. Both authors developed separate coding structures. After discussion with a third author, the final coding structure was developed and then checked by applying it to the entries.
Hence, an interdisciplinary research team read through the entire data set and identified, through a-priori consensus process, trust as a content area to be qualitatively examined. Within reflections addressing trust, themes were systematically and inductively derived from the data. Research team members read through the entire data set each independently and then as a group, identifying themes as well as latent and manifest content areas that emerged from the reflections [ 16 ]. Emerging themes and occurrences of communication were quantified/counted with the reflective entry as the unit of analysis and then sorted qualitatively and independently by one of the research assistants grouping together under higher order headings.
Similar to grounded theory as a philosophical approach and research method, the qualitative content analysis allowed explanatory framework to be developed through systematic gathering and analysis of data such that explanations are grounded in the data [ 17 ]. The method is in contradistinction to the hypothetico-deductive model usually used in science, in which a predetermined theory or hypothesis is developed and then tested using any of a variety of study designs. We used an iterative process of systematically and inductively identifying themes and creating categories within the reflections [ 16 ]. An undergraduate research assistant from Boston College served as the initial primary coder (MZ); she read and categorized all of the occurrences of trust independently and processed identified themes on a weekly basis with the other authors. In cases of disagreement, or questions, the team shifted and reorganized until consensus was reached. As an additional guard against arbitrary decision-making, we each re-analyzed the data together after developing categories to minimize force-fitting data.
Interpretation
All authors have extensive experience with qualitative research and implications of social construction of interpretations in research [ 18 ]. One researcher has a background in medical education, another has a background in human communication research, and the third researcher has a background in medicine and bioethics. Each investigator thus applied a unique frame of reference in the analysis. We used a reflexive approach to examine our own beliefs and judgments [ 19 ]. At each point in the process–after entry selection, initial coding, secondary coding, and final coding structure checking–the research group independently collected notes on their thoughts and then met to discuss and reflect on the findings to develop a framework based on consensus for analysis.
We identified 114 written reflections that contained one or more indicators that the writer was considering trust, either implicitly or explicitly. These codes were compiled into five dimensions.
Trust of self/trust as basis for confidence in decision making (n = 50 entries). Trust of self is demonstrated by an explicit assessment of one’s own knowledge, skill, or competence, which leads to a determined assessment of one’s competence to perform clinically. These entries reflected their explicit examination of their own knowledge, skill, or competence, or their assessment of their confidence, using phrases such as, “I don’t feel like I did a fantastic job,” “I don’t have much experience with…,” “I am quickly being reminded of the overwhelming amount of medical information that I do not know,” and, “it was a classic case but I hesitated making this diagnosis initially”. One resident wrote, “[I] just saw a challenging [patient]; amazing how powerful the creepy vibes are. [In] these scenarios I have to stick to my instincts because they are probably right.” In addition, they used entries to capture notes from lectures or direct lifts from information resources may indicate their acknowledgement of the perceived tenuousness of their knowledge.
Trust of others in the medical community (n = 24 entries). Trust in the community involves the ability to rely on others to aid in one’s care of a patient. These entries commented on residents’ level of trust in the healthcare systems or their colleagues to support the care they wished to provide for their patients. Some entries reflected an assessment of specialists or supervisors. For example, one person wrote, “well, I don’t feel as inadequate about my adolescent interview techniques after observing the ‘professionals’ suffer through a non-cooperative teenage patient.” Another wrote, “She saw [a specialist] who recommended using urea cream… I am a little skeptical of this.” Some entries reflected on the healthcare system in general: “Some of my biggest concerns over my limited time in residency stem from the inefficiency [and occasional un-safety (sic.)] of the systems we have in place”; “Peds was a circus too. The floor is so inefficient it should be featured in some business PowerPoint entitled ‘how not to do things.’ Some entries also questioned the value they perceived they would receive from specialists if they were to refer patients to them: “Thought about urology but didn’t think it would help much.”
Trust of the patient and its effect on clinician (n = 9 entries). These entries examined residents’ trust of a particular patient and how it affected them, either personally or their decision making. One resident reflected on a patient visit: “I felt torn, and a little defeated. Defeated because I knew that I would give this woman [an opioid] … Defeated because I didn’t want to do that, I wanted to talk to her longer, understand the history, understand more what her stressors were, and discourage the dependence… Torn because I feel for her, and that she has to manipulate and lie in order to feed her addiction. Torn because her provider, me, does not trust her, and that’s not a nice thing to feel.”
Particularly poignant entries focused on patients requesting medication for pain, (regarding a patient asking for a specific scan): “I guess I’m left with a feeling where it is hard for me to know how to act or think when I have patients who I’m not sure are telling me the truth. I want to believe them and help them and get to know them, but I’m afraid that they’re just using me.”
Assessment of the trust of them exhibited by the patient (n = 19 entries). Developing clinicians seemed to implicitly grasp the role of relationship development in their care, often commenting on their assessment of the trust or lack of trust exhibited by a particular patient. Several reflective entries seemed to marvel at the institutional trust conferred on clinicians, of patients not questioning them as a doctor or as their healthcare clinician. As an example, “Patients fully respected the title and had all the expectations of me that they would have of my preceptors. This is both exciting and scary.”
Developing clinicians also reflected on patients who did not seem to trust them: “I can’t believe she accused me of being racist of all things!”; and, “Right there in one fell swoop, I felt that I had cut ties with the mother and her daughter.”
Assessment of the effect of the patient’s trust on the patient’s behavior (n = 12 entries). Residents also commented on their assessment of the connection between the patient’s behavior and the resident’s assessment of the patient’s trust in them: “I do think I established a good rapport with the patient, and that she felt comfortable talking to me about her depression.” Commenting on a patient’s compliment, one resident wrote, “I’ve spent some time talking with him about his leg pain (which he is imminently worried about and is putting highest on the priority list, above his heart rate of 20, ARF, and serious need for a pacemaker) … Unlike all his other doctors, apparently, I could pretend to care, and take a little time to write some orders for pain meds and capsaicin cream. And, apparently, that made all the difference.”
Based on inductive analysis to develop an explanatory framework for the underlying structure of experiences [ 15 ] this article develops an explanatory framework for dimensions of trust (and mistrust) in early primary care practice based on healthcare clinicians’ reflections written over an academic year. This article identifies direct indications of trust, as well as.
more subtle cues that suggest concern or mistrust. Analysis provides evidence for five dimensions of trust including trust of self/trust as basis for confidence in decision making, trust of others in the medical community, trust of the patient and its effect on clinician, assessment of the trust of them exhibited by the patient, and assessment of the effect of the patient’s trust on the patient’s behavior. Examples indicate the importance of understanding trust through implicit or subtle cues in addition to explicit statements. Implicit cues indicative of trust (or mistrust) are important, because when we get to a point where we say “you can trust me,” or when we ask whether we can trust someone, we have missed something fundamental in the relationship or institutional context. Identified dimensions of trust extend previous research where measures of trust are based on biomedical competence and attentiveness indicative of health service quality [ 20 ].
Each concrete illustration from healthcare clinicians’ written reflections situate and exemplify the dimensions of trust that the authors identify. In healthcare interactions, diverse and even contrasting ways of experiencing trust (or mistrust) can occur at the same time or and can be spread in daily practice. In other words, trust is built on reciprocity over time, and, as with every relational process, trust is dynamic, fluid, and changing. Hence, trust can evolve; trust can be challenged and threatened. Multiple dimensions of trust facilitate the relationship between patients and healthcare professionals and vice versa; mistrust, on the contrary, damages the relationship.
The written reflections provide evidence that trust belongs to the realms of personal experience and of relationality. Hence, trust engages one’s identity. In particular, both patients and healthcare professionals can grow in trusting one another–for example, by sharing something about what matters in their lives–and this sharing reinforces their personal and professional identity. Conversely, when trust is abused, a person loses the ability to trust other people or institutions. Reflecting on trust requires a person to consider the experiences that influenced and shaped trust, how that person can recognize and name those experiences, how the person is still suffering from those experiences, how the person can still be trapped in mistrust, how the person has healed from mistrust, how previous experiences with trust (or mistrust) have empowered or disempowered the person.
Dimensions of trust
Examples in this article provide evidence for broader dimensionality of trust in healthcare than in previous research. Trust can begin as unidirectional and anonymous, like when we strap ourselves into a seat of a jet that will hurtle us from one place to another at 900 km per hour. We place our trust in a pilot, a piece of machinery, and the law of physics, perhaps initially without a second thought. Trust can be intra personal–I trust or do not trust myself–or inter personal–I can trust or not trust and, conversely, they can trust or not trust me. I can gain or lose the trust of another and gain or lose trust in the other.
Agents of institutions can be trusted, or mistrusted, based on institutional structures, organizational arrangements, dynamics in interactions with people, employees, groups, and communities. Trust, or mistrust, in science (medicine, drugs, public health measures, diagnostic tools, therapies), may be differ between clinicians and patients. Corruption that draws a social institution away from its mission and undermines its integrity can lead to broad mistrust of both the institution and its members [ 21 ]. We see this played out in the mistrust of agents of government, information sources, and other institutions. The focus on institutional trust in this article extends the framework of previous research describing mutual trust in terms of continuity of care or familiarity with the doctor [ 22 ].
Examples indicate how trust depends on truth but, more importantly, the trustors’ perception of the degree of truth. Trust can be contextual, e.g., I might trust my family doctor to understand my emotions but not to remove my appendix. Trust may ebb and flow, reinforced or negated by relationships. Mistrust can come from communication difficulties [ 22 ]. Trust can be earned (or not) or sometimes is granted provisionally without demonstration, especially when the need for trust is high. Patients may trust their healthcare clinician whom they have just met because they trust the profession. This lease on trust, based on the trust of the institution, will be ratcheted up or down based on additional experiences.
Healthcare clinicians trust conclusions derived from their education or research findings (evidence-based medicine) until their knowledge is called into question by their subsequent experiences. In addition, they need to, based on relational clues, trust both in the patient and in their own ability to address explicitly stated concerns as well as hints or cues of what the patient wants (and does not want).
Trust and relationships in healthcare
The process of dyadic interdependence in navigating trust is a communication process—sometimes that process translates into reciprocity in the interaction and in building and maintaining a relationship, even in power imbalanced or role-based positions. I am trusted, I trust. If I am not trusted, I may suspend my ability of trusting until trust can be restored, or I lose my ability of trusting until I heal from experiences of mistrust. As part of the diagnostic process and therapeutic alignment, healthcare clinicians need judge what the patient says and demands, what the patient needs, what the patient does not want, what the patient is unable to see. Experiences can reinforce trust in oneself, others, and institutions.
Trust is not only given: “I trust someone or something.” Trust is also received: “I am trusted by someone, for who I am, for what I am doing, for something I did, and for what I did not do.” In their reflective entries physicians indicate how the trust they received from the medical guild during their training, and from colleagues, staff, and patients in their daily practice, made them trust themselves more. In a way, trust builds trust: the way others trust us–because we are trustworthy–builds our ways of trusting ourselves as human beings and as professionals. Of course, trust is also nourished by formation, training, and experience.
Physicians describe how further study, repeated practice, attentive reflection, and critical analysis strengthen their trust in what they are able of doing, in their skills, and in their ability of learning from their omissions, uncertainties, reductive and limited diagnostic differential possibilities, and mistakes. Hence, trust is transformative, transforming in positive ways one’s being and doing. On the contrary, if one’s trust has been abused, the ability to trust other people or institutions might be lost. Such a loss can be provisional and temporary, waiting to see whether it could be possible to restore trust and what that would entail.
Trust in the institution of medicine
Trusting relationships are influenced by context. There is a reciprocity between trust between clinician and patient and how the institutions–medicine, science–are trusted. There is tacit acknowledgement of the interplay among what the residents do is good for the patient, good for themselves, and good for the medical institution. There is also, in the reflections, a marveling, especially by residents just beginning their training, of an implicit trust in their competence and benevolence because they, though previously not known to their patients, are part of the institution of medicine. They acknowledge that the trust given to them is only leased–that patients will provisionally trust them until such time that the residents’ behavior will confirm and reinforce this trust, or disprove it.
Institutions influence the healthcare practice and the agency both of healthcare professionals and of patients. Institutions can contribute to creating a trusting environment that fosters trust or they can jeopardize the development of trust (e.g., because of bureaucracy, because of costs, because of limited access, because of racial dynamics, because of hindrances to communication when patients’ languages and worldviews are not understood). Given the frequent and off-hand way of commenting on it, residents seemed to see trust development of them by the patient as being central to their effectiveness, building on the institutional trust that served as the basis for the visit.
Residents also exhibited or directly commented on their trust in themselves, either regarding their psychological suitability to provide care (either at that moment or in general) or in their clinical knowledge and prowess. For the latter, this conscious incompetence with the resulting lack of confidence is developmentally appropriate and a rationale for prolonged supervised practice. Trust in an institution derives from current and past experiences with that institution, what it does and did to me and to others, and from what does not do and did not do to me and to others; from its structures, organizational arrangements, dynamics in interactions with peoples, employees, groups, and those living in the surrounding territory.
Moreover, members of minorities know too well that trust goes beyond the personal relationship here and now. One could say that the “weight of history”–particularly in the case of histories of racial discrimination, abuses, and violence–burdens the possibility of trust, of trusting another, a healthcare professional, a healthcare institution, even the diagnostic and therapeutic processes. To heal trust and to restore trustworthy relationships demands more than good intentions, a strong will, and personal efforts. Social and institutional reparative and restorative processes leading to acknowledging those systemic and structural violations of trust are needed to create the conditions for social justice that are required to earn and experience trust.
The weight of personal histories matters too; for example, when one considers what concerns substance abuse. Because of these personal histories trust is challenged, in diverse ways, both by the healthcare professional and by the patient: the patient might not be trusted in her requests for more drugs, and the physician might not trust that giving those drugs will be beneficial for the patient. As personal accounts indicate, trust is elusive and maybe cannot be experienced in constrained and inhibiting relational dynamics.
Trust and communication behavior
Whether one focuses on intrapersonal understanding, interpersonal relationships, or building trust in organizations, trust is built over time. In the relationship science literature, a spiral theory of trust purports that, first, “trust, once established, remains relatively fixed, but also spirals over time to increase or decrease trust in response to verbal and nonverbal behavior of participants” [ 1 ]. This functional approach allows one to specify key communication goals and desired outcomes (e.g., building trust, shared decision-making to include patients’ values, or managing uncertainty) that need to be accomplished for quality healthcare. Second, this functional approach embraces the notion that communication to build trust is essentially goal-oriented and aims at achieving outcomes through communication that contribute to improving, or sustaining, patients’ health and well-being. Finally, such theoretical grounding helps predict how to reach identified goals.
Limitations and future directions
Although the identified dimensions of trust provide evidence for a broader conceptual foundation than in previous healthcare research, we recognize limitations in our study. First, written reflections came primarily from women working in early careers in primary healthcare and may be limited in the extent to which they represent men’s views or the views of non-binary identifying healthcare clinicians. Second, data come from an urban healthcare clinic in a large Northeastern city in the United States and therefore cannot claim to represent views of other cultures. For example, previous research indicates that trust in physicians in China appears quite low, and that Chinese patients with higher education and medical insurance indicate higher trust in physicians [ 23 ] Future research should elucidate dimensions of trust including nonverbal communication behavior indicative of trust (and mistrust).
Like many, if not most, medical education curricula and programs, the role of trust and the means of cultivating and assessing it are not part of the formal teaching in the residency program from which this sample of residents was drawn. Yet, trust seems to be acknowledged informally in healthcare education as witnessed by the explicit mentions of trust by these residents. Allowing emerging physicians to develop insight into the role of trust in their practice may be an unintended result of this reflective writing requirement. Perhaps the formal exploration of the role of trust in healthcare is an appropriate educational goal for healthcare curricula.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to the fact that the reflective entries come from an educational module and not technically a data set, but are available from the corresponding author on reasonable request.
Burgoon J, Dunbar N, Subrahmanian V. An integrated spiral model of trust. Terrorism, security, and computation. New York, NY: Springer International Publishing; 2021. 11–34.
Google Scholar
O’Reilly-Jacob M, Vicini A, Duggan A. Ethical considerations of telehealth: Access, inequity, trust, and overuse. J Health Ethics. 2022;18(1).
Fugelli P. James Mackenzie lecture. Trust–in general practice. Br J Gen Pract J R Coll Gen Pract. 2001 Jul;51(468):575–9.
Shockley-Zalabak P, Morreale S, Hackman M. Building the high trust organization: strategies for supporting five key dimensions of trust. San Francisco, CA: Jossey-Bass; 2010.
Tarrant C, Dixon-Woods M, Colman AM, Stokes T. Continuity and trust in primary care: a qualitative study informed by game theory. Ann Fam Med. 2010 Sep;8(5):440–6.
Bennett M. Should I do as I’m told? Trust, experts, and COVID-19. Kennedy Inst Ethics J. 2020;30(3):243–63.
Article Google Scholar
Thom D, Wong S, Guzman D, Wu A, Penko J, Miaskowski C, et al. Physician trust in the patient: development and validation of a new measure. Ann Fam Med. 2011 Apr;9(2):148–54.
Shaughnessy AF, Vaswani A, Andrews BK, Erlich DR, D’Amico F, Lexchin J, et al. Developing a clinician friendly tool to identify useful clinical practice guidelines: G-TRUST. Ann Fam Med. 2017 Sep;15(5):413–8.
Linzer M, Neprash H, Brown R, Williams E, Audi C, Poplau S, et al. Where trust flourishes: perceptions of clinicians who trust their organizations and are trusted by their patients. Ann Fam Med. 2021 Nov;19(1):521–6.
Wei D, Xu A, Wu X. The mediating effect of trust on the relationship between doctor-patient communication and patients’ risk perception during treatment. PsyCh J. 2020 Jun;9(3):383–91.
Bonds DE, Camacho F, Bell RA, Duren-Winfield VT, Anderson RT, Goff DC. The association of patient trust and self-care among patients with diabetes mellitus. BMC Fam Pract 2004 Nov 16;5:26.
Fritz Z, Holton R. Too much medicine: not enough trust? J Med Ethics. 2019 Jan;45(1):31–5.
Birkhäuer J, Gaab J, Kossowsky J, Hasler S, Krummenacher P, Werner C, et al. Trust in the health care professional and health outcome: a meta-analysis. PLoS ONE. 2017;12(2):e0170988.
Article PubMed PubMed Central Google Scholar
Kraetschmer N, Sharpe N, Urowitz S, Deber RB. How does trust affect patient preferences for participation in decision-making? Health Expect Int J Public Particip Health Care Health Policy. 2004 Dec;7(4):317–26.
Thomas DR. A General Inductive Approach for analyzing qualitative evaluation data. Am J Eval. 2006 Jun;27(2):237–46.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004 Feb;24(2):105–12.
Kennedy TJT, Lingard LA. Making sense of grounded theory in medical education. Med Educ. 2006 Feb;40(2):101–8.
Alharahsheh HH, Pius A. A review of key paradigms: Positivism VS interpretivism. Glob Acad J Humanit Soc Sci. 2020;2(3):39–43.
Dowling M. Approaches to reflexivity in qualitative research. Nurse Res. 2006;13(3):7–21.
Article PubMed Google Scholar
Gu L, Tian B, Xin Y, Zhang S, Li J, Sun Z. Patient perception of doctor communication skills and patient trust in rural primary health care: the mediating role of health service quality. BMC Prim Care. 2022 Sep;29(1):255.
Lessig L. Institutional corruption” defined. J Law Med Ethics. 2013;41(3):553–5.
Davey A, Asprey A, Carter M, Campbell JL. Trust, negotiation, and communication: young adults’ experiences of primary care services. BMC Fam Pract. 2013 Dec;30:14:202.
Li C, Khan MM. Public trust in physicians: empirical analysis of patient-related factors affecting trust in physicians in China. BMC Prim Care 2022 Aug 30;23(1):217.
Download references
Acknowledgements
Not applicable.
This project received funding from the Boston College Schiller Institute for Integrated Science and Society.
Author information
Authors and affiliations.
Department of Family Medicine, Tufts University School of Medicine, Boston, MA, USA
Allen F. Shaughnessy & Ashley P. Duggan
Theology Department, Boston College, 140 Commonwealth Ave, Chestnut Hill, MA, USA
Andrea Vicini, SJ
William F. Connell School of Nursing, Boston College, 140 Commonwealth Ave, Chestnut Hill, MA, USA
Monica O’Reilly-Jacob
Undergraduate Student, Boston College, 140 Commonwealth Ave, Chestnut Hill, MA, 02467, USA
Mary Zgurzynski
Communication Department, Boston College, 140 Commonwealth Ave, Chestnut Hill, MA, USA
Ashley P. Duggan
You can also search for this author in PubMed Google Scholar
Contributions
AD, AS, AV, and MZ analyzed and interpreted the clinician data and drafted and edited the manuscript. MOJ interpreted the clinician data and drafted and edited the manuscript. All authors reviewed the manuscript.
Corresponding author
Correspondence to Ashley P. Duggan .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Shaughnessy, A.F., Vicini, SJ, A., Zgurzynski, M. et al. Indicators of the dimensions of trust (and mistrust) in early primary care practice: a qualitative study. BMC Prim. Care 24 , 150 (2023). https://doi.org/10.1186/s12875-023-02098-2
Download citation
Received : 30 August 2022
Accepted : 03 July 2023
Published : 20 July 2023
DOI : https://doi.org/10.1186/s12875-023-02098-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Qualitative
- Primary care
- Resident physicians
- Family medicine
- Reflective writing
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]
- Open access
- Published: 20 June 2023
Trustworthy management in hospital settings: a systematic review
- Andreea Isabela Varga 1 ,
- Ivan Spehar 1 , 2 &
- Helge Skirbekk 1 , 3
BMC Health Services Research volume 23 , Article number: 662 ( 2023 ) Cite this article
2098 Accesses
2 Altmetric
Metrics details
Trustful relationships play a vital role in successful organisations and well-functioning hospitals. While the trust relationship between patients and providers has been widely studied, trust relations between healthcare professionals and their supervisors have not been emphasised. A systematic literature review was conducted to map and provide an overview of the characteristics of trustworthy management in a hospital setting.
We searched Web of Science, Embase, MEDLINE, APA PsycInfo, CINAHL, Scopus, EconLit, Taylor & Francis Online, SAGE Journals and Springer Link from database inception up until Aug 9, 2021. Empirical studies written in English undertaken in a hospital or similar setting and addressed trust relationships between healthcare professionals and their supervisors were included, without date restrictions. Records were independently screened for eligibility by two researchers. One researcher extracted the data and another one checked the correctness. A narrative approach, which involves textual and tabular summaries of findings, was undertaken in synthesising and analysing the data. Risk of bias was assessed independently by two researchers using two critical appraisal tools. Most of the included studies were assessed as acceptable, with some associated risk of bias.
Of 7414 records identified, 18 were included. 12 were quantitative papers and 6 were qualitative. The findings were conceptualised in two categories that were associated with trust in management, namely leadership behaviours and organisational factors. Most studies (n = 15) explored the former, while the rest (n = 3) additionally explored the latter. Leadership behaviours most commonly associated with employee’s trust in their supervisors include (a) different facets of ethical leadership, such as integrity, moral leadership and fairness; (b) caring for employee’s well-being conceptualised as benevolence, supportiveness and showing concern and (c) the manager’s availability measured as being accessible and approachable. Additionally, four studies found that leaders’ competence were related to perceptions of trust. Empowering work environments were most commonly associated with trust in management.
Conclusions
Ethical leadership, caring for employees’ well-being, manager’s availability, competence and an empowering work environment are characteristics associated with trustworthy management. Future research could explore the interplay between leadership behaviours and organisational factors in eliciting trust in management.
Peer Review reports
Trustful relationships between professionals are an important quality of both successful organisations and well-functioning hospitals [ 1 , 2 ]. Professional workers in high-trust organisations are happier, more productive, have more energy, collaborate better, and are more loyal to their organisations than people working in low-trust companies [ 2 ]. Studies in hospital settings seem to indicate similar findings. In Taylor & al.’s [ 1 ] systematic review study of factors and strategies associated with high performing hospitals, trustful relationships was found to be one of the more important factors. High performing hospitals demonstrated respectful and valued relations between staff members [ 3 , 4 ].
The phenomenon of trust has been widely studied. A commonly used definition is Mayer, Davis and Schoorman’s (1995) definition of trust as the “willingness of a party to be vulnerable to the action of another party based on the expectation that the other will perform a particular action important to the trustor, irrespective of the ability to monitor or control that other party” [ 5 ]. Within the healthcare sector, the published literature has explored many facets of trust, such as trust in healthcare in general [ 6 , 7 , 8 ], trust between patients and providers [ 9 , 10 , 11 ], trust between healthcare providers [ 12 , 13 ] and trust between healthcare providers and their supervisors [ 14 , 15 ].
Studies have showed that trust is important in relations between healthcare professionals and patients. Patient trust has an impact on patient satisfaction, adherence, and continued enrolment [ 16 , 17 , 18 , 19 ]. Trust is also highly important for the level of openness in communication between doctors and patient [ 20 ]. According to many theoretical approaches to the study of trust, a central aspect of trust relationships is the trustor’s lack of precautionary measures against the trustee [ 21 , 22 , 23 ]. Patients are vulnerable because of their illness, and the asymmetrical knowledge of medicine [ 24 , 25 , 26 ].
McCabe and Sambrook [ 27 ] studied the antecedents, attributes and consequences of trust between nurses and nurse managers. In terms of consequences, when trust was “high” there were positive outcomes such as professionalism, efficiency and a high quality patient care delivered; while the contexts where trust was low or lacking, led to negative effects such as conflict, absenteeism and turnover; reduced levels of teamwork, patient care quality, support, delegation and efficiency; and increased levels of work-related stress and surveillance [ 27 ].
These very different studies point in divergent directions. We understand that trust is often associated with positive outcomes for both patients and healthcare professionals. But we lack a systematic review of trust between healthcare providers and their supervisors. A handful of systematic literature reviews focused on patients’ trust in their healthcare providers [ 10 , 28 , 29 ], and one reviewed literature on healthcare professionals’ trust in patients [ 11 ]. In terms of trust relations between healthcare professionals and their supervisors, one systematic review explored how motivation is influenced by such relationships [ 13 ]. However, there is a lack in the overview of the published literature on what characterises this trust relationship between employees and their supervisors within a hospital setting.
Given this gap in knowledge, we aim to study the trust relationships, or lack thereof, between healthcare staff and their supervisors by conducting a systematic review that will map and provide an overview of the published literature on this topic. We want to study:
What are the characteristics of trustworthy and/or untrustworthy management, be it culture of sharing, management style and tools, manager characteristics, etc; in a hospital or a similar setting such as wards or large general/family practices?
Search strategy
Seven databases (Web of Science, Embase, MEDLINE, APA PsycInfo, CINAHL, Scopus and EconLit) and three publisher platforms (Taylor & Francis Online, SAGE Journals and Springer Link) were searched systematically to find eligible records. These sources were searched based on the relevance of the fields they covered to the subject of this review, such as medicine, social sciences, nursing and allied health and healthcare policy and management.
The search strategy used to identify relevant records was developed over the course of nine months. The final structure of the search strategy was the product of an iterative process which involved testing of different variations of the search strategy, and discussions among the authors and experts on systematic reviews. The input of an expert in running searches, a university librarian, was sought in order to reach a sound search strategy.
The search strategy has three components and has the following structure: 1) “hospital(s)” OR “ward(s)” AND 2) “health care professional(s)” OR “doctor(s)” OR “nurse(s)” OR “leader(s)” OR “manager(s)” AND 3) “trust” OR “reliance” OR “credibility”. The first component filters by the setting this review is focused on, namely hospitals. The second component establishes the actors/stakeholders within a hospital and is captured by the terms listed above and their synonyms. The third component represents the interaction or relationship between the actors and is linked to the search strategy with a proximity operator. Proximity operators were also used for some of the terms in the second component of the search strategy in order to make the strategy more specific, like “(healthcare NEAR/x professional$)”. Where applicable, the searches were limited to English language.
The detailed search strategy can be found in an additional file [see Additional file 1 ]. The final search was carried out on the 9th of August 2021.
Eligibility criteria
For records to be included in this review, several inclusion criteria were applied. Firstly, in terms of context and participants, eligible studies had to be undertaken in a hospital setting or similar settings where healthcare professionals and managers are present and patients are being treated. Secondly, related to topic, studies should have addressed and explored aspects relevant to the relationship of trust / trustworthiness of subordinates with their higher-ups. Thirdly, eligible records should be of empirical nature. Initially there was no exclusion based on study design; this criterion was later changed in the full-text screening review, as systematic reviews were excluded. However, this criterion remained broad as this review aimed to identify studies of qualitative, quantitative and mixed designs. This was motivated by our purpose to capture, on one hand, the objectiveness that quantitative studies offer on the topic, and on the other to capture the in-depth understanding that qualitative studies provide. Lastly, articles should be written in English. No limit on the year of publication was imposed.
Record selection
The processes of identification, screening and inclusion are depicted in Fig. 1 . Flow diagram.
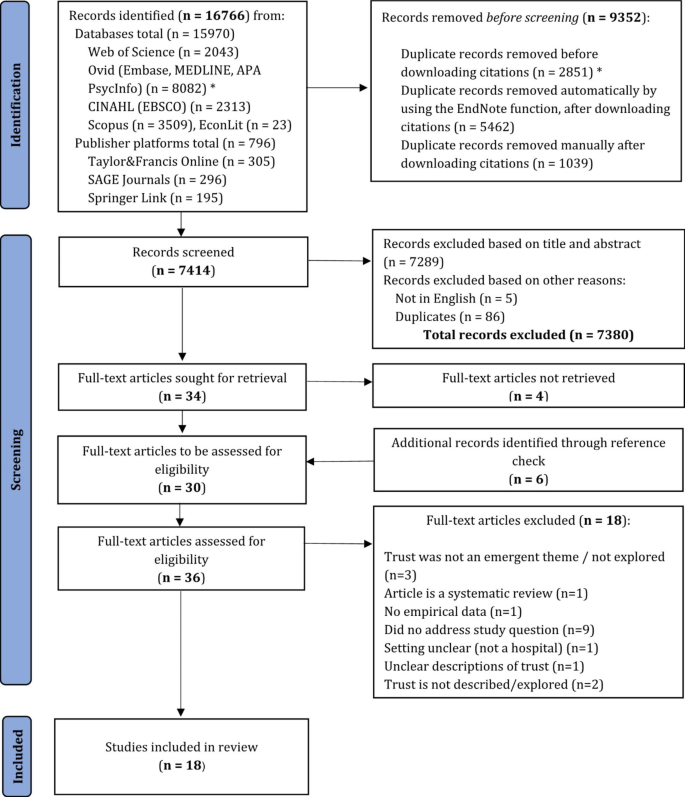
Flow diagram. * The Ovid platform provided the option of removing duplicates from the records identified before downloading the citations, as the search was performed in multiple databases at once. Adapted from Page, McKenzie [ 30 ]
The search resulted in a total of 16,766 records, 15,970 from databases searches and 796 from publisher platforms. Then 9352 duplicate records were removed before the screening process. More specifically, 2851 duplicates were removed before the citations were downloaded. These come from the search conducted in the Ovid platform, which allowed deduplication for the search performed in multiple databases (Embase, MEDLINE and APA PsycInfo) at once.
After the citations were downloaded and imported in the EndNote X9 reference manager, 5462 duplicates were automatically identified by the reference manager. An additional 1039 duplicates were identified manually and removed. Thus, after all duplicates were removed, a total of 7414 records were screened.
The first half and second half were independently screened by two researchers. IS and AIV screened the first half, while HS and AIV screened the second half. The screening comprised of scanning the titles and abstracts. A total of 7380 records were removed; 7289 did not meet the inclusion criteria, based on title and abstract, 5 records were not written in English and an additional 86 duplicate records were found. The 47 remaining publications were discussed by all three researchers, with a focus on the ones that we were in disagreement over. The discussions resulted in 2 records out of the 15 previously agreed upon to be excluded and 21 publications out of the 32 were agreed to be included in the full-text review. Thus, a total of 34 publications were sought for retrieval.
30 records were retrieved. For four records, a full-text version could not be retrieved. The authors of these papers were contacted through Research Gate, but no reply was given. An additional number of 6 papers were identified through reference check of the included records. These were retrieved, and a final number of 36 full-text articles were assessed for eligibility.
The full-text review was performed independently by all authors, and 18 articles met the inclusion criteria. The rest (n = 18) were excluded based on the reasons listed in Fig. 1 . The list of the excluded papers can be found under Additional file 2 .
Data analysis and synthesis
Given the descriptive nature of this review’s research question, and the inclusion of papers with different research designs (both qualitative and quantitative), a narrative approach to data analysis and synthesis was adopted. This entailed developing textual and tabular summaries of findings, which were then used to synthesise the findings under two separate sets of factors.
Data extraction was performed by one researcher (AIV) and checked for correctness by another (IS), and comprised of three categories. The first one relates to details about the included studies: author(s), year of publication, aim(s), methodology (design, setting, participants and sample, instrument and measured concepts, data analysis) and country. The detailed summary of included studies can be found under Additional file 3 . The second category comprises of results relevant to the research question and the concept of trust extracted from quantitative studies, such as hypotheses and whether they were supported or not. The extracted data for the second category is available under Additional file 4 . And the third category similarly gathered results pertinent to the research question from qualitative studies, such as themes identified by the authors of the included studies and their interpretations of supporting evidence quoted from interviews. The extracted data included in this category can be found under Additional file 5 .
Once all the data was extracted, based on his experience in the field of leadership, management and organisations, IS observed patterns in the results. More specifically, characteristics of trustworthy management were noticed to fit under two categories, namely leadership behaviours and organisational factors. IS then summarised and categorised the results into the two classifications. These summaries were presented and discussed with the two other authors during the process. All authors agreed that the summaries were representative of the original findings. The summaries were presented as tables in the results section.
The results section firstly described the study characteristics, then laid out common aspects identified between the qualitative and quantitative studies included in the review. The common aspects related to trust and ethics, trust and well-being, trust and availability and trust and competence. Aspects not common between the quantitative and qualitative studies were presented separately.
All included studies were critically appraised by two researchers. The qualitative studies (n = 6) were assessed by HS and AIV using the JBI Critical appraisal checklist for qualitative research [ 31 ] and the quantitative studies were appraised by IS and AIV using an adapted checklist by the National Institute for Health and Clinical Excellence (NICE) for a questionnaire study [ 32 ]. The NICE checklist did not provide response options, and in order to be consistent, we decided to use the ones from the JBI checklist (Yes, No, Unclear and Not applicable). The overall appraisal scale published by Roever [ 33 ] was used to rate the overall methodological quality of the studies included in this review. The results of the critical appraisal were used to provide an overall picture over the quality of the included studies and to determine whether there were any papers of poor quality, with significant flaws that would determine their exclusion from this review.
Research methods, setting and participants, journals and countries
Tables 1 and 2 lay out the summaries of the quantitative and qualitative included studies in a concise manner. The majority of the studies used a quantitative research design (n = 12), in which surveys (n = 5) and questionnaires (n = 7) were self-administered. With two exceptions, studies (n = 11) collected the data at one point in time. The first exception is a study in which the data was gathered sequentially; with two weeks between the collection of demographic, independent and dependent variables. And the second exception is a study that had a three-week follow-up, but no details are presented. The rest of the included studies had a qualitative design (n = 6); two of which solely collected data through interviews, while the rest (n = 4) used a combination of interviews, focus groups, document reviews or observations such as participant observations, facility audits and research memos.
In terms of setting, studies took place in hospitals (n = 12), hospitals and clinics (n = 3), cancer treatment facilities (n = 1), primary health centres that include inpatient departments (n = 1) and an early psychosis intervention (EPI) clinic (n = 1). Some of the quantitative studies were conducted from the perspective of healthcare employees (nurses and nursing staff) (n = 6), other studies focused on the perspective of employees in management, specialist or administrative positions (n = 3) and three studies included both perspectives. Similarly, one qualitative study captured the perspective of healthcare workers and key-informants, two studies described the management perspective and the rest (n = 3) included both.
Several studies (n = 6) were published in journals that include the healthcare field, such as leadership and management-oriented journals (n = 2), human resources journals (n = 2), industrial psychology (n = 1) and social behaviour (n = 1). While the rest (n = 12) were published in journals covering the healthcare area specifically. The journals were related to management (n = 2), policy and planning (n = 1), leadership (n = 3) and social science and medicine (n = 1) in a general sense, while a handful of studies were published in journals related to nursing specifically (administration and management) (n = 6).
Most of the studies were conducted in the Americas, namely USA (n = 3), Canada (n = 3) and Brazil (n = 1). Then other studies were conducted in European countries, more specifically Italy (n = 2), Poland (n = 1), Portugal (n = 1) and Sweden (n = 1) and the UK (n = 1). Four studies were conducted in countries on the African continent such as South Africa (n = 2), Nigeria (n = 1) and Zambia (n = 1); and one study was conducted in China.
Common aspects
This section firstly describes the two categories that were found to be associated with trust in management, namely leadership behaviours and organisational factors. Then, under the first category, four common aspects across both quantitative and qualitative papers are presented and can be seen under Table 3 .
Most of the studies explored leadership behaviours associated with trust in management only (n = 10)[ 15 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ]. While five studies described characteristics related to both leadership behaviours and organisational factors that were associated with trust in management [ 27 , 43 , 44 , 45 , 46 ]. Additionally, three studies explored organisational factors exclusively [ 47 , 48 , 49 ].
The common aspects are: trust and ethics, trust and well-being, trust and availability and trust and competence and were informed by the following leadership behaviours most commonly related to employees’ trust in their supervisor: different facets of ethical leadership (n = 5), caring for employees’ well-being (n = 5), the manager’s availability (n = 4) and leaders’ competence (n = 4). Each aspect and the studies that informed them are presented below.
Trust and ethics
This first aspect was informed by five studies, two qualitative papers [ 15 , 41 ] and three quantitative studies [ 34 , 36 , 37 ]. The different aspects of ethical leadership that were addressed included integrity [ 15 , 37 ], moral leadership [ 34 ], fairness [ 41 ], and ethical leadership, specifically [ 36 ].
Cregård and Eriksson investigated physician-managers’ and nurse-managers’ perceptions of other physicians’ trust in them; and revealed that trust is strengthened by physician-managers’ understanding of “healthcare issues from various perspectives”, but can decrease when physician-managers are “unable to prioritize both managerial and medical issues” or “fulfil professional demands” ([ 15 ], Table I. p.287).
In Topp and Chipukuma’s interview study [ 41 ], healthcare workers perceived their supervisors in charge of overall or departmental sites to be unfair and inconsistent, for example when selecting staff for workshops or trainings; which contributed to weak trust.
Results from survey studies showed that employee’s affective trust in their direct leaders was positively related to their moral leadership [ 34 ]; and that staff nurses’ trust in their ward/unit leader or immediate supervisor was in a positive relationship with ethical leadership [ 36 ].
Trust and well-being
One qualitative study [ 15 ] and four survey studies [ 37 , 43 , 44 , 46 ] informed the second aspect. Caring for employees’ well-being included measures of benevolence [ 15 , 37 ], supportiveness [ 46 ] and showing concern (one of five dimensions of empowering leadership in Bobbio et al.’s [ 44 ] study). In Araujo and Figueiredo’s study, trust was measured with five items, including: “The superiors care about my well-being at work” ([ 43 ], Table II.).
The qualitative study informing this aspect showcases that physician- and nurse-managers perceive that other physician’s trust in them is increased when the physician-manager shows care towards “patients, colleagues and other healthcare professionals” ([ 15 ], Table I. p.287).
In Wong and Cummings’s study [ 46 ], clinical (such as nurses, pharmacists, doctors and other professionals) and non-clinical employees (administrative, support and research staff) completed a survey with regards to trust in management; and the results were reported separately for the two samples. Supportiveness, as part of the leadership behaviour latent concept developed for the model that was tested in the study, had a significant indirect effect on trust in management among the clinical sample of employees ([ 46 ], p.14).
Trust and availability
This third aspect was developed based on two qualitative papers [ 27 , 38 ] and two quantitative papers [ 43 , 46 ]. The manager’s availability was measured as being accessible [ 43 ] and approachable [ 46 ]. McCabe and Sambrook [ 27 ] found that nurse managers who were considered accessible, approachable and involved were more likely to be trusted by nurses. The opposite was true for managers who were “perceived as ‘inaccessible’, ‘removed’ or those managers higher up within the organisational hierarchy” ([ 27 ], p. 821). In Freysteinson et al.’s [ 38 ] study, availability relates to leaders’ efforts to maintain a visible and accessible leadership presence (with emphasis on face-to-face interaction with the staff).
In Araujo and Figueiredo’s study, another one of the five items that measured trust relates to: “My superiors are accessible and open to dialogue” ([ 43 ], Table II.). In Wong and Cummings’s study [ 46 ], another of the leadership behaviours, relational transparency, had a direct and significant influence on perceptions of trust in management, but only among the non-clinical sample of employees. There were no other direct significant effects between leadership behaviours and trust in management ([ 46 ], p. 14 and 16); making this study the only one included in this review that found mixed or no results for relationships between leadership behaviours and trust.
Trust and competence
Three qualitative papers [ 15 , 27 , 41 ] and one quantitative study [ 37 ] informed this last aspect. The studies found that leaders’ competence, in terms of knowledge [ 37 ], medical competence [ 15 ] and decision making skills [ 27 , 41 ], were related to perceptions of trust.
The physician-manager’s medical competence, on one side, was deemed “valuable when managerial healthcare decisions are required” and the participants (physician- and nurse-managers) perceived this as a factor that increased trust in the physician-manager ([ 15 ], Table I. p.287). On the other side, the participants also perceived that “physician-managers should have extensive involvement in medical practice” in order to maintain competence in daily medical work ([ 15 ], Table I. p.287).
Organisational factors
One qualitative study [ 27 ] and seven quantitative studies [ 43 , 44 , 45 , 46 , 47 , 48 , 49 ] studied organisational factors associated with trust. Work environments in which employees experienced empowerment (n = 4) [ 43 , 45 , 47 , 48 ] were most commonly associated with trust in management. Salary, workload and administrative support was also related to trust in one study [ 46 ]. In the qualitative study [ 27 ], the authors found that antecedents of trust converged mainly on organisational factors such as immediate work environment, communication systems and new management practices.
Quantitative studies
The quantitative studies had different conceptualisations and measures of trust. Some studies measured trust as a one-dimensional concept, e.g. “trust in leader” [ 36 ] and “trust in supervisor” [ 49 ]. Other studies measured trust as a multi-dimensional concept. For example, in da Costa Freire and Azevedo’s [ 47 ] study, trust was operationalised as “perceptions of trustworthiness in the supervisor”, and measured on three dimensions (integrity, benevolence and ability). Laschinger, Finegan [ 48 ] separated trust into subscales measuring faith in the intentions of managers and confidence in managers’ actions. One study [ 43 ] conceptualised trust as one of nine dimensions related to internal climate at work.
Variations in the type of trust relationships investigated were also observed. For example, Bai et al. [ 34 ] studied general employees’ affective trust in their direct leaders. Bobbio et al. [ 44 ] and Bobbio and Manganelli [ 45 ] focused on nursing staff’s trust in leader (nurse manager in this case) and trust in the organisation; and similarly, another study [ 36 ] specified that nursing staff’s trust in leaders was understood as trust in their ward/unit leader or immediate supervisor. Additionally, one study [ 35 ] investigated workplace trust which was comprised of trust in organisation, trust in immediate supervisor and trust in co-workers.
Qualitative studies
Among the six qualitative studies, four studies explored trust explicitly in the research aim [ 15 , 27 , 40 , 41 ], while two studies identified trust as an emerging factor in the data analysis [ 38 , 42 ].
In two of the qualitative studies [ 15 , 38 ], trust was explored through managers’ own perspectives. Cregard and Eriksson [ 15 ] interviewed and conducted focus groups with physician managers and nurse-managers, with the aim of exploring trust in relation to physicians’ dual roles as managers and clinicians. According to the managers, aspects related to competence, benevolence, and integrity could influence physician employees’ trust in physician-managers. Difficulties related to combining the managerial and medical role was also described as a common reason for decreased trust. Freysteinson and colleagues [ 38 ] interviewed nursing leaders in American hospitals about their leadership experiences under the COVID-19 pandemic. The authors describe how the leaders became aware of face-to-face interaction as crucial to earning the trust of the employees, and that “leaders felt transparency increased trust” (p.1539). While the findings from these two studies were gathered from the lens of managers themselves, they are consistent with findings from other studies in our review.
Critical appraisal
Table 4 presents the assessment of risk of bias for each paper included in the review.
Out of the six qualitative papers assessed, most of them (n = 4) were rated as acceptable; while one paper was rated between acceptable and low quality and one paper as high quality. The majority of the quantitative papers (n = 10) were rated as acceptable and the rest (n = 2) were rated as high quality. Thus, most papers included in this study were assessed as acceptable. No study was excluded based on quality, as none were rated as poor (0).
Summary of findings
This systematic literature review aimed to provide an overview of the published literature over the characteristics of the trust relationship between employees and their supervisors within a hospital setting. Based on the included studies, these characteristics were categorised under two aspects: leadership behaviours and organisational factors associated with trust in management. Most studies explored leadership behaviours, and thus some common aspects emerged between the qualitative and quantitative papers. The common aspects are: trust and ethics, trust and well-being, trust and availability and trust and competence. These are discussed below.
Five included articles emphasised different aspects of ethical leadership for trust relationships to grow between employee and manager. Integrity, moral leadership, fairness and ethical leadership are mentioned specifically. In clinical studies on relationships between healthcare professionals and patients, it is more common to thematise reciprocity and “being taken seriously as a human being” [ 20 ]. Brown [ 50 ] has claimed that doctors’ standing as caring and competent now depends to a great degree on communication and involvement with the patient before trust can be earned. Showing reciprocal humanity creates common ground with the patient, and this review shows that similar effects play a role between leader and healthcare professionals.
Studies from other industries have also marked the impact ethical leadership has on trust in leader. For example, Newman et al. [ 51 ] showed that in a sample of n = 184 pairs of employees-supervisors from three Chinese firms, ethical leadership lead to higher levels of trust in leader (both cognitive and affective). Similarly, Dadhich and Bhal [ 52 ] found that ethical leadership predicted affective and cognitive trust in a sample of post-graduate engineering students in India.
Several included studies showed a connection between managers’ care for the employees’ well-being and trust relationships. Being available when concerns are voiced, and listening to employees’ worries is important. A survey study on 107 white-collar employees working in various organisations in Malaysia [ 53 ] highlighted that when employees perceived their supervisor to show benevolence, integrity and ability, trust in them was predicted both directly and indirectly. Studies on the trust relationship between healthcare professionals and patients emphasise this characteristic even more clearly, as many studies have focused on how trust is built [ 20 ], and we can see some similarities to how trust is built between healthcare staff and managers. E.g., Skirbekk & al. have shown how relationships between healthcare professionals and patients based on “open mandates of trust” are more resilient [ 19 ]. The findings from the studies included in our study show that managers’ care for employees’ well-being lead to more caring and empowering trust relationships.
Manager’s availability was another leadership characteristic associated with trust in management, as shown by four papers included in this review; and had to do with managers being perceived as accessible and approachable. While there are few studies directly exploring the relationship between a supervisor’s availability and employees’ trust towards the supervisor, some studies from other organisational contexts have indicated that a supervisor’s availability might improve the quality of relations between supervisors and employees, both in physical [ 54 ] and remote work settings [ 55 ].
Four included studies found the leaders’ competence to be an important characteristic for trust relationships. Employees need to be assured that the leaders know what they are doing, or at least that they have a plan for how the hospital should be run. Similarly, Manderson and Warren [ 56 ] have shown how competence is often the most important dimension of trust relations with healthcare professionals. Studies on the doctor-patient relationship in different medical contexts have shown that the better a patient feels informed about the treatment process, the greater trust he or she will experience [ 57 , 58 , 59 , 60 ]. This trust in competence makes it possible for the patients to bridge the knowledge gap [ 24 ] through a “leap of faith” [ 25 , 26 ]. There might be a similar “leap of faith” by health professionals towards their supervisors. Employees can rarely be expected to have knowledge on how hospitals should be run, but it is important for them to be able to trust that the leaders have this competence.
In terms of supervisors’ trustworthiness and competence, hospitals and related settings might place emphasis both on managerial and clinical competence. Studies of healthcare managers have found that doctors in management positions attempt to maintain their clinical competence. For example, Spehar & al. [ 61 ] found that Norwegian doctors in management positions in hospitals placed importance on “being perceived as a competent clinician in order to be taken seriously by the medical staff.“ The authors also found that clinical knowledge was important for “winning” arguments with the staff. This is in line with arguments by other authors on how doctors in management seek to maintain their clinical knowledge in order to sustain legitimacy among their staff, especially their professional colleagues [ 62 , 63 ].
Trust and culture
Studies have shown that there might be cultural differences in leader expectations and trust. Indeed, words such as «paternalistic», «feminine» and «masculine» are sometimes used to differentiate cultural expectations towards management [ 64 , 65 ]. For example, employees in Western countries might expect a more «feminine», or empowering leadership style, whereas employees in Asian countries might expect a more paternalistic leadership style [ 66 ]. But studies have also shown similarities in expectations across different countries. For example, most employees want managers who are perceived as inspirational, competent and fair [ 67 ].
We have not observed explicit cultural differences in our included studies in terms of trust, although the number of studies included in our analysis might not be conducive to a comprehensive comparison of cultural differences. However, the study by Bai et al. [ 34 ], included in our study, found that authoritarian leadership of direct leaders had positive impacts on employees’ personal initiative. We can therefore not rule out that cultural differences might influence perceptions of trustworthiness.

Methodological considerations
The fact that only one author extracted the data and no standardised data extraction form was used, could pose as a risk of error. This risk was reduced, as another author checked the correctness of the extracted data. Another drawback of this systematic literature review is that it was not registered and a formal review protocol was not used in guiding how this review was conducted. However, we did follow strict guidelines developed throughout years of experience and discussions with experienced reviewers. The expert knowledge of a librarian was also sought in the process of developing the search strategy. We also discussed conducting a more in-depth synthesis of the 6 qualitative papers, but we decided against it since we found the research questions in the included studies were not homogenous enough. This might be considered a missed opportunity.
Quality of the included papers
14 of the 18 included articles have an acceptable quality. According to the rating scale we used [ 33 ], this means that most criteria were met but there are “some flaws in the study with an associated risk of bias”. For the qualitative studies rated as acceptable (n = 4), the associated risk of bias mostly arises from studies not locating the researcher culturally or theoretically, and not addressing the influence of the researcher on the research. For the quantitative studies rated as acceptable (n = 10), the associated risk of bias arose mostly from studies being unclear regarding whether the sampling frame was sufficiently large and representative; and somewhat from studies not discussing potential response biases. One qualitative paper was evaluated as having a quality between acceptable and low. An associated risk of bias stemmed from the study not locating the researcher culturally or theoretically and not discussing his/her influence on the research. The reason for leaning towards rating this paper low quality is the study failing to provide a statement on whether ethical approval by an appropriate body was granted.
Although the quality of the included quantitative papers was acceptable, and high in two cases, the use of surveys and questionnaires to capture an abstract concept such as trust can be viewed as a limitation. However, claims for the validity and reliability of the instruments used have been made and were justified in all papers, except for three, where the claims related to validity were unclear.
Conclusion and future research
The aim of our study was to provide an overview of the existing literature related to characteristics of trustworthy management. We found that most of the studies explored leadership behaviours associated with trust in management. Leadership behaviours related to ethical leadership and caring for employees’ well-being were the most prominent in these studies. Based on our review, we present the following main suggestions for future research.
Firstly, based on the findings from the included studies, both leadership behaviours and organisational factors appear to be related to trust in management. However, these are not clearly distinct dimensions. For example, individual managers might positively or negatively influence employees’ perceptions of the work environment. Likewise, the work environment or organisational culture might influence individual leaders’ behaviours. Therefore, there is likely an interplay between factors in the work environment and individual leadership behaviours. More research is needed to untangle these relationships.
Secondly, we did not seek to explore whether certain leadership behaviours or organisational factors were more or less important in eliciting trust in management. The included studies did not explicitly aim to delineate such “hierarchies”. Future systematic review studies could explore possible causal relationships between leadership behaviours and organisational factors on employees’ trust in management.
Thirdly, the studies in our review explored characteristics of trustworthiness in formal managers. Informal leaders may also have a prominent role in some healthcare settings, but we cannot infer that the same characteristics will be relevant for understanding perceptions of trustworthiness in informal leaders. This is an aspect that could be researched further.
Lastly, only one study in our review reported results from two different samples (clinical and non-clinical workers). Future studies could investigate differences and similarities in how different employees in a medical setting (such as clinicians and non-clinicians) or healthcare professionals (such as nurses compared to physicians) view trustworthy management.
Data availability
All relevant data are within the paper and its attached Additional files.
Abbreviations
Oslo Metropolitan University
University of Oslo
National Institute for Health and Care Excellence
Early Psychosis Intervention
structural equation modelling
Taylor N, Clay-Williams R, Hogden E, Braithwaite J, Groene O. High performing hospitals: a qualitative systematic review of associated factors and practical strategies for improvement. BMC Health Serv Res. 2015;15(1):244.
Article PubMed PubMed Central Google Scholar
Zak PJ. The neuroscience of Trust. Management behaviors that foster employee engagement. Harvard Business Rev. 2017(Jan-Feb).
Bradley EH, Curry LA, Webster TR, Mattera JA, Roumanis SA, Radford MJ, et al. Achieving rapid door-to-balloon times: how top hospitals improve complex clinical systems. Circulation. 2006;113(8):1079–85.
Article PubMed Google Scholar
Landman AB, Spatz ES, Cherlin EJ, Krumholz HM, Bradley EH, Curry LA. Hospital collaboration with emergency medical services in the care of patients with acute myocardial infarction: perspectives from key hospital staff. Ann Emerg Med. 2013;61(3):185–95.
Mayer RC, Davis JH, Schoorman FD. An integrative model of organizational trust. Acad Manage Rev. 1995;20(3):709–34.
Article Google Scholar
Calnan M, Rowe R. Trust and Health Care. Sociol Compass. 2007;1(1):283–308.
Calnan MW, Sanford E. Public trust in health care: the system or the doctor? Qual Saf Health Care. 2004;13(2):92–7.
Article CAS PubMed PubMed Central Google Scholar
Gilson L. Trust in health care: theoretical perspectives and research needs. J Health Organ Manag. 2006;20(5):359–75.
Murray B, McCrone S. An integrative review of promoting trust in the patient–primary care provider relationship. J Adv Nurs. 2015;71(1):3–23.
Brennan N, Barnes R, Calnan M, Corrigan O, Dieppe P, Entwistle V. Trust in the health-care provider–patient relationship: a systematic mapping review of the evidence base. Int J Qual Health Care. 2013;25(6):682–8.
Sousa-Duarte F, Brown P, Mendes AM. Healthcare professionals’ trust in patients: a review of the empirical and theoretical literatures. Sociol Compass. 2020;14(10):e12828.
Sutherland BL, Pecanac K, LaBorde TM, Bartels CM, Brennan MB. Good working relationships: how healthcare system proximity influences trust between healthcare workers. J Interprof Care. 2021:1–9.
Okello DRO, Gilson L. Exploring the influence of trust relationships on motivation in the health sector: a systematic review. Hum Resour Health. 2015;13(1):16.
Mullarkey M, Duffy A, Timmins F. Trust between nursing management and staff in critical care: a literature review. Nurs Crit Care. 2011;16(2):85–91.
Cregård A, Eriksson N. Perceptions of trust in physician-managers. Leadersh Health Serv (Bradf Engl). 2015;28(4):281–97.
Anderson LA, Dederick RF. Development of the trust in physician scale: a measure to assess interpersonal trust in patient-physician relationships. Psychol Rep. 1990;67.
Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Q. 2001;79(4).
Safran D, Kosinski M, Tarlov, Rogers, Taira L et al. The Primary Care Assessment Survey: tests of Data Quality and Measurement Performance. Med Care. 1998;36.
Thom DH, Hall MA, Pawlson LG. Measuring patient’s trust in physicians when assessing quality of care. Health Aff. 2004;23.
Skirbekk H, Middelthon A-L, Hjortdahl P, Finset A. Mandates of Trust in the doctor-patient relationship. Qual Health Res. 2011;21(9):1182.
Grimen H. Gode institusjoners betydning for tillit. In: Skirbekk H, Grimen H, editors. Tillit i Norge. Oslo: Res Publica; 2012.
Google Scholar
Hertzberg L. On the attitude of Trust. Inquiry. 1988;31.
Skirbekk H. Presupposed or negotiated trust? Explicit & implicit interpretations of trust in a medical setting. Med Health Care Philos. 2009;12.
Calnan M, Rowe R. Trust relations in a changing health service. J Health Serv Res Policy. 2008;13(3suppl):97–103.
Möllering G. Trust: reason, routine. Reflexivity: Elsevier; 2006.
Simmel G. The philosophy of money. London: Routledge; 1978.
McCabe TJ, Sambrook S. The antecedents, attributes and consequences of trust among nurses and nurse managers: a concept analysis. Int J Nurs Stud. 2014;51(5):815–27.
Article CAS PubMed Google Scholar
Birkhäuer J, Gaab J, Kossowsky J, Hasler S, Krummenacher P, Werner C, et al. Trust in the health care professional and health outcome: a meta-analysis. PLoS ONE. 2017;12(2):e0170988.
Rørtveit K, Hansen BS, Leiknes I, Joa I, Testad I, Severinsson E. Patients’ experiences of trust in the patient-nurse relationship-a systematic review of qualitative studies. 2015.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
JBI. Checklist for qualitatie research. Critical appraisal tools for use in JBI Systematic Reviews. 2020.
NICE. Sickle cell Acute painful episode: management of an Acute painful sickle cell episode in Hospital. Guidelines NIfHaCE, editor. Manchester (UK): National Institute for Health and Clinical Excellence (NICE) copyright © 2012, National Institute for Health and Clinical Excellence.; 2012.
Roever L. Critical appraisal of a questionnaire study. Evid Based Med Pract. 2015;1(2):1–2.
Bai S, Lu F, Liu D. Subordinates’ responses to paternalistic leadership according to leader level. Social Behav Personality: Int J. 2019;47(11):1–14.
Coxen L, van der Vaart L, Stander MW. Authentic leadership and organisational citizenship behaviour in the public health care sector: The role of workplace trust. 2016. 2016;42(1).
Enwereuzor IK, Adeyemi BA, Onyishi IE. Trust in leader as a pathway between ethical leadership and safety compliance. Leadersh Health Serv. 2020;33(2):201–19.
Fleig-Palmer MM, Rathert C, Porter TH. Building trust: the influence of mentoring behaviors on perceptions of health care managers’ trustworthiness. Health Care Manage Rev. 2018;43(1):69–78.
Freysteinson WM, Celia T, Gilroy H, Gonzalez K. The experience of nursing Leadership in a Crisis: a hermeneutic phenomenological study. J Nurs Adm Manag. 2021;19.
Stander FW, de Beer LT, Stander MW. Authentic leadership as a source of optimism, trust in the organisation and work engagement in the public health care sector. Sa J Hum Resource Manage. 2015;13(1).
Stasiulis E, Gibson BE, Webster F, Boydell KM. Resisting governance and the production of trust in early psychosis intervention. Soc Sci Med. 2020;253.
Topp SM, Chipukuma JM. A qualitative study of the role of workplace and interpersonal trust in shaping service quality and responsiveness in zambian primary health centres. Health Policy Plan. 2016;31(2):192–204.
Weaver SH, Lindgren TG, Cadmus E, Flynn L, Thomas-Hawkins C. Report from the night shift: how administrative Supervisors achieve nurse and patient safety. Nurs Adm Q. 2017;41(4):328–36.
Araujo CAS, Figueiredo KF. Brazilian nursing professionals: leadership to generate positive attitudes and behaviours. Leadership in health services. (Bradford England). 2019;32(1):18–36.
Bobbio A, Bellan M, Manganelli AM. Empowering leadership, perceived organizational support, trust, and job burnout for nurses: a study in an italian general hospital. Health Care Manage Rev. 2012;37(1):77–87.
Bobbio A, Manganelli AM. Antecedents of hospital nurses’ intention to leave the organization: a cross sectional survey. Int J Nurs Stud. 2015;52(7):1180–92.
Wong CA, Cummings GG. The influence of authentic leadership behaviors on trust and work outcomes of health care staff. J Leadersh Stud. 2009;3(2):6–23.
da Costa Freire CMF, Azevedo RMM. Empowering and trustful leadership: impact on nurses’ commitment. Personnel Rev. 2015;44(5):702–19.
Laschinger HKS, Finegan J, Shamian J, Casier S. Organizational Trust and empowerment in Restructured Healthcare Settings: Effects on Staff Nurse Commitment. JONA: The Journal of Nursing Administration. 2000;30(9):413–25.
Article CAS Google Scholar
Simha A, Stachowicz-Stanusch A. The effects of ethical climates on trust in supervisor and trust in organization in a polish context. Manag Decis. 2015;53(1):24–39.
Brown PR. Trusting in the new NHS: instrumental versus communicative action. Sociol Health Illn. 2008;30(3):349–63.
Newman A, Kiazad K, Miao Q, Cooper B. Examining the cognitive and affective trust-based mechanisms underlying the relationship between ethical leadership and organisational citizenship: a case of the head leading the heart? J Bus Ethics. 2014;123(1):113–23.
Dadhich A, Bhal KT. Ethical leader behaviour and leader-member exchange as predictors of subordinate behaviours. Vikalpa. 2008;33(4):15–26.
Poon JM. Effects of benevolence, integrity, and ability on trust-in‐supervisor. Empl Relations. 2013.
Werbel JD, Lopes Henriques P. Different views of trust and relational leadership: supervisor and subordinate perspectives. J Managerial Psychol. 2009;24(8):780–96.
Connaughton SL, Daly JA. Identification with leader. Corp Communications: Int J. 2004;9(2):89–103.
Manderson L, Warren N. The art of (re) learning to walk: trust on the rehabilitation ward. Qual Health Res. 2010;20(10):1418–32.
Nannenga MR, Montori VM, Weymiller AJ, Smith SA, Christianson TJ, Bryant SC, et al. A treatment decision aid may increase patient trust in the diabetes specialist. The statin choice randomized trial. Health Expect. 2009;12(1):38–44.
Nagrampa D, Bazargan-Hejazi S, Neelakanta G, Mojtahedzadeh M, Law A, Miller M. A survey of anesthesiologists’ role, trust in anesthesiologists, and knowledge and fears about anesthesia among predominantly hispanic patients from an inner-city county preoperative anesthesia clinic. J Clin Anesth. 2015;27(2):97–104.
Hillen MA, De Haes HC, Smets EM. Cancer patients’ trust in their physician—a review. Psycho-oncology. 2011;20(3):227–41.
Conradsen S, Lara-Cabrera ML, Skirbekk H. Patients’ knowledge and their trust in surgical doctors. A questionnaire-based study and a theoretical discussion from Norway. Social Theory & Health. 2021:1–18.
Spehar I, Frich JC, Kjekshus LE. Clinicians in management: a qualitative study of managers’ use of influence strategies in hospitals. BMC Health Serv Res. 2014;14(1):251.
Berg NL, Byrkjeflot H. Management in hospitals. Int J Public Sector Manag. 2014;27(5):379–94.
Mo OT. Doctors as managers: moving towards general management? J Health Organ Manag. 2008;22(4):400–15.
Chen H-Y, Kao HS-R. Chinese paternalistic leadership and non-chinese subordinates’ psychological health. Int J Hum resource Manage. 2009;20(12):2533–46.
Helgstrand KK, Stuhlmacher AF. National culture: an influence on leader evaluations? Int J Organizational Anal. 1999.
Ling W, Chia RC, Fang L. Chinese implicit leadership theory. J Soc Psychol. 2000;140(6):729–39.
Den Hartog DN, House RJ, Hanges PJ, Ruiz-Quintanilla SA, Dorfman PW, Abdalla IA, et al. Culture specific and cross-culturally generalizable implicit leadership theories: are attributes of charismatic/transformational leadership universally endorsed? Leadersh Q. 1999;10(2):219–56.
Download references
Acknowledgements
We are grateful for the help and friendly advice we have received from librarian Pål Magnus Lykkja (UiO) and researcher Marita Sporstøl Fønhus (NK LMH). We would also like to acknowledge the valuable contribution of professor Frode Veggeland (HInn, UiO), with whom we had long discussions that helped shape the research objectives of this review. We are also grateful for the support we have received from UiO and OsloMet for this study.
All authors´ salaries were funded by their host institution. No funding body was involved in preparing the manuscript or the decision to submit the manuscript for publication in BMC Health Services Research.
Author information
Authors and affiliations.
Department of Health Management and Health Economics, Institute of Health and Society, Medical Faculty, University of Oslo (UiO), P.O. Box 1089, Oslo, NO-0317, Norway
Andreea Isabela Varga, Ivan Spehar & Helge Skirbekk
Institute of Psychology, Oslo New University College, Oslo, Norway
Ivan Spehar
Department of Nursing and Health Promotion, Faculty of Health Sciences, Oslo Metropolitan University, Oslo, Norway
Helge Skirbekk
You can also search for this author in PubMed Google Scholar
Contributions
Formulation/identification of the scientific problem and conceptual idea: HS had the conceptual idea. All three authors participated in the development and formulation of the scientific problems. Planning of the experiments and methodology design, including selection of methods and method development: All three authors participated in the development of the methodology. Involvement in data gathering/experimental work and interpretation/analysis: All three authors participated in the gathering and analyses of the data, and all papers were reviewed by at least two authors, but AIV contributed most substantially, as described in the manuscript. Presentation, and discussion of obtained data and work with the manuscript: All three authors participated in the discussion of data. All three authors contributed substantially to the work with the manuscript. AIV and HS wrote the Background section, the Methods section was written by AIV with a contribution by IS, the Results sections was written by AIV and IS with a contribution from HS, the Discussion section was written by all authors and IS wrote the Conclusion section. All authors read and approved the final manuscript. All authors contributed to the revised manuscript.
Corresponding author
Correspondence to Helge Skirbekk .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Additional file 1: Search strategies
Additional file 2: list of excluded papers and reasons, additional file 3: detailed summary of included studies, additional file 4: results from quantitative studies, additional file 5: results from qualitative studies, additional file 6: prisma 2020 checklist, additional file 7: prisma 2020 abstract checklist, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Varga, A.I., Spehar, I. & Skirbekk, H. Trustworthy management in hospital settings: a systematic review. BMC Health Serv Res 23 , 662 (2023). https://doi.org/10.1186/s12913-023-09610-5
Download citation
Received : 29 August 2022
Accepted : 26 May 2023
Published : 20 June 2023
DOI : https://doi.org/10.1186/s12913-023-09610-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Trustworthiness
- Trust relations
- Healthcare professionals
- Management roles
- Systematic review
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
You are using an outdated browser. This page doesn't support Internet Explorer 6, 7 and 8. Please upgrade your browser or activate Google Chrome Frame to improve your experience.
ORIGINAL RESEARCH
Trust in the transplant team associated with the level of chronic illness management—a secondary data analysis of the international bright study.

- 1 Department of Public Health, Faculty of Medicine, Institute of Nursing Sciences, University of Basel, Basel, Switzerland
- 2 College of Nursing, University of Illinois at Chicago, Chicago, IL, United States
- 3 Practice Development and Research Division, Medical Directorate, University Hospital Basel, Basel, Switzerland
- 4 Academic Center for Nursing and Midwifery, Department of Public Health and Primary Care, Faculty of Medicine, KU Leuven, Leuven, Belgium
- 5 School of Nursing and Health Studies, Kansas City, MO, United States
A trustful relationship between transplant patients and their transplant team (interpersonal trust) is essential in order to achieve positive health outcomes and behaviors. We aimed to 1) explore variability of trust in transplant teams; 2) explore the association between the level of chronic illness management and trust; 3) investigate the relationship of trust on behavioral outcomes. A secondary data analysis of the BRIGHT study (ID: NCT01608477; https://clinicaltrials.gov/ct2/show/NCT01608477?id=NCT01608477&rank=1 ) was conducted, including multicenter data from 36 heart transplant centers from 11 countries across four different continents. A total of 1,397 heart transplant recipients and 100 clinicians were enrolled. Trust significantly varied among the transplant centers. Higher levels of chronic illness management were significantly associated with greater trust in the transplant team (patients: AOR= 1.85, 95% CI = 1.47–2.33, p < 0.001; clinicians: AOR = 1.35, 95% CI = 1.07–1.71, p = 0.012). Consultation time significantly moderated the relationship between chronic illness management levels and trust only when clinicians spent ≥30 min with patients. Trust was significantly associated with better diet adherence (OR = 1.34, 95%CI = 1.01–1.77, p = 0.040). Findings indicate the relevance of trust and chronic illness management in the transplant ecosystem to achieve improved transplant outcomes. Thus, further investment in re-engineering of transplant follow-up toward chronic illness management, and sufficient time for consultations is required.
Introduction
The importance of interpersonal trust (i.e., trust between patients and healthcare providers) in the healthcare context has been widely reported [ 1 ]. Trust occurs in vulnerable situations where an individual believes that another individual will act in their best interest [ 2 ]. This is especially true for chronically ill populations such as heart transplanted (HTx) patients. HTx patients face a high level of vulnerability due to potentially life-threatening complications and lifelong dependency on the HTx team providing follow-up care [ 3 ]. Trust has to be understood as a continuum, meaning that it is a complex and evolving phenomenon that can increase or decrease over time. Interpersonal trust relationships are supposed to positively affect patients’ attitudes, experiences (e.g., satisfaction with care [ 4 – 6 ]) and behavior (e.g., increased adherence to medication and treatment [ 6 – 8 ]). Further, trust is linked to patients’ health outcomes [ 2 , 4 , 6 ], health-related quality of life [ 4 ], and symptom-related outcomes [ 4 ].
Several factors are associated with higher interpersonal trust, and either relate to the patient (e.g., patients who are white, women, or older, or those with a better health status or a higher number of healthcare visits) or the physician (e.g., better communication skills, higher competence, or higher consultation time). In addition, service factors, e.g., the type of delivery system, continuity in care, and absence of economic or other pressures, affect patients’ trust in healthcare professionals [ 2 , 7 , 8 ].
While patient and clinician factors have been extensively examined, the relationship between trust and service outcomes—level of chronic illness management (CIM)—remain understudied [ 9 ]. Chronic illness management refers to a comprehensive and coordinated approach that focusses on optimizing the care provided to individuals living with long-term medical conditions. CIM programs based on the Chronic Care Model (CCM) [ 10 ] are designed to transform acute care driven health programs into patient centered integrated care and to address needs of the chronically ill, i.e., continuity of care, behavioral, self-management, and psychosocial support and patient participation [ 11 ]. The CCM is a framework that guides the development of care delivery models for the chronically ill to effectively improve patients’ clinical and behavioral outcomes and to enhance proactive patient and healthcare provider interactions [ 12 ]. Such interactions (e.g., during consultations) require interpersonal trust [ 13 ]. To assess, how well elements of the CCM have been implemented in a specific care program, the level of chronic illness management can be determined. CIM is a construct that can be assessed using validated instruments that allow patients and healthcare professionals to report how they perceive characteristics of clinical care processes [ 14 , 15 ]. The higher the level of CIM, the more CCM elements were implemented. To our knowledge, there is no evidence on the association between CCM-based CIM programs and interpersonal trust, yet it is an important association with regards to teasing out a favorable ecosystem for HTx patients’ follow-up care, i.e., multilevel characteristics of care systems or processes that allow a CIM model of care to be implemented and sustained. Typically, HTx patients are cared for by an interdisciplinary HTx team across the transplant continuum in an HTx center with specific structural and care process characteristics. Studies that focus on interpersonal trust, however, do not consider the context in which these relationships occur. Therefore, this study aimed to 1) explore the variability of interpersonal trust in HTx teams among 36 HTx centers internationally; 2) explore whether the level of CIM of an HTx center is associated with trust in the HTx team; 3) investigate whether meso-level factors (e.g., time spent with the HTx team during follow-up) moderate the relationship between level of CIM and trust in the HTx team, and 4) investigate the relationship of trust in the HTx team on behavioral outcomes ( Figure 1 ).
FIGURE 1 . Conceptual model of studied variables and outcomes. Conceptualization of the Relationship between the Level of Chronic Illness Management (CIM) and Patients’ Interpersonal Trust in the Heart Transplant Team (HTx) on Health and Behavioral Outcomes.
Materials and Methods
Design, setting, and sample.
This study presents a secondary data analysis of the international, multicenter, cross-sectional Building Research Initiative Group: Chronic Illness Management and Adherence in Transplantation (BRIGHT) study (ID: NCT01608477; https://clinicaltrials.gov/ct2/show/NCT01608477?id=NCT01608477&rank=1 ). Detailed study procedures are described elsewhere [ 16 , 17 ]. Briefly, using a multistage sampling approach of HTx centers, clinicians, and patients, CIM practice patterns and multilevel factors related to medication non-adherence were examined in 36 HTx centers from 11 countries across four continents (Europe, North America, South America, and Australia). A minimum of two HTx centers per country were included, if they had performed more than 50 HTx during the past 12–60 months. A convenience sample of 100 clinicians (1–5 per center) was chosen, using a random sample if more than five were eligible who had worked in the center for more than 6 months. Clinicians had to have spent more than 50% of their employment in direct clinical practice and have been familiar with the posttransplant outpatient care at the center. HTx patients (≥18 years of age) followed up in a participating center were included randomly if they were between 1–5 years post-transplant, first and single-organ transplant, able to read, understand and provide written informed consent. Data were collected between March 2012 and October 2015. The study was approved by the ethics committee of the University Hospital Leuven, Belgium and the ethics committees of each participating center. Written informed consent was obtained from all participating patients.
Variables and Measurement
Data were collected from transplant directors, clinicians, and patients who completed a specific self-report BRIGHT questionnaire for each of these samples. In addition, patients’ sociodemographic data were collected during the enrollment interview and their clinical information was extracted from medical records ( Table 1 ).
TABLE 1 . Overview of variables and measurement tools.
Main Outcomes
Trust in the healthcare team was part of the patient questionnaire and adapted from the 10-item Wake Forest University Trust scale measuring the level of interpersonal trust, i.e., fidelity (caring and advocating for the patient’s welfare), competence, honesty, confidentiality, and global trust in the healthcare team [ 18 ]. The three negatively worded items were recoded and an average score was calculated for each patient-participant with a higher overall score (range 1–5) indicating higher trust. Given that the trust variable was not normally distributed, it was dichotomized using the median score for the patient-sample for easier interpretation of interaction terms. Sensitivity analysis was performed using tertiles instead of the median with similar results.
The level of CIM implemented in the HTx program was measured from two perspectives. First, patient-participants completed the 11-item short version of the Patient Assessment of Chronic Illness Care (PACIC) instrument [ 20 ]. This instrument measures specific actions or qualities of care in the delivery system, which are congruent with the CCM and were observed over a recall period of 6 months. The items were aggregated for each patient-participant, with the total score ranging from 11 to 55. Higher scores indicate a higher degree of CIM. The median score of the patient-sample was used to dichotomize the PACIC variable. Second, implementation of CIM was measured from the clinician’s perspective by applying the investigator-developed CIMI-BRIGHT clinician questionnaire (The Chronic Illness Management Implementation—Building Research Initiative Group: Chronic Illness Management and Adherence in Transplantation (CIMI-BRIGHT) instrument), which consists of 52 items covering the five building blocks of the Innovative Care for Chronic Conditions framework [ 22 ]. An average score was calculated for each clinician-participant and then the median score for the clinician-sample was used to dichotomize the CIMI-BRIGHT variable.
Potential Meso-Level Moderators
Time spent with patients during follow-up visits was assessed from two perspectives. Patient-participants were asked how much time all members of their HTx team spend with them on regular follow-up visits. Each participating clinician was asked for the average total time (in minutes) they spend with each patient at the outpatient HTx clinic. Both time variables were then dichotomized using 20 min and 30 min as the cut-off points—these time points were chosen given the distribution of the continuous clinician-time variable and how it aligned with the ordinal patient time-variable.
The typical number of visits within the first month, first 6 months, 1 year, and 3 years were extracted from the transplant director’s BRIGHT questionnaire. Similarly, information regarding the multidisciplinarity of the HTx team was collected from the director’s questionnaire. The CIM competencies of HTx team and CIM level of preparedness of healthcare workers were assessed using the investigator-developed clinician questionnaire including 24 and five items, respectively. Scores were averaged, with higher scores reflecting a higher degree of core competencies and preparedness.
Behavioral Outcomes
The patient questionnaire also included five health behaviors: Physical activity was measured by the 2-item Brief Physical Activity Assessment tool [ 23 ], asking if a patient was sufficiently active. Dietary adherence recorded patient’s self-reported adherence, as applicable, to low salt, low calorie, low saturated fat, low sugar, or other kind of dietary guidelines. Sun protection was measured using 4 items assessing consistency of protection against the sun [ 24 , 25 ]. Smoking status was based on whether patients were currently smoking, stopped less than 1 year ago, stopped more than 1 year ago, or never smoked [ 26 ]. Alcohol intake assessed the level of alcohol consumption by two items i.e., whether the patient used alcohol, and in case they did, how many alcoholic drinks were consumed per week. They were then categorized into non-drinkers; moderate drinkers, or heavy drinkers [ 27 ].
Language congruency was measured by asking patients during the interview if the HTx team communicated in their mother tongue or in a language they mastered fluently (either via an interpreter or directly). Health literacy was assessed as part of the written questionnaire by rating confidence in filling out medical forms, using a 5-point scale (1 = none of the time to 5 = all of the time) and then dichotomized into adequate (≥4) and inadequate (≤3) health literacy [ 28 ]. Lastly, number of comorbidities post-HTx was assessed using an adapted Charlson Comorbidity Index [ 30 ].
Statistical Analysis
Descriptive statistics were calculated for all study variables. The Kruskal-Wallis test was used to examine whether there were differences in trust in the HTx team across the 36 HTx centers. Whether level of CIM was associated with trust in the HTx team was examined using simple and multiple logistic regression. Meanwhile, moderation analysis was performed to determine whether meso-level factors affected the direction and/or strength of the relationship between level of CIM and trust. To examine whether trust could predict behavioral outcomes, simple and multiple logistic regressions were performed, whereby the multiple models were equally controlled for potential confounders that were statistically significant. Finally, marginal effects were calculated to better communicate the practical significance of the findings [ 31 ]. Analyses were conducted in Stata v16.1.
Characteristics of the participants are shown in Table 2 . The proportion of physicians and nurses included reflected the composition of HTx teams in clinical practice. Less than 2% of the data were missing; hence, no imputation was performed.
TABLE 2 . Patients’ demographic and clinical characteristics.
There was significant variability in the level of CIM [PACIC: chi-square (35 df, N = 36) = 209.3, p < 0.001; CIMI: chi-square (35 df, N = 36) = 1,396, p < 0.001] and trust in the healthcare team [chi-square (35 df, N = 36) = 221.5, p < 0.001] among the 36 HTx centers ( Supplementary Material ). HTx recipients who indicated that they had received higher levels of CIM were more likely to have greater trust in the HTx team. This finding was consistent whether level of CIM was measured from the patient’s perspective (adjusted odds ratio [AOR] = 1.85, 95% CI = 1.47 to 2.33, p < 0.001) or from the clinician’s perspective (AOR = 1.35, 95% CI = 1.07 to 1.71, p = 0.012), and even after controlling for potential confounders (age, gender, race, education level, employment status, number of years post HTx, health literacy, language congruency, and comorbidities) ( Table 3 ). However, when controlling for the country where the HTx center was located, the level of CIM from clinicians was no longer significant (AOR = 0.94, 95% CI = 0.67 to 1.30, p = 0.703). Using USA as reference group, HTx patients from France, Germany, and Switzerland had lower odds of having high trust (AOR = 0.16–0.46), while HTx patients from Canada and the UK had higher odds of having higher trust (AOR = 1.86). Meanwhile, education became significant ( p = 0.002- and p = 0.017), indicating that patients with higher education had greater odds of having higher trust (AOR = 1.67–1.96). The calculated marginal effects showed that an average HTx recipient who received lower levels of CIM had a 42.4% probability of trusting their HTx team. Meanwhile, a comparable HTx recipient who received higher levels of CIM had a 57.7% probability of trusting their HTx team.
TABLE 3 . Associations between chronic illness management level and trust.
Among the potential moderators, only time spent with the patients during follow-up visits was significant, i.e., the association between CIM and trust was stronger when consultation time was ≥30 min. This moderation effect was only present when consultation time was >20 min, measured from both the patient’s (OR = 1.61, 95% CI 1.03 to 2.53, p = 0.037) and from the clinician’s perspective (OR = 1.56, 95% CI 1.00 to 2.42, p = 0.048).
Results of the bivariate and multiple logistic regressions are presented in Table 4 . Bivariate analyses showed that trust in the HTx team was significantly associated with smoking and diet adherence. Wherein patients, who had greater trust in their HTx team, were less likely to smoke (OR = .46, 95% CI .25 to .84, p = 0.012) and more likely to adhere to their recommended diets (OR = 1.40, 95% CI 1.08 to 1.82, p = 0.012). However, after controlling for age, gender, race, education, employment status, years post HTx, health literacy, and comorbidities, only the relationship between trust and diet adherence remained significant (OR = 1.34, 95%CI 1.01 to 1.77, p = 0.040). The calculated marginal effects showed that an average HTx recipient who highly trusts their HTx team (i.e., Trust score = 5) is 2.5 times more likely to adhere to their recommended diet compared to an average HTx recipient who has low trust towards their HTx team (i.e., trust score = 1).
TABLE 4 . Associations between trust and health outcomes.
In this study, we observed significant variability in trust in HTx team across the 36 HTx centers. Additionally, associations of CIM, trust in the HTx team and one patient behavioral outcome in HTx follow-up were identified.
First, higher levels of CIM were associated with greater trust in the HTx team, even after adjusting for potential confounders. However, when we controlled for country, the level of CIM from the clinician’s perspective was no longer significant, indicating that the association between clinician-reported CIM levels and trust may be contingent upon the country context. Although country may not serve as an ideal indicator of social and cultural disparities, it is posited to be a more suitable indicator compared to race. Previous studies only focused on patient-level aspects of CIM, e.g., continuity of care [ 2 , 7 , 8 ] or physicians` communication skills [ 2 , 7 ], were positively associated with greater trust in individual healthcare professionals. Yet, the strength of our study is having examined CIM meso-level factors with validated measurement tools from both the patient and clinician perspectives, resulting in consistent findings in each case.
Also, visit duration has been described as important for establishing interpersonal trust [ 8 , 32 ]. In Fiscella et al.’s [ 32 ] study, visit duration independently predicted trust (0.05 SD, 95%CI 0.03–0.06). Patients’ trust in their primary care physician increased by every minute increase in visit duration (0.01 SD, 95% CI 0.001–0.02) [ 32 ]. However, in our study, a stronger association between the level of CIM and trust was found when visit duration was ≥30 min. Indeed, given the complexity of HTx follow-up care and its importance on patients’ health outcomes, it seems reasonable that HTx patients require more time for follow-up than patients in primary care settings. In addition, our findings shed light on the “dose” of time needed during consultations. Yet, further research on aspects contributing to trust during consultation is required.
In fact, the positive association of CIM and trust seems not surprising, when considering relevant components of CCM based CIM programs [ 10 ]. Largely overlapping with aspects increasing interpersonal trust, those components include availability of standards and training for clinicians (e.g., communication), patient-centered care, i.e., well informed and activated patients making their own choices, as well as care coordination of and advocacy for patients [ 33 ]. Another relevant aspect of CIM and driver of health outcomes include healthcare teams’ multidisciplinarity in HTx follow-up. In the BRIGHT study, the majority of included transplant centers (80.6%) involve multidisciplinary teams in HTx follow-up with no significant variability in the type of professionals within the HTx teams across HTx centers [ 34 ]. However, larger, multidisciplinary teams run the risk of individual healthcare providers working in silos and responsibilities for a patient not being clearly defined. To enable trust in multidisciplinary teams, care concepts based on CCM are needed in HTx centers to ensure, for example, continuity in care of the patient and support for self-management [ 35 ].
Second, we found trust significantly independently associated with diet adherence, even after controlling for potential confounders. In general, the association of trust in healthcare professionals and behavioral outcomes such as adherence (medication, exercise, diet), self-care activities, preventive care (r = 0.14, 95% CI 0.10–0.19, p < 0.001) was already described in Birkhäuer et al.’s [ 4 ] meta-analysis on 21 studies including a total of 26′642 patients. Further studies highlighted a positive influence of interpersonal trust on following physicians` recommendations (e.g., diet, lifestyle) [ 5 , 8 ], use of services (e.g., screening) [ 6 , 8 ] and adhering to medication and treatment [ 2 , 6 – 8 ]. However, these studies only focused on trust in individual professionals, whereas our study takes a broader perspective and focusses on trust in the HTx team, reflecting current HTx practice. Our findings indicate CIM, trust and patient outcomes are closely related. While only one behavioral outcome was significantly associated with trust in our multivariate analysis, CIM itself can have a positive effect on behavioral and health outcomes (e.g., patient survival one-year post-Tx) [ 15 ]. Further, studies in renal Tx research show associations of CIM with increased medication adherence [ 36 ], improved quality of life [ 36 ], fewer emergency room visits [ 37 ], fewer hospital admissions [ 37 , 38 ] and reduced mortality [ 38 ]. To enhance HTx patients’ behavioral and health outcomes, a systems perspective is needed, with not only focusing on interventions at patient-level, but also at re-engineering care processes in HTx follow-up towards CIM. This includes leadership accounting for trust as an important factor in HTx care, development of standards, best practices and training (e.g., communication and relationships skills) for the multidisciplinary HTx team, measuring, monitoring and reporting patient trust [ 33 ]. Further measures relevant to increasing patient’s trust in their HTx team include working towards an ecosystem that provides continuity of care and care coordination and allows patient centeredness and shared decision making within a CIM model [ 33 , 39 , 40 ]. The SMILe care model (Integrated Care Model (ICM) for SteM cell transplantatIon faciLitated by eHealth), for example, is one such care model that could potentially serve as a blueprint also for the care of HTx patients. Based on CIM building blocks, the SMILe-ICM aims to reengineer follow-up care of allogeneic stem cell transplanted patients and consists of four intervention modules to support patient self-management and health behaviors (i.e., monitoring & follow-up of vital signs, symptoms and health behavior; infection prevention; physical activity; medication adherence) [ 41 – 44 ].
However, the successful and sustainable implementation of complex interventions based on CIM principles and supporting trust into clinical practice is challenging due to healthcare, organizational, social, economic, and policy related barriers, among others [ 35 , 45 ]. Implementation science supports the uptake of such interventions into routine practice and thus improves both health care services’ quality and effectiveness [ 46 ]. Further, core and adaptable components of complex interventions can be adapted and fitted to the local context in which they will be delivered. Key implementation science elements supporting a shift towards CCM entail contextual analysis, stakeholder involvement, the use of strategies supporting implementation as well as research designs focusing on both implementation and effectiveness outcomes (i.e., hybrid designs) [ 47 ].
Limitations
Our study has several limitations. First, the cross-sectional study design does not allow causal inferences to be drawn. Second, a longitudinal analysis of trust over time could not be performed. Trust has to be understood as a continuum and may change over time. Since HTx patients usually receive life-long follow-up, changes in interpersonal trust relationships could point to aspects of CIM that are specifically relevant for patients’ trust throughout the transplant continuum. Those specific measures could be taken to support trust relationships in practice over time. Third, most data analyzed in this study rely on self-reports from patients and clinicians, introducing a potential for inaccuracies, which could be mitigated by incorporating routine data, for example. Fourth, since we included Tx survivors beyond one-year post-Tx, outcome events in the first year were not considered. These outcomes should be also included in further studies. Further, the fact that 86% of the patients were white limits the assessment of social and cultural differences in perceptions of interpersonal trust. Fifth, the majority of clinicians involved in this study (90%) were nurses. Nurses and other transplant clinicians might differ in their evaluation on the level of chronic illness management as nurses are typically more involved in patient self-management and also typically have a higher sensitivity of psychological issues. Finally, given the limitation due to using secondary data, we did not assess the link of trust on clinical outcomes moderated by service outcomes. Moreover, other potentially important factors such as use of eHealth, distance from Tx-center, health outcomes (e.g., acute rejection, survival) or emotional moderators such as the patient`s mental health concerns could not be examined given the nature of this study.
To our knowledge, this is the first study linking CIM and interpersonal trust to service-level outcomes. We observed significant associations between CIM levels and trust in the HTx team moderated by consultation time, and a significant association between trust and diet adherence. Our findings highlight the need to consider trust and CIM in the HTx follow-up ecosystem as important factors as a basis for optimal transplant outcomes. Thus, further investment in re-engineering of HTx follow-up toward CIM, as well as allowing sufficient time for consultations, is required. Using longitudinal study designs, further research should focus on changes in trust over the transplant continuum and its influences on behavioral and clinical outcomes.
Data Availability Statement
Original datasets are not openly available due to reasons of privacy and are available from the corresponding author upon reasonable request.
Ethics Statement
The studies involving humans were approved by the Ethics committee of the University Hospital Leuven, Belgium and the ethics committees of each participating center. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author Contributions
SD, CR, FD, SV, KD, MC, and JM had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. MC and JM contributed equally to this work. Concept and design of this secondary analysis: SD, JM, MC, and KD; Acquisition, analysis, or interpretation of data: MC and KD; Drafting of the manuscript: JM, MC, and KD; Statistical analysis: MC and KD; Critical revision of the manuscript for important intellectual content: SD, CR, FD, SV, KD, MC, and JM. Supervision: SD. All authors contributed to the article and approved the submitted version.
The BRIGHT Study Team
The BRIGHT Study Team consists of Lut Berben (Institute of Nursing Science, University of Basel, Switzerland); Marisa G. Crespo-Leiro (Complexo Hospitalario Universitario A Coruña (CHUAC), CIBERCV, INIBIC, Universidade da Coruña (UDC), La Coruña, Spain); Sandra Cupples (U.S. Department of Veterans Affairs, Veterans Health Administration, USA); Patricia M. Davidson (School of Nursing, The Johns Hopkins University, Baltimore, Maryland, USA); Paolo De Simone (Azienda Ospedaliero-Universitaria Pisana, Ospedale Cisanello, Pisa, Italy); Albert Groenewoud (Astellas Pharma Europe Ltd., UK); Christiane Kugler (Hannover Medical School, Germany); Linda Ohler (George Washington University, USA); Johan Van Cleemput (University Hospitals Leuven, Belgium); Alain Jean Poncelet (Cliniques Universitaires Saint-Luc, Brussels, Belgium); Laurent Sebbag (Hôpital Louis Pradel, Lyon, France); Magali Michel (Hôpital Nord Laennec, Nantes, France); Andrée Bernard (Hôpital Universitaire Pitié-Salpêtrière, Paris, France); Andreas Doesch (University Hospital Heidelberg, Germany; Asklepios Hospital Bad Salzungen, Bad Salzungen, Germany); Ugolino Livi (University Hospital Udine, Italy); Luciano Potenta (University of Bologna, Italy); Vicens Brossa-Loidi (Hospital de Sant Pau, Barcelona, Spain); Javier Segovia-Cubero (Hospital Puerta de Hierro, Madrid, Spain); Luis Almenar-Bonet (Hospital Universitari i Politècnic La Fe de Valencia, Spain); Carmen Segura Saint-Gerons (Hospital Univeritario Reina Sofia, Córdoba, Spain); Paul Mohacsi (University Hospital of Bern, Switzerland); Eva Horvath (University Hospital Zurich, Switzerland); Cheryl Riotto (Papworth Hospital, Cambridge, UK); Gareth Parry (Freeman Hospital, Newcastle, UK); Ashi Firouzi (Royal Brompton & Harefield NHS Foundation Trust, London, UK); Stella Kozuszko (Toronto General Hospital, Canada); Haissam Haddad (University of Ottawa Heart Institute, Canada); Annemarie Kaan (St Paul’s Hospital, Vancouver, Canada); Grant Fisher (London Health Sciences Centre, Ontario, Canada); Tara Miller (Duke University Hospital, North Carolina, USA); Maureen Flattery (Virginia Commonwealth University Health System, USA); Kristin Ludrosky (Cleveland Clinic, Ohio, USA); Bernice Coleman (Cedars-Sinai Medical Center, California, USA); Jacqueline Trammell (Kaiser Permanente Santa Clara Medical Center, California, USA); Flavio R. Epstein (Kaiser Permanente Santa Clara Medical Center, California, USA); Katherine St. Clair (St Luke’s Hospital, Missouri, USA); Andrew Kao (St Luke’s Hospital, Missouri, USA); Maria Molina (Hospital of the University of Pennsylvania, USA); Karyn Ryan Canales (Ochsner Medical Center, New Orleans, Louisiana, USA); Samira Scalso de Almeida (Hospital Israelita Albert Einstein, São Paulo & Hospit.al Municipal Vila Santa Catarina - Ministerio da Saude PROAD/-SUS, Sao Paulo, Brazil); Bartira de Aguiar Roza (Paulista School of Nursing, Federal University of Sao Paulo, Sao Paolo, Brazil); Andrea Cotait Ayoub (Instituto Dante Pazzanese de Cardiologia, São Paulo, Brazil); Fernanda Barone (Instituto do Coração da Universidade de São Paulo, Brazil); Michelle Harkess (St Vincent’s Hospital, Sydney, Australia); Joanne Maddicks-Law (The Prince Charles Hospital, Brisbane, Australia).
The authors declare that this study received funding from the International Transplant Nurses Society (ITNS) in 2008, the International Society for Heart and Lung Transplantation (ISHLT) in 2012, the Swiss Academy of Medical Sciences (SAMW) in 2013 as well as by an unrestricted research grant from Astellas Pharma. Co-financed with European Union Regional Development Funds (EURDF). The funding organizations were not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We wish to thank all of the patients and clinicians who participated in the BRIGHT study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontierspartnerships.org/articles/10.3389/ti.2024.11704/full#supplementary-material
Abbreviations
AOR, adjusted odds ratio; BRIGHT, Building Research Initiative Group: Chronic Illness Management and Adherence in Transplantation (BRIGHT) study; CCM, Chronic Care Model; CIM, chronic illness management; CIMI-BRIGHT, The Chronic Illness Management Implementation—Building Research Initiative Group: Chronic Illness Management and Adherence in Transplantation (CIMI-BRIGHT) instrument; HTx, heart transplantation; PACIC, Patient Assessment of Chronic Illness Care (PACIC) instrument.
1. Lynch, TJ, Wolfson, DB, and Baron, RJ. A Trust Initiative in Health Care: Why and Why Now? Acad Med (2019) 94(4):463–5. Epub 2019/01/17. doi:10.1097/acm.0000000000002599
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Hall, MA, Dugan, E, Zheng, B, and Mishra, AK. Trust in Physicians and Medical Institutions: What Is It, Can It Be Measured, and Does It Matter? Milbank Q (2001) 79(4):613–39. doi:10.1111/1468-0009.00223
3. Robinson, CA. Trust, Health Care Relationships, and Chronic Illness:A Theoretical Coalescence. Glob Qual Nurs Res (2016) 3:2333393616664823. doi:10.1177/2333393616664823
4. Birkhäuer, J, Gaab, J, Kossowsky, J, Hasler, S, Krummenacher, P, Werner, C, et al. Trust in the Health Care Professional and Health Outcome: A Meta-Analysis. PLoS One (2017) 12(2):e0170988. doi:10.1371/journal.pone.0170988
5. Calnan, M, and Rowe, R. Trust and Health Care. Sociol Compass (2007) 1(1):283–308. doi:10.1111/j.1751-9020.2007.00007.x
CrossRef Full Text | Google Scholar
6. LoCurto, J, and Berg, GM. Trust in Healthcare Settings: Scale Development, Methods, and Preliminary Determinants. SAGE Open Med (2016) 4:2050312116664224. doi:10.1177/2050312116664224
7. Thom, DH, Hall, MA, and Pawlson, GL. Measuring Patients’ Trust in Physicians When Assessing Quality of Care. Health Aff (2004) 23(4):124–32. doi:10.1377/hlthaff.23.4.124
8. Hillen, MA, de Haes, HCJM, and Smets, EMA. Cancer Patients' Trust in Their Physician—A Review. Psychooncology (2011) 20(3):227–41. doi:10.1002/pon.1745
9. Calnan, M, Rowe, R, and Entwistle, V. Trust Relations in Health Care: An Agenda for Future Research. J Health Organ Manag (2006) 20(5):477–84. doi:10.1108/14777260610701830
10. Wagner, EH, Austin, BT, Davis, C, Hindmarsh, M, Schaefer, J, and Bonomi, A. Improving Chronic Illness Care: Translating Evidence Into Action. Health Aff (2001) 20(6):64–78. doi:10.1377/hlthaff.20.6.64
11. Wagner, EH. Organizing Care for Patients With Chronic Illness Revisited. Milbank Q (2019) 97(3):659–64. Epub 2019/08/19. doi:10.1111/1468-0009.12416
12. Nuño, R, Coleman, K, Bengoa, R, and Sauto, R. Integrated Care for Chronic Conditions: The Contribution of the Iccc Framework. Health Policy (2012) 105(1):55–64. doi:10.1016/j.healthpol.2011.10.006
13. Oprea, L, Braunack-Mayer, A, Rogers, WA, and Stocks, N. An Ethical Justification for the Chronic Care Model (Ccm). Health Expect (2010) 13(1):55–64. doi:10.1111/j.1369-7625.2009.00581.x
14. Iglesias, K, De Geest, S, Berben, L, Dobbels, F, Denhaerynk, K, Russell, LC, et al. Validation of the Patient Assessment of Chronic Illness Care (Pacic) Short Form Scale in Heart Transplant Recipients: The International Cross-Sectional Bright Study. BMC Health Serv Res (2020) 20(1):160. doi:10.1186/s12913-020-5003-3
15. Cajita, MI, Denhaerynck, K, Berben, L, Dobbels, F, Van Cleemput, J, Crespo-Leiro, M, et al. Is Degree of Chronic Illness Management in Heart Transplant Centers Associated With Better Patient Survival? Findings From the Intercontinental Bright Study. Chronic Illn (2021) 18:806–17. doi:10.1177/17423953211039773
16. Berben, L, Denhaerynck, K, Dobbels, F, Engberg, S, Vanhaecke, J, Crespo-Leiro, MG, et al. Building Research Initiative Group: Chronic Illness Management and Adherence in Transplantation (Bright) Study: Study Protocol. J Adv Nurs (2015) 71(3):642–54. doi:10.1111/jan.12519
17. Denhaerynck, K, Berben, L, Dobbels, F, Russell, CL, Crespo-Leiro, MG, Poncelet, AJ, et al. Multilevel Factors Are Associated With Immunosuppressant Nonadherence in Heart Transplant Recipients: The International Bright Study. Am J Transpl (2018) 18(6):1447–60. doi:10.1111/ajt.14611
18. Hall, MA. Researching Medical Trust in the United States. J Health Organ Manag (2006) 20(5):456–67. doi:10.1108/14777260610701812
19. Hall, MA, Zheng, B, Dugan, E, Camacho, F, Kidd, KE, Mishra, A, et al. Measuring Patients’ Trust in Their Primary Care Providers. Med Care Res Rev (2002) 59(3):293–318. doi:10.1177/1077558702059003004
20. Gugiu, PC, Coryn, C, Clark, R, and Kuehn, A. Development and Evaluation of the Short Version of the Patient Assessment of Chronic Illness Care Instrument. Chronic Illn (2009) 5(4):268–76. doi:10.1177/1742395309348072
21. Iglesias, K, Burnand, B, and Peytremann-Bridevaux, I. Pacic Instrument: Disentangling Dimensions Using Published Validation Models. Int J Qual Health Care (2014) 26(3):250–60. doi:10.1093/intqhc/mzu042
22. Berben, L, Russell, CL, Engberg, S, Dobbels, F, and De Geest, S. Development, Content Validity and Inter-Rater Reliability Testing of the Chronic Illness Management Implementation – Building Research Initiative Group: Chronic Illness Management and Adherence in Transplantation: An Instrument to Assess the Level of Chronic Illness Management Implemented in Solid Organ Transplant Programmes. Int J Care Coord (2014) 17(1-2):59–71. doi:10.1177/2053435414540607
23. Marshall, AL, Smith, BJ, Bauman, AE, and Kaur, S. Reliability and Validity of a Brief Physical Activity Assessment for Use by Family Doctors. Br J Sports Med (2005) 39(5):294–7. doi:10.1136/bjsm.2004.013771
24. Swiss Childhood Cancer Registry. Swiss Study on the Health of People With Cancer, Leukemia or Tumor in Childhood .
25. Hussain, SH, Metthewes, G, Todd, P, and Chaudhry, A. Skin Cancer in Renal Transplant Patients (2011). Available from: https://bts.org.uk/wpcontent/uploads/2016/09/BTS_Abstract_pdf_2011.pdf (Accessed June 29, 2017).
Google Scholar
26. Swiss Federal Statistical Office. Gesundheit Und Gesundheitsverhalten in Der Schweiz 2007 (2007). Schweizerische Gesundheitsbefragung. Available from: http://www.bfs.admin.ch/bfs/portal/en/index.html (Accessed June 29, 2017).
27. U.S. Department of Health and Human Services. Agriculture USDo. Dietary Guidelines for Americans 2015-2020 (2015). Available from: https://health.gov/dietaryguidelines/2015/resources/2015-2020_Dietary_Guidelines.pdf (Accessed June 29, 2017).
28. Chew, LD, Bradley, KA, and Boyko, EJ. Brief Questions to Identify Patients With Inadequate Health Literacy. Fam Med (2004) 36(8):588–94.
PubMed Abstract | Google Scholar
29. Chew, LD, Griffin, JM, Partin, MR, Noorbaloochi, S, Grill, JP, Snyder, A, et al. Validation of Screening Questions for Limited Health Literacy in a Large Va Outpatient Population. J Gen Intern Med (2008) 23(5):561–6. doi:10.1007/s11606-008-0520-5
30. Fried, L, Bernardini, J, and Piraino, B. Charlson Comorbidity Index as a Predictor of Outcomes in Incident Peritoneal Dialysis Patients. Am J Kidney Dis (2001) 37(2):337–42. doi:10.1053/ajkd.2001.21300
31. Norton, EC, Dowd, BE, and Maciejewski, ML. Marginal Effects—Quantifying the Effect of Changes in Risk Factors in Logistic Regression Models. Jama (2019) 321(13):1304–5. doi:10.1001/jama.2019.1954
32. Fiscella, K, Sean, M, Franks, P, Cleveland, GS, Paul, D, McDaniel, SH, et al. Patient Trust: Is It Related to Patient-Centered Behavior of Primary Care Physicians? Med Care (2004) 42(11):1049–55. doi:10.1097/00005650-200411000-00003
33. Lee, TH, McGlynn, EA, and Safran, DG. A Framework for Increasing Trust Between Patients and the Organizations That Care for Them. JAMA (2019) 321(6):539–40. doi:10.1001/jama.2018.19186
34. Cajita, MI, Baumgartner, E, Berben, L, Denhaerynck, K, Helmy, R, Schonfeld, S, et al. Heart Transplant Centers With Multidisciplinary Team Show a Higher Level of Chronic Illness Management - Findings From the International Bright Study. Heart Lung (2017) 46(5):351–6. Epub 2017/06/19. doi:10.1016/j.hrtlng.2017.05.006
35. Lynch, T. Abim Foundation Forum Background Paper (2019). Available from: https://abimfoundation.org/wp-content/uploads/2019/07/2019-ABIM-Foundation-Forum-Background-Paper.pdf (Accessed October 25, 2021).
36. Schmid, A, Hils, S, Kramer-Zucker, A, Bogatyreva, L, Hauschke, D, De Geest, S, et al. Telemedically Supported Case Management of Living-Donor Renal Transplant Recipients to Optimize Routine Evidence-Based Aftercare: A Single-Center Randomized Controlled Trial. Am J Transpl (2017) 17(6):1594–605. doi:10.1111/ajt.14138
37. Bissonnette, J, Woodend, K, Davies, B, Stacey, D, and Knoll, GA. Evaluation of a Collaborative Chronic Care Approach to Improve Outcomes in Kidney Transplant Recipients. Clin Transpl (2013) 27(2):232–8. doi:10.1111/ctr.12068
38. Drewes, HW, Steuten, LMG, Lemmens, LC, Baan, CA, Boshuizen, HC, Elissen, AMJ, et al. The Effectiveness of Chronic Care Management for Heart Failure: Meta-Regression Analyses to Explain the Heterogeneity in Outcomes. Health Serv Res (2012) 47(5):1926–59. doi:10.1111/j.1475-6773.2012.01396.x
39. Rolfe, A, Cash-Gibson, L, Car, J, Sheikh, A, and McKinstry, B. Interventions for Improving Patients' Trust in Doctors and Groups of Doctors. Cochrane Database Syst Rev (2014) 2014(3):CD004134. doi:10.1002/14651858.CD004134.pub3
40. Greene, J, and Samuel-Jakubos, H. Building Patient Trust in Hospitals: A Combination of Hospital-Related Factors and Health Care Clinician Behaviors. Jt Comm J Qual Patient Saf (2021) 47(12):768–74. doi:10.1016/j.jcjq.2021.09.003
41. Leppla, L, Schmid, A, Valenta, S, Mielke, J, Beckmann, S, Ribaut, J, et al. Development of an Integrated Model of Care for Allogeneic Stem Cell Transplantation Facilitated by Ehealth-The Smile Study. Support Care Cancer (2021) 29:8045–57. Epub 2021/07/06. doi:10.1007/s00520-021-06328-0
42. Leppla, L, Hobelsberger, S, Rockstein, D, Werlitz, V, Pschenitza, S, Heidegger, P, et al. Implementation Science Meets Software Development to Create Ehealth Components for an Integrated Care Model for Allogeneic Stem Cell Transplantation Facilitated by Ehealth: The Smile Study as an Example. J Nurs Scholarsh (2020) 53:35–45. Epub 2020/12/22. doi:10.1111/jnu.12621
43. De Geest, S, Valenta, S, Ribaut, J, Gerull, S, Mielke, J, Simon, M, et al. The Smile Integrated Care Model in Allogeneic Stem Cell Transplantation Facilitated by Ehealth: A Protocol for a Hybrid Effectiveness-Implementation Randomised Controlled Trial. BMC Health Serv Res (2022) 22(1):1067. doi:10.1186/s12913-022-08293-8
44. Valenta, S, Ribaut, J, Leppla, L, Mielke, J, Teynor, A, Koehly, K, et al. Context-Specific Adaptation of an Ehealth-Facilitated, Integrated Care Model and Tailoring Its Implementation Strategies – A Mixed-Methods Study as a Part of the Smile Implementation Science Project. Front Health Serv (2023) 2:977564. doi:10.3389/frhs.2022.977564
45. Davy, C, Bleasel, J, Liu, H, Tchan, M, Ponniah, S, and Brown, A. Factors Influencing the Implementation of Chronic Care Models: A Systematic Literature Review. BMC Fam Pract (2015) 16:102. doi:10.1186/s12875-015-0319-5
46. Eccles, MP, and Mittman, BS. Welcome to Implementation Science. Implement Sci (2006) 1(1):1. doi:10.1186/1748-5908-1-1
47. De Geest, S, Zúñiga, F, Brunkert, T, Deschodt, M, Zullig, LL, Wyss, K, et al. Powering Swiss Health Care for the Future: Implementation Science to Bridge "The Valley of Death. Swiss Med Wkly (2020) 150:w20323. Epub 2020/10/07. doi:10.4414/smw.2020.20323
Keywords: trust, chronic illness management, heart transplant, transplant team, behavioral outcomes
Citation: Mielke J, Cajita MI, Denhaerynck K, Valenta S, Dobbels F, Russell CL, De Geest S and the BRIGHT study team (2024) Trust in the Transplant Team Associated With the Level of Chronic Illness Management—A Secondary Data Analysis of the International BRIGHT Study. Transpl Int 37:11704. doi: 10.3389/ti.2024.11704
Received: 19 June 2023; Accepted: 18 January 2024; Published: 11 March 2024.
Copyright © 2024 Mielke, Cajita, Denhaerynck, Valenta, Dobbels, Russell, De Geest and the BRIGHT study team. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sabina De Geest, [email protected]
† These authors share first authorship
THIS ARTICLE IS PART OF THE SPECIAL ISSUE View all 7 Articles
Living well after organ transplantation
ORIGINAL ARTICLE
People also looked at.
Generating Oncology Patient Trust in the Nurse: An Integrative Review
Affiliation.
- 1 School of Nursing, Duquesne University, Pittsburgh, PA, USA.
- PMID: 32493142
- DOI: 10.1177/0193945920930337
An integrative review was conducted to evaluate the extent and quality of literature regarding adult oncology patients' trust in nurses. Nineteen studies met the inclusion criteria. Three themes were identified, which are as follows: nurse trust facilitating behaviors, nurse attributes, and the influence of patient-nurse trust on health and psychosocial well-being. Findings indicate that the extent of literature is limited in specific examples of nurse interventions that facilitate interpersonal patient-nurse trust. Future research should include more detailed nurse actions and attributes that build patient-nurse trust to fully understand the benefits of trust in oncology patients.
Keywords: integrative review; interpersonal trust in the nurse; nursing interventions; oncology patient; patient-nurse relationship; trust in the nurse.
Publication types
- Medical Oncology*
- Neoplasms / nursing*
- Nurse-Patient Relations*
- Oncology Nursing*
- Trust / psychology*
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

A Paradigm for Understanding Trust and Mistrust in Medical Research: The Community VOICES Study
M. smirnoff.
1 Icahn School of Medicine at Mount Sinai
2 Montclair State University
3 National Health Service
4 New York Presbyterian Weill Cornell Hospital
5 University of Pittsburg
L. D. Richardson
To promote justice in research practice and rectify health disparities, greater diversity in research participation is needed. Lack of trust in medical research is one of the most significant obstacles to research participation. Multiple variables have been identified as factors associated with research participant trust/mistrust. A conceptual model that provides meaningful insight into the interplay of factors impacting trust may promote more ethical research practice and provide an enhanced, actionable understanding of participant mistrust.
A structured survey was developed to capture attitudes towards research conducted in emergency situations; this paper focuses on items designed to assess respondents’ level of trust or mistrust in medical research in general. Community-based interviews were conducted in English or Spanish with 355 New York City residents (white 42%, African American 29%, Latino 22%).
Generally favorable attitudes towards research were expressed by a majority (85.3%), but many respondents expressed mistrust. Factor analysis yielded four specific domains of trust/mistrust, each of which was associated with different demographic variables: General Trustworthiness (older age, not disabled); Perceptions of Discrimination (African American, Latino, Spanish language preference); Perceptions of Deception (prior research experience, African American); and Perceptions of Exploitation (less education).
Conclusions
The four domains identified in the analysis provide a framework for understanding specific areas of research trust/mistrust amongst disparate study populations. This model offers a conceptual basis for the design of tailored interventions that target specific groups to promote trust of individual researchers and research institutions as well as to facilitate broader research participation.
Introduction
In response to concerns over health disparities and a lack of diversity among research participants, the National Institutes of Health (NIH) mandated the inclusion of women and minorities in clinical research (1993, 2001). The mandate is rooted in the principle of justice with a goal to promote fairness in the research process by fostering access and inclusiveness ( Tilburt et al 2007 ). In the years since the policy was first initiated, there has been a 15.4 fold increase in the number of minority participants in NIH-funded clinical research studies, but this still represents only a modest increase in the percentage of NIH clinical research participants who are minorities (27.8%) ( DHHS 2010 ). Even with renewed recruitment efforts and the increase in minority research participation, health disparities experienced by minorities persist in both incidence (new cases) and prevalence (all existing cases) ( Schmotzer 2012 ). To identify more effective therapeutic interventions for groups disproportionately affected by particular health conditions, research on group-specific and subgroup-specific treatment effectiveness is needed.
Research Trust / Mistrust
Over the last decade, there has been considerable research into the barriers and facilitators associated with minority under-representation in research. A consensus has been reached that participant trust in research and research institutions is one of the most, if not the most, significant factors associated with research participation. This consensus is represented in an extensive literature that has been synthesized and summarized in four major systematic literature reviews; two focused on general clinical research and one each for emergency research and psychiatric research ( Schmotzer 2012 ; George et al. 2014 ; Limkakeng et al. 2014 ; Brown et al 2014 ). Combined, these meta-analyses include dozens of studies conducted in geographically diverse locales, involving thousands of participants across multiple racial/ethnic groups, and each affirms the role of trust/mistrust as a primary determinant of research participation. Common trust-related themes identified in these studies involve being mistreated or taken advantage of (by specific research practices like randomization, or being used “like guinea pigs”) and unintended consequences (involuntary admissions, side effects or stigmatization) ( Schmotzer 2012 ; George et al. 2014 ; Limkakeng et al. 2014 ; Brown et al 2014 ). It is not known if the respondent attitudes in these studies derive from personal experience of research.
A greater understanding is needed of the complexities involved in research trust. Referencing the literature on attitudes to doctors and healthcare, people distinguish between global trust in healthcare institutions and specific trust in their individual physician; specific trust in the latter is usually higher for all population groups ( Hall 2006a ). Global trust is typically based on institutional reputation and status, while specific trust is often based on the quality of the personal interaction. Armstrong et al. (2008) . found that mistrust among minorities towards the healthcare system is based on mistrust of values more than mistrust of clinical competency. Similarly, most research participants distinguish their relationship with “the researcher” from their relationship with the institution or study sponsor, with the individual relationship carrying greater weight ( McDonald et al. 2008 ).
Definitions of Research Trust / Mistrust
Although several authors have defined medical trust by its behaviors or characteristics such as fidelity, loyalty, honesty and competence ( Hall 2006a ), a Cochrane review ( McKrinsky et al. 2006 ) defines medical trust in terms of the classical doctor-patient relationship: “Patient trust is the belief that a doctor is working in the patient’s best interests.” Similarly, Armstrong et al. (2008) define trust as “the belief that an entity will act in one’s interest in the future,” in contrast to distrust, or “the belief that an entity will act against one’s interest in the future.” The terms distrust and mistrust are often used interchangeably, but distrust is most correctly based on a specific experience or information, while mistrust expresses a general sense of unease toward someone or something. Authors also make a distinction between mistrust/distrust and absence of trust because the former imply a more malignant state that may be critical to racial and ethnic disparities. For these reasons, in our discussion, the opposite of trust is mistrust, rather than distrust or lack of trust.
Clinical research trust is defined in this study as the belief by the study participant that his/her interests (e.g. full disclosure, balance of risk/benefit, prudent data usage) are considered before the interests of the study or the researcher. This would be reflective of Wright’s (2010) view, that a trustworthy researcher acknowledges the value of the trust that the participant vests in them and uses this to rationally decide how to act. Conversely, research mistrust is defined as the belief by the study participant that his/her needs are subordinate to those of the study or the researcher as evidenced by conditions such as withholding important information, risks that outweighs benefit, or data used to damage individuals or communities.
Measurement of Trust
The literature on trust has informed the development of several tools for measuring trust and mistrust in clinical research ( Corbie-Smith et al. 2002 ; Mainous 2006 ; Hall et al. 2007; Braunstein 2008 ) This paper describes the development and use of an interview instrument to assess research trust/mistrust and discusses the findings and implications of a survey using this instrument conducted in diverse communities in New York City. The survey was part of the Community VOICES Study (Views on Informed Consent in Emergency Situations). Emergency research refers to research performed in emergency situations that cannot realistically be done in controlled, clinical situations; e.g., development of new, effective treatments for cardiac arrest when the intervention must be initiated immediately and there is no time to obtain traditional informed consent. There is specific guidance on the proper conduct of research in emergency situations ( USDHSS 1996 ). The Community VOICES Study utilized mixed methods to examine the operational, ethical, educational, and social implications of the Exception from Informed Consent (EFIC) for Emergency Research regulations ( USDHSS 1996 ) and guidance ( USDHSS 2000 , 2006 , 2011 ; Richardson 2005 ). Since EFIC studies present special issues of trust and mistrust of medical researchers, the Community VOICES team was interested in assessing whether community members’ trust and mistrust of research in general influenced their attitudes towards EFIC studies.
The Community VOICES Study was reviewed by the Icahn School of Medicine at Mount Sinai Institutional Review Board and was deemed to be exempt from review.
Study participants were recruited from a stratified sample of 35 residential buildings in New York City that had participated in the Public Access Defibrillation Trial ( Ornato et al. 2003 ; The PAD Trial Investigators 2004 ) one of the earliest NIH-funded multicenter EFIC trials. A representative sample of buildings was obtained using a diversity score developed for the study. Buildings were categorized according to the average age, socioeconomic status (SES) and racial/ethnic composition of residents. A stratified random sampling procedure using these categories was used to obtain a representative sample of buildings.
Recruitment
The research team contacted the management of the residential buildings for permission to conduct active, on-site recruitment of residents for this study. Flyers posted in common areas and letters distributed to each apartment informed residents about the study. The interviews required no appointment and were conducted, in English or Spanish, at the point of contact, on-site, either in quiet public spaces in the buildings or in participants’ apartments.
Instrument Development
Using purposive sampling, based on gender, race, and ethnicity, of residents and employees from the cohort buildings, focus groups were conducted in English and Spanish to inform the development of the interview instrument. The interview instrument was pilot tested on a sample of building residents prior to study initiation. The interview instrument was translated into Spanish by native Spanish speakers then back translated by someone naive to the instrument and reconciled with the original to assure accuracy. The Community VOICES interview elicited information in several domains including: informed consent for research, definition of community, research risks/benefits/burdens, previous experience with research and with emergencies, knowledge of the previous study (PAD Trial), and medical mistrust.
The trust/mistrust questions on the interview were derived from the Group-Based Medical Mistrust Scale (GBMMS) ( Thompson et al. 2004 ), a measure developed to evaluate attitudes towards cancer screening among African American and Latina women. The instrument is “group-based” because it attempts to assess trust through the prism of group identity. It utilizes a 12-item Likert scale to measure suspicion of mainstream healthcare systems, healthcare professionals, and the treatments they provide to members of the respondent’s ethnic or racial group. The instrument has been tested in groups of minority women and men and found to be both reliable and valid ( Shelton et al. 2010 ; Thompson et al. 2004 ). Based on a review of the literature and focus group comments, the VOICES research team modified the GBMMS to address group based concerns about medical research and researchers. This synthesis yielded a 10-item Likert scale to measure research trust/mistrust that was embedded within the larger 8-item VOICES interview. This paper presents the results obtained from the interview questions concerning research trust/mistrust ( Table 3 ) and seventeen demographic questions. Findings from other sections of the interview have been published elsewhere ( Ragin et al. 2008 ).
Factor Analysis
Interview Administration
All participants were screened for eligibility prior to the interview. Eligible participants were at least 18 years old, and were either building employees who had worked in the participating building for at least 3 months prior to the survey or building residents who had lived in the building for a minimum of 3 months. All participant responses were anonymous and no participant identifiers were collected. Interviewers obtained verbal informed consent from each participant prior to the interview and advised them that they were not obliged to answer any question that made them uncomfortable or which they did not wish to answer. Participants were given the choice of being interviewed in either English or Spanish by bilingual study coordinators and each received their choice of a $20 New York City Metrocard (public transportation fare card) or a $20 phone card upon completion of the interview. Interviews were about 40-minutes long and were conducted during both daytime and evening hours, on both weekdays and weekends. Interviewing was initiated in January 2005 and completed in March 2006.
Data Analysis
All analyses were conducted using SAS v.9.2. Descriptive information (means, standard deviations, etc.) was obtained using the UNIVARIATE procedure. The factor analysis utilized a principal components solution with an oblique rotation (using the promax criterion). A General Linear Model approach was taken to assess the predictors of the Trust factors. Post-hoc tests of mean differences employed the Tukey-Kramer adjustment for multiple comparisons.
Management from thirty-one of the 35 selected buildings agreed to participate in the Community VOICES study. Two declined to participate and two sites did not respond despite repeated outreach attempts. Interviews were obtained from 288 residents and 68 employees for a total of 355 interviews. (One participant was both a resident and employee in the same building). The mean number of interviews per building was 11.5, ranging from 2 to 25 per building. The interviews were conducted in English (312 participants, 88%) and Spanish (43 participants, 12%).
Demographic Characteristics
The majority of participants were female (64%) and over 60 years of age (53%) (less than 25 years: 4%; 25–45 years: 21%; 46–60 years: 21%; 60–75 years: 23%; greater than 75 years: 30%). The largest single racial/ethnic group was White (42%) followed by Black (29%), Latino (22%) and other (6%). Other demographic factors, including household income and level of education, are shown in Table 1 . A summary of participant responses to the 10 trust items are shown in Table 2 .
Demographic Characteristics of Study Participants N=355
Research Trust/Mistrust Questions N=355
Factor Analysis Results
Survey responses were reviewed by the investigators and into four factors:
- “General Trustworthiness” included two positively worded statements focused on whether participants felt positive about research and whether researchers would subject participants to harm.
- “Perception of Deception” included three negatively worded statements about doctors/healthcare workers hiding and withholding information, or taking action without permission.
- “Perception of Exploitation” included two negatively worded statements which suggested that researchers “used” participants for their own personal gain or devalued the participants as individuals.
- “Perception of Discriminatory Treatment” included three statements about awareness of differences in treatment and research practices among racial/ethnic groups.
These factors were subject to further statistical analysis. Each Likert-type question had a score range of 1–5. These were summed to create a score range for the factor category. For example, on a factor with 3 items, the total score ranged between 3 and 15. Mean scores for each category and the demographic variables that were associated with significant difference in scores are shown in Table 3 . (Please note: in the following sections, we present the means and a t-test for domains in which all of the explanatory variables are categorical; for domains in which any of the significant explanatory variables are continuous, the F ratio is presented for all of the significant variables in that domain.)
For the domain of General Trustworthiness, not being disabled (F(1, 340)= 4.74; p= 0.0301) being older (F(1, 340)= 4.42; p= 0.0362) and/or having children living at home (F(1, 340)= 10.73; p= 0.0012) were associated with viewing researchers as trustworthy. Perception of Discriminatory Treatment was associated with totally different predictors. Those participants who preferred to be interviewed in Spanish (mean = 10.24) versus English (mean=9.23; t[1,339]=1.98; p=0.04) were more likely to perceive discriminatory treatment. African-American participants (mean=10.51) and Latinos (mean = 10.23) were marginally (t(1,339) = 2.49; p = 0.0627) were more likely to think that researchers were discriminatory compared to Caucasians.
Educational background was the only significant (F(3,342) = 4.14; p = 0.0066) factor associated with Perceptions of Exploitation. Those reporting high school education or less (mean = 5.97) were significantly (t[1,342] = 3.10; p = 0.011) more likely than others to say that researchers exploit participants.
There were three predictors of Perceptions of Deception. Those who had some experience with research were significantly (t[1,344] = −2.52; p = 0.0122) more likely to say that researchers are deceptive (mean 9.72) compared to those without research experience (mean = 9.00). Respondents who were divorced or separated were (t[1,344] = −2.71; p = 0.0358) more likely to say that researchers are deceptive (mean = 9.71) compared to those who were married or living with a significant other (mean = 8.82).
African Americans were marginally (t[1, 342] = 2.37; p = 0.0846) more likely to say that researchers deceive (mean = 9.97) compared to Latinos (mean = 9.12) and compared to participants of other races (mean = 8.69; t[1,342] = 2.33; p = 0.0935).
Correlation between factors
Correlation between the questions grouped in a single category supported the validity of grouping. There was a weakly negative correlation between the general trustworthiness scale and the factors which described perceptions of doctor/researcher behaviors that may negatively affect trust (correlation). This suggests that participants who felt a greater general sense of trust in researchers were less likely to see them as deceptive, exploitative, or treating patients differently according to race/ethnicity. Conversely, there were weakly positive correlations between trust and beliefs that researchers exploit, researchers deceive, and researchers treat people differently (correlations). Those who did not think that researchers are exploitative were also less likely to think they deceive or treat people differently (correlation). Conversely, those who thought researchers are exploitative were more likely to say they deceive research participants and that they treat people differently (correlation).
Sensitive evaluation tools are needed for measuring the complex relationships of race, ethnicity, and trust in the research setting. It is important to evaluate and disentangle aspects of both specific interpersonal trust (a participant’s personal relationship with a researcher) and global trust (a participant’s relationship with the medical research enterprise as a whole) as well as capturing determinants of trust in research that are specific to racial/ethnic identity. This study aimed to explore these influences on attitudes towards medical research participation and create a paradigm for greater understanding.
Conceptual Model: Domains of Trust
While confirming others’ findings, our study adds a new element to the literature with the identification of four domains that conceptualize the phenomenon of research trust/mistrust. In a racially and ethnically diverse cohort, these factors were differentially associated with socio-demographic variables, some of which have not previously been fully considered.
The General Trustworthiness factor was developed by other authors. Hall (2006a) has written extensively about the concept of global trust and reports that even where conceptual domains of trust are explored and measured, they are often indivisible from a global sense of trust. The current study identifies three other factors, which may be more properly described as determinants of trust.
Race and Ethnicity as a Predictor of Mistrust
The results of this study related to race and ethnicity may be particularly valuable as our participants closely approximated the racial/ethnic profile of the New York City target population: (white: NYC 44% vs. VOICES study 42%; black: NYC 25.5% vs. study 29%; Latino: NYC 28.6% vs. study 22%) ( Census 2010 ). As a microcosm of NYC, and perhaps other urban areas, these data may offer insight into attitudes of trust/mistrust towards research of a swath of the national population, more than two-thirds of which lives in urban areas ( Census 2010 ).
We found that although participants were generally more trusting than mistrusting, African-American race and Latino ethnicity were variables associated with Perceptions of Discrimination and Perceptions of Deception. This is a finding consistent with the work of other authors ( Hughes et al. 2015 ; Moreno et al. 2015 ; Lang et al. 2013 ; Brandon et al. 2005 ; Braunstien et al. 2008 ; Corbie-Smith et al. 2002 ; Hall 2006b ; Mainous et al. 2006 ). The U.S. history of racism towards blacks, illustrated by memories of the Tuskegee Syphilis Study, make our findings of Perceptions of Discrimination and Deception unsurprising in this group. Discrimination against the Latino community, with its own unique historical experiences, is well described ( Moreno-Jones 2004 ); in our survey Perceptions of Discrimination were also voiced by Latino respondents, an effect seen most strongly among those who chose to be interviewed in Spanish. Not just a historical memory or part of an extensive oral history, for many members of minority communities, their lived experience with the current healthcare system reinforces perceptions of injustice and discrimination on a daily basis ( Brandon et al. 2005 ; Corbie-Smith et al. 2007 ; Moreno-Jones et al. 2004 ; Scharf et al. 2010 ). These results also highlight the importance of not over-simplifying the effect of race/ethnicity on trust, especially by erroneously grouping all racial/ethnic minorities together. It is important to explore and address the roots of mistrust among different minority communities separately. The specific domains of mistrust that emerged from our data offer possibilities for targeted interventions. To alter Perceptions of Discrimination, evidence-based strategies that take into account the culture and diversity of a population to help health care providers give high-quality clinical care, might prove to be just as effective among investigators and research staff. Similarly, much of the current work on identifying and neutralizing implicit bias in the workplace might be transferrable to the research setting. Targeted interventions to alter Perceptions of Deception should focus on openness and transparency; researchers should actively seek to demonstrate that they are trustworthy. Among blacks, this may require that groundwork to build relationships with the community being researched precede specific research projects ( Yarborough 2013 ). Such relationships and the expectation of reciprocity between community and researcher are of particular importance in many minority communities ( Corbie-Smith et al. 2007 ; Kagawa-Singer 2000 ; McDonald 2008 ).
Neither race nor ethnicity was significantly associated with Perception of Exploitation; it was less education that predicted this domain, suggesting that more education mitigates feelings of susceptibility to exploitation among all racial and ethnic groups. The fact that the Community VOICES Study respondents included a range of educational and income levels within each racial and ethnic group allowed us to observe the distinct impacts of race/ethnicity and socioeconomic status on the various domains of trust.
At the same time, previous research experience was associated with Perception of Deception. This suggests something in the personal research experience may imbue an expectation of deception; whether this is due to a misunderstanding of certain research processes such as blinding or randomization or it is the result of actual deceptive acts by researchers is unclear. Furthermore, as in this study, other authors have noted that older age has greater association with trust than race does ( Farmer 2007 ). Feelings of trust may be related to older adults’ more frequent contact with the healthcare system.
Language Preference as a Predictor of Mistrust
The 12% of respondents who were more comfortable being interviewed in Spanish than in English had stronger Perceptions of Discriminatory Treatment compared to English language respondents. We did not explicitly assess English proficiency in our survey. While some of our respondents who chose to be interviewed in Spanish may be fluent in both languages, it is likely that most of those who were interviewed in Spanish had limited English proficiency. People who speak English “less than very well” are considered of limited English proficiency (LEP) and represent 8.5% of the total US population or 25 million people over the age of five, with higher rates in some regions, including New York City ( Census 2013 ). Nationally, those with LEP are more likely to live in poverty, have poorer health outcomes ( Fields 2016 ), be less educated ( Zong and Batalova 2015 ), and be underrepresented in clinical research. This underrepresentation of significant portions of the population in clinical trials results in research that may not be generalizable to those excluded populations ( Glickman et al. 2011 ).
To improve fair access to research participation and the resulting improvements in health and healthcare, interventions should be directed towards both the LEP and the research communities. Targeted linguistically and culturally fluent educational interventions geared towards LEP communities should be developed to explain the risks, benefits, and methods of clinical research. Sympathetic, culturally appropriate translations by native speakers rather than directly translated words, may avoid confusion due to discrepant meanings and cultural cues ( Brown 2014 ). Systemically, federal guidelines and individual IRBs must reconsider policies that address language barriers, especially in the informed consent process, to facilitate research participation by LEP individuals (Resnik 2006; Glickman 2011 ; Livaudais-Toman 2014 ). Fear of deportation amongst undocumented immigrants related to research participation has been identified as a source of mistrust and fear ( Brown 2014 ). As a corrective action, study policies on reporting of undocumented immigrants should be noted in each study protocol and explicitly described during participant recruitment.
Disability Status as a Predictor of Mistrust
People with disabilities, an often marginalized group, are a unique health disparities population (Healthy People 2020). Though they comprised only 4% of our cohort, 20% of all American adults are disabled and have disparate special health needs ( CDC 2012 ). This group is often under-represented in research, just as they were under-represented in our survey, and have been described as having pervasive research trust issues ( McDonald 2013 ). Correspondingly, respondents in this study who self-identified as disabled had significant concerns related to General Trust. More focused research is needed to identify specific issues of mistrust among this group and address health disparities amongst people with intellectual and physical disabilities. Researchers, with federal guidance, need to consider accommodations to special needs (physical plant access, readers for the blind) that would remove barriers, demonstrate respect, and promote fairness and inclusion in research.
Study Limitations
The Community VOICES Study was designed to explore attitudes towards a specific type of research (e.g. EFIC studies), not to investigate research trust/mistrust. The insights that can be gained from our data do, however, highlight important issues to consider in trying to understand and lessen mistrust in medical research of all types. Unfortunately, our survey did not include information about all groups that are underrepresented in research. One such group who may have special research trust issues that merit further study is the Lesbian, Gay, Bisexual, Transgender, and Queer/Questioning (LGBTQ) community and those who are Gender Non-Conforming. Often marginalized, members of sexual orientation and gender identity minorities encompass all genders, races, ethnicities, SESs, and educational backgrounds. There is published literature on LGBTQ attitudes towards research surrounding HIV/AIDS treatment and prevention, which shows high rates of mistrust, often strongly associated with fear of stigmatization ( Berg and Ross 2014 , Sevelius et al. 2016 , Loutfy 2014 ).
However, it is not known if this mistrust is related exclusively to HIV-specific research or impacts general medical research participation, resulting in this broadly categorized group being underrepresented in clinical research findings.
Ethical research processes can help achieve greater participant diversity. This in turn results in research findings that are generalizable to broader segments of the population. Both lack of trust by participants and lack of access to research opportunities may contribute to underrepresentation by certain groups. This study offers a paradigm to understand the lack of trust in clinical research: domains of General Trustworthiness, Perception of Deception, Perception of Exploitation, and Perception of Discrimination. The empirical data collected by this study, supported by systematic literature reviews, suggests specific concerns of underrepresented groups and conceptualizes a framework of global issues. These insights can propel researchers towards effective strategies to promote greater participation by developing and testing group-specific targeted interventions, based upon empirical data. In order to increase research participation among people from diverse racial, ethnic, and socioeconomic backgrounds, the sources of their mistrust will have to be addressed.
Each researcher, study, and study population is unique, requiring that protocols have tailored strategies for engaging the community and recruiting participants in ways that are responsive to these domains of concern. Suggestions for developing tailored and targeted interventions can be found in the extensive literature on community based participatory research ( Corbie-Smith et al. 2015 ; Salsberg et al. 2015 ). However, ethical behavior is not achieved through regulation alone, it requires an ethical character of researchers and institutions. Frequently, researchers view their social contract with the community under study as having well-defined boundaries of time and scope. For many investigators the research relationship commences at informed consent and ends at the final study visit. In order to develop a sense of trust, the individuals and community being researched may require a research relationship with more expansive boundaries ( Kerasidou and Parker 2014 )
Acknowledgments
FUNDING: The Community VOICES Study was supported by Grant # 1R01HL073387 from the National Heart, Lung and Blood Institute of the National Institutes of Health.
AUTHOR CONTRIBUTIONS: All authors made substantive contributions to study conception and design. Data was collected primarily by J. H. and C.C. All authors participated in data analysis with G.W. providing statistical guidance. M.S. and L.D.R. (Principal Investigator) were primary authors of the manuscript. All authors critically reviewed the document prior to giving approval for publication and agree to be accountable for all aspects of the work.
CONFLICTS OF INTEREST: None.
ETHICAL APPROVAL: This study was approved by the Icahn School of Medicine at Mount Sinai Institutional Review Board.
- Agency for Healthcare Research and Quality. National healthcare and disparities report. U.S. Department of Health & Human Services; 2010. [ Google Scholar ]
- Armstrong K, McMurphy S, Dean LT, Micco E, Putt M, Halbert CH, Schwartz JS, Sankar P, Pyeritz RE, Bernhardt B, Shea JA. Differences in the patterns of health care system distrust between blacks and whites. Journal of General Internal Medicine. 2008; 23 (6):827–33. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Berg RC, Ross MW. The Second Closet: A Qualitative Study of HIV Stigma Among Seropositive Gay Men in a Southern U.S. City. International Journal of Sexual Health. 2014; 26 (3):186–99. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brandon DT, Isaac LA, LaVeist TA. The legacy of Tuskegee and trust in medical care: Is Tuskegee responsible for race differences in mistrust of medical care? Journal of the National Medical Association. 2005; 97 (7):951–6. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Braunstein JB, Sherber NS, Schulman SP, Ding EL, Powe NR. Race, medical researcher distrust, perceived harm, and willingness to participate in cardiovascular prevention trials. Medicine (Baltimore) 2008; 87 (1):1–9. [ PubMed ] [ Google Scholar ]
- Brown G, Marshall M, Bower P, Woodham A, Waheed W. Barriers to recruiting ethnic minorities to mental health research: a systematic review. International Journal of Methods in Psychiatric Research. 2014; 23 (1):36–48. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Byrd GS, Edwards CK, Keklar VA, Phillips RG, Byrd JR, Pim-Pong DS, Starks TK, Taylor AL, McKinley RE, Li YJ, Pericak-Vance M. Recruiting intergenerational African American males for biomedical research studies: A major research challenge. Journal of the National Medical Association. 2011; 103 (6):480–487. [ PubMed ] [ Google Scholar ]
- Centers for Disease Control and Prevention. Inclusion of women and racial and ethnic minorities in research. U.S. Public Health Service; 2010. [ Google Scholar ]
- Centers for Disease Control and Prevention. Disability and Health. U.S. Public Health Service; 2012. [ Google Scholar ]
- Centers for Disease Control and Prevention, National Center for Health Statistics. Healthy People 2020: Disability and Health. 2015. [ Google Scholar ]
- Corbie-Smith G, Thomas SB, St George DM. Distrust, race and research. Archives of Internal Medicine. 2002; 162 :2458–2463. [ PubMed ] [ Google Scholar ]
- Corbie-Smith G, Moody-Ayers S, Thrasher AD. Closing the circle between minority inclusion in research and health disparities. Archives of Internal Medicine. 2004; 164 :1362–64. [ PubMed ] [ Google Scholar ]
- Cprbie-Smith G, Bryant AR, Walker DJ, Blumentahal C, Council B, Courtney D, Adimora A. Building capacity in community-based participatory research partnerships through a focus on process and multiculturalism. Progress in Community Health Partnerships. 2015; 9 (2):261–73. [ PubMed ] [ Google Scholar ]
- Corbie-Smith G, Williams IC, Blumenthal C, Dorrance J, Estroff JSE, Henderson GG. Relationships and communication in minority participation in research: Multidimensional and multidirectional. Journal of the National Medical Association. 2007; 99 (5):489–499. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Durant RW, Legedza AT, Marcantonio ER, Freeman MB, Landon BE. Different types of distrust in clinical research among Whites and African Americans. Journal of the National Medical Association. 2011; 103 (2):123–30. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Farmer DF, Jackson SA, Camacho G, Hall MA. Attitudes of African American and low socioeconomic status white women toward medical research. Journal of Health Care for the Poor and Underserved. 2007; 18 :85–99. [ PubMed ] [ Google Scholar ]
- Fields A, Abraham M, Gaughan J, Haines C, Hoehn KS. Language matters: Race, trust and outcomes in the pediatric emergency department. Pediatric Emergency Care. 2016; 32 :222–226. [ PubMed ] [ Google Scholar ]
- George S, Duran N, Norris K. A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. American Journal of Public Health. 2014; 104 (2):e16–e31. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Glickman SW, Ndubuizu A, Weinfurt KP, Hamilton CD, Glickman LT, Schulman KA, Cairns CB. Perspective: The case for research justice: Inclusion of patients with limited English proficiency in clinical research. Academic Medicine. 2011; 86 (3):389–93. [ PubMed ] [ Google Scholar ]
- Hall MA. Researching medical mistrust in the United States. Journal of Health Organization and Management. 2006a; 20 (5):456–467. [ PubMed ] [ Google Scholar ]
- Hall MA, Camacho F, Lawlor JS, DePuy V, Sugarman J, Weinfurt K. Measuring trust in medical researchers. Medical Care. 2006b; 44 (11):1048–1053. [ PubMed ] [ Google Scholar ]
- Hughes TB, Varma VR, Pettigrew C, Albert MS. African Americans and clinical research: Evidence concerning barriers and facilitators to participation and recruitment recommendations. Gerontologist. 2015 pii:gnv 118. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kagawa-Singer M. Improving the validity and generalizability of studies with underserved U.S. populations expanding the reach paradigm. Annals of Epidemiology. 2000; 10 :S92–S103. [ PubMed ] [ Google Scholar ]
- Kerasidou S, Parker M. Does science need bioethicists? Ethics and science collaboration in biomedical research. Research Ethics. 2014; 10 (4):214–226. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lang R, Kelkar VA, Byrd JR, Edwards CL, Pericak-Vance M, Byrd GS. African American participation in health-related research studies:indicators for effective recruitment. Journal of Public Health Management and Practice. 2013; 19 (2):110–18. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Limkakeng AT, de Oliveira LL, Moreira T, Phadtare A, Garcia Rodriques C, Hocker MB, McKinney R, Voils CI, Pietrobon R. Systematic review and metasummary of attitudes toward research in emergency medical conditions. Journal of Medical Ethics. 2014; 40 (6):401–8. [ PubMed ] [ Google Scholar ]
- Livaudais-Toman J, Burke NJ, Napoles A, Kaplan CP. Health literate organizations: Are clinical trial sites equipped to recruit minority and limited health literacy patients? Journal of Health Disparities and Research Practice. 2014; 7 (4):1–13. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Loutfy MR, LKV, Mohammed S, Wu W, Muchenje M, Masinde K, Salam K, Soje L, Gregorovich S, Thardo W. Recruitment of HIV positive women in research: Discussing barriers, facilitators and research personnel’s knowledge. Open AIDS Journal. 2014; 19 (8):58–65. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mainous AG, 3rd, Smith DW, Geesey ME, Tilley BC. Development of a measure to assess patient trust in medical researchers. Annals of Family Medicine. 2006; 4 (3):247–52. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- McDonald KE, Kidney CA, Patka M. You need to let your voice be heard: research participant views on research. Journal of Intellectual Disability Resarch. 2013; 57 (3):216–215. [ PubMed ] [ Google Scholar ]
- McDonald M, Townsend A, Cox SM, Paterson ND, LaFreniere D. Trust in health research relationships: Accounts of human subjects. Journal of Empirical Research in Human Research Ethics. 2008; 3 (4):35–47. [ PubMed ] [ Google Scholar ]
- McKinstry B, Ashcroft REE, Car J, Freeman GK, Sheikh A. Interventions for improving patients’ trust in doctors and groups of doctors. Cochrane Database System Review. 2006 doi: 10.1002/14651858.CD004134.pub2. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moreno G, Mangione CM, Meza CE, Kwon I, Seeman T, Trejo L, Moore M, Sarkisian CA. Perceptions from Latino and African American older adults about biological markers in research. Ethnicity and Disease. 2015; 25 (3):355–62. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Moreno-Jones G, Gachie CM, Fleming A, Napoles-Springer A, Mutran E, Manson SM, Perez-Stable EJ. Ethnic minority older adults participating in clinical research: Developing trust. Journal of Aging Health. 2004; 16 (5 supplement):93S–123S. [ PubMed ] [ Google Scholar ]
- Ornato JP, McBurnie MA, Nichol G, Salive M, Weisfeldt M, Riegel B, Christenson J, Terndrup T, Daya M PAD Trial Investigators. The public access defibrillation (PAD) trial: Study design and rationale. Resuscitation. 2003; 56 (2):135–47. [ PubMed ] [ Google Scholar ]
- Ragin DF, Ricci E, Rhodes J, Holohan R, Smirnoff M, Richardson LD. Defining the “community” in community consultation for emergency research: Findings from the Community VOICES Study. Social Science and Medicine. 2008; 66 (6):1379–92. [ PubMed ] [ Google Scholar ]
- Richardson LD. The ethics of research without consent in emergency situations. Mount Sinai Journal of Medicine. 2005; 72 (4):242–9. [ PubMed ] [ Google Scholar ]
- Richardson LD, Gunnels MD, Groh WJ, Peberdy MA, Pennington I, Wilets S, Campbell V, Van Ottingham L, McBurnie MA PAD Trial Investigators. Implementation of community-based public access defibrillation in the PAD trial. Academic Emergency Medicine. 2005; 12 (8):688–97. [ PubMed ] [ Google Scholar ]
- Salsberg J, Parry D, Pluye P, Macrides S, Herbert CP, Macaulay AC. Successful strategies to engage research partners for translating evidence into action in community health: A critical review. Journal of Environmental and Public Health. 2015; 2015 :191856. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Scharff DP, Mathews KJ, Jackson P, Hoffsuemmer J, Martin E, Edwards D. More than Tuskegee: Understanding mistrust about research participation. Journal of Health Care for the Poor and Underserved. 2010; 21 (3):879–97. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schmotzer GL. Barriers and facilitators to participation of minorities in clinical trials. Ethnicity and Disease. 2012; 22 (2):226–30. [ PubMed ] [ Google Scholar ]
- Sevelius JM, Deutsch MB, Grant R. The future of PrEP among transgender women: The critical role of gender affirmation in research and clinical practice. Journal of the International AIDS Society. 2016; 19 (7 Supp 6):21105. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shelton RC, Winkel SN, Davis G, Roberts N, Valdimarsdottir H, Hall SJ, Thompson HS. Journal of General Internal Medicine. 2010; 25 (6):549–55. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- PAD Trial Investigators. The Public Access Defibrillation and Survival from Out-of-Hospital Cardiac Arrest. New. England Journal of Medicine. 2004; 351 :637–46. [ PubMed ] [ Google Scholar ]
- Thompson HS, Valdimarsdottir HB, Winkel G, Jandorf L, Redd W. The Group-Based Medical Mistrust Scale: Psychometric properties and association with breast cancer screening. Preventive Medicine. 2004; 38 :209–218. [ PubMed ] [ Google Scholar ]
- Traverso-Yepez M, Maddalena V, Bavington W, Donovan C. Community capacity building for health: A critical look at the practical implications of this approach. SAGE Open. 2012 Jun;:1–12. [ Google Scholar ]
- Tilburt J, Ford JG, Howerton MW, Gary TL, Lai GY, Bolen S, Baffi C, Wilson RF, Tanpitukpongse TP, Powe NR, Bass EB, Sugarman J. Applying justice in clinical trials for diverse populations. Clinical Trials. 2007; 4 :264–269. [ PubMed ] [ Google Scholar ]
- U.S. Census Bureau. 2010 Census. U.S. Department of Commerce; 2010. [ Google Scholar ]
- U.S. Census Burea. America speaks: A demographic profile of foreign language speakers for the US: 2000. U.S. Department of Commerce; 2000. [ Google Scholar ]
- U.S. Census Bureau. American Community Survey 2013. U.S. Department of Commerce; 2013. [ Google Scholar ]
- US Department of Health & Human Services. NIH guidelines on the inclusion of women and minorities as subjects in clinical research. NIH GUIDE. 1993; 23 (11):59FR11146–11151. [ Google Scholar ]
- US Department of Health & Human Services. Protection of human subjects: Informed consent and waiver of informed consent requirements in certain emergency research. Final Rules. (21 CFR Part 50.24 and 45 CFR Part 46.1010) Federal Register. 1996 Oct 2; 61 :51498–533. [ PubMed ] [ Google Scholar ]
- US Department of Health & Human Services Food and Drug Administration. Guidance for Institutional Review Boards, Clinical Investigators and Sponsors: Exception from Informed Consent for Emergency Research. Federal Register. 2000 Mar 30; [ Google Scholar ]
- U.S. Department of Health & Human Services. Amendment: NIH Policy and Guidelines on the inclusion of women and minorities as subjects in clinical research. National Institutes of Health; 2001. [ Google Scholar ]
- US Department of Health and Human Services Food and Drug Administration. Draft Guidance for Institutional Review Boards, Clinical Investigators, and Sponsors: Exception from Informed Consent for Emergency Research, July 2006. 71. Federal Register. 2006 Aug 29;:51143. [ Google Scholar ]
- US Department of Health and HumanServices Food and Drug Administration. Guidance for Institutional Review Boards, Clinical Investigators, and Sponsors: Exception from Informed Consent for Emergency Research, March 2011. 76. Federal Register. 2011 Apr 4; 64 :18558–18559. [ Google Scholar ]
- U.S. Department of Health and Human Services National Institutes of Health. Monitoring Adherence to the NIH Policy on the Inclusion of Women and Minorities as Subjects in Clinical Research; Comprehensive Report: Tracking of Human Subjects Research as Reported in Fiscal Year 2008 and Fiscal Year 2009. 2010 http://orwh.od.nih.gov/research/inclusion/pdf/Inclusion-ComprehensiveReport-FY-2008-2009.pdf .
- Wright S. Trust and trustworthiness. Philosophia. 2010; 38 (3):615–27. [ Google Scholar ]
- Yarborough M, Edwards K, Espinoza P, Geller G, Sarwal A, Sharp R, Spicer P. Relationships hold the key to trustworthy and productive translational science: recommendations for expanding community engagement in biomedical research. Clinical Translational Science. 2013; 6 (4):310–3. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zong J, Batalova J. The limited English proficient population in the United States. Migration Policy Institue; 2015. [ Google Scholar ]
- Open access
- Published: 04 April 2024
Trust as a catalyst: revealing the impact of government trust and professional trust on public health policy compliance during a pandemic
- Guobang Chen ORCID: orcid.org/0009-0000-1594-6446 1 ,
- Hua Zhang ORCID: orcid.org/0000-0002-1690-2063 1 ,
- Yue Hu ORCID: orcid.org/0009-0006-7368-1494 1 &
- Chunyan Luo ORCID: orcid.org/0009-0006-4587-2496 1
BMC Public Health volume 24 , Article number: 957 ( 2024 ) Cite this article
213 Accesses
Metrics details
Existing research has extensively explored the relationship between government trust and compliance behaviour, but significant controversies exist. Some studies suggest a strong positive correlation between the two. Other studies have found that government trust hinders compliance behaviour. However, during the pandemic, the effectiveness of public health policies largely depends on the public’s compliance with these policies. To examine the aforementioned controversies, this study utilizes survey data on the Chinese population during the COVID-19 period to explore the relationship between compliance with public health policies and government trust.
The study conducted a questionnaire survey of 1,395 individuals from 25 provinces in China from mid-November to mid-December 2022. Firstly, we categorized the public’s compliance behaviour with public health policies based on the results of factor analysis. Subsequently, we examined the impact of government trust and professional trust on compliance behaviour with public health policies by constructing a structural equation model.
Based on the results of factor analysis, we classified public adherence to public health policies into protective compliance and restrictive compliance. Results from the structural equation model show a positive correlation between the public’s trust in the government and both protective and restrictive compliance, with a stronger influence on protective compliance. Government trust also exerts a positive impact on restrictive compliance behaviour through professional trust. Additionally, the study indicates a significant positive correlation between the public’s professional trust and restrictive compliance, while it does not significantly affect protective compliance. Moreover, the public from rural areas demonstrates a greater willingness to adhere to both types of public health policies. Married individuals exhibit a stronger inclination toward protective compliance, while females show a stronger tendency toward restrictive compliance.
The study revealed a significant positive impact of government trust and professional trust on compliance behaviour with public health policies during the COVID-19 pandemic, refuting any negative correlation between government trust and compliance behaviour. Normative motivations for compliance behaviour had a substantial impact on adherence. These findings offer valuable insights for future public health crisis management and public policy formulation.
Peer Review reports
Amid the COVID-19 pandemic, numerous nations’ authorities have instituted and enforced a range of containment measures, encompassing social distancing, travel constraints, and vaccination protocols. In the implementation of these policies, the level of public compliance is one of the key factors influencing their effectiveness [ 1 ]. However, stimulating public willingness to comply with the epidemic prevention policies remains a challenging task that governments need to address.
Previous studies have indicated that individuals evaluate the suitability and legitimacy of measures based on scientific, legal, moral, and values-based considerations [ 2 ]. Research on individual compliance behaviour has categorized motivations into calculative and normative motives. Calculative motives encompass the individual’s inclination to comply after considering the costs and benefits, drawing from theories such as deterrence theory, protection motivation theory, and prospect theory [ 3 , 4 , 5 , 6 ]. Previous research has extensively examined the influence of factors such as risk perception and self-efficacy on compliance behaviour [ 7 , 8 , 9 ]. In contrast, normative motives highlight individuals’ internal moral beliefs, values, and social norms, suggesting that these factors drive voluntary adherence to regulations [ 10 , 11 ]. Studies have widely explored the effects of factors such as trust in the government, professional trust, individual cognition, and cultural context on compliance behaviour [ 7 , 12 , 13 , 14 , 15 , 16 ].
Within these, research on the connection between trust in the government under normative motives and compliant behaviour is abundant, yet substantial differences in viewpoints exist. Some studies suggest a positive association between government trust and compliance behaviour, indicating that the public’s trust in the government leads to a greater inclination to support government measures and solutions, as well as a greater willingness to adhere to related policies [ 12 , 13 , 17 , 18 ]. Certain studies have found a weak correlation between government trust and compliance behaviour [ 19 , 20 ]. There are even studies that have discovered a negative association between government trust and compliance behaviour, exemplified by trust paradox perspectives and support paradox perspectives [ 21 , 22 ].
The aforementioned discrepancies emphasize the intricate correlation between government trust and compliance behaviour. In the context of contemporary society, the confluence of technological advancements and globalization has engendered a persistent stream of novel risks and uncertainties. People are confronted with complex risk challenges such as environmental pollution, technological disasters, and global climate change, necessitating joint efforts from society, governments, and individuals to address various issues within the realm of risk society [ 23 ]. Therefore, studying public compliance behaviour and its motivations is paramount. Our study seeks to investigate the relationship between government trust, professional trust, and compliance behaviour, employing a structural equation model for analysis. This model is commonly utilized to ascertain causal relationships between variables, encompassing both direct and indirect influences. Its strengths lie in evaluating the intricate interconnections among observed variables and testing complex theoretical models.
Theoretical background
Compliant behaviour and its motives.
Previous research on individual compliance behaviour has primarily been conducted from the perspectives of calculative motives and normative motives. Calculative motives encompass the individual’s motivation to comply after weighing the costs and benefits [ 24 ], including deterrence theory, protection motivation theory, and prospect theory. Deterrence theory posits that strict policies and enforcement will enhance the public’s motivation to comply with the policies [ 6 ]. The protection motivation theory emphasizes that individual decisions are driven by their perceptions of risk and self-efficacy [ 4 , 5 , 25 ], such as adherence to public health policies for the sake of safeguarding personal interests [ 26 ]. Prospect theory divides the decision-making process into two critical stages: an early editing phase that involves a preliminary analysis of the provided prospects, often leading to simplified presentations of these prospects. This is followed by an evaluation phase that assesses the edited prospects, selecting those with the highest value [ 3 ].
Differing from calculative motives, normative motives emphasize that individuals’ internal moral beliefs, values, and social norms drive them to voluntarily adhere to regulations. These may include an acknowledgment of social responsibility, concern for the health of others, trust in the government, policy legitimacy, and policy fairness, among other intrinsic values [ 10 , 11 ]. During the COVID-19 pandemic, research has found that normative motives are the primary driving force behind compliance behaviour [ 7 , 8 , 9 , 17 , 27 ]. Studies have also revealed that government trust and individual responsibility are the primary influencing factors for public compliance behaviour among young people in China during the COVID-19 pandemic [ 28 ]. In the context of a pandemic, as the majority of public health policies are issued by the government, government trust becomes a key factor motivating compliance behaviour.
Government trust and individual compliance behaviour
Government trust encompasses confidence in the government’s consistency in words and actions and its commitment fulfillment [ 12 ]. Generally, those who trust the government are more likely to support government measures and solutions and are more willing to comply with related policies [ 13 ]. Conversely, low government trust may result in the public’s reluctance to follow government decisions, leading the government to implement mandatory measures to enforce regulations, thus increasing the complexity and cost of governance [ 29 ]. Research has shown this to be the case during the COVID-19 pandemic as well. Studies have found that in regions with high government trust in Italy, the public responded actively to government calls, reducing their outings during the pandemic [ 17 ]. Other studies have indicated a negative correlation between government trust and the number of COVID-19 cases and mortality rates [ 30 ]. Furthermore, there is a mutually reinforcing relationship between the public’s trust in the government and the effectiveness of policies. An increase in government trust can enhance the management of the pandemic, and positive pandemic management outcomes not only restore damaged government trust but also create spillover effects, further increasing public trust in the government. This mutually reinforcing relationship is crucial for establishing a stable and sustainable pandemic management mechanism [ 31 , 32 ].
However, not all studies consistently demonstrate a positive correlation between government trust and compliance behaviour. Some studies have found a weak association between government trust and compliance behaviour [ 19 , 20 ]. Jørgensen et al.‘s (2020) research found that institutional trust had a relatively limited promoting effect on compliance behaviour during the first wave of the COVID-19 pandemic [ 19 ]. A study conducted in the Netherlands also indicated that higher levels of government trust were only positively related to the willingness to accept vaccination and unrelated to the willingness to adopt additional hygiene measures [ 25 ]. Some studies have even discovered a negative correlation between government trust and compliance behaviour. These perspectives are known as the “trust paradox” and the “support paradox.” The trust paradox perspective suggests that confidence in governmental institutions can alleviate the pressures associated with a pandemic. Consequently, the higher the public’s confidence in governmental institutions, the more they may perceive no need to take personal action to avoid infection and restrict the spread of the virus [ 22 ]. The fundamental assumption of the trust paradox perspective is that the COVID-19 pandemic is psychologically perceived as a stressor, and trust serves as a psychological defense mechanism, providing a sense of security and stability during uncertain times. Consequently, if the public has confidence in the government’s capabilities and decisions in managing the pandemic, they may be more inclined to believe that the measures taken by the government are sufficient to control the outbreak, thereby reducing the need for individuals to take additional protective measures [ 21 , 33 , 34 ].
Furthermore, the support paradox perspective posits that when the public perceives the government’s effective performance in managing the pandemic, their perception of risk may weaken. Consequently, they might underestimate the severity of the pandemic and their own risk, leading to a relaxation of the importance placed on personal protective measures and a decrease in the willingness to comply with regulations [ 21 ]. The support paradox perspective is based on the “trust, confidence, and cooperation (TCC)” model in the field of risk management, which suggests that when confidence is excessive or blind, people may ignore or underestimate potential risks because they excessively rely on a specific responsible party or institution. In such circumstances, higher confidence may lead to a decrease in risk perception. Conversely, when people lack confidence in the relevant parties, they may become more vigilant and sensitive, thus tending to adopt a cautious attitude toward risks. In this scenario, lower trust can lead to an increase in risk perception [ 21 , 23 ]. In the most severely affected regions in Italy, the effective performance of the regional systems during the pandemic enhanced people’s sense of security, thereby reducing their willingness to comply with restrictive measures, giving rise to the “support paradox” [ 21 ].
The role of professional trust
The aforementioned studies underscore the significant relationship between government trust and adherence to policy compliance. Additionally, research has indicated that public trust in professionals serves as a crucial predictive factor for policy compliance, particularly in the context of public health compliance behaviours, given the intricate and specialized nature of knowledge related to pandemics and infectious diseases [ 27 ]. For instance, after previous events such as the avian flu and the 2009 H1N1 influenza pandemic, public trust in professionals emerged as a novel predictive indicator for assessing the adherence to official recommendations concerning protective measures [ 7 ]. During the 2009 H1N1 period, following the French public health department’s calls for practices like frequent handwashing and mask-wearing, more than a third of the public reported an increased frequency of handwashing as a preventive measure [ 14 ]. A higher level of professional trust among the public corresponds to a greater willingness to seek healthcare assistance and a stronger inclination to adhere to disease prevention measures [ 35 ]. Conversely, a crisis of trust between the public and health authorities can have adverse effects, as individuals who harbor distrust in healthcare institutions may not comply with official guidance regarding protective measures [ 7 , 36 ]. Professional trust encompasses reliance on others’ competence, specialized knowledge, and judgment [ 37 ]. Moreover, some research suggests that professional trust acts as an intermediary variable between trust in the government and the adoption of personal protective measures by respondents. In cases where public trust in the government is low, professional trust motivates them to implement personal protective measures, ultimately resulting in satisfactory outcomes [ 26 ].
The research also points out that the public’s professional trust is influenced by a combination of various factors, among which trust in the government significantly and strongly affects professional trust [ 26 ]. Individuals with a positive and open-minded approach are more inclined to trust public health experts [ 38 ]. It is important to note that the public’s interpretation and understanding of pandemic information based on their own knowledge reservoirs can lead to a loss of confidence in health officials [ 39 ].
Research framework and hypotheses
Based on the literature reviewed above, we constructed a model of public health policy compliance behaviour incorporating government trust and professional trust. Public health policy compliance can manifest in various ways as different countries provided different recommendations to their populations during public health crises [ 40 ]. For the COVID-19 pandemic, common measures adopted by governments worldwide include wearing masks, hand hygiene, maintaining social distancing in public places, and vaccination. Some governments tended to implement additional measures to protect their populations as their understanding of the crisis deepened [ 40 ]. For instance, in order to identify infected individuals, China also implemented measures such as presenting nucleic acid test certificates, health codes and travel card, and refraining from going out during lockdowns. Numerous measures were implemented by various countries during the pandemic, and for the sake of simplicity in the model, we merged multiple types of measures. Some researchers have categorized public health policies into protective compliance and restrictive compliance. Drawing on previous research [ 28 ], we similarly divided the public health policies enacted by the Chinese government into protective compliance and restrictive compliance.
Firstly, previous research indicates that during the COVID-19 pandemic, public trust in the government has a significant impact on their adherence to public health measures. Some studies have found that the public’s trust in the government leads to a greater inclination to support and comply with government measures and solutions [ 1 , 12 , 13 , 17 ], while lower levels of government trust may result in the public’s reluctance to comply with government decisions, thereby forcing the government to resort to more coercive management measures [ 29 ]. Conversely, some scholars have proposed the trust paradox and support paradox viewpoints. The trust paradox viewpoint suggests that the level of public trust in government institutions is negatively correlated with their adherence to public health policies [ 22 ]. The support paradox viewpoint posits that during the COVID-19 pandemic, the public’s satisfaction with the government’s performance is negatively correlated with their willingness to adhere to regulations [ 21 ]. Therefore, this study presents competing hypotheses regarding the relationship between government trust and adherence to public health policies.
During public health crises, public trust in the government is positively correlated with compliance behaviour (protective compliance a; restrictive compliance b).
During public health crises, public trust in the government is negatively correlated with compliance behaviour (protective compliance a; restrictive compliance b).
In addition to trust in the government making it easier for people to accept existing regulations and restrictions, the public’s professional trust is also closely related to their compliance behaviour [ 14 , 27 ]. The stronger the public’s professional trust, the stronger their willingness to seek healthcare assistance and adhere to disease prevention measures [ 14 , 35 ]. Conversely, a trust crisis between the public and health authorities may have adverse effects on public adherence to recommendations [ 36 ], as those who do not trust healthcare institutions may not follow official protective measures [ 7 ]. Therefore, we propose hypotheses H2.1 and H2.2.
During the public health crisis, the public’s professional trust is positively correlated with protective compliance behaviour.
During the public health crisis, the public’s professional trust is positively correlated with restrictive compliance behaviour.
Previous research has also indicated that professional trust plays a mediating role between government trust and respondents’ adoption of personal protective measures. When the public has lower levels of trust in the government, professional trust prompts them to take individual protective measures, ultimately yielding satisfactory results. Therefore, we propose hypotheses H3.1 and H3.2.
Government trust has a positive effect on protective compliance through professional trust.
Government trust has a positive effect on restrictive compliance through professional trust.
Figure 1 illustrates the theoretical framework and hypotheses of this study.
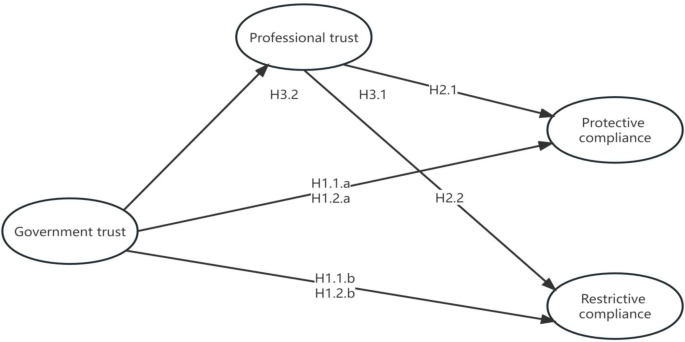
The hypothesized theoretical model with a structural equation model
Materials and methods
Data collection.
The questionnaire for this study was distributed from mid-November to late December 2022. Due to the restrictions of the home isolation policy, from mid-November to early December, we only distributed the questionnaire to university students through online platforms such as email and social media. In mid-December 2022, with the lifting of the home isolation policy, we used offline methods to distribute the questionnaire to on-campus students. A total of 1436 university students completed the questionnaire, distributed across 25 administrative regions. To ensure that participants would not be coerced into completing the questionnaire, we included an anonymous statement in the first part of the questionnaire. After completing the data collection, we excluded invalid questionnaires that were duplicates or incomplete, ultimately obtaining 1395 valid questionnaires.
Statistical methods
After the completion of data collection, we conducted statistical analysis using STATA 15.1 software. Firstly, descriptive analysis of the data was performed. Subsequently, we conducted factor analysis and constructed a structural equation model to delve into the impact of public trust in the government and professional trust on their compliance with public health policies.
Standard protocol approvals, registrations, and participants consent
Standard protocol approvals, registrations, and participants consent Informed consent was obtained from all the participants in the study. The study was approved by the Academic Ethics Committee of School of Politics Science and Public Administration, Guangxi Minzu University. The present study was conducted in accordance with the principles of the 2013 Declaration of Helsinki.
Variables and measurements
- Compliance behaviour
The public’s compliance with public health policies is the main outcome variable of the study. Compliance with public health policies can take various forms, as different countries have provided their populations with different recommendations during public health crises [ 40 ]. During the COVID-19 pandemic, wearing masks, handwashing, maintaining social distance in public places, and vaccination have been commonly adopted policies by governments worldwide. Following a deeper understanding of the crisis, some governments inclined towards implementing additional measures to protect the public [ 40 ]. For instance, in China, measures such as presenting nucleic acid test certificates, health codes and travel card, and refraining from going outside during lockdown periods were adopted to identify infected individuals. To assess the public’s adherence to public health policies during the COVID-19 pandemic, we employed a Likert five-point scale to measure respondents’ compliance with seven official recommendations (wearing masks, handwashing, maintaining social distance in public places, vaccination, presenting nucleic acid test certificates, presenting health codes and travel card, and refraining from going outside during lockdown periods) (Cronbach’s alpha = 0.81). Participants were required to select a numerical value ranging from 1 to 5 based on statements, with 1 indicating “never complied” and 5 indicating “always complied.” Higher scores indicate a higher level of compliance with public health policies among the respondents.
According to the results of the factor analysis of the seven compliance behaviours, after orthogonal rotation, two factors with eigenvalues greater than 1 were obtained, namely 2.188 and 1.636. The variance explained by the two factors was 0.6614 and 0.4945, respectively. Based on the results of the factor analysis and drawing on the research by Huang (et al., 2023) [ 28 ], we divided the public’s compliance with public health policies into two main factors (see Table 1 ). Factor 1 was named “Restrictive Compliance” (Cronbach’s alpha = 0.79), including vaccination, presenting nucleic acid test certificates, presenting health codes and travel card, and refraining from going outside during lockdown periods, with factor loadings of 0.6121, 0.7941, 0.8384, and 0.5637, respectively. Factor 2 was named “Protective Compliance” (Cronbach’s alpha = 0.82), including wearing masks, handwashing, and maintaining social distance in public places, with factor loadings of 0.6692, 0.6819, and 0.7102, respectively.
- Government trust
Government trust is a key independent variable in this study. To measure respondents’ levels of trust in the government, we asked the following two questions: “Currently, how satisfied are you with the central government?” and “Currently, how satisfied are you with the local government in your district/county?” Participants were required to select a value within the range of 1 to 5, where 1 represented “very dissatisfied” and 5 represented “very satisfied.” Higher scores indicated a higher level of trust in the government among the respondents (Cronbach’s alpha = 0.83).In our study, the government trust variable was constructed through exploratory factor analysis, examining the questions “Currently, how satisfied are you with the central government?” and “Currently, how satisfied are you with the local district/county government?” After orthogonal rotation, a factor with an eigenvalue of 1.217 and a variance explained of 1.203 was obtained, with a factor loading of 0.78 (see Table 1 ).
- Professional trust
Professional trust is also a crucial variable in this study. To measure respondents’ levels of professional trust, we asked the following two questions: “How much do you trust healthcare professionals?” and “How much do you trust healthcare institutions?” Participants were required to select a value between 1 and 5, where 1 represented “strongly distrust” and 5 represented “strongly trust.” Higher scores indicated a higher level of professional trust among the respondents (Cronbach’s alpha = 0.88).The professional trust variable was also constructed through exploratory factor analysis, examining the questions “How much do you trust healthcare professionals?” and “How much do you trust healthcare institutions?” After orthogonal rotation, a factor with an eigenvalue of 1.429 and a variance explained of 1.128 was obtained, with a factor loading of 0.845 (see Table 1 ).
Demographic variables
Previous research has shown that age, gender, and marital status have important effects on individual compliance behaviour [ 41 , 42 , 43 ]. In our study, we used four demographic variables: the respondent’s gender (0 = male, 1 = female); the respondent’s marital status (0 = single, 1 = married); the respondent’s political affiliation (0 = Chinese Communist Party member, 1 = non-Chinese Communist Party member); the respondent’s household registration (0 = rural household registration, 1 = urban household registration).
Demographic characteristics
Table 2 displays the basic characteristics of the control variables. Among the 1395 samples, male citizens accounted for 22.58%, while female citizens accounted for 77.42%; Citizens under the age of 24 account for 93.32%, citizens between 24 and 35 years old account for 5.52%, and citizens over the age of 35 account for 1.15%.citizens with urban household registration accounted for 37.92%, while those with rural household registration accounted for 62.08%. Citizens with membership in the Chinese Communist Party accounted for 7.60% of the total sample, while citizens without membership accounted for 92.40%.Single citizens account for 94.77%, married citizens account for 5.23%. Citizens with education below college level account for 9.46%, while citizens with college education or above account for 90.54%.
Descriptive statistics and correlation analysis of study variables
Table 3 presents the descriptive statistics and correlation analysis of the study variables. Among the seven compliance behaviours, “Providing health codes and travel card” had the highest average score (4.85), followed by “Providing nucleic acid test certificates” (4.80), “Vaccination” (4.77), “Compliance with not going out during lockdown periods” (4.74), “Wearing masks” (4.42), “Handwashing” (4.40), and the lowest average score was for “Maintaining social distance in public places” (3.90). Regarding government trust, the average score for the central government was 4.10, slightly higher than that for the district/county government (3.83). As for professional trust, the average score for trust in healthcare professionals (4.07) did not differ much from the average score for trust in healthcare institutions (4.03).
During the COVID-19 pandemic, the average scores for the four restrictive compliance behaviours, “Presenting health codes and travel card,” “Presenting nucleic acid test certificates,” “Vaccination,” and “Compliance with not going out during lockdown periods,” were much higher than the average scores for protective compliance (handwashing, wearing masks, maintaining social distance in public places). This result is consistent with our research expectations. This is because during the COVID-19 pandemic, the Chinese government implemented strict restrictive public health policies to ensure the safety of public mobility, and non-compliance with these policies would result in direct consequences of restricted mobility.
During the COVID-19 pandemic, we observed a series of behavioural differences related to public characteristics, which to some extent reflected different responses to prevention and control measures (see Table 3 ). We found that individuals with rural household registration were more willing to wear masks ( p = 0.025), handwashing ( p = 0.016), present nucleic acid test certificates ( p < 0.001), present health codes and travel card ( p = 0.003) and comply with not going out during lockdown periods ( p = 0.001). Citizens with membership in the Chinese Communist Party were more willing to get vaccinated ( p = 0.036). Additionally, males showed a higher willingness to maintain social distance in public places ( p = 0.018), while females were more willing to present nucleic acid test certificates ( p = 0.013) and health codes and travel card ( p = 0.004). Married individuals paid more attention to hand hygiene during the pandemic ( p = 0.034).
The results of SEM
In order to further explore the impact of government trust and professional trust on public compliance with public health policies, we constructed a structural equation model (see Fig. 2 ). The model showed statistical significance (χ² = 461.70, df = 93, p <0.001) and exhibited acceptable fit indices (CFI = 0.940, TLI = 0.921, RMSEA = 0.057, SRMR = 0.077).
The structural equation model results indicate that public trust in the government significantly influences several factors. Firstly, public trust in the government is significantly positively correlated with protective compliance (a = 0.28, p <0.001; see Table 4 ). Hypothesis H1.1.a is supported, while its competing hypothesis H1.2.a is not supported. Secondly, public trust in the government is also significantly positively correlated with restrictive compliance (a = 0.21, p <0.001; see Table 4 ). Hypothesis H1.1.b is supported, while its competing hypothesis H1.2.b is not supported. Additionally, government trust is significantly positively correlated with professional trust (a = 0.66, p <0.001; see Table 4 ).
We also found that public professional trust is significantly positively correlated with restrictive compliance (a = 0.099, p <0.001; see Table 4 ), confirming hypothesis H2.b. However, we did not find a significant effect of public professional trust on protective compliance (a = 0.028, p = 0.57; see Table 4 ), and hypothesis H2.a was not supported.
Furthermore, we also found that government trust has a significant positive effect on restrictive compliance through professional trust (indirect effect = 0.032, 95% confidence interval [0.002, 0.062]; see Table 4 ), confirming hypothesis H3.b. However, government trust did not have a significant positive effect on protective compliance through professional trust (indirect effect = 0.013, 95% confidence interval [-0.033, 0.06]; see Table 4 ), and hypothesis H3.a was not supported. These findings emphasize the shaping role of government trust during the COVID-19 pandemic on professional trust, protective compliance, and restrictive compliance, as well as the significant influence of professional trust on public restrictive compliance behaviour.
In terms of controlling variables, the results of the structural equation model show that there is no significant correlation between respondents’ age and protective compliance ( p = 0.06) or restrictive compliance ( p = 0.49); respondents’ gender is not significantly correlated with protective compliance ( p = 0.33), and it is significantly negatively correlated with restrictive compliance (β=-0.07, p = 0.017), although this association is weak; respondents’ household registration is not significantly correlated with protective compliance ( p = 0.24) or restrictive compliance ( p = 0.09); respondents’ political affiliation is not significantly correlated with protective compliance ( p = 0.76) or restrictive compliance ( p = 0.22); respondents’ educational level is not significantly correlated with protective compliance ( p = 0.93), and it is significantly negatively correlated with restrictive compliance (β = 0.07, p = 0.012), although this association is weak; respondents’ marital status is not significantly correlated with protective compliance ( p = 0.1) or restrictive compliance ( p = 0.07).
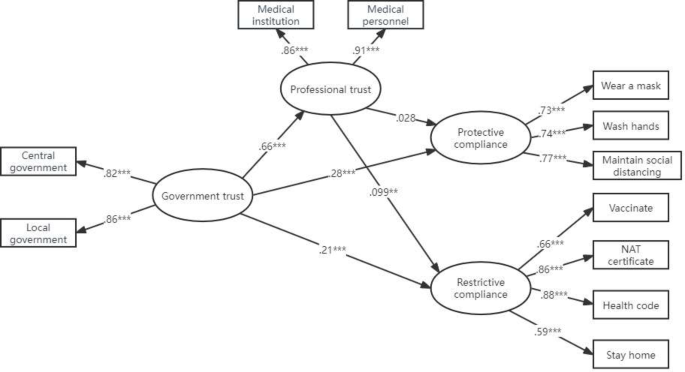
Mediation model with SEM. Note Control variables (gender, age, education, marital status, political landscape and household registration) were included in this model but not presented in this figure
During the COVID-19 pandemic, compliance with epidemic prevention measures is not only an individual’s autonomous choice but also a responsible act and an expression of care for the entire society. Adhering to public health policies, such as wearing masks, maintaining social distance, and getting vaccinated, can effectively slow the spread of the virus, reduce the risk of infection, and protect vulnerable groups and healthcare workers from the virus. Therefore, during the pandemic, the public’s compliance behaviour is a crucial element in overcoming the virus and maintaining social security. Although existing research has indicated that public trust in the government and professional trust are important factors influencing compliance behaviour, there are still some controversies regarding this relationship. Hence, this study constructed a structural equation model to examine the impact of government trust and professional trust under normative motivation on compliance with public health policies during the COVID-19 pandemic.
Vaccination: self-protection or external pressure?
The research findings indicate that, following factor analysis, vaccination was classified as a form of restrictive compliance behaviour. This contradicts previous research, which regarded vaccination during pandemics as a proactive self-protective measure taken by the public [ 28 ]. We suggest two explanations for this phenomenon. Firstly, during the COVID-19 pandemic, many countries have implemented restrictive policies targeting unvaccinated individuals, leading to various limitations on their travel, education, employment, and accommodation in hotels [ 44 , 45 ]. Secondly, widespread vaccine hesitancy regarding the safety of COVID-19 vaccines exists globally [ 46 , 47 , 48 , 49 , 50 ]. This suggests that individual vaccination may be more driven by meeting external demands rather than purely self-protective motives.
Government trust and compliance behavior
The results of the structural equation model indicate that public trust in the government significantly affects both protective compliance and restrictive compliance, with a stronger impact on protective compliance. Our study initially confirmed the positive association between government trust and compliance behaviour [ 13 , 17 , 18 ], not supporting a weak correlation or a negative association between government trust and compliance behaviour. Citizens who trust the government are inclined to perceive government-recommended actions as more beneficial, with fewer obstacles and disadvantages, and as more feasible [ 51 ]. Therefore, they are more likely to support government-proposed measures and solutions, including preventive measures, fiscal aid and economic stimuli, as well as epidemic control solutions [ 12 ]. Moreover, during the COVID-19 pandemic, if some individuals begin to express satisfaction with and support for the government’s measures, this positive sentiment could spread to their social circles, influencing more people to adhere to the government’s epidemic guidance, as they perceive the government as trustworthy and taking appropriate measures to address the crisis. This phenomenon can be described as a cascade of confidence, wherein confidence spreads from one individual or group to another, creating a chain reaction [ 22 ].
Government trust and professional trust
The study results further indicate that the public’s trust in the government also makes them more likely to trust professional healthcare institutions and medical personnel. This suggests that the government plays a crucial role in maintaining the independence and credibility of healthcare institutions and medical personnel [ 26 ]. When formulating public health risk policies and governance decisions, the government often relies on expert systems for decision-making and risk assessment. In the eyes of the public, both expert systems and the government are perceived as “rational-legitimate” authorities [ 52 ]. This leads to the common association of trust in expert systems with trust in the government, forming a shared basis of trust in this context [ 52 ].
Professional trust is significantly positively correlated with restrictive compliance
Our study also confirms the positive influence of professional trust on compliance with public health policies, consistent with previous research [ 7 , 26 , 35 , 36 , 38 , 41 , 53 ]. When the public perceives the medical knowledge of healthcare institutions and medical staff as trustworthy, they are more likely to actively follow their recommendations [ 7 ]. Furthermore, we observed the mediating effect of professional trust, where government trust positively influences compliance with restrictive measures through professional trust. During a crisis, professional trust serves as a complementary mechanism, enhancing the likelihood of the government’s ability to encourage individuals to adopt personal protective measures [ 26 ]. When both government trust and professional trust are strong, the pandemic can be better controlled [ 26 ].
Professional trust has no significant impact on protective compliance
However, this study found that the public’s trust in professional healthcare institutions and medical staff tends to lean towards compliance with restrictive measures rather than protective measures. The results of the structural equation model also demonstrate that professional trust, as an intermediary for government trust, only affects compliance with restrictive measures and does not impact the effect of protective compliance. One possible explanation is that professional healthcare institutions and medical staff play a critical role in implementing restrictive measures, such as vaccine administration, providing nucleic acid test certificates, displaying health codes and travel card, and adhering to home quarantine during lockdown periods. In contrast, protective measures rely more on the voluntary compliance of the public, as these measures require spontaneous actions from the public, with relatively less involvement from professional healthcare institutions and medical staff. In China, the public’s vaccine administration and nucleic acid testing are primarily managed by professional healthcare institutions and medical staff, while the management of health codes and travel cards, as well as home quarantine during lockdowns, is a joint responsibility of the government and professional healthcare institutions [ 54 , 55 , 56 , 57 ]. Therefore, the public’s trust in professional healthcare institutions and medical staff tends to be more aligned with compliance with restrictive measures.
Analysis of compliance behavior differences among different demographic groups
We also analyzed the behavioural differences among different groups during the COVID-19 pandemic. We found that the public with rural household registration displayed a higher willingness to comply with public health policies, consistent with existing research findings [ 28 ]. This could be attributed to the relatively poor economic conditions in rural areas, leading them to rely more on the healthcare and sanitation resources provided by the government to ensure access to necessary medical services. Additionally, some rural communities may possess strong traditional cultural values that prompt the public to participate more actively in social activities and respond to government calls, such as adhering to public health policies. Finally, we observed that women exhibited a stronger inclination toward restrictive compliance, which could be due to their better understanding of COVID-19 and their relatively lower likelihood of engaging in risky behaviours [ 15 , 58 ].
The impact of research results on public health policies
To further enhance public compliance with public health policies during public health crises, it is essential to consolidate and enhance trust in the government. Firstly, there should be continued efforts to strengthen transparency and communication. Timely, transparent, and accurate dissemination of information to the public during public health crises forms the foundation of trust. Secondly, it is necessary to flexibly address the diverse needs of citizens. Different groups and regions may have varying needs and challenges during public health crises. By considering the diversity of public needs and tailoring policies accordingly, the government can better gain public understanding and support, thus enhancing trust. Additionally, to further improve public compliance with public health policies during public health crises, it is crucial to consolidate and enhance trust in medical professionalism. Healthcare institutions and the government should actively communicate authentic information about the pandemic, explain the scientific basis behind health policies, and share opinions and advice from medical professionals. Clear communication enables the public to better understand the urgency and necessity of healthcare decisions, thereby increasing trust in the healthcare system. Finally, ensuring that public health policies and practices adhere to international standards and professional guidelines can enhance public trust in professionalism. This includes providing scientific explanations about vaccination, treatment methods, preventive measures, and timely updates on medical information to adapt to the evolving pandemic situation.
Limitations and future directions of the study
Nevertheless, it is important to acknowledge some limitations of this study. Firstly, the study employed a convenience sampling method, targeting university students. Therefore, the representativeness of the sample might be somewhat limited, making it difficult to generalize to the entire Chinese population. Secondly, the study relied on self-reported data from the respondents, which could lead to memory biases and social desirability biases. Participants might exaggerate or underestimate their compliance with public health policies or be influenced by social expectations, leading to inaccuracies in the data. In conclusion, although this study provides useful information about the compliance behaviour and trust levels of the Chinese public during the COVID-19 pandemic, the aforementioned limitations need to be considered when interpreting and generalizing the research findings. As of January 8, 2023, China has lifted the preventive and control measures for COVID-19, and COVID-19 is no longer classified as a class A infectious disease under quarantine management. Therefore, future research could further expand the sample size, enhance the representativeness of the sample, and consider more potential factors to study in depth the relationship between public compliance behaviour and trust during health crises.
This study delved into the influence of government trust and professional trust on public compliance with public health policies under normative motivations, and categorized public compliance behaviour into protective compliance and restrictive compliance, making the research conclusions more specific. The study found that during the COVID-19 pandemic, both government trust and professional trust significantly impacted the public’s adherence to public health measures. To enhance public compliance with COVID-19 preventive measures, it is important to reinforce the public’s sense of moral obligation and establish trust in government authorities to encourage active participation [ 59 ]. Governments can reduce the negative impact of information conflicts on government trust by providing fair, transparent, authentic, and two-way communication, as well as by building and popularizing e-governance [ 60 , 61 , 62 , 63 ]. During crises, it is also essential to emphasize the role of crisis interventions in restoring government trust [ 32 ], thereby maintaining the credibility of professional medical institutions and healthcare personnel to better understand and address public health challenges. These findings are not only significant for the current health crisis but also provide valuable insights for future health crises and government policy-making.
Data availability
If you need us to provide data, please contact the correspondence author.
Abbreviations
China Communist Party
Pak A, et al. Does High Public Trust Amplify Compliance with stringent COVID-19 Government Health guidelines? A multi-country analysis using data from 102,627 individuals. Risk Manage Healthc Policy. 2021;14:293–302.
Article Google Scholar
Spahl W, et al. Understanding compliance as multi-faceted: values and practices during the COVID-19 pandemic in Austria. Crit Public Health. 2022;32:665–76.
Kahneman D, Tversky A. PROSPECT THEORY: AN ANALYSIS OF DECISION UNDER RISK. Econometrica. 1979;47:263–91.
Floyd DL, et al. A meta-analysis of research on protection motivation theory. J Appl Soc Psychol. 2000;30:407–29.
de Zwart O, et al. Avian influenza risk perception, Europe and Asia. Emerg Infect Dis. 2007;13:290–3.
Article PubMed PubMed Central Google Scholar
Egüez A. Compliance with the EU Waste Hierarchy: it is a Matter of Stringency, Enforcement… and Time! Eur Economics: Agric (2020): n. pag.
Gilles I, et al. Trust in medical organizations predicts pandemic (H1N1) 2009 vaccination behavior and perceived efficacy of protection measures in the Swiss public. Eur J Epidemiol. 2011;26:203–10.
Article PubMed Google Scholar
Murphy K, et al. Why people comply with COVID-19 social distancing restrictions: self-interest or duty? Australian New Z J Criminol. 2020;53:477–96.
Chong YY et al. The Role of Illness Perceptions, Coping, and Self-Efficacy on Adherence to Precautionary Measures for COVID-19. International Journal of Environmental Research and Public Health 17 (2020): n. pag.
Rogers RW. Cognitive and physiological processes in fear appeals and attitude change: a revised theory of prote. (1983).
Amirkhanyan AA, et al. Managing in the Regulatory Thicket: Regulation Legitimacy and Expertise. Public Adm Rev. 2017;77:381–94.
Vu V, Thanh. Public Trust in Government and Compliance with Policy during COVID-19 pandemic: empirical evidence from Vietnam. Public Organ Rev. 2021;21:779–96.
Fu C et al. Behavioral Implementation and Compliance of Anti-Epidemic Policy in the COVID-19 Crisis. International Journal of Environmental Research and Public Health 18 (2021): n. pag.
van Cauteren D, et al. Burden of influenza, healthcare seeking behaviour and hygiene measures during the A(H1N1)2009 pandemic in France: a population based study. BMC Public Health. 2012;12:947–947.
Zhong B-L, et al. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci. 2020;16:1745–52.
Brouard S et al. Sociodemographic and Psychological Correlates of Compliance with the COVID-19 Public Health measures in France. Can J Political Sci Revue Canadienne De Sci Politique (2020): 1–6.
Bargain O, Aminjonov U. Trust and compliance to public health policies in times of COVID-19. J Public Econ. 2020;192:104316–104316.
Lalot F et al. Distrustful Complacency and the COVID-19 Vaccine: How Concern and Political Trust Interact to Affect Vaccine Hesitancy. Political Psychology (2021): n. pag.
Jørgensen FJ et al. Compliance Without Fear: Individual-Level Predictors of Protective Behavior During the First Wave of the COVID-19 Pandemic. (2020).
Raude J et al. Determinants of Preventive Behaviors in Response to the COVID-19 Pandemic in France: Comparing the Sociocultural, Psychosocial, and Social Cognitive Explanations. Frontiers in Psychology 11 (2020): n. pag.
Earle TC, Siegrist M. Trust, confidence and Cooperation model: a framework for understanding the relation between trust and risk perception. Int J Global Environ Issues. 2008;8:17–29.
Guglielmi S et al. Public acceptability of containment measures during the COVID-19 pandemic in Italy: how institutional confidence and specific political support matter. International Journal of Sociology and Social Policy (2020): n. pag.
Adam B et al. The Risk Society and Beyond: Critical Issues for Social Theory. (2000).
Berkowitz LJ. Social norms, feelings, and other factors affecting helping and Altruism1. Adv Exp Soc Psychol. 1972;6:63–108.
van der Weerd W, et al. Monitoring the level of government trust, risk perception and intention of the general public to adopt protective measures during the influenza A (H1N1) pandemic in the Netherlands. BMC Public Health. 2011;11:575–575.
Saechang O, et al. Public Trust and Policy Compliance during the COVID-19 pandemic: the role of Professional Trust. Healthcare. 2021;9:pag.
Zimmermann B. Motivations and limits for COVID-19 policy compliance in Germany and Switzerland. Int J Health Policy Manage. 2021;11:1342–53.
Google Scholar
Huang Y, et al. To what extent do young Chinese elites comply with COVID-19 prevention and control measures? BMC Public Health. 2023;23:pag.
Marien S, Hooghe M. Does political trust matter? An empirical investigation into the relation between political trust and support for law compliance. Eur J Polit Res. 2011;50:267–91.
Farzanegan M, Reza, Hofmann HP. A matter of trust? Political trust and the COVID-19 pandemic. Int J Sociol. 2022;52:476–99.
Goldfinch S, et al. Trust in government increased during the Covid-19 pandemic in Australia and New Zealand. Australian J Public Adm. 2021;80:3–11.
Fang M, Zhang H. How can crisis intervention repair government trust? ——the moderating effect of risk communication and community support. J Public Adm. 2021;14(06):4–23.
Brooks SK, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet (London England). 2020;395:912–20.
Article CAS PubMed Google Scholar
Zettler I et al. The role of personality in COVID-19-Related perceptions, evaluations, and Behaviors Findings across Five Samples, nine traits, and 17 criteria. Social Psychol Personality Sci (2021) 194855062110016.
Vinck P, et al. Institutional trust and misinformation in the response to the 2018-19 Ebola outbreak in North Kivu, DR Congo: a population-based survey. Lancet Infect Dis. 2019;19(5):529–36.
Larson H Jane and, Heymann DL. Public health response to influenza A(H1N1) as an opportunity to build public trust. JAMA. 2010;303(3):271–2.
Zand DE. Trust and Managerial Problem solving. Adm Sci Q. 1972;17:229.
Cohen AS, Think I, Act TI, et al. The influence of critical reasoning ability on Trust and Behavior during the COVID-19 pandemic. Risk Anal. 2021;42:1073–85.
Michelle Driedger S, et al. Damned if you do, and damned if you don’t’: communicating about uncertainty and evolving science during the H1N1 influenza pandemic. J Risk Res. 2018;24:574–92.
Clements JM. Knowledge and behaviors toward COVID-19 among U.S. residents during the early days of the pandemic. medRxiv (2020): n. pag.
Ali-Saleh O, Obeid S. Compliance with COVID-19 preventive guidelines among Minority communities: the case of Israeli arabs. J Racial Ethnic Health Disparities (2022): 1–12.
Dai B, et al. The effects of Governmental and Individual predictors on COVID-19 protective behaviors in China: a path analysis Model. Public Adm Rev. 2020;80:797–804.
Almutairi AF, et al. Public Trust and Compliance with the precautionary measures against COVID-19 employed by authorities in Saudi Arabia. Risk Manage Healthc Policy. 2020;13:753–60.
Lendacki FR et al. COVID-19 vaccination requirements, encouragement and hesitancy among non-health care, non-congregate workers in Chicago: results from the WEVax survey. BMC Public Health 23 (2023): n. pag.
Wang Y-C, Chen T-CT. Analyzing the impact of COVID-19 vaccination requirements on travelers’ selection of hotels using a fuzzy multi-criteria decision-making approach. Volume 2. New York, N.y.: Healthcare Analytics; 2022. pp. 100064–100064.
Wang J, et al. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines. 2020;8:pag.
Chen W, Zhigang G, Yongcheng L, et al. Investigation on the influence of Shandong’s 2016 illegal vaccine sales case on the attitudes and behaviors of Tianjin’s children’s parents towards preventive vaccination. Chin J Public Health. 2016;32(07):881–4.
Zhou Qian L, Weimin C, Linxiang, et al. Influence of Shandong’s series of illegal vaccine sales cases on the attitudes and behaviors of Children’s parents in Shenzhen towards Preventive Vaccination. Chin J Vaccines Immun. 2018;24(02):230–6. https://doi.org/10.19914/j.cjvi.2018.02.022 .
Dror AA, et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35:775–9.
Article CAS PubMed PubMed Central Google Scholar
Troiano G, Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health. 2021;194:245–51.
Goren T, et al. Count on trust: the indirect effect of trust in government on policy compliance with health behavior instructions. Policy Sci. 2022;55:593–630.
Teng L. Hu Xiangming. Government Trust in Public Health Risks: challenges and Constructions. Journal of Northwest Minzu University (Philosophy and Social Sciences Edition) (2021) 04: 149–56. https://doi.org/10.14084/j.cnki.cn62-1185/c.20210702.001 .
Dincer O. Trust in Government and Compliance with Stay at Home orders in American States. Public Economics: Miscellaneous Issues eJournal (2021): n. pag.
Jiang Changyun J. Review of the impact of COVID-19 Epidemic Prevention and Control on National Emergency Management System and Capacity. Manage World. 2020;36:8–18. https://doi.org/10.19744/j.cnki.11-1235/f.2020.0115 .
Zhao H. Restriction and Boundaries of Individual Rights under Epidemic Prevention and Control. Comp Law Res. 2020;02:11–24.
Zha Yunfei. Health Code: automated evaluation and utilization of individual epidemic risk. Zhejiang Acad J. 2020;03:28–35. https://doi.org/10.16235/j.cnki.33-1005/c.2020.03.005 .
Zhang X. Improvement of the Epidemic Prevention administrative isolation system from the perspective of the rule of Law: a study on the Administrative Isolation of Individuals for Epidemic Prevention. Administrative management reform (2020) 08: 27–33. https://doi.org/10.14150/j.cnki.1674-7453.2020.08.004 .
Ward DJ. Gender differences in compliance with infection control precautions. Br J Infect Control. 2004;5:17–9.
Nivette AE et al. Non-compliance with COVID-19-related public health measures among young adults in Switzerland: Insights from a longitudinal cohort study. Social Science & Medicine (1982) 268 (2020): 113370–113370.
Liu J et al. Government Response Measures and Public Trust during the COVID-19 Pandemic: Evidence from Around the World. British Journal of Management (2021): n. pag.
Guan B, et al. Two-way risk communication, Public Value Consensus, and citizens’ policy compliance willingness about COVID-19: Multilevel Analysis based on a Nudge View. Adm Soc. 2021;53:1106–49.
Vaughan E, Tinker TL. Effective health risk communication about pandemic influenza for vulnerable populations. Am J Public Health 99 Suppl 2 (2009): S324–32.
Im T, et al. Internet, Trust in Government, and Citizen Compliance. J Public Adm Res Theor. 2014;24:741–63.
Download references
Acknowledgements
Professional English language editing support provided by Asia Edit (asiaedit.com).
This work is supported by a research project from Guangxi Philosophy and Social Science Foundation(22FMZ029).
Author information
Authors and affiliations.
School of Political Science and Public Administration, Guangxi Minzu University, Nanning, Guangxi, China
Guobang Chen, Hua Zhang, Yue Hu & Chunyan Luo
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization, Guobang Chen, Hua Zhang and Yue Hu; methodology, Guobang Chen, Hua Zhang and Yue Hu; writing-original draft preparation, Guobang Chen; writing-review and editing, Guobang Chen, Yue Hu, Hua Zhang and Chunyan Luo. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Hua Zhang .
Ethics declarations
Ethics approval and consent to participate.
Informed consent was obtained from all the participants in the study. The study was approved by the Academic Ethics Committee of School of Politics Science and Public Administration, Guangxi Minzu University. The present study was conducted in accordance with the principles of the 2013 Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Chen, G., Zhang, H., Hu, Y. et al. Trust as a catalyst: revealing the impact of government trust and professional trust on public health policy compliance during a pandemic. BMC Public Health 24 , 957 (2024). https://doi.org/10.1186/s12889-024-18449-2
Download citation
Received : 31 October 2023
Accepted : 26 March 2024
Published : 04 April 2024
DOI : https://doi.org/10.1186/s12889-024-18449-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Such findings from personality and social psychology have clear potential relevance to patient-provider relationships, particularly the relationship between patients and psychotherapists. For example, level of patient trust in the therapist may be critical to working through ruptures in the therapeutic relationship.
Older patients tend to have higher levels of trust in their ... Most respondents (93%) had a score of 3 or higher. The mean score of 4.03 among the respondents indicates relatively high level of trust in their physician. ... which might have led to acquiescence bias. However, WF-D has been validated [46] and frequently used for trust research ...
In the United States, trust in health care institutions is considerably lower than it is for one's regular clinician. A 2018 national survey found that only 20% of adults reported strong trust in most hospitals and that only 16% reported strong trust in the health care system, while nearly two thirds of respondents who had a personal physician reported that they strongly trusted their physician.
Hence, patients' general satisfaction affects their confidence and trust in the physician for medical care and treatment. Previous studies have also found that a higher level of patient satisfaction is associated with a higher level of patient-provider trust . Thus, we hypothesize that an increase in patients' general satisfaction with ...
Introduction The aim of this scoping review is to systematically search the literature to identify the nature and or level of trust between the patient, the users of health services (eg, clients seeking health promotion and preventive healthcare services) and the individual healthcare providers (doctors, nurses and physiotherapists/ occupational therapists), across public and private ...
The current findings present a novel method that advocates for using a more holistic assessment of patients' feelings during interactions with clinicians—verbal cues of trust and distrust. Few studies have directly observed patient-clinician dyads for trust research and have thus relied merely on self-report surveys after clinician visits.
Based on an integrated model of doctor-patient psychological mechanisms, the formation mechanism of doctor--patient trust was systematically demonstrated from the healthcare professional (HCP)'s perspective integrating intergroup relations (expectations), interpersonal relations (communication), and psychosocial (stereotypes). The results of a survey of 3000 doctors and nurses from 14 ...
Our findings, which indicate higher trust levels among managers in the private health sector compared to the public setting are in line with Niv-Yagoda's work, which showed an association between low levels of trust in the public healthcare system and the public's perception regarding the importance of patient's autonomy (e.g., selecting ...
Sentiment analysis revealed that 91.5 percent (32,205) were positive, a much higher positive proportion than we find for most issues explored in this way. This high-level finding suggests that patients want to trust their caregivers and are delighted when they find evidence that their trust is well placed.
For example, previous research indicates that trust in physicians in China appears quite low, and that Chinese patients with higher education and medical insurance indicate higher trust in physicians Future research should elucidate dimensions of trust including nonverbal communication behavior indicative of trust (and mistrust).
Trust, mistrust, and distrust influence people's ability to utilize critical resources and make decisions that are best for their health and well-being. Trust is necessary for optimizing health research, eliminating healthcare disparities, and achieving health equity, but efforts to build trust to increase healthcare utilization and research participation may have little effect on attitudes or ...
Their own research found that higher levels of physician mistrust, but not medical system mistrust, were associated with longer time since the last visit to an HIV provider. Understanding how these levels are simultaneously related and distinct would help potential influences of trust target their efforts more precisely. Rate-Limiting Challenges
Our findings, which indicate higher trust levels among managers in the private health sector compared to the public setting are in line with Niv-Yagoda's work, which showed an association between low levels of trust in the public healthcare system and the public's perception regarding the importance of patient's autonomy (e.g., selecting ...
A higher value indicates patients' preference for less control over their medical decisions. The score for patient preference in decision-making is moderate (M = 2.96, SD = 1.19). ... Low levels of patient trust have become a serious problem in the Chinese healthcare system. In efforts to resolve the problem, communication during medical ...
Trustful relationships play a vital role in successful organisations and well-functioning hospitals. While the trust relationship between patients and providers has been widely studied, trust relations between healthcare professionals and their supervisors have not been emphasised. A systematic literature review was conducted to map and provide an overview of the characteristics of trustworthy ...
Main Outcomes. Trust in the healthcare team was part of the patient questionnaire and adapted from the 10-item Wake Forest University Trust scale measuring the level of interpersonal trust, i.e., fidelity (caring and advocating for the patient's welfare), competence, honesty, confidentiality, and global trust in the healthcare team [].The three negatively worded items were recoded and an ...
1. Introduction. Trust, which requires an individual to rely on another person or entity, is increasingly recognized as a key element of quality health care [1], [2].Patient trust in one's regular doctor, or one's regular clinician if not a doctor (together referred to as "clinician" in this paper), [3] is related to a wide range of positive health behaviors, including better ...
Our findings indicate that knowledge about treatment was a significant predictor of trust, and that the lowest levels of knowledge were associated with lower levels of trust.
Findings indicate that the extent of literature is limited in specific examples of nurse interventions that facilitate interpersonal patient-nurse trust. Future research should include more detailed nurse actions and attributes that build patient-nurse trust to fully understand the benefits of trust in oncology patients.
AAMC FL 1 P/S #50. I had A as my initial answer, but then saw that the passage mentioned "The amount of social distance between patients and physicians impacts healthcare quality and treatment adherence in important ways. The social distance hypothesis suggests that patients who have more in common with their physicians in terms of class ...
The Trust in Physician Form is an 11-question instrument that assesses patient trust in their physician with a higher score indicating higher trust. 16 The questions were expressed on a 5-point Likert scale, where a value of 1 was designated for "strongly disagree" and 5 for "strongly agree.".
For these reasons, in our discussion, the opposite of trust is mistrust, rather than distrust or lack of trust. Clinical research trust is defined in this study as the belief by the study participant that his/her interests (e.g. full disclosure, balance of risk/benefit, prudent data usage) are considered before the interests of the study or the ...
A higher level of professional trust among the public corresponds to a greater willingness to seek healthcare assistance and a stronger inclination to adhere to disease prevention measures . ... The research findings indicate that, following factor analysis, vaccination was classified as a form of restrictive compliance behaviour.