- Open access
- Published: 28 March 2024

Medical student wellbeing during COVID-19: a qualitative study of challenges, coping strategies, and sources of support
- Helen M West ORCID: orcid.org/0000-0001-8712-5890 1 ,
- Luke Flain ORCID: orcid.org/0000-0001-7296-6304 2 ,
- Rowan M Davies 3 , 4 ,
- Benjamin Shelley 3 , 5 &
- Oscar T Edginton ORCID: orcid.org/0000-0001-5298-9402 3 , 6
BMC Psychology volume 12 , Article number: 179 ( 2024 ) Cite this article
25 Accesses
Metrics details
Medical students face challenges to their mental wellbeing and have a high prevalence of mental health problems. During training, they are expected to develop strategies for dealing with stress. This study investigated factors medical students perceived as draining and replenishing during COVID-19, using the ‘coping reservoir’ model of wellbeing.
In synchronous interactive pre-recorded webinars, 78 fourth-year medical students in the UK responded to reflective prompts. Participants wrote open-text comments on a Padlet site. Responses were analysed using reflexive thematic analysis.
Analysis identified five themes. COVID-19 exacerbated academic pressures, while reducing the strategies available to cope with stress. Relational connections with family and friends were affected by the pandemic, leading to isolation and reliance on housemates for informal support. Relationships with patients were adversely affected by masks and telephone consultations, however attending placement was protective for some students’ wellbeing. Experiences of formal support were generally positive, but some students experienced attitudinal and practical barriers.
Conclusions
This study used a novel methodology to elicit medical students’ reflections on their mental wellbeing during COVID-19. Our findings reinforce and extend the ‘coping reservoir’ model, increasing our understanding of factors that contribute to resilience or burnout. Many stressors that medical students typically face were exacerbated during COVID-19, and their access to coping strategies and support were restricted. The changes to relationships with family, friends, patients, and staff resulted in reduced support and isolation. Recognising the importance of relational connections upon medical students’ mental wellbeing can inform future support.
Peer Review reports
Medical students are known to experience high levels of stress, anxiety, depression and burnout due to the nature, intensity and length of their course [ 1 ]. Medical students are apprehensive about seeking support for their mental wellbeing due to perceived stigma and concerns about facing fitness to practice proceedings [ 2 ], increasing their vulnerability to poor mental health.
Research has identified that the stressors medical students experience include a demanding workload, maintaining work–life balance, relationships, personal life events, pressure to succeed, finances, administrative issues, career uncertainty, pressure around assessments, ethical concerns, and exposure to patient death [ 3 , 4 ]. In March 2020, the COVID-19 pandemic introduced additional stressors into medical students’ lives. These included sudden alterations to clinical placements, the delivery of online teaching, uncertainty around exams and progression, ambiguity regarding adequate Personal Protective Equipment (PPE), fear of infection, and increased exposure to death and dying [ 5 , 6 ]. Systematic reviews have reported elevated levels of anxiety, depression and stress among medical students during COVID-19 [ 7 ] and that the prevalence of depression and anxiety during COVID-19 was higher among medical students than in the general population or healthcare workers [ 8 ].
While training, medical students are expected to develop awareness of personal mental wellbeing and learn healthy coping strategies for dealing with stress [ 9 ]. Developing adaptive methods of self-care and stress reduction is beneficial both while studying medicine, and in a doctor’s future career. Protecting and promoting psychological wellbeing has the potential to improve medical students’ academic attainment, as well as their physical and mental wellbeing [ 10 ], and it is therefore important for medical educators to consider how mental wellbeing is fostered. Feeling emotionally supported while at medical school reduces the risk of psychological distress and burnout, and is related to whether students contemplate dropping out of medical training [ 11 ]. In their systematic narrative review of support systems for medical students during COVID-19, Ardekani et al. [ 12 ] propose a framework incorporating four levels: policies that promote a supportive culture and environment, active support for students at higher risk of mental health problems, screening for support needs, and provision for students wishing to access support. This emphasis on preventative strategies aligns with discussions of trauma-informed approaches to medical education, which aim to support student learning and prevent harm to mental wellbeing [ 13 ]. Dunn et al. [ 14 ] proposed a ‘coping reservoir’ model to conceptualise the factors that deplete and restore medical students’ mental wellbeing (Fig. 1 ). This reservoir is drained and filled repeatedly, as a student faces demands for their time, energy, and cognitive and emotional resources. This dynamic process leads to positive or negative outcomes such as resilience or burnout.
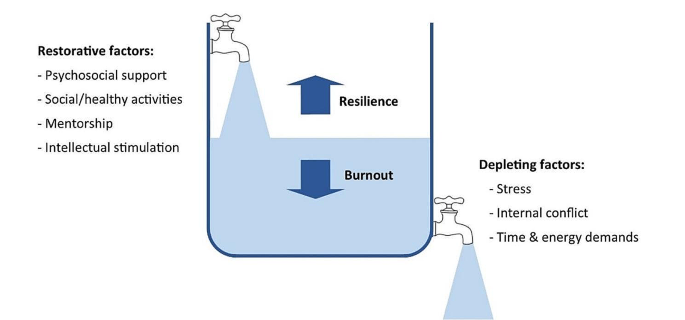
Coping reservoir model– adapted from Dunn et al. [ 14 ], with permission from the authors and Springer Nature
At present we have limited evidence to indicate why medical students’ mental wellbeing was so profoundly affected by COVID-19 and whether students developed coping strategies that enhanced their resilience, as suggested by Kelly et al. [ 15 ]. This study therefore sought to conceptualise the challenges medical students experienced during COVID-19, the coping strategies they developed in response to these stressors, and the supportive measures they valued. The ‘coping reservoir’ model [ 14 ] was chosen as the conceptual framework for this study because it includes both restorative and depleting influences. Understanding the factors that mediate medical students’ mental wellbeing will enable the development of interventions and support that are effective during crises such as the pandemic and more generally.
Methodology
This research study is based on a critical realist paradigm, recognising that our experience of reality is socially located [ 16 ]. Participant responses were understood to represent a shared understanding of that reality, acknowledging the social constructivist position that subjective meanings are formed through social norms and interactions with others, including while participating in this study. It also draws on hermeneutic phenomenology in aiming to interpret everyday experienced meanings for medical students during COVID-19 [ 17 ]. The use of an e-learning environment demonstrates an application of connectivism [ 18 ], a learning theory in which students participate in technological enabled networks. We recognise that meaning is co-constructed by the webinar content, prompts, ‘coping reservoir’ framework and through the process of analysis.
The multidisciplinary research team included a psychologist working in medical education, two medical students, and two Foundation level doctors. The team’s direct experience of the phenomenon studied was an important resource throughout the research process, and the researchers regularly reflected on how their subjective experiences and beliefs informed their interpretation of the data. Reflexive thematic analysis was chosen because it provides access to a socially contextualised reality, encompasses both deductive and inductive orientations so that analysis could be informed by the ‘coping reservoir’ while also generating unanticipated insights, and enables actionable outcomes to be produced [ 19 ].
Ethical approval
Approval was granted by the University of Liverpool Institute of Population Health Research Ethics Committee (Reference: 8365).
Participants
Fourth-year medical students at the University of Liverpool were invited to participate in the study during an online webinar in their Palliative Medicine placement. During six webinars between November 2020 and June 2021, 78 out of 113 eligible students participated, giving a response rate of 69%. This was a convenience sample of medical students who had a timetabled session on mental wellbeing. At the time, these medical students were attending clinical placements, however COVID-19 measures in the United Kingdom meant that academic teaching and support was conducted online, travel was limited, and contact with family and friends was restricted.
Students were informed about the study prior to the synchronous interactive pre-recorded webinar and had an opportunity to ask questions. Those who consented to participate accessed a Padlet ( www.padlet.com ) site during the webinar that provided teaching on mental wellbeing, self-care and resilience in the context of palliative medicine. Padlet is a collaborative online platform that hosts customisable virtual bulletin boards. During this recording, participants were asked to write anonymous open-text responses to reflective prompts developed from reviewing the literature (Appendix 1 ), and post these on Padlet. The Padlet board contained an Introduction to the webinar, sections for each prompt, links to references, and signposting to relevant support services. Data files were downloaded to Excel and stored securely, in line with the University of Liverpool Research Data Management Policy.
The research team used the six steps of reflexive thematic analysis to analyse the dataset. This process is described in Table 1 , and the four criteria for trustworthiness in qualitative research proposed by Lincoln and Guba [ 20 ] are outlined in Table 2 . We have used the purposeful approach to reporting thematic analysis recommended by Nowell et al. [ 21 ] and SRQR reporting standards [ 22 ] (Appendix 2 ).
Five themes were identified from the analysis:
COVID-19 exacerbated academic pressures.
COVID-19 affected students’ lifestyles and reduced their ability to cope with stress.
COVID-19 changed relationships with family and friends, which affected mental wellbeing.
COVID-19 changed interactions with patients, with positive and negative effects.
Formal support was valued but seeking it was perceived as more difficult during COVID-19.
COVID-19 exacerbated academic pressures
‘Every day feels the same, it’s hard to find motivation to do anything.’
Many participants reported feeling under chronic academic pressure due to studying medicine. Specific stressors reported were exams, revision, deadlines, workload, specific course requirements, timetables, online learning, placement, and communication from University. Some participants also reported negative effects on their mental wellbeing from feelings of comparison and competition, feeling unproductive, and overthinking.
Massive amounts of work load that feels unachievable.
COVID-19 exacerbated these academic stresses, with online learning and monotony identified as particularly draining. However, other students found online learning beneficial, due to reduced travelling.
I miss being able to see people face to face and zoom is becoming exhausting. My mental wellbeing hasn’t been great recently and I think the effects of the pandemic are slowly beginning to affect me.
I also prefer zoom as it is less tiring than travelling to campus/placement.
Clinical placements provided routine and social interaction. However, with few social interactions outside placement, this became monotonous. A reduction in other commitments helped some students to focus on their academic requirements.
Most social activity only taking place on placement has made every day feel the same.
Some students placed high value on continuing to be productive and achieve academically despite the disruption of a pandemic, potentially to the detriment of their mental wellbeing. Time that felt unproductive was frustrating and draining.
Having a productive day i.e. going for a run and a good amount of work completed in the day.
Unproductive days of revision or on placement.
COVID-19 affected students’ lifestyles and reduced their ability to cope with stress
‘Everyone’s mental well-being decreased as things they used for mental health were no longer available’.
Students often found it difficult to sustain motivation for academic work without the respite of their usual restorative activities challenging.
Not being able to balance work and social life to the same extent makes you resent work and placement more.
The competing demands medical students encounter for their time and energy were repeatedly reported by participants.
Sometimes having to go to placement + travel + study + look after myself is really tough to juggle!
However, removing some of the boundaries around academic contact and structure of extracurricular activities heightened the impact of stressors. Many participants focused on organising and managing their time to cope with this. Students were aware that setting time aside for relaxation, enjoyment, creativity, and entertainment would be beneficial for their wellbeing.
Taking time off on the weekends to watch movies.
However, they found it difficult to prioritise these without feeling guilty or believing they needed to ‘earn’ them, and academic commitments were prioritised over mental wellbeing.
Try to stop feeling guilty for doing something that isn’t medicine. Would like to say I’d do more to increase my mental wellbeing but finals are approaching and that will probably have to take priority for the next few months.
Medical students were generally aware that multiple factors such as physical activity, time with loved ones, spiritual care, nourishment and hobbies had a positive impact on their mental wellbeing. During COVID-19, many of the coping strategies that students had previously found helpful were unavailable.
Initially it improved my mental well-being as I found time to care for myself, but with time I think everyone’s mental well-being decreased as things they used for mental health were no longer available e.g. gym, counselling, seeing friends.
Participants adapted to use coping strategies that remained available during the pandemic. These included walks and time spent outdoors, exercise, journaling, reflection, nutrition, and sleep.
'Running’. ‘Yoga’. ‘Fresh air and walks'.
A few students also reported that they tried to avoid unhelpful coping strategies, such as social media and alcohol.
Not reading the news, not using social media.
Avoiding alcohol as it leads to poor sleep and time wasted.
Many participants commented on increased loneliness, anxiety, low mood, frustration, and somatic symptoms.
Everyone is worn out and demotivated. Feel that as I am feeling low I don’t want to bring others down. ‘Feel a lot more anxious than is normal and also easily annoyed and irritable.’
However, not all students reported that COVID-19 had a negative effect on wellbeing. A small minority responded that their wellbeing had improved in some way.
I think covid-19 has actually helped me become more self reliant in terms of well-being.
COVID-19 changed relationships with family and friends, which affected mental wellbeing
‘Family are a huge support for me and I miss seeing them and the lack of human contact.’
Feeling emotionally supported by family and friends was important for medical students to maintain good mental wellbeing. However, COVID-19 predominantly had a negative impact on these relationships. Restrictions, such as being unable to socialise or travel during lockdowns, led to isolation and poor mental wellbeing.
Not being able to see friends or travel back home to see friends/family there.
Participants frequently reported that spending too much time with people, feeling socially isolated, being unable to see people, or having negative social experiences had an adverse effect on their mental wellbeing. Relationships with housemates were a key source of support for some students. However, the increased intensity in housemate relationships caused tension in some cases, which had a particularly negative effect.
Much more difficult to have relationships with peers and began feeling very isolated. Talk about some of the experiences I’ve had on placement with my housemates. Added strain on my housemates to be the only ones to support me.
Knowing that their peers were experiencing similar stressors helped to normalise common difficulties. The awareness that personal contacts were also struggling sometimes curtailed seeking informal support to avoid being a burden.
Actually discussing difficulties with friends has been most helpful, as it can sometimes feel like you’re the only one struggling, when actually most people are finding this year really difficult. Family and friends, but also don’t want to burden them as I know I can feel overwhelmed if people are always coming to me for negative conversations.
COVID-19 changed interactions with patients, with positive and negative effects
‘With patients there has been limited contact and I miss speaking to patients.’
Some students reported positive effects on relationships with patients, and feeling a sense of purpose in talking to patients when their families were not allowed to visit. Medical students felt a moral responsibility to protect patients and other vulnerable people from infection, which contributed to a reduction in socialising even when not constrained by lockdown.
Talking to patients who can’t get visitors has actually made me feel more useful. Anxiety over giving COVID-19 to patients or elderly relatives.
Students occasionally reported that wearing PPE made interactions with patients more challenging. Students’ contact with patients changed on some placements due to COVID-19, for example replacing in-person appointments with telephone consultations, and they found this challenging and disappointing.
Masks are an impediment to meaningful connections with new people. GP block when I saw no patients due to it all being on the telephone.
Formal support was valued but seeking it was perceived as more difficult during COVID-19
‘Feel a burden on academic and clinical staff/in the way/annoying so tend to just keep to myself.’
Many participants emphasised the primary importance of support from family and friends, and their responses indicated that most had not sought formal support. While staff remained available and created opportunities for students to seek support, factors such as online learning and increased clinical workloads meant that some students found it harder to build supportive relationships with academic and placement staff and felt disconnected from them, which was detrimental for wellbeing and engagement.
Staff have been really helpful on placement but it was clear that in some cases, staff were overwhelmed with the workload created by COVID. Even though academic staff are available having to arrange meetings over zoom rather than face to face to discuss any problem is off putting.
A few students described difficulty knowing what support was available, and identifying when they needed it.
It’s difficult to access support when you’re not sure what is available. Also you may feel your problems aren’t as serious as other people’s so hold off on seeking support.
Formal support provided within the University included meetings with Academic Advisors, the School of Medicine wellbeing team, and University counselling service and mental health advisory team. It was also available from NHS services, such as GPs and psychological therapies. Those who had accessed formal support mostly described positive experiences with services. However, barriers to seeking formal support, such as perceived stigma, practicalities, waiting times for certain services, and concern that it may impact their future career were reported by some participants.
It is good that some services offer appointments that are after 5pm- this makes it more accessible to healthcare students. Had good experience with GPs about mental health personally. Admitting you need help or asking for help would make you look weak. Reassurance should be provided to medical students that accessing the wellbeing team is not detrimental to their degree. If anything it should be marketed as a professional and responsible thing to do.
Some students preferred the convenience of remote access, others found phone or video impersonal and preferred in-person contact.
Students expressed that it was helpful when wellbeing support was integrated with academic systems, for example Academic Advisors or placement supervisors.
My CCT [primary-care led small group teaching] makes sure to ask how we are getting on and how our placements are going, so I think small groups of people with more contact with someone are more useful then large groups over zoom. Someone to speak to on palliative care placement, individual time with supervisor to check how we are doing (wellbeing, mental health) - would be a nice quick checkup.
Participants typically felt able to share openly in an anonymous forum. Reading peers’ comments helped them to see that other students were having similar experiences and challenged unhealthy comparisons.
I definitely shared more than I would have done on a zoom call. I loved this session as it makes you feel like you’re not alone. Reassuring to know that there are others going through similar things as you.
Our findings demonstrate that the COVID-19 pandemic exacerbated the stressors medical students experience, and removed some rewarding elements of learning, while reducing access to pre-existing coping strategies. The results support many aspects of the ‘coping reservoir’ framework [ 14 ]. Findings corroborate the restorative effects of psychosocial support and social/healthy activities such as sleep and physical activity, and the depletion of wellbeing due to time and energy demands, stress, and disruptions relating to the pandemic such as online teaching and limited social interaction. Feeling a sense of purpose, from continuing studying or interactions with patients for example, was restorative for wellbeing. Mentorship and intellectual stimulation were present in the responses, but received less attention than psychosocial support and social/healthy activities. Internal conflict is primarily characterised by Dunn et al. [ 14 ] as ambivalence about pursuing a career in medicine, which was not expressed by participants during the study. However, participants identified that their wellbeing was reduced by feeling unproductive and lacking purpose, feeling guilty about taking time for self-care, competing priorities, and comparison with peers, all of which could be described as forms of internal conflict. Different restorative and draining factors appeared to not be equally weighted by the participants responding to the prompts: some appear to be valued more highly, or rely on other needs being met. Possible explanations are that students may be less likely to find intellectual stimulation and mentorship beneficial if they are experiencing reduced social support or having difficulty sleeping, and internal conflict about pursuing a career in medicine might be overshadowed by more immediate concerns, for example about the pandemic. This prioritisation resembles the relationship between physiological and psychological needs being met and academic success [ 23 ], based on Maslow’s hierarchy of needs [ 24 ]. A revised ‘coping reservoir’ model is shown in Fig. 2 .
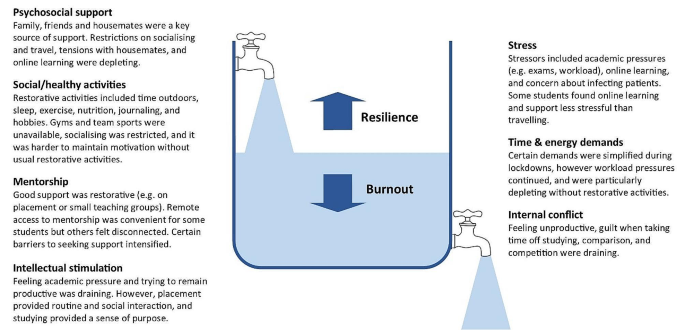
Coping reservoir model - the effects of COVID-19 on restorative and depleting factors for medical students, adapted from Dunn et al. [ 14 ], with permission from the authors and Springer Nature
Relational connections with family, friends, patients, and staff were protective factors for mental wellbeing. Feeling emotionally supported by family and friends is considered especially important for medical students to maintain good mental wellbeing [ 11 ]. These relationships usually mitigate the challenges of medical education [ 25 ], however they were fundamentally affected by the pandemic. Restrictions affecting support from family and friends, and changes to contact with patients on placement, had a negative effect on many participants’ mental wellbeing. Wellbeing support changed during the pandemic, with in-person support temporarily replaced by online consultations due to Government guidelines. Barriers to seeking formal support, such as perceived stigma, practicalities, and concern that it may impact their future career were reported by participants, reflecting previous research [ 26 ]. Despite initiatives to increase and publicise formal support, some students perceived that this was less available and accessible during COVID-19, due to online learning and awareness of the increased workload of clinicians, as described by Rich et al. [ 27 ]. These findings provide further support for the job demand-resources theory [ 28 , 29 ] where key relationships and support provide a protective buffer against the negative effects of challenging work.
In line with previous research, many participants reported feeling under chronic academic pressure while studying medicine [ 3 ]. Our findings indicate that medical students often continued to focus on achievement, productivity and competitiveness, despite the additional pressures of the pandemic. Remaining productive in their studies might have protected some students’ mental wellbeing by providing structure and purpose, however students’ responses primarily reflected the adverse effect this mindset had upon their wellbeing. Some students felt guilty taking time away from studying to relax, which contributes to burnout [ 30 ] , and explicitly prioritised academic achievement over their mental wellbeing.
Students were aware of the factors that have a positive impact on their mental wellbeing, such as physical activity, time with loved ones, spiritual care, nourishment and hobbies [ 31 ]. However, COVID-19 restrictions affected many replenishing factors, such as socialising, team sports, and gyms, and intensified draining factors, such as academic stressors. Students found ways to adapt to the removal of most coping strategies, for example doing home workouts instead of going to the gym, showing how they developed coping strategies that enhanced their resilience [ 15 ]. However, they found it more difficult to mitigate the effect of restrictions on relational connections with peers, patients and staff, and this appears to have had a particularly negative impact on mental wellbeing. While clinical placements provided helpful routine, social interaction and a sense of purpose, some students reported that having few social interactions outside placement became monotonous.
Our findings show that medical students often felt disconnected from peers and academic staff, and reported loneliness, isolation and decreased wellbeing during COVID-19. This corresponds with evidence that many medical students felt isolated [ 32 ], and students in general were at higher risk of loneliness than the general population during COVID-19 lockdowns [ 33 ]. Just as ‘belongingness’ mediates subjective wellbeing among University students [ 34 ], feeling connected and supported acts as a protective buffer for medical students’ psychological wellbeing [ 25 ].
Translation into practice
Based on the themes identified in this study, specific interventions can be recommended to support medical students’ mental wellbeing, summarised in Table 3 . This study provides evidence to support the development of interventions that increase relational connections between medical students, as a method of promoting mental wellbeing and preventing burnout. Our findings highlight the importance of interpersonal relationships and informal support mechanisms, and indicate that medical student wellbeing could be improved by strengthening these. Possible ways to do this include encouraging collaboration over competition, providing sufficient time off to visit family, having a peer mentor network, events that encourage students to meet each other, and wellbeing sessions that combine socialising with learning relaxation and mindfulness techniques. Students could be supported in their interactions with patients and peers by embedding reflective practice such as placement debrief sessions, Schwartz rounds [ 35 ] or Balint groups [ 36 ], and simulated communication workshops for difficult situations.
Experiencing guilt [ 30 ] and competition [ 4 ] while studying medicine are consistently recognised as contributing to distress and burnout, so interventions targeting these could improve mental wellbeing. Based on the responses from students, curriculum-based measures to protect mental wellbeing include manageable workloads, supportive learning environments, cultivating students’ sense of purpose, and encouraging taking breaks from studying without guilt. Normalising sharing of difficulties and regularly including content within the curriculum on self-care and stress reduction would improve mental wellbeing.
In aiming to reduce psychological distress among medical students, it is important that promotion of individual self-care is accompanied by reducing institutional stressors [ 11 , 29 ]. While the exploration of individual factors is important, such as promoting healthy lifestyle habits, reflection, time management, and mindset changes, this should not detract from addressing factors within the culture, learning and work environment that diminish mental wellbeing [ 37 ]. Heath et al. [ 38 ] propose a pro-active, multi-faceted approach, incorporating preventative strategies, organisational justice, individual strategies and organisational strategies to support resilience in healthcare workers. Similarly, trauma-informed medical education practices [ 13 ] involve individual and institutional strategies to promote student wellbeing.
Students favoured formal support that was responsive, individualised, and accessible. For example, integrating conversations about wellbeing into routine academic systems, and accommodating in-person and remote access to support. There has been increased awareness of the wellbeing needs of medical students in recent years, especially since the start of the pandemic, which has led to improvements in many of these areas, as reported in reviews by Ardekani et al. [ 12 ] and Klein and McCarthy [ 39 ]. Continuing to address stigma around mental health difficulties and embedding discussions around wellbeing in the curriculum are crucial for medical students to be able to seek appropriate support.
Strengths & limitations
By using qualitative open-text responses, rather than enforcing preconceived categories, this study captured students’ lived experience and priorities [ 4 , 31 ]. This increased the salience and depth of responses and generated categories of responses beyond the existing evidence, which is particularly important given the unprecedented experiences of COVID-19. Several strategies were used to establish rigour and trustworthiness, based on the four criteria proposed by Lincoln and Guba [ 20 ] (Table 2 ). These included the active involvement of medical students and recent medical graduates in data analysis and the development of themes, increasing the credibility of the research findings.
Potential limitations of the study are that participants may have been primed to think about certain aspects of wellbeing due to data being collected during a webinar delivered by medical educators including the lead author at the start of their palliative medicine placement, and the choice of prompts. Data was collected during the COVID-19 pandemic, and therefore represents fourth year medical students’ views in specific and unusual circumstances. Information on this context is provided to enable the reader to evaluate whether the findings have transferability to their setting. Responses were visible to others in the group, so participants may have influenced each other to give socially acceptable responses. This process of forming subjective meanings through social interactions is recognised as part of the construction of a shared understanding of reality, and we therefore view it as an inherent feature of this methodology rather than a hindrance. Feedback on the webinar indicated that students benefitted from this process of collective meaning-making. Similarly, researcher subjectivity is viewed as a contextual resource for knowledge generation in reflexive thematic analysis, rather than a limitation to be managed [ 19 ]. The study design meant that different demographic groups could not be compared.
Padlet provided a novel and acceptable method of data collection, offering researchers and educators the potential benefits of an anonymous forum in which students can see their peers’ responses. The use of an interactive webinar demonstrated a potential application of connectivist pedagogical principles [ 18 ]. Researchers are increasingly using content from online forums for qualitative research [ 40 ], and Padlet has been extensively used as an educational tool. However, to the authors’ knowledge, Padlet has not previously been used as a data collection platform for qualitative research. Allowing anonymity carried the risk of students posting comments that were inappropriate or unprofessional. However, with appropriate guidance it appeared to engender honesty and reflection, provided a safe and collaborative learning environment, and student feedback was overwhelmingly positive. It would be useful to evaluate the effects of this reflective webinar on medical students’ mental wellbeing, given that it acted as an intervention in addition to a teaching session and research study.
Students were prompted to plan what they would do following the webinar to improve their mental wellbeing. A longitudinal study to determine how students enacted these plans would allow a more detailed investigation of students’ self-care behaviour.
While we hope that the stressors of COVID-19 will not be repeated, this study provides valuable insight into medical students’ mental wellbeing, which can inform support beyond this exceptional time. The lasting impact of the pandemic upon medical education and mental wellbeing remains to be seen. Nevertheless, our findings reinforce and extend the coping reservoir model proposed by Dunn et al. [ 14 ], adding to our understanding of the factors that contribute to resilience or burnout. In particular, it provides evidence for the development of interventions that increase experiences of relational connectedness and belonging, which are likely to act as a buffer against emotional distress among medical students.
Data availability
The datasets generated and analysed during the study are available from the corresponding author on reasonable request.
Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students. JAMA. 2016;316(21):2214.
Article PubMed PubMed Central Google Scholar
Awad F, Awad M, Mattick K, Dieppe P. Mental health in medical students: time to act. Clin Teach. 2019;16(4):312–6.
Article PubMed Google Scholar
Dyrbye LN, Thomas MR, Shanafelt TD. Medical student distress: causes, consequences, and proposed solutions. Mayo Clin Proc. 2005;80(12):1613–22.
Hill MR, Goicochea S, Merlo LJ. In their own words: stressors facing medical students in the millennial generation. Med Educ Online. 2018;23(1):1530558.
Papapanou M, Routsi E, Tsamakis K, Fotis L, Marinos G, Lidoriki I, et al. Medical education challenges and innovations during COVID-19 pandemic. Postgrad Med J. 2021;0:1–7.
Google Scholar
De Andres Crespo M, Claireaux H, Handa AI. Medical students and COVID-19: lessons learnt from the 2020 pandemic. Postgrad Med J. 2021;97(1146):209–10.
Paz DC, Bains MS, Zueger ML, Bandi VR, Kuo VY, Cook K et al. COVID-19 and mental health: a systematic review of international medical student surveys. Front Psychol. 2022;(November):1–13.
Jia Q, Qu Y, Sun H, Huo H, Yin H, You D. Mental health among medical students during COVID-19: a systematic review and meta-analysis. Front Psychol. 2022;13:846789.
General Medical Council. Outcomes for Graduates. London; 2020 https://www.gmc-uk.org/education/standards-guidance-and-curricula/standards-and-outcomes/outcomes-for-graduates [accessed 13 Feb 2024].
Shiralkar MT, Harris TB, Eddins-Folensbee FF, Coverdale JH. A systematic review of stress-management programs for medical students. Acad Psychiatry. 2013;37(3):158–64.
McLuckie A, Matheson KM, Landers AL, Landine J, Novick J, Barrett T, et al. The relationship between psychological distress and perception of emotional support in medical students and residents and implications for educational institutions. Acad Psychiatry. 2018;42(1):41–7.
Ardekani A, Hosseini SA, Tabari P, Rahimian Z, Feili A, Amini M. Student support systems for undergraduate medical students during the COVID-19 pandemic: a systematic narrative review of the literature. BMC Med Educ. 2021;21:352.
Brown T, Berman S, McDaniel K, Radford C, Mehta P, Potter J, et al. Trauma-informed medical education (TIME): advancing curricular content and educational context. Acad Med. 2021;96(5):661–7.
Dunn LB, Iglewicz A, Moutier C. Promoting resilience and preventing burnout. Acad Psychiatry. 2008;32(1):44–53.
Kelly EL, Casola AR, Smith K, Kelly S, Syl M, Cruz D, De. A qualitative analysis of third-year medical students ’ reflection essays regarding the impact of COVID-19 on their education. BMC Med Educ. 2021;21(481).
Pilgrim D. Some implications of critical realism for mental health research. Soc Theory Heal. 2014;12:1–21.
Article Google Scholar
Henriksson C, Friesen N. Introduction. In: Friesen N, Henriksson C, Saevi T, editors. Hermeneutic phenomenology in education. Sense; 2012. pp. 1–17.
Goldie JGS, Connectivism. A knowledge learning theory for the digital age? Med Teach. 2016;38(10):1064–9.
Braun V, Clarke V. Thematic analysis: a practical guide. SAGE Publications Ltd; 2021.
Lincoln YS, Guba EG. Naturalistic inquiry. Beverly Hills, California: SAGE; 1985.
Book Google Scholar
Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving tomeet thetrustworthiness criteria. 2017;16:1–13.
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for Reporting Qualitative Research: Acad Med. 2014;89(9):1245–51.
PubMed Google Scholar
Freitas FA, Leonard LJ. Maslow’s hierarchy of needs and student academic success. Teach Learn Nurs. 2011;6(1):9–13.
Maslow AH. Motivation and personality. 3rd ed. New York: Longman; 1954.
MacArthur KR, Sikorski J. A qualitative analysis of the coping reservoir model of pre-clinical medical student well-being: human connection as making it worth it. BMC Med Educ. 2020;20(1):1–11.
Simpson V, Halpin L, Chalmers K, Joynes V. Exploring well-being: medical students and staff. Clin Teach. 2019;16(4):356–61.
Rich A, Viney R, Silkens M, Griffin A, Medisauskaite A. UK medical students ’ mental health during the COVID-19 pandemic: a qualitative interview study. BMJ Open. 2023;13:e070528.
Bakker AAB, Demerouti E. Job demands-resources theory: taking stock and looking forward. J Occup Health Psychol. 2017;22(3):273–85.
Riley R, Kokab F, Buszewicz M, Gopfert A, Van Hove M, Taylor AK et al. Protective factors and sources of support in the workplace as experienced by UK foundation and junior doctors: a qualitative study. BMJ Open. 2021;11(6).
Greenmyer JR, Montgomery M, Hosford C, Burd M, Miller V, Storandt MH, et al. Guilt and burnout in medical students. Teach Learn Med. 2021;34(1):69–77.
Ayala EE, Omorodion AM, Nmecha D, Winseman JS, Mason HRC. What do medical students do for self-care? A student-centered approach to well-being. Teach Learn Med. 2017;29(3):237–46.
Wurth S, Sader J, Cerutti B, Broers B, Bajwa MN, Carballo S, et al. Medical students’ perceptions and coping strategies during the first wave of the COVID-19 pandemic: studies, clinical implication, and professional identity. BMC Med Educ. 2021;21(1):620.
Bu F, Steptoe A, Fancourt D. Who is lonely in lockdown? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health. 2020;186:31–4.
Arslan G, Loneliness C, Belongingness. Subjective vitality, and psychological adjustment during coronavirus pandemic: development of the college belongingness questionnaire. J Posit Sch Psychol. 2021;5(1):17–31.
Maben J, Taylor C, Dawson J, Leamy M, McCarthy I, Reynolds E et al. A realist informed mixed-methods evaluation of Schwartz center rounds in England. Heal Serv Deliv Res. 2018;6(37).
Monk A, Hind D, Crimlisk H. Balint groups in undergraduate medical education: a systematic review. Psychoanal Psychother. 2018;8734:1–26.
Dyrbye L, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ. 2016;50(1):132–49.
Heath C, Sommerfield A, Von Ungern-Sternberg BS. Resilience strategies to manage psychological distress among healthcare workers during the COVID-19 pandemic: a narrative review. Anaesthesia. 2020;75(10):1364–71.
Klein HJ, McCarthy SM. Student wellness trends and interventions in medical education: a narrative review. Humanit Soc Sci Commun. 2022;9(92).
Smedley RM, Coulson NS. A practical guide to analysing online support forums. Qual Res Psychol. 2021;18(1):76–103.
Download references
Acknowledgements
We would like to thank Dr P Byrne for providing guidance, Mrs A Threlfall and Professor VCT Goddard-Fuller for commenting on drafts, and the medical students who participated in the webinars.
This study was unfunded.
Author information
Authors and affiliations.
Department of Psychology, University of Liverpool, Eleanor Rathbone Building, Bedford Street South, Liverpool, L69 7ZA, UK
Helen M West
Liverpool University Hospitals NHS Foundation Trust, Liverpool, UK
School of Medicine, University of Liverpool, Liverpool, UK
Rowan M Davies, Benjamin Shelley & Oscar T Edginton
Salford Royal NHS Foundation Trust, Manchester, UK
Rowan M Davies
Calderdale and Huddersfield NHS Foundation Trust, West Yorkshire, UK
Benjamin Shelley
Leeds Teaching Hospitals NHS Foundation Trust, Leeds, UK
Oscar T Edginton
You can also search for this author in PubMed Google Scholar
Contributions
HMW conceptualised the study and collected the data. HMW, LF, RMD, BS and OTE conducted data analysis. HMW, LF, RMD and OTE wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Correspondence to Helen M West .
Ethics declarations
Ethical approval and consent to participate.
Approval was granted by the University of Liverpool Institute of Population Health Research Ethics Committee (Reference: 8365). Students were fully informed about the study prior to the workshop and had an opportunity to ask questions. Participants provided informed consent, completing an electronic consent form before responding to prompts. The study was conducted in accordance with relevant guidelines and regulations, including the University of Liverpool Research Ethics and Research Data Management Policies, and the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
West, H.M., Flain, L., Davies, R.M. et al. Medical student wellbeing during COVID-19: a qualitative study of challenges, coping strategies, and sources of support. BMC Psychol 12 , 179 (2024). https://doi.org/10.1186/s40359-024-01618-8
Download citation
Received : 12 December 2023
Accepted : 22 February 2024
Published : 28 March 2024
DOI : https://doi.org/10.1186/s40359-024-01618-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Mental wellbeing
- Medical student
- Student doctor
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 23 March 2022
Student wellness trends and interventions in medical education: a narrative review
- Harrison J. Klein 1 &
- Sarah M. McCarthy 1
Humanities and Social Sciences Communications volume 9 , Article number: 92 ( 2022 ) Cite this article
12k Accesses
16 Citations
1 Altmetric
Metrics details
- Science, technology and society
Medical education is a time wrought with personal and professional stressors, posing serious challenges to maintaining student wellness. Extensive research has thus been conducted to identify these stressors and develop practical solutions to alleviate their harmful effects. This narrative review of quantitative and qualitative literature summarizes trends in student wellness and examines interventions deployed by medical schools to ameliorate student distress. Current trends indicate that mental illness, substance use, and burnout are more prevalent in medical students compared to the general population due to excessive academic, personal, and societal stressors. Pass/fail grading systems and longitudinal, collaborative learning approaches with peer support appear to be protective for student wellness. Additionally, maintaining enjoyable hobbies, cultivating social support networks, and developing resiliency decrease distress in medical students on an individual level. Faculty and administrator development is also a necessary component to ensuring student wellness. The COVID-19 pandemic has posed unique challenges to the medical education system and has stimulated unprecedented innovation in educational technology and adaptability. Particularly, the discontinuation of the clinical skill evaluation components for both osteopathic and allopathic students should be a focus of medical student wellness research in the future.
Similar content being viewed by others
Impact of the SARS-CoV-2 pandemic on pediatric subspecialists’ well-being and perception of workplace value
Jeanie L. Gribben, Samuel M. Kase, … Andrea S. Weintraub

Academic burnout among master and doctoral students during the COVID-19 pandemic
Diego Andrade, Icaro J. S. Ribeiro & Orsolya Máté

Online education and the mental health of faculty during the COVID-19 pandemic in Japan
Yosuke Kita, Shoko Yasuda & Claudia Gherghel
Defining student wellness
Defining student wellness has challenged stakeholders throughout the medical education system. The term “wellness” first appeared in literature following World War II, though the concept extends back to Christian ethics of the 19th century that linked physical well-being to moral character (Kirkland, 2014 ). Implicit within these origins of wellness is a responsibility of the individual to contribute to their own well-being. This is reflected in Kirkland’s premise that “each individual can and should strive to achieve a state of optimal functioning” ( 2014 ). Contemporary researchers characterize wellness similarly to the World Health Organization’s (WHO) definition of human health. In the preamble to the WHO’s constitution, health is defined as a “state of complete physical, mental, and social well-being and not merely the absence of disease” (Grad, 2002 ). Wellness can therefore be succinctly defined as self-aware, intentional prevention of distress and promotion of well-being (Kirkland, 2014 ).
Human wellness’s inherent multidimensionality often poses a challenge to quantitative research methods. Most studies thus ultimately measure some combination of indicators for distress and well-being. Addiction, mental disorders, suicidal ideation, and burnout are common indicators of distress assessed through various screening methods (Jackson et al., 2016 ; Moir et al., 2018 ; Dyrbye and Shanafelt, 2016 ). On the contrary, Gallup-Healthways Well-Being Index Composite Score examines well-being across several domains of life, including: life evaluation, emotional health, physical health, healthy behavior, work environment, and basic access. The Well-Being Composite Score thus emphasizes the presence of health rather than absence of disease (Kirkland, 2014 ). Though methodologies and definitions vary across studies and reviews, the fundamental characteristics of wellness appear constant: absence of disease and presence of health. Investigations using this paradigm have identified professional education, particularly medical education, as a time of increased distress and diminished wellness (Dyrbye et al., 2014 ). We have thus undertaken a review of contemporary literature to identify trends in student wellness, as well as the interventions deployed to address such trends. This narrative review outlines the prevalence and contributing factors to mental illness, addiction, and burnout in the medical student population. We then describe several intervention strategies used by medical schools to address student wellness deficits, including: wellness committees, pass-fail (P/F) grading, mindfulness training, curricular alterations, and developing more wellness-aware faculty/administration. In compiling this review, we hope to provide a snapshot of contemporary student wellness that may be used to guide medical schools seeking to improve the student experience during the COVID-19 pandemic and its aftermath.
Mental well-being
As previously mentioned, directly measuring wellness is a challenge in educational research. Therefore, most studies assess wellness of student populations by examining rates of mental illness or distress (Kirkland, 2014 ). Numerous studies have revealed that mental health issues are virtually ubiquitous in the medical education system. Dyrbye and colleagues report that medical school appears to be a peak time for distress in a physician’s training ( 2014 ). Localization of distress to the training process is evidenced by higher rates of depression, fatigue, and suicidal ideation in medical students as compared to age-matched controls from the general population, with these symptoms declining to the same levels as control populations within 5 years after completing post-graduate education (Dyrbye et al., 2014 ). Further, Jackson et al determined that a majority of medical students exhibited either burnout, depressive symptoms, suicidal ideation, alcohol abuse/dependence, or a combination of these factors at the time of survey ( 2016 ). A meta-analysis conducted by Rosenstein and colleagues revealed that 27% of medical students met criteria specifically for depression or depressive symptoms ( 2016 ). This increased prevalence of mental illness is not restricted to medical education. A survey of law students revealed that 17% screened positively for depression, 37% screened positively for anxiety, and 27% screened positively for an eating disorder. These statistics indicate increasing trends of mental illness across graduate education as a whole, rather than medical education alone (Organ et al., 2016 ).
This prolific mental distress can substantially impact medical students’ ability to meet academic demands (Dyrbye et al., 2014 ). As such, substantial research has been conducted investigating factors that contribute to mental illness in an academic setting. Surprisingly, students begin medical school with mental health better than similarly aged peers. However, these roles quickly reverse, with medical student mental health ultimately becoming worse than control populations (Dyrbye and Shanafelt, 2016 ). It seems that medical education may actually select for individuals prone to developing psychological distress (Bergmann et al., 2019 ). Moir et al. report that the majority of medical students are considered Type A individuals, displaying high levels of ambition and competition. Though these qualities facilitate academic success, they also lead to hostility and frustration with challenging situations (Moir et al., 2018 ). Medical students were also found to have high levels of conscientiousness (Moir et al., 2018 ). Conscientiousness is a component of the Big 5 Personality model, which uses the qualities of neuroticism, extraversion, openness, agreeableness, and conscientiousness as the most basic descriptors of an individual’s personality (Shi et al., 2018 ). Conscientiousness is characterized by diligence and careful attention to detail, thus predicting high levels of academic success. However, increased conscientiousness may also exacerbate the likelihood of mental and physical distress due to inordinate demands placed on one’s self (Bergmann et al., 2019 ). Student age was also found to correlate with mental well-being. Younger students were found to approach their studies with dualistic orientations, seeking an explicit, incontrovertible knowledge of medicine. Diagnostic challenges and knowledge gaps ubiquitous in clinical medicine can thus be frustrating to younger students (Lonka et al., 2008 ). It is worth noting that, despite the importance of addressing mental health issues, some authors feel categorizing symptoms of depression and burnout leads to over-medicalization of human suffering and is not useful (Moir et al., 2018 ).
The aforementioned qualities of medical students facilitate development of both maladaptive perfectionism and imposter syndrome, heightening mental wellness concerns in this population (Bubenius and Harendza, 2019 ; Hu et al., 2019 ; Henning et al., 1998 ; Seeliger and Harendza, 2017 ; Thomas and Bigatti, 2020 ). The prevalence of imposter syndrome has been estimated between 22.5–46.6% in medical students, however, the prevalence of perfectionism has proven much more difficult to measure (Thomas and Bigatti, 2020 ). Maladaptive perfectionism is a multifactorial entity encompassing inordinate self-expectations, negative reactions to failure, and a persistent lack of satisfaction in performance (Bubenius and Harendza, 2019 ; Thomas and Bigatti, 2020 ). This emphasis on perfection prevents students from appreciating their vulnerability and thus delays self-recognition of mental distress (Seeliger and Harendza, 2017 ). Not surprisingly, maladaptive perfectionism has thus demonstrated an association with anxiety, depression, bulimia nervosa, anorexia nervosa, and chronic fatigue syndrome (Thomas and Bigatti, 2020 ). The strength of these associations was further demonstrated by Bubenius and Harendza’s use of maladaptive perfectionism as a predictor of depressive symptoms in German medical school applicants ( 2019 ). Imposter syndrome is a phenomenon often associated with maladaptive perfectionism and is characterized by anxiety, lack of self-confidence, depression, and frustration with one’s performance (Clance and Imes, 1978 ). While imposter syndrome bears an uncanny resemblance to perfectionism, the difference lies in imposter syndrome’s characteristic fear of being discovered as undeserving of a place in medical school, regardless of actual accomplishments (Clance and Imes, 1978 ). Imposter syndrome has been associated with a lack of resilience and this, similar to perfectionism, can increase psychological distress (Levant et al., 2020 ). The combined effects of imposter syndrome and maladaptive perfectionism predispose students to mental health issues and thus deserve special attention in studies geared toward well-being interventions. Of note, preliminary work by Chand and colleagues has demonstrated that cognitive behavioral therapy may be especially effective in ameliorating the deleterious effects of maladaptive perfectionism (Chand et al., 2018 ). Treatment for imposter syndrome, however, appears to be a significant gap in wellness literature (Bravata et al., 2020 ).
Deeply intertwined with imposterism and perfectionism is the medical student’s experience of shame. Shame is characterized as a negative emotional response to life events. These life events can take many forms, though personal mistakes within a hostile environment are a common instigator of shame (Bynum et al., 2019 ). Perfectionism and imposter syndrome thus provide a fertile soil of negative self-evaluation in which shame can flourish (Bynum et al., 2020 ). Feelings of shame are further exacerbated by factors within the medical school environment. Mistreatment by colleagues or preceptors, receiving low test scores, underrepresentation within classes, institutional expectations, and social comparison were reported as contributors to shame by medical students in a hermeneutic analysis (Bynum et al., 2021 ). Regardless of origin, shame has been recognized as a “destabilizing emotion,” leading to student isolation, psychological distress, and difficulty with identity formation (Bynum et al., 2021 ). Explorations of shame as a contributor to medical student distress are limited in the current literature. Thus, wellness researchers must dedicate studies to characterizing and preventing this significant, but potentially modifiable, contributor to student distress (Bynum et al., 2019 ).
Medical students’ educational environment can also have a profound impact on mental health, particularly during the early days of training. The transition between college and professional school is marked by anxiety, stress, and financial upheaval. Thus, students may feel more vulnerable than ever as they begin their professional education in a new environment in which they are unaware of available mental health resources, leading to isolation and unnecessary suffering (Organ et al., 2016 ). Even for those aware of these resources, significant stigma still surrounds mental illness in professional education. This is emphasized in Organ et al’s finding that only 50% of law students with mental health issues actually receive professional counseling. Their findings suggest that this reluctance largely stems from fear of professional repercussions if administrators discover a student’s mental health diagnosis (Organ et al., 2016 ). While this study was conducted in law students, Hankir et al found similar trends in both medical students and physicians by examining autobiographical narratives published to combat the stigma against help-seeking behavior (Hankir et al., 2014 ). Hankir and colleagues have elucidated several phenomena that contribute to medical students delaying or even avoiding treatment for mental distress. Self-stigma operates as a powerful deterrent to help-seeking and seems to stem from internalization of society’s expectation that medical students are mentally and physically invincible. This leads to feelings of decreased self-esteem and self-efficacy, as well as fear of stigmatization from the general public (Hankir et al., 2014 ; Fischbein and Bonfine, 2019 ). Rahael Gupta, now a psychiatry resident, brought this stigma to public light as she shared her personal experience with depression during medical school in her short film project entitled “Physicians Connected.” The film, conveyed line-by-line through Gupta’s colleagues at the University of Michigan, highlights the unspoken rule that mental distress is a black mark on a future physician’s career (Gupta, 2018 ). Gupta’s efforts, and those similar, underscore a growing call for public discourse, rather than concealment, of mental well-being within the medical profession. This call is echoed with Robyn Symon’s film “Do No Harm: Exposing the Hippocratic Hoax,” which further explores the toxic culture of medical education that drives physicians and medical students to commit suicide. Both Gupta and Symon highlight the taboo of mental distress within the medical field, which instead prioritizes efficiency and academic success over student and physician well-being. Both films characterize this lack of help-seeking behavior as products of the healthcare system’s toxic structure, rather than individual student distress interacting with a demanding work life (Gupta, 2018 ; Symon 2020 ).
Substance use
In addition to impaired academic performance, mental illness also increases risk for development of substance use disorder in medical students (McLellan, 2017 ). Thus, the pervasiveness of mental illness during medical education warrants careful analysis of substance use patterns in the student population. Alcohol abuse or dependence has already been well documented in the professional education system (Dyrbye and Shanafelt, 2016 ; Organ et al., 2016 ; Jackson et al., 2016 ). Alarmingly, despite 43% of law students reporting a recent occurrence of binge drinking, only 4% had sought professional assistance for alcohol or drug misuse. This trend again highlights significant mental health and addiction stigma throughout the graduate education system (Organ et al., 2016 ). Medical students, and all those in the medical field, may be uniquely affected by this prevalence of substance use. For example, the American Foundation for Suicide Prevention produced a documentary entitled “Struggling in Silence: Physician Depression and Suicide,” which highlights the powerful role that substance use plays in medical student and physician suicide specifically. With a greater knowledge of and access to potentially lethal substances, those in the medical field are at heightened risk for suicide completion, especially with the inhibition-lowering effects of some drugs (AFSP, 2002 ).
Alcohol dependence is of particular concern in medical education due to implications in hindering student career progression and compromised patient safety. Despite this concern, alcohol use is prevalent among medical students. A survey of 855 medical students across 49 schools in the United States revealed that 33.8% of students reported consuming 5 or more drinks in one sitting within the past two weeks, meeting the criteria for binge drinking (Ayala et al., 2017 ). Further, survey responses from 4402 medical students in the U.S. demonstrated that 32.4% met criteria for alcohol abuse/dependence, compared to 15.6% in a control sample of similarly aged but non-medical student counterparts (Jackson et al., 2016 ). The substantial academic stress of a professional education is a clear driving force behind this trend, though several compounding risk factors have been identified. Young males were identified as at an increased risk for alcohol dependence compared to their female colleagues (Jackson et al., 2016 ; Organ et al., 2016 ). Jackson and colleagues further identified that students who were unmarried, diagnosed with a mood disorder, low-income, or burdened with educational debt from professional and undergraduate studies were at increased risk for alcohol dependence ( 2016 ). While ethnicity’s relationship to alcohol use was not explored in medical students, a survey of over 11,000 law students from 15 law schools in 2016 determined that ethnic minorities were more likely to report an increase in drinking whereas Caucasian students were more likely to demonstrate a positive CAGE screening (Organ et al., 2016 ). The CAGE screen is a 4-item questionnaire developed by John Ewing in 1984 to identify drinking problems. The CAGE screen has a 93% sensitivity and 76% specificity for identifying problem drinking whereas alcoholism identification has a sensitivity of 91% and specificity of 77% (Williams, 2014 ). This increased alcohol use in both Caucasian and ethnic minority students demonstrates a need for culturally tailored and inclusive prevention programs.
Though alcohol is the most commonly abused drug amongst medical students, illicit drug use has also been reported at concerning levels. A survey of 36 United States medical schools revealed that approximately one-third of students had used illicit drugs within the past 12 months (Shah et al., 2009 ). Papazisis and colleagues similarly examined illicit drug use in undergraduate medical students in Greece, finding a lifetime substance use rate of ~25% ( 2017 ). Marijuana was the most common illicit drug used in both studies (Shah et al., 2009 ; Papazisis et al., 2017 ). Use of prescription medications without a prescription was also found amongst law students, particularly stimulants such as Ritalin, Adderall, and Concerta (Organ et al., 2016 ). These findings suggest that the competitive culture of graduate education may drive students to engage in recreational drug use, particularly those struggling to meet academic demands or suffering from mental distress.
Student burnout
Burnout was canonically defined by Freudenberger in 1974 as a state of physical and mental exhaustion caused by or related to work activities, often manifesting when heightened professional stress conflicts with personal ideals or expectations (Freudenberger, 1974 ; Rodrigues et al., 2018 ; Baro Vila et al., 2022 ). Though originally a descriptive disorder, burnout is now recognized in the International Classification of Diseases, 10th revision, under code Z73.0 (Lacy and Chan, 2018 ). Burnout is traditionally diagnosed with the Maslach Burnout Inventory, a 22-item questionnaire that characterizes each of the three burnout domains: emotional exhaustion, depersonalization, and personal accomplishment (Dyrbye and Shanafelt, 2016 ). Emotional exhaustion is associated with feelings of being overworked and a subsequent loss of compassion. Depersonalization is characterized by a sense of detachment from colleagues/patients and, when combined with emotional exhaustion, can result in unprofessional behavior. The personal accomplishment domain mainly describes an individual’s feelings of competence and professional satisfaction (Lacy and Chan, 2018 ). In addition to each domain’s unique consequences, burnout domains interact to cause an extinction of motivation when efforts no longer produce desired results (Vidhukumar and Hamza, 2020 ). Approximately 50% of fourth year medical students were found to have burnout when surveyed with the Maslach Burnout Inventory (Dyrbye and Shanafelt, 2016 ). This value holds true internationally according to a survey of medical students conducted in India (Vidhukumar and Hamza, 2020 ). Additionally, burnout increases as training progresses, particularly the depersonalization component (Dyrbye and Shanafelt, 2016 ). Burnout thus increases feelings of callousness towards patients, leading to unprofessional and potentially dangerous conduct. Burnout in medical school also appears to affect specialty choice; burned out individuals were more likely to choose specialties with more controllable lifestyles and higher pay (Dyrbye and Shanafelt, 2016 ). Investigating causes of burnout is thus of utmost importance to understand potential influences on medical student career trajectory and ensuring patient safety.
Identified causes of burnout appear to differ between the years of medical training. Preclinical years are characterized by dissatisfaction with the learning environment and lack of faculty support. Clinical years are characterized by dissatisfaction with the learning environment, clerkship disorganization, and working with cynical or abusive residents and/or attending physicians (Dyrbye and Shanafelt, 2016 ). Reed and colleagues found a positive correlation between the time spent in exams and burnout whereas a negative correlation was observed with increased patient interaction ( 2011 ). Several correlates of burnout outside of medical schools’ learning environments and curricula have also been described, including: female gender, dissatisfaction with career options, non-ethnic minority status, high educational debt, residency competition, expanding knowledge-base, workforce shortage, and stressful events in one’s personal life (Dyrbyre and Shanafelt, 2016 ; Vidhukumar and Hamza, 2020 ). Erosion of social ties during medical education also contributes to the burnout spiral, as socialization is protective against burnout symptoms (Bergmann et al., 2019 ; Busireddy et al., 2017 ). No associations between contact days, time in didactic learning or clinical experiences, and any measure of student well-being and burnout prevalence were found (Reed et al., 2011 ).
Interventions to improve well-being
Medical schools have implemented several interventions to reduce student distress and enhance wellness. Though interventional approaches are varied, researchers have identified salient features common to most successful wellness interventions. For example, Dyrbye and colleagues underline the importance of well-being committees that can liaise between administration, faculty, and students, lessening fear of admonishment for seeking help or acknowledging distress ( 2019 ). Additionally, Moir et al reports that student buy-in is absolutely essential, as disengaged wellness lectures offer little, if any, benefit ( 2016 ). Interventions appear most effective when they are designed to reduce student burdens, rather than adding to the already overwhelming schedule and content of medical school (Busireddy et al., 2017 ). Finally, administrations often pose an obstacle to wellness initiatives, especially those who believe that well-being is of minor importance. This obstacle is reflected by the low prevalence of medical schools with official wellness competencies built into the curriculum (Dyrbye et al., 2019 ). We will now explore some of the specific interventions medical schools have employed to improve student wellness.
Transitioning to a Pass/Fail (P/F) grading scheme is a wellness initiative that has received substantial attention in the United States, especially in light of findings that grade evaluation systems are a larger determinant of student well-being compared to content of educational contact hours (Reed et al., 2011 ; Spring et al., 2011 ). The Mayo Medical School examined the feasibility and effects of P/F grading by introducing the system to first-year medical students in 2006. Rohe and colleagues found that these first-year medical students reported less stress, better overall mood, and greater group cohesion compared to their graded peers. These characteristics persisted into the second year of medical school, even when grading reverted to a traditional 5-level schema (Rohe et al., 2006 ). While critics of P/F grading argue that students will be less motivated to excel academically, evidence suggests that first-year residents from P/F schools performed similarly to residents from graded schools (Rohe et al., 2006 ). Additionally, a P/F system reduces extrinsic motivation and intense competition while increasing cohesion and peer cooperation (Moir et al., 2018 ; Rohe et al., 2006 ). These qualities are essential in the increasingly team-based healthcare landscape. Though transitioning to a P/F system reduced medical student distress during the preclinical years, it is important to note that the transition did not decrease test anxiety for the United States Medical Licensing Exam (USMLE) Step 1 (Williams et al., 2015 ; Rohe et al., 2006 ). Determining test anxiety for USMLE Step 1 will be an active area of research in the face of a new P/F grading for the licensure exam.
Allopathic and osteopathic medical programs are infamous for their academic rigors and intense curricular designs. These curricula are often described as competitive, leisure and socialization-deficient, and requiring exclusive dedication. These characteristics predispose medical students to decreased quality of life (Bergmann et al., 2019 ). As such, altering the curricula of these programs has been investigated as a means to prevent, rather than react to, student distress through a person-in-context perspective (Dyrbye et al., 2005 ; Slavin et al., 2012 ; Slavin et al., 2014 ). It has long been documented that the undergraduate medical curriculum is overflowing with information (D’Eon and Crawford, 2005 ). Rather than identifying salient features for inclusion in courses, medical school faculty often address this surplus of information by cramming unrealistic amounts of information into lectures (D’Eon and Crawford, 2005 ; Dyrbye et al., 2005 ). As mentioned earlier, wellness initiatives are often more effective when they reduce student burdens, rather than adding additional requirements (Busireddy et al., 2017 ). Though this may lead one to believe that shortening curricular hours is an intuitive wellness initiative, this measure only led to workload compression and feelings of being unprepared for clinical practice when used as a unifocal intervention (Dyrbye and Shanafelt 2016 ; Busireddy et al., 2017 ; Dyrbye et al., 2019 ). This continually expanding mass of information thus poses two challenges to wellness initiatives. First, medical students’ schedules are often too consumed by curricular hours to engage in additional wellness programming, especially without an external motivator. Second, the amount of information itself imposes feelings of distress on students, exacerbating the already-stressful nature of medical school and predisposition to mental health issues. Beyond the quantity of curricular hours, delivery and content of those hours is also important to student wellness. Lonka and colleagues found that a collaborative approach to learning increased satisfaction and decreased the perceived workload ( 2008 ). The collaborative environment of problem-based learning may thus offer some improvement to curriculum-induced stress, though current evidence is weak (Camp et al., 1994 ). Incorporating self-care workshops into the curriculum also appears to ameliorate the depersonalization component of burnout (Busireddy et al., 2017 ). In light of these promising results, it follows that the most powerful approach to improving student wellness through curricular restructuring is a multifactorial one. This multifactorial approach is best appreciated in the wellness initiatives within the Vanderbilt University School of Medicine and the Saint Louis University School of Medicine (Drolet and Rodgers, 2010 ; Slavin et al., 2014 ).
The Vanderbilt wellness initiative is composed of three arms: the Advisory College System, the Student Wellness Committee, and Vanderbilt Medical Student LIVE. The Advisory College is composed of both students and faculty that offer personalized advising and mentorship to students within the school. The Student Wellness Committee emphasizes student-led wellness initiatives and serves as an interface with faculty. Lastly, Vanderbilt Medical Student LIVE is an adjunct curriculum that fosters self-care and personal growth amongst the physicians in training (Drolet and Rodgers, 2010 ). The wellness program at the Saint Louis University School of Medicine is structured differently, though shares similar goals. The program entitled Mental Health 3.0 radically, but feasibly and efficiently, altered the structure of the School’s curriculum. Grading was converted to a P/F basis, with only the median exam score and 75 th percentile reported to students. Student contact hours were reduced by 10% during the preclinical curriculum and faculty were advised on how to appropriately identify topics for inclusion in their lectures. Longitudinal electives were instituted following contact hour reduction to encourage student growth and interest identification while forming relationships with fellow students and faculty. These electives were complemented by the formation of five learning communities to further enhance student immersion in areas of interest. Lastly, resilience and mindfulness training was incorporated into the mandatory curriculum while offering an increased number of social events (Slavin et al., 2014 ; Slavin, 2019 ). This wellness initiative was continually expanded and improved to include an early entry and exit to third-year clinical rotations, which minimized stress entering fourth year, and a confidential depression/anxiety tracking system to screen students for worrisome mental health issues (Slavin and Chibnall, 2016 ; Slavin, 2019 ). Comparison between these wellness initiatives reveals that whereas Slavin and colleagues have produced significant declines in student depression, anxiety, and stress with increased group cohesion (Slavin et al., 2014 ; Slavin, 2019 ), the impacts of curricular changes at the Vanderbilt University School of Medicine have not yet been quantified (Drolet and Rodgers, 2010 ). In addition to minimizing student distress, the Mental Health 3.0 program also increased student flourishing (Slavin and Chibnall, 2016 ). The success of Mental Health 3.0 provides strong evidence that diminished medical student well-being is likely a product of multiple factors within the medical learning environment rather than intrinsic student qualities alone (Slavin, 2019 ).
Mindfulness practices have also become increasingly popular as a wellness intervention. Mindfulness is defined as the non-judgmental awareness of one’s own experience with the goal of increasing concentration, insight, and relaxation. Employing mindfulness techniques has been demonstrated to decrease stress and anxiety, though its effects are not as apparent in reducing burnout symptoms (Williams et al., 2015 ). This lack of effect on burnout symptoms may be due to the focus of mindfulness practices, which is on the individual experience rather than improving the structural entities that cause burnout in the first place (Moir et al., 2018 ). Mindfulness practices implemented through peer-support groups in a United States medical school failed to demonstrate improvement in student anxiety, depression, quality of life, or resiliency. Though this may have been due to insufficient peer training, a non-blinded study design, or limited participation, these results lend further support to the need for structural corrections to the medical education system rather than improvement in students’ attitudes or outlooks (Moir et al., 2018 ). This is in contrast to the results obtained when primary care doctors underwent a 52-hour mindfulness training course. Post-course surveys revealed reduced burnout and improved empathy sustained for 3 months post-intervention (Dyrbye and Shanafelt, 2016 ). Comparison of factors contributing to burnout between medical students and practicing clinicians, as well as determining prerequisites for successful implementation of mindfulness programs, may thus be potential areas for research.
Administration and faculty personnel serve as educators and role models for students. Interventions centered on these individuals can thus facilitate a top-down approach to increasing student wellness. A primary concern for German medical students was a lack of coherent information management by faculty with regard to academic expectations, exacerbating the stress of exams and assignments. Solutions offered by students included recording lectures for later viewing and professors providing explicit learning objectives. These students also reported that attendance policies are often too strict and may impede self-care practices, such as utilizing the school counseling system. Proposed solutions were to loosen attendance requirements via a self-reporting absence system (Dederichs et al., 2020 ). Beyond their academic roles, faculty also often serve as mentors to students. The Liaison Committee on Medical Education requires that schools implement a mentoring system for their students, and these mentors are typically medical school faculty. However, Andre et al proposed a vertical mentoring system that complements faculty involvement with senior students in a program entitled “Mentors in Medicine.” This peer-mentoring system was found to be better suited for day-to-day navigation of medical school, while faculty were better suited to offer more long-term career support (Andre et al., 2017 ). Further integration of mentoring to include financial advisors may reduce distress in students with large amounts of educational debt (Dyrbye et al., 2019 ). Faculty commitment to wellness initiatives facilitates the development of communal concern for student wellness, extending beyond the Office of Student Affairs (Slavin et al., 2014 ). Moving forward, faculty and administration will continue to play pivotal roles in student wellness as the medical education system adapts to the technology and challenges of a post-pandemic landscape.
Though a majority of reviewed literature focused on the preclinical years of medical school, important developments have been made in clinical education as well. Dyrbye and Shanafelt found that a longitudinal rotation curriculum, in which students spend several contiguous months at one training site rather than smaller stints at several training sites, facilitates development of meaningful relationships with preceptors, increasing satisfaction and reducing burnout (Dyrbye and Shanafelt, 2016 ). This is congruent with Slavin and Chibnall’s finding that deploying effective wellness initiatives is made difficult by the changing environment of clinical rotations and lack of control over clinician interactions with students (Slavin and Chibnall, 2016 ). Further work by Slavin and Chibnall indicates that negative experiences (e.g., mistreatment) during clinical years are a product of resident burnout, which itself results from toxic healthcare structures and environments (Slavin and Chibnall, 2016 ). For example, residents often experience sleep deprivation, adjustment difficulties, interpersonal conflict, demanding workloads, and a lack of control over their schedule. Interplay between these factors and resident burnout increases likelihood for development of depression and suicidal ideation (Nene and Tadi, 2021 ). These deleterious resident symptoms may then translate to negative interactions with medical students. Improving the medical student experience can thus be facilitated by ameliorating resident burnout. A potential target for resident burnout interventions is resiliency, which has demonstrated a protective effect against burnout (Sheer et al., 2021 ; Nituica et al., 2021 ; Rodrigues et al., 2018 ). For example, implementation of the Gabbe Health and Wellness program, which was structured around an interprofessional Mindfulness in Motion training, significantly increased resiliency in residents at the Ohio State University Wexner Medical Center (Moffatt-Bruce et al., 2019 ). The Mindfulness in Motion training consists of a weekly group meeting with five sequential segments: prompted reflective writing, video presentation on mind/body connectivity, voluntary sharing of reflective responses, video instruction on yoga and mindfulness practices, and a closing meditation (Klatt et al., 2020 ). Though yielding promising results, these methods remain reactive, similar to most medical student wellness initiatives, and do not address the underlying structural causes of burnout within the healthcare system. While current literature lacks specific explorations of the healthcare system’s tendency toward reactive change, as opposed to proactive, this may be an extension of the field’s prioritization of efficiency and academic success over well-being, as mentioned previously (Gupta, 2018 ; Symon, 2020 ). Addressing the correction of such structures is beyond the scope of this review, but deserves serious attention in wellness research. In addition, further explorations of student and resident wellness may involve elucidating the specific motivations within medical culture that keep wellness a low priority within program structuring.
Based on reviewed literature, the following interventions were demonstrated to improve student well-being: transitioning to a P/F grading system, collaborative learning approaches, longitudinal clinical rotation sites, and peer-mentoring programs. General measures for reducing distress include: maintaining hobbies, socialization, positive outlook, avoiding delayed gratification mindsets, learned resiliency, and choosing medicine based off of one’s own interests. Mental Health 3.0 offers an evidence-based approach for successfully implementing these interventions. Measures that did not demonstrate significant improvement include: peer-led mindfulness groups and shortening curricular hours (Vidhukumar and Hamza, 2020 ; Dyrbye and Shanafelt, 2016 ).
The COVID-19 pandemic caused both immediate and long-term changes to the delivery of medical education. At the onset of the pandemic, medical students were removed from clinical rotations to protect against infection. While this ensured their safety, these students were also deprived of peer-engagement due to asynchronous virtual learning. This shift undoubtedly contributed to increased feelings of isolation and risk for burnout (Klasen et al., 2021 ). Despite numerous challenges, the pandemic has also provided opportunities for medical educators to innovate with new technology. For example, senior students on emergency medicine rotations have served as a source of virtual follow-up for emergency department (ED) visits after reviewing medical records. This has allowed students to continue clinical skill development while ensuring safety from infection and proper supervision. Virtual ED follow-ups reflect a growing trend for web-side encounters to serve as a temporary substitute or supplement for clinical rotations (Klasen et al., 2021 ). These digital learning structures were well-received by students, which predicts the persistence of virtual learning in medical school curricula after the COVID-19 pandemic resolves (Dederichs et al., 2020 ). Despite this apparent positive reception, online learning poses challenges to students’ psychological well-being. The asynchronous nature of virtual education modalities lends to feelings of isolation and a lack of motivation during the preclinical years of medical school (Klasen et al., 2021 ). Combined with the already taxing nature of medical education, the stressors of online learning may ultimately exacerbate existing student wellness concerns. Students featured in “Four Years in Blue: The University of Michigan Medical School Documentary” expressed concern for their future clinical training, specifically with regard to availability of personal protective equipment and physician safety. The students also reported feelings of sadness due to a loss of participation in important class milestones, such as a residency match day celebration (Michigan Medicine, 2020 ). Future alterations to the global medical education system in light of the pandemic will thus be an active area of research for years to come. Most notably, the pandemic appears to have served as an impetus for the National Board of Medical Examiners and National Board of Osteopathic Medical Examiners to indefinitely suspend the Step 2-Clinical Skills and Level 2-Performance Evaluation requirement for both allopathic and osteopathic students, respectively (AACOM, 2021 ; USMLE, 2021 ). Student response to this change and its potential effect on student performance should be thoroughly evaluated in future research.
Conclusions and future work
Further reports of wellness programs and interventions aimed at reducing student stress, developing coping strategies, and preventing burnout are needed. As demand for physicians increases and medical school curricula continue to expand, the potential for worsening student wellness increases. COVID-19, stress of licensure exam preparation, and the increasing cost of medical school all add to the brewing pot of pervasive mental illness, substance use, and burnout in the medical student population. Our review of contemporary literature suggests that transitioning to a P/F grading system and implementing longitudinal, collaborative learning approaches with peer support offer solutions to deteriorating medical student wellness. Electives should also be incorporated within the curriculum to further enhance student engagement and excitement for learning (Slavin, 2014 ). Academic faculty should be specifically targeted with instruction on how to reduce extraneous information within courses (Slavin et al., 2014 ; Slavin, 2019 ). Students should also be encouraged to maintain enjoyable hobbies, cultivate social support networks, and maintain a positive outlook to develop resiliency and protect their mental health (Vidhukumar and Hamza, 2020 ; Dyrbyre and Shanafelt, 2016 ). Cognitive behavioral therapy and training in cognitive restructuring techniques should be made available to students in order to address feelings of shame, maladaptive perfectionism, and imposter syndrome (Bynum et al., 2020 ; Chand et al., 2018 ; Slavin et al., 2014 ; Slavin, 2019 ). Confidential depression/anxiety tracking systems to screen students for worrisome mental health issues may also aid in identifying at risk students before mental distress becomes fulminant (Slavin, 2019 ). Faculty and administrators must also strive to improve student wellness from a top-down approach, ensuring that students feel safe to express wellness concerns and seek support when necessary. This may be accomplished through faculty training sessions or development of student liaison committees (Dyrbye et al., 2019 ; Andre et al., 2017 ). Programs at the Saint Louis University School of Medicine and Vanderbilt University School of Medicine offer successful templates for implementation of such programming. With the implementation of any intervention, of course, stringent evaluation guidelines must be employed to ensure optimal improvement to student wellness while avoiding unnecessary burdens to students’ overwhelming schedule.
Data availability
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
American Association of Colleges of Osteopathic Medicine (2021) AACOM, AOA, NBOME support suspension of COMLEX-USA Level 2-PE and continued osteopathic assessment. AACOM. https://www.aacom.org/news-and-events/news-detail/2021/02/17/aacom-aoa-nbome-support-suspension-of-comlex-usa-level-2-pe-and-continued-osteopathic-assessment . Accessed 16 Apr 2021
American Foundation for Suicide Prevention (2002) Struggling in silence: physician depression and suicide. State of the Art, Inc
Andre C, Deerin J, Leykum L (2017) Students helping students: vertical peer mentoring to enhance the medical school experience. BMC Res Note 10(1):176. https://doi.org/10.1186/s13104-017-2498-8
Article Google Scholar
Ayala EE, Roseman D, Winseman JS, Mason HRC (2017) Prevalence, perceptions, and consequences of substance use in medical students. Med Educ Online 22(1):1392824. https://doi.org/10.1080/10872981.2017.1392824
Article PubMed PubMed Central Google Scholar
Baro Vila RC, Burgos LM, Sigal A, Costabel JP, Alves de Lima A (2022) Burnout syndrome in cardiology residents. Impact of the COVID-19 pandemic on burnout syndrome in cardiology residents. Curr Probl Cardiol 47(1):100873. https://doi.org/10.1016/j.cpcardiol.2021.100873
Article PubMed Google Scholar
Bergmann C, Muth T, Loerbroks A (2019) Medical students’ perceptions of stress due to academic studies and its interrelationships with other domains of life: a qualitative study. Med Educ Online 24(1):1603526. https://doi.org/10.1080/10872981.2019.1603526
Bravata DM, Watts SA, Keefer AL, Madhusudhan DK, Taylor KT, Clark DM, Nelson RS, Cokley KO, Hagg HK (2020) Prevalence, predictors, and treatment of impostor syndrome: a systematic review. J Gen Intern Med 35(4):1252–1275. https://doi.org/10.1007/s11606-019-05364-
Busireddy KR, Miller JA, Ellison K, Ren V, Qayyum R, Panda M (2017) Efficacy of interventions to reduce resident physician burnout: a systematic review. J Grad Med Educ 9(3):294–301. https://doi.org/10.4300/JGME-D-16-00372.1
Bußenius L, Harendza S (2019) The relationship between perfectionism and symptoms of depression in medical school applicants. BMC Med Educ 19(1):370. https://doi.org/10.1186/s12909-019-1823-4
Bynum IV WE, Artino AR, Uijtdehaage S, Webb A, Varpio L (2019) Sentinel emotional events: the nature, triggers, and effects of shame experiences in medical residents. Acad Med 94(1):85–93. https://doi.org/10.1097/ACM.0000000000002479
Bynum IV WE, Teunissen WP, Varpio L (2021) In the “Shadow of Shame”: a phenomenological exploration of the nature of shame experiences in medical students. Acad Med 96(11S):S23–S30. https://doi.org/10.1097/ACM.0000000000004261
Bynum IV WE, Uijtdehaage S, Artino Jr AR, Fox JW (2020) The Psychology of shame: a resilience seminar for medical students. MedEdPORTAL 16:11052. https://doi.org/10.15766/mep_2374-8265.11052
Bynum IV WE, Varpio L, Lagoo J, Teunissen PW (2021) ‘I’m unworthy of being in this space’: The origins of shame in medical students. Med Educ 55(2):185–197. https://doi.org/10.1111/medu.14354
Camp DL, Hollingsworth MA, Zaccaro DJ, Cariaga-Lo LD, Richards BF (1994) Does a problem-based learning curriculum affect depression in medical students? Acad Med 69(10 Suppl):S25–7. https://doi.org/10.1097/00001888-199410000-00031 . PMID: 7916817
Article CAS PubMed Google Scholar
Chand SP, Chibnall JT, Slavin SJ (2018) Cognitive behavioral therapy for maladaptive perfectionism in medical students: a preliminary investigation. Acad Psychiatry 42(1):58–61. https://doi.org/10.1007/s40596-017-0708-2
Clance PR, Imes SA (1978) The imposter phenomenon in high achieving women: dynamics and therapeutic intervention. Psychothe. Theory Res Pract 15:241–247. https://doi.org/10.1037/h0086006
Dederichs M, Weber J, Muth T, Angerer P, Loerbroks A (2020) Students’ perspectives on interventions to reduce stress in medical school: a qualitative study. PLoS ONE 15(10):e0240587. https://doi.org/10.1371/journal.pone.0240587
Article CAS PubMed PubMed Central Google Scholar
D’Eon M, Crawford R (2005) The elusive content of the medical-school curriculum: a method to the madness. Med Teach 27(8):699–703. https://doi.org/10.1080/01421590500237598
Drolet BC, Rodgers S (2010) A comprehensive medical student wellness program—design and implementation at Vanderbilt School of Medicine. Acad Med 85:103–110. https://doi.org/10.1097/00001888-199410000-00031
Dyrbye LN, Sciolla AF, Dekhtyar M, Rajasekaran S, Allgood JA, Rea M, Knight AP, Haywood A, Smith S, Stephens MB (2019) Medical school strategies to address student well-being: a national survey. Acad Med 94(6):861–868. https://doi.org/10.1097/ACM.0000000000002611
Dyrbye LN, Shanafelt T (2016) A narrative review on burnout experienced by medical students and residents. Med Educ 50(1):132–149. https://doi.org/10.1111/medu.12927
Dyrbye LN, Thomas MR, Shanafelt TD (2005) Medical student distress: causes, consequences, and proposed solutions. Mayo Clin Proc 80(12):1613–22. https://doi.org/10.4065/80.12.1613
Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, Shanafelt TD (2014) Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med 89(3):443–451. https://doi.org/10.1097/ACM.0000000000000134
Fischbein R, Bonfine N (2019) Pharmacy and medical students’ mental health symptoms, experiences, attitudes and help-seeking behaviors. Am J Pharm Educ 83(10):7558. https://doi.org/10.5688/ajpe7558
Freudenberger H (1974) Staff burn-out. J Soc Issues 30(1):159–165. https://doi.org/10.1111/j.1540-4560.1974.tb00706.x
Grad FP (2002) The preamble of the constitution of the World Health Organization. Bull WHO 80(12):981–984
PubMed Google Scholar
Gupta R (2018) Physicians connected. https://www.youtube.com/watch?v=Xtfsrqp9XH4&t=191s . Accessed 9 Jan 2022
Hankir AK, Northall A, Zaman R (2014) Stigma and mental health challenges in medical students. BMJ Case Rep. https://doi.org/10.1136/bcr-2014-205226 . PMID: 25183806; PMCID: PMC4158203
Henning K, Ey S, Shaw D (1998) Perfectionism, the imposter phenomenon and psychological adjustment in medical, dental, nursing and pharmacy students. Med Educ 32(5):456–64. https://doi.org/10.1046/j.1365-2923.1998.00234.x
Hu KS, Chibnall JT, Slavin SJ (2019) Maladaptive perfectionism, imposterism, and cognitive distortions: threats to the mental health of pre-clinical medical students. Acad Psychiatry 43:381–385. https://doi.org/10.1007/s40596-019-01031-z
Jackson ER, Shanafelt TD, Hasan O, Satele DV, Dyrbye LN (2016) Burnout and alcohol abuse/dependence among U.S. medical students. Acad Med 91(9):1251–1256. https://doi.org/10.1097/ACM.0000000000001138
Kirkland A (2014) What is wellness now? J Health Polit Policy Law 39(5):957–70. https://doi.org/10.1215/03616878-2813647
Klasen JM, Meienberg A, Bogie BJM (2021) Medical student engagement during COVID‐19: lessons learned and areas for improvement. Med Educ 55(1):115–118. https://doi.org/10.1111/medu.14405
Klatt MD, Bawa R, Gabram O, Blake A, Steinberg B, Westrick A, Holliday S (2020) Embracing change: a mindful medical center meets COVID-19. Glob Adv Health Med 9(Dec):2164956120975369. https://doi.org/10.1177/2164956120975369
Lacy BE, Chan JL (2018) Physician burnout: the hidden health care crisis. Clin Gastroenterol Hepatol 16(3):311–317. https://doi.org/10.1016/j.cgh.2017.06.043
Levant B, Villwock JA, Manzardo AM (2020) Imposterism in third-year medical students: an item analysis using the Clance imposter phenomenon scale. Perspect Med Educ 9(2):83–91. https://doi.org/10.1007/s40037-020-00562-8
Lonka K, Sharafi P, Karlgren K, Masiello I, Nieminen J, Birgegard G, Josephson A (2008) MED NORD–A tool for measuring medical students’ well-being and study orientations. Med Teach 30(1):72–79. https://doi.org/10.1080/01421590701769555
McLellan AT (2017) Substance misuse and substance use disorders: why do they matter in healthcare? Trans Am Clin Climatol Assoc 128:112–130
PubMed PubMed Central Google Scholar
Moffatt-Bruce SD, Nguyen MC, Steinberg B, Holliday S, Klatt M (2019) Interventions to Reduce Burnout and Improve Resilience: Impact on a Health System’s Outcomes. Clin Obstet Gynecol 63(3):432–443
Moir F, Henning M, Hassed C, Moyes SA, Elley CR (2016) A peer-support and mindfulness program to improve the mental health of medical students. Teach Learn Med 28(3):293–302. https://doi.org/10.1080/10401334.2016.1153475
Moir F, Yielder J, Sanson J, Chen Y (2018) Depression in medical students: current insights. Adv Med Educ Pract 9:323–333. https://doi.org/10.2147/AMEP.S137384
Nene Y, Tadi P (2021) Resident Burnout In: StatPearls. StatPearls Publishing. Available via: https://www.ncbi.nlm.nih.gov/books/NBK553176/?report=classic . Accessed 19 Feb 2022
Nituica C, Bota OA, Blebea J, Cheng CI, Slotman GJ (2021) Factors influencing resilience and burnout among resident physicians-a National Survey. BMC Med Educ 21(1):514. https://doi.org/10.1186/s12909-021-02950-y
Organ JM, Jaffe DB, Bender KM (2016) Suffering in silence: the survey of law student well-being and the reluctance of law students to seek help for substance use and mental health concerns. J Legal Educ 66(1):116–156
Google Scholar
Papazisis G, Tsakiridis I, Koulas I, Dagklis T, Kouvelas D (2017) Prevalence of illicit drug use among medical students in Northern Greece and association with smoking and alcohol use. Hippokratia 21(1):13–18
CAS PubMed PubMed Central Google Scholar
Reed DA, Shanafelt TD, Satele DW, Power DV, Eacker A, Harper W, Moutier C, Durning S, Massie FS, Thomas MR, Sloan JA, Dyrbye LN (2011) Relationship of pass/fail grading and curriculum structure with well-being among preclinical medical students: a multi-institutional study. Acad Med 86(11):1367–1373. https://doi.org/10.1097/ACM.0b013e3182305d81
Rodrigues H, Cobucci R, Oliveira A, Cabral JV, Medeiros L, Gurgel K, Souza T, Gonçalves AK (2018) Burnout syndrome among medical residents: a systematic review and meta-analysis. PLoS ONE 13(11):e0206840. https://doi.org/10.1371/journal.pone.0206840
Rohe DE, Barrier PA, Clark MM, Cook DA, Vickers KS, Decker PA (2006) The benefits of pass-fail grading on stress, mood, and group cohesion in medical students. Mayo Clin Proc 81(11):1443–1148. https://doi.org/10.4065/81.11.1443
Rosenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, Sen C, Mata DA (2016) Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA 31(21):2214
Seeliger H, Harendza S (2017) Is perfect good?-dimensions of perfectionism in newly admitted medical students. BMC Med Educ 17(1):206. https://doi.org/10.1186/s12909-017-1034-9
Shah AA, Bazargan-Hejazi S, Lindstrom RW, Wolf KE (2009) Prevalence of at-risk drinking among a national sample of medical students. Subst Abus 30(2):141–149. https://doi.org/10.1080/08897070902802067
Sheer AJ, Estores IM, Nickels R, Radhakrishnan N, Goede DL, Mramba LK, Lo MC (2021) Improving burnout and well-being among medicine residents: impact of a grassroots intervention compared to a formal program curriculum. J Educ Health Promot 10:250. https://doi.org/10.4103/jehp.jehp_1378_20
Shi J, Yao Y, Zhan C, Mao Z, Yin F, Zhao X (2018) The relationship between big five personality traits and psychotic experience in a large non-clinical youth sample: the mediating role of emotion regulation. Front Psychiatry 9:648. https://doi.org/10.3389/fpsyt.2018.00648
Slavin S (2019) Reflections on a decade leading a medical student well-being initiative. Acad Med 94(6):771–774. https://doi.org/10.1097/ACM.0000000000002540
Slavin SJ, Chibnall JT (2016) Finding the why, changing the how: improving the mental health of medical students, residents, and physicians. Acad Med 91(9):1194–1196. https://doi.org/10.1097/ACM.0000000000001226
Slavin SJ, Schindler D, Chibnall JT (2014) Mental health 3.0: improving student wellness through curricular changes. Acad Med 89(4):573–577. https://doi.org/10.1097/ACM.0000000000000166 . Medical Student
Slavin SJ, Schindler D, Chibnall JT, Fendell G, Shoss M (2012) PERMA: A model for institutional leadership and culture change. Acad Med 87:1481
Spring L, Robillard D, Gehlbach L, Simas TA (2011) Impact of pass/fail grading on medical students’ well-being and academic outcomes. Med Educ 45(9):867–77. https://doi.org/10.1111/j.1365-2923.2011.03989.x . PMID: 21848714
Symon R (2020) Do no harm: exposing the hippocratic hoax. Symon Productions
Thomas M, Bigatti S (2020) Perfectionism, imposter phenomenon, and mental health in medicine: a literature review. Int J Med Educ 11:201–213. https://doi.org/10.5116/ijme.5f54.c8f8
United States Medical Licensing Examination (2021) Work to relaunch USMLE Step 2 CS discontinued. USMLE. https://www.usmle.org/announcements/?ContentId=309 . Accessed 16 Apr 2021
University of Michigan Medical School (2020) Four Years in Blue: The University of Michigan Medical School Documentary. Michigan Medicine
Vidhukumar K, Hamza M (2020) Prevalence and correlates of burnout among undergraduate medical students-a cross-sectional survey. Indian J Psychol Med 42(2):122–127
Article CAS Google Scholar
Williams D, Tricomi G, Gupta J, Janise A (2015) Efficacy of burnout interventions in the medical education pipeline. Acad Psychiatry 39(1):47–54. https://doi.org/10.1007/s40596-014-0197-5
Williams N (2014) The CAGE questionnaire. Occup Med 64(6):473–474. https://doi.org/10.1093/occmed/kqu058
Download references
Acknowledgements
We thank Ericka Allen, of the Lake Erie College of Osteopathic Medicine, for assistance in proofreading and revisions of this manuscript.
Author information
Authors and affiliations.
Lake Erie College of Osteopathic Medicine, Erie, PA, USA
Harrison J. Klein & Sarah M. McCarthy
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sarah M. McCarthy .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethical approval
Not applicable.
Informed consent
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Klein, H.J., McCarthy, S.M. Student wellness trends and interventions in medical education: a narrative review. Humanit Soc Sci Commun 9 , 92 (2022). https://doi.org/10.1057/s41599-022-01105-8
Download citation
Received : 30 August 2021
Accepted : 24 February 2022
Published : 23 March 2022
DOI : https://doi.org/10.1057/s41599-022-01105-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Medical Student Research: An Integrated Mixed-Methods Systematic Review and Meta-Analysis
Affiliations.
- 1 Faculty of Medicine, Cairo University, Cairo, Egypt; Okinawa Institute of Science and Technology Graduate University, Okinawa, Japan.
- 2 Okinawa Institute of Science and Technology Graduate University, Okinawa, Japan.
- 3 European Institute of Oncology (IEO), Milano, Italy.
- 4 National Cancer Institute, Cairo University, Cairo, Egypt.
- PMID: 26086391
- PMCID: PMC4472353
- DOI: 10.1371/journal.pone.0127470
Importance: Despite the rapidly declining number of physician-investigators, there is no consistent structure within medical education so far for involving medical students in research.
Objective: To conduct an integrated mixed-methods systematic review and meta-analysis of published studies about medical students' participation in research, and to evaluate the evidence in order to guide policy decision-making regarding this issue.
Evidence review: We followed the PRISMA statement guidelines during the preparation of this review and meta-analysis. We searched various databases as well as the bibliographies of the included studies between March 2012 and September 2013. We identified all relevant quantitative and qualitative studies assessing the effect of medical student participation in research, without restrictions regarding study design or publication date. Prespecified outcome-specific quality criteria were used to judge the admission of each quantitative outcome into the meta-analysis. Initial screening of titles and abstracts resulted in the retrieval of 256 articles for full-text assessment. Eventually, 79 articles were included in our study, including eight qualitative studies. An integrated approach was used to combine quantitative and qualitative studies into a single synthesis. Once all included studies were identified, a data-driven thematic analysis was performed.
Findings and conclusions: Medical student participation in research is associated with improved short- and long- term scientific productivity, more informed career choices and improved knowledge about-, interest in- and attitudes towards research. Financial worries, gender, having a higher degree (MSc or PhD) before matriculation and perceived competitiveness of the residency of choice are among the factors that affect the engagement of medical students in research and/or their scientific productivity. Intercalated BSc degrees, mandatory graduation theses and curricular research components may help in standardizing research education during medical school.
Publication types
- Meta-Analysis
- Systematic Review
- Biomedical Research* / methods
- Students, Medical* / psychology
Grants and funding
Research and Training Opportunities
New section.
Looking for ways to enrich your medical school experience? Check out our directories of clinical, research, and public health opportunities.

Looking for ways to enrich your medical school experience? Search for fellowships, internships, summer programs, scholarships, and grants currently available in the United States and abroad.

Earn two degrees in four to five years to improve the health of the individuals and communities you serve.
The National Institutes of Health (NIH) Medical Research Scholars Program (MRSP) is a comprehensive, year-long research enrichment program designed to attract the most creative, research-oriented medical, dental, and veterinary students to the intramural campus of the NIH in Bethesda, MD.
Summer programs at the National Institutes of Health (NIH) provide an opportunity to spend a summer working at the NIH side-by-side with some of the leading scientists in the world, in an environment devoted exclusively to biomedical research.
A Realistic Guide to Medical School
Written by UCL students for students
Top 10 Tips: Getting into Research as a Medical Student
Introducing our new series: Top 10 Tips – a simple guide to help you achieve your goals!
In this blog post, Jessica Xie (final year UCL medical student) shares advice on getting into research as a medical student.

Disclaimers:
- Research is not a mandatory for career progression, nor is it required to demonstrate your interest in medicine.
- You can dip into and out of research throughout your medical career. Do not feel that you must continue to take on new projects once you have started; saying “no, thank you” to project opportunities will allow you to focus your energy and time on things in life that you are more passionate about for a more rewarding experience.
- Do not take on more work than you are capable of managing. Studying medicine is already a full-time job! It’s physically and mentally draining. Any research that you get involved with is an extracurricular interest.

I decided to write this post because, as a pre-clinical medical student, I thought that research only involved wet lab work (i.e pipetting substances into test tubes). However, upon undertaking an intercalated Bachelor of Science (iBSc) in Primary Health Care, I discovered that there are so many different types of research! And academic medicine became a whole lot more exciting…
Here are my Top 10 Tips on what to do if you’re a little unsure about what research is and how to get into it:
TIP 1: DO YOUR RESEARCH (before getting into research)
There are three questions that I think you should ask yourself:
- What are my research interests?
Examples include a clinical specialty, medical education, public health, global health, technology… the list is endless. Not sure? That’s okay too! The great thing about research is that it allows deeper exploration of an area of Medicine (or an entirely different field) to allow you to see if it interests you.
2. What type of research project do I want to do?
Research evaluates practice or compares alternative practices to contribute to, lend further support to or fill in a gap in the existing literature.
There are many different types of research – something that I didn’t fully grasp until my iBSc year. There is primary research, which involves data collection, and secondary research, which involves using existing data to conduct further research or draw comparisons between the data (e.g. a meta-analysis of randomised control trials). Studies are either observational (non-interventional) (e.g. case-control, cross-sectional) or interventional (e.g. randomised control trial).
An audit is a way of finding out if current practice is best practice and follows guidelines. It identifies areas of clinical practice could be improved.
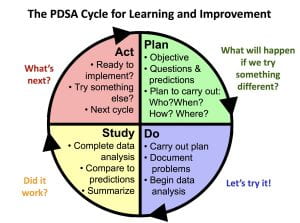
Another important thing to consider is: how much time do I have? Developing the skills required to lead a project from writing the study protocol to submitting a manuscript for publication can take months or even years. Whereas, contributing to a pre-planned or existing project by collecting or analysing data is less time-consuming. I’ll explain how you can find such projects below.
3. What do I want to gain from this experience?
Do you want to gain a specific skill? Mentorship? An overview of academic publishing? Or perhaps to build a research network?
After conducting a qualitative interview study for my iBSc project, I applied for an internship because I wanted to gain quantitative research skills. I ended up leading a cross-sectional questionnaire study that combined my two research interests: medical education and nutrition. I sought mentorship from an experienced statistician, who taught me how to use SPSS statistics to analyse and present the data.
Aside from specific research skills, don’t forget that you will develop valuable transferable skills along the way, including time-management, organisation, communication and academic writing!
TIP 2: BE PROACTIVE
Clinicians and lecturers are often very happy for medical students to contribute to their research projects. After a particularly interesting lecture/ tutorial, ward round or clinic, ask the tutor or doctors if they have any projects that you could help them with!
TIP 3: NETWORKING = MAKING YOUR OWN LUCK
Sometimes the key to getting to places is not what you know, but who you know. We can learn a lot from talking to peers and senior colleagues. Attending hospital grand rounds and conferences are a great way to meet people who share common interests with you but different experiences. I once attended a conference in Manchester where I didn’t know anybody. I befriended a GP, who then gave me tips on how to improve my poster presentation. He shared with me his experience of the National institute of Health Research (NIHR) Integrated Academic Training Pathway and motivated me to continue contributing to medical education alongside my studies.
TIP 4: UTILISE SOCIAL MEDIA
Research opportunities, talks and workshops are advertised on social media in abundance. Here are some examples:
Search “medical student research” or “medsoc research” into Facebook and lots of groups and pages will pop up, including UCL MedSoc Research and Academic Medicine (there is a Research Mentoring Scheme Mentee Scheme), NSAMR – National Student Association of Medical Research and International Opportunities for Medical Students .
Search #MedTwitter and #AcademicTwitter to keep up to date with ground-breaking research. The memes are pretty good too.
Opportunities are harder to come by on LinkedIn, since fewer medical professionals use this platform. However, you can look at peoples’ resumes as a source of inspiration. This is useful to understand the experiences that they have had in order to get to where they are today. You could always reach out to people and companies/ organisations for more information and advice.
TIP 5: JOIN A PRE-PLANNED RESEARCH PROJECT
Researchers advertise research opportunities on websites and via societies and organisations such as https://www.remarxs.com and http://acamedics.org/Default.aspx .
TIP 6: JOIN A RESEARCH COLLABORATIVE
Research collaboratives are multiprofessional groups that work towards a common research goal. These projects can result in publications and conference presentations. However, more importantly, this is a chance to establish excellent working relationships with like-minded individuals.
Watch out for opportunities posted on Student Training and Research Collaborative .
Interested in academic surgery? Consider joining StarSurg , BURST Urology , Project Cutting Edge or Academic Surgical Collaborative .
Got a thing for global health? Consider joining Polygeia .
TIP 7: THE iBSc YEAR: A STEPPING STONE INTO RESEARCH
At UCL you will complete an iBSc in third year. This is often students’ first taste of being involved in research and practicing academic writing – it was for me. The first-ever project that I was involved in was coding data for a systematic review. One of the Clinical Teaching Fellows ended the tutorial by asking if any students would be interested in helping with a research project. I didn’t really know much about research at that point and was curious to learn, so I offered to help. Although no outputs were generated from that project, I gained an understanding of how to conduct a systematic review, why the work that I was contributing to was important, and I learnt a thing or two about neonatal conditions.
TIP 8: VENTURE INTO ACADEMIC PUBLISHING
One of the best ways to get a flavour of research is to become involved in academic publishing. There are several ways in which you could do this:
Become a peer reviewer. This role involves reading manuscripts (papers) that have been submitted to journals and providing feedback and constructive criticism. Most journals will provide you with training or a guide to follow when you write your review. This will help you develop skills in critical appraisal and how to write an academic paper or poster. Here are a few journals which you can apply to:
- https://thebsdj.cardiffuniversitypress.org
- Journal of the National Student Association of Medical Researchjournal.nsamr.ac.uk
- https://cambridgemedicine.org/about
- https://www.bmj.com/about-bmj/resources-reviewers
Join a journal editorial board/ committee. This is a great opportunity to gain insight into how a medical journal is run and learn how to get published. The roles available depend on the journal, from Editor-in-Chief to finance and operations and marketing. I am currently undertaking a Social Media Fellowship at BJGP Open, and I came across the opportunity on Twitter! Here are a few examples of positions to apply for:
- Journal of the National Student Association of Medical Researchjournal.nsamr.ac.uk – various positions in journalism, education and website management
- https://nsamr.ac.uk – apply for a position on the executive committee or as a local ambassador
- Student BMJ Clegg Scholarship
- BJGP Open Fellowships
TIP 9: GAIN EXPERIENCE IN QUALITY IMPROVEMENT
UCL Be the Change is a student-led initiative that allows students to lead and contribute to bespoke QIPs. You will develop these skills further when you conduct QIPs as part of your year 6 GP placement and as a foundation year doctor.
TIP 10: CONSIDER BECOMING A STUDENT REPRESENTATIVE
You’ll gain insight into undergraduate medical education as your role will involve gathering students’ feedback on teaching, identifying areas of curriculum that could be improved and working with the faculty and other student representatives to come up with solutions.
It may not seem like there are any research opportunities up for grabs, but that’s where lateral thinking comes into play: the discussions that you have with your peers and staff could be a source of inspiration for a potential medical education research project. For example, I identified that, although we have lectures in nutrition science and public health nutrition, there was limited clinically-relevant nutrition teaching on the curriculum. I then conducted a learning needs assessment and contributed to developing the novel Nutrition in General Practice Day course in year 5.
Thanks for reaching the end of this post! I hope my Top 10 Tips are useful. Remember, research experience isn’t essential to become a great doctor, but rather an opportunity to explore a topic of interest further.
One thought on “Top 10 Tips: Getting into Research as a Medical Student”
This article was extremely helpful! Alothough, I’m only a junior in high school I have a few questions. First, is there anyway to prepare myself mentally for this challenging road to becoming a doctor? check our PACIFIC best medical college in Rajasthan
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Copyright © 2018 UCL
- Freedom of Information
- Accessibility
- Privacy and Cookies
- Slavery statement
- Reflect policy
Please check your email to activate your account.
« Go back Accept

Medical Student Research
Medical research informs everything we do in medicine. Basic research helps us understand how the human body works at the molecular and cellular levels. Applied research in the lab gives rise to potential new diagnostic and therapeutic modalities. Clinical research tells us what medical interventions work and do not work in humans. Health services research helps us understand the best way to deliver medical care, including ongoing issues with health disparities. Quality improvement research helps make our care better. Epidemiologic research, population health research, and health policy research guide us in the realm of public health. And finally, medical education research helps us understand the best way to teach the next generation of doctors. Translational research and dissemination and implementation science bring these different research approaches together to bridges the gap from bench to bedside..
Given the importance of research within the medical profession, Case Western Reserve University School of Medicine requires a mentored research project and associated written MD Thesis to graduate. All areas of exploration on the biomedical research spectrum, detailed above, are open for these projects. The Office of Medical Student Research is committed to helping you have a productive and positive experience, whatever your previous research background. We have numerous resources available, including a needs assessment delivered to all incoming medical students, in-person workshops, online learning modules, an easy-to-use website that links faculty research mentors and interested students together, and a dedicated faculty and staff team give you individualized support through the research process.
Being involved in research during medical school will help you in your career at every stage, including residency, fellowship, and beyond. Understanding medical research—what it is, how it is done, what it shows us and its limitations—allows you to practice both the science and art of medicine after graduation and beyond, whether you are doing the research yourself in an academic setting or serving patients or communities. Research can also be personally rewarding, opening doors to travel, collaboration, and lifelong learning.
If you are a CWRU faculty member interested in being a medical student research mentor, please click on the ‘Submit a Project’ link and take a few minutes to enter one or more projects that would be applicable to medical students. If you have many projects, enter your research interests and contact information and indicate that students should contact you. As of 2023, the large majority of required medical student research occurs over 12 weeks of summer. Many students continue the same project or join another one beyond this required experience. You can submit projects that are appropriate for either timeline.
If you are a current CWRU medical student, please click on the ‘Search for Project’ link to search the database for potential research mentors and projects. This requires CWRU single sign-on.
We also keep a partial list of potential student research opportunities external to CWRU, of which we are aware. Click on the ‘External Research Opportunities’ link to explore these.
If you need help or want more information, please email [email protected].
Rosa K Hand, PhD, RDN, LD, FAND
Associate Professor, Nutrition Director, Medical Student Research & Scholarship
Sharon Callahan Administrative Director, Medical Student Research & Scholarship
- Prospective Students
- Current Students
- Residents & Fellows
- Give to SMHS

Medical Student Research

Research is a key feature of the GW experience and mission. GW and our partners at Children's National Hospital work together on the CTSI-CN to enhance Clinical and Translational Research. Groundbreaking research takes place in our biomedical research laboratories as well as in clinical settings and with our community partners. Medical students can experience research firsthand through a variety of programs.
The AAMC Careers in Medicine® program supports medical students in their research into career options, specialty choices, and individual residency programs. The American Physician Scientists Association is a student run organization that enhances the future of translational medicine. The AAMC Careers in Medicine® Residency and Fellowship Program Search includes profiles of thousands of residency programs.
GW SMHS medical students can explore the following:
- Medical Student Research: Beaumont Society
- Medical Student Funding
- Research Scholarly Concentration
- Fusion magazine
Boston University Medical Student Research
There are numerous opportunities for medical students to engage in mentored research projects at boston university chobanian & avedisian school of medicine. we are here to help connect you to these resources., medical student research opportunities @ bu chobanian & avedisian school of medicine.

My Research @ BU Chobanian & Avedisian School of Medicine
Piers Klein is working under the mentorship of Dr. Thanh Nguyen and Dr. Mohamad Abdalkader in the departments of Neurology and Radiology at Boston Medical Center and the Chobanian & Avedisian School of Medicine. His research focuses on the epidemiology, diagnosis, medical and interventional treatment of cerebrovascular disease.
Research Opportunities

- Mission and Vision
- Scientific Advancement Plan
- Science Visioning
- Research Framework
- Minority Health and Health Disparities Definitions
- Organizational Structure
- Staff Directory
- About the Director
- Director’s Messages
- News Mentions
- Presentations
- Selected Publications
- Director's Laboratory
- Congressional Justification
- Congressional Testimony
- Legislative History
- NIH Minority Health and Health Disparities Strategic Plan 2021-2025
- Minority Health and Health Disparities: Definitions and Parameters
- NIH and HHS Commitment
- Foundation for Planning
- Structure of This Plan
- Strategic Plan Categories
- Summary of Categories and Goals
- Scientific Goals, Research Strategies, and Priority Areas
- Research-Sustaining Activities: Goals, Strategies, and Priority Areas
- Outreach, Collaboration, and Dissemination: Goals and Strategies
- Leap Forward Research Challenge
- Future Plans
- Research Interest Areas
- Research Centers
- Research Endowment
- Community Based Participatory Research Program (CBPR)
- SBIR/STTR: Small Business Innovation/Tech Transfer
- Solicited and Investigator-Initiated Research Project Grants
- Scientific Conferences
- Training and Career Development
- Loan Repayment Program (LRP)
- Data Management and Sharing
- Social and Behavioral Sciences
- Population and Community Health Sciences
- Epidemiology and Genetics
- Medical Research Scholars Program (MRSP)
- Coleman Research Innovation Award
- Health Disparities Interest Group
- Art Challenge
- Breathe Better Network
- Healthy Hearts Network
- DEBUT Challenge
- Healthy Mind Initiative
- Mental Health Essay Contest
- Science Day for Students at NIH
- Fuel Up to Play 60 en Español
- Brother, You're on My Mind
- Celebrating National Minority Health Month
- Reaching People in Multiple Languages
- Funding Strategy
- Active Funding Opportunities
- Expired Funding Opportunities
- Technical Assistance Webinars

- Community Health and Population Sciences
- Clinical and Health Services Research
- Integrative Biological and Behavioral Sciences
- Intramural Research Program
- Training and Diverse Workforce Development
- Inside NIMHD
- ScHARe HDPulse PhenX SDOH Toolkit Understanding Health Disparities For Research Applicants For Research Grantees Research and Training Programs Reports and Data Resources Health Information for the Public Science Education

- NIMHD Programs
- NIMHD Intramural Research Program
NIH Medical Research Scholars Program

- Extramural Research
- NIMHD Collaborations
- Education and Outreach
- COVID-19 Information and Resources
Program Helps Medical, Dental, Veterinary Students Enter the Pathway to Biomedical Research Careers
2023-2024 MRSP Application Period: October 1, 2022 - January 6, 2023
The National Institutes of Health (NIH) Medical Research Scholars Program (MRSP) is a comprehensive, year long research enrichment program designed to attract the most creative, research-oriented medical, dental, and veterinary students to the intramural campus of the NIH in Bethesda, MD.
Student scholars engage in a mentored basic, clinical, or translational research project on the main NIH campus in Bethesda, or nearby NIH facilities that matches their research interests and career goals.
NIMHD is proud to participate with other NIH Institutes and Centers in the MRSP. Our goal is to introduce the MRSP to medical, dental, and veterinary students from diverse racial and ethnic backgrounds and encourage them to consider biomedical research as a career.
MRSP Eligibility Requirements for the NIH
In order to be eligible to apply for a Medical Research Scholars Program at the NIH, you must meet the following requirements :
- This program is intended for medical, dental, osteopathic, and veterinary students attending accredited institutions location in the U.S., U.S. Commonwealth territories, or Canada. Candidates must currently be enrolled in a medical school accredited by the Liaison Committee on Medical Education, a dental school that is accredited by the Commission on Dental Accreditation, an osteopathic school that is accredited by the American Osteopathic Association, or a veterinary medical college that is accredited by the American Veterinary Medical Association, Council on Education.
- Candidates currently enrolled in PhD or MD/PhD programs are not eligible to apply.
- The Medical Research Scholars Program is designed for students who have completed their clinical rotations, i.e., third-year, but does not exclude students with strong research interests from applying prior to having completed their clinical rotations.
- Candidates must be U.S. citizens or permanent residents.
- Fourth-year students qualify to apply and participate in the Medical Research Scholars Program. However, they must not participate in the National Residency Match Program and must defer graduation.
For more information, visit Medical Research Scholars Program
NIMHD Featured Scholar Bio

Jamie Ko (2021-2022 MRSP Scholar) is a fourth-year medical student at the University of California, Los Angeles (UCLA). She is completing a yearlong research fellowship through the NIH’s Medical Research Scholars Program under the mentorship of Dr. Anna M. Nápoles, Scientific Director of the National Institute on Minority Health and Health Disparities, and Dr. Paula Strassle, staff scientist in NIMHD's Division of Intramural Research.
As a first-generation college graduate and child of immigrants from China, she became intimately aware of how social factors affected the health of under-resourced communities. Throughout Ms. Ko’s academic studies, she developed a passion for exploring and addressing health inequities.
As an undergraduate student at Yale, she integrated her interests in health sciences with public health, resulting in a double major in molecular, cellular, and developmental biology, as well as sociology with a health concentration. To further her understanding of health inequities, she completed a master's degree in public health in chronic disease epidemiology at the Yale School of Public Health.
During medical school, she continued to pursue her interest in health disparities, merging her epidemiology skill set with health policy and patient advocacy. She served as a co-president and delegate of the UCLA American Medical Association and California Medical Association chapters, a committee member on the American Medical Association’s Council on Global Public Health, and Research Director of the Los Angeles Human Rights Initiative.
Ms. Ko plans to apply to a general surgery residency and pursue a career in academic surgery devoted to providing equitable surgical care for patients. Currently, her research focuses on surgical and COVID-19 health disparities. During her free time, she enjoys playing the violin, singing in choirs, running, and reading.
Previous NIMHD Scholars
- 2020-2021 MRSP Scholar
- 2019-2020 MRSP Scholar
- 2018-2019 MRSP Scholar
- 2017-2018 MRSP Scholars
Page updated October 31, 2022
Program Contact
Dr. Anna María Nápoles NIMHD [email protected] -->
More Information
Program Brochure
Meet Current and Alumni Scholars
NIH announces 2019-2020 Medical Research Scholars Program Class
NIH announces 2018-2019 Medical Research Scholars Program Class
NIH announces 2017-2018 Medical Research Scholars Program Class
MSRP Inquiries [email protected]

Staying Connected
- Funding Opportunities
- News & Events
- HHS Vulnerability Disclosure
- Privacy/Disclaimer/Accessibility Policy
- Viewers & Players
- Share full article
Advertisement
Supported by
Body Language
The Unbearable Vagueness of Medical ‘Professionalism’
Since its inception, this murky term has straddled the dual role of disciplining and inspiring.

By Rachel E. Gross
When Joel Bervell thought about professionalism as an undergrad, he thought of “Grey’s Anatomy.” Specifically, he thought about how residents on the show were expected to be, although often were not: on time, prepared for their cases and respectful to everyone around them.
“That was the only standard that I had of what it meant to be a doctor — especially someone like me, who doesn’t come from a family of doctors,” said Mr. Bervell, 28 , a fourth-year medical student at Washington State University. Mr. Bervell, who is Ghanaian American, is one of the first Black medical students at the medical college, which opened in 2017.
From the moment students set foot in medical school, they are instilled with the concept of medical professionalism: their sacred responsibility to conduct themselves with the values of a profession that is granted automatic trust in society. “It is the first thing they tell you: You are now literally a medical professional,” Mr. Bervell said.
The same metric can be used to determine whether or not a med student becomes a doctor at all.
Starting in their third year, Mr. Bervell learned, he and his classmates would be regularly assessed on their professional behavior , along with other attributes like communication skills. Faculty, staff and other students could also report specific concerns about an individual’s professionalism, resulting in write-ups, the contents of which could become attached to their permanent records, following them like scarlet letters.
The problem, as many medical students have also learned, is that where “professional” is vague, “unprofessional” is even more so. Depending on who makes the call, unprofessional behavior can mean hugging your program director, letting a bra strap show , wearing braids , donning a swimsuit over the weekend or wearing a “Black Lives Matter” sweatshirt in the E.R.
As a result, professionalism exists at two levels, as both a lofty standard of behavior and a ( sometimes literal) list of dos and don’ts that blur ethics and appearance. That second meaning can prove particularly pernicious to residents of color, said Dr. Adaira Landry, an adviser at Harvard Medical School and co-author on a recent journal article on the “overpolicing” of Black residents.
The article, published in The New England Journal of Medicine , adds to growing literature documenting the ways residents of color are disciplined or pushed out of medicine. In 2015-16, 20 percent of trainees dismissed from their residency were Black, although Black students make up only 5 percent of residents, according to unpublished data from the Accreditation Council for Graduate Medical Education, or A.C.G.M.E.
For students who did not grow up in the culture of medicine or do not resemble an outdated notion of what a doctor should look like (white, male, elite), these opaque rules can present a minefield. “The environment is so restrictive of what is allowed that when you behave or look or speak differently, it feels like it’s unprofessional,” Dr. Landry said.
Among minority students with whom Dr. Landry works and who are facing probation or dismissal, she has seen a common thread. “I have never had a student reach out to me that they’re being kicked out because of an academic grade,” she said. “The overwhelming theme is that it’s interpersonal conflicts, labeled as professionalism challenges.”
From ethics code to dress code
The lofty ideals that Mr. Bervell encountered on his first day are more in line with how professionalism was originally conceived, said Dr. David C. Leach, who served as executive director of the A.C.G.M.E. from 1997 to 2007.
At the time, medicine was at a crossroads. Giant companies were snapping up individual practices and turning them into for-profit enterprises. Doctors saw their time with patients dwindle, and patients saw their quality of care decline.
“There was a rising public perception that doctors were just like everyone else: They’re just looking to make a buck,” said Dr. Matthew Wynia, a medical ethicist studying the ethics of managed care during this period. “The fear was that our sense of professionalism was being lost.”
In response, the council set out to define a set of general competencies: measurable outcomes that a resident needed to demonstrate before moving forward in the journey to becoming a physician.
Of the six competencies the council ultimately established, professionalism came closest to the heart of what it meant to be a doctor. “It is a set of promises about the trustworthiness of both the profession as a whole and the individuals practicing in it,” Dr. Leach wrote in 2014. Many believed that professionalism was key to helping medicine re-establish its values as an ethics-based altruistic profession — one committed to patients, not the bottom line.
Professionalism was also the vaguest competency on the list. The 1999 definition characterized professionalism as “a commitment to carrying out professional responsibilities, adherence to ethical principles and sensitivity to a diverse patient population.” Doctors were also expected to demonstrate an array of attributes in every interaction, including compassion, respect, humility, integrity, accountability.
Residency directors complained that, compared to things like patient care and medical knowledge, professionalism was squishy and difficult to measure. The concerns boiled down to, “I’m a really busy program director, so what the hell am I supposed to do?” recalled Dr. Leach.
The vagueness problem never went away, said Dr. Deborah Powell, a former executive dean at the University of Kansas School of Medicine, who was on the A.C.G.M.E. board at the time. In the 2000s, conversations about what constituted professionalism often devolved to focus on how doctors should dress. “You shouldn’t have beards, you shouldn’t have long hair, women should wear skirts,” Dr. Powell said. “It was crazy. We went overboard.”
Those conversations are still happening today. Dr. Londyn Robinson, now a resident at Duke University, learned the second definition of professionalism in 2020. While looking for tips on applying to residencies, she stumbled across an article in the journal Vascular Surgery titled “Prevalence of Unprofessional Social Media Content Among Young Vascular Surgeons.”
The authors had trawled the social media accounts of 500 surgery trainees and rated them for professionalism without their knowledge. By the authors’ definition, potentially unprofessional content included photos of residents holding alcoholic drinks, wearing Halloween costumes or “provocative posing in bikinis/swimwear.”
To Dr. Robinson, who is the first in her family to earn an M.D., the paper revealed that, for some, professionalism had been reduced to superficial attributes rather than to ethical behavior with patients. “Basically, they said the quiet part out loud,” she said.
A new ideal
As Dr. Robinson learned, professionalism now radiates beyond the clinic or classroom. Mr. Bervell’s instructors had cautioned him about the consequences of social media: Because medical students represented the profession at all times, they said, being a professional meant thinking twice before talking online about politics or hot-button issues like abortion.
Mr. Bervell didn’t exactly heed that warning. During the Covid-19 pandemic, he began making TikTok videos pointing out racial bias in medical tools like the pulse oximeter and lung function tests . (Both are less accurate for non-white patients, studies have found), earning him the moniker of “medical mythbuster.” His videos have been added to medical school syllabuses, drawn praise from the American Medical Association and earned him a seat on the White House’s Healthcare Leaders in Social Media Roundtable.
By the standards of his own school, Mr. Bervell said, his social media activism could be seen as unprofessional. But, he added, he saw challenging health care’s gaping racial disparities is part of his role in changing medicine — and, maybe, giving doctors something better than “Grey’s Anatomy” as a model for how to be a professional.
The vagueness of professionalism can pose a challenge not only for students of color but for anyone who falls outside the historical stereotype of a doctor. Dr. Robinson noted that the people being judged for their swimwear in the Vascular Surgery paper were more often women than men.
In 2020, incensed by the paper, she posted a photo of herself in a bikini top and shorts on X, formerly known as Twitter, with the hashtag #MedBikini. “I’ll say it: I wear bikinis. I am going to be a doctor,” Dr. Robinson wrote. By the next day, her post had gone viral , and the paper was formally retracted.
In an apology , the editors of the journal acknowledged that “professionalism has historically been defined by and for white, heterosexual men and does not always speak to the diversity of our work force or our patients.”
As the face of medicine changes and platforms like TikTok and Twitter transform the way that medical knowledge is shared, the original architects of professionalism still believe that the core tenets of the term will remain central to medicine.
For Dr. Leach, the definition is simple. “Are you discerning and telling the truth? Are you putting the patient’s interests ahead of your own? And are you developing practical wisdom that can incorporate the best science with the particulars of this particular patient to come up with a creative clinical decision?” he said. “If you’re doing those three things, then you’re professional.”
He added: “And a dress code is so far and away from those three things.”
- Washington State University
- Announcements & Notices
- Awards & Achievements
- Business Operations
- Campus Announcements
- Community & Culture
- Professional Resources & Training
- Student News
- WSU College of Medicine
Medical Students Present at Inland Northwest Research Symposium

Ben Caruso and Xiang Yu Gao, both first-year medical students at the WSU College of Medicine, presented a poster at the Inland Northwest Research Symposium on the WSU Spokane campus this week.
Their case report is intended to raise awareness of potential complications following a Roux-en-Y gastric bypass surgery in patients with diffuse large B-cell lymphoma involving the gastrointestinal tract. They say emphasizing the importance of prompt diagnosis of the complication can lead to improved patient outcomes.
- Open access
- Published: 20 March 2024
Evaluation and associated factors of public health emergency management among medical college students in a city in Southwest China: a cross-sectional study
- Xinrui Chen 1 ,
- Meng Zhang 1 ,
- Qingqing Bu 1 ,
- Bo Tan 1 &
- Dan Deng 1
BMC Medical Education volume 24 , Article number: 314 ( 2024 ) Cite this article
183 Accesses
1 Altmetric
Metrics details
Colleges and universities face an increased risk of public health emergencies. Among them, medical colleges and universities deserve more attention as they serve as the play a fundamental role in providing public health emergency services and in cultivating medical professionals. Effectively managing infectious disease prevention and control, as well as responding to public health emergencies in medical colleges and universities, is of great importance for enhancing the capacity of social emergency governance and improving the completeness of the public health system. This study aims to understand the management of public health emergencies in medical colleges in a city in southwest China, explore the factors associated with medical college students ’ evaluations, and provide recommendations for emergency management mechanisms in colleges and universities.
In total, 781 medical college students were selected through stratified random sampling and surveyed using a questionnaire. The main factors affecting students ’ evaluation of emergency management were analyzed using multiple linear regression and structural equation modeling.
The overall emergency management situation in medical colleges was relatively complete, with satisfactory results. Medical college students ’ satisfaction with the timeliness of prevention measures was the highest, while the publicity and education were the lowest. Multiple linear regression analysis showed that grades, emergency education, -simulation training, -information reporting, and dynamic adjustment measures were associated with the evaluation of emergency management by medical students.
Conclusions
Although the evaluation of emergency management in medical colleges was generally positive, certain limitations still existed. To improve the development of the public health system, colleges and universities should constantly reform and innovate emergency management mechanisms according to the important links in the prevention and control processes.
Peer Review reports
The construction of healthy China requires prioritizing people’s health, and effectively doing a good job in the prevention and control of infectious diseases and the response to public health emergencies [ 1 ]. A public health emergency refers to the sudden occurrence of severe infectious diseases, rapidly spreading diseases with unknown causes, widespread food and occupational poisoning, and other events or natural disasters threatening public health [ 2 , 3 ]. Public health emergencies, especially outbreaks of infectious diseases, have become increasingly frequent. Recent public health emergencies have included severe acute respiratory syndrome (SARS) in 2003, influenza A (H1N1) in 2010, avian influenza A(H7N9) in 2013, and Corona Virus Disease 2019 (COVID-19); [ 4 , 5 ] all posed a serious threat to global human health, economic development, and social stability [ 6 , 7 ]. Southwest China has a large population, abundant biodiversity, a hot and humid climate, and a complex terrain These characteristics create favorable conditions for the emergence and spread of epidemiological threats to public health. Thus, it is imperative that this region of China strengthens its prevention and control measures for managing public health emergencies [ 8 ].
Colleges and universities are characterized by a large population density, frequent personnel turnover, the presence of shared public spaces, and high social attention, thereby placing them at an increased risk for public health emergencies [ 9 ]. Previous research has found that more than 70% of public health emergencies in China have occurred in schools; more than 80% were infectious disease epidemics or food poisoning incidents [ 10 ]. These emergencies considerably disrupted the schools’ operations and adversely affected the mental health of teachers, students, and other personnel, and also posed challenges with respect to the improvement of emergency plans and management mechanisms for responding to public health emergencies [ 11 ]. Other studies show that emergency prevention and control challenges remain for some colleges and universities, such as administrators’ insufficient attention, students’ inadequate understanding, poor medical facilities, professionals’ lack of coping skills, and imperfect information reporting systems [ 12 , 13 , 14 ], which render the emergency management of public health emergencies in colleges and universities difficult. Therefore, it is particularly important to strengthen emergency service guarantees for students, standardize internal emergency prevention and control management on campuses, and develop more effective strategies for dealing with public health emergencies.
At present, research on managing public emergencies in universities in other countries is gradually developing in the direction of systematization, specialization, and qualitative analysis [ 15 ]. However, the theoretical research on emergency management in China’s colleges and universities started late; most existing research focuses on descriptive research and case studies, and they have revealed the lack of comprehensive and evidenced-based management systems. Thus, their discussions of prevention and control management show a certain one-sidedness and sundry limitations [ 16 ]. In addition, although international research on the topic is relatively mature, the different national conditions of each country mean that their findings, while insightful, are not fully generalizable to China’s colleges and universities. Therefore, it is imperative to explore management strategies applicable to China when responding to public health emergencies.
Medical colleges and universities play a fundamental role in providing public health emergency services and in cultivating medical professionals [ 17 ]. The administrators of medical colleges and universities must ensure the safety and stability of students’ education by normalizing, standardizing, and specializing the schools’ emergency management. This requires timely identification of weak links in their emergency-response implementation and recommending improvements [ 18 ]. However, few studies have offered specific suggestions for public health emergency management in medical colleges and universities in China [ 19 ]. Students are the direct beneficiaries of public health emergency management systems in colleges and universities, and medical students have relevant professional theoretical knowledge and practical skills; therefore, they have professional advantages in dealing with public health emergencies [ 20 ]. Assessing the degree of satisfaction among medical students regarding emergency management in colleges and universities can facilitate the exploration of strategies to optimize public health emergency management in educational institutes. Therefore, this study aimed to investigate medical colleges’ management of public health emergencies in a city in Southwest China, systematically summarizing their emergency prevention and control implementation and their prevention and control achievements.
The study had several goals. First, it surveyed medical students’ satisfaction levels regarding schools’ emergency management and control measures. Second, it explored factors associated with their evaluations of the schools’ early prevention management, mid-crisis interventions, and late-stage security management. Finally, it re-examined some previously identified shortcomings in medical college and university emergency prevention and control for public health emergencies. The findings of this study may help Southwest China’s medical colleges and universities develop comprehensive, effective emergency management systems.
Study design and participants
The researchers used stratified random sampling to recruit students from several medical colleges and universities in one city in Southwest China. Each school was stratified by grade, and students with different majors were randomly selected from each grade. The study commenced only after the researchers communicated and coordinated with the schools’ administrators and obtained written informed consent from the participating students. The students completed a electronic questionnaire developed in line with the study’s objectives and issued through the schools’ student affairs offices, the survey period is March to April 2022. Of the 803 questionnaires collected, 781 were deemed valid, yielding an response rate of 97.26%. This study, which involved human subjects, was reviewed and approved by the Ethics Committee of Chongqing Medical University. And all methods were performed in accordance with the relevant guidelines and regulations.
Quality control
To ensure the authenticity of the questionnaire, quality control measures were implemented. (1) Through preliminary literature research and expert consultation, based on the current situation of emergency management in colleges and universities and the policy direction of the National Health and Health Commission, the questionnaire preparation was completed and pre-investigation was conducted. Prior to the investigation, project investigators were trained. (2) The training for investigators emphasized the importance of introducing the purpose and significance of the study to participants before conducting the survey. Additionally, the training highlighted the need to clarify the requirements for filling out the questionnaire and any precautions that should be taken. And the survey should be completed anonymously to ensure the confidentiality of the participants’ responses. (3) Questionnaires requiring the same IP address could only be answered once. (4) After the questionnaire was submitted, questionnaires with any missing items and missing or unqualified basic information were deemed invalid.
Questionnaire
The questionnaire contents were designed to satisfy the principles of relevance, universality, applicability and non-inductivity [ 21 ]. The survey included basic demographic information, the current situation as implemented, and medical students’ opinions on the schools’ prevention and control measures for public health emergencies. Seven items were used to evaluate the student’s views. The items covered publicity and education; emergency measures; daily monitoring; aftercare work; timeliness of announcements; timeliness of prevention and control measures; timeliness of administrators’ responses to public opinions The participants ranked each item using a five-point Likert scale from “1 = very dissatisfied” to “5 = very satisfied” for a total score of 35. The higher the score, the more satisfied the students. When the reliability and validity of the scale were assessed, Cronbach’s α coefficient was 0.930, the KMO validity coefficient was 0.920, and Bartlett’s test of sphericity p was < 0.001. Thus, the scale was considered to have good reliability and validity.
Statistical analysis
Data were analyzed using IBM SPSS Statistics for Windows, Version 25.0, and Amos Version 24.0. The count data were described using percentages, and the satisfaction score were presented as (‾ x ± s ). Mann-Whitney U test and Kruskal-Wallis H test were used to measure differences in quantitative data with non-normal distribution. Multiple linear regression and structural equation modeling were used to analyze the factors associated with medical students’ evaluations of public health emergency management (α = 0.05).
Descriptive statistics
Among the 781 medical students, 227 (29.07%) were male, and 554 (70.93%) were female; 327 were freshmen (41.87%), 245 sophomores (31.37%), 174 juniors (22.28%), and 35 seniors or above (4.48%); 739 were undergraduate students (94.62%), and 42 were junior college students (5.38%).
Medical colleges’ emergency responses to public health emergencies
When asked about publicity and education, 60.2% of the students said their school conducted emergency-related publicity and education once every six months. On emergency drills, 46.6% said their schools conducted emergency drills for public health incidents once a year. On emergency facilities, more than half of the students stated their school had public health facilities and conspicuously posted health safety signs. On preventive measures, more than 90% of the students reported their school had taken emergency preventive measures such as screening personnel for infections; controlling personnel activities; providing epidemic prevention materials; monitoring and reporting daily health conditions; and disinfecting key areas. On the administrators’ response to public opinions, 92.7% said their school issues timely responses and reports and informed the campus about the preventive measures, and 87.8% reported their schools regularly corrected disinformation and clarified unconfirmed statements. On emergency supplies, 97.8% of students stated their school distributed masks, disinfectants, thermometers, and other supplies. On aftercare counseling, 91.2% of the students stated their school provided mental health counseling and coping strategies.
Medical colleges’ public health emergency prevention and control
The results showed that because of their school’s emergency management, the medical students reported their awareness of public health emergency prevention had improved greatly (60.1%), moderately (34.2%), or slightly (5.0%); only 0.8% thought it had not improved. Further, 58.6% thought that their school’s emergency prevention and control management ability had improved greatly compared to before the COVID-19 pandemic, 33.2% thought it had moderately improved, and 7.6% thought it had improved slightly; only 0.7% thought it had not improved.
Medical students’ satisfaction with their schools’ management of public health emergencies
The students rated their satisfaction with their schools’ publicity and education, emergency measures, daily monitoring and management, aftercare work, timeliness of announcements, prevention and control measures, and the administrators’ responses to public opinions. The mean total score of their satisfaction ± standard deviation ( SD ) was 31.38 ± 4.06. The mean satisfaction score for the timeliness of the schools’ prevention and control measures was the highest (4.60 ± 0.60); the mean satisfaction score for publicity and education on food safety, laboratory safety, or epidemic prevention and control in schools was the lowest (4.31 ± 0.76). According to the single factor difference analyses (the Mann-Whitney U test and the Kruskal-Wallis H test), there were intergroup differences in the satisfaction scores of different grades and schools regarding the need for the following: emergency education, emergency drills, information notification, dynamically adjusted prevention and control measures, public opinion responses, and psychological counseling, which were all statistically significant ( p < 0.05). Table 1 presents these results.
Analysis of the factors influencing the medical students’ evaluations
Multiple linear regression.
The independent variables in the regression were factors with statistical significance in the univariate analysis; the dependent variable was the satisfaction score for emergency management in medical colleges. The results showed that the main influencing factors were grade; whether the school carried out emergency education, emergency drills, and information notification; and whether the school dynamically adjusted prevention and control measures ( p < 0.05). Compared to the students in the lower grades, the students in the higher grades were less satisfied with the schools’ overall emergency management; and the higher the emergency management evaluation of the university carrying out emergency education, emergency drills, information notification, and dynamically adjusting the prevention and control measures. Furthermore, according to the standardized regression coefficient, whether the school carried out information notification had the greatest impact on the evaluations, followed by whether the school carried out emergency drills. Table 2 presents these results.
Structural equation model
The researchers used structural equation modeling (SEM) to explore the determinants of the medical students’ evaluations of their schools’ emergency management and the relationship between these factors. The SEM model included these variables: grade; whether the school carried out emergency education, emergency drills, or information notification; whether the school dynamically adjusted its prevention and control measures; whether the schools rapidly responded to public opinions; whether the school provided psychological counseling; and the students’ satisfaction scores. The SEM model used these factors to explore the influences on the students’ evaluations of the public health emergency management of their colleges and universities and the correlation among the associated factors. Figure 1 shows an SEM path analysis diagram.
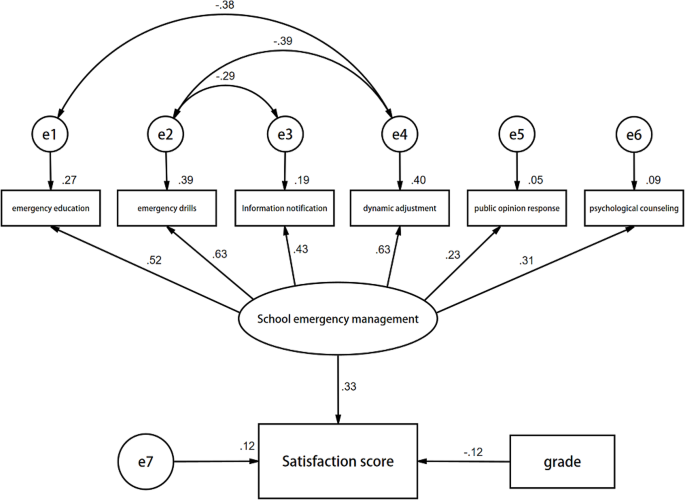
Structural equation model analysis of emergency management evaluation in medical colleges
The model showed that grades and the schools’ emergency management measures directly impacted the students’ evaluations ( p < 0.001). The standardized path coefficients were − 0.12 and 0.33, respectively. When the other variables were constant, the grades negatively influenced the evaluations, and the schools’ emergency management measures positively influenced the evaluations. These results aligned with the results of the multiple linear regression. In addition, the fitness indices met the requirements of the test statistics. Table 3 summarizes the results.
Understanding what influences medical students’ evaluations of their schools’ public health emergency management and responses could help colleges and universities in China improve their emergency management strategies [ 22 ] This study found that the satisfaction score of the timeliness of prevention and control measures taken by schools was the highest, indicating that the city’s medical colleges quickly implemented appropriate epidemic prevention policies and instituted timely and effective prevention and control measures to avoid the spread of COVID-19; thus, they would respond equally well with other epidemics and public health emergencies. Xu and Chen [ 23 ] also found that the timeliness of schools’ emergency measures effectively improved college students’ sense of security. Although more than half of the students said that their school carried out emergency education on food safety, laboratory safety, or epidemic prevention and control once every six months, the lowest satisfaction scores were for the schools’ emergency education, indicating that the medical colleges and universities lacked targeted, systematic, and universal education systems while ensuring the quantity of education, resulting in poor quality and insufficient epidemiological information. These findings align with Liu [ 24 ].
The students’ grades and the schools’ implementation of emergency management measures were the main factors associated with students’ evaluations. The students in the higher grades were less satisfied with the schools’ emergency management, and the difference was statistically significant. Zhu and Zhang [ 25 ] also confirmed this conclusion. They believe that the proportion of senior students who were confident of coping with disasters is not very high, and the proportion who believe that disaster education is beneficial to coping with disasters is also not very high. The reason might be that emergency-related education is mainly handled during freshmen enrollment, and with the deepening of professional understanding, the demand and expectation of senior students to take emergency management measures is increasing gradually. The schools had higher evaluation scores for emergency drills, epidemic prevention information, and the dynamic adjustment of prevention and control measures, consistent with Wang [ 26 ]. As emergency education can increase students’ emergency knowledge reserve, emergency drills can boost their emergency prevention and rapid response skills. Timely, comprehensive, and dynamically adjusted prevention and control measures and information can mitigate emergencies’ inconveniences and adverse effects, increasing students’ trust in the schools’ emergency management competence.
The study’s results showed that emergency prevention and intervention measures are critical in managing public health emergencies in colleges and universities, as reported by Li [ 27 ]. The administrations of medical and other colleges and universities should actively implement and improve campus emergency response systems. These systems should consider the factors influencing students’ evaluations, to ensure the continuous improvement of the schools’ prevention and control management strategies of public health emergencies, as follows.
1) Provide comprehensive education on preventing and handling public health emergencies [ 28 ]. Medical school administrations must establish a reasonable emergency education system; regularly provide high-quality, understandable, science-based information and training on epidemic prevention and control to the medical students at every level of study, especially the seniors; and ensure campus-wide compliance with posted guidelines on public health safety regulations.
2) Have professionals conduct regular, standardized public health emergency drills [ 29 ]. Colleges and universities should have professionals on-site trained in managing public health emergencies, Regularly carrying out emergency drills under the guidance of the local party committee and the government, and instructing students, teachers, and staff about emergency-response topics such as remote classes; campus closures or restrictions; health-related isolation and treatment; health data collection, sorting, and analysis; epidemic investigation and tracing; and regional detection and quarantines to expedite emergency response.
3) Dynamically respond to the needs of students, teachers, and the staff during a public health crisis. Public health emergency underscored the need for rapid, flexible, accurate communication and control strategies. Universities and colleges should provide crisis-related information; prevention, transmission, and treatment guidance; and up-to-date news and official school announcements. It is vital to keep everyone informed about everything from the nature of the emergency to teaching adjustments, such as temporarily transitioning to remote learning [ 30 ].
4) Ensure the students’ physical and mental well-being. Colleges and universities should anticipate how public health emergencies can adversely affect students’ physical and mental health [ 31 ]. They should discuss this in medical students’ classes—before, during, and after a health crisis—and provide mental health education and psychological counseling.
5) Respond honestly and swiftly to questions and concerns. Misinformation and the lack of information can exacerbate public health emergencies [ 32 ]. Medical school administrators should establish mechanisms for handling the public’s questions and concerns by building effective communication channels between colleges and students.
Limitations
The index system used in this study should be improved further, more research indicators can be included according to the specific conditions of different university types. And this study was a cross sectional design, it was aimed to explore the association between certain variables and the outcomes of interest, rather than to establish a causal relationship. In addition, the use of self-reported data may introduce some limitations to the study, as students may have answered the questions as they felt required by the university or government, rather than reflecting their true perceptions. To mitigate potential response bias and ensure validity and reliability, we conducted repetitive questionnaire designs and pilot experiments.
This study evaluated the factors influencing medical students’ satisfaction with their schools’ emergency management systems and responses in a city in Southwest China and examined the existing problems in emergency prevention and control of public health emergencies in colleges and universities. Students’ grades and the implementation of emergency management measures in schools were important factors affecting the evaluation of emergency management of public health emergencies in colleges and universities. Since today’s medical students will be tomorrow’s professionals entrusted with responding to public health emergencies, improving the medical schools’ management strategies for public health emergencies is vital.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Corona Virus Disease 2019
Internet protocol address
Severe acute respiratory syndrome
Structural equation modeling
People’s Daily Online. Commentator of People’s Daily: Giving strategic priority to safeguarding people’s health——on studying and implementing the speeches of Chinese President Xi Jinping at a symposium attended by experts and representatives from China’s education, culture, health and sports sectors. September 26,2020; http://theory.people.com.cn/n1/2020/0926/c40531-31875772.html . Accessed May 18,2021.
Zhan S. Epidemiology (National University Course Book. for Preventive Medical Specialty); 2017.
Yu Y, Qin YX, Liao YX, et al. A cross-sectional study on the response abilities of clinical and preventive medical students in public health emergency. Front Public Health. 2022;10:1017063.
Article PubMed PubMed Central Google Scholar
Li Z, Gao GF. Infectious disease trends in China since the SARS outbreak. Lancet Infect Dis Nov. 2017;17(11):1113–5.
Article Google Scholar
Zhang TT, Wang Q, Wang Y, Bai G, Dai RM, Luo L. Early surveillance and public health emergency responses between novel coronavirus disease 2019 and avian influenza in China: a case-comparison study. Front Public Health. 2021;9:629295.
Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet Feb. 2020;15(10223):470–3.
Weston D, Ip A, Amlôt R. Examining the application of behaviour change theories in the context of infectious disease outbreaks and emergency response: a review of reviews. BMC Public Health Oct. 2020;1(1):1483.
Huang P, Pan HY, Peng L, Chen TT, Xu J. Temporal and spatial variation characteristics of disaster resilience in Southwest China’s mountainous regions against the background of urbanization. Nat Hazards. 2020;103:3783–802.
Zhang H, Huang YY, Geng Z. A comprehensive management protocol for campus emergencies. Paper presented at: 2021 International Conference on Cyber-Physical Social Intelligence (ICCSI), 2021.
Kong YW, Wang LG, Song HB. Summary of key links of infectious disease prevention and control in schools. Mod Prev Med. 2020;47(6):1113–5.
Google Scholar
Zhang L. Research on the construction of university public health emergency management system based on psychological counseling intervention. J Healthc Eng. 2022;2022:2033018.
ADS PubMed PubMed Central Google Scholar
Wang CY, Cheng Z, Yue XG, McAleer M. Risk management of COVID-19 by universities in China. J Risk Financ Manag. 2020;13(2):36.
Article CAS Google Scholar
Chang ZX, Chen T, Lei BL, Ma N, Li ZH, Zheng HJ. Research on the construction of emergency plan system in colleges and universities. Paper presented at: 2020 International Conference on Modern Education and Information Management (ICMEIM), 2020.
Huang F. Brief analysis of infectious disease prevention and control in universities. Nanfang Lunkan. 2019;05:70–2. 100.
Song P, Zhao J, Mubarak SMA, Taresh SM. Critical success factors for epidemic emergency management in colleges and universities during COVID-19: a study based on DEMATEL method. Saf Sci. 2022;145:105498.
Article PubMed Google Scholar
Wang D. Research on the long-term mechanism of ideological and political education in colleges and universities under the normalization of emergency management. 2022.
Wang WM. Medical education in China: progress in the past 70 years and a vision for the future. BMC Med Educ. 2021;21(1):1–6.
Wang J, Wang Z, Strengths. Weaknesses, Opportunities and Threats (SWOT) Analysis of China’s Prevention and Control Strategy for the COVID-19 Epidemic. Int J Environ Res Public Health Mar 26 2020;17(7).
Fang X, Zhao L, Pang R, Li H, Ye P. Responsibility of education in improving medical college students’ ability to prevent and respond to public health emergencies in China–A systematic review. Front Public Health. 2023;11.
Nalunkuma R, Nkalubo J, Abila DB. Knowledge on infection prevention and control and associated factors among undergraduate health professional students at Makerere University College of Health Sciences, Uganda. PLoS ONE. 2021;16(8):e0255984.
Article CAS PubMed PubMed Central Google Scholar
Slattery EL, Voelker CC, Nussenbaum B, Rich JT, Paniello RC, Neely JG. A practical guide to surveys and questionnaires. Otolaryngol Head Neck Surg Jun. 2011;144(6):831–7.
Jiang H, Islam AA, Gu X, Spector JM. Online learning satisfaction in higher education during the COVID-19 pandemic: a regional comparison between Eastern and Western Chinese universities. Educ Inform Technol. 2021:1–23.
Xu W, Chen CY. Research on the influencing factors and management countermeasures of college students’ sense of security under the environment of big data-an empirical analysis based on the event of COVID-19. Paper presented at: Proceedings of the 2020 The 3rd International Conference on Big Data and Education, 2020.
Liu YY, Zhou W, Song Y. Evaluation of college students’ emergency response capability based on questionnaire-TOPSIS innovative algorithm. Complexity. 2021;2021:1–12.
Article ADS Google Scholar
Zhu TT, Zhang YJ. An investigation of disaster education in elementary and secondary schools: evidence from China. Nat Hazards. 2017;89:1009–29.
Wang N, Zhang W, Cao XH, et al. Evaluation and associated factors of the responses to public health emergencies among college students in Shandong Province. Chin J Sch Health. 2021;42(07):996–9.
Li HW, Chen JB, Ding XX et al. Research on Emergency Management System of Universities Based on the Perspective of PPRR Theory:Taking Some Colleges and Universities in Southern Zhejiang as an Example. Paper presented at: 2nd International Conference on Management and Education, Humanities and Social Sciences (MEHSS 2022), 2023.
Gillam S, Maudsley G. Public health education for medical students: rising to the professional challenge. J Public Health. 2010;32(1):125–31.
Cristal NS, Metcalf N, Kreisberg D, Little CM. Integrating simulation-based exercises into public health emergency management curricula. Disaster Med Public Health Prep. 2019;13(4):777–81.
Bawa P. Learning in the age of SARS-COV-2: a quantitative study of learners’ performance in the age of emergency remote teaching. Comput Educ Open. 2020;1:100016.
Copeland WE, McGinnis E, Bai Y, et al. Impact of COVID-19 pandemic on college student mental health and wellness. J Am Acad Child Adolesc Psychiatry. 2021;60(1):134–41. e132.
Yan H, Wang L, Jang X, Shen Y, Yang S. Research on emergency management mode of public health emergencies in universities based on information technology. Paper presented at: 2021 International Conference on Management Science and Software Engineering (ICMSSE), 2021.
Download references
Acknowledgements
The authors would like to thank all the participating organizations and participants.
This study was supported by the Key Project on Epidemics and Education in the 2020 “13th Five-Year Plan” of Chongqing Education Science (2020-YQ-04).And it was also supported by the Program for Youth Innovation in Future Medicine, Chongqing Medical University (W0063).
Author information
Authors and affiliations.
School of Public Health, Chongqing Medical University, Chongqing, China
Xinrui Chen, Meng Zhang, Qingqing Bu, Bo Tan & Dan Deng
You can also search for this author in PubMed Google Scholar
Contributions
XC collected and analyzed the data and wrote the manuscript; MZ, QB, and BT designed the study and collected data; DD designed the study and revised the manuscript. All authors have reviewed and approved the final manuscript.
Corresponding author
Correspondence to Dan Deng .
Ethics declarations
Ethics approval and consent to participate.
The Chongqing Medical University Ethics Committee reviewed and approved this study. Before commencing the study, the researchers explained the purpose of the study to each participant, emphasized that their participation was voluntary and anonymous, and obtained written informed consent to participate from the participants, their legal guardians, or next of kin.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Chen, X., Zhang, M., Bu, Q. et al. Evaluation and associated factors of public health emergency management among medical college students in a city in Southwest China: a cross-sectional study. BMC Med Educ 24 , 314 (2024). https://doi.org/10.1186/s12909-024-05317-1
Download citation
Received : 29 September 2023
Accepted : 14 March 2024
Published : 20 March 2024
DOI : https://doi.org/10.1186/s12909-024-05317-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical college
- Public health emergency
- Management evaluation
- Associated factors
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Support Dal
- Current Students
- Faculty & Staff
- Family & Friends
- Agricultural Campus (Truro)
- Halifax Campuses
- Campus Maps
- Brightspace
Dalhousie University

- Student Life
- Media Centre
- DAL Magazine
Most Commented
News archive.
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
Big research, little time: Medical neuroscience student wins 3 Minute Thesis finals
Mia Samardzic - March 28, 2024
Last week, 10 graduate students took to the stage to compete in Dal’s annual 3 Minute Thesis (3MT) competition, with medical neuroscience PhD student Reynaldo Popoli earning this year’s winning title with his presentation on improving the quality of life for patients living with the neurological disorder ALS.
The 3MT finals, held Tuesday, March 19 in the Dalhousie Student Union Building, challenged competitors to present their research to a non-specialist audience in three engaging minutes or less, using only one static PowerPoint slide as a visual aid.
Five master’s and five PhD students shared their research, representing the Faculties of Medicine, Science and Health.
Making strides in medicine
Along with taking home the title of Dal’s newest 3MT champion after winning over the judging panel, Popoli won a cash prize of $1,000 and the opportunity to represent Dalhousie at the Eastern 3MT regionals at the Institut national de la recherche scientifique in Quebec this June.
“I feel incredibly grateful, especially to my colleagues that allowed me to practice my presentation and provided invaluable feedback,” he says.

Popoli’s presentation called attention to the devastating impacts of ALS — a disease that affects the cells in our bodies that control our muscles. These cells originate in the brain and spinal cord and travel to the muscles, forming connections called neuromuscular junctions. In ALS, the cells withdraw from the muscles, and these connections are left non-functional.
“The goal of my research is to understand some of the changes that occur in ALS. More precisely, in the connections between the cells that control our movements and their respective muscles. By understanding these changes, we hope we can use different therapeutic approaches to slow down disease progression and improve symptoms,” he says.
Popoli’s research looks at drugs that help regulate and maintain the integrity of the neuromuscular junction. He has shown that the use of these drugs in ALS make symptoms progress much slower and maintain neuromuscular junctions for longer, allowing for a 10 per cent increase in life expectancy and better quality of life for patients.
“My work is far from over, but I’m hopeful that with this novel research, we’ll be able to find new treatments for this devastating disease.”
Prize-worthy presentations
Pooyan Moradi, another PhD student in medical neuroscience, and Kaela Trumble, a master’s student in rehabilitation research, were also selected as top finalists by the judging panel.
Moradi earned second place and a $500 prize, presenting on the use of artificial intelligence to detect seizures in animals and how this model can be applied to better predict epilepsy in humans who have suffered head injuries.

Trumble placed third in the competition and won $250 with a presentation covering the differences in how people develop health problems as they age in relation to heart disease.

The remaining eight finalists each earned $100 prizes for their inspiring presentations.
Also receiving the most votes for the People’s Choice Award, biochemistry and molecular biology master’s student Dina Rogers captivated the crowd when describing a biological recycling process by which PET plastic can be repurposed into new materials by protein engineering to combat climate change. The award, valued at $500, was generously sponsored by Estelle Joubert, assistant dean of the Faculty of Graduate Studies, and entrepreneur Paul Doerwald.

Recommended reading: Where experience meets impact: Introducing Dalhousie’s 2023 Top Co‑op Students of the Year
Distilling big ideas
This year's 3MT finals opened with a traditional Mi'kma'ki welcome with Elder Ann LaBillois. The event was enthusiastically hosted by CBC reporter and video journalist Brett Ruskin for a sixth time.
Judges for the competition were Dr. Frank Harvey, Dal's provost and vice-president academic, Grace Jefferies-Aldridge, Dal’s vice-president, people and culture, and Kristan Hines, senior vice-president of corporate and public affairs at NATIONAL Public Relations.
Organized by the Faculty of Graduate Studies, the event served as an opportunity for members of the Dal community and beyond to learn about the impactful work the university’s graduate students are engaged in.
“For many of us, the 3 Minute Thesis competition is the highlight of the year at Dalhousie,” says Dr. Marty Leonard, dean of the Faculty of Graduate Studies. “It challenges students to take what could be very technologically or theoretically complex research — or better yet, both — and make it accessible and interesting to anyone.”
Dalhousie President Dr. Kim Brooks invited the crowd to relish the opportunity to celebrate the extraordinary research happening on campus.

“If you have the privilege of spending time in a university, one of the things you get to do often in your academic life is trace an idea back to its origins,” she says. “And almost every time you find a new idea, a unique contribution, and you trace it back to its origins, you find a graduate student.”

See below for a complete list of this year’s 3MT finalists and their presentations:
Dina Rogers , MSc, Biochemistry and Molecular Biology
Proteins vs. Pollution: A Biochemical Solution to a Brighter Future
Kateryna Rudenko , MES, Environmental Studies
Weaving Mi’kma’ki from Stories We Share
Joy Liu , MSc, Statistics
From Approximate to Accurate: Improving Sea Scallop Meat Weight Estimates in the Bay of Fundy through Statistical Modeling
Reynaldo Popoli , PhD, Medical Neuroscience
How a life changes forever in just 12 months
Kaela Trumble, MSc, Rehabilitation Research
How will your heart age?
Eniko Zsoldos , PhD, Chemistry
Improving Battery Sustainability by Limiting Charging
Divya Rathore , PhD, Physics and Atmospheric Science
Many Shades of Green
Sophie Inkpen , MSc, Kinesiology
Taking Action Through Activity: A Program for Patients with Acquired Brain Injury
Pooyan Moradi , PhD, Medical Neuroscience
Cloudy with a Chance of Epilepsy
Fatemeh Mahdizadeh Karizaki , PhD in Health
Promoting Health and Wellbeing: Access and Inclusion to Childcare and Early Learning for Children with Disabilities in Nova Scotia
Dal News welcomes discussion from members of the Dalhousie community and beyond, but urge comment writers to be respectful and refrain from personal attacks. False or unsubstantiated allegations, libellous statements and offensive language are not allowed. External links must be appropriate and relevant to the subject being discussed.
We encourage commenters to use their real first and last names.
Please note that comments that appear on the site are not the opinion of Dal News or Dalhousie University but only of the comment writer. The editors reserve the right to post, or not to post comments, edit or not edit, at their discretion.
Halifax, Nova Scotia, Canada B3H 4R2 1-902-494-2211
Agricultural Campus Truro, Nova Scotia, Canada B2N 5E3 1-902-893-6600
- Campus Directory
- Student Career Services
- Employment with Dalhousie
- For Parents
- For Employers
- Privacy Statement
- Terms of Use
Dalhousie University Halifax, Nova Scotia, Canada B3H 4R2 1.902.494.2211
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Medical Student Research Journals: The International Journal of Medical Students (IJMS) Legacy
Kiera liblik.
1 BSc. Faculty of Medicine, Queen’s University, Kingston, ON, Canada. Associate Editor, IJMS
Patricio Garcia-Espinosa
2 Social Service Medical Doctor. School of Medicine, Universidad Autónoma de Nuevo León, Monterrey, México and Mexican Institute of Social Security. Palliative Care Unit. High Specialty Medical Unit #25, Monterrey, México. Student Editor, IJMS
Ahmed Nahian
3 BS/DO Medical Student. California Baptist University-Lake Erie College of Osteopathic Medicine, Riverside, CA. United States. Student Editor, IJMS
Surobhi Chatterjee
4 MBBS, Intern Doctor. Department of Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India. Student Editor, IJMS
Mihnea-Alexandru Găman
5 MD, PhD student. Faculty of Medicine, “Carol Davila” University of Medicine and Pharmacy, 050474 Bucharest, Romania & Department of Hematology, Center of Hematology and Bone Marrow Transplantation, Fundeni Clinical Institute, 022328 Bucharest, Romania. Scientific Editor, IJMS
6 Medical Student. Humanitas University, Humanitas Research Hospital, Milan, Italy. Deputy Editor, IJMS
Juan C. Puyana
7 MD, FRCSC, FACS, FACCP. School of Medicine, Department of Surgery, Professor of Surgery, Critical Care Medicine, and Clinical Translational Science, Director for Global Health-Surgery, University of Pittsburgh, Pittsburgh, PA, United States. Editorial Board Member, IJMS
Francisco J. Bonilla-Escobar
8 MD, MSc, PhD(c). Researcher, Department of Ophthalmology; Institute for Clinical Research Education (ICRE), University of Pittsburgh, Pittsburgh, PA, United States. CEO, Fundación Somos Ciencia al Servicio de la Comunidad, Fundación SCISCO/Science to Serve the Community Foundation, SCISCO Foundation, Cali, Colombia. Grupo de investigación en Visión y Salud Ocular, VISOC, Universidad del Valle, Cali, Colombia. Editor in Chief, IJMS
Author Contributions
As the longest-standing, non-interrupted, International Journal for Medical Students with a high impact, visibility, and an international inclusive editorial board, the objective of the International Journal of Medical Students (IJMS) is to be the primary diffusion platform for early-career scientists in medicine, using evidence-based standards in the process of scientific publication. 1 It is crucial that medical students are valued and credited for their work which, in turn, can lead to tremendous impact on the quality of research output generated and education of the next generation of the global medical-scientific community. This objective has been met since 2013 with the first issue of the IJMS, starting from a unique idea reached during a discussion at an international congress of medical students in 2009. 1 , 2
Since, the history of the IJMS has been anything but meager. It has achieved a significant milestone sought by emerging medical journals worldwide; the indexing of a publication in PubMed Central (PMC). 2 A group of researchers, including medical students, were funded by the National Institute of Health (NIH) of the United States and chose IJMS for their high-quality article. 3 This demonstrates that, indeed, a journal focusing on medical students and created and edited by themselves is not at odds with quality, despite traditional misconceptions. 4
Times are changing. The process of scientific production has traditionally ‘punished’ medical students, in the words of Corral-Reyes, I. 5 The process that the medical student must carry out is even greater than those that some renowned authors must take, even if they are practically the same. The publication process is complicated not because of the lack of quality but because of the stigma around their scientific production. Although, as the same author emphasizes, there is a lack of valuation of their own work and lack of expertise when it comes to perceiving how, when, and where to publish; the absence of a publication culture. 5
Therefore, it is necessary to encourage medical student journals to value student growth and commitment to research, giving rise to space for visualization and training. This culture began in Latin America in 1961 with the Cuban magazine “16 de Abril” (April 16). 5 This tradition of more than 60 years is precisely what has opened and seeded the path for journals like the IJMS to flourish in a difficult and sometimes arid environment for medical student research.
What started as an international project from Latin-America has become a Journal whose team represents 34 different nationalities across all the continents, made up of researchers, mentors, and experts in various fields of medicine. The IJMS focuses on the growth and expansion of the scientific medical-student community. Thus, creating a space not only for sharing science and innovation, but a voice behind the experiences, failures, and hardships inclusive and representative of the diverse, dynamic, medical student global community. Moreover, it is important to highlight that all Student and Associate Editors of the IJMS, as well as its Executive Committee, are graduates of the peer-review training courses offered by Web of Science Academy.
The scientific literature includes a wide range of medical student journals, pursuing different objectives, goals, and strategies to achieve their respective aims. An overview of these journals is shown in Table 1 (excluding those that do not publish original research).
Medical Student Research Journals Around the World.
Considering only Journals with Original Articles and Medical Students as authors.
AMSJ: Australian Medical Student Journal, AMSRJ: American Medical Student Research Journal, ANACEM: Asociación Nacional Científica de Estudiantes de Medicina, CIMEL: Ciencia e Investigación Médica Estudiantil Latinoamericana, CRMJ: Cooper Rowan Medical Journal, DMJ: Dalhousie Medical Journal, FMSRJ: Florida Medical Student Research Journal, FMSRP: Florida Medical Student Research Publications, IJMS: International Journal of Medical Students, NZMSJ: New Zealand Medical Student Journal, SJHR-Africa: Students’ Journal of Health Research Africa, UBCMJ: University of British Columbia Medical Journal, UTMJ: University of Toronto Medical Journal.
Those data not found are marked with the legend N/D: No Data.
Although the success of these journals has been noteworthy and has been framed by decades of continuous publication, others, sadly, have not been able to prevail to the challenge of publishing scientific articles by medical students. Particularly, these journals have the tasks of reviewing, editing, and publishing; which sometimes must be accompanied by correction, education, and teaching of the next generation of medical scientists. This is not a small task and has led to the demise of these journals. Among them we can find the Medical Student Journal of Australia, Trinity Student Medical Journal, Asian Student Medical Journal Genesis, MJM, International Journal of Students’ Research, Dares Salam Medical Students’ Journal, Scottish Universities Medical Journal, Acta Cientifica Estudiantil, Esculapio, SCEMUSS, SCientifica, among others. 27 , 28
Though the IJMS is published in English for ease of integration into mainstream literature, the IJMS has a tremendous advantage in that our diversity of authors encompasses 39 different countries in the past year alone. 26 Accordingly, we are newly integrating a summary for non-scientific audiences of each article in the language where the research was carry out. This serves to streamline the translation of scientific knowledge, allowing easy access for knowledge users in the context in which the research was conducted.
The present issue, composed of 16 articles, showcases work by authors from a wide variety of countries, including India, Mexico, the Philippines, the United Kingdom, Kenya, Ireland, and different parts of the United States. Authors include students, early career researchers, and mentors with impressive academic qualifications. To believe that because a journal is formative, orienting, and attractive to medical students, that it is less impactful is to proverbially judge a book by its cover. Some of the greatest revolutions in medicine and beyond were led by trainees and the IJMS aims to be one such in providing academic representation to students.
In this issue, we are publishing 10 original research papers: 7 original articles, 1 short communication, 1 review, and 1 case report. In addition, we are publishing 6 experiences from medical students worldwide that could be of help when facing the realities of medical education. The contents of this work is summarized, as follows.
In addition, we are publishing six experiences from medical students worldwide to aid in understanding the realities of medical education during a time of global unrest. First, an editorial about the war on Ukraine and how this is impacting medical education in the country. This is the first time that the IJMS has published an editorial on political conflict. Though, as discussed in the previous IJMS volume, medical students are global citizens and affected by global situations, such as wars and climate change. 29 – 31 It is critical that these issues be discussed and addressed. In our editorial we make a call for violent conflict to be halted and to use discussion and collaboration in the context of political discourse. 32
Due to the high degree of reported distress experienced by medical trainees, it is critical that reliable metrics are developed to elucidate key stressors in this population. Thus, medical student Montano et al. sought to determine the reliability of the Medical Student Stressor Questionnaire. They determined that the reliability of the questionnaire is excellent and that stressors varied by sex. 33 In terms of measuring perceived competency, recent medical school graduate Canton et al. assessed the efficacy of a surgical scrubbing, gowning, and gloving checklist for trainees. Their checklist had high inter-rater reliability and internal consistency. 34 Another interesting study on training, a cross-sectional study conducted with the fifth-year medical student Nidhi Thomas, showed that of students who chose an elective rotation, the minority pursued a specialty in that discipline. 35 Notably, Huang et al. found that one of the barriers to matching to specialties is socioeconomic inequality impacting interviews due to connection and audio problems. 36 It is similarly important that the perspectives of medical educators be integrated in the evaluation of education. Educators have had to adapt to online teaching during the COVID-19 pandemic, with a lack of adequate warning or training. Final-year medical student Andrew Thomas collaborated with a team of investigators to determine educators’ attitudes to online learning. They reported a need for better infrastructure to support interactive learning in an online format. Interestingly, almost half of the participants supported continued online learning. 37
Beyond online learning, telecommunication is one of the most utilized medical tools during the COVID-19 pandemic. Park et al. describe the role of telerehabilitation as a safe, accessible, efficient, and comfortable alternative to in-person interventions for people with spinal cord injuries. 38 The pandemic has also influenced bedside care. Accordingly, Farley et al. present an epidemiological profile of a pediatric hospital before and during the COVID-19 pandemic. They describe a significant decrease in the number of patients admitted for respiratory conditions and speculate the reasons for this stark change. 39 Another study focused on pediatric medicine was conducted by Murerwa et al., critically reviewing the literature on prenatal and postnatal mercury exposure due to skin lightening agents with inorganic mercury. The authors advocate that prevention is the only way to reduce mercury poisoning and toxicity. 40
Patient advocacy is an important role of the medical professional, including gender diverse patients. Bonasia K, et al. highlighted differences in access to healthcare for transgender and gender-diverse patients. Their article sought to determine knowledge and perception on the subject by medical students and institutions. They conclude that clinical skills were less valued when dealing with non-binary patients as compared to a cis-gender patients. 41 Another point where improvement must be made in medical education is in teaching on commonly missed and misdiagnosed diseases. Urs et al. present a case on Dyke-Davidoff-Masson syndrome, a commonly missed and serious cause of refractory epilepsy which requires an understanding of pertinent imaging and clinical reasoning. 42 Interestingly, although ischemic heart disease is the leading global cause of death there is a lack of literature discussing the predictors of early versus late readmission to hospital following discharge for an ischemic event. Third-year medical student George Cholack et al. conducted a retrospective study of patients hospitalized for acute coronary syndrome and found that female patients were more likely to have late rehospitalization as well as non-white individuals, and those who initially required intensive care unit admission. This information can be used to inform follow-up after ischemic heart events, aiming to reduce morbidity and mortality. 43
Finally, important perspectives of medical trainees are highlighted. Patricio Garcia-Espinosa shares his experience as the first cohort of undergraduates allowed to rotate in the palliative care ward in Mexico. His impactful description of the role of palliative medicine, the need for undergraduates to learn and rotate in this specialty, and its inclusion in the undergraduate curriculum is worth reflecting upon. 44 Similarly, Waisberg shares an experience of an “eye opening” mission trip to an underserved community in Montemorelos, Mexico that provided him new contacts, mentors, networking possibilities, and novel cultural experiences in different nations are all important insights into a specialty. 45 On the other side of the world, Rocha et al. describes an experience of post-graduate interns helping their community by participating in COVID-19 vaccination drives in the Philippines, gaining practical knowledge and hands-on experience. 46 Patel et al. also describe inaccessible and inequitable care, but for dermatological disease in underrepresented and underserved communities forming the basis of the Student Dermatological Clinic for the Underserved and a collaborative service-learning model in Pittsburgh. 47 Another student initiative, Mulwalkar describes the journey of creating a student-oriented research and innovation council, ASPIRE, in India. 48
We hope that you enjoy reading this issue as we did in making it a reality. This is a tremendous effort of more than 70 team members volunteering to make the vision of showcasing medical students research a reality.
Conflict of Interest Statement & Funding
The Authors have no conflicts of interest to disclose. Dr. Juan C. Puyana work is partially funded by the National Institute of Health (NIH) of the United States with the grant 5UG3HL151595. The opinions expressed in this article are the author’s own and do not reflect the view of the National Institutes of Health, the Department of Health and Human Services, or the United States government.
- Seeking Patient Care?
Home / News / Grants and Awards / Graduate Studies
Graduate Students’ Discoveries Shine During Best Research Awards

Each year, the University of Miami Miller School of Medicine’s Medical Faculty Association honors Ph.D. students with Best Research Awards. This year, students researching cancer, HIV and cerebral amyloid angiopathy garnered the awards.
“The annual Best Research Awards highlight the powerful and innovative research our Ph.D. students conduct,” said Ana Fiallos, Ph.D., director of career services for the Office of Graduate Studies. “While we can only have four winners, the recognition is a testament to the hard work and creativity our students and faculty show every day.”
Fighting Brain Tumors
Fourth-place awardee Jiaqi Liu studies gliomas, a type of brain tumor, in the Zhai Lab. Her work has shown that the protein NMNAT, an enzyme crucial in the final step of nicotinamide adenine dinucleotide (NAD+) synthesis, plays a significant role in the growth and progression of gliomas.
Experiments with fruit flies which were validated in human glioma cells showed that increased NMNAT activity allowed glial cells with harmful mutations to survive and multiply. This work could offer two advantages. NMNAT could be used as a biomarker to identify patients at high risk for cancer progression. It could also be used as a therapeutic target.
“It’s possible to develop an inhibitor that targets this protein to suppress brain tumors before they become deadly,” said Liu. “We could potentially use such an inhibitor in the brain after surgery to help eliminate residual cancer.”
HIV-Associated Neurocognitive Disorders
Third place went to Oandy Naranjo in the Toborek Lab. Naranjo investigates the consequences of HIV-1 infection and focuses on HIV-associated neurocognitive disorders. He is studying cells in the blood-brain barrier (BBB), called pericytes, that harbors HIV and may contribute to cognitive loss.
Anti-retroviral drugs do not penetrate the BBB as well as other parts of the body. Infected cells produce viral particles, which generate inflammation. Though HIV patients can live almost normal life spans, this long-term inflammation can have a powerful impact on the brain. Naranjo wants to understand how pericytes behave differently when infected and hopes these insights will lead to treatments.
“We created a big database of latent, active and uninfected cells and how they’re different from each other,” said Naranjo. “This could give us insights into how specific genes could be used to treat HIV-associated neurocognitive disorders.”
Cerebral Amyloid Angiopathy
Olivia Osborne, who placed second, also works in the Toborek Lab, studying the molecular mechanisms that affect post-stroke neurogenesis (brain tissue growth) in people with cerebral amyloid angiopathy (CAA). Osborne was awarded an F31 fellowship from the National Institutes of Health to advance her dissertation on “Ischemic Stroke in Cerebral Amyloid Angiopathy: Microvascular Injury and Recovery.”
In CAA, amyloid beta (Aβ) proteins, which have been linked to Alzheimer’s disease, weaken small blood vessels, sometimes causing bleeding. Osborne wants to understand how these mechanisms affect people who have suffered a stroke.
“My central hypothesis is that Aβ accumulation in cerebral vasculature exacerbates ischemic stroke outcomes and delays post-stroke recovery,” said Osborne. “My work focuses on the blood vessels after damage occurs. There’s some sort of dysregulation that might disrupt signaling to other cells in the area and delay recovery. If we can find that signaling pathway, we could potentially target it therapeutically.”
Chronic Lymphocytic Leukemia
Skye Montoya from the Taylor Lab won top Best Research Award honors. She studies mutations in chronic lymphocytic leukemia (CLL), focusing on Bruton’s tyrosine kinase (BTK), an enzyme that drives cancer growth.
Montoya wants to identify small molecules that could regulate BTK and slow or even stop CLL. Cancers have a bad habit of learning how to resist targeted therapies, and Montoya and colleagues are trying to figure out ways to overcome that resistance. Montoya was first author on a recent paper, published in the journal “Science,” that identified previously unknown BTK mutations and showed a potential therapy (NX-2127) could be effective.
“Each BTK mutant we study can cause resistance to multiple BTK inhibitors, which can really limit therapeutic options for patients harboring these mutations,” said Montoya. “We were all excited to see positive responses in both cell lines and patients, regardless of BTK mutational status.”
Tags: Best Research Awards , Medical Faculty Association
Graduate Student Creates App to Aid Brain Recovery
Olivia Osborne created a mobile app that tracks cognitive function and dovetails with her research on stroke and the brain.
Mentor and Mentee: A Win-Win
With several collaborative studies behind them, Justin Taylor, M.D., and mentee Skye Montoya look forward to even more promising research.
Ph.D. Students Receive Research Internships at Eli Lilly, Merck
Three Miller School of Medicine Ph.D. students will be extending their training after accepting internships at the prominent companies.
- Clinical Care
- Community Outreach
- Grants and Awards
- Medical Education
- Research and Innovation
- Infectious Diseases
- Neurosciences
- Ophthalmology
- Orthopaedics
- Otolaryngology
- Philanthropy
- Cardiovascular Medicine
- Digestive Health and Liver Diseases
Share this Story
This article was printed from The Miller School of Medicine Medical News at the following URL: https://news.med.miami.edu/medical-faculty-association-best-research-awards/
Copyright © 2024 University of Miami Health System


VIDEO
COMMENTS
The American Medical Association offers a wide range of resources and programs to get you started and thriving in research, gaining valuable hands-on experience you can build on throughout your career. With an AMA membership, medical students can take advantage of these opportunities: Research Challenge: March 17, 2023-Feb. 29, 2024 ...
Furthermore, there are barriers within medical education systems that further hinder students' exposure and participation in research. Medical students are deterred by the practical difficulties such as the lack of learning opportunities , and challenges in securing research-associated opportunities, particularly if they lack relevant skills .
Medical students reported positive attitudes toward research. 1-3 Studies have shown that students' involvement in research is strongly associated with post-graduate research initiatives. 4 Students must develop a positive attitude toward scientific research from the start of their medical careers.
Participating in research gives students great skills and opportunities. Anna Taylor and Sarah Purdy explain how to get started ### This article contains: Students often go into medicine because of a desire to help others and improve patients' physical and mental wellbeing. In the early years of medical school, however, it can seem as if you are not making much difference to patient care ...
The multidisciplinary research team included a psychologist working in medical education, two medical students, and two Foundation level doctors. The team's direct experience of the phenomenon studied was an important resource throughout the research process, and the researchers regularly reflected on how their subjective experiences and ...
Introduction. Research and scholarly pursuits are an important aspect of any medical student's training. A meta-analysis of medical student research found that 72% of medical students were interested in performing research, and 31% of medical students were interested in a career that involved research [Reference Amgad, Man Kin Tsui, Liptrott and Shash 1].
Medical education is a time wrought with personal and professional stressors, posing serious challenges to maintaining student wellness. Extensive research has thus been conducted to identify ...
1.1. Research in the medical career: when and why? The main reason for researching and publishing high quality scientific articles lies in learning to use and critique evidence for responsible decision making based on it, trying to avoid as much as possible medical failures during clinical practice [11,12].On the other hand, this tool helps to optimize overall critical thinking, personal ...
Research in Medical Education: A Primer for Medical Students II. Why should I do a MedEd research project? Why are medical students especially qualified to do MedEd research? As medical students, you are front and center of the medical education process! Oftentimes, great ideas about "what works" in education are dashed on the shoals of ...
Background Research is essential for advancing medical knowledge and improving patient care. However, research capacity and output are low in low- and middle-income countries due to various challenges, including a lack of research training among medical students. Integrating research training into undergraduate medical curricula can help address this issue. Methods A cross-sectional study was ...
Importance: Despite the rapidly declining number of physician-investigators, there is no consistent structure within medical education so far for involving medical students in research. Objective: To conduct an integrated mixed-methods systematic review and meta-analysis of published studies about medical students' participation in research, and to evaluate the evidence in order to guide ...
Student Research. HMS MD students will find hundreds of opportunities to carry out research, from hypothesis-based research in the basic and clinical sciences to research in the social sciences, arts and medical humanities. Faculty at Harvard-based labs and affiliated hospitals all offer opportunities for HMS students.
Summer programs at the National Institutes of Health (NIH) provide an opportunity to spend a summer working at the NIH side-by-side with some of the leading scientists in the world, in an environment devoted exclusively to biomedical research. Find opportunities available for current medical students.
Comprehensive Guide to Research from the Perspective of a Medical Student. By Dmitry Zavlin, M.D. February 9, 2017. Medical Student, Pre-med. Research. LinkedIn. G uest post from Dmitry Zavlin, MD, a research fellow in Houston, Texas. He has been highly productive in his research endeavors and below describes a comprehensive guide to getting ...
Search "medical student research" or "medsoc research" into Facebook and lots of groups and pages will pop up, including UCL MedSoc Research and Academic Medicine (there is a Research Mentoring Scheme Mentee Scheme), NSAMR - National Student Association of Medical Research and International Opportunities for Medical Students. Twitter
The Office of Medical Student Research is committed to helping you have a productive and positive experience, whatever your previous research background. We have numerous resources available, including a needs assessment delivered to all incoming medical students, in-person workshops, online learning modules, an easy-to-use website that links ...
GW SMHS medical students can explore the following: Medical Student Research: Beaumont Society. Medical Student Funding. Research Scholarly Concentration. METEOR. Fusion magazine. Research is a key feature of the GW experience and mission. GW and our partners at Children's National Hospital work together on the CTSI-CN to enhance Clinical and ...
According to analyses of student publications, 86% of Johns Hopkins medical students graduating in the years 2011-2020 publish at least one manuscript based on research done in medical school [mean (SD) of 3.1 (3.8) publications per student]. The majority (56%) of students published at least one manuscript as first author [mean (SD) of 1.2 (1.7 ...
Involving medical students in research. Undergraduate research is not a new phenomenon in medicine. Charles Best was a medical student at the time that he and his supervisor, Frederick Banting, discovered insulin. Insulin arises from the pancreatic islets of Längerhans, themselves discovered in 1869 by medical student Paul Längerhans.
Boston University Medical Student Research. There are numerous opportunities for medical students to engage in mentored research projects at Boston University Chobanian & Avedisian School of Medicine. We are here to help connect you to these resources. Research Year Program Application Due March 15!
The Office for Research and Scholarship is dedicated to supporting DGSOM medical students' interest in research and scholarly work. For the academic Year 2023-2024, we are able to offer up to $600 in support to all DGSOM students who have had their research abstract accepted to a journal, meeting, or conference.
The NIH Medical Research Scholars Program (MRSP) helps medical, dental and veterinary students enter the pathway to biomedical research careers. 2024-2025 MRSP application period to be announced. The National Institutes of Health (NIH) Medical Research Scholars Program (MRSP) is a comprehensive, yearlong research enrichment program designed to ...
In 2015-16, 20 percent of trainees dismissed from their residency were Black, although Black students make up only 5 percent of residents, according to unpublished data from the Accreditation ...
Ben Caruso and Xiang Yu Gao, both first-year medical students at the WSU College of Medicine, presented a poster at the Inland Northwest Research Symposium on the WSU Spokane campus this week. Their case report is intended to raise awareness of potential complications following a Roux-en-Y gastric bypass surgery in patients with diffuse large B ...
Understanding what influences medical students' evaluations of their schools' public health emergency management and responses could help colleges and universities in China improve their emergency management strategies This study found that the satisfaction score of the timeliness of prevention and control measures taken by schools was the ...
More than half of the 115 students who matched — 54% — will join a primary care residency following graduation. The inner workings of the matchmaker. Medical students spend part of their final year in school deciding which specialty field and training program to pursue.
Pooyan Moradi, another PhD student in medical neuroscience, and Kaela Trumble, a master's student in rehabilitation research, were also selected as top finalists by the judging panel. Moradi earned second place and a $500 prize, presenting on the use of artificial intelligence to detect seizures in animals and how this model can be applied to ...
It has achieved a significant milestone sought by emerging medical journals worldwide; the indexing of a publication in PubMed Central (PMC). 2 A group of researchers, including medical students, were funded by the National Institute of Health (NIH) of the United States and chose IJMS for their high-quality article. 3 This demonstrates that ...
"The annual Best Research Awards highlight the powerful and innovative research our Ph.D. students conduct," said Ana Fiallos, Ph.D., director of career services for the Office of Graduate Studies. "While we can only have four winners, the recognition is a testament to the hard work and creativity our students and faculty show every day."