

‘You have to suffer for your PhD’: poor mental health among doctoral researchers – new research
Lecturer in Social Sciences, University of Westminster
Disclosure statement
Cassie Hazell has received funding from the Office for Students.
University of Westminster provides funding as a member of The Conversation UK.
View all partners
PhD students are the future of research, innovation and teaching at universities and beyond – but this future is at risk. There are already indications from previous research that there is a mental health crisis brewing among PhD researchers.
My colleagues and I studied the mental health of PhD researchers in the UK and discovered that, compared with working professionals, PhD students were more likely to meet the criteria for clinical levels of depression and anxiety. They were also more likely to have significantly more severe symptoms than the working-professional control group.
We surveyed 3,352 PhD students, as well as 1,256 working professionals who served as a matched comparison group . We used the questionnaires used by NHS mental health services to assess several mental health symptoms.
More than 40% of PhD students met the criteria for moderate to severe depression or anxiety. In contrast, 32% of working professionals met these criteria for depression, and 26% for anxiety.
The groups reported an equally high risk of suicide. Between 33% and 35% of both PhD students and working professionals met the criteria for “suicide risk”. The figures for suicide risk might be so high because of the high rates of depression found in our sample.
We also asked PhD students what they thought about their own and their peers’ mental health. More than 40% of PhD students believed that experiencing a mental health problem during your PhD is the norm. A similar number (41%) told us that most of their PhD colleagues had mental health problems.
Just over a third of PhD students had considered ending their studies altogether for mental health reasons.
There is clearly a high prevalence of mental health problems among PhD students, beyond those rates seen in the general public. Our results indicate a problem with the current system of PhD study – or perhaps with academic more widely. Academia notoriously encourages a culture of overwork and under-appreciation.
This mindset is present among PhD students. In our focus groups and surveys for other research , PhD students reported wearing their suffering as a badge of honour and a marker that they are working hard enough rather than too much. One student told us :
“There is a common belief … you have to suffer for the sake of your PhD, if you aren’t anxious or suffering from impostor syndrome, then you aren’t doing it "properly”.
We explored the potential risk factors that could lead to poor mental health among PhD students and the things that could protect their mental health.
Financial insecurity was one risk factor. Not all researchers receive funding to cover their course and personal expenses, and once their PhD is complete, there is no guarantee of a job. The number of people studying for a PhD is increasing without an equivalent increase in postdoctoral positions .
Another risk factor was conflict in their relationship with their academic supervisor . An analogy offered by one of our PhD student collaborators likened the academic supervisor to a “sword” that you can use to defeat the “PhD monster”. If your weapon is ineffective, then it makes tackling the monster a difficult – if not impossible – task. Supervisor difficulties can take many forms. These can include a supervisor being inaccessible, overly critical or lacking expertise.
A lack of interests or relationships outside PhD study, or the presence of stressors in students’ personal lives were also risk factors.
We have also found an association between poor mental health and high levels of perfectionism, impostor syndrome (feeling like you don’t belong or deserve to be studying for your PhD) and the sense of being isolated .
Better conversations
Doctoral research is not all doom and gloom. There are many students who find studying for a PhD to be both enjoyable and fulfilling , and there are many examples of cooperative and nurturing research environments across academia.
Studying for a PhD is an opportunity for researchers to spend several years learning and exploring a topic they are passionate about. It is a training programme intended to equip students with the skills and expertise to further the world’s knowledge. These examples of good practice provide opportunities for us to learn about what works well and disseminate them more widely.
The wellbeing and mental health of PhD students is a subject that we must continue to talk about and reflect on. However, these conversations need to happen in a way that considers the evidence, offers balance, and avoids perpetuating unhelpful myths.
Indeed, in our own study, we found that the percentage of PhD students who believed their peers had mental health problems and that poor mental health was the norm, exceeded the rates of students who actually met diagnostic criteria for a common mental health problem . That is, PhD students may be overestimating the already high number of their peers who experienced mental health problems.
We therefore need to be careful about the messages we put out on this topic, as we may inadvertently make the situation worse. If messages are too negative, we may add to the myth that all PhD students experience mental health problems and help maintain the toxicity of academic culture.
- Mental health
- Academic life
- PhD research

Senior Research Development Coordinator

Audience Development Coordinator (fixed-term maternity cover)

Lecturer (Hindi-Urdu)

Director, Defence and Security

Opportunities with the new CIEHF
- Open access
- Published: 26 August 2020
Understanding the mental health of doctoral researchers: a mixed methods systematic review with meta-analysis and meta-synthesis
- Cassie M. Hazell ORCID: orcid.org/0000-0001-5868-9902 1 ,
- Laura Chapman 2 ,
- Sophie F. Valeix 3 ,
- Paul Roberts 4 ,
- Jeremy E. Niven 5 &
- Clio Berry 6
Systematic Reviews volume 9 , Article number: 197 ( 2020 ) Cite this article
13k Accesses
58 Citations
81 Altmetric
Metrics details
Data from studies with undergraduate and postgraduate taught students suggest that they are at an increased risk of having mental health problems, compared to the general population. By contrast, the literature on doctoral researchers (DRs) is far more disparate and unclear. There is a need to bring together current findings and identify what questions still need to be answered.
We conducted a mixed methods systematic review to summarise the research on doctoral researchers’ (DRs) mental health. Our search revealed 52 articles that were included in this review.
The results of our meta-analysis found that DRs reported significantly higher stress levels compared with population norm data. Using meta-analyses and meta-synthesis techniques, we found the risk factors with the strongest evidence base were isolation and identifying as female. Social support, viewing the PhD as a process, a positive student-supervisor relationship and engaging in self-care were the most well-established protective factors.
Conclusions
We have identified a critical need for researchers to better coordinate data collection to aid future reviews and allow for clinically meaningful conclusions to be drawn.
Systematic review registration
PROSPERO registration CRD42018092867
Peer Review reports
Student mental health has become a regular feature across media outlets in the United Kingdom (UK), with frequent warnings in the media that the sector is facing a ‘mental health crisis’ [ 1 ]. These claims are largely based on the work of regulatory authorities and ‘grey’ literature. Such sources corroborate an increase in the prevalence of mental health difficulties amongst students. In 2013, 1 in 5 students reported having a mental health problem [ 2 ]. Only 3 years later, however, this figure increased to 1 in 4 [ 3 ]. In real terms, this equates to 21,435 students disclosing mental health problems in 2013 rising to 49,265 in 2017 [ 4 ]. Data from the Higher Education Statistics Agency (HESA) demonstrates a 210% increase in the number of students terminating their studies reportedly due to poor mental health [ 5 ], while the number of students dying by suicide has consistently increased in the past decade [ 6 ].
This issue is not isolated to the UK. In the United States (US), the prevalence of student mental health problems and use of counselling services has steadily risen over the past 6 years [ 7 ]. A large international survey of more than 14,000 students across 8 countries (Australia, Belgium, Germany, Mexico, Northern Ireland, South Africa, Spain and the United States) found that 35% of students met the diagnostic criteria for at least one common mental health condition, with highest rates found in Australia and Germany [ 8 ].
The above figures all pertain to undergraduate students. Finding equivalent information for postgraduate students is more difficult, and where available tends to combine data for postgraduate taught students and doctoral researchers (DRs; also known as PhD students or postgraduate researchers) (e.g. [ 4 ]). The latest trend analysis based on data from 36 countries suggests that approximately 2.3% of people will enrol in a PhD programme during their lifetime [ 9 ]. The countries with the highest number of DRs are the US, Germany and the UK [ 10 ]. At present, there are more than 281,360 DRs currently registered across these three countries alone [ 11 , 12 ], making them a significant part of the university population. The aim of this systematic review is to bring attention specifically to the mental health of DRs by summarising the available evidence on this issue.
Using a mixed methods approach, including meta-analysis and meta-synthesis, this review seeks to answer three research questions: (1) What is the prevalence of mental health difficulties amongst DRs? (2) What are the risk factors associated with poor mental health in DRs? And (3) what are the protective factors associated with good mental health in DRs?
Literature search
We conducted a search of the titles and abstracts of all article types within the following databases: AMED, BNI, CINAHL, Embase, HBE, HMIC, Medline, PsycInfo, PubMed, Scopus and Web of Science. The same search terms were used within all of the databases, and the search was completed on the 13th April 2018. Our search terms were selected to capture the variable terms used to describe DRs, as well as the terms used to describe mental health, mental health problems and related constructs. We also reviewed the reference lists of all the papers included in this review. Full details of the search strategy are provided in the supplementary material .
Inclusion criteria
Articles meeting the following criteria were considered eligible for inclusion: (1) the full text was available in English; (2) the article presented empirical data; (3) all study participants, or a clearly delineated sub-set, were studying at the doctoral level for a research degree (DRs or equivalent); and (4) the data collected related to mental health constructs. The last of these criteria was operationalised (a) for quantitative studies as having at least one mental health-related outcome measure, and (b) for qualitative studies as having a discussion guide that included questions related to mental health. We included university-published theses and dissertations as these are subjected to a minimum level of peer-review by examiners.
Exclusion criteria
In order to reduce heterogeneity and focus the review on doctoral research as opposed to practice-based training, we excluded articles where participants were studying at the doctoral level, but their training did not focus on research (e.g. PsyD doctorate in Clinical Psychology).
Screening articles
Papers were screened by one of the present authors at the level of title, then abstract, and finally at full text (Fig. 1 ). Duplicates were removed after screening at abstract. At each level of screening, a random 20% sub-set of articles were double screened by another author, and levels of agreement were calculated (Cohen’s kappa [ 13 ]). Where disagreements occurred between authors, a third author was consulted to decide whether the paper should or should not be included. All kappa values evidence at least moderate agreement between authors [ 14 ]—see Fig. 1 for exact kappa values.
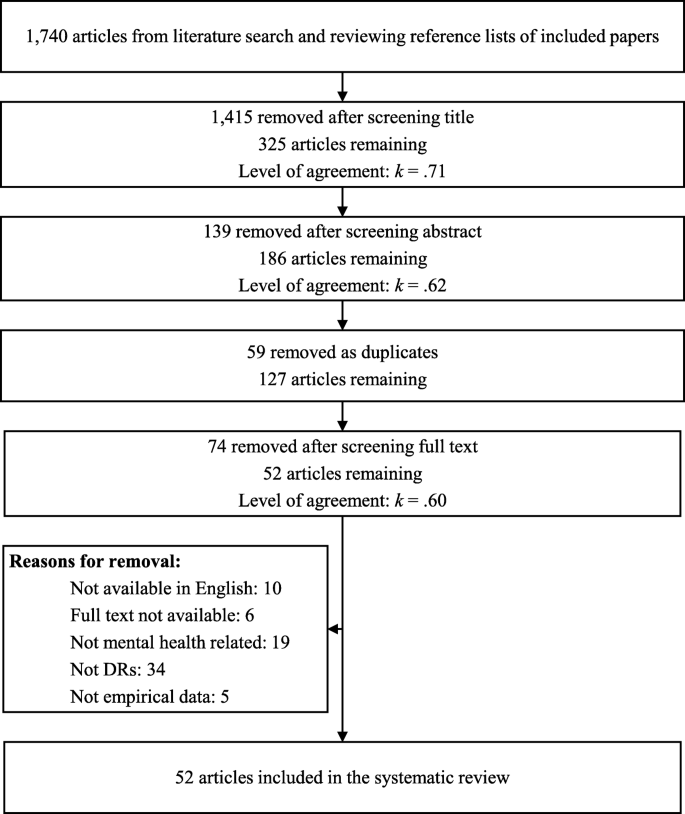
PRISMA diagram of literature review process
Data extraction
This review reports on both quantitative and qualitative findings, and separate extraction methods were used for each. Data extraction was performed by authors CH, CB, SV and LC.
Quantitative data extraction
The articles in this review used varying methods and measures. To accommodate this heterogeneity, multiple approaches were used to extract quantitative data. Where available, we extracted (a) descriptive statistics, (b) correlations and (c) a list of key findings. For all mental health outcome measures, we extracted the means and standard deviations for the DR participants, and where available for the control group (descriptive statistics). For studies utilising a within-subjects study design, we extracted data where a mental health outcome measure was correlated with another construct (correlations). Finally, to ensure that we did not lose important findings that did not use descriptive statistics or correlations, we extracted the key findings from the results sections of each paper (list of key findings). Key findings were identified as any type of statistical analysis that included at least one mental health outcome.
Qualitative data extraction
In line with the meta-ethnographic method [ 15 ] and our interest in the empirical data as well as the authors’ interpretations thereof, i.e. the findings of each article [ 16 ], the data extracted from the articles comprised both results/findings and discussion/conclusion sections. For articles reporting qualitative findings, we extracted the results and discussion sections from articles verbatim. Where articles used mixed methods, only the qualitative section of the results was extracted. Methodological and setting details from each article were also extracted and provided (see Appendix A) in order to contextualise the studies.
Data analysis
Quantitative data analysis, descriptive statistics.
We present frequencies and percentages of the constructs measured, the tools used and whether basic descriptive statistics ( M and SD ) were reported. The full data file is available from the first author upon request.
Effect sizes
Where studies had a control group, we calculated a between-group effect size (Cohen’s d ) using the formula reported by Wilson [ 17 ], and interpreted using the standard criteria [ 13 ]. For all other studies, we sought to compare results with normative data where the following criteria were satisfied: (a) at least three studies reported data using the same mental health assessment tool; (b) empirical normative data were available; and (c) the scale mean/total had been calculated following original authors’ instructions. Only the Perceived Stress Scale (PSS) 10- [ 18 ] and 14-item versions [ 19 ] met these criteria. Normative data were available from a sample of adults living in the United States: collected in 2009 for the 10-item version ( n = 2000; M = 15.21; SD = 7.28) [ 20 ] and in 1983 for the 14-item version ( n = 2355; M = 19.62; SD = 7.49) [ 18 ].
The meta-analysis of PSS data was conducted using MedCalc [ 21 ], and based on a random effects model, as recommended by [ 22 ]. The between-group effect sizes (DRs versus US norms) were calculated comparing PSS means and standard deviations in the respective groups. The effect sizes were weighted using the variable variances [ 23 ].
Correlations
Where at least three studies reported data reflecting a bivariate association between a mental health and another variable, we summarised this data into a meta-analysis using the reported r coefficients and sample sizes. Again, we used MedCalc [ 21 ] to conduct the analysis using a random effects model, based on the procedure outlined by Borenstein, Hedges, Higgins and Rothstein [ 24 ]. This analysis approach involves converting correlation coefficients into Fisher’s z values [ 25 ], calculating the summary of Fisher’s z , and then converting this to a summary correlation coefficient ( r ). The effect sizes were weighted in line with the Hedges and Ollkin [ 23 ] method. Heterogeneity was assessed using the Q statistic, and I 2 value—both were interpreted according to the GRADE criteria [ 26 ]. Where correlations could not be summarised within a meta-analysis, we have reported these descriptively.
Due to the heterogenous nature of the studies, the above methods could not capture all of the quantitative data. Therefore, additional data (e.g. frequencies, statistical tests) reported in the identified articles was collated into a single document, coded as relating to prevalence, risk or protective factors and reported as a narrative review.
Qualitative data analysis
We used thematic analytic methods to analyse the qualitative data. We followed the thematic synthesis method [ 16 , 27 ] and were informed by a thematic analysis approach [ 28 , 29 ]. We took a critical realist epistemological stance [ 30 , 31 ] and aimed to bring together an analysis reflecting meaningful patterns amongst the data [ 29 ] or demi-regularities, and identifying potential social mechanisms that might influence the experience of such phenomena [ 31 ]. The focus of the meta-synthesis is interpretative rather than aggregative [ 32 ].
Coding was line by line, open and complete. Following line-by-line coding of all articles, a thematic map was created. Codes were entered on an article-by-article basis and then grouped and re-grouped into meaningful patterns. Comparisons were made across studies to attempt to identify demi-regularities or patterns and contradictions or points of departure. The thematic map was reviewed in consultation with other authors to inductively create and refine themes. Thematic summaries were created and brought together into a first draft of the thematic structure. At this point, each theme was compared against the line-by-line codes and the original articles in order to check its fit and to populate the written account with illustrative quotations.
Research rigour
The qualitative analysis was informed by independent coding by authors CB and SV, and analytic discussions with CH, SV and LC. Our objective was not to capture or achieve inter-rater reliability, rather the analysis was strengthened through involvement of authors from diverse backgrounds including past and recent PhD completion, experiences of mental health problems during PhD completion, PhD supervision experience, experience as employees in a UK university doctoral school and different nationalities. In order to enhance reflexivity, CB used a journal throughout the analytic process to help notice and bracket personal reflections on the data and the ways in which these personal reflections might impact on the interpretation [ 29 , 33 ]. The ENTREQ checklist [ 34 ] was consulted in the preparation of this report to improve the quality of reporting.
Quality assessment
Quantitative data.
The quality of the quantitative papers was assessed using the STROBE combined checklist [ 35 ]. A random 20% sub-sample of these studies were double-coded and inter-rater agreement was 0.70, indicating ‘substantial’ agreement [ 14 ]. The maximum possible quality score was 23, with a higher score indicating greater quality, with the mean average of 15.97, and a range from 0 to 22. The most frequently low-scoring criteria were incomplete reporting regarding the management of missing data, and lack of reported efforts to address potential causes of bias.
Qualitative data
There appeared to be no discernible pattern in the perceived quality of studies; the highest [ 36 , 37 , 38 , 39 , 40 ] and lowest scoring [ 41 , 42 , 43 , 44 , 45 , 46 ] studies reflected both theses and journal publications, a variety of locations and settings and different methodologies. The most frequent low-scoring criteria were relating to the authors’ positions and reflections thereof (i.e. ‘Qualitative approach and research paradigm’, ‘Researcher characteristics and reflexivity’, ‘Techniques to enhance trustworthiness’, ‘Limitations’, ‘Conflict of interest and Funding’). Discussions of ethical issues and approval processes was also frequently absent. We identified that we foregrounded higher quality studies in our synthesis in that these studies appeared to have greater contributions reflected in the shape and content of the themes developed and were more likely to be the sources of the selected illustrative quotes.
Mixed methods approach
The goal of this review is to answer the review questions by synthesising the findings from both quantitative and/or qualitative studies. To achieve our goal, we adopted an integrated approach [ 47 ], whereby we used both quantitative and qualitative methods to answer the same review question, and draw a synthesised conclusion. Different analysis approaches were used for the quantitative and qualitative data and are therefore initially reported separately within the methods. A separate synthesised summary of the findings is then provided.
Overview of literature
Of the 52 papers included in this review (Table 1 ), 7 were qualitative, 29 were quantitative and 16 mixed methods. Most articles (35) were peer-reviewed papers, and the minority were theses (17). Only four of the articles included a control group; in three instances comprising students (but not DRs) and in the other drawn from the general population.
Quantitative results
Thirty-five papers reported quantitative data, providing 52 reported sets of mental health related data (an average of 1.49 measures per study): 24 (68.57%) measured stress, 10 (28.57%) anxiety, 9 (25.71%) general wellbeing, 5 (14.29%) social support, 3 (8.57%) depression and 1 (2.86%) self-esteem. Five studies (9.62%) used an unvalidated scale created for the purposes of the study. Fifteen studies (28.85%) did not report descriptive statistics.
Of the four studies that included a control group, only two of these reported descriptive statistics for both groups on a mental health outcome [ 66 , 69 ]. There is a small (Cohen’s d = 0.27) and large between-group effect (Cohen’s d = 1.15) when DRs were compared to undergraduate and postgraduate clinical psychology students respectively in terms of self-reported stress.
The meta-analysis of DR scores on the PSS (both 10- and 14-item versions) compared to population normative data produced a large and significant between-group effect size ( d = 1.12, 95% CI [0.52, 1.73]) in favour of DRs scoring higher on the PSS than the general population (Fig. 2 ), suggesting DRs experience significantly elevated stress. However, these findings should be interpreted in light of the significant between-study heterogeneity that can be classified as ‘considerable’ [ 26 ].
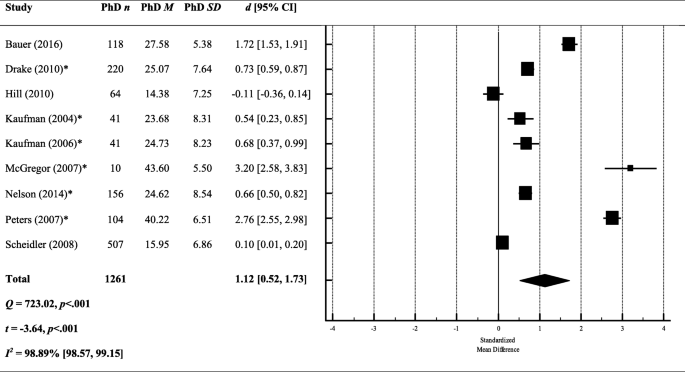
A meta-analysis of between-group effect sizes (Cohen’s d ) comparing PSS scores (both 10- and 14-item versions) from DRs and normative population data. *Studies using the 14 item version of the PSS; a positive effect size indicates DRs had a higher score on the PSS; a negative effect size indicates that the normative data produced a higher score on the PSS; black diamond = total effect size (based on random effects model); d = Cohen’s d ; Q = heterogeneity; Z = z score; I 2 = proportion of variance due to between-study heterogeneity; p = exact p value
To explore this heterogeneity, we re-ran the meta-analysis separately for the 10- and 14-item versions. The effect size remained large and significant when looking only at the studies using the 14-item version ( k = 6; d = 1.41, 95% CI [0.63, 2.19]), but was reduced and no longer significant when looking at the 10-item version only ( k = 3; d = 0.57, 95% CI [− 0.51, 1.64]). However, both effect sizes were still marred by significant heterogeneity between studies (10-item: Q = 232.02, p < .001; 14-item: Q = 356.76, p < .001).
Studies reported sufficient correlations for two separate meta-analyses; the first assessing the relationship between stress (PSS [ 18 , 19 ]) and perceived support, and the second between stress (PSS) and academic performance.
Stress x support
We included all measures related to support irrespective of whom that support came from (e.g. partner support, peer support, mentor support). The overall effect size suggests a small and significant negative correlation between stress and support ( r = − .24, 95% CI [− 0.34, − 0.13]) (see Fig. 3 ), meaning that low support is associated with greater perceived stress. However, the results should be interpreted in light of the significant heterogeneity between studies. The I 2 value quantifies this heterogeneity as almost 90% of the variance being explained by between-study heterogeneity, which is classified as ‘substantial’ (26).
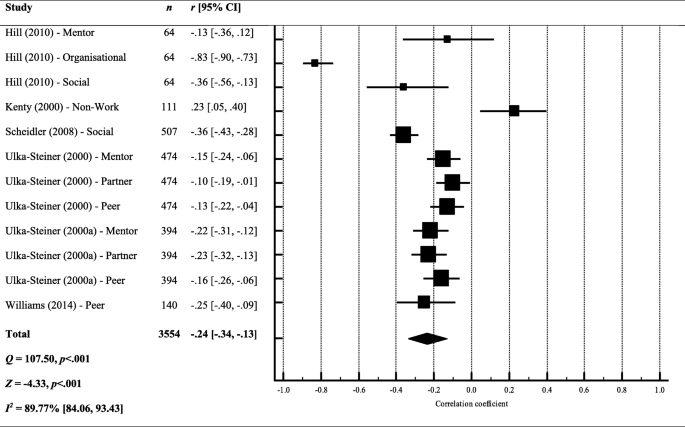
Forest plot and meta-analysis of correlation coefficients testing the relationship between stress and perceived support. Black diamond = total effect size (based on random effects model); r = Pearson’s r ; Q = heterogeneity; Z = z score; I 2 = proportion of variance due to between-study heterogeneity; p = exact p value
Stress x performance
The overall effect size suggests that there is no relationship between stress and performance in their studies ( r = − .07, 95% CI [− 0.19, 0.05]) (see Fig. 4 ), meaning that DRs perception of their progress was not associated with their perceived stress This finding suggests that the amount of progress that DRs were making during their studies was not associated with stress levels.
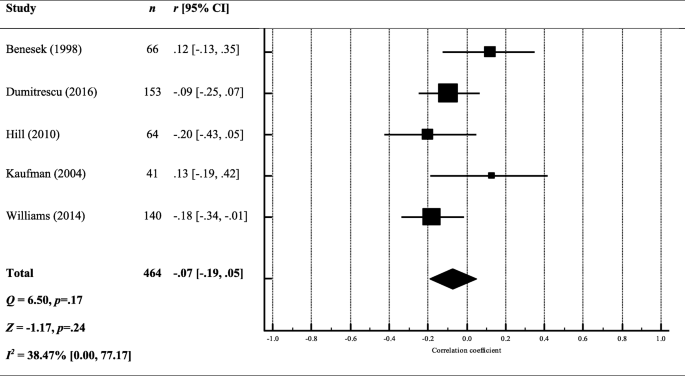
Forest plot and meta-analysis of correlation coefficients testing the relationship between stress and performance. Black diamond = total effect size (based on random effects model); r = Pearson’s r ; Q = heterogeneity; Z = z score; I 2 = proportion of variance due to between-study heterogeneity; p = exact p value
Other correlations
Correlations reported in less than three studies are summarised in Fig. 5 . Again, stress was the most commonly tested mental health variable. Self-care and positive feelings towards the thesis were consistently found to negatively correlate with mental health constructs. Negative writing habits (e.g. perfectionism, blocks and procrastination) were consistently found to positively correlate with mental health constructs. The strongest correlations were found between stress, and health related quality of life ( r = − .62) or neuroticism ( r = .59), meaning that lower stress was associated with greater quality of life and reduced neuroticism. The weakest relationships ( r < .10) were found between mental health outcomes and: faculty concern, writing as knowledge transformation, innate writing ability (stress and anxiety), years married, locus of control, number of children and openness (stress only).
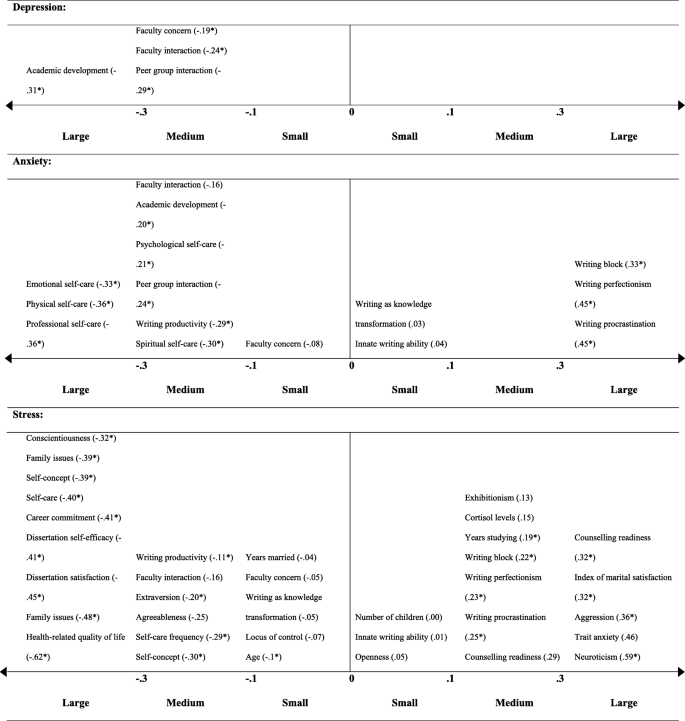
Correlation coefficients testing the relationship between a mental health outcome and other construct. Correlation coefficients are given in brackets ( r ); * p < .05; each correlation coefficient reflects the results from a single study
Several studies reported DR mental health problem prevalence and this ranged from 36.30% [ 54 ] to 55.9% [ 67 ]. Using clinical cut-offs, 32% were experiencing a common psychiatric disorder [ 64 ]; with another study finding that 53.7% met the questionnaire cut-off criteria for depression, and 41.9% for anxiety [ 67 ]. One study compared prevalence amongst DRs and the general population, employees and other higher education students; in all instances, DRs had higher levels of psychological distress (non-clinical), and met criteria for a clinical psychiatric disorder more frequently [ 64 ].
Risk factors
Demographics Two studies reported no significant difference between males and females in terms of reported stress [ 57 , 73 ], but the majority suggested female DRs report greater clinical [ 80 ], and non-clinical problems with their mental health [ 37 , 64 , 79 , 83 , 89 ].
Several studies explored how mental health difficulties differed in relation to demographic variables other than gender, suggesting that being single or not having children was associated with poorer mental health [ 64 ] as was a lower socioeconomic status [ 71 ]. One study found that mental health difficulties did not differ depending on DRs’ ethnicity [ 51 ], but another found that Black students attending ‘historically Black universities’ were significantly more anxious [ 87 ]. The majority of the studies were conducted in the US, but only one study tested for cross-cultural differences: reporting that DRs in France were more psychologically distressed than those studying in the UK [ 67 ].
Work-life balance Year of study did not appear to be associated with greater subjective stress in a study involving clinical psychology DRs (Platt and Schaefer [ 75 ]), although other studies suggested greater stress reported by those in the latter part of their studies [ 89 ], who viewed their studies as a burden [ 81 ], or had external contracts, i.e. not employed by their university [ 85 ]. Regression analyses revealed that a common predictor of poor mental health was uncertainty in DR studies; whether in relation to uncertain funding [ 64 ] or uncertain progress [ 80 ]. More than two-thirds of DRs reported general academic pressure as a cause of stress, and a lack of time as preventing them from looking after themselves [ 58 ]. Being isolated was also a strong predictor of stress [ 84 ].
Protective factors
DRs who more strongly endorsed all of the five-factor personality traits (openness, conscientiousness, extraversion, agreeableness and neuroticism) [ 66 ], self-reported higher academic achievement [ 40 ] and viewed their studies as a learning process (rather than a means to an end) [ 82 ] reported fewer mental health problems. DRs were able to mitigate poor mental health by engaging in self-care [ 72 ], having a supervisor with an inspirational leadership style [ 64 ] and building coping strategies [ 56 ]. The most frequently reported coping strategy was seeking support from other people [ 37 , 58 ].
Qualitative results
Meta-synthesis.
Four higher-order themes were identified: (1) Always alone in the struggle, (2) Death of personhood, (3) The system is sick and (4) Seeing, being and becoming. The first two themes reflect individual risk/vulnerability factors and the processes implicated in the experience of mental distress, the third represents systemic risk and vulnerability factors and the final theme reflects individual and systemic protective mechanisms and transformative influences. See Table 2 for details of the full thematic structure with illustrative quotes.
Always alone in the struggle
‘Always alone in the struggle’ reflects the isolated nature of the PhD experience. Two subthemes reflect different aspects of being alone; ‘Invisible, isolated and abandoned’ represents DRs’ sense of physical and psychological separation from others and ‘It’s not you, it’s me’ represents DRs’ sense of being solely responsible for their PhD process and experience.
Invisible, isolated and abandoned
Feeling invisible and isolated both within and outside of the academic environment appears a core DR experience [ 39 , 43 , 81 ]. Isolation from academic peers seemed especially salient for DRs with less of a physical presence on campus, e.g. part-time and distance students, those engaging in extensive fieldwork, outside employment and those with no peer research or lab group [ 36 , 52 , 68 ]. Where DRs reported relationships with DR peers, these were characterised as low quality or ‘not proper friendships’ and this appeared linked to a sense of essential and obvious competition amongst DRs with respect to current and future resources, support and opportunities [ 39 ], in which a minority of individuals were seen to receive the majority share [ 36 , 74 ]. Intimate sharing with peers thus appeared to feel unsafe. This reflected the competitive environment but also a sense of peer relationships being predicated on too shared an experience [ 39 ].
In addition to poor peer relations, a mismatch between the expected and observed depth of supervisor interest, engagement and was evident [ 40 , 81 ]. This mismatch was clearly associated with disappointment and anger, and a sense of abandonment, which appeared to impact negatively on DR mental health and wellbeing [ 42 ] (p. 182). Moreover, DRs perceived academic departments as complicit in their isolation; failing to offer adequate opportunities for academic and social belonging and connections [ 42 , 81 ] and including PGRs only in a fleeting or ‘hollow’ sense [ 37 ]. DRs identified this isolation as sending a broader message about academia as a solitary and unsupported pursuit; a message that could lead some DRs to self-select out of planning for future in academia [ 37 , 42 ]. DRs appeared to make sense of their lack of belonging in their department as related to their sense of being different, and that this difference might suggest they did not ‘fit in’ with academia more broadly [ 74 ]. In the short-term, DRs might expend more effort to try and achieve a social and/or professional connection and equitable access to support, opportunities and resources [ 74 ]. However, over the longer-term, the continuing perception of being professionally ‘other’ also seemed to undermine DRs’ sense of meaning and purpose [ 81 ] and could lead to opting out of an academic career [ 62 , 74 ].
Isolation within the PhD was compounded by isolation from one’s personal relationships. This personal isolation was first physical, in which the laborious nature of the PhD acted as a catalyst for the breakdown of pre-existing relationships [ 76 ]. Moreover, DRs also experienced a sense of psychological detachment [ 45 , 74 ]. Thus, the experience of isolation appeared to be extremely pervasive, with DRs feeling excluded and isolated physically and psychologically and across both their professional and personal lives.
It’s not you, it’s me
‘It’s not you, it’s me’ reflects DRs’ perfectionism as a central challenge of their PhD experience and a contributor to their sense of psychological isolation from other people. DRs’ perfectionism manifested in four key ways; firstly, in the overwhelming sense of responsibility experienced by DRs; secondly, in the tendency to position themselves as inadequate and inferior; thirdly, in cycles of perfectionist paralysis; and finally, in the tendency to find evidence which confirms their assumed inferiority.
DRs positioned themselves as solely responsible for their PhD and for the creation of a positive relationship with their supervisor [ 36 , 52 , 81 ]. DRs expressed a perceived need to capture their supervisors’ interest and attention [ 36 , 52 , 74 ], feeling that they needed to identify and sell to their supervisors some shared characteristic or interest in order to scaffold a meaningful relationship. DRs appeared to feel it necessary to assume sole responsibility for their personal lives and to prohibit any intrusion of the personal in to the professional, even in incredibly distressing circumstances [ 42 ].
DRs appeared to compare themselves against an ideal or archetypal DR and this comparison was typically unfavourable [ 37 ], with DRs contrasting the expected ideal self with their actual imperfect and fallible self [ 37 , 42 , 52 ]. DRs’ sense of inadequacy appeared acutely and frequently reflected back to them by supervisors in the form of negative or seemingly disdainful feedback and interactions [ 41 , 76 ]. DRs framed negative supervisor responses as a cue to work harder, meaning they were continually striving, but never reaching, the DR ideal [ 76 ]. This ideal-actual self-discrepancy was associated with a tendency towards punitive self-talk with clear negative valence [ 38 ].
DRs appear to commonly use self-castigation as a necessary (albeit insufficient) means to motivate themselves to improve their performance in line with perfectionistic standards [ 38 , 41 ]. The oscillation between expectation and actuality ultimately resulted in increased stress and anxiety and reduced enjoyment and motivation. Low motivation and enjoyment appeared to cause procrastination and avoidance, which lead to a greater discrepancy between the ideal and actual self; in turn, this caused more stress and anxiety and further reduced enjoyment and motivation leading to a sense of stuckness [ 76 ].
The internalisation of perceived failure was such that DRs appeared to make sense of their place, progress and possible futures through a lens of inferiority, for example, positioning themselves as less talented and successful compared to their peers [ 37 ]. Thus, instances such as not being offered a job, not receiving funding, not feeling connected to supervisors, feeling excluded by academics and peers were all made sense of in relation to DRs’ perceived relative inadequacy [ 36 ].
Death of personhood
The higher-order theme ‘Death of personhood’ reflects DRs’ identity conflict during the PhD process; a sense that DRs’ engage in a ‘Sacrifice of personal identity’ in which they feel they must give up their pre-existing self-identity, begin to conceive of themselves as purely ‘takers’ personally and professionally, thus experiencing the ‘Self as parasitic’, and ultimately experience a ‘Death of self-agency’ in relation to the thesis, the supervisor and other life roles and activities.
A sacrifice of personal identity
The sacrifice of personal identity first manifests as an enmeshment with the PhD and consequent diminishment of other roles, relationships and activities that once were integral to the DRs’ sense of self [ 59 , 76 ]. DRs tended to prioritise PhD activities to the extent that they engaged in behaviours that were potentially damaging to their personal relationships [ 76 ]. DRs reported a sense of never being truly free; almost physically burdened by the weight of their PhD and carrying with them a constant ambient guilt [ 37 , 38 , 44 , 76 ]. Time spent on non-PhD activities was positioned as selfish or indulgent, even very basic activities of living [ 76 ].
The seeming incompatibility of aspects of prior personal identity and the PhD appears to result in a sense of internal conflict or identity ‘collision’ [ 59 ]. Friends and relatives often provided an uncomfortable reflection of the DR’s changing identity, leaving DRs feeling hyper-visible and carrying the burden of intellect or trailblazer status [ 74 ]; providing further evidence for the incompatibility of their personal and current and future professional identities. Some DRs more purposefully pruned their relationships and social activities; to avoid identity dissonance, to conserve precious time and energy for their PhD work, or as an acceptance of total enmeshment with academic work as necessary (although not necessarily sufficient) for successful continuation in academia [ 40 , 52 , 77 ]. Nevertheless, the diminishment of the personal identity did not appear balanced by the development of a positive professional identity. The professional DR identity was perceived as unclear and confusing, and the adoption of an academic identity appeared to require DRs to have a greater degree of self-assurance or self-belief than was often the case [ 37 , 81 ].
Self as parasitic
Another change in identity manifested as DRs beginning to conceive of themselves as parasitic. DRs spoke of becoming ‘takers’, feeling that they were unable to provide or give anything to anyone. For some DRs, being ‘parasitic’ reflected them being on the bottom rung of the professional ladder or the ‘bottom of the pile’; thus, professionally only able to receive support and assistance rather than to provide for others. Other DRs reported more purposefully withdrawing from activities in which they were a ‘giver’, for example voluntary work, as providing or caring for others required time or energy that they no longer had [ 38 , 44 ]. Furthermore, DRs appeared to conceive of themselves as also causing difficulty or harm to others [ 81 ], as problems in relation to their PhD could lead them to unwillingly punishing close others, for example, through reducing the duration or quality of time spent together [ 38 ].
Feeling that close others were offering support appeared to heighten the awareness of the toll of the PhD on the individual and their close relationships, emphasising the huge undertaking and the often seemingly slow progress, and actually contributing to the sense of ambient guilt, shame, anger and failure [ 38 ]. Moreover, DRs spoke of feeling extreme guilt in perceiving that they had possibly sacrificed their own, and possibly family members’, current wellbeing and future financial security [ 49 ].
Death of self-agency
In addition to their sense of having to sacrifice their personal identity, DRs also expressed a loss of their sense of themselves as agentic beings. DRs expressed feeling powerless in various domains of their lives. First, DRs positioned the thesis as a powerful force able to overwhelm or swallow them [ 46 , 52 , 59 ]. Secondly, DRs expressed a sense of futility in trying to retain any sense of personal power in the climate of academia. An acute feeling of powerlessness especially in relation to supervisors was evident, with many examples provided of being treated as means to an end, as opposed to ends in themselves [ 39 , 42 , 62 ]. Supervisors did not interact with DRs in a holistic way that recognised their personhood and instead were perceived as prioritising their own will, or the will of other academics, above that of the DR [ 39 , 62 ].
Furthermore, DRs reported feeling as if they were used as a means for research production or furthering their supervisors’ reputations or careers [ 62 ]. DRs perceived that holding on to a sense of personal agency sometimes felt incompatible with having a positive supervisor relationship [ 42 ]. Thus whilst emotional distress, anger, disappointment, sadness, jealousy and resentment were clearly evident in relation to feeling excluded, used or over-powered by supervisors [ 37 , 42 , 52 , 62 ], DRs usually felt unable to change supervisor irrespective of how seriously this relationship had degraded [ 37 , 62 ]. Instead, DRs appeared to take on a position of resignation or defensive pessimism, in which they perceived their supervisors as thwarting their personhood, personal goals and preferences, but typically felt compelled to accept this as the status quo and focus on finishing their PhDs [ 42 ]. DRs resignation was such that they internalised this culture of silence and silenced themselves; tending to share litanies of problems with supervisors whilst prefacing or ending the statements with some contradictory or undermining phrase such as ‘but that’s okay’ [ 42 , 52 ].
The apparent lack of self-agency extended outward from the PhD into DRs not feeling able to curate positive life circumstances more generally [ 76 ]. A lack of time was perhaps the key struggle across both personal and professional domains, yet DRs paradoxically reported spending a lot of time procrastinating and rarely (if ever) mentioned time management as a necessary or desired coping strategy for the problem of having too little time [ 46 ]. The lack of self-agency was not only current but also felt in reference to a bleak and uncertain future; DRs lack of surety in a future in academia and the resultant sense of futility further undermined their motivation to engage currently with PhD tasks [ 38 , 40 ].
The system is sick
The higher-order theme ‘The system is sick’ represents systemic influences on DR mental health. First, ‘Most everyone’s mad here’ reflects the perceived ubiquity mental health problems amongst DRs. ‘Emperor’s new clothes’ reflects the DR experience of engaging in a performative piece in which they attempt to live in accordance with systemic rather than personal values. Finally, ‘Beware the invisible and visible walls’ reflects concerns with being caught between ephemeral but very real institutional divides.
Most everyone’s mad here
No studies focused explicitly on experiences of DRs who had been given diagnoses of mental health problems. Some study participants self-disclosed mental health problems and emphasised their pervasive impact [ 50 ]. Further lived experiences of mental distress in the absence of explicit disclosure were also clearly identifiable. The ‘typical’ presentation of DRs with respect to mental health appeared characterised as almost unanimous [ 39 ] accounts of chronic stress, anxiety and depression, emotional distress including frustration, anger and irritability, lack of mental and physical energy, somatic problems including appetite problems, headaches, physical pain, nausea and problems with drug and alcohol abuse [ 39 , 46 , 59 , 76 ]. Health anxiety, concerns regarding perceived new and unusual bodily sensations and perceived risks of developing stress-related illnesses were also common [ 46 , 59 , 76 ]. A PhD-specific numbness and hypervigilance was also reported, in which DRs might be less responsive to personal life stressors but develop an extreme sensitivity and reactivity to PhD-relevant stimuli [ 39 ].
An interplay of trait and state factors were suggested to underlie the perceived ubiquity of mental health problems amongst DRs. Etiological factors associated with undertaking a PhD specifically included the high workload, high academic standards, competing personal and professional demands, social isolation, poor resources in the university, poor living conditions and poverty, future and career uncertainty [ 36 , 41 , 43 , 46 , 49 , 76 ]. The ‘nexus’ of these factors was such that the PhD itself acted as a crucible; a process of such intensity that developing mental health problems was perhaps inevitable [ 39 ].
The perceived inevitability of mental health problems was such that DRs described people who did not experience mental health problems during a PhD as ‘lucky’ [ 39 ]. Supervisors and the wider academic system were seen to promote an expectation of suffering, for example, with academics reportedly normalising drug and alcohol problems and encouraging unhealthy working practices [ 39 ]. Furthermore, DRs felt that academics were uncaring with respect to the mental challenge of doing a PhD [ 39 ]. Nevertheless, academics were suggested to deny any culpability or accountability for mental health problems amongst DRs [ 39 , 59 , 74 ]. The cycle of indigenousness was further maintained by a lack of mental health literacy and issues with awareness, availability and access to help-seeking and treatment options amongst DRs and academics more widely [ 39 ]. Thus, DRs appeared to feel they were being let down by a system that was almost set up to cause mental distress, but within which there was a widespread denial of the size and scope of the problem and little effort put into identifying and providing solutions [ 39 , 59 ]. DRs ultimately felt that the systemic encouragement of unhealthy lifestyles in pursuit of academic success was tantamount to abuse [ 62 ].
A performance of optimum suffering
Against a backdrop of expected mental distress, DRs expressed their PhD as a performative piece. DRs first had to show just the right amount of struggle and difficulty; feeling that if they did not exhibit enough stress, distress and ill-health, their supervisors or the wider department might not believe they were taking their PhD seriously enough [ 40 ]. At the same time, DRs felt that their ‘researcher mettle’ was constantly being tested and they must rise to this challenge. This included first guarding against presenting oneself as intellectually inferior [ 36 ]. Yet it also seemed imperative not to show vulnerability more broadly [ 74 ]. Disclosing mental or physical health problems might lead not only to changed perceptions of the DR but to material disadvantage [ 74 ]. The poor response to mental health disclosures suggested to some DRs that universities might be purposefully trying to dissuade or discourage DRs with mental health problems or learning disabilities from continuing [ 74 ]. The performative piece is thus multi-layered, in that DRs must experience extreme internal psychological struggles, exhibit some lower-level signs of stress and fatigue for peer and faculty observance, yet avoid expressing any real academic or interpersonal weakness or the disclosure of any diagnosable disability or disease.
Emperor’s new clothes
DRs described feeling beholden to the prevailing culture in which it was expected to prioritise above all else developing into a competitive, self-promoting researcher in a high-performing research-active institution [ 39 , 42 ]. Supervisors often appeared the conduit for transmission of this academic ideal [ 74 ]. DRs felt reticent to act in any way which suggested that they did not personally value the pursuit of a leading research career above all else. For example, DRs felt that valuing teaching was non-conformist and could endanger their continuing success within their current institution [ 55 ]. Many DRs thus exhibited a sense of dissonance as their personal values often did not align with the institutional values they identified [ 74 ]. Yet DRs expressed a sense of powerlessness and a feeling of being ‘caught up’ in the values of the institution even when such values were personally incongruent [ 74 ]. The psychological toll of this sense of inauthenticity seemed high [ 55 ]. Where DRs acted in ways which ostensibly suggested values other than prioritising a research career, for example becoming pregnant, they sensed disapproval [ 76 ]. DRs also felt unable to challenge other ‘institutional myths’ for example, the perceived institutional denial of the duration of and financial struggle involved in completing a PhD [ 49 ]. There was a perceived tendency of academics to locate problems within DRs as opposed to acknowledging institutional or systemic inequalities [ 49 ]. DRs expressed strongly a sense in which there is inequity in support, resources and opportunities, yet universities were perceived as ignoring such inequity or labelling such divisions as based on meritocracy [ 36 , 74 ].
Beware the invisible and visible walls
DRs described the reality of working in academia as needing to negotiate a maze of invisible and visible walls. In the former case, ‘invisible walls’ reflect ephemeral norms and rules that govern academia. DRs felt that a big part of their continuing success rested upon being able to negotiate such rules [ 39 ]. Where rules were violated and explicit or implicit conflicts occurred, DRs were seen to be vulnerable to being caught in the ‘crossfire’ [ 36 ]. DRs identified academic groups and departments as being poor in explicitly identifying, discussing and resolving conflicts [ 37 ]. The intangibility of the ‘invisible walls’ gave rise to a sense of ambient anxiety about inadvertently transgressing norms and divides, such that some DRs reported behaving in ways that surprised even themselves [ 37 ].
Gendered and racial micropolitics of academic institutions were seen to manifest as more visible walls between people, with institutions privileging those with ‘insider’ status [ 36 ]. Women and people of colour typically felt excluded or disadvantaged in a myriad of observable and unobservable ways, with individuals able to experience both insider and outsider statuses simultaneously [ 36 , 37 ], for example when a male person of colour [ 36 ]. Female DRs suggested that not only must women prove themselves to a greater extent than men to receive equal access to resources, opportunities and acclaim but also are typically under additional pressure in both their professional and personal lives [ 37 , 52 , 76 ]. Women also felt that they had to take on more additional roles and responsibilities and encountered more conflicts in their personal lives compared to men [ 52 ]. Examples of professionally successful women in DRs’ departments were described as those who had crossed the divide and adopted a more traditionally male role [ 40 ]. Thus, being female or non-White were considered visible characteristics that would disadvantage people in the competitive academic environment and could give rise to a feeling of increased stress, pressure, role conflicts, and a feeling of being unsafe.
Seeing, being and becoming
The higher-order theme of ‘Seeing, being and becoming’ reflects protective and transformative influences on DR mental health. ‘De-programming’ refers to the DRs disentangling their personal beliefs and values from systemic values and also from their own tendency towards perfectionism. ‘The power of being seen’ reflects the positive impact on DR mental health afforded by feeling visible to personal and professional others. ‘Finding hope, meaning and authenticity’ refers to processes by which DRs can find or re-locate their own self-agency, purpose and re/establish a sense of living in accordance with their values. ‘The importance of multiple goals, roles and groups’ represents the beneficial aspects of accruing and sustaining multiple aspects to one’s identity and connections with others and activities outside the PhD. Finally, ‘The PhD as a process of transcendence’ reflects how the struggles involved in completing a PhD can be transformative and self-actualising.
De-programming
DRs reported being able to protect their mental health by ‘de-programming’ and disentangling their attitudes and practices from social and systemic values and norms. This disentangling helped negate DRs’ adopting unhealthy working practices and offered some protection against experiencing inauthenticity and dissonance between personal and systemic values.
First, DRs spoke of rejecting the belief that they should sacrifice or neglect personal relationships, outside interests and their self-identity in pursuit of academic achievement. DRs could opt-out entirely by choosing a ‘user-friendly’ programme [ 44 ] which encouraged balance between personal and professional goals, or else could psychologically reject the prevailing institutional discourse [ 40 ]. Rather than halting success, de-programming from the prioritisation of academia above all else was seen to be associated not only with reduced stress but greater confidence, career commitment and motivation [ 40 , 50 ]. It was also suggested possible to ‘de-programme’ in the sense of choosing not to be preoccupied by the ‘invisible walls’ of academia and psychologically ‘opt out’ of being concerned by potential conflicts, norms and rules governing academic workplace conduct [ 36 ]. Interaction with people outside of academia was seen to scaffold de-programming, by helping DRs to stay ‘grounded’ and offering a model what ‘normal’ life looks like. People outside of academia could also help DRs to see the truth by providing unbiased opinions regarding systemic practices [ 39 ].
A further way in which de-programming manifested was in DRs challenging their perfectionist beliefs. This include re-framing the goal as not trying to be the archetype of a perfect DR, and accepting that multiple demands placed on one individual invariably requires compromise [ 40 , 76 ]. DRs spoke of the need to conceptualise the PhD as a process, rather than just a product [ 46 , 82 ]. The process orientation facilitated framing of the PhD as just one-step in the broader process of becoming an academic as opposed to providing discrete evidence of worth [ 82 ]. Within this perspective, uncertainty itself could be conceived as a privilege [ 81 ]. The PhD was then seen as an opportunity rather than a test [ 37 , 46 ]. Moreover, the process orientation facilitated viewing the PhD as a means of growing into a contributing member of the research community, as opposed to needing to prove oneself to be accepted [ 82 ]. Remembering the temporary nature of the PhD was advised [ 45 ] as was holding on to a sense that not completing the PhD was also a viable life choice [ 76 ]. DRs also expressed, implicitly or explicitly, a decision to change their conceptualisation of themselves and their progress; choosing not to perceive themselves as stuck, but planning, learning and progressing [ 38 , 39 , 81 , 82 ]. This new perspective appeared to be helpful in reducing mental distress.
The power of being seen
DRs described powerful benefits to feeling seen by other people, including a sense of belonging and mattering, increased self-confidence and a sense of positive progress [ 37 ]. Being seen by others seems to provoke the genesis of an academic identity; it brings DRs into existence as academics. Being seen within the academic institution also supports mental health and can buffer emotional exhaustion [ 37 , 52 , 55 , 81 ]. DRs expressed a need to feel that supervisors, academics and peers were interested in them as people, their values, goals, struggles and successes; yet they also needed to feel that they and their research mattered and made a difference within and outside of the institution [ 42 , 52 , 81 ]. It was clear that DRs could find in their disciplinary communities the sense of belonging that often eluded them within their immediate departments [ 42 ]. Feeling a sense of belonging to the academic community seemed to buffer disengagement and amotivation during the PhD [ 81 ]. Positive engagement with the broader community was scaffolded by a sense of trust in the supervisor [ 81 ]. DRs often felt seen and supported by postdocs, especially where supervisors appeared absent or unsupportive [ 50 ].
Spending time with peers could be beneficial when there was a sense of shared experience and walking alongside each other [ 39 ]. Friendship was seen to buffer stress and protect against mental health problems through the provision of social and emotional support and help in identifying struggles [ 39 , 43 ]. In addition to relational aspects, the provision of designated physical spaces on campus or in university buildings also seemed important to being seen [ 37 ]. Peers in the university could provide DRs with further physical embodiments of being seen, for example, gift-giving in response to their birthdays or returning from leave [ 37 , 50 ]. Outside of the academic institution, DRs described how being seen by close others could support DRs to be their authentic selves, providing an antidote to the invisible walls of academia [ 50 ]. Good quality friendships within or outside academia could be life-changing, providing a visceral sense of connection, belonging and authenticity that can scaffold positive mental health outcomes during the PhD [ 39 ]. Pets could also serve to help DRs feel seen but without needing to extend too much energy into maintaining social relationships [ 50 ].
Finally, DRs also needed to see themselves, i.e. to begin to see themselves as burgeoning academics as opposed to ‘just students’ [ 81 ]. Feeling that the supervisor and broader academic community were supportive, developing one’s own network of process collaborators and successfully obtaining grant funding seemed tangible markers that helped DRs to see themselves as academics [ 37 , 81 ]. Seeing their own work published was also helpful in providing a boost in confidence and being a joyful experience [ 42 ]. Moreover, with sufficient self-agency, DRs can not only see themselves but render themselves visible to other people [ 37 ].
Multiple goals, roles and groups
In antidote to the diminished personal identity and enmeshment with the PhD, DRs benefitted from accruing and sustaining multiple goals, roles, occupations, activities and social group memberships. Although ‘costly’ in terms of increased stress and role conflicts, sustaining multiple roles and activities appeared essential for protecting against mental health problems [ 50 , 68 ].
Leisure activities appeared to support mental health through promoting physical health, buffering stress, providing an uplift to DRs’ mood and through the provision of another identity other than as an academic [ 44 , 50 , 76 ]. Furthermore, engagement in activities helped DRs to find a sense of freedom, allowing them to carve up leisure and work time and psychologically detach from their PhD [ 68 , 76 ]. Competing roles, especially family, forced DRs to distance themselves from the PhD physically which reinforced psychological separation [ 50 , 59 ]. Engaging in self-care and enjoyable activities provided a sense of balance and normalcy [ 39 , 44 , 68 ]. This normalcy was a needed antidote to abnormal pressure [ 59 ]. Even in the absence of fiercely competing roles and priorities, DRs still appeared to benefit from treating their PhD as if it is only one aspect of life [ 59 ]. Additional roles and activities reduced enmeshment with the PhD to the extent that considering not completing the PhD was less averse [ 40 ]. This position appeared to help DRs to be less overwhelmed and less sensitive to perceived and anticipated failures.
Finding hope, meaning and authenticity
Finding hopefulness and meaning within the PhD can scaffold a sense of living a purposeful, enjoyable, important and authentic life. Hopefulness is predicated on the ability to identify a goal, i.e. to visualise and focus on the desired outcome and to experience both self-agency and potential pathways towards the goal. Hopefulness was enhanced by the ability to break down tasks into smaller goals and progress in to ‘baby steps’ [ 38 , 59 ]. In addition, DRs benefitted from finding explicit milestones against which they can compare their progress [ 59 ], as this appeared to feed back into the cycle of hopeful thinking and spur further self-agency and goal pursuit.
The experience of meaning manifested in two main ways; first as the more immediate lived experience of passion in action [ 76 ]. Secondly, DRs found meaning in feeling that in their PhD and lives more broadly they were living in accordance with their values, for example, experiencing their own commitment in action through continuing to work on their PhD even when it was difficult to do so [ 76 ]. DRs who were able to locate their PhD within a broader sense of purpose appeared to derive wellbeing benefits. There was a need to ensure that values were in alignment, for example, finding homeostasis between emotional, intellectual, social and spiritual parts of the self [ 46 , 59 , 90 ].
The processes of finding hopefulness and meaning appear to be largely relational. Frequent contact with supervisors in person and social and academic contact with other DRs were basic scaffolds for hope and meaning [ 52 ]. DRs spoke of how a sense that their supervisors believed in them inspired their self-agency and motivation [ 42 , 62 , 76 ]. Partners, friends and family could also inspire motivation for continuing in PhD tasks [ 44 , 76 ]. Other people also could help instil a sense of motivation to progress and complete the PhD; a sense of being seen is to be beholden to finish [ 39 ]. Meaning appeared to be scaffolded by a sense of contribution, belonging and mattering [ 81 ] and could arise from the perception of putting something into the collective pot, inspiring hopefulness and helping others [ 39 , 42 ]. Moreover, hopefulness, meaning and authenticity also appeared mutually reinforcing [ 81 ]. Finding meaning and working on a project which is in accordance with personal values, preferences and interests is also helpful in completing the PhD and provides a feedback loop into hope, motivation and agentic thinking [ 39 , 81 ]. Furthermore, DRs could use agentic action to source a community of people who share their values, enabling them to engage in collective authenticity [ 39 ].
The PhD as a process of transcendence
The immense challenge of the PhD could be a catalyst for growth, change and self-actualisation, involving empowerment through knowledge, self-discovery, and developing increased confidence, maturity, capacity for self-direction and use of one’s own autonomy [ 44 , 82 ]. The PhD acted as a forge in which DRs were tested and became remoulded into something greater than they had been before [ 44 , 82 , 90 ]. The struggles endured during the PhD caused DRs to reconsider their sense of their own capacities, believing themselves to be more able than they previously would have thought [ 50 ]. The struggles endured added to the sense of accomplishment. A trusted and trusting supervisor appears to aid in the PhD being a process of transcendence [ 62 ].
More broadly, the PhD also helped DRs to transcend personal tragedy, allowing immersion in a meaningful activity which begins as a means of coping and becomes something completely [ 39 ]. The PhD could also serve as a transformative selection process for DRs’ social relationships, with some relationships cast aside and yet others formed anew [ 39 ]. Overall, therefore, the very aspects of the PhD which were challenging, and distressing could allow DRs to transcend their former selves and, through the struggle, become something more.
Summation of results
The findings regarding the risk and protective factors associated with DR mental health have been summarised in Table 3 in relation to (1) the type of research evidencing the factor (i.e. whether the evidence is quantitative only, part of the meta-synthesis only, or evident in both results sections); and (2) the volume of evidence (i.e. whether the factor was found in a single study or across multiple studies). The factors in the far-right column (i.e. the factors found across multiple research studies utilising both qualitative and quantitative methods) are the ones with the strongest evidence at present.
This systematic review summarises a heterogeneous research area, with the aim of understanding the mental health of DRs, including possible risk and protective factors. The qualitative and quantitative findings presented here suggest that poor mental health is a pertinent problem facing DRs; stress appears to be a key issue and significantly in excess of that experienced in the general population. Several risk and protective factors at the individual, interpersonal and systemic levels emerged as being important in determining the mental health of DRs. The factors with the strongest evidence-base (i.e. those supported by multiple studies using qualitative and quantitative findings) denote that being female and isolated increases the risk of the mental health problems, whereas seeing the PhD as a process, feeling socially supported, having a positive supervisor relationship and engaging in self-care is protective.
Results in context
Stress can be defined as (1) the extent to which a stimulus exerts pressure on an individual, and their propensity to bear the load; (2) the duration of the response to an aversive stimuli, from initial alert to exhaustion; or (3) a dynamic (im)balance between the demands and personal resource to manage those demands [ 91 ]. The Perceived Stress Scale (PSS) [ 18 , 19 ] used in our meta-analysis is aligned with the third of these definitions. As elaborated upon within the Transactional Model of Stress [ 92 ], stress is conceptualised as a persons’ appraisal of the internal and external demands put upon them, and whether these exceed their available resources. Thus, our results suggest that, when compared to the general population, PhD students experience a greater maladaptive imbalance between their available resources and the demands placed upon them. Stress in itself is not a diagnosable mental health problem, yet chronic stress is a common precipitant to mental health difficulties such as depression and posttraumatic stress disorder [ 93 , 94 ]. Therefore, interventions should seek to bolster DRs’ resources and limit demands placed on them to minimise the risks associated with acute stress and limit its chronicity.
Individual factors
Female DRs were identified as being at particular risk of developing mental health difficulties. This may result from additional hurdles when studying in a male-dominated profession [ 95 , 96 , 97 ], and the expectation that in addition to their doctoral studies, females should retain sole or majority responsibility for the domestic and/or caring duties within their family [ 52 , 76 ]. It may also be that females are more willing to disclose and seek help for mental health difficulties [ 98 ]. Nevertheless, the World Health Organisation (WHO) mental health survey results indicate that whilst anxiety and mood disorders are more prevalent amongst females, externalising disorders are more common in males [ 99 ]. As the vast majority of studies in this review focussed on internalising problems (e.g. stress, anxiety and depression) [ 37 , 64 , 79 , 80 , 83 , 89 ], this may explain the gender differences found in this review. Further research is needed to explore which perspective, if any, may explain gender gap in our results.
Perhaps unsurprisingly, self-care was associated with reduced mental health problems. The quantitative findings suggest that all types of self-care are likely to be protective of mental health (i.e. physical, emotional, professional and spiritual self-care). Self-care affords DRs the opportunity to take time away from their studies and nurture their non-PhD identities. However, the results from our meta-synthesis suggest that DRs are not attending to their most basic needs much less engaging in self-care behaviours that correspond to psychological and/or self-fulfilment needs [ 100 ]. Consequently, an important area for future enquiry will be identifying the barriers preventing DRs from engaging in self-care.
Interpersonal factors
Across both quantitative and qualitative studies, interpersonal factors emerged as the most salient correlate of DR mental health. That is, isolation was a risk factor, whereas connectedness to others was a protective factor. There was some variability in how these constructs were conceptualised across studies, i.e. (1) isolation: a lack of social support, having fewer social connections, feeling isolated or being physically separate from others; and (2) social connectedness: multiple group membership, academic relationships or non-academic relationships; but there was no indication that effects varied between concepts. The relationship between isolation and negative health consequences is well-established, for example both physical and mental health problems [ 101 ], and even increased mortality [ 102 ]. Conversely, social support is associated with reduced stress in the workplace [ 103 , 104 ]. Reducing isolation is therefore a promising interventional target for improving DRs’ mental health.
The findings regarding isolation are even more alarming when considered alongside the findings from several studies that PhD studies are consistently reported to dominate the lives of DRs, resulting in poor ‘work-life balance’ and losing non-PhD aspects of their identities. The negative impact of having fewer identities [ 105 ] can be mitigated by having a strong support network [ 106 ], and increasing multiple group memberships [ 107 ]. But for DRs, it is perhaps the absence of this social support, combined with identity impoverishment, which can explain the higher than average prevalence of stress found in our meta-analysis.
Systemic factors
DRs’ attitudes towards their studies may be a product of top-down systemic issues in academia more broadly. Experiencing mental health problems was reported as being the ‘norm’, but also appeared to be understood as a sign of weakness. The meta-synthesis results suggest that DRs believed their respective universities prioritise academic success over workplace wellbeing and encourage unhealthy working habits. Working in an unsupportive and pressured environment is strongly associated with negative psychological outcomes, including increased depression, anxiety and burnout [ 108 ]. The supervisory relationship appeared a particularly important aspect of the workplace environment. The quantitative analysis found a negative correlation between inspirational supervision and mental health problems. Meta-synthetic finding suggested toxic DR-supervisor relationships characterised by powerlessness and neglect, as well as relationships where DRs felt valued and respected—the former of these being associated with poor mental health, and the latter being protective. The association between DR-supervisor relationship characteristics needs to be verified using quantitative methods. Furthermore, DRs’ sense that they needed to exhibit ‘optimum suffering’, which appears to reflect a PhD-specific aspect of a broader academic performativity [ 109 ], is an important area for consideration. An accepted narrative around DRs needing to experience a certain level of dis/stress would likely contribute to poor mental health and as an impediment to the uptake and effectiveness of proffered interventions. Although further research is needed, it is apparent that individual interventions alone are not sufficient to improve DR mental health, and that a widespread culture shift is needed in order to prevent the transmission of unhealthy work attitudes and practices.
Limitations of the literature
Although we found a respectable number of articles in this area, the focus and measures used varied to the extent that typical review analysis procedures could not be used. That is, there was much heterogeneity in terms of how mental health was conceptualised and measured, as well as the range of risk and protective factors explored. Similarly, the quality of the studies was hugely variable. Common flaws amongst the literature include small sample sizes, the use of unvalidated tools and the incomplete reporting of results. Furthermore, for qualitative studies specifically, there appeared to be a focus on breadth instead of depth, particularly in relation to studies using mixed methods.
The generalisability of our findings is limited largely due to the lack of research conducted outside of the US, but also because we limited our review to papers written in English only. The nature of doctoral studies varies in important ways between studies. For example, in Europe, PhD studies usually apply for funding to complete their thesis within 3–4 years and must know their topic of interest at the application stage. Whereas in the US, PhD studies usually take between 5 and 6 years, involve taking classes and completing assignments, and the thesis topic evolves over the course of the PhD. These factors, as well as any differences in the academic culture, are likely to affect the prevalence of mental health problems amongst DRs and the associated risk and protective factors. More research is needed outside of the US.
‘Mental health’ in this review was largely conceptualised as a type of general wellbeing rather than a clinically meaningful construct. None of the studies were ostensibly focused on sampling DRs who were currently experiencing or had previously experienced mental health problems per se, meaning the relevance of the risk, vulnerability and protective factors identified in the meta-synthesis may be more limited in this group. Few studies used clinically meaningful measures. Where clinical measures were used, they captured data on common mental health problems only (i.e. anxiety and depression). Due to these limitations, we are unable to make any assertions about the prevalence of clinical-level mental health problems amongst DRs.
Limitations of this review
As a result of the heterogeneity in this research area, some of the results presented within this review are based on single studies (e.g. correlation data; see Fig. 5 ) rather than the amalgamation of several studies (e.g. meta-analysis/synthesis). To aid clarity when interpreting the results of this review, we have (Table 3 ) summarised the volume of evidence supporting risk and protective factors. Moreover, due to the small number of studies eligible for inclusion in this review, we were unable to test whether any of our findings are related to the study characteristics (e.g. year of publication, country of origin, methodology).
We were able to conduct three meta-analyses, one of which aimed to calculate the between-group effect size on the PSS [ 18 , 19 ] between DRs and normative population data. Comparing these data allowed us to draw some initial conclusions about the prevalence of stress amongst DRs, yet we were unable to control for other group differences which might moderate stress levels. For example, the population data was from people in the United States (US) in 1 year, whereas the DR data was multi-national at a variety of time points; and self-reported stress levels may vary with nationality [ 110 ] or by generation [ 111 , 112 ]. Moreover, two of the three meta-analyses showed significant heterogeneity. This heterogeneity could be explained by differences in the sample characteristics (e.g. demographics, country of origin), doctoral programme characteristics (e.g. area of study, funding status, duration of course) or research characteristics (e.g. study design, questionnaires used). However, due to the small number of studies included in these meta-analyses, we were unable to test any of these hypotheses and are therefore unable to determine the cause of this heterogeneity. As more research is conducted on the mental health of DRs, we will be able to conduct larger and more robust meta-analyses that have sufficient power and variance to statistically explore the causes of this heterogeneity. At present, our findings should be interpreted in light of this limitation.
Practice recommendations
Although further research is clearly needed, we assert that this review has identified sufficient evidence in support of several risk and protective factors to the extent that they could inform prevention and intervention strategies. Several studies have evidenced that isolation is toxic for DRs, and that social support can protect against poor mental health. Initiatives that provide DRs with the opportunity to network and socialise both in and outside of their studies are likely to be beneficial. Moreover, there is support for psychoeducation programmes that introduce DRs to a variety of self-care strategies, allow them to find the strategies that work for them and encourage DRs to make time to regularly enact their chosen strategies. Finally, the supervisory relationship was identified as an important correlate of DR mental health. Positive supervision was characterised as inspirational and inclusive, whereas negative supervision productised DRs or neglected them altogether. Supervisor training programmes should be reviewed in light of these findings to inform how institutions shape supervisory practices. Moreover, the initial findings reported here evidence a culture of normalising and even celebrating suffering in academia. It is imperative therefore that efforts to improve and protect the mental health of DRs are endorsed by the whole institution.
Research recommendations
First, we encourage further large-scale mental health prevalence studies that include a non-PhD comparison group and use validated clinical tools. None of the existing studies focused on the presence of serious mental health problems—this should be a priority for future studies in this area. Mixed-methods explorations of the experiences of DRs who have mental health problems, including serious problems, and in accessing mental health support services would be a welcome addition to the literature. More qualitative studies involving in-depth data collection, for example interview and focus group techniques, would be useful in further supplementing findings from qualitative surveys. Our review highlights a need for better communication and collaboration amongst researchers in this field with the goal of creating a level of consistency across studies to strengthen any future reviews on this subject.
The results from this systematic review, meta-analysis and meta-synthesis suggest that DRs reported greater levels of stress than the general population. Research regarding the risk and protective factors associated with the mental health of DRs is heterogenous and disparate. Based on available evidence, robust risk factors appear to include being isolated and being female, and robust protective factors include social support, viewing the PhD as a process, a positive DR-supervisor relationship and engaging in self-care. Further high-quality, controlled research is needed before any firm statements can be made regarding the prevalence of clinically relevant mental health problems in this population.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Confidence intervals
Doctoral researchers
Higher Education Statistics Agency
Perceived Stress Scale
Standard deviation
United Kingdom
United States
Baron E. Eleven sketches inspired by the university mental health crisis—in pictures. The Guardian. 2017. Available from: https://www.theguardian.com/education/gallery/2017/jun/27/eleven-sketches-university-mental-health-crisis . Cited 2017 Oct 6.
Google Scholar
National Union of Students. 20 per cent of students consider themselves to have a mental health problem: National Union of Students; 2013. Available from: https://www.nus.org.uk/en/news/20-per-cent-of-students-consider-themselves-to-have-a-mental-health-problem/ . Cited 2017 Oct 6.
YouGov. One in four students suffer from mental health problems. 2016. Available from: https://d25d2506sfb94s.cloudfront.net/cumulus_uploads/document/obtomdatp4/Survey_Results.pdf . Cited 2017 Oct 6.
Universities UK. Minding Our Future: starting a conversation about the support of student mental health. London: Universities UK; 2017. Available from: https://www.universitiesuk.ac.uk/minding-our-future .
The Guardian. Number of university dropouts due to mental health problems trebles. The Guardian. 2017. Available from: https://www.theguardian.com/society/2017/may/23/number-university-dropouts-due-to-mental-health-problems-trebles . Cited 2017 Oct 6.
Thorley C. Not By Degrees: Improving student mental health in the UK’s universities. London; 2017. Available from: www.ippr.org . Cited 2017 Oct 6.
Oswalt SB, Lederer AM, Chestnut-Steich K, Day C, Halbritter A, Ortiz D. Trends in college students’ mental health diagnoses and utilization of services, 2009–2015. J Am Coll Health. 2018;68:41–51.
Auerbach RP, Mortier P, Bruffaerts R, Alonso J, Benjet C, Cuijpers P, et al. WHO world mental health surveys international college student project: prevalence and distribution of mental disorders. J Abnorm Psychol. 2018;127(7):623–38.
PubMed PubMed Central Google Scholar
OECD. Education at a Glance 2019. Education at a Glance: OECD Indicators: OECD; 2019. (Education at a Glance). Available from: http://gpseducation.oecd.org/Content/EAGCountryNotes/BRA.pdf . Cited 2020 Mar 26.
OECD. OECD Science, Technology and Innovation Outlook 2016. OECD Science, technology and innovation outlook 2016. 2016. Available from: http://www.oecd.org/sti/STIO 10 key technology trends for the future.pdf. Cited 2020 Mar 26.
Higher Education Statistics Agency (HESA). Higher education student statistics: UK, 2016/17: HESA; 2018. Available from: https://www.hesa.ac.uk/news/11-01-2018/sfr247-higher-education-student-statistics/numbers .
NCES. Number of doctoral degrees earned in the United States from 1949/50 to 2028/29, by gender. 2019. Available from: https://www.statista.com/statistics/185167/number-of-doctoral-degrees-by-gender-since-1950/ .
Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46 Available from: http://psycnet.apa.org/index.cfm?fa=search.displayRecord&uid=1960-06759-001 .
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159 Available from: http://www.jstor.org/stable/2529310?origin=crossref . Cited 2017 Mar 8.
CAS PubMed Google Scholar
Noblit GW, Hare RD. Meta-ethnography: Synthesizing qualitative studies: Sage Publications; 1988. p. 88.
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:45.
Wilson DB. Meta-analysis stuff. 2011. Available from: http://mason.gmu.edu/~dwilsonb/ma.html . Cited 2017 Dec 3.
Cohen S, Williamson GM. Perceived stress in a probability sample of the U.S. In: Spacapam S, Oskamp S, editors. The social psychology of health: Claremont Symposium on Applied Social Psychology. Newbury Park, CA: Sage; 1988.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96.
Cohen S, Janicki-Deverts D. Who’s Stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. J Appl Soc Psychol. 2012;42(6):1320–34.
MedCalc Software bvba. MedCalc Statistical Software. Belgium: Ostend; 2016.
Viechtbauer W. Bias and efficiency of Meta-analytic variance estimators in the random-effects model. J Educ Behav Stat. 2005;30(3):261–93 Available from: http://jeb.sagepub.com/cgi/doi/10.3102/10769986030003261 . Cited 2017 Mar 8.
Hedges LV, Ollkin L. Statistical methods for meta-analysis. New York: Academic Press; 1985. Available from:. https://doi.org/10.1002/9780470743386.refs .
Book Google Scholar
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Chichester: Wiley; 2009. Cited 2019 Jan 10. Available from. https://doi.org/10.1002/9780470743386 .
Fisher RA. Frequency distribution of the values of the correlation coefficient in samples from an indefinitely large population. Biometrika. 1915;10(4):507–21 Available from: https://www.statista.com/statistics/185167/number-of-doctoral-degrees-by-gender-since-1950/ .
Schünemann H, Brożek J, Guyatt G, Oxman A. Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach: GRADE Working Group; 2013. Available from: gdt.guidelinedevelopment.org/app/handbook/handbook.html .
Lachal J, Revah-Levy A, Orri M, Moro MR. Metasynthesis: an original method to synthesize qualitative literature in psychiatry. Front Psychiatry. 2017;8:269.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Braun V, Clarke V. Successful qualitative research: a practical guide for beginners. London: Sage Publications Ltd; 2013.
Bhaskar R. The possibility of naturalism: a philosophical critique of the contemporary human sciences. London: Routledge; 2014.
Fletcher AJ. Applying critical realism in qualitative research: methodology meets method. Int J Soc Res Methodol. 2017;20(2):181–94.
Walsh D, Downe S. Meta-synthesis method for qualitative research: a literature review. J Adv Nurs. 2005;50(2):204–11.
PubMed Google Scholar
Maton K. Reflexivity, relationism, & research: Pierre Bourdieu and the epistemic conditions of social scientific knowledge. Sp Cult. 2003;6(1):52–65.
Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12(1):181.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for Reporting Observational Studies. Ann Intern Med. 2007;147(8):573. Cited 2019 Sep 27. Available from. https://doi.org/10.7326/0003-4819-147-8-200710160-00010 .
Article Google Scholar
Acker S, Haque E. The struggle to make sense of doctoral study. High Educ Res Dev. 2015;34(2):229–41. Available from. https://doi.org/10.1080/07294360.2014.956699 .
Appel ML, Dahlgren LG. Swedish doctoral students’ experiences on their journey towards a PhD: obstacles and opportunities inside and outside the academic building. Scand J Educ Res. 2003;47(1):89–110. Available from. https://doi.org/10.1080/00313830308608 .
Devonport TJ, Lane AM. In it together: Dyadic coping among doctoral students and partners. J Hosp Leis Sport Tour Educ. 2014;15:124–34. Available from. https://doi.org/10.1016/j.jhlste.2014.08.002 .
Enzor J. Friendship, mental health, and doctoral education: a generic qualitative thematic analysis: Capella University; 2017.
Kurtz-Costes B, Helmke LA, Ülkü-Steiner B. Gender and doctoral studies: the perceptions of Ph.D. students in an American university. Gend Educ. 2006;18(2):137–55.
Bazrafkan L, Shokrpour N, Yousefi A, Yamani N. Management of stress and anxiety among PhD students during thesis writing: a qualitative study. The Health Care Manager. 2016;35:231–40.
Cotterall S. More than just a brain: emotions and the doctoral experience. High Educ Res Dev. 2013;32(2):174–87.
Kaufman JA. Personal perceptions of stress and self-perceived need for social support among doctoral psychology students in a distance education university sample: Capella University; 2004.
Kenty JR. Stress management strategies for women doctoral students. Nurse Educ. 2000;25(5):251–4 Available from: http://pesquisa.bvsalud.org/portal/resource/pt/mdl-16646205 .
Scrubb MM. An examination of the doctoral student stress survey (DSSS) as an instrument for measuring the effects of stress as perceived by doctoral students in a distance learning university: Walden University; 1997.
Usman Yousaf S, Akram M, Usman B. Exploring the causes of stress and coping with it amongst doctoral level students: highlighting the importance of information collection and management. Pakistan J Inf Manag Libr. 2016;18(2):12–25 Available from: https://search.proquest.com/openview/68246cbba8a9da0ec067d56631b479f1/1?pq-origsite=gscholar&cbl=54989 .
Sandelowski M, Voils CI, Barroso J. Defining and designing mixed research synthesis Studies. Res Sch. 2006;13(1):29 Available from: http://www.ncbi.nlm.nih.gov/pubmed/20098638%0A http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC2809982 .
Bauer J. Personality factors, self-care, and perceived stress levels on counselor education and counseling psychology doctoral students. Dissertations: Western Michigan University; 2016.
Begun AL, Carter JR. Career Implications of Doctoral Social Work Student Debt Load. J Soc Work Educ. 2017;53(2):161–73. Available from. https://doi.org/10.1080/10437797.2016.1243500 .
Benjamin S, Williams J, Maher MA. Focusing the lens to share the story: using photographs and interviews to explore doctoral students’ sense of well-being. Int J Dr Stud. 2017;12:197–217.
Benesek JP. Stress and coping among psychology doctoral students: a comparison of self-reported stress levels and coping styles of PhD and PsyD students: University of Hartford; 1998.
Bireda AD. Challenges to the doctoral journey: a case of female doctoral students from Ethiopia. Open Prax. 2015;7(4):287–97.
Bolliger DU, Halupa C. Student perceptions of satisfaction and anxiety in an online doctoral program. Distance Educ. 2012;33(1):81–98.
Cole LJ. Academic worry and frequent mental distress among online doctoral students: Walden University; 2008.
Devine K, Hunter KH. PhD student emotional exhaustion: the role of supportive supervision and self-presentation behaviours. Innov Educ Teach Int. 2017;54(4):335–44.
Drake KL. Psychology graduate student well-being: the relationship between stress, coping, and health outcomes: University of Cincinnati; 2010.
Dumitrescu GA. Self-efficacy, locus of control , perceived stress and student satisfaction as correlates of dissertation completion: Andrews University; 2016.
El-Ghoroury NH, Galper DI, Sawaqdeh A, Bufka LF. Stress, coping, and barriers to wellness among psychology graduate students. Train Educ Prof Psychol. 2012;6(2):122–34.
Haynes C, Bulosan M, Citty J, Grant-Harris M, Hudson J, Koro-Ljungberg M. My world is not my doctoral program…Or is it?: Female students’ perceptions of well-being. Int J Dr Stud. 2012;7:001–17.
Hill LM. Perceived stress, academic support, social support, and professional support factors as predictors of student success in distributed-learning doctoral education: Fielding Graduate University; 2010.
Holahan CK. Stress experienced by women doctoral students, need for support, and occupational sex typing: An interactional view. Sex Roles. 1979;5(4):425–36.
Hunter KH, Devine K. Doctoral students’ emotional exhaustion and intentions to leave academia. Int J Doctoral Stud. 2016;11.
Kaufman JA. Stress and social support among online doctoral psychology students. J College Stud Psychother. 2006;20(3):79–88 Available from: http://search.proquest.com/docview/57185202?accountid=12253%5Cn http://man-fe.hosted.exlibrisgroup.com/openurl/44MAN/44MAN_services_page?url_ver=Z39.88-2004&rft_val_fmt=journal&genre=unknown&sid=ProQ:ProQ%3Aeducation&atitle=Stress+and+Social+Support+among +.
Levecque K, Anseel F, De Beuckelaer A, Van Der Heyden J, Gisle L. Work organization and mental health problems in PhD students. Res Policy. 2017;46:868–79.
Lonka K, Chow A, Keskinen J, Hakkarainen K, Sandström N, Pyhältö K. How to measure PhD students’ conceptions of academic writing - and are they related to wellbeing? J Writ Res. 2014;5(3):245–69.
Lowe RL. The relationship between personality, self-care, stress, and perceived wellness in psychology doctoral students: Tennessee University; 2015.
Marais GAB, Shankland R, Haag P, Fiault R, Juniper B. A survey and a positive psychology intervention on French PhD student well-being. Int J Dr Stud. 2018;13:109–38.
Martinez E, Ordu C, Sala MRD, McFarlane A. Striving to obtain a school-work-life balance: The full-time doctoral student. Int J Dr Stud. 2013;8:39–59.
McGregor BA, Antoni MH, Ceballos R, communication BBBS. very low CD19+ B-lymphocyte percentage is associated with high levels of academic stress among healthy graduate students. Stress Heal. 2008;24(5):413–8.
Nelson K. Academic progress in doctoral students: Levels of hope, subjective well-being, and stress: Walden University; 2014. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc12&NEWS=N&AN=2015-99151-189 .
Nottingham K. A predictive analysis of the psychosocial outcomes of doctoral students: Capella University; 2017.
Orozco AB. Self-care effects on anxiety in doctoral students: Fielding Graduate University; 2014. p. 35–61.
Peters BM. The relationships among physiological and perceived stress, quality of life, self-care and impairment in doctoral students: State University of New York at Buffalo; 2007.
Pifer MJ, Baker VL. “It could be just because I’m different”: Otherness and its outcomes in doctoral education. J Divers High Educ. 2014;7(1):14–30.
Platt J, Schaefer C. Clinical psychological students’ subjective stress ratings during their doctoral training. Psychol Rep. 1995;76:994 Available from: http://www.ncbi.nlm.nih.gov/pubmed/7568619 .
Pychyl TA. Personal projects, subjective well-being and the lives of doctoral students. Ottawa: Carleton University; 1995.
Pychyl TA, Little BR. Dimensional specificity in the prediction of subjective well-being: Personal projects in pursuit of the PhD. Soc Indic Res. 1998;45(1–3):423–73 Available from: file://d/d/Texte/Guenter/Literatu/Original/Journals/SIR98-45-423-473.pdf.
Rocha-Singh IA. Perceived stress among graduate students: development and validation of the Graduate Stress Inventory. Educ Psychol Meas. 1994;54(3):714–27.
Scheidler JA. Effects of perceived stress and perceived social support on marital satisfaction in doctoral students: Walden University. 2008;20.
Sekas G, Wile MZ. Stress-related illnesses and sources of stress: comparing M.D., Ph.D., M.D. and Ph.D. students. J Med Educ. 1980;55:440–6 Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L10000589%5Cn http://sfx.library.uu.nl/utrecht?sid=EMBASE&issn=00222577&id=doi:&atitle=Stress-related+illnesses+and+sources+of+stress%3A+comparing+M.D.-Ph.D.%2C+M.D.+and+Ph.D.+student .
Stubb J, Pyhältö K, Lonka K. Balancing between inspiration and exhaustion: PhD students’ experienced socio-psychological well-being. Stud Contin Educ. 2011;33(1):33–50.
Stubb J, Pyhältö K, Lonka K. The experienced meaning of working with a PhD thesis. Scand J Educ Res. 2012;56(4):439–56.
Ülkü-Steiner B, Kurtz-Costes B, Kinlaw CR. Doctoral student experiences in gender-balanced and male-dominated graduate programs. J Educ Psychol. 2000;92(2):296–307.
Volkert D, Candela L, Bernacki M. Student motivation, stressors, and intent to leave nursing doctoral study: a national study using path analysis. Nurse Educ Today. 2018;61:210–5. Available from. https://doi.org/10.1016/j.nedt.2017.11.033 .
Article PubMed Google Scholar
Waaijer CJF, Heyer A, Kuli S. Effects of appointment types on the availability of research infrastructure, work pressure, stress, and career attitudes of PhD candidates of a Dutch university. Res Eval. 2016;25(4):349–57.
Wang C-H, Chen Y-W, Wu T-Y. Self-guided bibliotherapy: a case study of a Taiwanese doctoral student. Int J Humanties. 2010;8(1):413–22.
Williams MD. HBCU vs. PWI: institutional integration at PWIs and Black doctoral student depression, anxiety, and stress: University of Minnesota; 2014.
Wright T. Issues in brief counselling with postgraduate research students. Couns Psychol Q. 2006;19(4):357–72.
Scrubb MM. An examination of the Doctoral Student Stress Survey (DSSS) as an instrument for measuring the effects of stress as perceived by doctoral students in a distance learning university, vol. 58: Walden University; 1998. p. 3041. Dissertation Abstracts International Section A: Humanities and Social Sciences. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc3&NEWS=N&AN=1998-95003-070 .
Hadden BW, Smith CV. I gotta say, today was a good (and meaningful) day: daily meaning in life as a potential basic psychological need. J Happiness Stud. 2017:1–18.
Butler G. Definitions of stress. Occas Pap R Coll Gen Pract. 1993;(61):1–5 Available from: http://www.ncbi.nlm.nih.gov/pubmed/8199583%0A http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC2560943 .
Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York: Springer Publishing Company; 1984.
Siegrist J. Chronic psychosocial stress at work and risk of depression: evidence from prospective studies. Eur Arch Psychiatry Clin Neurosci. 2008;258(SUPPL. 5):115–9.
Marin MF, Lord C, Andrews J, Juster RP, Sindi S, Arsenault-Lapierre G, et al. Chronic stress, cognitive functioning and mental health. Neurobiol Learn Mem. 2011;96(4):583–95. Available from. https://doi.org/10.1016/j.nlm.2011.02.016 .
Ward M. The gender salary gap in British academia. Appl Econ. 2001;33(13):1669–81. Cited 2019 May 23. Available from. https://doi.org/10.1080/00036840010014445 .
Howe-Walsh L, Turnbull S. Barriers to women leaders in academia: tales from science and technology. Stud High Educ. 2016;41(3):415–28. Cited 2019 May 23. Available from. https://doi.org/10.1080/03075079.2014.929102 .
Gardiner M, Tiggemann M. Gender differences in leadership style, job stress and mental health in male- and female-dominated industries. J Occup Organ Psychol. 1999;72(3):301–15.
Mackenzie CS, Gekoski WL, Knox VJ. Age, gender, and the underutilization of mental health services: the influence of help-seeking attitudes. Aging Ment Health. 2006;10(6):574–82 Cited 2017 May 12. Available from: http://www.tandfonline.com/action/journalInformation?journalCode=camh20 .
Seedat S, Scott KM, Sampson NA, Williams D, Kessler RC. Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys. Arch Gen Pschiatry. 2013;66(7):785–95.
Maslow AH. A theory of human motivation. Psychol Rev. 1943;50(4):370–96 Available from: http://content.apa.org/journals/rev/50/4/370 . Cited 2019 Jun 10.
Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–71 Available from: https://doi.org/10.1016/j.puhe.2017.07.035 .
Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality. Perspect Psychol Sci. 2015;10(2):227–37. Available from. https://doi.org/10.1177/1745691614568352 .
Viswesvaran C, Sanchez JI, Fisher J. The role of social support in the process of work stress: a meta-analysis. J Vocat Behav. 1999;54(2):314–34.
Michie S, Williams S. Reducing work related psychological ill health and sickness absence: a systematic literature review. Occup Environ Med. 2003;60(1):3–9.
CAS PubMed PubMed Central Google Scholar
Brook AT, Garcia J, Fleming M. The effects of multiple identities on psychological well-being. Personal Soc Psychol Bull. 2008;34(12):1588–600.
Thoits PA. Self, Identity, Stress, and Mental Health. In: Aneshensel CS, Phelan JC, Bierman A, editors. Handbook of the Sociology of Mental Health. Dordrecht: Springer; 2012. p. 357–77.
Haslam C, Jetten J, Cruwys T, Dingle G, Haslam A. The new psychology of health: Unlocking the social cure. New York: Routledge; 2018.
Faragher EB, Cass M, Cooper CL. The relationship between job satisfaction and health: a meta-analysis. Occup Environ Med. 2005;62(2):105–12.
Macfarlane B. Student performativity in higher education: converting learning as a private space into a public performance. High Educ Res Dev. 2015;34(2):338–50.
Daniels K. Perceived risk from occupational stress: a survey of 15 European countries. Occup Environ Med. 2004;61(5):467–70.
American Psychiatric Association (APA). Stress in America: missing the health care connection. Washington: American Psychiatric Association (APA). 2013.
Twenge JM. Time period and birth cohort differences in depressive symptoms in the U.S., 1982–2013. Soc Indic Res. 2015;121(2):437–54.
Download references
Acknowledgements
Thank you to the Office for Students for their funding to support this work; and thank you to the University of Sussex Doctoral school and our steering group for championing and guiding the ‘Understanding the mental health of Doctoral Researchers (U-DOC)’ project.
The present project was supported by the Office for Students Catalyst Award. The funder had no involvement in the design of the study, the collection, analysis or interpretation of the data, nor the writing of this manuscript.
Author information
Authors and affiliations.
School of Social Sciences, University of Westminster, 115 New Cavendish Street, London, W1W 6UW, UK
Cassie M. Hazell
School of Psychology, University of Sussex, Falmer, Brighton, BN1 9QJ, UK
Laura Chapman
Research and Enterprise, University of Sussex, Falmer, Brighton, BN1 9RH, UK
Sophie F. Valeix
Centre for Higher Education and Equity Research, University of Sussex, Falmer, Brighton, BN1 9RH, UK
Paul Roberts
School of Life Sciences, University of Sussex, Falmer, Brighton, BN1 9QG, UK
Jeremy E. Niven
Primary Care and Public Health, Brighton and Sussex Medical School and School of Psychology, University of Sussex, Falmer, Brighton, BN1 9PH, UK
You can also search for this author in PubMed Google Scholar
Contributions
CH contributed to the conceptualisation, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, supervision, validation, visualisation, writing—original draft preparation and writing—review and editing of this paper. LC contributed to the data curation, investigation, project administration, validation and writing—review and editing of this paper. SV contributed to the data curation, formal analysis, investigation, project administration, validation and writing—review and editing of this paper. PR contributed to the funding acquisition, project administration, supervision and writing—review and editing of this paper. JN contributed to the conceptualisation, funding acquisition, methodology, project administration, supervision, validation, writing—original draft preparation and writing—review and editing of this paper. CB contributed to the conceptualisation, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, supervision, validation, visualisation, writing—original draft preparation and writing—review and editing of this paper. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Clio Berry .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was not needed for the present study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hazell, C.M., Chapman, L., Valeix, S.F. et al. Understanding the mental health of doctoral researchers: a mixed methods systematic review with meta-analysis and meta-synthesis. Syst Rev 9 , 197 (2020). https://doi.org/10.1186/s13643-020-01443-1
Download citation
Received : 15 June 2020
Accepted : 31 July 2020
Published : 26 August 2020
DOI : https://doi.org/10.1186/s13643-020-01443-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- PhD students
- doctoral researchers
- Postgraduate researchers
- Systematic review
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Sustainability
- Latest News
- News Reports
- Documentaries & Shows
- TV Schedule
- CNA938 Live
- Radio Schedule
- Singapore Parliament
- Mental Health
- Interactives
- Entertainment
- Style & Beauty
- Experiences
- Remarkable Living
- Send us a news tip
- Events & Partnerships
- Business Blueprint
- Health Matters
- The Asian Traveller
Trending Topics
Follow our news, recent searches, commentary: phd students suffer academia's notorious culture of overwork and underappreciation, advertisement.
There is a mental health crisis brewing among PhD researchers, with the culture of wearing their suffering as a badge of honour fuelling the problem, says a social sciences lecturer.
(Photo: iStock/PonyWang)
Cassie M Hazell
LONDON: PhD students are the future of research, innovation and teaching at universities and beyond – but this future is at risk.
There are already indications from previous research that there is a mental health crisis brewing among PhD researchers.
My colleagues and I studied the mental health of PhD researchers in the UK and discovered that, compared with working professionals, PhD students were more likely to meet the criteria for clinical levels of depression and anxiety.
They were also more likely to have significantly more severe symptoms than the working-professional control group.
MORE THAN FOUR IN 10 MEET CRITERIA FOR DEPRESSION OR ANXIETY
We surveyed 3,352 PhD students, as well as 1,256 working professionals who served as a matched comparison group. We used the questionnaires used by NHS mental health services to assess several mental health symptoms.
More than 40 per cent of PhD students met the criteria for moderate to severe depression or anxiety. In contrast, 32 per cent of working professionals met these criteria for depression, and 26 per cent for anxiety.
The groups reported an equally high risk of suicide. Between 33 per cent and 35 per cent of both PhD students and working professionals met the criteria for “suicide risk”.

Commentary: Concerns over giving people ideas undermine needed conversations on suicide

Commentary: Decriminalising attempted suicide in Singapore does not mean less help for vulnerable people

Commentary: Working together towards a zero-suicide Singapore
The figures for suicide risk might be so high because of the high rates of depression found in our sample.
We also asked PhD students what they thought about their own and their peers’ mental health. More than 40 per cent of PhD students believed that experiencing a mental health problem during your PhD is the norm.
A similar number (41 per cent) told us that most of their PhD colleagues had mental health problems.
Just over a third of PhD students had considered ending their studies altogether for mental health reasons.
There is clearly a high prevalence of mental health problems among PhD students, beyond those rates seen in the general public.
A CULTURE OF OVERWORK
Our results indicate a problem with the current system of PhD study – or perhaps with academia more widely. Academia notoriously encourages a culture of overwork and under-appreciation.

This mindset is present among PhD students. In our focus groups and surveys for other research, PhD students reported wearing their suffering as a badge of honour and a marker that they are working hard enough rather than too much. One student told us:
“There is a common belief … you have to suffer for the sake of your PhD, if you aren’t anxious or suffering from impostor syndrome, then you aren’t doing it "properly”.
We explored the potential risk factors that could lead to poor mental health among PhD students and the things that could protect their mental health.
Financial insecurity was one risk factor. Not all researchers receive funding to cover their course and personal expenses, and once their PhD is complete, there is no guarantee of a job.
The number of people studying for a PhD is increasing without an equivalent increase in postdoctoral positions.
Another risk factor was conflict in their relationship with their academic supervisor. An analogy offered by one of our PhD student collaborators likened the academic supervisor to a “sword” that you can use to defeat the “PhD monster”.
If your weapon is ineffective, then it makes tackling the monster a difficult – if not impossible – task. Supervisor difficulties can take many forms. These can include a supervisor being inaccessible, overly critical or lacking expertise.


Commentary: Can mental health apps replace face-to-face therapy?

Commentary: Mental health generally declined during COVID-19, but some with depression fared better

Commentary: Focus on parents to fight mental health issues among young
A lack of interests or relationships outside PhD study, or the presence of stressors in students’ personal lives were also risk factors.
We have also found an association between poor mental health and high levels of perfectionism, impostor syndrome (feeling like you don’t belong or deserve to be studying for your PhD) and the sense of being isolated.
BETTER CONVERSATIONS NEEDED
Doctoral research is not all doom and gloom. There are many students who find studying for a PhD to be both enjoyable and fulfilling, and there are many examples of cooperative and nurturing research environments across academia.
Studying for a PhD is an opportunity for researchers to spend several years learning and exploring a topic they are passionate about.
It is a training programme intended to equip students with the skills and expertise to further the world’s knowledge. These examples of good practice provide opportunities for us to learn about what works well and disseminate them more widely.
The wellbeing and mental health of PhD students is a subject that we must continue to talk about and reflect on. However, these conversations need to happen in a way that considers the evidence, offers balance, and avoids perpetuating unhelpful myths.
Is this generation of youth 'weaker' when it comes to mental health? IMH CEO Dr Daniel Fung and SUSS peer support group president Daryl Soh discuss on CNA's Heart of the Matter:
Indeed, in our own study, we found that the percentage of PhD students who believed their peers had mental health problems and that poor mental health was the norm, exceeded the rates of students who actually met diagnostic criteria for a common mental health problem.
That is, PhD students may be overestimating the already high number of their peers who experienced mental health problems.
We therefore need to be careful about the messages we put out on this topic, as we may inadvertently make the situation worse.
If messages are too negative, we may add to the myth that all PhD students experience mental health problems and help maintain the toxicity of academic culture.
Cassie M Hazell is a Lecturer in Social Sciences at the University of Westminster. This commentary first appeared in The Conversation.

Commentary: Stress can make you stronger if you learn to identify when extra attention is needed

Commentary: Despite flexible work arrangements, work stress has worsened

Commentary: High stress levels a silent culprit behind diabetes
Related topics, also worth reading, this browser is no longer supported.
We know it's a hassle to switch browsers but we want your experience with CNA to be fast, secure and the best it can possibly be.
To continue, upgrade to a supported browser or, for the finest experience, download the mobile app.
Upgraded but still having issues? Contact us
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- CBE Life Sci Educ
- v.20(3); Fall 2021
PhDepression: Examining How Graduate Research and Teaching Affect Depression in Life Sciences PhD Students
Logan e. gin.
† Research for Inclusive STEM Education Center, School of Life Sciences, Arizona State University, Tempe, AZ 85281
Nicholas J. Wiesenthal
§ Department of Biology, University of Central Florida, Orlando, FL 32816
Katelyn M. Cooper
Graduate students are more than six times as likely to experience depression compared with the general population. However, few studies have examined how graduate school specifically affects depression. In this qualitative interview study of 50 life sciences PhD students from 28 institutions, we examined how research and teaching affect depression in PhD students and how depression in turn affects students’ experiences teaching and researching. Using inductive coding, we identified factors that either positively or negatively affected student depression. Graduate students more commonly mentioned factors related to research that negatively affected their depression and factors related to teaching that positively affected their depression. We identified four overarching aspects of graduate school that influenced student depression: the amount of structure in teaching and research, positive and negative reinforcement, success and failure, and social support and isolation. Graduate students reported that depression had an exclusively negative effect on their research, primarily hindering their motivation and self-confidence, but that it helped them to be more compassionate teachers. This work pinpoints specific aspects of graduate school that PhD programs can target to improve mental health among life sciences graduate students.
INTRODUCTION
In 2018, researchers found that graduate students were more than six times as likely to report experiencing depression and anxiety compared with the general population and subsequently declared a “graduate student mental health crisis” ( Evans et al. , 2018 ; Flaherty, 2018 ). Calls to identify which factors exacerbate graduate student mental health problems followed (“The Mental Health of PhD Researchers,” 2019; Woolston, 2019a ). However, few studies have taken an inductive approach to identifying what aspects of graduate school in particular affect student mental health. More commonly, large quantitative studies propose a limited number of factors that may affect student mental health that participants select from, few of which directly relate to graduate research or teaching ( Peluso et al. , 2011 ; Levecque et al. , 2017 ; Evans et al. , 2018 ; Liu et al. , 2019 ). In this interview study, we focus on depression in life sciences PhD students and examine which specific aspects of research and teaching graduate students report as affecting their depression. We also explore how depression affects students’ experiences in graduate school.
The American Psychiatric Association defines depression as a common and serious medical illness that negatively affects how one feels, the way one thinks, and how one acts ( American Psychiatric Association, 2020 ). Depression is characterized by nine symptoms: depressed mood; markedly diminished interest or pleasure in activities; reduced ability to think or concentrate, or indecisiveness; feelings of worthlessness, or excessive or inappropriate guilt; recurrent thoughts of death or suicidal ideation, or suicide attempts or plans; insomnia or hypersomnia; significant change in appetite or weight; psychomotor agitation or retardation; and fatigue or loss of energy ( American Psychiatric Association, 2013 ; Schmidt and Tolentino, 2018 ). For depression to be diagnosed, the presence of at least five of the symptoms is required most of the day, nearly every day, for at least 2 weeks in addition to the occurrence of either depressed mood or diminished interest or pleasure ( American Psychiatric Association, 2013 ). In the general U.S. population, depression affects approximately 6.7% of individuals and is estimated to affect 16.6% of individuals at some point in their lifetime.
Graduate students are far more likely to report experiencing depression compared with the general population ( Evans et al. , 2018 ; Barreira et al. , 2020 ). Specifically, a recent study of master’s and PhD students in programs across the world, spanning a variety of disciplines, found that 39% of graduate students reported having moderate to severe depression ( Evans et al. , 2018 ). Similar studies have demonstrated high rates of depression in graduate students in specific disciplines such as economics ( Barreira et al. , 2020 ), biochemistry ( Helmers et al. , 1997 ), pharmacology ( Helmers et al. , 1997 ), and physiology ( Helmers et al. , 1997 ). Depression rates have surged in recent years among graduate students ( American College Health Association, 2014 , 2019 ). Talking about depression has become more socially acceptable, particularly among younger adults ( Anxiety and Depression Association of America, 2015 ; Lipson et al. , 2019 ), which may have contributed to the number of students willing to reveal that they are struggling with mental health. Additionally, depression is highly related to burnout, defined as a work-related chronic stress syndrome involving emotional exhaustion, depersonalization, and reduced personal accomplishment ( Maslach et al. , 2001 ; Bianchi et al. , 2014 ). Graduate work environments appear to be increasingly characterized as stressful and demanding ( American College Health Association, 2014 , 2019 ; Woolston, 2017 ), which may also be contributing to the increase in graduate depression rates.
Increasingly, scientists, psychologists, and education researchers are recognizing graduate student mental health as a concern and calling for further investigation of graduate student mental health in hopes of identifying interventions to improve graduate student quality of life (“The Mental Health of PhD Researchers,” 2019; Woolston, 2019a , b ). For example, in 2019, Nature added a question to its annual survey of PhD students asking students from around the world whether they had sought help for anxiety or depression, and more than one-third (36%) confirmed they had ( Woolston, 2019b ). Additionally, notable publication outlets such as Nature (“The Mental Health of PhD Researchers,” 2019), Scientific American ( Puri, 2019 ), and Science ( Pain, 2018 ) have published blogs or editorials spotlighting the need to improve graduate student mental health.
Some recent studies have sought to uncover the factors affecting depression in graduate students. Primarily, survey studies with predetermined factors that researchers hypothesized impact student mental health have identified poor mentor–mentee relationships ( Peluso et al. , 2011 ; Evans et al. , 2018 ; Hish et al. , 2019 ; Liu et al. , 2019 ; Charles et al. , 2021 ), financial stress ( Hish et al. , 2019 ; Jones-White et al. , 2020 ; Charles et al. , 2021 ), and lack of work–life balance ( Evans et al. , 2018 ; Liu et al. , 2019 ) to be associated with depression or depressive symptoms among graduate students in various disciplines. Other variables shown to be predictive of depression include low research self-efficacy, defined as low confidence in one’s ability to do research ( Liu et al. , 2019 ), difficulty publishing papers ( Liu et al. , 2019 ), hours worked per week ( Peluso et al. , 2011 ), and perceived institutional discrimination ( Charles et al. , 2021 ). Factors that appear to be protective of depressive symptoms include social support ( Charles et al. , 2021 ), mastery, defined as the extent to which individuals perceive themselves to be in control of the forces that impact their lives ( Hish et al. , 2019 ), positive departmental social climate ( Charles et al. , 2021 ), optimism about career prospects ( Charles et al. , 2021 ), and sense of belonging to one’s graduate program ( Jones-White et al. , 2020 ). While these studies have identified some depression-related factors associated with graduate school broadly and emphasize the importance of positive mentor–mentee relationships, few studies have explored factors specifically associated with research and teaching, the two activities that graduate students engage in most frequently during their time in a program. Additionally, the extant literature has primarily focused on surface causes of graduate student depression, yet understanding the underlying causes may be key to developing meaningful interventions. For example, while it is well established that student perception of poor mentorship is related to student depression ( Evans et al. , 2018 ; Hish et al. , 2019 ; Liu et al. , 2019 ; Charles et al. , 2021 ), it is less well understood what specific behaviors mentors exhibit and how such behaviors negatively affect the cognitive and behavioral underpinnings of graduate student depression. Without this knowledge, it is difficult to develop strategies to help mentors be more inclusive of students.
Theories of depression seek to explain the causes of depression. No theoretical model is widely accepted as an overarching framework for depression within the psychological and psychiatric communities ( Mcleod, 2015 ; Ramnerö et al. , 2016 ); instead, there are a number of models addressing how different aspects of depression are associated with the disorder. Arguably, the three most prominent models are cognitive ( Beck et al. , 1979 ), behavioral ( Martell et al. , 2001 ), and psychodynamic ( Busch et al. , 2016 ). In brief, cognitive theories focus on an individual’s beliefs and propose that changes in thinking precede depressive symptoms; for example, negative views of oneself, the world, and the future are thought to be common for individuals with depression ( Beck et al. , 1979 ; Leahy, 2002 ). Behavioral theories emphasize that depression is a result of one’s interaction with the environment; depressive symptoms are thought to be the result of decreased reward, lack of positive reinforcement, encouragement of depressive or passive behaviors, and discouragement of healthy behaviors ( Lewinsohn, 1974 ; Martell et al. , 2001 ; Carvalho et al. , 2011 ). Psychodynamic theories of depression consider the role of feelings and behaviors in the etiology and persistence of depressive symptoms; these theories often focus on 1) one’s biology and temperamental vulnerabilities, 2) earliest attachment relationships, and 3) childhood experiences associated with frustration, helplessness, loss, guilty, or loneliness ( Busch et al. , 2016 ). While each group of theories has been critiqued and no one theory fully explains one’s experience with depression ( Mcleod, 2015 ; Ramnerö et al. , 2016 ), we propose that each may be helpful in understanding how aspects of graduate school may affect depression among PhD students.
The thoughts and behaviors associated with depression may in turn affect students’ experiences in graduate school, particularly their experiences with research and teaching. While no studies have examined how depression explicitly affects graduate students’ research experiences, studies have identified ways in which depression can affect students’ experiences in undergraduate research ( Cooper et al. , 2020a , b ). Undergraduate researchers report that their depression negatively affected their motivation, ability to concentrate and remember, intellectual engagement, and creativity in research ( Cooper et al. , 2020b ). Undergraduates described that their depression also caused them to be overly self-critical, less social, and ultimately negatively affected their research productivity. Additionally, undergraduates have been reluctant to share their depression with others in the lab, because they fear that they will be judged ( Cooper et al. , 2020b ). While these studies provide some insight into how depression may affect graduate students’ experience in research, there is much less information about how depression may affect graduate teaching.
In this study, we interviewed 50 PhD students in the life sciences who self-identified with having depression with the intent of answering two research questions that address gaps in the literature: 1) What specific aspects of graduate research and teaching affect PhD student depression? 2) How does PhD students’ depression affect their experience in research and teaching?
Student Interviews
This study was done under an approved Arizona State University Institutional Review Board protocol (no. 00011040).
In Fall 2019, we surveyed graduate students by sending an email out to program administrators of all life sciences graduate programs in the United States that are listed in U.S. News & World Report (2019) . Of the 259 graduate programs that we contacted, 75 (29.0%) program administrators agreed to forward our survey to students enrolled in their graduate programs. Of the 840 graduate students who participated in the survey, 459 (54.6%) self-identified as having depression based on general demographic questions on the survey. Of the 459 students who identified as having depression, 327 (71.2%) agreed to be contacted for a follow-up interview. In Summer 2020, we sent a recruitment email out to the 327 students who identified as having depression, asking to interview them about their experiences with depression in a PhD program. We specifically did not require that students be diagnosed with depression in order to participate in the interview study. We did not want to bias our sample, as mental health care is disproportionately unavailable to Black and Latinx individuals, as well as to those who come from low socioeconomic backgrounds ( Howell and McFeeters, 2008 ; Kataoka et al. , 2002 ; Santiago et al. , 2013 ). Of the students who were contacted, 50 PhD students (15.3%) enrolled across 28 life sciences PhD programs completed an interview.
The interview script was based on a previous interview script that we had developed, which successfully elicited what aspects of research affect depression in undergraduates and how depression affects their research ( Cooper et al. , 2020a ). Our previous work has shown that research experiences do not exclusively worsen depression, but that aspects of research can also help students manage their depression ( Cooper et al. , 2020a ). As such, our interview questions explored what aspects of research helped students manage their depression (positively affecting depression), and what aspects worsened students’ depression (negatively affecting depression). Additionally, we hypothesized that other prominent aspects of graduate school, such as teaching, would also affect PhD student depression and revised the interview script to include questions focused on examining the relationship between depression and teaching. We asked students what aspects of graduate research and teaching made their depression worse and what aspects helped them manage their depression. Participants were invited to come up with as many aspects as possible. We also asked how students perceived their depression affected their research and teaching. With the knowledge that we would be conducting interviews during summer of 2020 in the midst of the COVID-19 pandemic, and that the pandemic had likely exacerbated graduate student depression ( Chirikov et al. , 2020 ), we directed students to not reference aspects of research and teaching that were uniquely related to the pandemic (e.g., teaching remotely or halted research) when discussing the relationship between research, teaching, and depression. We were specifically interested in aspects of teaching and research that affected student depression before the pandemic and would presumably affect student depression afterward. We conducted think-aloud interviews with four graduate students who identified as having depression to ensure that our questions would not offend anyone with depression and to establish cognitive validity of the interview script by ensuring that each student understood what each question was asking. The interview script was iteratively revised after each think-aloud interview ( Trenor et al. , 2011 ). A final copy of the interview script can be found in the Supplemental Material.
All interviews were conducted using Zoom by one of two researchers (L.E.G. or K.M.C.). The average interview time was about 45 minutes. After the interview, all participants were sent a short survey to collect their demographics and additional information about their depression (a copy of the survey can be found in the Supplemental Material). Participants were provided a small monetary gift card in exchange for their time. All interviews were deidentified and transcribed before analysis.
Interview Analysis
Three researchers (L.E.G., N.J.W., and K.M.C.) independently reviewed 12 of the same randomly selected interviews to explore each idea that a participant expressed and to identify recurring themes ( Charmaz, 2006 ). Each researcher took detailed analytic notes during the review. After, the three researchers met to discuss their notes and to identify an initial set of recurring themes that occurred throughout the interviews ( Saldaña, 2015 ). The authors created an initial codebook outlining each theme and the related description. Together, the authors then reviewed the same set of five additional interviews to validate the themes outlined in the codebook and to identify any themes that may have been missed during the initial review. The researchers used constant comparison methods to compare quotes from the interviews to each theme and to establish whether any quotes were different enough from a particular theme to warrant an additional code ( Glesne and Peshkin, 1992 ). Together, the three researchers revised the codebook until they were confident that it captured the most common themes and that no new themes were emerging. A final copy of the codebook can be found in the Supplemental Material. Two authors (L.E.G. and N.J.W.) used the final codebook to code five randomly selected interviews (10% of all interviews) and their Cohen’s κ interrater score was at an acceptable level (κ = 0.94; Landis and Koch, 1977 ). Then, one researcher (N.J.W.) coded the remaining 45 interviews. In the text, we present themes mentioned by at least 10% of interviewees and use quotes to highlight themes. Some quotes were lightly edited for clarity.
Author Positionality
Some of the authors identify as having depression and some do not. One author had completed a PhD program (K.M.C.), one author was in the process of completing a PhD program (L.E.G.), and two authors were undergraduates (N.J.W. and I.F.) at the time when the interviews and analyses took place.
Interview Participants
Fifty PhD students agreed to participate in the study. Students were primarily women (58%), white (74%), and continuing-generation college students (78%). Twelve percent of students were international students, and the average age of the participants was 28 years old. While 20% of students were unsure of their career goals, 32% of students planned to pursue a career in academia, and 24% were planning to pursue a career in industry. Students reported how severe they perceived their depression to be, on average, during the time they had spent in their PhD programs. Most students reported their depression as either moderate (50%) or severe (28%). Eighty percent of students reported being diagnosed with depression, and 74% reported receiving treatment for depression. Participants were at different stages in their PhD programs ranging from first year to sixth year or more. Three students had graduated between the time they completed the initial survey and when they participated in the interview in Summer 2020. Students self-reported their main research areas and represented a broad range, with ecology and evolutionary biology (26%), animal science (14%), molecular biology (14%), and neurobiology (10%) being the most common. Eighty-six percent of students had experience teaching undergraduates, primarily as teaching assistants (TAs), at the time of the interviews. All student demographics are summarized in Table 1 .
Participant demographics
The Effect of Research on Graduate Student Depression
Students more commonly identified ways that research negatively affected their depression than ways research positively affected their depression. Considering all factors that students listed and not just those that were most common, students on average listed two ways in which an aspect of research negatively affected their depression and one way in which an aspect of research positively affected their depression.
The most commonly reported aspect of research that worsened students’ depression was experiencing failures, obstacles, or setbacks in research. Specifically, students cited that failed experiments, failed research projects, and the rejection of manuscripts and grants was particularly difficult for their depression. Conversely, students highlighted that their depression was positively affected when they were able to make substantial progress on their research projects; for example, if they wrote part of a manuscript or if an experiment worked. Students also explained that accomplishing smaller or mundane research tasks was helpful for their depression, both because they felt as though they were checking off a box and also because it allowed them to focus on something other than the negative thoughts often associated with depression.
Students also highlighted that the unstructured nature of graduate research worsened their depression. Specifically, students described that, in graduate research, there are often no clear directions, sets of guidelines, or deadlines to help structure their day-to-day activities. Without this structure, students need to rely on their own motivation to outline goals, accomplish tasks, or seek help, which participants described can be difficult when one is experiencing a depressive episode. However, students also felt as though the unstructured nature of research benefited their depression, because it allowed for flexibility. Those who did not have frequent deadlines or strict schedules were able to not conduct research on days when they needed to recover from a depressive episode or schedule research around therapy or other activities that had a positive impact on their depression. Finally, students highlighted that their passion for their research was protective against depression. Their love for the subject of their research or thinking about how their work may have a positive impact on others could positively affect their motivation or mood.
Students described that their relationships with others in the lab also affected their depression. Specifically, if their mentors or others in their lab had unreasonable or overwhelming expectations of them, it could make them feel as though they would never be able to meet such expectations. Research also provides an environment for students to constantly compare themselves with others, both those in supervisory roles as well as peers. Notably, when students mentioned comparing themselves with others, this comparison never made them feel good about themselves, but was exclusively detrimental to their depression; they felt as though they would never be able to accomplish what others had already accomplished. Students’ relationships with their mentors also seemed to have a notable impact on their depression. Having a positive relationship with their mentors or a mentor who provided psychosocial support positively affected their depression, whereas perceiving a negative relationship with their mentors, particularly a mentor who provided consistently harsh or negative feedback, was detrimental. Students who had absent mentors or mentors who provided infrequent technical support and guidance also felt as though this situation worsened their depression, because it prevented or prolonged their success in research. Finally, students highlighted that conducting graduate research can be isolating, because you are often working on something different from those in the lab or because those outside graduate school cannot relate to the stress and struggles associated with research. However, in instances in which students were able to collaborate with others, this could be protective against depression, because it gave students a sense of comradery or validated their feelings about specific aspects of research. The most common research-related factors that students reported negatively and positively affected their depression and example student quotes of each factor are reported in Tables 2 and and3, 3 , respectively.
Research-related factors that PhD students reported negatively affected their depression
Research-related factors that PhD students reported positively affected their depression
The Effect of Teaching on Graduate Student Depression
We asked all graduate students who had teaching experience ( n = 43) how teaching affected their depression. Graduate students more commonly identified ways that teaching positively affected their depression than ways teaching negatively affected their depression. On average, considering all factors that graduate students listed and not just those that were most common, participants listed two ways in which teaching positively affected their depression and one way in which teaching negatively affected their depression.
Graduate students most commonly highlighted that teaching provided positive reinforcement from undergraduates, which helped them manage their depression. This positive reinforcement came in multiple forms ranging from formal teaching evaluations to positive verbal comments from undergraduates about how good a graduate student was at teaching to watching undergraduates accomplish academic goals or grasp complex concepts. A subset of graduate students highlighted that teaching was good for their depression, because it was something they were passionate about or that they genuinely enjoyed. As such, it was a source of happiness, as was being able to collaborate and form friendships with other TAs or instructors. Some graduate students also acknowledged that they felt confident teaching, often because they had mastered content that undergraduates had not. However, this was not always the case; some graduate students highlighted that a lack of teaching training and preparation negatively affected their self-efficacy as instructors, which in turn exacerbated their depression. This was further exacerbated by the pressure that graduate students put on themselves to perform well as instructors. The potential to have a negative impact on undergraduates and their learning experiences could worsen students’ depression by increasing the stress surrounding their performance as a teacher. Additionally, some graduate students received negative reinforcement from undergraduates, in the form of negative comments on formal teaching evaluations or disrespectful behavior from undergraduates such as groans or eye rolls, which graduate students explained negatively affected their self-efficacy, further worsening their depression.
Students also highlighted that teaching could negatively affect their depression because it interfered with the time they felt they needed to be spending on research or added to the large number of responsibilities they had as graduate students. However, some students welcomed time away from research; teaching sometimes served as a distraction from research-related stressors. Students also highlighted that teaching is structured, which positively affected their depression. That is, there are concrete tasks, such as grading, that need to be accomplished or places that the graduate student needs to be during a specific time. This structure helped motivate them to accomplish teaching goals, even if they were feeling a lack of motivation because of their depression. The most common teaching-related factors that graduate students reported negatively and positively affected their depression and example student quotes for each factor are reported in Tables 4 and and5, 5 , respectively.
Teaching-related factors that PhD students reported negatively affected their depression
a Forty-three out of the 50 students who participated in the study had experience teaching undergraduates either as a TA or as an instructor of record. We only considered the responses from the TAs with teaching experiences when calculating the percent of students who reported each factor.
Teaching-related factors that PhD students reported positively affected their depression
The Effect of Depression on Graduate Research
In the interviews, we asked graduate students how their depression affected their graduate research, if at all. They identified three primary ways in which depression could affect research, all of which were negative. The most common way depression affected research was interfering with students’ motivation, which in turn affected their productivity. Students described that their productivity was affected immediately, for example, struggling to execute daily tasks like collecting or analyzing data. However, graduate students described that their lack of motivation ultimately resulted in larger consequences, such as delays in getting papers submitted and published. In fact, some graduate students explicitly stated that they felt as though they would have been able to graduate earlier if they had not had depression. The second way in which depression affected graduate students’ research is that it interfered with their ability to focus or concentrate. Students primarily explained that the lack of focus did not delay their research but caused their research to be less enjoyable or made them frustrated because they had to expend additional mental energy to execute tasks. Depression also caused students to be less confident or overly critical of themselves. Specifically, if an experiment did not go right or they experienced rejection of a manuscript, they tended to internalize it and blame themselves. This lack of confidence often inhibited students’ abilities to make decisions about research or take risks in research. They described frequently second-guessing themselves, which made decisions and taking risks in research more difficult. The most common ways students reported that their depression affected their research and example student quotes are reported in Table 6 .
Self-reported ways that depression affected PhD students’ research or the student as a researcher
The Effect of Depression on Teaching
Graduate students described one positive way and two negative ways that depression affected their teaching. Students explained that, because they had experienced depression, they were more compassionate and empathetic toward the undergraduates in their courses. Specifically, they felt they could better understand some of the struggles that undergraduates experience and were sometimes more likely to be flexible or lenient about course requirements and deadlines if an undergraduate was struggling. However, graduate students reported that depression also negatively affected their teaching. Specifically, depression could cause graduate students to feel disconnected or disengaged from undergraduates. It could also cause graduate students to feel as though they had a lack of energy or felt down when teaching. The common self-reported ways that depression affected PhD students’ teaching and example quotes are reported in Table 7 .
Self-reported ways that depression affected PhD students’ teaching or the graduate student as an instructor
a Forty-three out of the 50 students who participated in the study had experience teaching undergraduates either as a TA or as an instructor of record. We only considered the responses from the TAs with teaching experiences when calculating the percent of students who reported each theme.
Despite the increasing concern about graduate student mental health among those in the scientific community ( Pain, 2018 ; “The Mental Health of PhD Researchers,” 2019; Puri, 2019 ), there is a lack of information about how specific aspects of science PhD programs affect students with depression. This is the first study to explicitly investigate which particular aspects of research and teaching affect depression among life sciences PhD students and how depression, in turn, affects graduate students’ experiences in research and teaching. Overall, graduate students highlighted factors related to teaching and research that both alleviated and exacerbated their symptoms of depression. Graduate students more commonly brought up ways that research negatively affected their depression, than ways that it positively affected their depression. Conversely, graduate students more commonly mentioned ways that teaching had a positive effect on their depression compared with a negative effect. The requirement and opportunity to teach differs among life sciences graduate programs ( Schussler et al. , 2015 ; Shortlidge and Eddy, 2018 ). As such, future research should investigate whether the amount of teaching one engages in during graduate school is related to levels of graduate student depression. Despite differences in how teaching and research affect student depression, this study unveiled factors that protect against or worsen depressive symptoms. Specifically, four overarching factors affecting graduate student depression emerged from the interviews: 1) Structure; 2) Positive and Negative Reinforcement; 3) Failure and Success; 4) Social Support and Isolation. We discuss here how each of these factors may positively and negatively affect graduate student depression.
One stark contrast between research and teaching is the amount of structure in each activity. That is, students expressed that research goals are often amorphous, that there are not concrete instructions for what needs to be accomplished, and that there is often no set schedule for when particular tasks need to be accomplished. Conversely, with teaching, graduate students often knew what the goals were (e.g., to help students learn), exactly what they needed to accomplish each week (e.g., what to grade, what to teach), and when and where they needed to show up to teach (e.g., a class meets at a particular time). Graduate students highlighted that a lack of structure, particularly in research, was detrimental for their depression. Their depression often made it difficult for them to feel motivated when there was not a concrete task to accomplish. Major depression can interfere with executive function and cognition, making goal setting and goal achievement particularly difficult ( Elliott, 1998 ; Watkins and Brown, 2002 ). In fact, research has documented that individuals with depression generate less specific goals and less specific explanations for approaching a goal than individuals who do not have depression ( Dickson and Moberly, 2013 ). As such, it may be particularly helpful for students with depression when an activity is structured, relieving the student from the need to articulate specific goals and steps to achieve goals. Students noted that the lack of structure or the flexibility in research was helpful for their depression in one way: It allowed them to better treat their depression. Specifically, students highlighted that they were able to take time to go to therapy or to not go into the lab or to avoid stressful tasks, which may be important for successful recovery from a depressive episode ( Judd et al. , 2000 ).
Compared with conducting research, many participants reported that the concrete tasks associated with teaching undergraduates were helpful for their depression. This is supported by literature that illustrates that concrete thinking, as opposed to abstract thinking, can reduce difficulty making decisions in individuals with depression ( Dey et al. , 2018 ), presuming that teaching often requires more concrete thinking compared with research, which can be more abstract. Additionally, cognitive-behavioral treatments for depression have demonstrated that developing concrete goals for completing tasks is helpful for individuals with depression ( Detweiler-Bedell and Whisman, 2005 ), which aligns with graduate students’ perceptions that having concrete goals for completing teaching tasks was particularly helpful for their depression.
Positive and Negative Reinforcement
Graduate students reported that the negative reinforcement experienced in research and teaching had a significant negative effect on their depression, while the positive reinforcement students experienced only in teaching had a positive effect. Notably, students did not mention how positive reinforcement affected their depression in the context of research. Based on student interviews, we predict that this is not because they were unaffected by positive reinforcement in research, but because they experienced it so infrequently. Drawing from behavioral theories of depression, the concept of response-contingent positive reinforcement (RCPR; Lewinsohn, 1974 ; Kanter et al. , 2004 ) helps explain this finding. As summarized by Kanter and colleagues (2004) , RCPR describes someone seeking a response and being positively reinforced; for example, graduate students seeking feedback on their research are told that what they have accomplished is impressive. Infrequent RCPR may lead to cognitive symptoms of depression, such as low self-esteem or guilt, resulting in somatic symptoms of depression, such as fatigue and dysphoria ( Lewinsohn, 1974 ; Martell et al. , 2001 ; Manos et al. , 2010 ). RCPR is determined by three factors. 1) How many potential events may be positively reinforcing to an individual. For example, some people may find an undergraduate scoring highly on an exam in a class they are teaching to be reinforcing and others may find that they only feel reinforced when an undergraduate explicitly compliments their teaching. 2) The availability of reinforcing events in the environment. If graduate students’ mentors have the ability to provide them with RCPR but are never able to meet with them, these reinforcing events are unavailable to them. 3) The instrumental behavior of an individual. Does the individual exhibit the behavior required to obtain RCPR? If graduate students do not accomplish their research-related tasks on time, they may not receive RCPR from their mentor. If individuals are not positively reinforced for a particular behavior, they may stop exhibiting it, further exacerbating the depressive cycle ( Manos et al. , 2010 ). Therefore, the lack of positive reinforcement in research may be particularly damaging to graduate students, because it may discourage them from completing tasks, leading to additional depressive symptoms. Conversely, teaching presents many opportunities for positive reinforcement. Every time graduate students teach, they have the opportunity to receive positive reinforcement from their students or to witness a student’s academic accomplishment, such as an undergraduate expressing excitement when they understand a concept. As such, it is not surprising that positive reinforcement was the primary teaching-related factor that graduate students reported helped with their depression. Despite the positive reinforcement of teaching for graduate students with depression, we are not suggesting that graduate students should take on additional teaching loads or that teaching should be viewed as the sole respite for graduate students with depression. Overwhelming students with increased responsibilities may counteract any positive impact that teaching could have on students’ depression.
Failure and Success
Failure and success affected student depression, but only in the context of research; contrary to research, students rarely mentioned concrete metrics for success and failure in teaching. While graduate students highlighted receiving positive or negative reinforcement from undergraduates, they did not relate this to being a “successful” instructor. It is unsurprising that graduate students did not mention failing or succeeding at teaching, given that experts in teaching agree that it is difficult to objectively evaluate quality teaching ( d’Apollonia and Abrami, 1997 ; Kember et al. , 2002 ; Gormally et al. , 2014 ). In fact, the lack of teacher training and knowledge about how to teach effectively negatively affected student depression, because it could cause students to feel unprepared as an instructor. Integrating teacher training into graduate programs has been championed for decades ( Torvi, 1994 ; Tanner and Allen, 2006 ; Schussler et al. , 2015 ); however, the potential for such training to bolster graduate student mental health is new and should be considered in future research. With regard to graduate students’ research, the concept of success and failure was far more concrete; students mentioned failing in terms of failed experiments, research projects, and rejected manuscripts and grant proposals. Successes included accepted manuscripts, funded grant proposals, and concrete progress on significant tasks, such as writing or conducting an experiment that yielded usable data. Failure has been shown to negatively affect depression among undergraduate researchers ( Cooper et al. , 2020a ), who are hypothesized to be inadequately prepared to experience failure in science ( Henry et al. , 2019 ). However, it is less clear how well prepared graduate students are to experience failure ( Simpson and Maltese, 2017 ). Drawing from cognitive theories of depression, depression is associated with dysfunctional cognitive schemas or dysfunctional thinking that can lead individuals with depression to have negative thoughts about the world, themselves, and the future and to interpret information more negatively than is actually the case (called negative information-processing biases; Beck, 1967 ; Beck et al. , 1979 ; Gotlib and Krasnoperova, 1998 ; Maj et al. , 2020 ). Related to failure, individuals with dysfunctional cognitive schemas may harbor beliefs such as if something fails at work (or in graduate research), they are a failure as a person or that a small failure can be as detrimental as a larger failure ( Weissman, 1979 ; Miranda and Persons, 1988 ). As such, setbacks in research may be particularly difficult for PhD students with depression. Graduate students in our study also mentioned how failing in research was often out of their control, particularly failure related to experiments and research projects. The extent to which one feels they can control their environment is important for mental health, and lower estimates of control have been hypothesized to be an important factor for depression ( Grahek et al. , 2019 ). Therefore, this feeling of being unable to control success in research may further exacerbate student depression, but this would need to be tested. Importantly, these findings do not imply that individuals with depression are unable to cope with failure; they only suggest that individuals perceive that failure in science can exacerbate their depression.
Social Support and Isolation
Graduate students reported that feelings of isolation in research could worsen their depression. Specifically, they highlighted that it can be difficult for their mental health when their friends outside graduate school cannot relate to their struggles in research and when others in their research group are not working on similar projects. One study of more than 1400 graduate students at a single university found that feeling isolated from fellow graduate students and faculty positively predicted imposter phenomenon ( Cohen and McConnell, 2019 ), defined as the worry that they were fooling others about their abilities and that their fraudulence would be exposed ( Clance and Imes, 1978 ), which is positively correlated with depression among college students ( McGregor et al. , 2008 ). Developing a positive lab environment, where undergraduates, graduate students, and postgraduates develop positive relationships, has been shown to positively affect undergraduates ( Cooper et al. , 2019 ) and may also positively affect graduate students who experience such feelings of isolation. Graduate students in this study described that both teaching and research had the potential to be a source for relationship development and social support. Students who described positive collaborative relationships in research and teaching felt this had a positive impact on their depression, which aligns with a review of studies in psychiatry concluding that being connected to a large number of people and having individuals who are able to provide emotional support by listening or giving advice is protective against depression ( Santini et al. , 2015 ), as well as a study that found that social support is protective against depression, specifically among the graduate population ( Charles et al. , 2021 ).
These four factors provide clear targets for graduate programs looking to improve the experiences of students with depression. For example, increasing structure in research could be particularly helpful for graduate students with depression. Ensuring that students have concrete plans to accomplish each week may not only positively impact depression by increasing structure, but ultimately by increasing a student’s success in research. Research mentors can also emphasize the role of failure in science, helping students realize that failure is more common than they may perceive. Increasing opportunities for positive reinforcement in teaching and research may be another avenue to improving student mental health. Providing students with appropriate teacher training is a first step to enhancing their teaching skills and potential for positive reinforcement from undergraduate students ( Schussler et al. , 2015 ). Additionally, teaching evaluations, a common form of both positive and negative reinforcement, are known to be biased and disadvantage women, People of Color, and those with non–English speaking backgrounds ( Fan et al. , 2019 ; Chávez and Mitchell, 2020 ) and arguably should not be used to assess teaching. In research, mentors can make an effort to provide positive feedback or praise in meetings in addition to critiques. Finally, to provide social support to graduate students with depression, graduate programs could consider creating specific initiatives that are related to supporting the mental health of graduate students in their departments, such as a support group for students to meet and discuss their experiences in graduate school and how those experience pertain to their mental health.
Limitations and Directions for Future Research
In this study, we chose to only interview students with the identity of interest (depression), as is common with exploratory studies of individuals with underserved, underrepresented, or marginalized identities (e.g. Carlone and Johnson, 2007 ; Cooper and Brownell, 2016 ; Barnes et al. , 2017 , 2021 ; Downing et al. , 2020 ; Gin et al. , 2021 ; Pfeifer et al. , 2021 ). However, in future studies, it would be beneficial to also examine the experiences of individuals who do not have depression. This would provide information about the extent to which specific aspects of graduate research and teaching are disproportionately beneficial or challenging for students with depression. In this study, we did not explicitly examine whether there was a relationship between students’ identities and depression because of the small number of students in particular demographic groups. However, a theme that occurred rather infrequently (but is included in the Supplemental Material) is that discrimination or prejudice in the lab or academia could affect depression, which was reported exclusively by women and People of Color. As such, disaggregating whether gender and race/ethnicity predicts unique factors that exacerbate student depression is an important next step in understanding how to create more equitable and inclusive research and teaching environments for graduate students. Moreover, our sample included a significant number of students from ecology and evolutionary biology PhD programs, which may limit the generalizability of some findings. It is important to acknowledge potential subdisciplinary differences when considering how research may affect depression. Additionally, some of the factors that affect student depression, such as lack of teaching training and confidence in teaching, may be correlated with time spent in a graduate program. Future quantitative studies would benefit from examining whether the factors that affect student depression depend on the student’s subdiscipline and time spent in the graduate program. The primary focus of this study was the relationship between depression and graduate teaching/research. Many of the factors that emerged from the interviews are also associated with burnout ( Bianchi et al. , 2014 ; Maslach et al. , 2001 ). Burnout and depression are known to be highly related and often difficult to disaggregate ( Bianchi et al. , 2014 ). It was beyond the scope and design of this study to disaggregate which factors relate exclusively to the condition of burnout. Additionally, the interviews in this study were collected at a single time point. Thus, we are unable to differentiate between students who had depression before starting graduate school and students who experienced depression after starting graduate school. Future longitudinal studies could explore the effects of students’ experiences in research and teaching on their depression over time as well as on long-term outcomes such as persistence in graduate programs, length of time for degree completion, and career trajectory. This study identified a number of factors that graduate programs can address to benefit graduate student mental health, and we hope that future studies design and test interventions designed to improve the experiences of graduate students in teaching and research.
In this interview study of 50 life sciences PhD students with depression, we examined how graduate research and teaching affect students’ depressive symptoms. We also explored how depression affected graduate students’ teaching and research. We found that graduate students more commonly highlighted ways that research negatively affected their depression and ways that teaching positively affected their depression. Four overarching factors, three of which were related to both teaching and research, were commonly associated with student depression, including the amount of structure provided in research and teaching, failure and success, positive and negative reinforcement, and social connections and isolation. Additionally, graduate students identified depression as having an exclusively negative effect on their research, often hindering motivation, concentration, and self-esteem. However, they did note that depression made them more compassionate teachers, but also could cause them to have low energy or feel disconnected when teaching. This study provides concrete factors that graduate programs can target in hopes of improving the experiences of life sciences PhD students with depression.
Important Note
There are resources available if you or someone you know is experiencing depression and want help. Colleges and universities often have crisis hotlines and counseling services designed to provide students, staff, and faculty with treatment for depression. These can often be found by searching the university website. Additionally, there are free 24/7 services such as Crisis Text Line, which allows you to text a trained live crisis counselor (text “CONNECT” to 741741; Text Depression Hotline, 2019 ), and phone hotlines such as the National Suicide Prevention Lifeline at 1-800-273-8255 (TALK). If you would like to learn more about depression or depression help and resources near you, visit the Anxiety and Depression Association of American website: https://adaa.org ( Anxiety and Depression Association of America, 2019 ) and the Depression and Bipolar Support Alliance: http://dbsalliance.org ( Depression and Bipolar Support Alliance, 2019 ).
Acknowledgments
We are incredibly grateful to the 50 graduate students who were willing to share their personal experiences with us. We thank Sara Brownell, Tasneem Mohammed, Carly Busch, Maddie Ostwald, Lauren Neel, and Rachel Scott for their helpful feedback on earlier drafts of this work. L.E.G. was supported by an NSF Graduate Fellowship (DGE-1311230). Any opinions, findings, conclusions, or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the NSF.
- American College Health Association. (2014). Graduate/ professional reference group report, Spring 2014 (American College Health Association National College Health Assessment II) . Retrieved March 15, 2021, from www.acha.org/documents/ncha/NCHA-II_WEB-PAPER_SPRING2014_GRADUATE_PROFESSIONAL_REFERENCEGROUP_DATAREPORT.pdf
- American College Health Association. (2019). Graduate/ professional reference group report, Spring 2019 (American College Health Association National College Health Assessment II) . Retrieved March 15, 2021, from www.acha.org/documents/ncha/NCHA-II_SPRING_2019_GRADUATE_AND_PROFESSIONAL_REFERENCE_GROUP_DATA_REPORT.pdf
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Publishing. [ Google Scholar ]
- American Psychiatric Association. (2020). What is depression? Retrieved March 15, 2021, from www.psychiatry.org/patients-families/depression/what-is-depression
- Anxiety and Depression Association of America. (2015). A survey about mental health and suicide in the United States . Retrieved March 15, 2021, from https://adaa.org/sites/default/files/College-Aged_Adults_Survey_Summary-1.14.16.pdf
- Anxiety and Depression Association of America. (2019). Retrieved October 1, 2019, from https://adaa.org
- Barnes, M. E., Truong, J. M., Brownell, S. E. (2017). Experiences of Judeo-Christian students in undergraduate biology . CBE—Life Sciences Education , 16 ( 1 ), ar15. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Barnes, M. E., Maas, S. A., Roberts, J. A., Brownell, S. E. (2021). Christianity as a concealable stigmatized identity (CSI) among biology graduate students . CBE—Life Sciences Education , 20 ( 1 ), ar9. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Beck, A. T. (1967). Depression: Clinical, experimental and theoretical aspects . New York: Harper & Row. [ Google Scholar ]
- Beck, A. T., Rush, A. J., Shaw, B. F. (1979). Cognitive therapy of depression . New York, NY: Guilford. [ Google Scholar ]
- Bianchi, R., Schonfeld, I. S., Laurent, E. (2014). Is burnout a depressive disorder? A reexamination with special focus on atypical depression . International Journal of Stress Management , 21 ( 4 ), 307. [ Google Scholar ]
- Barreira, P., Basilico, M., Bolotnyy, V. (2020). Graduate student mental health: Lessons from American economics departments . Working Paper. Cambridge, MA: Harvard University. https://scholar.harvard.edu/bolotnyy/publications/graduate-student-mental-health-lessons-american-economics-departments [ Google Scholar ]
- Busch, F. N., Rudden, M., Shapiro, T. (2016). Psychodynamic treatment of depression . Washington, DC: American Psychiatric Publishing. [ Google Scholar ]
- Carlone, H. B., Johnson, A. (2007). Understanding the science experiences of successful women of color: Science identity as an analytic lens . Journal of Research in Science Teaching , 44 ( 8 ), 1187–1218. [ Google Scholar ]
- Carvalho, J., Trent, L. R., Hopko, D. R. (2011). The impact of decreased environmental reward in predicting depression severity: Support for behavioral theories of depression . Psychopathology , 44 ( 4 ), 242–252. [ PubMed ] [ Google Scholar ]
- Charles, S. T., Karnaze, M. M., Leslie, F. M. (2021). Positive factors related to graduate student mental health . Journal of American College Health , 1–9. 10.1080/07448481.2020.1841207 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Charmaz, K. (2006). Constructing grounded theory: A practical guide through qualitative research . Thousand Oaks, CA: Sage. [ PubMed ] [ Google Scholar ]
- Chávez, K., Mitchell, K. M. (2020). Exploring bias in student evaluations: Gender, race, and ethnicity . PS: Political Science & Politics , 53 ( 2 ), 270–274. [ Google Scholar ]
- Chirikov, I., Soria, K. M., Horgos, B., Jones-White, D. (2020). Undergraduate and graduate students’ mental health during the COVID-19 pandemic . Oakland, CA: California Digital Library, University of California. [ Google Scholar ]
- Clance, P. R., Imes, S. A. (1978). The imposter phenomenon in high achieving women: Dynamics and therapeutic intervention . Psychotherapy: Theory, Research & Practice , 15 ( 3 ), 241. [ Google Scholar ]
- Cohen, E. D., McConnell, W. R. (2019). Fear of fraudulence: Graduate school program environments and the impostor phenomenon . Sociological Quarterly , 60 ( 3 ), 457–478. [ Google Scholar ]
- Cooper, K. M., Brownell, S. E. (2016). Coming out in class: Challenges and benefits of active learning in a biology classroom for LGBTQIA students . CBE—Life Sciences Education , 15 ( 3 ), ar37. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cooper, K. M., Gin, L. E., Akeeh, B., Clark, C. E., Hunter, J. S., Roderick, T. B., ... & Brownell, S. E. (2019). Factors that predict life sciences student persistence in undergraduate research experiences . PLoS ONE , 14 ( 8 ). 10.1371/journal.pone.0220186 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cooper, K. M., Gin, L. E., Barnes, M. E., Brownell, S. E. (2020a). An exploratory study of students with depression in undergraduate research experiences . CBE—Life Sciences Education , 19 ( 2 ), ar19. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cooper, K. M., Gin, L. E., Brownell, S. E. (2020b). Depression as a concealable stigmatized identity: What influences whether students conceal or reveal their depression in undergraduate research experiences? International Journal of STEM Education , 7 , 1–18. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- d’Apollonia, S., Abrami, P. C. (1997). Navigating student ratings of instruction . American Psychologist , 52 ( 11 ), 1198. [ PubMed ] [ Google Scholar ]
- Depression and Bipolar Support Alliance. (2019). Retrieved March 15, 2021, from http://dbsalliance.org
- Detweiler-Bedell, J. B., Whisman, M. A. (2005). A lesson in assigning homework: Therapist, client, and task characteristics in cognitive therapy for depression . Professional Psychology: Research and Practice , 36 ( 2 ), 219. [ Google Scholar ]
- Dey, S., Newell, B. R., Moulds, M. L. (2018). The relative effects of abstract versus concrete thinking on decision-making in depression . Behaviour Research and Therapy , 110 , 11–21. [ PubMed ] [ Google Scholar ]
- Dickson, J. M., Moberly, N. J. (2013). Reduced specificity of personal goals and explanations for goal attainment in major depression . PLoS ONE , 8 ( 5 ), e64512. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Downing, V. R., Cooper, K. M., Cala, J. M., Gin, L. E., Brownell, S. E. (2020). Fear of negative evaluation and student anxiety in community college active-learning science courses . CBE—Life Sciences Education , 19 ( 2 ), ar20. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Elliott, R. (1998). The neuropsychological profile in unipolar depression . Trends in Cognitive Sciences , 2 ( 11 ), 447–454. [ PubMed ] [ Google Scholar ]
- Evans, T. M., Bira, L., Gastelum, J. B., Weiss, L. T., Vanderford, N. L. (2018). Evidence for a mental health crisis in graduate education . Nature Biotechnology , 36 ( 3 ), 282. [ PubMed ] [ Google Scholar ]
- Fan, Y., Shepherd, L. J., Slavich, E., Waters, D., Stone, M., Abel, R., Johnston, E. L. (2019). Gender and cultural bias in student evaluations: Why representation matters . PLoS ONE , 14 ( 2 ), e0209749. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Flaherty, C. (2018). New study says graduate students’ mental health is a “crisis.” Inside Higher Ed . Retrieved March 15, 2021, from www.insidehighered.com/news/2018/03/06/new-study-says-graduate-students-mental-health-crisis [ Google Scholar ]
- Gin, L. E., Guerrero, F. A., Brownell, S. E., Cooper, K. M. (2021). COVID-19 and undergraduates with disabilities: Challenges resulting from the rapid transition to online course delivery for students with disabilities in undergraduate STEM at large-enrollment institutions . CBE—Life Sciences Education , 20 ( 3 ), ar36. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Glesne, C., Peshkin, A. (1992). Becoming qualitative researchers: An introduction . London, UK: Longman. [ Google Scholar ]
- Gormally, C., Evans, M., Brickman, P. (2014). Feedback about teaching in higher ed: Neglected opportunities to promote change . CBE—Life Sciences Education , 13 ( 2 ), 187–199. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gotlib, I. H., Krasnoperova, E. (1998). Biased information processing as a vulnerability factor for depression . Behavior Therapy , 29 ( 4 ), 603–617. [ Google Scholar ]
- Grahek, I., Shenhav, A., Musslick, S., Krebs, R. M., Koster, E. H. (2019). Motivation and cognitive control in depression . Neuroscience & Biobehavioral Reviews , 102 , 371–381. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Helmers, K. F., Danoff, D., Steinert, Y., Leyton, M., Young, S. N. (1997). Stress and depressed mood in medical students, law students, and graduate students at McGill University . Academic Medicine , 72 ( 8 ), 708–714. [ PubMed ] [ Google Scholar ]
- Henry, M. A., Shorter, S., Charkoudian, L., Heemstra, J. M., Corwin, L. A. (2019). FAIL is not a four-letter word: A theoretical framework for exploring undergraduate students’ approaches to academic challenge and responses to failure in STEM learning environments . CBE—Life Sciences Education , 18 ( 1 ), ar11. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hish, A. J., Nagy, G. A., Fang, C. M., Kelley, L., Nicchitta, C. V., Dzirasa, K., Rosenthal, M. Z. (2019). Applying the stress process model to stress–burnout and stress–depression relationships in biomedical doctoral students: A cross-sectional pilot study . CBE—Life Sciences Education , 18 ( 4 ), ar51. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Howell, E., McFeeters, J. (2008). Children’s mental health care: Differences by race/ethnicity in urban/rural areas . Journal of Health Care for the Poor and Underserved , 19 ( 1 ), 237–247. [ PubMed ] [ Google Scholar ]
- Jones-White, D. R., Soria, K. M., Tower, E. K., Horner, O. G. (2020). Factors associated with anxiety and depression among US doctoral students: Evidence from the gradSERU survey . Journal of American College Health , 1–12. 10.1080/07448481.2020.1865975 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Judd, L. L., Paulus, M. J., Schettler, P. J., Akiskal, H. S., Endicott, J., Leon, A. C., ... & Keller, M. B. (2000). Does incomplete recovery from first lifetime major depressive episode herald a chronic course of illness? American Journal of Psychiatry , 157 ( 9 ), 1501–1504. [ PubMed ] [ Google Scholar ]
- Kanter, J. W., Callaghan, G. M., Landes, S. J., Busch, A. M., Brown, K. R. (2004). Behavior analytic conceptualization and treatment of depression: Traditional models and recent advances . Behavior Analyst Today , 5 ( 3 ), 255. [ Google Scholar ]
- Kataoka, S. H., Zhang, L., Wells, K. B. (2002). Unmet need for mental health care among US children: Variation by ethnicity and insurance status . American Journal of Psychiatry , 159 ( 9 ), 1548–1555. [ PubMed ] [ Google Scholar ]
- Kember, D., Leung, D. Y., Kwan, K. (2002). Does the use of student feedback questionnaires improve the overall quality of teaching? Assessment & Evaluation in Higher Education , 27 ( 5 ), 411–425. [ Google Scholar ]
- Landis, J. R., Koch, G. G. (1977). “ An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers . Biometrics , 363–374. [ PubMed ] [ Google Scholar ]
- Leahy, R. (2002). Clinical advances in cognitive psychotherapy: Theory and application . New York, NY: Springer. [ Google Scholar ]
- Levecque, K., Anseel, F., De Beuckelaer, A., Van der Heyden, J., Gisle, L. (2017). Work organization and mental health problems in PhD students . Research Policy , 46 ( 4 ), 868–879. [ Google Scholar ]
- Lewinsohn, P. M. (1974). The psychology of depression: Contemporary theory and research . Sydney, Australia: Halsted Press. [ Google Scholar ]
- Lipson, S. K., Lattie, E. G., Eisenberg, D. (2019). Increased rates of mental health service utilization by US college students: 10-year population-level trends (2007–2017) . Psychiatric Services , 70 ( 1 ), 60–63. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Liu, C., Wang, L., Qi, R., Wang, W., Jia, S., Shang, D., ... & Yan, S. (2019). Prevalence and associated factors of depression and anxiety among doctoral students: The mediating effect of mentoring relationships on the association between research self-efficacy and depression/anxiety . Psychology Research and Behavior Management , 12 , 195. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Maj, M., Stein, D. J., Parker, G., Zimmerman, M., Fava, G. A., De Hert, M., ... & Wittchen, H.-U. (2020). The clinical characterization of the adult patient with depression aimed at personalization of management . World Psychiatry , 19 ( 3 ), 269–293. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Manos, R. C., Kanter, J. W., Busch, A. M. (2010). A critical review of assessment strategies to measure the behavioral activation model of depression . Clinical Psychology Review , 30 ( 5 ), 547–561. [ PubMed ] [ Google Scholar ]
- Martell, C. R., Addis, M. E., Jacobson, N. S. (2001). Depression in context: Strategies for guided action . New York: Norton. [ Google Scholar ]
- Maslach, C., Schaufeli, W. B., Leiter, M. P. (2001). Job burnout . Annual Review of Psychology , 52 ( 1 ), 397–422. [ PubMed ] [ Google Scholar ]
- McGregor, L. N., Gee, D. E., Posey, K. E. (2008). I feel like a fraud and it depresses me: The relation between the imposter phenomenon and depression . Social Behavior and Personality: An International Journal , 36 ( 1 ), 43–48. [ Google Scholar ]
- Mcleod, S. A. (2015). Psychological Theories of Depression . Simply Psychology , Retrieved March 15, 2021, from https://www.simplypsychology.org/depression.html [ Google Scholar ]
- Miranda, J., Persons, J. B. (1988). Dysfunctional attitudes are mood-state dependent . Journal of Abnormal Psychology , 97 ( 1 ), 76. [ PubMed ] [ Google Scholar ]
- The mental health of PhD researchers demands urgent attention [Editorial] . (2019). Nature , 575 ( 7782 ), 257–258. 10.1038/d41586-019-03489-1 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pain, E. (2018, March 6). Graduate students need more mental health support, study highlights . Science. Retrieved March 15, 2021, from www.sciencemag.org/careers/2018/03/graduate-students-need-more-mental-health-support-new-study-highlights [ Google Scholar ]
- Peluso, D. L., Carleton, R. N., Asmundson, G. J. (2011). Depression symptoms in Canadian psychology graduate students: Do research productivity, funding, and the academic advisory relationship play a role? Canadian Journal of Behavioural Science/Revue Canadienne des Sciences du Comportement , 43 ( 2 ), 119. [ Google Scholar ]
- Pfeifer, M. A., Reiter, E. M., Cordero, J. J., Stanton, J. D. (2021). Inside and out: Factors that support and hinder the self-advocacy of undergraduates with ADHD and/or specific learning disabilities in STEM . CBE—Life Sciences Education , 20 ( 2 ), ar17. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Puri, P. (2019). The emotional toll of graduate school . Scientific American Blog Network . Retrieved March 15, 2021, from https://blogs.scientificamerican.com/observations/the-emotional-toll-of-graduate-school/
- Ramnerö, J., Folke, F., Kanter, J. W. (2016). A learning theory account of depression . Scandinavian Journal of Psychology , 57 ( 1 ), 73–82. [ PubMed ] [ Google Scholar ]
- Saldaña, J. (2015). The coding manual for qualitative researchers . Thousand Oaks, CA: Sage. [ Google Scholar ]
- Santiago, C. D., Kaltman, S., Miranda, J. (2013). Poverty and mental health: How do low-income adults and children fare in psychotherapy? Journal of Clinical Psychology , 69 ( 2 ), 115–126. [ PubMed ] [ Google Scholar ]
- Santini, Z. I., Koyanagi, A., Tyrovolas, S., Mason, C., Haro, J. M. (2015). The association between social relationships and depression: A systematic review . Journal of Affective Disorders , 175 , 53–65. [ PubMed ] [ Google Scholar ]
- Schmidt, S. L., Tolentino, J. C. (2018). DSM-5 criteria and depression severity: Implications for clinical practice . Frontiers in Psychiatry , 9 , 450. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schussler, E. E., Read, Q., Marbach-Ad, G., Miller, K., Ferzli, M. (2015). Preparing biology graduate teaching assistants for their roles as instructors: An assessment of institutional approaches . CBE—Life Sciences Education , 14 ( 3 ), ar31. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shortlidge, E. E., Eddy, S. L. (2018). The trade-off between graduate student research and teaching: A myth? PLoS ONE , 13 ( 6 ), e0199576. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Simpson, A., Maltese, A. (2017). “ Failure is a major component of learning anything”: The role of failure in the development of STEM professionals . Journal of Science Education and Technology , 26 ( 2 ), 223–237. [ Google Scholar ]
- Tanner, K., Allen, D. (2006). Approaches to biology teaching and learning: On integrating pedagogical training into the graduate experiences of future science faculty . CBE—Life Sciences Education , 5 ( 1 ), 1–6. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Text Depression Hotline. (2019). Crisis text line . Retrieved March 15, 2021, from www.crisistextline.org/depression
- Torvi, D. A. (1994). Engineering graduate teaching assistant instructional programs: Training tomorrow’s faculty members . Journal of Engineering Education , 83 ( 4 ), 376–382. [ Google Scholar ]
- Trenor, J. M., Miller, M. K., Gipson, K. G. (2011). Utilization of a think-aloud protocol to cognitively validate a survey instrument identifying social capital resources of engineering undergraduates . Vancouver, BC: American Society for Engineering Education. [ Google Scholar ]
- U.S. News & World Report: News, Rankings and Analysis on Politics, Education, Healthcare and More. (2019). Retrieved October 1, 2019, from https://www.usnews.com/best-graduate-schools/top-science-schools/biological-sciences-rankings
- Watkins, E., Brown, R. G. (2002). Rumination and executive function in depression: An experimental study . Journal of Neurology, Neurosurgery & Psychiatry , 72 ( 3 ), 400–402. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Weissman, A. (1979). Dysfunctional Attitude Scale (DAS) . Acceptance and Commitment Therapy. Measures Package , 54–56. http://www.integrativehealthpartners.org/downloads/ [ Google Scholar ]
- Woolston, C. (2017). Graduate survey: A love–hurt relationship . Nature , 550 ( 7677 ), 549–552. [ Google Scholar ]
- Woolston, C. (2019a, August 30). A better future for graduate-student mental health . Nature . 10.1038/d41586-019-02584-7 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Woolston, C. (2019b). PhDs: The tortuous truth . Nature , 575 ( 7782 ), 403–406. 10.1038/d41586-019-03459-7 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Doctor of Philosophy (PhD)
Offered By: Department of Mental Health
Onsite | Full-Time | 4 – 5 years
- MAS Application Fee Waiver Requirements
- Master of Arts (MA) in Geography and Environmental Engineering
- Master of Arts and Master of Science in Public Health (MA/MSPH)
- Master of Arts in Public Health Biology (MAPHB)
- Master of Bioethics (MBE)
- MHA Frequently Asked Questions
- Mission, Vision, and Values
- MHA Executive in Residence and Alumni
- Student Experience
- Program Outcomes
- Bachelor's/MHA Program
- Master of Health Science (MHS) - Department of Biochemistry and Molecular Biology
- Master of Health Science (MHS) - Department of Epidemiology
- Alumni Update
- MHS Combined with a Certificate Program
- Master of Health Science (MHS) - Department of Molecular Microbiology and Immunology
- Alumni Highlights
- Post-Baccalaureate Program in Environmental Health for Pre-Medicine Students
- Bachelor's/MHS in Health Economics and Outcomes Research
- MHS HEOR Careers
- Frequently Asked Questions
- Master of Health Science (MHS)
- Concurrent School-Wide Master of Health Science Program in Biostatistics
- Master of Health Science - Department of Population, Family and Reproductive Health
- Master of Health Science Online (MHS) - Department of Population, Family and Reproductive Health
- Careers in Health Economics
- Core Competencies
- Meet the Director
- What is Health Economics
- MPH Capstone Schedule
- Concentrations
- Online/Part-Time Format
- Requirements
Tuition and Funding
- Executive Board Faculty
- Master of Science (MS) in Geography and Environmental Engineering
- Independent Professional Project and Final Essay
- Program Objectives and Outcomes
- Internships
- Master of Science (ScM) - Department of Biochemistry and Molecular Biology
- Master of Science (ScM) - Department of Biostatistics
- Master of Science (ScM) - Department of Epidemiology
- Master of Science (ScM) - Department of Molecular Microbiology and Immunology
- ScM Faculty Advisers
- Master of Science in Engineering (MSE) in Geography and Environmental Engineering
- Bachelor's/MSPH in Health Policy
- FAQ for MSPH in Health Policy
- Field Placement Experience
- MSPH Capstone
- MSPH Practicum
- Required and Elective Courses
- Student Timeline
- Career Opportunities
- 38-Week Dietetics Practicum
- Completion Requirements
- MSPH/RD Program FAQ
- Program Goals
- Master's Essay Titles
- Application Fee Waiver Requirements
- Doctor of Philosophy (PhD) - Department of Biostatistics
- Doctor of Philosophy (PhD) - Department of Epidemiology
- Program Goals and Expectations
- Doctor of Philosophy (PhD) - Department of Molecular Microbiology and Immunology
- Doctor of Philosophy (PhD) - Department of Population, Family and Reproductive Health
- Doctor of Philosophy (PhD) in Clinical Investigation
- Track in Environmental Sustainability, Resilience, and Health
- Track in Exposure Sciences and Environmental Epidemiology
- Track in Health Security
- Track in Toxicology, Physiology and Molecular Mechanisms
- PhD in Geography and Environmental Engineering Faculty Advisers
- Recent Graduates and Dissertation Titles
- PhD Funding
- PhD TA Requirement
- Recent Dissertation Titles
- JHU-Tsinghua Doctor of Public Health
- Core Course Requirements
- Concentration in Women’s and Reproductive Health
- Custom Track
- Concentration in Environmental Health
- Concentration in Global Health: Policy and Evaluation
- Concentration in Health Equity and Social Justice
- Concentration in Health Policy and Management
- Concentration in Implementation Science
- Meet Current Students
- Combined Bachelor's / Master's Programs
- Concurrent MHS Option for BSPH Doctoral Students
- Concurrent MSPH Option for JHSPH Doctoral students
- Doctor of Medicine and Doctor of Philosophy (MD/PhD)
- Adolescent Health Certificate Program
- Bioethics Certificate Program
- Climate and Health Certificate Program
- Clinical Trials Certificate Program
- Community- Based Public Health Certificate Program
- Demographic Methods Certificate Program
- Environmental and Occupational Health Certificate Program
- Epidemiology for Public Health Professionals Certificate Program
- Evaluation: International Health Programs Certificate Program
- Food Systems, the Environment and Public Health Certificate Program
- Frequently Asked Questions for Certificate Programs
- Gender and Health Certificate Program
- Gerontology Certificate Program
- Global Digital Health Certificate Program
- Global Health Certificate Program
- Global Health Practice Certificate Program
- Health Communication Certificate Program
- Health Disparities and Health Inequality Certificate Program
- Health Education Certificate Program
- Health Finance and Management Certificate Program
- Health and Human Rights Certificate Program
- Healthcare Epidemiology and Infection Prevention and Control Certificate Program
- Humane Sciences and Toxicology Policy Certificate Program
- Humanitarian Health Certificate Program
- Implementation Science and Research Practice Certificate Program
- Injury and Violence Prevention Certificate Program
- International Healthcare Management and Leadership Certificate Program
- Leadership for Public Health and Healthcare Certificate Program
- Lesbian, Gay, Bisexual, Transgender, and Queer (LGBTQ) Public Health Certificate Program
- Maternal and Child Health Certificate Program
- Mental Health Policy, Economics and Services Certificate Program
- Non-Degree Students General Admissions Info
- Pharmacoepidemiology and Drug Safety Certificate Program
- Population Health Management Certificate Program
- Population and Health Certificate Program
- Product Stewardship for Sustainability Certificate Program
- Public Health Advocacy Certificate Program
- Public Health Economics Certificate Program
- Public Health Informatics Certificate Program
- Public Health Practice Certificate Program
- Declaration of Intent - Public Health Preparedness
- Public Health Training Certificate for American Indian Health Professionals
- Public Mental Health Research Certificate Program
- Quality, Patient Safety and Outcomes Research Certificate Program
- Quantitative Methods in Public Health Certificate Program
- Requirements for Successful Completion of a Certificate Program
- Rigor, Reproducibility, and Responsibility in Scientific Practice Certificate Program
- Risk Sciences and Public Policy Certificate Program
- Spatial Analysis for Public Health Certificate Program
- Training Certificate in Public Health
- Tropical Medicine Certificate Program
- Tuition for Certificate Programs
- Vaccine Science and Policy Certificate Program
- Online Student Experience
- Online Programs for Applied Learning
- Barcelona Information
- Fall Institute Housing Accommodations
- Participating Centers
- Registration, Tuition, and Fees
- Agency Scholarship Application
- General Scholarship Application
- UPF Scholarship Application
- Course Evaluations
- Online Courses
- Registration
- General Institute Tuition Information
- International Students
- Directions to the Bloomberg School
- All Courses
- Important Guidance for ONSITE Students
- D.C. Courses
- Registration and Fees
- Cancellation and Closure Policies
- Application Procedures
- Career Search
- Current Activities
- Current Trainees
- Related Links
- Process for Appointing Postdoctoral Fellows
- Message from the Director
- Program Details
- Admissions FAQ
- Current Residents
- Elective Opportunities for Visiting Trainees
- What is Occupational and Environmental Medicine?
- Admissions Info
- Graduates by Year
- Compensation and Benefits
- How to Apply
- Academic Committee
- Course Details and Registration
- Tuition and Fees
- ONLINE SOCI PROGRAM
- Principal Faculty
- Johns Hopkins RAPID Psychological First Aid
- General Application
- JHHS Application
- Areas of Study
- Important Dates
- Our Faculty
- Welcome Letter
- Descripción los Cursos
- Programa en Epidemiología para Gestores de Salud, Basado en Internet
- Consultants
- Britt Dahlberg, PhD
- Joke Bradt, PhD, MT-BC
- Mark R. Luborsky, PhD
- Marsha Wittink, PhD
- Rebekka Lee, ScD
- Su Yeon Lee-Tauler, PhD
- Theresa Hoeft, PhD
- Vicki L. Plano Clark, PhD
- Program Retreat
- Mixed Methods Applications: Illustrations
- Announcements
- 2023 Call for Applications
- Jennifer I Manuel, PhD, MSW
- Joke Bradt, PhD
- Josiemer Mattei, PhD, MPH
- Justin Sanders, MD, MSc
- Linda Charmaran, PhD
- Nao Hagiwara, PhD
- Nynikka R. A. Palmer, DrPH, MPH
- Olayinka O. Shiyanbola, BPharm, PhD
- Sarah Ronis, MD, MPH
- Susan D. Brown, PhD
- Tara Lagu, MD, MPH
- Theresa Hoft, PhD
- Wynne E. Norton, PhD
- Yvonne Mensa-Wilmot, PhD, MPH
- A. Susana Ramírez, PhD, MPH
- Animesh Sabnis, MD, MSHS
- Autumn Kieber-Emmons, MD, MPH
- Benjamin Han, MD, MPH
- Brooke A. Levandowski, PhD, MPA
- Camille R. Quinn, PhD, AM, LCSW
- Justine Wu, MD, MPH
- Kelly Aschbrenner, PhD
- Kim N. Danforth, ScD, MPH
- Loreto Leiva, PhD
- Marie Brault, PhD
- Mary E. Cooley, PhD, RN, FAAN
- Meganne K. Masko, PhD, MT-BC/L
- PhuongThao D. Le, PhD, MPH
- Rebecca Lobb, ScD, MPH
- Allegra R. Gordon, ScD MPH
- Anita Misra-Hebert, MD MPH FACP
- Arden M. Morris, MD, MPH
- Caroline Silva, PhD
- Danielle Davidov, PhD
- Hans Oh, PhD
- J. Nicholas Dionne-Odom, PhD RN ACHPN
- Jacqueline Mogle, PhD
- Jammie Hopkins, DrPH, MS
- Joe Glass, PhD MSW
- Karen Whiteman, PhD MSW
- Katie Schultz, PhD MSW
- Rose Molina, MD
- Uriyoán Colón-Ramos, ScD MPA
- Andrew Riley, PhD
- Byron J. Powell, PhD, LCSW
- Carrie Nieman MD, MPH
- Charles R. Rogers, PhD, MPH, MS, CHES®
- Emily E. Haroz, PhD
- Jennifer Tsui, Ph.D., M.P.H.
- Jessica Magidson, PhD
- Katherine Sanchez, PhD, LCSW
- Kelly Doran, MD, MHS
- Kiara Alvarez, PhD
- LaPrincess C. Brewer, MD, MPH
- Melissa Radey, PhD, MA, MSSW
- Sophia L. Johnson, PharmD, MPH, PhD
- Supriya Gupta Mohile, MD, MS
- Virginia McKay, PhD
- Andrew Cohen, MD, PhD
- Angela Chen, PhD, PMHNP-BC, RN
- Christopher Salas-Wright, PhD, MSW
- Eliza Park MD, MS
- Jaime M. Hughes, PhD, MPH, MSW
- Johanne Eliacin, PhD, HSPP
- Lingrui Liu ScD MS
- Meaghan Kennedy, MD
- Nicole Stadnick, PhD, MPH
- Paula Aristizabal, MD
- Radhika Sundararajan, MD
- Sara Mamo, AuD, PhD
- Tullika Garg, MD MPH FACS
- Allison Magnuson, DO
- Ariel Williamson PhD, DBSM
- Benita Bamgbade, PharmD, PhD
- Christopher Woodrell MD
- Hung-Jui (Ray) Tan, MD, MSHPM
- Jasmine Abrams, PhD
- Jose Alejandro Rauh-Hain, MD
- Karen Flórez, DrPH, MPH
- Lavanya Vasudevan, PhD, MPH, CPH
- Maria Garcia, MD, MPH
- Robert Brady, PhD
- Saria Hassan, MD
- Scherezade Mama, DrPH
- Yuan Lu, ScD
- 2021 Scholars
- Sign Up for Our Email List
- Workforce Training
- Cells-to-Society Courses
- Course/Section Numbers Explained
- Pathway Program with Goucher College
- The George G. Graham Lecture
About the PhD in Mental Health Program
The PhD degree is a research-oriented doctoral degree. In the first two years, students take core courses in the Departments of Mental Health, Biostatistics, and Epidemiology, in research ethics, and attend weekly department seminars. Students must complete a written comprehensive exam (in January of their second year), a preliminary exam, two presentations and a final dissertation including presentation and defense. Throughout their time in the department, we encourage all doctoral students to participate in at least one research group of the major research programs in the department: Substance Use Epidemiology, Global Mental Health, Mental Health and Aging, Mental Health Services and Policy, Methods, Prevention Research, Psychiatric and Behavioral Genetic Epidemiology, Psychiatric Epidemiology, and Autism and Developmental Disabilities.
PhD in Mental Health Program Highlights
mental health dept. in a school of public health
World renowned faculty
who are experts in the field
Students conduct
original research
Research opportunities
in the US and globally
What Can You Do With a Graduate Degree In Mental Health?
Sample careers.
- Assistant Professor
- Postdoctoral Fellow
- Psychiatric Epidemiologist
- Prevention Scientist
- Social and Behavioral Scientist
Curriculum for the PhD in Mental Health
Browse an overview of the requirements for this PhD program in the JHU Academic Catalogue , explore all course offerings in the Bloomberg School Course Directory .
Current students can view the Department of Mental Health's student handbook on the Info for Current Students page .
Research Areas
The Department of Mental Health covers a wide array of topics related to mental health, mental illness and substance abuse. Faculty and students from multiple disciplines work together within and across several major research areas.
Admissions Requirements
For general admissions requirements, please visit the How to Apply page.
Standardized Test Scores
Standardized test scores are not required and not reviewed for this program. If you have taken a standardized test such as the GRE, GMAT, or MCAT and want to submit your scores, please note that they will not be used as a metric during the application review. Applications will be reviewed holistically based on all required application components.
Program Faculty Spotlight

Judith K. Bass
Judith Bass, PhD '04, MPH, MIA, is an implementation science researcher, with a broad background in sociology, economic development studies, and psychiatric epidemiology.

Renee M. Johnson
Renee M. Johnson, PhD, MPH, uses social epidemiology and behavioral science methods to investigate injury/violence, substance use, and overdose prevention.

George W. Rebok
George Rebok, PhD, MA, is a life-span developmental psychologist who develops community-based interventions to prevent age-related cognitive decline and reduce dementia risk.

Heather E. Volk
Heather Volk, PhD, MPH, seeks to identify factors that relate to the risk and progression of neurodevelopment disorders.
All full-time PhD students will receive the following support for the first four years of the program: full tuition, individual health insurance, University Health Services clinic fee, vision insurance, and dental insurance. Stipends are available for students accepted into an NIH-funded training grant in the areas of Psychiatric Epidemiology, Global Mental Health, Substance Use Epidemiology, Aging, and Mental Health Services and Systems. To be considered for a NIH-funded training grants you must be a US Citizen or permanent resident of the US.
Need-Based Relocation Grants Students who are admitted to PhD programs at JHU starting in Fall 2023 or beyond can apply to receive a $1500 need-based grant to offset the costs of relocating to be able to attend JHU. These grants provide funding to a portion of incoming students who, without this money, may otherwise not be able to afford to relocate to JHU for their PhD program. This is not a merit-based grant. Applications will be evaluated solely based on financial need. View more information about the need-based relocation grants for PhD students .
Questions about the program? We're happy to help.
Academic Program Administrator Patricia Scott [email protected] 410-955-1906
Compare Programs
- Check out similar programs at the Bloomberg School to find the best fit.
- Doctor of Philosophy (PhD) in International Health
- Doctor of Philosophy (PhD) in Epidemiology
- Doctor of Philosophy (PhD) in Health Policy and Management
- International edition
- Australia edition
- Europe edition

Dark thoughts: why mental illness is on the rise in academia
Mental health problems are on the rise among UK academics amid the pressures of greater job insecurity, constant demand for results and an increasingly marketised higher education system.
University counselling staff and workplace health experts have seen a steady increase in numbers seeking help for mental health problems over the past decade, with research indicating nearly half of academics show symptoms of psychological distress.
"Culture of acceptance"
A recent blog on the Guardian Higher Education Network blog , which highlighted a "culture of acceptance" in universities around mental health issues, has received an unprecedented response, pointing to high levels of distress among academics.
The article, which reported instances of depression, sleep issues, eating disorders, alcoholism, self-harming, and even suicide attempts among PhD students, has been shared hundreds of thousands of times and elicited comments outlining similar personal experiences from students and academics.
But while anecdotal accounts multiply, mental health issues in academia are little-researched and hard data is thin on the ground.
However, a study published in 2013 by the University and College Union (UCU) used health and safety executive measures, assessed against a large sample of over 14,000 university employees, to reveal growing stress levels among academics prompted by heavy workloads, a long hours culture and conflicting management demands. Academics experience higher stress than those in the wider population, the survey revealed.
Tackling perfectionism
Pat Hunt, head of Nottingham University's counselling service for staff and students and a member of the UK body for heads of university counselling services, said all universities were experiencing an increase in mental health problems.
"There are increasing levels of anxiety, both generalised and acute, levels of stress, of depression and levels of what I would call perfectionism," she says.
"By that I mean when someone is aiming for and constantly expecting really high standards, so that even when there is a positive outcome they feel they have fallen short. So instead of internal aspiration helping them to do well it actually hinders them."
Academics are also caught up in a range of cycles, from league tables and student satisfaction surveys to research league tables, that dominate thinking, she adds. In one case, a department's top position in a research profile "became a poisonous thing because everyone then fights to maintain that".
Hunt said higher education should not be stigmatised for the increase in mental health issues, since it reflected a similar increase in wider society. Figures show more working days are now lost to the mental health problems than any other health issue.
Nottingham offers one-to-one and group help to students and staff, including support specifically targeted at men, who make up only a third of those seeking help, a figure likely to reflect the continuing stigma over seeking help for mental illness.
Increased workloads partly to blame
Dr Alan Swann of Imperial College London, chair of the higher education occupational physicians committee, blamed "demands for increased product and productivity" for rising levels of mental health problems among academics.
He says: "They all have to produce results – you are only as good as your research rating or as good as your ability to bring in funding for research."
Swann says most academics are stressed rather than mentally unwell: "They are thinking about their work and the consequences of not being as good as they should be; they're having difficulty switching off and feeling guilty if they're not working seven days a week."
Academics and researchers can become isolated and not realise how "out of kilter" their working lives are, he says.
The intense pressure of doctoral and post-doctoral study, and early-career academia can also reveal existing mental health problems, he adds. Universities , including Imperial, have improved systems to help, yet academia remains "pretty macho".
Uncaring academic environment
"There's still a degree of 'if you can't stand the heat, you shouldn't be here'," says Swann. He says there are "still people in senior positions in academia who actually don't care".
He adds: "But there are measures to counter that and there has been a lot of change for the good. What we have not been able to get rid of are the external pressures from government funding and the academic marketplace."
Research by Gail Kinman, professor of occupational health psychology at the University of Bedfordshire, on behalf of the UCU, offers one of the few pieces of data on mental health problems among academics.
Kinman used the health and safety executive's health and safety at work framework to assess the views of some 20,000 academics, and found "considerably higher" levels of psychological distress than in the population as a whole.
She points to poor work-life balance as a key factor, with academics putting in increasing hours as they attempt to respond to high levels of internal and external scrutiny, a fast pace of change and the notion of students as customers – leading to demands such as 24-hour limit for responses to student queries.
Internalised values hard to shake
There are examples of good practice within universities which could be shared across the sector, Kinman says, but, as an independently-minded group who are strongly committed to their work, academics are not always straightforward to support. "We don't like being told 'you can't email at two in the morning'. You can't impose solutions from other sectors – academics are quite different and there's no 'one size fits all'."
And internalised values are hard to shake. Nadine Muller, lecturer in English literature and cultural history at Liverpool John Moores University, suggests that academia promotes the blurring of lines between the personal and the professional – often described as "doing what you love".
"This means that doctoral and early-career scholars are seldom trained in how to firmly draw that line and value themselves beyond their work," says Muller.
UCU says issues relating to mental health are frequently encountered by its representatives. General secretary Sally Hunt says sufferers experience particular prejudice at work. "Further and higher education workers who experience issues relating to mental health face ignorance, discrimination and stigma from their managers and colleagues.
"Negative and inflexible attitudes can often exclude those with mental health conditions from being able to do their job. Often these attitudes can intimidate a person away from feeling able to disclose their mental health condition at all."
John Hamilton, head of safety, health and wellbeing at Leeds Metropolitan University, says academics' problems are often a question of burnout, which he defines as a "significant disengagement" with an employer, in which a staff member no longer feels in charge of their role.
Some universities, including his own, are working hard to offer support, he says, but while many could "definitely do more", there remains a fundamental problem that some academics simply do not like the changes in their sector that have taken place over the last 20 years. "For some, it's going to be a case of 'I'm sorry, but this is the way it is, this is the political landscape'. So there's an element of putting up with it."
If academics already in post must wrestle with the stresses of fast change, what of their successors? Edward Pinkney, a mental health consultant working in education, says: "Institutions have a broader civic duty to educate potential academics about the university environment, so that prospective academics can make a more informed decision about whether or not to proceed.
"As universities become increasingly businesslike, there's a growing need for them to be independently monitored to ensure that they are not just meeting basic standards of support for their members, but also that they are providing an accurate representation of academic life and not misselling it."
Mental health in academia: experiences from around the world
PhD in health sciences at a Canadian university
"At the beginning of my PhD, the director of the department gave our entire cohort a lecture about not getting pregnant and told one of my friends when she applied for maternity leave that the PhD should be a time of celibacy. Some of our supervisors publicly and proudly exchanged stories of failed marriages as if this was the ultimate proof of their devotion to research. Others gossiped about promising colleagues who 'would have achieved so much more' had they not had children. All of these subtle and not so subtle hints guaranteed that no graduate student, especially those with families, would ever sacrifice enough for their research and would thus, by implication, always be a failure in some respect."
Lecturer at the Open University, UK
"I had only been working for the university for two years when I suffered a severe breakdown and was hospitalised. It was very difficult indeed to even contemplate going back to work but thanks to transition counselling from the union I was able to resume work after nine months. The transition counselling was invaluable for a number of reasons; it was linked to work so helped me to begin to think about going back; it carried on during my first few weeks back in the workplace, so it was invaluable in dealing with my feelings at returning to that environment again; and it enabled me to see my mental health problem as being no different to any physical one. One of the hardest things to face after a breakdown is facing the stigma (both real and perceived) that occurs in the workplace. The union gave practical and psychological support, without which I would not have been able to return work."
University of Maine School of Law, US
" During my three years of law school, I had to come to grips with my acceptance of and seeking treatment for depression and PTSD. I've been lucky to have had a lot of support from close friends, but I've never shared these issues with the faculty. The law school culture is effectively one along the lines of 'suck it up'. When I worked in the law school clinic, I actually hid and lied to my professor about the fact that I was struggling with suicidal thoughts because I was afraid of simply being booted out of a clinic I loved. While a very large amount of law students I have known have coped with mental health issues and even school-related nervous breakdowns, it's not talked about, or even admitted beyond close friends."
PhD in chemistry, Bangor University, Wales
"In 2010 I started a PhD in chemistry. A year on, and the pressure began to build, reaching the point where I had a nervous breakdown. I spent time going to counselling for help, but then decided to take a 10-month break from the research I was doing. Upon returning I was able to work for a few months before falling back into depression because I felt I had no chance of gaining the qualification I desired. I eventually got to the stage where I felt I was going nowhere and cleared my desk late one Saturday, saying nothing to anyone that I was leaving. While suffering from depression, I felt isolated, as everyone around me was able to get on with their PhDs . I felt I was the problem. I feel I received some support for my issues but more could have been done to ease me back into full-time study after returning."
PhD in molecular biology, Uppsala University, Sweden
"My university and department supported me after I admitted I had been diagnosed with depression. In the beginning I took advantage of studenthälsan, the university's student health centre. Their team of psychologists and psychiatrists helped me to find the right long-term support. Later, my depression worsened and I was offered a private psychologist at the cost of the department. Yes, my PhD studies are still a demanding job full of stress, mentally as well as physically, but I am glad that in the days where death was the only solution to everything, my colleagues, supervisors and other officials became friends that just wanted to help me."
If you have been affected by any of the issues mentioned in this piece, contact Samaritans or Nightline .
Are universities doing enough to support academics with mental health issues? Share your thoughts in the comments below, citing any relevant research.
This content is brought to you by Guardian Professional . Looking for your next university role? Browse Guardian jobs for hundreds of the latest academic, administrative and research posts.
- Universities
- Student experience
- Higher education

Survey: 25% of UK architecture students treated for mental health problems

How Cambridge University almost killed me

How academics can help ensure students’ wellbeing

Six things students can do to boost their mental health

Tuition fees 'have led to surge in students seeking counselling'

Feeling worthless, hopeless … who'd be a university student in Britain?

Students: where to get help for your mental health

Student mental health: a new model for universities

Student mental health: if you can't see a counsellor, consider other options

Uni counselling services challenged by growing demand
Comments (…), most viewed.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- CAREER FEATURE
- 11 May 2021
How to blow the whistle on an academic bully
- Virginia Gewin 0
Virginia Gewin is a freelance writer in Portland, Oregon.
You can also search for this author in PubMed Google Scholar
Bullying is endemic in academia, an environment riddled with hierarchies and hyper-competition, exacerbated by an over-reliance on temporary contracts and the pressure to land highly coveted tenured positions.
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
Nature 593 , 299-301 (2021)
doi: https://doi.org/10.1038/d41586-021-01252-z
Related Articles

- Research management
Brazil’s postgraduate funding model is about rectifying past inequalities
Correspondence 09 APR 24
Declining postdoc numbers threaten the future of US life science

How we landed job interviews for professorships straight out of our PhD programmes
Career Column 08 APR 24

How I harnessed media engagement to supercharge my research career
Career Column 09 APR 24

Three ways ChatGPT helps me in my academic writing

How two PhD students overcame the odds to snag tenure-track jobs
Adopt universal standards for study adaptation to boost health, education and social-science research
Correspondence 02 APR 24
PhD position (all genders) in AI for biomedical data analysis
PhD position (all genders) in AI for biomedical data analysis Part time | Temporary | Arbeitsort: Hamburg-Eppendorf UKE_Zentrum für Molekulare Ne...
Hamburg (DE)
Personalwerk GmbH
Postdoctoral fellow in structure determination of membrane proteins using cryo-EM
The Institute of Biomedicine is involved in both research and education. In both of these areas, we focus on fundamental knowledge of the living ce...
Gothenburg (Stad), Västra Götaland (SE)
University of Gothenburg
Postdoctoral Associate- Endometriosis
Houston, Texas (US)
Baylor College of Medicine (BCM)
Postdoctoral Research Fellow at the Dalian Institute of Chemical Physics
Located in the beautiful coastal city of Dalian, surrounded by mountains and sea, DICP seeks all talents from around the globe.
Dalian, Liaoning, China
The Dalian Institute of Chemical Physics (DICP)
Postdoctoral Research Associate
Qualifications: PhD degree in chemistry, radiochemistry, or nuclear medicine technology with at least 3 years of PET radiochemistry work experience i
Charlottesville, Virginia
University of Virginia Health
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Nervous Breakdown what is it?

What is a Nervous Breakdown or Mental Breakdown ?
Nervous breakdown and mental breakdown are very outdated terms still used by the lay person typically describing emotional or physical stress that makes someone unable to function in day-to-day life.
Though once used as umbrella term for a wide range of mental illnesses, mental health professionals do not use the term “nervous breakdown” or “mental breakdown” or “emotional breakdown” to describe any specific medical or psychiatric condition. There is no such diagnosis in the DSM-V nor the ICD-10 .
- The symptoms of a so-called “nervous breakdown” vary widely between individuals.
- Medically speaking, there is no such thing as a “nervous breakdown”.
- Treatment for a nervous or “mental breakdown” depends on the cause or multi-causes and risk factors (i.e. etiologies).
Nonetheless, a so-called “nervous breakdown” remains as a presentation underlying many mental health conditions, such as depression , anxiety, psychosis, or post-traumatic stress disorder (PTSD).
The signs and symptoms of what some people may still call a “nervous breakdown” depend on the underlying medical and/or psychiatric condition.
Diagnosis of a “Nervous Breakdown”
It is no longer a recognized medical term, so, technically, there is no way to diagnose using the term: “nervous breakdown” or “emotional breakdown” .
Doctors of mental health: Clinical Psychologists and Psychiatrists will try to identify contributing causes and/or medical problems that may be contributing etiologies to the so-called “nervous breakdown”. These doctors will ask questions about symptoms and signs, conduct a BioPsychoSocial examination, review an individual’s medical history, and order tests.
18 Common Signs and Symptoms
Since it is not associated with any specific medical condition, a nervous or mental breakdown does not have any defined symptoms aside from difficulty or inability to function “normally.”
What it takes for a person to be considered “fully functioning” differs across cultures, religions or belief systems, and even families.
However, there are 18 common signs and symptoms (some or all) that are often a reported by the lay person when they state they are having a “nervous or mental breakdown”:
- Feeling anxious, depressed, fearful, irritable
- Feeling helpless, hopeless, despair
- Negative ruminative binge thinking
- Social withdrawal or avoiding normal social situations (i.e isolation)
- Missing work, appointments, calling in sick
- Dysregulated sleep patterns, sleeping too much (hypersomnia) or difficulty falling a sleep or staying a sleep (insomnia)
- Loss of appetite, overeating, or unhealthy eating
- Lack hygiene and grooming, often due to people forgetting or not being motivated to clean and groom oneself.
- Difficulty focusing, impaired attention, and/ or remembering recent events or recent conversations.
- Feeling frequently emotionally drained and physically exhausted
- Impaired of motivation and lack of interest in things
- Unable to get enjoyment or fulfillment from things that normally bring joy or satisfaction (i.e. anhedonia)
- Unexplained general body aches and pains
- Difficulty getting along with or tolerating other people
- suicidal thoughts or thinking about harming oneself
- Lack of interest in sex and changes in menstrual cycle
- Moving or speaking more slowly than normal
- Traumatic flashbacks, severe nightmares, and fight-flight-freeze symptoms, such as racing heartbeat, dry mouth, and sweating, when there is no threat or danger
In extreme or untreated cases, especially when related to mental health conditions associated with psychosis , symptoms may also include hallucinations, paranoia, delusions, and lack of insight.
Treatment, Intervention, and Prevention of a “Nervous BreakDown” or “Mental BreakDown”
There are a few things that may help reduce symptoms of emotional breakdown and physical stress. Additionally, most of the treatment option interventions for a nervous breakdown also help prevent the condition.
Common treatment and prevention strategies for a nervous breakdown include:
- Seek psychotherapy with a Clinical Psychologist
- Reduce, avoid, or resolve sources of stressors, such as conflicts at home or workplace demands
- Deep breathing and meditation to support mental and physical relaxation.
- yoga and tai chi that promote gentle stretching or movement coupled with controlled breathing
- Exercise daily at least 30 minutes of moderate-intensity.
- Spend time outside in nature or finding hobbies that encourage going outdoors
- Set up healthy hygiene, sleeping, and eating schedules.
- Create a distraction-free sleeping environment to encourage quality sleep
- Avoid the excessive use of caffeine, alcohol, and nicotine.
- Avoid junk food (processed food) and eat clean (fruits & vegetables).
- Take multivitamin and drink plenty of electrolyte water and drink probiotics (e.g. Kombucha) daily.
- Avoid the use of illicit drugs
Causes and risk factors of nervous or “emotional breakdown”
Anything that causes more emotional and physical stress than the body and mind can handle can lead to a nervous breakdown or trigger an underlying medical condition. They are causative and correlational MindBody.
There are certain situations, genetic factors, and experiences that are more commonly associated with nervous or mental breakdowns than others.
Causes and risk factors for “nervous break down” include:
- extreme grief
- traumatizing experiences
- an abusive relationship
- jobs involving high-stress situations
- jobs associated with emotional burnout
- family history of mental health conditions
- severe personal isolation
- traumatizing and unrelenting stress
- severe social conflict, especially if impacting work and home life
- severe or chronic medical conditions or physical injuries that also affect emotional health
When to See a Doctor who Specializes in Mental Health
It is a good idea to talk with a doctor (psychiatrist and clinical psychologist) who specializes in mental health anytime physical or emotional stress interferes with day-to-day life, routines, or activities. Early intervention is key. Prevention is also key.
However, often people experiencing so-called “nervous breakdown” are not able to recognize the extent of their symptoms or that they may need help.
Unfortunately, many people are reluctant to seek outside help for mental conditions out of fear that they will be judged (i.e. Stigma).
They may also think that what is happening to them is somehow their fault, or that there are no treatment options available. However, this is not true.
If a loved one, friend, or roommate is showing several of the signs of a “nervous breakdown”, they should be encouraged to seek mental health assessment by a psychiatrist or clinical psychologist and be provided the support to do so.
Shawna Freshwater, PhD
Hi, I am Dr. Shawna Freshwater, a PhD licensed Clinical Psychologist, Neuropsychologist, and Holistic Practitioner. ** I provide Psychotherapy, Coaching, Healing, Diagnostic testing & Mental Health Check-ups. ** I meet the needs of my patients and clients that are confidential and convenient to their schedule. ** I offer Remote / Online secure interactive video conferencing to USA residents and International clients. ** I also provide Concierge services at your home, office, or private location of your choice if you reside in South Florida Major Cities. ***Please see my website for more information about my credentials and areas of expertise. www.SpaciousTherapy.com Thank you. Dr. Freshwater
Thank you Dr. Freshwater I appreciate so much the comprehensive information provided. You have quite a library of articles in your Blog section. Thank you for providing so much free information.
Just because the medical community removes the word for a condition from its nomenclature does not mean the condition no longer can occur in persons. I am 70 years old and experienced a neurological event in the hospital back in 1972, for which I am still recovering. That is, I have been recovering for over 48 years. This neurological event was produced by a tragic collapse of my relationship with my psychiatrist due to his breaking of the transference that I had established with him. For some reason, of which I still do not know , he suddenly broke this transference during a session relating to a personal problem that I was addressing with him. This transference was required to support me during time of great personal conflict involving my parents. I was hospitalized immediately after the transference break. I experienced the neurological event while being escorted into the hospital. I will not describe the quality of the experience here in my comment ; however I would like to put forth my understanding of the nature of that neurological event. First , I have earned a B.A. in Physics in college, and was educated in the methods of research. The transference was needed to contain an intrusion into my life, at the age of 22 years, of childhood trauma that I had experienced at a very early age. The transference , as it were, was operating to defend against this intrusion, keeping it under. The sudden breaking of this transference resulted in the sudden onrush of this trauma into my consciousness. It resulted in a massive reordering of the neurological pathways in certain areas of my brain. Over the past 48 years, these pathways have been slowly been reordered through therapy and a very close personal relationship with my God. After having studied the nature of my recovery process in great detail, I have come to understand that the words “nervous breakdown”are entirely appropriate in describing my neurological event. The normal neural connections in areas of my conscienceness were “broken down” and replaced with a very disordered array of neural connections which contain the elements of the trauma mixed with a normal. consciousness. True, psychotic episodes do occur in people, and result in a “breakdown” in their ability to function. However, after about 6 months from the onset of the neurological event, I was functioning pretty much normally on the outside–working and relating to people pretty much normally. However, my mental and emotional life was filled with a hellish experience, for which there are no words. It wasn’t until recently that enough of my brain has been reordered to a normal state that I am again beginning to feel normal and healthy, my thoughts free of the elements of the trauma that had so devastatingly intruded into my brain and life. I would like to end this comment with my observation that I have met others who I instinctively knew had experienced a similar neurological event in their lives . Don’t assume that the phrase”nervous breakdown” does not faithfully describe serious mental and emotional states of damage in the brains and lived of others. Thank you for giving me the opportunity to share my experiences regarding this tragic event in my life.
Sincerely, Paul
Leave a Comment Cancel Reply
How much is a PhD Worth?

I recently helped conduct the statistical analysis of the UPA 2009 salary survey [pdf] , and used this opportunity to look into the data to see if I could calculate how much a PhD affects salaries in this profession.
The dataset contains salary information for a wide range of jobs in the profession—usability engineers, designers, managers and information architects.
The vast majority of the data comes from North America and the UK. According to the salary survey data, around 10% of the usability profession has a PhD. I suspect a much larger percentage probably wonders if a PhD pays off financially.
Regression Analysis
To help answer that question I used a statistical technique called regression analysis. Regression analysis allows you to see which combination of variables best predicts some outcome variable, called the dependent variable. We will use salary, converted into US dollars as the dependent variable. Although there are many variables that can affect salary, there are only a few that have significant predictive power (this is true of regression analysis in general).
There are several variables collected in the salary survey: gender, country, job title, techniques performed on the job, and software tools used to name a few. The variable that has the largest impact on salary is years of experience. That shouldn’t be too surprising. We would expect that with more experience you’ll have a larger salary. The next two most important variables that have the greatest impact were being a manager and having a PhD. Surprisingly, having a Master’s degree didn’t make a significant contribution over having a Bachelor’s degree. Roughly 48% have Masters and 37% have Bachelors as their highest degrees.
With regression analysis, each added variable must provide more information than what is contained in the other variables. So being a manager (or not) and having a PhD tells us more than just the total years of experience.
Just knowing the years of experience explains (accounts for) about 28% of the variation in salaries. Adding the variables of manager and PhD adds another 4 percentage points. That means knowing the years of experience, whether you are a manager and if you have a PhD can explain about 1/3 of the differences in salaries (Adjusted R-squared = 31.6%). The other 68% is due to other factors such as individual merit, company differences, and geographic differences, as well as many unknown factors.
That may seem like a lot of unknown variation (68%), but in the world of behavioral science 31% of explaining power is a lot. As a point of reference, the SAT (the high-stakes college entrance exam taken in the US) and high-school grades together explain about 36% of first year college performance (in case you wondered).
The combination of variables that best predicts salary (called the regression equation) is:
To use the regression equation we plug in the values for the variables to get a predicted salary. Both PhD and Manager are indicator (or dummy) variables, for which you just insert 1’s or 0’s to represent their absence or presence.
For example, if you have 5 years of experience, don’t have a PhD and are not a manager, your predicted salary is $52,484 + $2,941(5) + $16,880(0) + $11,108 (0) = $67,189.
Someone with the same experience but with a PhD would have $16,880 more dollars or $84,069. Someone without a PhD but who is a manager with 10 years of experience would expect to make around $93,002.
We can see a few things from the regression equation.
- A year of experience is worth about $3k in the usability profession.
- Starting salaries (0 years of experience, no PhD, and not being a manager) are around $52k.
- Having a PhD is worth almost $17k more per year than someone with the same amount of experience.
- Being a manager nets you about $11k more per year.
For all their predictive power, regression equations have a tendency to be heavily influenced by a few outliers in a dataset. One therefore needs to interpret the coefficients as reasonable approximations as opposed to immutable numbers. For that reason it is helpful to provide 95% confidence intervals around each regression coefficient. In so doing, we have the following confidence intervals:
Table 1: 2009 Salary regression coefficients 95% Confidence Interval boundaries.
The confidence intervals tell us that if we were to have data on all professionals in the usability profession, we’d expect a PhD to add, on average, between $11.5 and $22.4k to a salary. Keep in mind that this is about the average salary based on these factors. It does not mean that you cannot earn a lot more than this amount because of a PhD, it just means that on average a PhD will contribute around $17k more per year.
2005 Salary Data vs. 2009 Salary Data
As an additional check on the stability of this estimate of the value of a PhD, I also examined the 2005 Salary survey data. In 2005, certainly a different economic climate than 2009, the estimates are strikingly similar. The 2005 regression equation is:
Table 2: 2005 Salary regression coefficients 95% Confidence Interval boundaries.
Figure 1 (below) shows the mean and 95% confidence intervals for the 2005 and 2009 data. There was some fluctuation in the data with a bit more money going to PhD’s in 2009 than 2005 and a bit less for managers. The large overlap in the confidence intervals suggests that much of the fluctuation is due to the random variability of the sample.So how many dollars is a PhD worth? Our best guess is about $17k per year. If we need a firm estimate, we can be 95% sure it’s worth at least $12k. Over a career $12-17k per year can add up, but is it worth it financially?
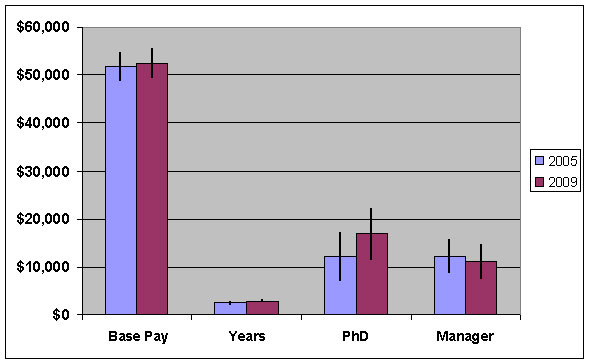
Is a PhD worth it financially?
The education and experience garnered from a PhD is undoubtedly valuable in other ways and you’re in an elite group in this profession. But does it pay off financially? We can use the data here to get a rough idea. There is a 5-figure annual premium for PhD’s, but there is also an opportunity cost assuming you pursue the degree full time and delay entrance into the usability profession. We’ll assume the PhD costs nothing (all expenses paid for by the school), which is of course a big assumption. Let’s also assume it takes 5 years to complete a PhD after completing a bachelor’s degree. If you had skipped the extra years at school and took a job right after getting your bachelor’s degree, then you would have forgone around $50k per year, plus the $3k annual increase from your experience. After 5 years, the baccalaureate usability professional would have made approximately $292k—which is the opportunity cost.
Upon entering the workforce, with PhD in hand, you immediately get a higher pay of around $68k, but you’re well behind the bachelor. Assuming you slog it out in the profession (and we’re all still around in 25 years) you’d never quite catch up because the premium of $17k becomes a smaller and smaller proportion of the lifetime earnings. To help make up the difference the PhD perhaps should consider becoming a manager, although even this wouldn’t be enough. Another alternative is to consider pursuing a PhD part-time where you don’t have to forgo a full-salary (especially if any tuition is offset by an employer).
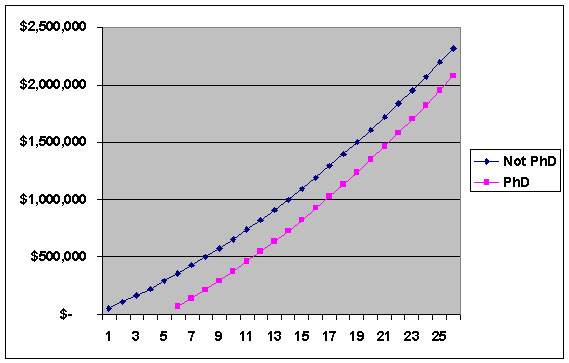
I haven’t met a PhD in the field who regrets their commitment and the long hours in the library with drunken undergraduates. A PhD opens doors to academic positions (where it is usually required) and may even help you get a job faster. I do know many who have or had considered pursuing a PhD full-time and wondered if they could justify it financially. Individual differences will play a large role in compensation, but the data here suggests that on average a full-time PhD should be pursued for more than just financial reasons.
Deployed Military Mental Health, Suicidality + Prevention + My Mental Breakdown Manic in Miami
- Mental Health
SSG Johan Tocre helps us understand mental breakdowns from stress (w me as current example), military operational + combat stress, his special Warrior Fitness Project, a mental health program for deployed military, suicide + suicidality, PTSD, MH preventative measures + long term recovery. (00:00) intro (00:37) my mental breakdown: got acute stress? (05:39) military operational and combat stress (09:43) Johan’s deployed military service mental health program (20:39) sexual assault in the military (21:51) mental illness + suicidality in the military (24:21) suicide/ideation, suicide prevention + techniques (28:00) efficacy of long term outcomes in military PTSD + stress --- Send in a voice message: https://podcasters.spotify.com/pod/show/manicinmiami/message
- Episode Website
- More Episodes
- Holly Hurricane

IMAGES
VIDEO
COMMENTS
More than 40% of PhD students met the criteria for moderate to severe depression or anxiety. In contrast, 32% of working professionals met these criteria for depression, and 26% for anxiety. The ...
2. Feeling hopeless, guilty, and worthless. Although at some point, many PhD students and postdocs will be made to feel like they are worthless, if this becomes a regular occurrence, it is time to take note. This may be combined with a feeling of guilt and worthlessness. It is important to remember your value as a PhD.
At that time, 29% of 5,700 respondents listed their mental health as an area of concern — and just under half of those had sought help for anxiety or depression caused by their PhD study. Things ...
Isolation within the PhD was compounded by isolation from one's personal relationships. This personal isolation was first physical, in which the laborious nature of the PhD acted as a catalyst for the breakdown of pre-existing relationships . Moreover, DRs also experienced a sense of psychological detachment [45, 74]. Thus, the experience of ...
I've seen PhD students with depression, sleep issues, eating disorders, and thoughts of suicide. Mental health in academia is an issue that needs to be addressed
Mental health problems among graduate students in doctoral degree programs have received increasing attention 1,2,3,4.Ph.D. students (and students completing equivalent degrees, such as the Sc.D ...
The wellbeing and mental health of PhD students is a subject that we must continue to talk about and reflect on. However, these conversations need to happen in a way that considers the evidence ...
Doing a PhD - Student Depression, anxiety, and stress. Among researchers, PhD student mental health is perhaps the most under pressure. The CACTUS Mental Health Survey 2020 Summary Report 6 notes that PhD students are consistently the most likely to report feelings of being overwhelmed. PhD students are usually expected to learn new concepts ...
So, I think the breakdown of that link between my actions and the outcome, that was hard." ... "The Mental Health of PhD Researchers," 2019; Puri, 2019), there is a lack of information about how specific aspects of science PhD programs affect students with depression. This is the first study to explicitly investigate which particular ...
Forty-two percent of PhD students agreed with the statement that "developing a mental-health problem during your PhD is the norm". The narrative that mental-health problems are just a part of ...
These are among the top concerns for Ph.D. students, according to a new survey by Nature. By Colleen Flaherty. Nature. More than a third of Ph.D. students have sought help for anxiety or depression caused by Ph.D. study, according to results of a global survey of 6,300 students from Nature. Thirty-six percent is a very large share, considering ...
25. It can be incredibly difficult for a student to discuss any sort of health issue with his/her advisor or committee members and yet doing so can make all the difference. Personally, I left my PhD program after two years rather than discuss my ongoing health problems with my advisor. I deeply regret that decision.
tl;dr young doctoral student having a mental breakdown. List of contents: Introduction. 1. impostor 2. teaching 3. money 4. supervisor 5. attention span 6. bipolar. Conclusions and begging for a good word. I'm [26F] in my second year of PhD studies in banking at the best university in my country (somewhere over the rainbow... actually in Europe).
The PhD degree is a research-oriented doctoral degree. In the first two years, students take core courses in the Departments of Mental Health, Biostatistics, and Epidemiology, in research ethics, and attend weekly department seminars. Students must complete a written comprehensive exam (in January of their second year), a preliminary exam, two ...
PhD in chemistry, Bangor University, Wales "In 2010 I started a PhD in chemistry. A year on, and the pressure began to build, reaching the point where I had a nervous breakdown.
A nervous or mental breakdown does not have any defined symptoms, aside from difficulty or inability to function "normally." ... Medically reviewed by Marney A. White, PhD, MS, Psychology ...
One in five of the graduate students who responded to Nature's 2019 global PhD survey reported ... of being bullied caused a mental breakdown, and led to the collapse of his personal ...
Mental breakdown would stand for a blackout where you transiently forget everything you know due to being overly nervous. Likewise, in Ireland, where I did my PhD, if your supervisor allows you to defend your thesis it would take unlikely catastrophic circumstances to fail the actual examination.
Mental breakdown+1yr break after 1yr of PhD. I got into a beautiful lab in China two years ago. Been a year of being at the only international lab with international students. I obviously felt extremely out of place on campus and to add covid on top of it. I have severe body image issues and my meds for the mental health issues made me put on a ...
mental breakdown or. phd candidate here writing dissertation and losing their mind. i had a mental breakdown weeks ago and, although i'm back on track with my dissertation, i disappeared from my part-time job because of it. now i'm getting back and don't know what to say to my boss. i'd really like to avoid going into the specifics, but how ...
Nervous breakdown and mental breakdown are very outdated terms still used by the lay person typically describing emotional or physical stress that makes someone unable to function in day-to-day life. Though once used as umbrella term for a wide range of mental illnesses, mental health professionals do not use the term "nervous breakdown" or ...
A PhD is worth about $17k per year. We can see a few things from the regression equation. A year of experience is worth about $3k in the usability profession. Starting salaries (0 years of experience, no PhD, and not being a manager) are around $52k. Having a PhD is worth almost $17k more per year than someone with the same amount of experience ...
SSG Johan Tocre helps us understand mental breakdowns from stress (w me as current example), military operational + combat stress, his special Warrior Fitness Project, a mental health program for deployed military, suicide + suicidality, PTSD, MH preventative measures + long term recovery. (00:00) intro (00:37) my mental breakdown: got acute ...