Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- How to Write a Literature Review | Guide, Examples, & Templates

How to Write a Literature Review | Guide, Examples, & Templates
Published on January 2, 2023 by Shona McCombes . Revised on September 11, 2023.
What is a literature review? A literature review is a survey of scholarly sources on a specific topic. It provides an overview of current knowledge, allowing you to identify relevant theories, methods, and gaps in the existing research that you can later apply to your paper, thesis, or dissertation topic .
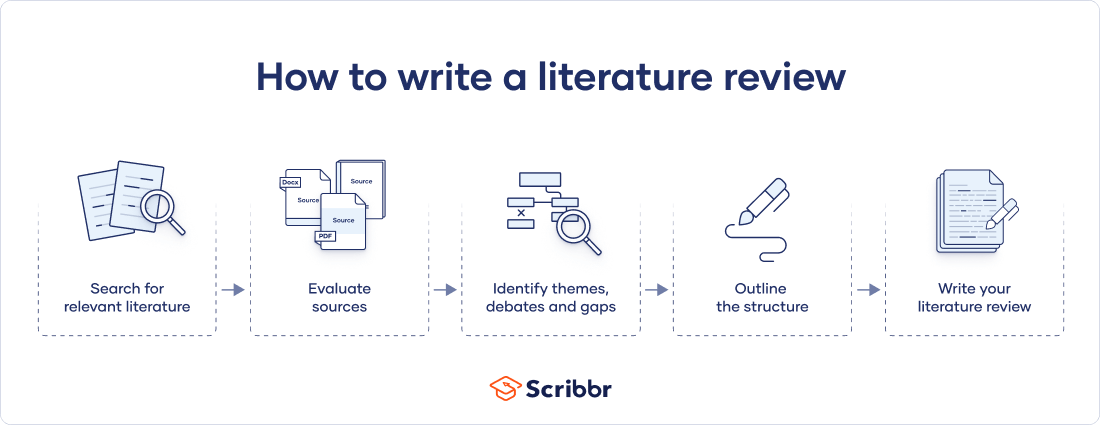
There are five key steps to writing a literature review:
- Search for relevant literature
- Evaluate sources
- Identify themes, debates, and gaps
- Outline the structure
- Write your literature review
A good literature review doesn’t just summarize sources—it analyzes, synthesizes , and critically evaluates to give a clear picture of the state of knowledge on the subject.
Instantly correct all language mistakes in your text
Upload your document to correct all your mistakes in minutes

Table of contents
What is the purpose of a literature review, examples of literature reviews, step 1 – search for relevant literature, step 2 – evaluate and select sources, step 3 – identify themes, debates, and gaps, step 4 – outline your literature review’s structure, step 5 – write your literature review, free lecture slides, other interesting articles, frequently asked questions, introduction.
- Quick Run-through
- Step 1 & 2
When you write a thesis , dissertation , or research paper , you will likely have to conduct a literature review to situate your research within existing knowledge. The literature review gives you a chance to:
- Demonstrate your familiarity with the topic and its scholarly context
- Develop a theoretical framework and methodology for your research
- Position your work in relation to other researchers and theorists
- Show how your research addresses a gap or contributes to a debate
- Evaluate the current state of research and demonstrate your knowledge of the scholarly debates around your topic.
Writing literature reviews is a particularly important skill if you want to apply for graduate school or pursue a career in research. We’ve written a step-by-step guide that you can follow below.
Here's why students love Scribbr's proofreading services
Discover proofreading & editing
Writing literature reviews can be quite challenging! A good starting point could be to look at some examples, depending on what kind of literature review you’d like to write.
- Example literature review #1: “Why Do People Migrate? A Review of the Theoretical Literature” ( Theoretical literature review about the development of economic migration theory from the 1950s to today.)
- Example literature review #2: “Literature review as a research methodology: An overview and guidelines” ( Methodological literature review about interdisciplinary knowledge acquisition and production.)
- Example literature review #3: “The Use of Technology in English Language Learning: A Literature Review” ( Thematic literature review about the effects of technology on language acquisition.)
- Example literature review #4: “Learners’ Listening Comprehension Difficulties in English Language Learning: A Literature Review” ( Chronological literature review about how the concept of listening skills has changed over time.)
You can also check out our templates with literature review examples and sample outlines at the links below.
Download Word doc Download Google doc
Before you begin searching for literature, you need a clearly defined topic .
If you are writing the literature review section of a dissertation or research paper, you will search for literature related to your research problem and questions .
Make a list of keywords
Start by creating a list of keywords related to your research question. Include each of the key concepts or variables you’re interested in, and list any synonyms and related terms. You can add to this list as you discover new keywords in the process of your literature search.
- Social media, Facebook, Instagram, Twitter, Snapchat, TikTok
- Body image, self-perception, self-esteem, mental health
- Generation Z, teenagers, adolescents, youth
Search for relevant sources
Use your keywords to begin searching for sources. Some useful databases to search for journals and articles include:
- Your university’s library catalogue
- Google Scholar
- Project Muse (humanities and social sciences)
- Medline (life sciences and biomedicine)
- EconLit (economics)
- Inspec (physics, engineering and computer science)
You can also use boolean operators to help narrow down your search.
Make sure to read the abstract to find out whether an article is relevant to your question. When you find a useful book or article, you can check the bibliography to find other relevant sources.
You likely won’t be able to read absolutely everything that has been written on your topic, so it will be necessary to evaluate which sources are most relevant to your research question.
For each publication, ask yourself:
- What question or problem is the author addressing?
- What are the key concepts and how are they defined?
- What are the key theories, models, and methods?
- Does the research use established frameworks or take an innovative approach?
- What are the results and conclusions of the study?
- How does the publication relate to other literature in the field? Does it confirm, add to, or challenge established knowledge?
- What are the strengths and weaknesses of the research?
Make sure the sources you use are credible , and make sure you read any landmark studies and major theories in your field of research.
You can use our template to summarize and evaluate sources you’re thinking about using. Click on either button below to download.
Take notes and cite your sources
As you read, you should also begin the writing process. Take notes that you can later incorporate into the text of your literature review.
It is important to keep track of your sources with citations to avoid plagiarism . It can be helpful to make an annotated bibliography , where you compile full citation information and write a paragraph of summary and analysis for each source. This helps you remember what you read and saves time later in the process.
The only proofreading tool specialized in correcting academic writing - try for free!
The academic proofreading tool has been trained on 1000s of academic texts and by native English editors. Making it the most accurate and reliable proofreading tool for students.

Try for free
To begin organizing your literature review’s argument and structure, be sure you understand the connections and relationships between the sources you’ve read. Based on your reading and notes, you can look for:
- Trends and patterns (in theory, method or results): do certain approaches become more or less popular over time?
- Themes: what questions or concepts recur across the literature?
- Debates, conflicts and contradictions: where do sources disagree?
- Pivotal publications: are there any influential theories or studies that changed the direction of the field?
- Gaps: what is missing from the literature? Are there weaknesses that need to be addressed?
This step will help you work out the structure of your literature review and (if applicable) show how your own research will contribute to existing knowledge.
- Most research has focused on young women.
- There is an increasing interest in the visual aspects of social media.
- But there is still a lack of robust research on highly visual platforms like Instagram and Snapchat—this is a gap that you could address in your own research.
There are various approaches to organizing the body of a literature review. Depending on the length of your literature review, you can combine several of these strategies (for example, your overall structure might be thematic, but each theme is discussed chronologically).
Chronological
The simplest approach is to trace the development of the topic over time. However, if you choose this strategy, be careful to avoid simply listing and summarizing sources in order.
Try to analyze patterns, turning points and key debates that have shaped the direction of the field. Give your interpretation of how and why certain developments occurred.
If you have found some recurring central themes, you can organize your literature review into subsections that address different aspects of the topic.
For example, if you are reviewing literature about inequalities in migrant health outcomes, key themes might include healthcare policy, language barriers, cultural attitudes, legal status, and economic access.
Methodological
If you draw your sources from different disciplines or fields that use a variety of research methods , you might want to compare the results and conclusions that emerge from different approaches. For example:
- Look at what results have emerged in qualitative versus quantitative research
- Discuss how the topic has been approached by empirical versus theoretical scholarship
- Divide the literature into sociological, historical, and cultural sources
Theoretical
A literature review is often the foundation for a theoretical framework . You can use it to discuss various theories, models, and definitions of key concepts.
You might argue for the relevance of a specific theoretical approach, or combine various theoretical concepts to create a framework for your research.
Like any other academic text , your literature review should have an introduction , a main body, and a conclusion . What you include in each depends on the objective of your literature review.
The introduction should clearly establish the focus and purpose of the literature review.
Depending on the length of your literature review, you might want to divide the body into subsections. You can use a subheading for each theme, time period, or methodological approach.
As you write, you can follow these tips:
- Summarize and synthesize: give an overview of the main points of each source and combine them into a coherent whole
- Analyze and interpret: don’t just paraphrase other researchers — add your own interpretations where possible, discussing the significance of findings in relation to the literature as a whole
- Critically evaluate: mention the strengths and weaknesses of your sources
- Write in well-structured paragraphs: use transition words and topic sentences to draw connections, comparisons and contrasts
In the conclusion, you should summarize the key findings you have taken from the literature and emphasize their significance.
When you’ve finished writing and revising your literature review, don’t forget to proofread thoroughly before submitting. Not a language expert? Check out Scribbr’s professional proofreading services !
This article has been adapted into lecture slides that you can use to teach your students about writing a literature review.
Scribbr slides are free to use, customize, and distribute for educational purposes.
Open Google Slides Download PowerPoint
If you want to know more about the research process , methodology , research bias , or statistics , make sure to check out some of our other articles with explanations and examples.
- Sampling methods
- Simple random sampling
- Stratified sampling
- Cluster sampling
- Likert scales
- Reproducibility
Statistics
- Null hypothesis
- Statistical power
- Probability distribution
- Effect size
- Poisson distribution
Research bias
- Optimism bias
- Cognitive bias
- Implicit bias
- Hawthorne effect
- Anchoring bias
- Explicit bias
A literature review is a survey of scholarly sources (such as books, journal articles, and theses) related to a specific topic or research question .
It is often written as part of a thesis, dissertation , or research paper , in order to situate your work in relation to existing knowledge.
There are several reasons to conduct a literature review at the beginning of a research project:
- To familiarize yourself with the current state of knowledge on your topic
- To ensure that you’re not just repeating what others have already done
- To identify gaps in knowledge and unresolved problems that your research can address
- To develop your theoretical framework and methodology
- To provide an overview of the key findings and debates on the topic
Writing the literature review shows your reader how your work relates to existing research and what new insights it will contribute.
The literature review usually comes near the beginning of your thesis or dissertation . After the introduction , it grounds your research in a scholarly field and leads directly to your theoretical framework or methodology .
A literature review is a survey of credible sources on a topic, often used in dissertations , theses, and research papers . Literature reviews give an overview of knowledge on a subject, helping you identify relevant theories and methods, as well as gaps in existing research. Literature reviews are set up similarly to other academic texts , with an introduction , a main body, and a conclusion .
An annotated bibliography is a list of source references that has a short description (called an annotation ) for each of the sources. It is often assigned as part of the research process for a paper .
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
McCombes, S. (2023, September 11). How to Write a Literature Review | Guide, Examples, & Templates. Scribbr. Retrieved April 9, 2024, from https://www.scribbr.com/dissertation/literature-review/
Is this article helpful?
Shona McCombes
Other students also liked, what is a theoretical framework | guide to organizing, what is a research methodology | steps & tips, how to write a research proposal | examples & templates, unlimited academic ai-proofreading.
✔ Document error-free in 5minutes ✔ Unlimited document corrections ✔ Specialized in correcting academic texts
Purdue Online Writing Lab Purdue OWL® College of Liberal Arts
Writing a Literature Review

Welcome to the Purdue OWL
This page is brought to you by the OWL at Purdue University. When printing this page, you must include the entire legal notice.
Copyright ©1995-2018 by The Writing Lab & The OWL at Purdue and Purdue University. All rights reserved. This material may not be published, reproduced, broadcast, rewritten, or redistributed without permission. Use of this site constitutes acceptance of our terms and conditions of fair use.
A literature review is a document or section of a document that collects key sources on a topic and discusses those sources in conversation with each other (also called synthesis ). The lit review is an important genre in many disciplines, not just literature (i.e., the study of works of literature such as novels and plays). When we say “literature review” or refer to “the literature,” we are talking about the research ( scholarship ) in a given field. You will often see the terms “the research,” “the scholarship,” and “the literature” used mostly interchangeably.
Where, when, and why would I write a lit review?
There are a number of different situations where you might write a literature review, each with slightly different expectations; different disciplines, too, have field-specific expectations for what a literature review is and does. For instance, in the humanities, authors might include more overt argumentation and interpretation of source material in their literature reviews, whereas in the sciences, authors are more likely to report study designs and results in their literature reviews; these differences reflect these disciplines’ purposes and conventions in scholarship. You should always look at examples from your own discipline and talk to professors or mentors in your field to be sure you understand your discipline’s conventions, for literature reviews as well as for any other genre.
A literature review can be a part of a research paper or scholarly article, usually falling after the introduction and before the research methods sections. In these cases, the lit review just needs to cover scholarship that is important to the issue you are writing about; sometimes it will also cover key sources that informed your research methodology.
Lit reviews can also be standalone pieces, either as assignments in a class or as publications. In a class, a lit review may be assigned to help students familiarize themselves with a topic and with scholarship in their field, get an idea of the other researchers working on the topic they’re interested in, find gaps in existing research in order to propose new projects, and/or develop a theoretical framework and methodology for later research. As a publication, a lit review usually is meant to help make other scholars’ lives easier by collecting and summarizing, synthesizing, and analyzing existing research on a topic. This can be especially helpful for students or scholars getting into a new research area, or for directing an entire community of scholars toward questions that have not yet been answered.
What are the parts of a lit review?
Most lit reviews use a basic introduction-body-conclusion structure; if your lit review is part of a larger paper, the introduction and conclusion pieces may be just a few sentences while you focus most of your attention on the body. If your lit review is a standalone piece, the introduction and conclusion take up more space and give you a place to discuss your goals, research methods, and conclusions separately from where you discuss the literature itself.
Introduction:
- An introductory paragraph that explains what your working topic and thesis is
- A forecast of key topics or texts that will appear in the review
- Potentially, a description of how you found sources and how you analyzed them for inclusion and discussion in the review (more often found in published, standalone literature reviews than in lit review sections in an article or research paper)
- Summarize and synthesize: Give an overview of the main points of each source and combine them into a coherent whole
- Analyze and interpret: Don’t just paraphrase other researchers – add your own interpretations where possible, discussing the significance of findings in relation to the literature as a whole
- Critically Evaluate: Mention the strengths and weaknesses of your sources
- Write in well-structured paragraphs: Use transition words and topic sentence to draw connections, comparisons, and contrasts.
Conclusion:
- Summarize the key findings you have taken from the literature and emphasize their significance
- Connect it back to your primary research question
How should I organize my lit review?
Lit reviews can take many different organizational patterns depending on what you are trying to accomplish with the review. Here are some examples:
- Chronological : The simplest approach is to trace the development of the topic over time, which helps familiarize the audience with the topic (for instance if you are introducing something that is not commonly known in your field). If you choose this strategy, be careful to avoid simply listing and summarizing sources in order. Try to analyze the patterns, turning points, and key debates that have shaped the direction of the field. Give your interpretation of how and why certain developments occurred (as mentioned previously, this may not be appropriate in your discipline — check with a teacher or mentor if you’re unsure).
- Thematic : If you have found some recurring central themes that you will continue working with throughout your piece, you can organize your literature review into subsections that address different aspects of the topic. For example, if you are reviewing literature about women and religion, key themes can include the role of women in churches and the religious attitude towards women.
- Qualitative versus quantitative research
- Empirical versus theoretical scholarship
- Divide the research by sociological, historical, or cultural sources
- Theoretical : In many humanities articles, the literature review is the foundation for the theoretical framework. You can use it to discuss various theories, models, and definitions of key concepts. You can argue for the relevance of a specific theoretical approach or combine various theorical concepts to create a framework for your research.
What are some strategies or tips I can use while writing my lit review?
Any lit review is only as good as the research it discusses; make sure your sources are well-chosen and your research is thorough. Don’t be afraid to do more research if you discover a new thread as you’re writing. More info on the research process is available in our "Conducting Research" resources .
As you’re doing your research, create an annotated bibliography ( see our page on the this type of document ). Much of the information used in an annotated bibliography can be used also in a literature review, so you’ll be not only partially drafting your lit review as you research, but also developing your sense of the larger conversation going on among scholars, professionals, and any other stakeholders in your topic.
Usually you will need to synthesize research rather than just summarizing it. This means drawing connections between sources to create a picture of the scholarly conversation on a topic over time. Many student writers struggle to synthesize because they feel they don’t have anything to add to the scholars they are citing; here are some strategies to help you:
- It often helps to remember that the point of these kinds of syntheses is to show your readers how you understand your research, to help them read the rest of your paper.
- Writing teachers often say synthesis is like hosting a dinner party: imagine all your sources are together in a room, discussing your topic. What are they saying to each other?
- Look at the in-text citations in each paragraph. Are you citing just one source for each paragraph? This usually indicates summary only. When you have multiple sources cited in a paragraph, you are more likely to be synthesizing them (not always, but often
- Read more about synthesis here.
The most interesting literature reviews are often written as arguments (again, as mentioned at the beginning of the page, this is discipline-specific and doesn’t work for all situations). Often, the literature review is where you can establish your research as filling a particular gap or as relevant in a particular way. You have some chance to do this in your introduction in an article, but the literature review section gives a more extended opportunity to establish the conversation in the way you would like your readers to see it. You can choose the intellectual lineage you would like to be part of and whose definitions matter most to your thinking (mostly humanities-specific, but this goes for sciences as well). In addressing these points, you argue for your place in the conversation, which tends to make the lit review more compelling than a simple reporting of other sources.
Libraries | Research Guides
Literature reviews, what is a literature review, learning more about how to do a literature review.
- Planning the Review
- The Research Question
- Choosing Where to Search
- Organizing the Review
- Writing the Review
A literature review is a review and synthesis of existing research on a topic or research question. A literature review is meant to analyze the scholarly literature, make connections across writings and identify strengths, weaknesses, trends, and missing conversations. A literature review should address different aspects of a topic as it relates to your research question. A literature review goes beyond a description or summary of the literature you have read.
- Sage Research Methods Core Collection This link opens in a new window SAGE Research Methods supports research at all levels by providing material to guide users through every step of the research process. SAGE Research Methods is the ultimate methods library with more than 1000 books, reference works, journal articles, and instructional videos by world-leading academics from across the social sciences, including the largest collection of qualitative methods books available online from any scholarly publisher. – Publisher
- Next: Planning the Review >>
- Last Updated: Jan 17, 2024 10:05 AM
- URL: https://libguides.northwestern.edu/literaturereviews
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, automatically generate references for free.
- Knowledge Base
- Dissertation
- What is a Literature Review? | Guide, Template, & Examples
What is a Literature Review? | Guide, Template, & Examples
Published on 22 February 2022 by Shona McCombes . Revised on 7 June 2022.
What is a literature review? A literature review is a survey of scholarly sources on a specific topic. It provides an overview of current knowledge, allowing you to identify relevant theories, methods, and gaps in the existing research.
There are five key steps to writing a literature review:
- Search for relevant literature
- Evaluate sources
- Identify themes, debates and gaps
- Outline the structure
- Write your literature review
A good literature review doesn’t just summarise sources – it analyses, synthesises, and critically evaluates to give a clear picture of the state of knowledge on the subject.
Instantly correct all language mistakes in your text
Be assured that you'll submit flawless writing. Upload your document to correct all your mistakes.

Table of contents
Why write a literature review, examples of literature reviews, step 1: search for relevant literature, step 2: evaluate and select sources, step 3: identify themes, debates and gaps, step 4: outline your literature review’s structure, step 5: write your literature review, frequently asked questions about literature reviews, introduction.
- Quick Run-through
- Step 1 & 2
When you write a dissertation or thesis, you will have to conduct a literature review to situate your research within existing knowledge. The literature review gives you a chance to:
- Demonstrate your familiarity with the topic and scholarly context
- Develop a theoretical framework and methodology for your research
- Position yourself in relation to other researchers and theorists
- Show how your dissertation addresses a gap or contributes to a debate
You might also have to write a literature review as a stand-alone assignment. In this case, the purpose is to evaluate the current state of research and demonstrate your knowledge of scholarly debates around a topic.
The content will look slightly different in each case, but the process of conducting a literature review follows the same steps. We’ve written a step-by-step guide that you can follow below.
The only proofreading tool specialized in correcting academic writing
The academic proofreading tool has been trained on 1000s of academic texts and by native English editors. Making it the most accurate and reliable proofreading tool for students.

Correct my document today
Writing literature reviews can be quite challenging! A good starting point could be to look at some examples, depending on what kind of literature review you’d like to write.
- Example literature review #1: “Why Do People Migrate? A Review of the Theoretical Literature” ( Theoretical literature review about the development of economic migration theory from the 1950s to today.)
- Example literature review #2: “Literature review as a research methodology: An overview and guidelines” ( Methodological literature review about interdisciplinary knowledge acquisition and production.)
- Example literature review #3: “The Use of Technology in English Language Learning: A Literature Review” ( Thematic literature review about the effects of technology on language acquisition.)
- Example literature review #4: “Learners’ Listening Comprehension Difficulties in English Language Learning: A Literature Review” ( Chronological literature review about how the concept of listening skills has changed over time.)
You can also check out our templates with literature review examples and sample outlines at the links below.
Download Word doc Download Google doc
Before you begin searching for literature, you need a clearly defined topic .
If you are writing the literature review section of a dissertation or research paper, you will search for literature related to your research objectives and questions .
If you are writing a literature review as a stand-alone assignment, you will have to choose a focus and develop a central question to direct your search. Unlike a dissertation research question, this question has to be answerable without collecting original data. You should be able to answer it based only on a review of existing publications.
Make a list of keywords
Start by creating a list of keywords related to your research topic. Include each of the key concepts or variables you’re interested in, and list any synonyms and related terms. You can add to this list if you discover new keywords in the process of your literature search.
- Social media, Facebook, Instagram, Twitter, Snapchat, TikTok
- Body image, self-perception, self-esteem, mental health
- Generation Z, teenagers, adolescents, youth
Search for relevant sources
Use your keywords to begin searching for sources. Some databases to search for journals and articles include:
- Your university’s library catalogue
- Google Scholar
- Project Muse (humanities and social sciences)
- Medline (life sciences and biomedicine)
- EconLit (economics)
- Inspec (physics, engineering and computer science)
You can use boolean operators to help narrow down your search:
Read the abstract to find out whether an article is relevant to your question. When you find a useful book or article, you can check the bibliography to find other relevant sources.
To identify the most important publications on your topic, take note of recurring citations. If the same authors, books or articles keep appearing in your reading, make sure to seek them out.
You probably won’t be able to read absolutely everything that has been written on the topic – you’ll have to evaluate which sources are most relevant to your questions.
For each publication, ask yourself:
- What question or problem is the author addressing?
- What are the key concepts and how are they defined?
- What are the key theories, models and methods? Does the research use established frameworks or take an innovative approach?
- What are the results and conclusions of the study?
- How does the publication relate to other literature in the field? Does it confirm, add to, or challenge established knowledge?
- How does the publication contribute to your understanding of the topic? What are its key insights and arguments?
- What are the strengths and weaknesses of the research?
Make sure the sources you use are credible, and make sure you read any landmark studies and major theories in your field of research.
You can find out how many times an article has been cited on Google Scholar – a high citation count means the article has been influential in the field, and should certainly be included in your literature review.
The scope of your review will depend on your topic and discipline: in the sciences you usually only review recent literature, but in the humanities you might take a long historical perspective (for example, to trace how a concept has changed in meaning over time).
Remember that you can use our template to summarise and evaluate sources you’re thinking about using!
Take notes and cite your sources
As you read, you should also begin the writing process. Take notes that you can later incorporate into the text of your literature review.
It’s important to keep track of your sources with references to avoid plagiarism . It can be helpful to make an annotated bibliography, where you compile full reference information and write a paragraph of summary and analysis for each source. This helps you remember what you read and saves time later in the process.
You can use our free APA Reference Generator for quick, correct, consistent citations.
To begin organising your literature review’s argument and structure, you need to understand the connections and relationships between the sources you’ve read. Based on your reading and notes, you can look for:
- Trends and patterns (in theory, method or results): do certain approaches become more or less popular over time?
- Themes: what questions or concepts recur across the literature?
- Debates, conflicts and contradictions: where do sources disagree?
- Pivotal publications: are there any influential theories or studies that changed the direction of the field?
- Gaps: what is missing from the literature? Are there weaknesses that need to be addressed?
This step will help you work out the structure of your literature review and (if applicable) show how your own research will contribute to existing knowledge.
- Most research has focused on young women.
- There is an increasing interest in the visual aspects of social media.
- But there is still a lack of robust research on highly-visual platforms like Instagram and Snapchat – this is a gap that you could address in your own research.
There are various approaches to organising the body of a literature review. You should have a rough idea of your strategy before you start writing.
Depending on the length of your literature review, you can combine several of these strategies (for example, your overall structure might be thematic, but each theme is discussed chronologically).
Chronological
The simplest approach is to trace the development of the topic over time. However, if you choose this strategy, be careful to avoid simply listing and summarising sources in order.
Try to analyse patterns, turning points and key debates that have shaped the direction of the field. Give your interpretation of how and why certain developments occurred.
If you have found some recurring central themes, you can organise your literature review into subsections that address different aspects of the topic.
For example, if you are reviewing literature about inequalities in migrant health outcomes, key themes might include healthcare policy, language barriers, cultural attitudes, legal status, and economic access.
Methodological
If you draw your sources from different disciplines or fields that use a variety of research methods , you might want to compare the results and conclusions that emerge from different approaches. For example:
- Look at what results have emerged in qualitative versus quantitative research
- Discuss how the topic has been approached by empirical versus theoretical scholarship
- Divide the literature into sociological, historical, and cultural sources
Theoretical
A literature review is often the foundation for a theoretical framework . You can use it to discuss various theories, models, and definitions of key concepts.
You might argue for the relevance of a specific theoretical approach, or combine various theoretical concepts to create a framework for your research.
Like any other academic text, your literature review should have an introduction , a main body, and a conclusion . What you include in each depends on the objective of your literature review.
The introduction should clearly establish the focus and purpose of the literature review.
If you are writing the literature review as part of your dissertation or thesis, reiterate your central problem or research question and give a brief summary of the scholarly context. You can emphasise the timeliness of the topic (“many recent studies have focused on the problem of x”) or highlight a gap in the literature (“while there has been much research on x, few researchers have taken y into consideration”).
Depending on the length of your literature review, you might want to divide the body into subsections. You can use a subheading for each theme, time period, or methodological approach.
As you write, make sure to follow these tips:
- Summarise and synthesise: give an overview of the main points of each source and combine them into a coherent whole.
- Analyse and interpret: don’t just paraphrase other researchers – add your own interpretations, discussing the significance of findings in relation to the literature as a whole.
- Critically evaluate: mention the strengths and weaknesses of your sources.
- Write in well-structured paragraphs: use transitions and topic sentences to draw connections, comparisons and contrasts.
In the conclusion, you should summarise the key findings you have taken from the literature and emphasise their significance.
If the literature review is part of your dissertation or thesis, reiterate how your research addresses gaps and contributes new knowledge, or discuss how you have drawn on existing theories and methods to build a framework for your research. This can lead directly into your methodology section.
A literature review is a survey of scholarly sources (such as books, journal articles, and theses) related to a specific topic or research question .
It is often written as part of a dissertation , thesis, research paper , or proposal .
There are several reasons to conduct a literature review at the beginning of a research project:
- To familiarise yourself with the current state of knowledge on your topic
- To ensure that you’re not just repeating what others have already done
- To identify gaps in knowledge and unresolved problems that your research can address
- To develop your theoretical framework and methodology
- To provide an overview of the key findings and debates on the topic
Writing the literature review shows your reader how your work relates to existing research and what new insights it will contribute.
The literature review usually comes near the beginning of your dissertation . After the introduction , it grounds your research in a scholarly field and leads directly to your theoretical framework or methodology .
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the ‘Cite this Scribbr article’ button to automatically add the citation to our free Reference Generator.
McCombes, S. (2022, June 07). What is a Literature Review? | Guide, Template, & Examples. Scribbr. Retrieved 9 April 2024, from https://www.scribbr.co.uk/thesis-dissertation/literature-review/
Is this article helpful?
Shona McCombes
Other students also liked, how to write a dissertation proposal | a step-by-step guide, what is a theoretical framework | a step-by-step guide, what is a research methodology | steps & tips.
- UConn Library
- Literature Review: The What, Why and How-to Guide
- Introduction
Literature Review: The What, Why and How-to Guide — Introduction
- Getting Started
- How to Pick a Topic
- Strategies to Find Sources
- Evaluating Sources & Lit. Reviews
- Tips for Writing Literature Reviews
- Writing Literature Review: Useful Sites
- Citation Resources
- Other Academic Writings
What are Literature Reviews?
So, what is a literature review? "A literature review is an account of what has been published on a topic by accredited scholars and researchers. In writing the literature review, your purpose is to convey to your reader what knowledge and ideas have been established on a topic, and what their strengths and weaknesses are. As a piece of writing, the literature review must be defined by a guiding concept (e.g., your research objective, the problem or issue you are discussing, or your argumentative thesis). It is not just a descriptive list of the material available, or a set of summaries." Taylor, D. The literature review: A few tips on conducting it . University of Toronto Health Sciences Writing Centre.
Goals of Literature Reviews
What are the goals of creating a Literature Review? A literature could be written to accomplish different aims:
- To develop a theory or evaluate an existing theory
- To summarize the historical or existing state of a research topic
- Identify a problem in a field of research
Baumeister, R. F., & Leary, M. R. (1997). Writing narrative literature reviews . Review of General Psychology , 1 (3), 311-320.
What kinds of sources require a Literature Review?
- A research paper assigned in a course
- A thesis or dissertation
- A grant proposal
- An article intended for publication in a journal
All these instances require you to collect what has been written about your research topic so that you can demonstrate how your own research sheds new light on the topic.
Types of Literature Reviews
What kinds of literature reviews are written?
Narrative review: The purpose of this type of review is to describe the current state of the research on a specific topic/research and to offer a critical analysis of the literature reviewed. Studies are grouped by research/theoretical categories, and themes and trends, strengths and weakness, and gaps are identified. The review ends with a conclusion section which summarizes the findings regarding the state of the research of the specific study, the gaps identify and if applicable, explains how the author's research will address gaps identify in the review and expand the knowledge on the topic reviewed.
- Example : Predictors and Outcomes of U.S. Quality Maternity Leave: A Review and Conceptual Framework: 10.1177/08948453211037398
Systematic review : "The authors of a systematic review use a specific procedure to search the research literature, select the studies to include in their review, and critically evaluate the studies they find." (p. 139). Nelson, L. K. (2013). Research in Communication Sciences and Disorders . Plural Publishing.
- Example : The effect of leave policies on increasing fertility: a systematic review: 10.1057/s41599-022-01270-w
Meta-analysis : "Meta-analysis is a method of reviewing research findings in a quantitative fashion by transforming the data from individual studies into what is called an effect size and then pooling and analyzing this information. The basic goal in meta-analysis is to explain why different outcomes have occurred in different studies." (p. 197). Roberts, M. C., & Ilardi, S. S. (2003). Handbook of Research Methods in Clinical Psychology . Blackwell Publishing.
- Example : Employment Instability and Fertility in Europe: A Meta-Analysis: 10.1215/00703370-9164737
Meta-synthesis : "Qualitative meta-synthesis is a type of qualitative study that uses as data the findings from other qualitative studies linked by the same or related topic." (p.312). Zimmer, L. (2006). Qualitative meta-synthesis: A question of dialoguing with texts . Journal of Advanced Nursing , 53 (3), 311-318.
- Example : Women’s perspectives on career successes and barriers: A qualitative meta-synthesis: 10.1177/05390184221113735
Literature Reviews in the Health Sciences
- UConn Health subject guide on systematic reviews Explanation of the different review types used in health sciences literature as well as tools to help you find the right review type
- << Previous: Getting Started
- Next: How to Pick a Topic >>
- Last Updated: Sep 21, 2022 2:16 PM
- URL: https://guides.lib.uconn.edu/literaturereview
- Resources Home 🏠
- Try SciSpace Copilot
- Search research papers
- Add Copilot Extension
- Try AI Detector
- Try Paraphraser
- Try Citation Generator
- April Papers
- June Papers
- July Papers

How To Write A Literature Review - A Complete Guide

Table of Contents
A literature review is much more than just another section in your research paper. It forms the very foundation of your research. It is a formal piece of writing where you analyze the existing theoretical framework, principles, and assumptions and use that as a base to shape your approach to the research question.
Curating and drafting a solid literature review section not only lends more credibility to your research paper but also makes your research tighter and better focused. But, writing literature reviews is a difficult task. It requires extensive reading, plus you have to consider market trends and technological and political changes, which tend to change in the blink of an eye.
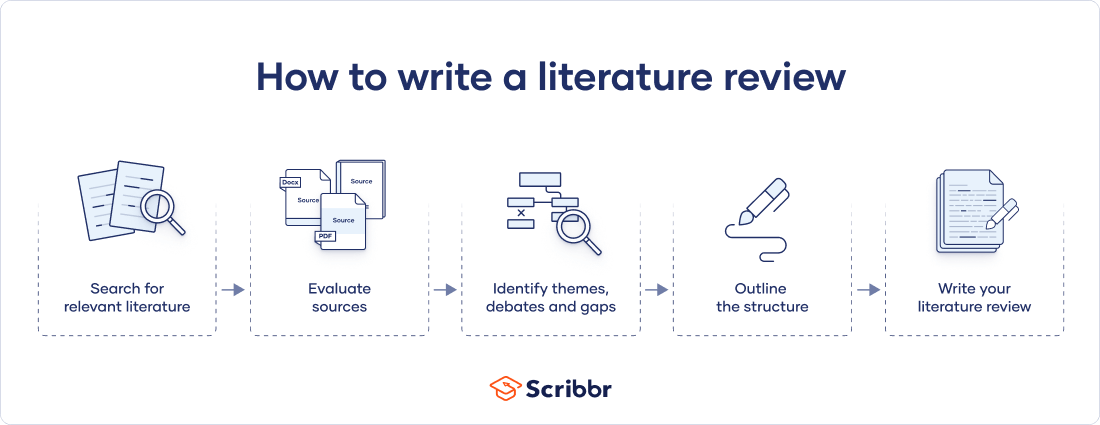
Now streamline your literature review process with the help of SciSpace Copilot. With this AI research assistant, you can efficiently synthesize and analyze a vast amount of information, identify key themes and trends, and uncover gaps in the existing research. Get real-time explanations, summaries, and answers to your questions for the paper you're reviewing, making navigating and understanding the complex literature landscape easier.
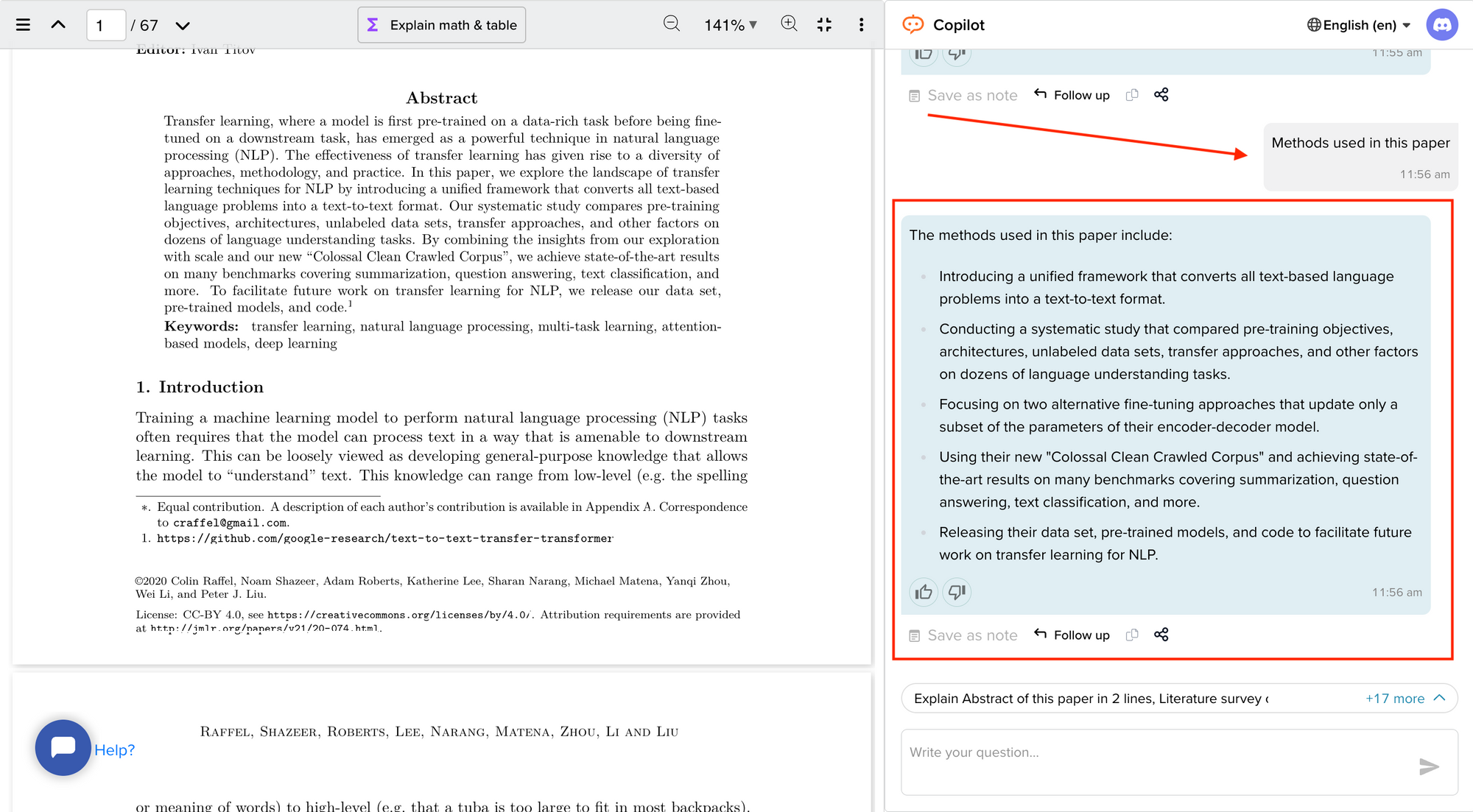
In this comprehensive guide, we will explore everything from the definition of a literature review, its appropriate length, various types of literature reviews, and how to write one.
What is a literature review?
A literature review is a collation of survey, research, critical evaluation, and assessment of the existing literature in a preferred domain.
Eminent researcher and academic Arlene Fink, in her book Conducting Research Literature Reviews , defines it as the following:
“A literature review surveys books, scholarly articles, and any other sources relevant to a particular issue, area of research, or theory, and by so doing, provides a description, summary, and critical evaluation of these works in relation to the research problem being investigated.
Literature reviews are designed to provide an overview of sources you have explored while researching a particular topic, and to demonstrate to your readers how your research fits within a larger field of study.”
Simply put, a literature review can be defined as a critical discussion of relevant pre-existing research around your research question and carving out a definitive place for your study in the existing body of knowledge. Literature reviews can be presented in multiple ways: a section of an article, the whole research paper itself, or a chapter of your thesis.
A literature review does function as a summary of sources, but it also allows you to analyze further, interpret, and examine the stated theories, methods, viewpoints, and, of course, the gaps in the existing content.
As an author, you can discuss and interpret the research question and its various aspects and debate your adopted methods to support the claim.
What is the purpose of a literature review?
A literature review is meant to help your readers understand the relevance of your research question and where it fits within the existing body of knowledge. As a researcher, you should use it to set the context, build your argument, and establish the need for your study.
What is the importance of a literature review?
The literature review is a critical part of research papers because it helps you:
- Gain an in-depth understanding of your research question and the surrounding area
- Convey that you have a thorough understanding of your research area and are up-to-date with the latest changes and advancements
- Establish how your research is connected or builds on the existing body of knowledge and how it could contribute to further research
- Elaborate on the validity and suitability of your theoretical framework and research methodology
- Identify and highlight gaps and shortcomings in the existing body of knowledge and how things need to change
- Convey to readers how your study is different or how it contributes to the research area
How long should a literature review be?
Ideally, the literature review should take up 15%-40% of the total length of your manuscript. So, if you have a 10,000-word research paper, the minimum word count could be 1500.
Your literature review format depends heavily on the kind of manuscript you are writing — an entire chapter in case of doctoral theses, a part of the introductory section in a research article, to a full-fledged review article that examines the previously published research on a topic.
Another determining factor is the type of research you are doing. The literature review section tends to be longer for secondary research projects than primary research projects.
What are the different types of literature reviews?
All literature reviews are not the same. There are a variety of possible approaches that you can take. It all depends on the type of research you are pursuing.
Here are the different types of literature reviews:
Argumentative review
It is called an argumentative review when you carefully present literature that only supports or counters a specific argument or premise to establish a viewpoint.
Integrative review
It is a type of literature review focused on building a comprehensive understanding of a topic by combining available theoretical frameworks and empirical evidence.
Methodological review
This approach delves into the ''how'' and the ''what" of the research question — you cannot look at the outcome in isolation; you should also review the methodology used.
Systematic review
This form consists of an overview of existing evidence pertinent to a clearly formulated research question, which uses pre-specified and standardized methods to identify and critically appraise relevant research and collect, report, and analyze data from the studies included in the review.
Meta-analysis review
Meta-analysis uses statistical methods to summarize the results of independent studies. By combining information from all relevant studies, meta-analysis can provide more precise estimates of the effects than those derived from the individual studies included within a review.
Historical review
Historical literature reviews focus on examining research throughout a period, often starting with the first time an issue, concept, theory, or phenomenon emerged in the literature, then tracing its evolution within the scholarship of a discipline. The purpose is to place research in a historical context to show familiarity with state-of-the-art developments and identify future research's likely directions.
Theoretical Review
This form aims to examine the corpus of theory accumulated regarding an issue, concept, theory, and phenomenon. The theoretical literature review helps to establish what theories exist, the relationships between them, the degree the existing approaches have been investigated, and to develop new hypotheses to be tested.
Scoping Review
The Scoping Review is often used at the beginning of an article, dissertation, or research proposal. It is conducted before the research to highlight gaps in the existing body of knowledge and explains why the project should be greenlit.
State-of-the-Art Review
The State-of-the-Art review is conducted periodically, focusing on the most recent research. It describes what is currently known, understood, or agreed upon regarding the research topic and highlights where there are still disagreements.
Can you use the first person in a literature review?
When writing literature reviews, you should avoid the usage of first-person pronouns. It means that instead of "I argue that" or "we argue that," the appropriate expression would be "this research paper argues that."
Do you need an abstract for a literature review?
Ideally, yes. It is always good to have a condensed summary that is self-contained and independent of the rest of your review. As for how to draft one, you can follow the same fundamental idea when preparing an abstract for a literature review. It should also include:
- The research topic and your motivation behind selecting it
- A one-sentence thesis statement
- An explanation of the kinds of literature featured in the review
- Summary of what you've learned
- Conclusions you drew from the literature you reviewed
- Potential implications and future scope for research
Here's an example of the abstract of a literature review
Is a literature review written in the past tense?
Yes, the literature review should ideally be written in the past tense. You should not use the present or future tense when writing one. The exceptions are when you have statements describing events that happened earlier than the literature you are reviewing or events that are currently occurring; then, you can use the past perfect or present perfect tenses.
How many sources for a literature review?
There are multiple approaches to deciding how many sources to include in a literature review section. The first approach would be to look level you are at as a researcher. For instance, a doctoral thesis might need 60+ sources. In contrast, you might only need to refer to 5-15 sources at the undergraduate level.
The second approach is based on the kind of literature review you are doing — whether it is merely a chapter of your paper or if it is a self-contained paper in itself. When it is just a chapter, sources should equal the total number of pages in your article's body. In the second scenario, you need at least three times as many sources as there are pages in your work.
Quick tips on how to write a literature review
To know how to write a literature review, you must clearly understand its impact and role in establishing your work as substantive research material.
You need to follow the below-mentioned steps, to write a literature review:
- Outline the purpose behind the literature review
- Search relevant literature
- Examine and assess the relevant resources
- Discover connections by drawing deep insights from the resources
- Structure planning to write a good literature review
1. Outline and identify the purpose of a literature review
As a first step on how to write a literature review, you must know what the research question or topic is and what shape you want your literature review to take. Ensure you understand the research topic inside out, or else seek clarifications. You must be able to the answer below questions before you start:
- How many sources do I need to include?
- What kind of sources should I analyze?
- How much should I critically evaluate each source?
- Should I summarize, synthesize or offer a critique of the sources?
- Do I need to include any background information or definitions?
Additionally, you should know that the narrower your research topic is, the swifter it will be for you to restrict the number of sources to be analyzed.
2. Search relevant literature
Dig deeper into search engines to discover what has already been published around your chosen topic. Make sure you thoroughly go through appropriate reference sources like books, reports, journal articles, government docs, and web-based resources.
You must prepare a list of keywords and their different variations. You can start your search from any library’s catalog, provided you are an active member of that institution. The exact keywords can be extended to widen your research over other databases and academic search engines like:
- Google Scholar
- Microsoft Academic
- Science.gov
Besides, it is not advisable to go through every resource word by word. Alternatively, what you can do is you can start by reading the abstract and then decide whether that source is relevant to your research or not.
Additionally, you must spend surplus time assessing the quality and relevance of resources. It would help if you tried preparing a list of citations to ensure that there lies no repetition of authors, publications, or articles in the literature review.
3. Examine and assess the sources
It is nearly impossible for you to go through every detail in the research article. So rather than trying to fetch every detail, you have to analyze and decide which research sources resemble closest and appear relevant to your chosen domain.
While analyzing the sources, you should look to find out answers to questions like:
- What question or problem has the author been describing and debating?
- What is the definition of critical aspects?
- How well the theories, approach, and methodology have been explained?
- Whether the research theory used some conventional or new innovative approach?
- How relevant are the key findings of the work?
- In what ways does it relate to other sources on the same topic?
- What challenges does this research paper pose to the existing theory
- What are the possible contributions or benefits it adds to the subject domain?
Be always mindful that you refer only to credible and authentic resources. It would be best if you always take references from different publications to validate your theory.
Always keep track of important information or data you can present in your literature review right from the beginning. It will help steer your path from any threats of plagiarism and also make it easier to curate an annotated bibliography or reference section.
4. Discover connections
At this stage, you must start deciding on the argument and structure of your literature review. To accomplish this, you must discover and identify the relations and connections between various resources while drafting your abstract.
A few aspects that you should be aware of while writing a literature review include:
- Rise to prominence: Theories and methods that have gained reputation and supporters over time.
- Constant scrutiny: Concepts or theories that repeatedly went under examination.
- Contradictions and conflicts: Theories, both the supporting and the contradictory ones, for the research topic.
- Knowledge gaps: What exactly does it fail to address, and how to bridge them with further research?
- Influential resources: Significant research projects available that have been upheld as milestones or perhaps, something that can modify the current trends
Once you join the dots between various past research works, it will be easier for you to draw a conclusion and identify your contribution to the existing knowledge base.
5. Structure planning to write a good literature review
There exist different ways towards planning and executing the structure of a literature review. The format of a literature review varies and depends upon the length of the research.
Like any other research paper, the literature review format must contain three sections: introduction, body, and conclusion. The goals and objectives of the research question determine what goes inside these three sections.
Nevertheless, a good literature review can be structured according to the chronological, thematic, methodological, or theoretical framework approach.
Literature review samples
1. Standalone
2. As a section of a research paper
How SciSpace Discover makes literature review a breeze?
SciSpace Discover is a one-stop solution to do an effective literature search and get barrier-free access to scientific knowledge. It is an excellent repository where you can find millions of only peer-reviewed articles and full-text PDF files. Here’s more on how you can use it:
Find the right information
Find what you want quickly and easily with comprehensive search filters that let you narrow down papers according to PDF availability, year of publishing, document type, and affiliated institution. Moreover, you can sort the results based on the publishing date, citation count, and relevance.
Assess credibility of papers quickly
When doing the literature review, it is critical to establish the quality of your sources. They form the foundation of your research. SciSpace Discover helps you assess the quality of a source by providing an overview of its references, citations, and performance metrics.
Get the complete picture in no time
SciSpace Discover’s personalized suggestion engine helps you stay on course and get the complete picture of the topic from one place. Every time you visit an article page, it provides you links to related papers. Besides that, it helps you understand what’s trending, who are the top authors, and who are the leading publishers on a topic.
Make referring sources super easy
To ensure you don't lose track of your sources, you must start noting down your references when doing the literature review. SciSpace Discover makes this step effortless. Click the 'cite' button on an article page, and you will receive preloaded citation text in multiple styles — all you've to do is copy-paste it into your manuscript.
Final tips on how to write a literature review
A massive chunk of time and effort is required to write a good literature review. But, if you go about it systematically, you'll be able to save a ton of time and build a solid foundation for your research.
We hope this guide has helped you answer several key questions you have about writing literature reviews.
Would you like to explore SciSpace Discover and kick off your literature search right away? You can get started here .
Frequently Asked Questions (FAQs)
1. how to start a literature review.
• What questions do you want to answer?
• What sources do you need to answer these questions?
• What information do these sources contain?
• How can you use this information to answer your questions?
2. What to include in a literature review?
• A brief background of the problem or issue
• What has previously been done to address the problem or issue
• A description of what you will do in your project
• How this study will contribute to research on the subject
3. Why literature review is important?
The literature review is an important part of any research project because it allows the writer to look at previous studies on a topic and determine existing gaps in the literature, as well as what has already been done. It will also help them to choose the most appropriate method for their own study.
4. How to cite a literature review in APA format?
To cite a literature review in APA style, you need to provide the author's name, the title of the article, and the year of publication. For example: Patel, A. B., & Stokes, G. S. (2012). The relationship between personality and intelligence: A meta-analysis of longitudinal research. Personality and Individual Differences, 53(1), 16-21
5. What are the components of a literature review?
• A brief introduction to the topic, including its background and context. The introduction should also include a rationale for why the study is being conducted and what it will accomplish.
• A description of the methodologies used in the study. This can include information about data collection methods, sample size, and statistical analyses.
• A presentation of the findings in an organized format that helps readers follow along with the author's conclusions.
6. What are common errors in writing literature review?
• Not spending enough time to critically evaluate the relevance of resources, observations and conclusions.
• Totally relying on secondary data while ignoring primary data.
• Letting your personal bias seep into your interpretation of existing literature.
• No detailed explanation of the procedure to discover and identify an appropriate literature review.
7. What are the 5 C's of writing literature review?
• Cite - the sources you utilized and referenced in your research.
• Compare - existing arguments, hypotheses, methodologies, and conclusions found in the knowledge base.
• Contrast - the arguments, topics, methodologies, approaches, and disputes that may be found in the literature.
• Critique - the literature and describe the ideas and opinions you find more convincing and why.
• Connect - the various studies you reviewed in your research.
8. How many sources should a literature review have?
When it is just a chapter, sources should equal the total number of pages in your article's body. if it is a self-contained paper in itself, you need at least three times as many sources as there are pages in your work.
9. Can literature review have diagrams?
• To represent an abstract idea or concept
• To explain the steps of a process or procedure
• To help readers understand the relationships between different concepts
10. How old should sources be in a literature review?
Sources for a literature review should be as current as possible or not older than ten years. The only exception to this rule is if you are reviewing a historical topic and need to use older sources.
11. What are the types of literature review?
• Argumentative review
• Integrative review
• Methodological review
• Systematic review
• Meta-analysis review
• Historical review
• Theoretical review
• Scoping review
• State-of-the-Art review
12. Is a literature review mandatory?
Yes. Literature review is a mandatory part of any research project. It is a critical step in the process that allows you to establish the scope of your research, and provide a background for the rest of your work.
But before you go,
- Six Online Tools for Easy Literature Review
- Evaluating literature review: systematic vs. scoping reviews
- Systematic Approaches to a Successful Literature Review
- Writing Integrative Literature Reviews: Guidelines and Examples
You might also like

Consensus GPT vs. SciSpace GPT: Choose the Best GPT for Research

Literature Review and Theoretical Framework: Understanding the Differences

Types of Essays in Academic Writing - Quick Guide (2024)
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
What is a literature review?

A literature review is a critical analysis of the literature related to your research topic. It evaluates and critiques the literature to establish a theoretical framework for your research topic and/or identify a gap in the existing research that your research will address.
A literature review is not a summary of the literature. You need to engage deeply and critically with the literature. Your literature review should show your understanding of the literature related to your research topic and lead to presenting a rationale for your research.
A literature review focuses on:
- the context of the topic
- key concepts, ideas, theories and methodologies
- key researchers, texts and seminal works
- major issues and debates
- identifying conflicting evidence
- the main questions that have been asked around the topic
- the organisation of knowledge on the topic
- definitions, particularly those that are contested
- showing how your research will advance scholarly knowledge (generally referred to as identifying the ‘gap’).
This module will guide you through the functions of a literature review; the typical process of conducting a literature review (including searching for literature and taking notes); structuring your literature review within your thesis and organising its internal ideas; and styling the language of your literature review.
The purposes of a literature review
A literature review serves two main purposes:
1) To show awareness of the present state of knowledge in a particular field, including:
- seminal authors
- the main empirical research
- theoretical positions
- controversies
- breakthroughs as well as links to other related areas of knowledge.
2) To provide a foundation for the author’s research. To do that, the literature review needs to:
- help the researcher define a hypothesis or a research question, and how answering the question will contribute to the body of knowledge;
- provide a rationale for investigating the problem and the selected methodology;
- provide a particular theoretical lens, support the argument, or identify gaps.
Before you engage further with this module, try the quiz below to see how much you already know about literature reviews.
Research and Writing Skills for Academic and Graduate Researchers Copyright © 2022 by RMIT University is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Clinics (Sao Paulo)
Approaching literature review for academic purposes: The Literature Review Checklist
Debora f.b. leite.
I Departamento de Ginecologia e Obstetricia, Faculdade de Ciencias Medicas, Universidade Estadual de Campinas, Campinas, SP, BR
II Universidade Federal de Pernambuco, Pernambuco, PE, BR
III Hospital das Clinicas, Universidade Federal de Pernambuco, Pernambuco, PE, BR
Maria Auxiliadora Soares Padilha
Jose g. cecatti.
A sophisticated literature review (LR) can result in a robust dissertation/thesis by scrutinizing the main problem examined by the academic study; anticipating research hypotheses, methods and results; and maintaining the interest of the audience in how the dissertation/thesis will provide solutions for the current gaps in a particular field. Unfortunately, little guidance is available on elaborating LRs, and writing an LR chapter is not a linear process. An LR translates students’ abilities in information literacy, the language domain, and critical writing. Students in postgraduate programs should be systematically trained in these skills. Therefore, this paper discusses the purposes of LRs in dissertations and theses. Second, the paper considers five steps for developing a review: defining the main topic, searching the literature, analyzing the results, writing the review and reflecting on the writing. Ultimately, this study proposes a twelve-item LR checklist. By clearly stating the desired achievements, this checklist allows Masters and Ph.D. students to continuously assess their own progress in elaborating an LR. Institutions aiming to strengthen students’ necessary skills in critical academic writing should also use this tool.
INTRODUCTION
Writing the literature review (LR) is often viewed as a difficult task that can be a point of writer’s block and procrastination ( 1 ) in postgraduate life. Disagreements on the definitions or classifications of LRs ( 2 ) may confuse students about their purpose and scope, as well as how to perform an LR. Interestingly, at many universities, the LR is still an important element in any academic work, despite the more recent trend of producing scientific articles rather than classical theses.
The LR is not an isolated section of the thesis/dissertation or a copy of the background section of a research proposal. It identifies the state-of-the-art knowledge in a particular field, clarifies information that is already known, elucidates implications of the problem being analyzed, links theory and practice ( 3 - 5 ), highlights gaps in the current literature, and places the dissertation/thesis within the research agenda of that field. Additionally, by writing the LR, postgraduate students will comprehend the structure of the subject and elaborate on their cognitive connections ( 3 ) while analyzing and synthesizing data with increasing maturity.
At the same time, the LR transforms the student and hints at the contents of other chapters for the reader. First, the LR explains the research question; second, it supports the hypothesis, objectives, and methods of the research project; and finally, it facilitates a description of the student’s interpretation of the results and his/her conclusions. For scholars, the LR is an introductory chapter ( 6 ). If it is well written, it demonstrates the student’s understanding of and maturity in a particular topic. A sound and sophisticated LR can indicate a robust dissertation/thesis.
A consensus on the best method to elaborate a dissertation/thesis has not been achieved. The LR can be a distinct chapter or included in different sections; it can be part of the introduction chapter, part of each research topic, or part of each published paper ( 7 ). However, scholars view the LR as an integral part of the main body of an academic work because it is intrinsically connected to other sections ( Figure 1 ) and is frequently present. The structure of the LR depends on the conventions of a particular discipline, the rules of the department, and the student’s and supervisor’s areas of expertise, needs and interests.

Interestingly, many postgraduate students choose to submit their LR to peer-reviewed journals. As LRs are critical evaluations of current knowledge, they are indeed publishable material, even in the form of narrative or systematic reviews. However, systematic reviews have specific patterns 1 ( 8 ) that may not entirely fit with the questions posed in the dissertation/thesis. Additionally, the scope of a systematic review may be too narrow, and the strict criteria for study inclusion may omit important information from the dissertation/thesis. Therefore, this essay discusses the definition of an LR is and methods to develop an LR in the context of an academic dissertation/thesis. Finally, we suggest a checklist to evaluate an LR.
WHAT IS A LITERATURE REVIEW IN A THESIS?
Conducting research and writing a dissertation/thesis translates rational thinking and enthusiasm ( 9 ). While a strong body of literature that instructs students on research methodology, data analysis and writing scientific papers exists, little guidance on performing LRs is available. The LR is a unique opportunity to assess and contrast various arguments and theories, not just summarize them. The research results should not be discussed within the LR, but the postgraduate student tends to write a comprehensive LR while reflecting on his or her own findings ( 10 ).
Many people believe that writing an LR is a lonely and linear process. Supervisors or the institutions assume that the Ph.D. student has mastered the relevant techniques and vocabulary associated with his/her subject and conducts a self-reflection about previously published findings. Indeed, while elaborating the LR, the student should aggregate diverse skills, which mainly rely on his/her own commitment to mastering them. Thus, less supervision should be required ( 11 ). However, the parameters described above might not currently be the case for many students ( 11 , 12 ), and the lack of formal and systematic training on writing LRs is an important concern ( 11 ).
An institutional environment devoted to active learning will provide students the opportunity to continuously reflect on LRs, which will form a dialogue between the postgraduate student and the current literature in a particular field ( 13 ). Postgraduate students will be interpreting studies by other researchers, and, according to Hart (1998) ( 3 ), the outcomes of the LR in a dissertation/thesis include the following:
- To identify what research has been performed and what topics require further investigation in a particular field of knowledge;
- To determine the context of the problem;
- To recognize the main methodologies and techniques that have been used in the past;
- To place the current research project within the historical, methodological and theoretical context of a particular field;
- To identify significant aspects of the topic;
- To elucidate the implications of the topic;
- To offer an alternative perspective;
- To discern how the studied subject is structured;
- To improve the student’s subject vocabulary in a particular field; and
- To characterize the links between theory and practice.
A sound LR translates the postgraduate student’s expertise in academic and scientific writing: it expresses his/her level of comfort with synthesizing ideas ( 11 ). The LR reveals how well the postgraduate student has proceeded in three domains: an effective literature search, the language domain, and critical writing.
Effective literature search
All students should be trained in gathering appropriate data for specific purposes, and information literacy skills are a cornerstone. These skills are defined as “an individual’s ability to know when they need information, to identify information that can help them address the issue or problem at hand, and to locate, evaluate, and use that information effectively” ( 14 ). Librarian support is of vital importance in coaching the appropriate use of Boolean logic (AND, OR, NOT) and other tools for highly efficient literature searches (e.g., quotation marks and truncation), as is the appropriate management of electronic databases.
Language domain
Academic writing must be concise and precise: unnecessary words distract the reader from the essential content ( 15 ). In this context, reading about issues distant from the research topic ( 16 ) may increase students’ general vocabulary and familiarity with grammar. Ultimately, reading diverse materials facilitates and encourages the writing process itself.
Critical writing
Critical judgment includes critical reading, thinking and writing. It supposes a student’s analytical reflection about what he/she has read. The student should delineate the basic elements of the topic, characterize the most relevant claims, identify relationships, and finally contrast those relationships ( 17 ). Each scientific document highlights the perspective of the author, and students will become more confident in judging the supporting evidence and underlying premises of a study and constructing their own counterargument as they read more articles. A paucity of integration or contradictory perspectives indicates lower levels of cognitive complexity ( 12 ).
Thus, while elaborating an LR, the postgraduate student should achieve the highest category of Bloom’s cognitive skills: evaluation ( 12 ). The writer should not only summarize data and understand each topic but also be able to make judgments based on objective criteria, compare resources and findings, identify discrepancies due to methodology, and construct his/her own argument ( 12 ). As a result, the student will be sufficiently confident to show his/her own voice .
Writing a consistent LR is an intense and complex activity that reveals the training and long-lasting academic skills of a writer. It is not a lonely or linear process. However, students are unlikely to be prepared to write an LR if they have not mastered the aforementioned domains ( 10 ). An institutional environment that supports student learning is crucial.
Different institutions employ distinct methods to promote students’ learning processes. First, many universities propose modules to develop behind the scenes activities that enhance self-reflection about general skills (e.g., the skills we have mastered and the skills we need to develop further), behaviors that should be incorporated (e.g., self-criticism about one’s own thoughts), and each student’s role in the advancement of his/her field. Lectures or workshops about LRs themselves are useful because they describe the purposes of the LR and how it fits into the whole picture of a student’s work. These activities may explain what type of discussion an LR must involve, the importance of defining the correct scope, the reasons to include a particular resource, and the main role of critical reading.
Some pedagogic services that promote a continuous improvement in study and academic skills are equally important. Examples include workshops about time management, the accomplishment of personal objectives, active learning, and foreign languages for nonnative speakers. Additionally, opportunities to converse with other students promotes an awareness of others’ experiences and difficulties. Ultimately, the supervisor’s role in providing feedback and setting deadlines is crucial in developing students’ abilities and in strengthening students’ writing quality ( 12 ).
HOW SHOULD A LITERATURE REVIEW BE DEVELOPED?
A consensus on the appropriate method for elaborating an LR is not available, but four main steps are generally accepted: defining the main topic, searching the literature, analyzing the results, and writing ( 6 ). We suggest a fifth step: reflecting on the information that has been written in previous publications ( Figure 2 ).

First step: Defining the main topic
Planning an LR is directly linked to the research main question of the thesis and occurs in parallel to students’ training in the three domains discussed above. The planning stage helps organize ideas, delimit the scope of the LR ( 11 ), and avoid the wasting of time in the process. Planning includes the following steps:
- Reflecting on the scope of the LR: postgraduate students will have assumptions about what material must be addressed and what information is not essential to an LR ( 13 , 18 ). Cooper’s Taxonomy of Literature Reviews 2 systematizes the writing process through six characteristics and nonmutually exclusive categories. The focus refers to the reviewer’s most important points of interest, while the goals concern what students want to achieve with the LR. The perspective assumes answers to the student’s own view of the LR and how he/she presents a particular issue. The coverage defines how comprehensive the student is in presenting the literature, and the organization determines the sequence of arguments. The audience is defined as the group for whom the LR is written.
- Designating sections and subsections: Headings and subheadings should be specific, explanatory and have a coherent sequence throughout the text ( 4 ). They simulate an inverted pyramid, with an increasing level of reflection and depth of argument.
- Identifying keywords: The relevant keywords for each LR section should be listed to guide the literature search. This list should mirror what Hart (1998) ( 3 ) advocates as subject vocabulary . The keywords will also be useful when the student is writing the LR since they guide the reader through the text.
- Delineating the time interval and language of documents to be retrieved in the second step. The most recently published documents should be considered, but relevant texts published before a predefined cutoff year can be included if they are classic documents in that field. Extra care should be employed when translating documents.
Second step: Searching the literature
The ability to gather adequate information from the literature must be addressed in postgraduate programs. Librarian support is important, particularly for accessing difficult texts. This step comprises the following components:
- Searching the literature itself: This process consists of defining which databases (electronic or dissertation/thesis repositories), official documents, and books will be searched and then actively conducting the search. Information literacy skills have a central role in this stage. While searching electronic databases, controlled vocabulary (e.g., Medical Subject Headings, or MeSH, for the PubMed database) or specific standardized syntax rules may need to be applied.
In addition, two other approaches are suggested. First, a review of the reference list of each document might be useful for identifying relevant publications to be included and important opinions to be assessed. This step is also relevant for referencing the original studies and leading authors in that field. Moreover, students can directly contact the experts on a particular topic to consult with them regarding their experience or use them as a source of additional unpublished documents.
Before submitting a dissertation/thesis, the electronic search strategy should be repeated. This process will ensure that the most recently published papers will be considered in the LR.
- Selecting documents for inclusion: Generally, the most recent literature will be included in the form of published peer-reviewed papers. Assess books and unpublished material, such as conference abstracts, academic texts and government reports, are also important to assess since the gray literature also offers valuable information. However, since these materials are not peer-reviewed, we recommend that they are carefully added to the LR.
This task is an important exercise in time management. First, students should read the title and abstract to understand whether that document suits their purposes, addresses the research question, and helps develop the topic of interest. Then, they should scan the full text, determine how it is structured, group it with similar documents, and verify whether other arguments might be considered ( 5 ).
Third step: Analyzing the results
Critical reading and thinking skills are important in this step. This step consists of the following components:
- Reading documents: The student may read various texts in depth according to LR sections and subsections ( defining the main topic ), which is not a passive activity ( 1 ). Some questions should be asked to practice critical analysis skills, as listed below. Is the research question evident and articulated with previous knowledge? What are the authors’ research goals and theoretical orientations, and how do they interact? Are the authors’ claims related to other scholars’ research? Do the authors consider different perspectives? Was the research project designed and conducted properly? Are the results and discussion plausible, and are they consistent with the research objectives and methodology? What are the strengths and limitations of this work? How do the authors support their findings? How does this work contribute to the current research topic? ( 1 , 19 )
- Taking notes: Students who systematically take notes on each document are more readily able to establish similarities or differences with other documents and to highlight personal observations. This approach reinforces the student’s ideas about the next step and helps develop his/her own academic voice ( 1 , 13 ). Voice recognition software ( 16 ), mind maps ( 5 ), flowcharts, tables, spreadsheets, personal comments on the referenced texts, and note-taking apps are all available tools for managing these observations, and the student him/herself should use the tool that best improves his/her learning. Additionally, when a student is considering submitting an LR to a peer-reviewed journal, notes should be taken on the activities performed in all five steps to ensure that they are able to be replicated.
Fourth step: Writing
The recognition of when a student is able and ready to write after a sufficient period of reading and thinking is likely a difficult task. Some students can produce a review in a single long work session. However, as discussed above, writing is not a linear process, and students do not need to write LRs according to a specific sequence of sections. Writing an LR is a time-consuming task, and some scholars believe that a period of at least six months is sufficient ( 6 ). An LR, and academic writing in general, expresses the writer’s proper thoughts, conclusions about others’ work ( 6 , 10 , 13 , 16 ), and decisions about methods to progress in the chosen field of knowledge. Thus, each student is expected to present a different learning and writing trajectory.
In this step, writing methods should be considered; then, editing, citing and correct referencing should complete this stage, at least temporarily. Freewriting techniques may be a good starting point for brainstorming ideas and improving the understanding of the information that has been read ( 1 ). Students should consider the following parameters when creating an agenda for writing the LR: two-hour writing blocks (at minimum), with prespecified tasks that are possible to complete in one section; short (minutes) and long breaks (days or weeks) to allow sufficient time for mental rest and reflection; and short- and long-term goals to motivate the writing itself ( 20 ). With increasing experience, this scheme can vary widely, and it is not a straightforward rule. Importantly, each discipline has a different way of writing ( 1 ), and each department has its own preferred styles for citations and references.
Fifth step: Reflecting on the writing
In this step, the postgraduate student should ask him/herself the same questions as in the analyzing the results step, which can take more time than anticipated. Ambiguities, repeated ideas, and a lack of coherence may not be noted when the student is immersed in the writing task for long periods. The whole effort will likely be a work in progress, and continuous refinements in the written material will occur once the writing process has begun.
LITERATURE REVIEW CHECKLIST
In contrast to review papers, the LR of a dissertation/thesis should not be a standalone piece or work. Instead, it should present the student as a scholar and should maintain the interest of the audience in how that dissertation/thesis will provide solutions for the current gaps in a particular field.
A checklist for evaluating an LR is convenient for students’ continuous academic development and research transparency: it clearly states the desired achievements for the LR of a dissertation/thesis. Here, we present an LR checklist developed from an LR scoring rubric ( 11 ). For a critical analysis of an LR, we maintain the five categories but offer twelve criteria that are not scaled ( Figure 3 ). The criteria all have the same importance and are not mutually exclusive.

First category: Coverage
1. justified criteria exist for the inclusion and exclusion of literature in the review.
This criterion builds on the main topic and areas covered by the LR ( 18 ). While experts may be confident in retrieving and selecting literature, postgraduate students must convince their audience about the adequacy of their search strategy and their reasons for intentionally selecting what material to cover ( 11 ). References from different fields of knowledge provide distinct perspective, but narrowing the scope of coverage may be important in areas with a large body of existing knowledge.
Second category: Synthesis
2. a critical examination of the state of the field exists.
A critical examination is an assessment of distinct aspects in the field ( 1 ) along with a constructive argument. It is not a negative critique but an expression of the student’s understanding of how other scholars have added to the topic ( 1 ), and the student should analyze and contextualize contradictory statements. A writer’s personal bias (beliefs or political involvement) have been shown to influence the structure and writing of a document; therefore, the cultural and paradigmatic background guide how the theories are revised and presented ( 13 ). However, an honest judgment is important when considering different perspectives.
3. The topic or problem is clearly placed in the context of the broader scholarly literature
The broader scholarly literature should be related to the chosen main topic for the LR ( how to develop the literature review section). The LR can cover the literature from one or more disciplines, depending on its scope, but it should always offer a new perspective. In addition, students should be careful in citing and referencing previous publications. As a rule, original studies and primary references should generally be included. Systematic and narrative reviews present summarized data, and it may be important to cite them, particularly for issues that should be understood but do not require a detailed description. Similarly, quotations highlight the exact statement from another publication. However, excessive referencing may disclose lower levels of analysis and synthesis by the student.
4. The LR is critically placed in the historical context of the field
Situating the LR in its historical context shows the level of comfort of the student in addressing a particular topic. Instead of only presenting statements and theories in a temporal approach, which occasionally follows a linear timeline, the LR should authentically characterize the student’s academic work in the state-of-art techniques in their particular field of knowledge. Thus, the LR should reinforce why the dissertation/thesis represents original work in the chosen research field.
5. Ambiguities in definitions are considered and resolved
Distinct theories on the same topic may exist in different disciplines, and one discipline may consider multiple concepts to explain one topic. These misunderstandings should be addressed and contemplated. The LR should not synthesize all theories or concepts at the same time. Although this approach might demonstrate in-depth reading on a particular topic, it can reveal a student’s inability to comprehend and synthesize his/her research problem.
6. Important variables and phenomena relevant to the topic are articulated
The LR is a unique opportunity to articulate ideas and arguments and to purpose new relationships between them ( 10 , 11 ). More importantly, a sound LR will outline to the audience how these important variables and phenomena will be addressed in the current academic work. Indeed, the LR should build a bidirectional link with the remaining sections and ground the connections between all of the sections ( Figure 1 ).
7. A synthesized new perspective on the literature has been established
The LR is a ‘creative inquiry’ ( 13 ) in which the student elaborates his/her own discourse, builds on previous knowledge in the field, and describes his/her own perspective while interpreting others’ work ( 13 , 17 ). Thus, students should articulate the current knowledge, not accept the results at face value ( 11 , 13 , 17 ), and improve their own cognitive abilities ( 12 ).
Third category: Methodology
8. the main methodologies and research techniques that have been used in the field are identified and their advantages and disadvantages are discussed.
The LR is expected to distinguish the research that has been completed from investigations that remain to be performed, address the benefits and limitations of the main methods applied to date, and consider the strategies for addressing the expected limitations described above. While placing his/her research within the methodological context of a particular topic, the LR will justify the methodology of the study and substantiate the student’s interpretations.
9. Ideas and theories in the field are related to research methodologies
The audience expects the writer to analyze and synthesize methodological approaches in the field. The findings should be explained according to the strengths and limitations of previous research methods, and students must avoid interpretations that are not supported by the analyzed literature. This criterion translates to the student’s comprehension of the applicability and types of answers provided by different research methodologies, even those using a quantitative or qualitative research approach.
Fourth category: Significance
10. the scholarly significance of the research problem is rationalized.
The LR is an introductory section of a dissertation/thesis and will present the postgraduate student as a scholar in a particular field ( 11 ). Therefore, the LR should discuss how the research problem is currently addressed in the discipline being investigated or in different disciplines, depending on the scope of the LR. The LR explains the academic paradigms in the topic of interest ( 13 ) and methods to advance the field from these starting points. However, an excess number of personal citations—whether referencing the student’s research or studies by his/her research team—may reflect a narrow literature search and a lack of comprehensive synthesis of ideas and arguments.
11. The practical significance of the research problem is rationalized
The practical significance indicates a student’s comprehensive understanding of research terminology (e.g., risk versus associated factor), methodology (e.g., efficacy versus effectiveness) and plausible interpretations in the context of the field. Notably, the academic argument about a topic may not always reflect the debate in real life terms. For example, using a quantitative approach in epidemiology, statistically significant differences between groups do not explain all of the factors involved in a particular problem ( 21 ). Therefore, excessive faith in p -values may reflect lower levels of critical evaluation of the context and implications of a research problem by the student.
Fifth category: Rhetoric
12. the lr was written with a coherent, clear structure that supported the review.
This category strictly relates to the language domain: the text should be coherent and presented in a logical sequence, regardless of which organizational ( 18 ) approach is chosen. The beginning of each section/subsection should state what themes will be addressed, paragraphs should be carefully linked to each other ( 10 ), and the first sentence of each paragraph should generally summarize the content. Additionally, the student’s statements are clear, sound, and linked to other scholars’ works, and precise and concise language that follows standardized writing conventions (e.g., in terms of active/passive voice and verb tenses) is used. Attention to grammar, such as orthography and punctuation, indicates prudence and supports a robust dissertation/thesis. Ultimately, all of these strategies provide fluency and consistency for the text.
Although the scoring rubric was initially proposed for postgraduate programs in education research, we are convinced that this checklist is a valuable tool for all academic areas. It enables the monitoring of students’ learning curves and a concentrated effort on any criteria that are not yet achieved. For institutions, the checklist is a guide to support supervisors’ feedback, improve students’ writing skills, and highlight the learning goals of each program. These criteria do not form a linear sequence, but ideally, all twelve achievements should be perceived in the LR.
CONCLUSIONS
A single correct method to classify, evaluate and guide the elaboration of an LR has not been established. In this essay, we have suggested directions for planning, structuring and critically evaluating an LR. The planning of the scope of an LR and approaches to complete it is a valuable effort, and the five steps represent a rational starting point. An institutional environment devoted to active learning will support students in continuously reflecting on LRs, which will form a dialogue between the writer and the current literature in a particular field ( 13 ).
The completion of an LR is a challenging and necessary process for understanding one’s own field of expertise. Knowledge is always transitory, but our responsibility as scholars is to provide a critical contribution to our field, allowing others to think through our work. Good researchers are grounded in sophisticated LRs, which reveal a writer’s training and long-lasting academic skills. We recommend using the LR checklist as a tool for strengthening the skills necessary for critical academic writing.
AUTHOR CONTRIBUTIONS
Leite DFB has initially conceived the idea and has written the first draft of this review. Padilha MAS and Cecatti JG have supervised data interpretation and critically reviewed the manuscript. All authors have read the draft and agreed with this submission. Authors are responsible for all aspects of this academic piece.
ACKNOWLEDGMENTS
We are grateful to all of the professors of the ‘Getting Started with Graduate Research and Generic Skills’ module at University College Cork, Cork, Ireland, for suggesting and supporting this article. Funding: DFBL has granted scholarship from Brazilian Federal Agency for Support and Evaluation of Graduate Education (CAPES) to take part of her Ph.D. studies in Ireland (process number 88881.134512/2016-01). There is no participation from sponsors on authors’ decision to write or to submit this manuscript.
No potential conflict of interest was reported.
1 The questions posed in systematic reviews usually follow the ‘PICOS’ acronym: Population, Intervention, Comparison, Outcomes, Study design.
2 In 1988, Cooper proposed a taxonomy that aims to facilitate students’ and institutions’ understanding of literature reviews. Six characteristics with specific categories are briefly described: Focus: research outcomes, research methodologies, theories, or practices and applications; Goals: integration (generalization, conflict resolution, and linguistic bridge-building), criticism, or identification of central issues; Perspective: neutral representation or espousal of a position; Coverage: exhaustive, exhaustive with selective citations, representative, central or pivotal; Organization: historical, conceptual, or methodological; and Audience: specialized scholars, general scholars, practitioners or policymakers, or the general public.

Literature Reviews
- Types of reviews
- Getting started
Types of reviews and examples
Choosing a review type.
- 1. Define your research question
- 2. Plan your search
- 3. Search the literature
- 4. Organize your results
- 5. Synthesize your findings
- 6. Write the review
- Artificial intelligence (AI) tools
- Thompson Writing Studio This link opens in a new window
- Need to write a systematic review? This link opens in a new window

Contact a Librarian
Ask a Librarian
- Meta-analysis
- Systematized
Definition:
"A term used to describe a conventional overview of the literature, particularly when contrasted with a systematic review (Booth et al., 2012, p. 265).
Characteristics:
- Provides examination of recent or current literature on a wide range of subjects
- Varying levels of completeness / comprehensiveness, non-standardized methodology
- May or may not include comprehensive searching, quality assessment or critical appraisal
Mitchell, L. E., & Zajchowski, C. A. (2022). The history of air quality in Utah: A narrative review. Sustainability , 14 (15), 9653. doi.org/10.3390/su14159653
Booth, A., Papaioannou, D., & Sutton, A. (2012). Systematic approaches to a successful literature review. London: SAGE Publications Ltd.
"An assessment of what is already known about a policy or practice issue...using systematic review methods to search and critically appraise existing research" (Grant & Booth, 2009, p. 100).
- Assessment of what is already known about an issue
- Similar to a systematic review but within a time-constrained setting
- Typically employs methodological shortcuts, increasing risk of introducing bias, includes basic level of quality assessment
- Best suited for issues needing quick decisions and solutions (i.e., policy recommendations)
Learn more about the method:
Khangura, S., Konnyu, K., Cushman, R., Grimshaw, J., & Moher, D. (2012). Evidence summaries: the evolution of a rapid review approach. Systematic reviews, 1 (1), 1-9. https://doi.org/10.1186/2046-4053-1-10
Virginia Commonwealth University Libraries. (2021). Rapid Review Protocol .
Quarmby, S., Santos, G., & Mathias, M. (2019). Air quality strategies and technologies: A rapid review of the international evidence. Sustainability, 11 (10), 2757. https://doi.org/10.3390/su11102757
Grant, M.J. & Booth, A. (2009). A typology of reviews: an analysis of the 14 review types and associated methodologies. Health Information & Libraries Journal , 26(2), 91-108. https://www.doi.org/10.1111/j.1471-1842.2009.00848.x
Developed and refined by the Evidence for Policy and Practice Information and Co-ordinating Centre (EPPI-Centre), this review "map[s] out and categorize[s] existing literature on a particular topic, identifying gaps in research literature from which to commission further reviews and/or primary research" (Grant & Booth, 2009, p. 97).
Although mapping reviews are sometimes called scoping reviews, the key difference is that mapping reviews focus on a review question, rather than a topic
Mapping reviews are "best used where a clear target for a more focused evidence product has not yet been identified" (Booth, 2016, p. 14)
Mapping review searches are often quick and are intended to provide a broad overview
Mapping reviews can take different approaches in what types of literature is focused on in the search
Cooper I. D. (2016). What is a "mapping study?". Journal of the Medical Library Association: JMLA , 104 (1), 76–78. https://doi.org/10.3163/1536-5050.104.1.013
Miake-Lye, I. M., Hempel, S., Shanman, R., & Shekelle, P. G. (2016). What is an evidence map? A systematic review of published evidence maps and their definitions, methods, and products. Systematic reviews, 5 (1), 1-21. https://doi.org/10.1186/s13643-016-0204-x
Tainio, M., Andersen, Z. J., Nieuwenhuijsen, M. J., Hu, L., De Nazelle, A., An, R., ... & de Sá, T. H. (2021). Air pollution, physical activity and health: A mapping review of the evidence. Environment international , 147 , 105954. https://doi.org/10.1016/j.envint.2020.105954
Booth, A. (2016). EVIDENT Guidance for Reviewing the Evidence: a compendium of methodological literature and websites . ResearchGate. https://doi.org/10.13140/RG.2.1.1562.9842 .
Grant, M.J. & Booth, A. (2009). A typology of reviews: an analysis of the 14 review types and associated methodologies. Health Information & Libraries Journal , 26(2), 91-108. https://www.doi.org/10.1111/j.1471-1842.2009.00848.x
"A type of review that has as its primary objective the identification of the size and quality of research in a topic area in order to inform subsequent review" (Booth et al., 2012, p. 269).
- Main purpose is to map out and categorize existing literature, identify gaps in literature—great for informing policy-making
- Search comprehensiveness determined by time/scope constraints, could take longer than a systematic review
- No formal quality assessment or critical appraisal
Learn more about the methods :
Arksey, H., & O'Malley, L. (2005) Scoping studies: towards a methodological framework. International Journal of Social Research Methodology , 8 (1), 19-32. https://doi.org/10.1080/1364557032000119616
Levac, D., Colquhoun, H., & O’Brien, K. K. (2010). Scoping studies: Advancing the methodology. Implementation Science: IS, 5, 69. https://doi.org/10.1186/1748-5908-5-69
Example :
Rahman, A., Sarkar, A., Yadav, O. P., Achari, G., & Slobodnik, J. (2021). Potential human health risks due to environmental exposure to nano-and microplastics and knowledge gaps: A scoping review. Science of the Total Environment, 757 , 143872. https://doi.org/10.1016/j.scitotenv.2020.143872
A review that "[compiles] evidence from multiple...reviews into one accessible and usable document" (Grant & Booth, 2009, p. 103). While originally intended to be a compilation of Cochrane reviews, it now generally refers to any kind of evidence synthesis.
- Compiles evidence from multiple reviews into one document
- Often defines a broader question than is typical of a traditional systematic review
Choi, G. J., & Kang, H. (2022). The umbrella review: a useful strategy in the rain of evidence. The Korean Journal of Pain , 35 (2), 127–128. https://doi.org/10.3344/kjp.2022.35.2.127
Aromataris, E., Fernandez, R., Godfrey, C. M., Holly, C., Khalil, H., & Tungpunkom, P. (2015). Summarizing systematic reviews: Methodological development, conduct and reporting of an umbrella review approach. International Journal of Evidence-Based Healthcare , 13(3), 132–140. https://doi.org/10.1097/XEB.0000000000000055
Rojas-Rueda, D., Morales-Zamora, E., Alsufyani, W. A., Herbst, C. H., Al Balawi, S. M., Alsukait, R., & Alomran, M. (2021). Environmental risk factors and health: An umbrella review of meta-analyses. International Journal of Environmental Research and Public Dealth , 18 (2), 704. https://doi.org/10.3390/ijerph18020704
A meta-analysis is a "technique that statistically combines the results of quantitative studies to provide a more precise effect of the result" (Grant & Booth, 2009, p. 98).
- Statistical technique for combining results of quantitative studies to provide more precise effect of results
- Aims for exhaustive, comprehensive searching
- Quality assessment may determine inclusion/exclusion criteria
- May be conducted independently or as part of a systematic review
Berman, N. G., & Parker, R. A. (2002). Meta-analysis: Neither quick nor easy. BMC Medical Research Methodology , 2(1), 10. https://doi.org/10.1186/1471-2288-2-10
Hites R. A. (2004). Polybrominated diphenyl ethers in the environment and in people: a meta-analysis of concentrations. Environmental Science & Technology , 38 (4), 945–956. https://doi.org/10.1021/es035082g
A systematic review "seeks to systematically search for, appraise, and [synthesize] research evidence, often adhering to the guidelines on the conduct of a review" provided by discipline-specific organizations, such as the Cochrane Collaboration (Grant & Booth, 2009, p. 102).
- Aims to compile and synthesize all known knowledge on a given topic
- Adheres to strict guidelines, protocols, and frameworks
- Time-intensive and often takes months to a year or more to complete
- The most commonly referred to type of evidence synthesis. Sometimes confused as a blanket term for other types of reviews
Gascon, M., Triguero-Mas, M., Martínez, D., Dadvand, P., Forns, J., Plasència, A., & Nieuwenhuijsen, M. J. (2015). Mental health benefits of long-term exposure to residential green and blue spaces: a systematic review. International Journal of Environmental Research and Public Health , 12 (4), 4354–4379. https://doi.org/10.3390/ijerph120404354
"Systematized reviews attempt to include one or more elements of the systematic review process while stopping short of claiming that the resultant output is a systematic review" (Grant & Booth, 2009, p. 102). When a systematic review approach is adapted to produce a more manageable scope, while still retaining the rigor of a systematic review such as risk of bias assessment and the use of a protocol, this is often referred to as a structured review (Huelin et al., 2015).
- Typically conducted by postgraduate or graduate students
- Often assigned by instructors to students who don't have the resources to conduct a full systematic review
Salvo, G., Lashewicz, B. M., Doyle-Baker, P. K., & McCormack, G. R. (2018). Neighbourhood built environment influences on physical activity among adults: A systematized review of qualitative evidence. International Journal of Environmental Research and Public Health , 15 (5), 897. https://doi.org/10.3390/ijerph15050897
Huelin, R., Iheanacho, I., Payne, K., & Sandman, K. (2015). What’s in a name? Systematic and non-systematic literature reviews, and why the distinction matters. https://www.evidera.com/resource/whats-in-a-name-systematic-and-non-systematic-literature-reviews-and-why-the-distinction-matters/

- Review Decision Tree - Cornell University For more information, check out Cornell's review methodology decision tree.
- LitR-Ex.com - Eight literature review methodologies Learn more about 8 different review types (incl. Systematic Reviews and Scoping Reviews) with practical tips about strengths and weaknesses of different methods.
- << Previous: Getting started
- Next: 1. Define your research question >>
- Last Updated: Apr 3, 2024 12:40 PM
- URL: https://guides.library.duke.edu/lit-reviews

Services for...
- Faculty & Instructors
- Graduate Students
- Undergraduate Students
- International Students
- Patrons with Disabilities
- Harmful Language Statement
- Re-use & Attribution / Privacy
- Support the Libraries

- Locations and Hours
- UCLA Library
- Research Guides
- Biomedical Library Guides
Systematic Reviews
- Types of Literature Reviews
What Makes a Systematic Review Different from Other Types of Reviews?
- Planning Your Systematic Review
- Database Searching
- Creating the Search
- Search Filters & Hedges
- Grey Literature
- Managing & Appraising Results
- Further Resources
Reproduced from Grant, M. J. and Booth, A. (2009), A typology of reviews: an analysis of 14 review types and associated methodologies. Health Information & Libraries Journal, 26: 91–108. doi:10.1111/j.1471-1842.2009.00848.x
- << Previous: Home
- Next: Planning Your Systematic Review >>
- Last Updated: Apr 10, 2024 11:08 AM
- URL: https://guides.library.ucla.edu/systematicreviews
Penn State University Libraries
Soc 001: introductory sociology.
- Literature Reviews: Strategies for Writing
- Fake News and Evaluating Sources

Literature Reviews
What is a Literature Review? The literature review is a critical look at the existing research that is significant to the work that you are carrying out. This overview identifies prominent research trends in addition to assessing the overall strengths and weaknesses of the existing research.
Purpose of the Literature Review
- To provide background information about a research topic.
- To establish the importance of a topic.
- To demonstrate familiarity with a topic/problem.
- To “carve out a space” for further work and allow you to position yourself in a scholarly conversation.
Characteristics of an effective literature review In addition to fulfilling the purposes outlined above, an effective literature review provides a critical overview of existing research by
- Outlining important research trends.
- Assessing strengths and weaknesses (of individual studies as well the existing research as a whole).
- Identifying potential gaps in knowledge.
- Establishing a need for current and/or future research projects.
Steps of the Literature Review Process
1) Planning: identify the focus, type, scope and discipline of the review you intend to write. 2) Reading and Research: collect and read current research on your topic. Select only those sources that are most relevant to your project. 3) Analyzing: summarize, synthesize, critique, and compare your sources in order to assess the field of research as a whole. 4) Drafting: develop a thesis or claim to make about the existing research and decide how to organize your material. 5) Revising: revise and finalize the structural, stylistic, and grammatical issues of your paper.
This process is not always a linear process; depending on the size and scope of your literature review, you may find yourself returning to some of these steps repeatedly as you continue to focus your project.
These steps adapted from the full workshop offered by the Graduate Writing Center at Penn State.
Literature Review Format
Introduction
- Provide an overview of the topic, theme, or issue.
- Identify your specific area of focus.
- Describe your methodology and rationale. How did you decide which sources to include and which to exclude? Why? How is your review organized?
- Briefly discuss the overall trends in the published scholarship in this area.
- Establish your reason for writing the review.
- Find the best organizational method for your review.
- Summarize sources by providing the most relevant information.
- Respectfully and objectively critique and evaluate the studies.
- Use direct quotations sparingly and only if appropriate.
Conclusion
- Summarize the major findings of the sources that you reviewed, remembering to keep the focus on your topic.
- Evaluate the current state of scholarship in this area (ex. flaws or gaps in the research, inconsistencies in findings)
- Identify any areas for further research.
- Conclude by making a connection between your topic and some larger area of study such as the discipline.
- << Previous: Home
- Next: Fake News and Evaluating Sources >>
- Last Updated: Oct 20, 2023 10:48 AM
- URL: https://guides.libraries.psu.edu/shenangosoc001
- Open access
- Published: 09 April 2024
Patient characteristics of, and remedial interventions for, complaints and medico-legal claims against doctors: a rapid review of the literature
- Timothy J. Schultz ORCID: orcid.org/0000-0003-1419-3328 1 ,
- Michael Zhou 2 ,
- Jodi Gray 1 ,
- Jackie Roseleur 1 ,
- Richard Clark 1 , 3 ,
- Dylan A. Mordaunt 1 , 4 ,
- Peter D. Hibbert 5 , 6 ,
- Georgie Haysom 7 &
- Michael Wright 7 , 8
Systematic Reviews volume 13 , Article number: 104 ( 2024 ) Cite this article
257 Accesses
1 Altmetric
Metrics details
It is uncertain if patient’s characteristics are associated with complaints and claims against doctors. Additionally, evidence for the effectiveness of remedial interventions on rates of complaints and claims against doctors has not been synthesised.
We conducted a rapid review of recent literature to answer: Question 1 “What are the common characteristics and circumstances of patients who are most likely to complain or bring a claim about the care they have received from a doctor?” and Question 2 “What initiatives or interventions have been shown to be effective at reducing complaints and claims about the care patients have received from a doctor?”. We used a systematic search (most recently in July 2023) of PubMed, Scopus, Web of Science and grey literature. Studies were screened against inclusion criteria and critically appraised in duplicate using standard tools. Results were summarised using narrative synthesis.
From 8079 search results, we reviewed the full text of 250 studies. We included 25 studies: seven for Question 1 (6 comparative studies with controls and one systematic review) and 18 studies for Question 2 (14 uncontrolled pre-post studies, 2 comparative studies with controls and 2 systematic reviews). Most studies were set in hospitals across a mix of medical specialties.
Other than for patients with mental health conditions (two studies), no other patient characteristics demonstrated either a strong or consistent effect on the rate of complaints or claims against their treating doctors.
Risk management programs (6 studies), and communication and resolution programs (5 studies) were the most studied of 6 intervention types. Evidence for reducing complaints and medico-legal claims, costs or premiums and more timely management was apparent for both types of programs. Only 1 to 3 studies were included for peer programs, medical remediation, shared decision-making, simulation training and continuing professional development, with few generalisable results.
Few patient characteristics can be reliably related to the likelihood of medico-legal complaints or claims. There is some evidence that interventions can reduce the number and costs of claims, the number of complaints, and the timeliness of claims. However, across both questions, the strength of the evidence is very weak and is based on only a few studies or study designs that are highly prone to bias.
Peer Review reports
Up to 10% of hospital patients experience an adverse event [ 1 ]. Medical negligence or the failure to meet the standard of care reasonably expected of an ‘average’ doctor is a contributing factor to a small proportion of adverse events [ 1 , 2 ]. Medico-legal claims seeking compensation for medical negligence may be filed against doctors by patients through civil litigation. For less serious events or to express dissatisfaction with care, patients may also make a formal complaint, either directly to their care provider or the provider’s employer or to medical and other regulators and health complaints entities [ 3 ].
Doctors’ demographic (e.g. gender, age, years spent in practice) and workplace-related factors (e.g. greater number of patient lists) are associated with the risk of complaints and malpractice claims [ 4 , 5 ]. It is less clear what, if any, patient characteristics are associated with complaints and claims, and anecdotal evidence suggests that the rate of complaints and claims is rising [ 6 ]. Though females may be more likely to complain, and complaints and claims are often raised by patients’ living or bereaved relatives [ 7 , 8 ], there are no relevant systematic reviews on this topic. This led to the following review question (Question 1) “What are the common characteristics and circumstances of patients who are most likely to complain or bring a claim about the care they have received from a doctor?”.
In addition to the impact on patient wellbeing, doctors involved in adverse events experience serious emotional and psychological impacts [ 9 ]. Additionally, the financial cost to health systems from medico-legal claims is significant, potentially jeopardising the long-term financial sustainability of some public health systems [ 10 ]. Doctors, hospitals, health services, health regulators, representative medical organisations and medical insurers are therefore all highly motivated to provide safe, high-quality care that minimises complaints and claims against them, their staff, stakeholders and members. For example, medical colleges, practitioner regulation boards and medical indemnity insurers maintain professional standards of their members and conduct activities such as continuing professional development (CPD) [ 11 ], remediation programs [ 12 ] and communication and resolution programs (CRPs) [ 13 ]. Despite a recent scoping review describing how remediation programs are delivered to regulated health professionals [ 14 ], there is no substantive review of the literature across the wide range of stakeholders and potential interventions applicable to reduce complaints and claims against doctors. We therefore posed the following additional review question (Question 2): “What initiatives or interventions have been shown to be effective at reducing complaints and claims about the care patients have received from a doctor?” [ 6 ].
Review objective and research questions
The purpose of this review was to provide an evidence-based foundation to understand which patient factors influence complaints or claims and what interventions can support a reduction in complaints or claims [ 6 ]. This information could be used by clinicians, hospital administrators, healthcare regulators and medical indemnity insurers to inform their practice and policy. For the purposes of this study, a “claim” was defined as an assertion of wrongdoing that forms the basis for a request for compensation [ 15 ]; an “unwarranted” claim occurred when the care provided had not been below the expected standard and the complaint was not otherwise warranted [ 6 ].
A protocol defining the scope of the review (PEO/PICO, inclusion and exclusion criteria, search strategy and limits) was developed according to Sax Institute guidelines [ 16 ] but was not prospectively registered. The review was conducted according to guidance provided by the Cochrane Rapid Review method [ 17 ] and the SelecTing Approaches for Rapid Reviews (STARR) approach [ 18 ]. The updated Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) checklist was used to report review findings [ 19 ].
Scope of the review
The review focussed on health systems of high-income Commonwealth countries including Australia, New Zealand, Canada and the United Kingdom (UK). Additionally, studies from the United States of Amercia (USA), Ireland and Western Europe were included to inform the review. The review focussed on the peer-reviewed literature although grey literature of similar quality was also searched. The review was conducted over an 8-week period from September to October 2022. The search was repeated in September 2023.
Inclusion and exclusion criteria
The inclusion and exclusion criteria for Question 1 and Question 2 are included in Table 1 . The settings were hospitals (excluding the emergency department), primary care and secondary care. Regulatory complaints, complaints to practices or hospitals and claims for compensation were included, while complaints on social media were excluded. For Question 1, the review focussed on correlations between the ‘exposure’ (e.g. patient characteristics) and the number, type or nature of complaints/claims. For Question 2, the review included interventions implemented primarily to reduce the number of complaints/claims against doctors, although other secondary outcomes included the costs of claims or insurance premiums, the duration of the claims management process, doctor risk profile or performance, doctor confidence/knowledge/satisfaction, workplace culture, and patient outcomes (e.g. morbidity) or patient satisfaction.
Only English language studies using quantitative study designs included in the National Health and Medical Research Council (NHRMC) guidelines [ 20 ] were included (e.g. ranging from level I systematic review, level II randomised controlled trial, level III pseudorandomised trial/comparative study with or without concurrent controls, and level IV case series with either post-test or pre-test/post-test outcomes). Cross-sectional studies were excluded.
Search strategy and selection criteria
Given the aetiological nature of studies relevant to Question 1 in particular, we used a PEO approach (Participant, Exposure, Outcome) [ 21 ] to frame the search strategy (see Supplementary Table S 1 , S 2 , S 3 ). Terms relating to ‘participants’ included doctors and health services. Terms relating to ‘exposure’ included patient characteristics (such as demographics, socio-economic status, and health literacy) for Question 1, and patient safety interventions (such as checklists, care bundles and teamwork) or clinical risk management programs (such as medical education, risk mitigation, peer program and communication and resolution) for Question 2. Terms relating to ‘outcomes’ included malpractice, negligence, complaint, claim management and medico-legal.
We searched three bibliographic databases (PubMed, Scopus and Web of Science) and grey literature sources (Google, Proquest Theses, GreyLit.org and Mednar) for relevant studies. The reference lists and citation searching of included studies were included as other search methods. To ensure applicability to a modern healthcare system only studies published since 2011 were included. The search was conducted first in September 2022 and then repeated in July 2023.
Screening based on title and abstract was conducted independently in pairs by four members of the research team (TS, MZ, JG, JR) following training on two sets of 100 studies.
Quality appraisal
The quality of included studies was appraised independently in pairs by four members of the research team (TS, JG, JR, PH) using AMSTAR 2 for systematic reviews [ 22 ] and National Institute of Health tools for case–control studies and uncontrolled pre-post studies [ 23 ]. These tools include 16 items (systematic reviews) or 12 items (case–control studies and uncontrolled pre-post), which were scored as ‘Yes’, ‘No’, ‘Not applicable’ or ‘Cannot determine’ [ 23 ], AMSTAR 2 also uses ‘Probably yes’.
Data collection
Data was extracted from each paper into a Microsoft Excel spreadsheet that had been pilot tested by three reviewers. Extraction was conducted by a single reviewer (TS or MZ) and then checked by a second reviewer (JG, JR).
A narrative synthesis was used to describe the key findings for both review questions. For review Question 1, results are presented separately for each patient characteristic, grouped according to patient demographics (e.g. age, sex, complainant), patient risk factors (e.g. American Society of Anaesthesiologists’ (ASA) score, the existence of a mental disorder, re-operation) and the therapeutic context (e.g. aspects of treatment, diagnosis, setting and/or phase of care including length of stay (LOS) and complications). For review Question 2, results are presented for seven different types of programs implemented to reduce the number of complaints and/or claims against doctors. The consistency, clinical impact, generalisability, and applicability of study findings were appraised using the NHRMC matrix which ranks each component’s strength using a four-point scale (excellent, good, satisfactory and poor) [ 20 ].
Literature search
Nearly 8900 studies were identified across the search strategy, of which 255 full texts were reviewed (Fig. 1 ). Of these, 230 were excluded as not relevant or due to an ineligible study design. A total of seven studies were included for Question 1, and 18 studies were included for Question 2 (Supplementary Table S 4 ).
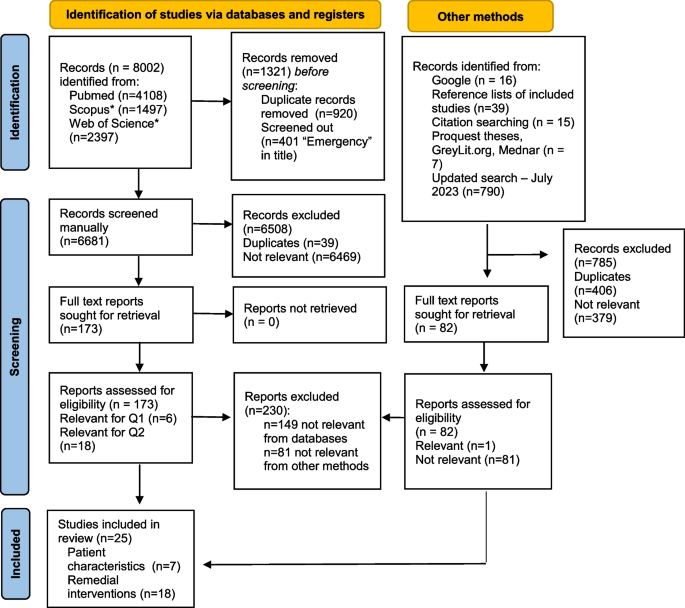
PRISMA study flow diagram [ 19 ]. * filters applied to these search results (Australia, New Zealand, Canada, UK)
The characteristics of the studies included for Question 1 are presented in Table 2 . There were six comparative studies with concurrent controls (three from the USA [ 24 , 25 , 26 ], two from the UK [ 27 , 28 ]) and one from Italy [ 29 ] and one systematic reviews of non-randomised control trials [ 3 ]. The in-patient hospital setting was most common ( n = 5) across a range of specialties and conditions, most commonly surgery. In total, there were 27 variables reported across the seven studies, 17 of these were included in multiple studies. Sex ( n = 6) and age ( n = 5) were the most frequently recorded patient demographics. For patient risk factors, ASA score, mental disorders, tobacco use and body mass index (BMI) > 30 were measured in two studies. For therapeutic context, LOS, setting, complications and treatment were measured in two studies.
Quality assessment is summarised in Table 2 , Supplementary Table S 5 (comparative studies) and Supplementary Table S 6 (systematic reviews). For the 6 comparative studies, 6 to 10 (mean 8.3, SD = 1.4) of 12 criteria were met; for the systematic review, 4 of the 16 criteria were met (or probably met).
In general, there was very limited evidence for the existence of significant relationships between patient characteristics and the rate of complaints or claims (Table 3 ). For demographics, one study identified that a 10-year increase in the age of paediatric surgery patients led to a near 50% greater odds (OR = 1.47, CI 1.04–2.08) of a complaint and that male gender reduced odds of a complaint in adults by 34% (OR = 0.66, CI 0.47–0.92) [ 25 ]. However, sex and age were not significant predictors in five and four other studies, respectively. A systematic review of 36 studies (comprising 44,211 complaints) estimated that 64% of complainants were patients and 26% were family members; the remaining 10% was not specified [ 3 ]. Of patient risk factors, patients with mental, behavioural, or neurodevelopmental disorders were significantly more likely to complain following hand and upper extremity surgery [ 24 ] and spine surgery [ 26 ] (Table 3 ).
In terms of therapeutic context, there were lower odds of a complaint for two procedural features: (i) use of a general anaesthetic in both paediatric and adult populations provided odds ratios, respectively, of 0.22 (CI 0.07–0.62) and 0.67 (CI 0.47–0.95) compared to no general anaesthetic, and (ii) a 1-h delay in actual start time led to slightly higher odds of a complaint, more notably in paediatrics (OR = 1.27, CI 1.10–1.47) than in adults (OR = 1.05, CI 0.95–1.16) [ 25 ]. The odds of a complaint were seven times greater for patients undergoing surgery (CI 5.2–9.6) [ 26 ]. The overuse of non-beneficial interventions and underuse of treatment escalation plans predicted complaints from the next-of-kin of patients who died in hospital [ 28 ]. For example, treatment escalation limitation plans were used significantly less frequently in complaints (23.8% versus 47.2%, P = 0.013) [ 28 ]. Other components of therapeutic context, including LOS, setting, and experiencing complications and harms, were not significant predictors of complaints (Table 3 ).
Uncontrolled pre-post studies ( n = 14) were the most common study design included for Question 2, followed by comparative studies with concurrent controls ( n = 2) and systematic reviews ( n = 2) (Table 4 ). Studies were set in the USA ( n = 12) [ 13 , 15 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 ], Canada ( n = 2) [ 40 , 41 ], the UK [ 12 ], Ireland [ 42 ] and New Zealand [ 43 ] ( n = 1, each). The studies addressed malpractice claims ( n = 9), complaints ( n = 5), and regulatory notifications ( n = 2) and a mix of outcomes ( n = 1). In-patient hospital ( n = 11) was the most common setting, followed by mixed ( n = 4), primary care and secondary care ( n = 1, each). There were seven types of interventions for Question 2 studies: risk management ( n = 6), CRPs ( n = 5) (note one study [ 31 ] assessed both), medical remediation ( n = 3), peer program ( n = 2) and, CPD, simulation training and shared decision-making ( n = 1, each). Quality assessment is summarised in Table 3 , Supplementary Table S 5 (comparative studies), Table S 7 (uncontrolled pre-post studies) and Supplementary Table S 6 (systematic reviews). Eight of the 12 criteria were met for the one comparative study; 3 to 11 of the 12 criteria were met for the 14 uncontrolled pre-post studies (mean 7.6, SD = 2.6); and 8 and 11 of the 16 criteria were met for the two systematic reviews.
Findings and definitions for Question 2 across the seven types of interventions and eight included outcomes are presented in Table 5 . No studies examined doctor satisfaction or patient outcomes (such as mortality or morbidity).
The six studies of risk management programs [ 31 , 32 , 34 , 38 , 40 , 42 ], also called risk reduction programs, were heterogeneous in nature, and included enhanced evaluation of, and response to, complaints [ 42 ], active engagement of physicians in risk assessment [ 32 ], lectures followed by a mock lawsuit [ 34 ], and education [ 38 , 40 ]. Evidence from these studies of risk management programs supported reductions in claims, complaints and claims costs (Table 5 ). Other benefits included more timely complaints management, improved patient safety culture and staff confidence.
Evidence for communication and resolution programs (CRPs, five studies [ 13 , 15 , 31 , 33 , 35 ]) was consistent across four studies. There were lower rates of claims and complaints, lower claim amounts, and faster resolution of claims following the implementation of CRPs (Table 5 ) [ 15 , 31 , 33 , 35 ]. However, results were less supportive in a study using an interrupted time series (ITS) design [ 13 ]. One study demonstrated improved patient satisfaction [ 33 ].
Three studies of medical remediation showed either a reduction in claims rates [ 12 ] or an improved doctor risk profile [ 29 , 43 ].
Two studies of peer review, or the use of peer messengers, demonstrated a reduction in either complaint rates [ 36 ] or improved doctor risk profile [ 37 ] (Table 5 ).
A systematic review of five studies concluded that there was insufficient evidence to determine whether or not shared decision-making reduces claims [ 44 ]. A retrospective pre-post program evaluation of simulation training on malpractice claims among obstetrician-gynaecologists reported that the rate of claims after simulation training was halved to 5.7 claims per 100 physician years of coverage. Attending more sessions was associated with a greater reduction in claims, although there was no difference in the total costs of paid claims before and after the training [ 39 ].
In one included study of CPD, doctors who reported participation in CPD activities were significantly less likely (OR 0.60; CI 0.39 to 0.95) to receive quality of care-related complaints than those who did not report participating in CPD [ 41 ]. Participants in group-based CPD were less likely (OR 0.68; CI 0.47 to 0.98) to receive quality of care-related complaints than individual or assessment-based CPD [ 41 ].
Summary of the evidence
A summary of the included studies’ evidence base, consistency, clinical impact, generalisability and applicability is included in Table 6 . The evidence base was rated as poor for both Question 1 and 2 (Table 6 ). Consistency and clinical impact were slightly higher for Question 2 than Question 1, whereas generalisability and applicability were satisfactory for both Question 1 and Question 2.
This review has identified a clear lack of recent high-quality studies to inform an in-depth understanding of either review Question 1 or Question 2. For Question 1, seven patient characteristics were associated with patients’ likelihood to complain or make a medico-legal claim against a doctor; however, only one of these findings (presence of a mental disorder) was replicated. This may be related to the paucity of studies, for example, only half of the patient characteristics were evaluated in more than one study. While more studies were included for Question 2, the low quality of the predominant study design (case series) severely limits the strength of the review’s findings.
The main finding for Question 1 of a relationship between a patient’s mental health status and complaint behaviour may reflect non-modifiable associations between underlying mental health conditions, poorer outcomes and reduced satisfaction after surgery [ 24 , 26 ]. Alternatively, the finding may reflect the impact of stigma experienced by these patients in healthcare settings. Mental illness-related stigma is prevalent in healthcare [ 51 ]. Stigma creates barriers to accessing healthcare, such as delays in help-seeking, treatment discontinuation, suboptimal therapeutic relationships, patient safety concerns and poorer quality care [ 52 ]. The presence of these barriers may be associated with a complaint about a healthcare provider.
Findings for Question 2 offer some evidence to support most of the included interventions, particularly risk management programs and CRPs. Some of the commonly occurring attributes of risk management programs were the evaluation and analysis of complaints and claims, targeted medico-legal education, and implementation of patient safety measures. The majority of the risk management programs were developed and delivered internally, either at the level of hospital department [ 38 ], hospital-wide [ 32 , 34 ] or general practice-level [ 42 ]. Local contextualisation, incorporating the site-specific nature of malpractice claims and legislation, and delivery of risk management programs apparently enhance the acceptability of risk management programs for surgeons, in particular [ 53 , 54 , 55 ]. Nevertheless, in one study, the Society of Obstetricians and Gynaecologists of Canada partnered with a healthcare insurance representative body to support the international expansion of a risk management program [ 40 ].
Studies of CRPs were generally consistent in showing lower rates of claims and complaints, lower claim amounts, and faster resolution of claims following the implementation of CRPs. However, limited adherence to the key components of CRP, including a proliferation of partial apology laws, may detract from the effectiveness of CRP in meeting the needs of injured patients [ 56 , 57 , 58 ]. Patients involved in CRP have expressed a greater desire for information provision from hospitals about efforts to prevent recurrences of the event [ 59 ].
Interventions such as caps on compensation, attorney fees, and alternative payment systems and liabilities [ 31 ] were excluded from the review as they are not doctor-directed interventions. The impacts of these medical malpractice reforms have been recently summarised [ 60 , 61 ].
The small number of included studies (Question 1) and the low quality of included studies (Question 2) represent major gaps in the evidence. For Question 1, there were a large number of excluded studies that were uncontrolled or unadjusted cross-sectional studies of complaints or claims that simply report the underlying characteristics of a claims database. Due to the lack of a control group, these studies do not provide particularly useful insights into the relationship between patient characteristics and the rate of complaints or claims. While more studies were included for Question 2, the predominant study design (i.e. uncontrolled pre-post) is weak as it does not permit adjustments for other secular trends in claims or confounders, or include control sites. Therefore, very little strength could be offered for recommendations emanating from either Question 1 or Question 2.
For Question 1, only one study specified whether a complaint was warranted or unwarranted [ 41 ]. No study included both types of complaints to determine predictors of successful interventions targeting unwarranted claims/complaints. The finding that a substantial subset of complaints originate from non-patient sources is likely to reduce the predictive value of patient characteristics for claims and complaints in this analysis. For Question 2, no studies assessed staff satisfaction or patient outcomes, such as mortality or morbidity. Additionally, there is rarely any evidence provided about generalisability or the potential for implementation and sustainability of the intervention, and most studies are limited to a single hospital/health service. Only one included study reported on the impact on organisational culture [ 40 ] or patient satisfaction [ 33 ].
All stages of the rapid review were conducted independently in duplicate to minimise the risk of errors. However, we only included studies published since 2011. This may have excluded relevant, older literature, which may be a limitation to this rapid review. Additionally, we filtered search results from the Scopus and Web of Science databases to countries with similar health systems (Australia, New Zealand, Canada and the UK) and screened out studies with ‘emergency’ in the title.
Conclusions
Despite substantial efforts made to collect information about patient complaints and claims, research has generally failed to robustly determine patient characteristics associated with complaints and claims. There is a small amount of evidence that patients with mental health conditions are more likely to complain.
The evidence for the effectiveness of interventions to reduce the likelihood of a doctor receiving a complaint or claim is also weak, as it is dominated by low-quality, uncontrolled pre-post studies. Only one or two studies were included for five types of programs (peer programs, medical remediation, shared decision-making, simulation training and CPD). More evidence, however, offers support for the effectiveness of risk management programs and CRPs in reducing complaints and claims.
Availability of data and materials
The datasets analysed during the current study are available from the corresponding author on reasonable request.
Runciman W, Merry A, Walton M. Safety and Ethics in Healthcare: A Guide to Getting it Right. Aldershot: Ashgate; 2007.
Google Scholar
Grober ED, Bohnen JMA. Defining medical error. Can J Surg. 2005;48(1):39–44.
PubMed PubMed Central Google Scholar
Reader TW, Gillespie A, Roberts J. Patient complaints in healthcare systems: a systematic review and coding taxonomy. BMJ Qual Saf. 2014;23(8):678–89.
Article PubMed PubMed Central Google Scholar
Austin EE, Do V, Nullwala R, Fajardo Pulido D, Hibbert PD, Braithwaite J, et al. Systematic review of the factors and the key indicators that identify doctors at risk of complaints, malpractice claims or impaired performance. BMJ Open. 2021;11(8):e050377.
Unwin E, Woolf K, Wadlow C, Potts HWW, Dacre J. Sex differences in medico-legal action against doctors: a systematic review and meta-analysis. BMC Med. 2015;13(1):172.
Institute S. Evidence Check: Doctors challenges and Patient complaints. Sydney: Sax Insititute; 2022.
Daniel AE, Burn RJ, Horarlk S. Patients’ complaints about medical practice. MJA. 1999;170(12):598–602.
CAS PubMed Google Scholar
Vincent C, Young M, Phillips A. Why do people sue doctors? A study of patients and relatives taking legal action. Lancet. 1994;343(8913):1609–13.
Article CAS PubMed Google Scholar
Wu AW. Medical error: the second victim. BMJ. 2000;320(7237):726.
Article CAS PubMed PubMed Central Google Scholar
Forrest C, O'Donoghue K, Collins DC, O'Reilly S. Current Irish medicolegal landscape: an unsustainable trajectory. BMJ Open Qual. 2023;12(3).
Forsetlund L, O'Brien MA, Forsén L, Mwai L, Reinar LM, Okwen MP, et al. Continuing education meetings and workshops: effects on professional practice and healthcare outcomes. Cochrane Database of Systematic Reviews. 2021(9).
O’Brien M, Dinwoodie M, Hartwig B, Blaney D. The Clinical Communication Program: an effective intervention for reducing future risk for high-risk physicians. Asia Pacific J Health Manage. 2014;9(1):8–13.
Kachalia A, Sands K, Niel MV, Dodson S, Roche S, Novack V, et al. Effects of a communication-and-resolution program on hospitals’ malpractice claims and costs. Health Aff. 2018;37(11):1836–44.
Article Google Scholar
Kennedy G, Jacobs N, Freemark L, Madan S, Chan N, Tran Y, et al. Remediation programs for regulated health care professionals: a scoping review. J Contin Educ Health Prof. 2022;42(1):36–46.
Article PubMed Google Scholar
Adams MA, Elmunzer BJ, Scheiman JM. Effect of a health system’s medical error disclosure program on gastroenterology-related claims rates and costs. Am J Gastroenterol. 2014;109(4):460–4.
Sax Institute. Evidence Check: a fast and accurate summary of the latest health evidence. Sydney: Sax Institute; 2022. [Available from: https://www.saxinstitute.org.au/wp-content/uploads/2022-Evidence-Check-Flyer.pdf .
Garritty C, Gartlehner G, Nussbaumer-Streit B, King VJ, Hamel C, Kamel C, et al. Cochrane rapid reviews methods group offers evidence-informed guidance to conduct rapid reviews. J Clin Epidemiol. 2021;130:13–22.
Pandor A, Kaltenthaler E, Martyn-St James M, Wong R, Cooper K, Dimairo M, et al. Delphi consensus reached to produce a decision tool for SelecTing Approaches for Rapid Reviews (STARR). J Clin Epidemiol. 2019;114:22–9.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
National Health and Medical Research Council. NHMRC levels of evidence and grades for recommendations for guideline developers. Canberra: NHMRC; 2009.
Moola S, Munn Z, Sears K, Sfetcu R, Currie M, Lisy K, et al. Conducting systematic reviews of association (etiology): the Joanna Briggs Institute’s approach. Int J Evid Based Healthc. 2015;13(3):163–9.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
NIH. Study Quality Assessment Tools 2021. Available from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools .
Grandizio LC, Barreto Rocha DF, Piper JP, Hayes DS, Klena JC. An analysis of formal patient complaints and malpractice events involving hand and upper extremity surgeons. J Am Acad Orthop Surg. 2021;29(15):659–65.
Kynes JM, Schildcrout JS, Hickson GB, Pichert JW, Han X, Ehrenfeld JM, et al. An analysis of risk factors for patient complaints about ambulatory anesthesiology care. Anesth Analg. 2013;116(6):1325–32.
Rae M, Barreto Rocha DF, Hayes DS, Haak M, Maniar H, Grandizio LC. Formal Patient Complaints and Malpractice Events Involving Orthopedic Spine Surgeons: A Ten-Year Analysis. Spine (Phila Pa 1976). 2022;47(14):E521-e6.
Jones K, Davies B, Stubbs DJ, Komashie A, Burnstein RM, Hutchinson P, et al. Can compliment and complaint data inform the care of individuals with chronic subdural haematoma (cSDH)? BMJ Open Qual. 2021;10(3).
Robin Taylor D, Bouttell J, Campbell JN, Lightbody CJ. A case-controlled study of relatives’ complaints concerning patients who died in hospital: the role of treatment escalation/limitation planning. Int J Qual Health C. 2020;32(3):212–8.
Facchin F, Pagani A, Perozzo FAG, Scarpa C, Bassetto F, Vindigni V. Litigation Cases After Post-Bariatric Surgery: Lesson from the Past. Aesthetic Plast Surg. 2023.
Cosman BC, Alverson AD, Boal PA, Owens EL, Norcross WA. Assessment and remedial clinical education of surgeons in California. Arch Surg. 2011;146(12):1411–5.
Cardoso R, Zarin W, Nincic V, Barber SL, Gulmezoglu AM, Wilson C, et al. Evaluative reports on medical malpractice policies in obstetrics: a rapid scoping review. Syst Rev. 2017;6(1):181.
Diraviam SP, Sullivan PG, Sestito JA, Nepps ME, Clapp JT, Fleisher LA. Physician engagement in malpractice risk reduction: A UPHS case study. Jt Comm J Qual Patient Saf. 2018;44(10):605–12.
PubMed Google Scholar
Fustino NJ, Moore P, Viers S, Cheyne K. Improving patient experience of care providers in a multispecialty ambulatory pediatrics practice. Clin Pediatr (Phila). 2019;58(1):50–9.
Juo YY, Lewis C, Hanna C, Reber HA, Tillou A. An innovative approach for familiarizing surgeons with malpractice litigation. J Surg Educ. 2019;76(1):127–33.
LeCraw FR, Montanera D, Jackson JP, Keys JC, Hetzler DC, Mroz TA. Changes in liability claims, costs, and resolution times following the introduction of a communication-and-resolution program in Tennessee. J Patient Saf Risk Manage. 2018;23(1):13–8.
Nassiri AM, Pichert JW, Domenico HJ, Galloway MB, Cooper WO, Bennett ML. Unsolicited patient complaints among otolaryngologists. Otolaryngol Head Neck Surg. 2019;160(5):810–7.
Pichert JW, Moore IN, Karrass J, Jay JS, Westlake MW, Catron TF, et al. An intervention model that promotes accountability: peer messengers and patient/family complaints. Jt Comm J Qual Patient Saf. 2013;39(10):435–46.
Raper SE, Rose D, Nepps ME, Drebin JA. Taking the initiative: risk-reduction strategies and decreased malpractice costs. J Am Coll Surg. 2017;225(5):612–21.
Schaffer AC, Babayan A, Einbinder JS, Sato L, Gardner R. Association of simulation training with rates of medical malpractice claims among obstetrician-gynecologists. Obstet Gynecol. 2021;138(2):246–52.
Milne JK, Walker DE, Vlahaki D. Reflections on the Canadian MORE(OB) obstetrical risk management programme. Best Pract Res Clin Obstet Gynaecol. 2013;27(4):563–9.
Wenghofer EF, Campbell C, Marlow B, Kam SM, Carter L, McCauley W. The effect of continuing professional development on public complaints: a case-control study. Med Educ. 2015;49(3):264–75.
Barragry RA, Varadkar LE, Hanlon DK, Bailey KF, O’Dowd TC, O’Shea BJ. An analytic observational study on complaints management in the general practice out of hours care setting: who complains, why, and what can we do about it? BMC Fam Pract. 2016;17(1):87.
Lillis S, Takai N, Francis S. Long-term outcomes of a remedial education program for doctors with clinical performance deficits. J Contin Educ Heal Prof. 2014;34(2):96–101.
Durand MA, Moulton B, Cockle E, Mann M, Elwyn G. Can shared decision-making reduce medical malpractice litigation? A systematic review. BMC Health Serv Res. 2015;15.
Price T, Archer J. UK policy on doctor remediation: trajectories and challenges. J Contin Educ Health Prof. 2017;37(3):207–11.
Price T, Brennan N, Wong G, Withers L, Cleland J, Wanner A, et al. Remediation programmes for practising doctors to restore patient safety: the RESTORE realist review. Health Serv Deliv Res. 2021;9(11):1–116.
Rout A, Roberts P. Peer review in nursing and midwifery: a literature review. J Clin Nurs. 2008;17(4):427–42.
Travaglia J, Debono D. Peer review in medicine: a comprehensive review of the literature. Sydney: Centre for Clinical Governance Research in Health; 2009.
Lateef F. Simulation-based learning: Just like the real thing. J Emerg Trauma Shock. 2010;3(4):348–52.
Royal Australasian College of Physicians. Continuing Professional Development (CPD) Participation Policy. Sydney: RACP; 2020.
Corrigan PW, Druss BG, Perlick DA. The impact of mental illness stigma on seeking and participating in mental health care. Psychol Sci Public Interest. 2014;15(2):37–70.
Knaak S, Mantler E, Szeto A. Mental illness-related stigma in healthcare: barriers to access and care and evidence-based solutions. Healthc Manage Forum. 2017;30(2):111–6.
Raper SE, Gupta M, Okusanya O, Morris JB. Improving communication skills: a course for academic medical center surgery residents and faculty. J Surg Educ. 2015;72(6):e202–11.
Raper SE, Joseph J, Seymour WG, Sullivan PG. Tipping the scales: educating surgeons about medical malpractice. J Surg Res. 2016;206(1):206–13.
Raper SE, Joseph J. Informed consent for academic surgeons: a curriculum-based update. MedEdPORTAL. 2020;16:10985.
Ross NE, Newman WJ. The role of apology laws in medical malpractice. J Am Acad Psychiatry Law. 2021;49(3):406–14.
Fields AC, Mello MM, Kachalia A. Apology laws and malpractice liability: what have we learned? BMJ Qual Saf. 2021;30(1):64–7.
Gallagher TH, Mello MM, Sage WM, Bell SK, McDonald TB, Thomas EJ. Can communication-and-resolution programs achieve their potential? Five key questions Health Affairs. 2018;37(11):1845–52.
Moore J, Bismark M, Mello MM. Patients’ experiences with communication-and-resolution programs after medical injury. JAMA Intern Med. 2017;177(11):1595–603.
Liu J, Hyman DA. The impact of medical malpractice reforms. Annual Rev Law Soc Sci. 2020. p. 405–19.
Agarwal R, Gupta A, Gupta S. The impact of tort reform on defensive medicine, quality of care, and physician supply: A systematic review. Health Services Research. 2019 2019/08//:851+.
Download references
Acknowledgements
We acknowledge the support of Eileen Goldberg and Richa Jaswal who brokered the review through the Sax Institute.
The project was funded by Avant Insurance Limited, Australia, which advised on the study protocol and approved publication. The authors alone are responsible for the views expressed in this review, and they do not necessarily represent the decisions, policies, or views of Avant Insurance Limited, Australia.
Author information
Authors and affiliations.
College of Medicine and Public Health, Flinders Health and Medical Research Institute, Flinders University, Adelaide, Australia
Timothy J. Schultz, Jodi Gray, Jackie Roseleur, Richard Clark & Dylan A. Mordaunt
College of Nursing and Health Sciences, Flinders University, Adelaide, Australia
Michael Zhou
HealthFX, Melbourne, Australia
Richard Clark
Southern Adelaide Local Health Network, Adelaide, Australia
Dylan A. Mordaunt
Australian Institute of Health Innovation, Macquarie University, Sydney, Australia
Peter D. Hibbert
IIMPACT in Health, Allied Health and Human Performance, University of South Australia, Adelaide, Australia
Avant Mutual, Sydney, Australia
Georgie Haysom & Michael Wright
Centre for Health Economics Research and Evaluation, University of Technology Sydney, Sydney, Australia
Michael Wright
You can also search for this author in PubMed Google Scholar
Contributions
TJS obtained funding, developed review methods, conducted the search, screened, critically appraised, extracted data, interpreted results, and wrote the manuscript. MZ screened, extracted data, interpreted results, and wrote the manuscript. JG and JR screened, critically appraised, extracted data; RC and DAM interpreted results. PDH critically appraised, interpreted results. GH and MW developed the protocol and interpreted results. All authors reviewed the manuscript and approved the submitted version. All authors are personally accountable for their own contributions.
Corresponding author
Correspondence to Timothy J. Schultz .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
Authors TJS, MZ, JG, JR, RC, DAM, and PDH declare no competing interests.
Authors GH and MW are employees of Avant Insurance Limited, Australia, a provider of medico-legal insurance.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: table s1..
Pubmed search - 8 September 2022. Table S2. Scopus search - 8 September 2022. Table S3. Web of Science - 8 September 2022. Table S4. Summary of study design for included studies for Question 1 and 2 using NHMRC levels of evidence [20]. Table S5. Summary of quality appraisal for eight comparative studies with concurrent controls, six for Question 1 (Q1) and two for Question 2 (Q2). Table S6. Summary of quality appraisal for three systematic reviews (one for Question 1 (Q1) and two for Question 2 (Q2)). Table S7. Summary of quality appraisal for 14 uncontrolled pre-post studies for Question 2 (Q2).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Schultz, T.J., Zhou, M., Gray, J. et al. Patient characteristics of, and remedial interventions for, complaints and medico-legal claims against doctors: a rapid review of the literature. Syst Rev 13 , 104 (2024). https://doi.org/10.1186/s13643-024-02501-8
Download citation
Received : 14 December 2023
Accepted : 20 February 2024
Published : 09 April 2024
DOI : https://doi.org/10.1186/s13643-024-02501-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medico-legal claims
- Communication and resolution program
- Risk management program
- Patient characteristics
- Patient safety
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Forensic neuropathology in the past decade: a scoping literature review
- Open access
- Published: 13 July 2023
Cite this article
You have full access to this open access article
- Petteri Oura 1 , 2 ,
- Antti Hakkarainen 1 , 2 &
- Antti Sajantila 1 , 2
1120 Accesses
1 Altmetric
Explore all metrics
While there has been notable research activity in the field of clinical neuropathology over the recent years, forensic approaches have been less frequent. This scoping literature review explored original research on forensic neuropathology over the past decade (January 1, 2010, until February 12, 2022) using the MEDLINE database. The aims were to (1) analyze the volume of research on the topic, (2) describe meta-level attributes and sample characteristics, and (3) summarize key research themes and methods. Of 5053 initial hits, 2864 fell within the target timeframe, and 122 were included in the review. Only 3–17 articles were published per year globally. Most articles originated from the Europe (39.3%) and Asia (36.1%) and were published in forensic journals (57.4%). A median sample included 57 subjects aged between 16 and 80 years. The most common research theme was traumatic intracranial injury (24.6%), followed by anatomy (12.3%) and substance abuse (11.5%). Key methods included immunotechniques (31.1%) and macroscopic observation (21.3%). Although a number of novel findings were reported, most were of preliminary nature and will require further validation. In order to reach breakthroughs and validate novel tools for routine use, more research input is urged from researchers across the world. It would be necessary to ensure appropriate sample sizes and make use of control groups.
Similar content being viewed by others

Forensic neurology: a distinct subspecialty at the intersection of neurology, neuroscience and law
R. Ryan Darby, Ciaran Considine, … William C. Darby

Forensic Pathology Historical Roots and Modern Evolution

Research on the Potential Biomarkers of Mild Traumatic Brain Injury: a Systematic Review and Bibliometric Analysis
Yishu Liu, Chudong Wang, … Jifeng Cai
Avoid common mistakes on your manuscript.
Introduction
Neurological diseases [ 1 ] and trauma to the central nervous system (CNS) [ 2 ] are common causes of death globally. A comprehensive postmortem examination of the CNS often requires particular expertise and sophisticated tissue processing techniques [ 3 , 4 ]. Neuropathological expertise is therefore of high value in both clinical [ 5 ] and forensic pathology [ 3 ]. While there has been notable research activity in the field of clinical neuropathology over the recent years [ 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 ], forensic approaches appear less frequent [ 16 , 17 , 18 , 19 , 20 ]. However, the role of CNS remains important in the medico-legal practice [ 21 , 22 , 23 , 24 ], as CNS-related findings may have pivotal significance in cause-of-death investigation [ 3 ] and legal proceedings [ 25 , 26 ].
Literature reviews aid in the efficient utilization of current knowledge. Systematic approaches are needed to summarize and disseminate research findings and identify gaps in the existing literature [ 27 ]. However, to the best of the authors’ knowledge, there are no broad-scoped overviews summarizing literature on forensic neuropathology, at least from the past decade. This scoping literature review explored literature on forensic neuropathology from January 1, 2010, until February 12, 2022. The aims were to (1) analyze the volume of research on the topic, (2) describe meta-level attributes and sample characteristics, and (3) summarize key research themes and methods.
Materials and methods
Research questions.
Scoping reviews are exploited to determine the scope and volume of literature on a given topic and to identify key concepts [ 28 , 29 ]. In contrast to systematic reviews, scoping reviews are particularly useful when the research question is broad and the body of literature has not been comprehensively reviewed before. We conducted a MEDLINE-based scoping review to explore scientific literature on forensic neuropathology published over the past decade.
The following research questions were formulated in accordance with the general aims of the study:
Volume of research
What is the volume of original research on forensic neuropathology per year?
Meta-level attributes and sample characteristics
Which journals publish studies on forensic neuropathology in terms of subspecialty and impact?
What is the geographical distribution of publications?
What kind of samples are used in terms of size and age distribution?
Research themes and methods
What are the key concepts, i.e., main research themes and methodological approaches in forensic neuropathology?
Are there knowledge gaps?
This review did not aim to summarize or classify particular findings of the studies; however, these are addressed in the supplementary material .
Search strategy, inclusion, and exclusion criteria
The search strategy was developed by the first author (P.O.) and reviewed by the last author of the paper (A.S.). Table 1 presents the specific search terms used in MEDLINE. Figure 1 is a flowchart demonstrating the article selection process with exclusions.
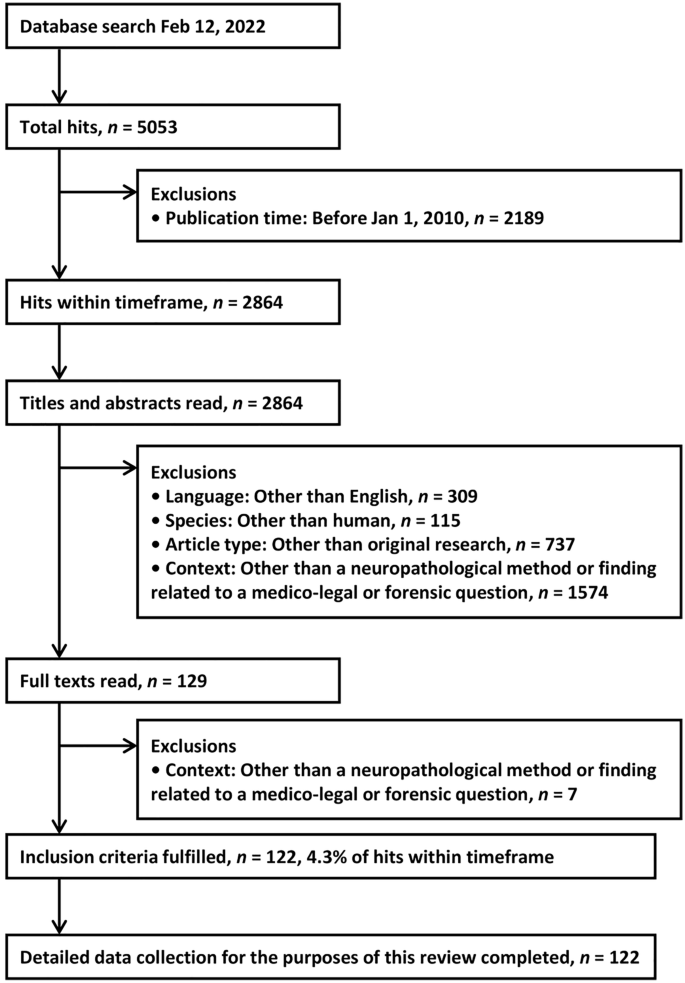
Flowchart demonstrating the article selection process with exclusions
We aimed to find peer-reviewed, original articles that addressed a neuropathological method or finding related to a medico-legal or forensic question in a human sample. A neuropathological method was defined as a macroscopic, microscopic, or other laboratory technique used to examine a tissue sample obtained from the CNS or intracranial structures including vasculature. We focused on English-language articles that were published and indexed in MEDLINE between January 1, 2010, and the database search date. Short communications, retrospective summaries of autopsy findings, and other similar publication types were included if they were original articles based on authentic human samples. Studies that solely focused on postmortem imaging, analysis of body fluids, human identification, or skull fractures without the use of neuropathological methods were excluded.
The search was conducted in the MEDLINE database February 12, 2022. First, P.O. screened all hits on the basis of titles, abstracts, and full texts, if necessary. Each hit was assigned with a rationale for inclusion or exclusion to be later validated by A.S.
Data extraction and synthesis
Data extraction was performed with the help of an Excel spreadsheet. Table 2 presents the variables collected in the data extraction process. The spreadsheet was a priori planned by P.O. and reviewed by A.S.; an internal pilot was carried out in the beginning of data collection (20 hits from the year 2010). Data extraction was performed on the basis of full texts and potential supplementary material of the articles. While P.O. was primarily responsible for extracting the data, the spreadsheet was reviewed and commented by A.S. A formal risk of bias assessment was not performed, as it is not customary in scoping reviews [ 28 ], and was not considered necessary in relation to the present research questions.
Data synthesis was conducted in accordance with the predefined research questions. The distributions of publication year, journal characteristics, geographical location, sample characteristics, primary research theme, and methodological approach were tabulated using frequencies with percentages or medians with interquartile ranges, as appropriate. In addition to these summary statistics, a supplementary table containing the extracted data of individual studies was constructed.
- Literature search
Of 5053 initial hits, 2864 fell within the target timeframe, and 122 were finally included in the review [ 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 , 141 , 142 , 143 , 144 , 145 , 146 , 147 , 148 , 149 , 150 , 151 ], corresponding to 4.3% of hits within timeframe (Fig. 1 ). Most exclusions were due to wrong context (e.g., forensic psychiatry) or article type (i.e., not original article). Individual summaries of the 122 included articles, together with aims and main findings, are presented in Supplementary Table 1 .
Meta-level attributes
Table 3 shows the annual distribution of publications over the review period; 3 to 17 articles were published per year globally. Table 4 is a bibliographic and geographic summary of the studies. Forensic journals were the most common publication channel (57.4%), followed by clinical journals (e.g., general medicine, neurology, or pediatric journals; 23.0%), and pathology journals (8.2%). Median impact factor was 2.3, while 11.5% of studies were published in journals without an Impact Factor. As for geographical distribution, Europe (39.3%) and Asia (36.1%) were the two most common study regions.
- Sample characteristics
Table 5 is a summary of sample characteristics. A median sample included 57 subjects (interquartile range 29–101; full range 4–1222), which included both cases and controls, if applicable. Control groups were utilized in less than half of the studies (43.4%). Medians of minimum and maximum ages were 16 and 80 years, respectively. A total of 30.3% of studies were based on adult-only samples, another 30.3% had both adults and minors, and 12.3% were based on minors. Subject ages were not stated in over a quarter of the studies (27.0%).
Lists of research themes and methodological approaches are presented in Table 6 . Individual summaries of the articles, together with aims and main findings, are presented in Supplementary Table 1 .
The most common research theme was traumatic intracranial injury (24.6%), which comprised focal and diffuse traumatic brain injuries [ 30 , 31 , 39 , 43 , 54 , 55 , 64 , 83 , 85 , 86 , 94 , 106 , 107 , 115 , 116 , 120 , 123 , 130 , 132 , 139 , 150 ] and traumatic intracranial hemorrhages [ 30 , 47 , 54 , 57 , 58 , 65 , 83 , 87 , 99 , 113 , 114 , 130 , 141 , 150 ]. Studies often used immunotechniques to identify traumatic changes and estimate the age of injury [ 39 , 85 , 86 , 87 , 94 , 106 , 107 , 115 , 120 , 132 , 139 ]. While some studies described macroscopic injury patterns and combinations in accident and assault scenarios [ 30 , 47 , 65 , 99 , 114 , 116 , 130 , 141 ], others used conventional histology [ 57 , 58 , 113 ] or several methods [ 31 , 43 , 54 , 55 , 64 , 83 , 150 ] to address varying research questions.
The second most common entity was anatomy (12.3%). While most studies described the anatomical variants of vasculature [ 41 , 68 , 75 , 105 , 126 , 127 , 135 ] and other intracranial structures [ 44 , 73 , 74 , 151 ], some aimed to generate reference values for brain weight in various populations [ 69 , 98 , 102 , 125 ]. The main techniques were macroscopic observation, conventional histology, and weight measurement. Moreover, one study evaluated the biomechanical properties of the dura mater [ 151 ].
Substance abuse was the primary entity in 11.5% of the studies. Both chronic and acute abuse were represented. The selection of substances included alcohols [ 38 , 52 , 82 ], opioids [ 38 , 100 , 109 , 117 , 118 , 119 ], stimulants [ 38 , 53 , 81 , 136 , 147 ], and other or multiple substances [ 48 , 50 , 117 , 118 ]. Immunotechniques [ 38 , 48 , 50 , 117 , 118 , 147 ], genetic techniques [ 81 ], or the two together [ 119 , 136 ] were often utilized to identify brain damage and distinguish substance abuse from other causes of death. Some studies primarily reported macroscopic observations [ 52 , 53 , 82 , 109 ] or brain weight [ 100 ] among substance abusers.
Laboratory methods were the main focus in 7.4% of the studies [ 45 , 67 , 70 , 72 , 97 , 111 , 133 , 138 , 148 ]. The studies showed notable heterogeneity, addressing technical aspects of, e.g., formalin pigment deposition [ 45 ], immunohistochemistry [ 133 ], DNA extraction [ 67 ], and freezing preparation of putrefied brain tissue [ 97 ].
Sudden unexpected deaths in infancy and childhood were addressed in 6.6% of the studies [ 33 , 40 , 51 , 61 , 66 , 79 , 84 , 91 ]. Immunotechniques [ 33 , 40 , 79 ], genetic techniques [ 51 ], conventional histology [ 91 ], and brain weight measurement [ 61 ] were used to uncover underlying mechanisms and identify brain tissue markers in these cases. Moreover, one study suggested an optimal neuropathologic examination protocol for these deaths in a medico-legal setting [ 66 ].
Other research themes were rarely addressed (< 5% each). Neurodegenerative diseases in medico-legal settings were approached using immunotechniques [ 128 , 143 , 144 ], image analysis [ 129 ], or a combination of several methods [ 104 , 112 ]. As for suicide, immunotechniques [ 32 , 89 ], genetic techniques [ 62 , 88 ], and brain weight measurement [ 146 ] were applied to identify factors that differentiate suicide victims from controls. Brain tissue markers of hypothermia and hyperthermia were studied by means of immunotechniques [ 78 , 140 , 145 ] and genetic techniques [ 60 ]. Studies that aimed to improve the estimation of postmortem interval were mainly based on immunotechniques [ 42 , 92 ] and genetic techniques [ 134 ]. Asphyxia and brain hypoxia [ 35 , 77 , 108 ], brain edema [ 36 , 37 , 96 ], brain tissue identification [ 95 , 121 , 122 ], drowning [ 34 , 71 ], and sudden unexpected death in epilepsy [ 63 , 149 ] were addressed in two to three individual studies each.
One article studied the markers of traumatic brain injury and mechanical asphyxiation using genetic techniques [ 49 ], while another focused on the potential markers of hypothermia, hyperthermia, and intoxication using immunotechniques and genetic techniques [ 59 ]. Finally, the following entities had one study each: sudden unexplained nocturnal death syndrome [ 46 ], pediatric subdural hemosiderin deposits [ 56 ], iron in fetal and infant leptomeninges [ 80 ], DNA identification based on brain tissue swab [ 76 ], zinc in brain tissue [ 90 ], intracranial aneurysms and dissections [ 101 ], age estimation [ 103 ], electrocution [ 124 ], insulin homicide [ 131 ], fire fatalities [ 137 ], phosphine poisoning [ 93 ], and carbon monoxide poisoning [ 142 ].
Main findings
This scoping review identified 122 original articles on forensic neuropathology from the years 2010–2022. Only 3–17 articles were published per year globally. Most articles originated from the Europe and Asia and were published in forensic journals. A median sample included 57 subjects aged between 16 and 80 years. The most common research theme was traumatic intracranial injury, followed by anatomy and substance abuse. Main methods included immunotechniques and macroscopic observation. To the best of the authors’ knowledge, this is the first scoping review to systematically explore literature on forensic neuropathology over the past decade.
Meta-level considerations
The annual volume of research output was relatively low, which may indicate rather mild research activity in the field globally. It is obvious that breakthroughs will require consistent scientific effort and active involvement of forensic pathologists in research projects. Clinical neuropathology may have outpowered the forensic branch, possibly due to stronger translational potential and active interplay with clinicians [ 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 ]. Neuropathology is an interdisciplinary field, touching upon neighboring fields such as neurology, neurosurgery, psychiatry, legal medicine, and general pathology. Forensic neuropathology is aligned in the midway between clinical and forensic pathology, often requiring particular expertise from a general forensic pathologist [ 22 ]. Interdisciplinary cooperation may thus be the key to increasing research activity in the field.
Articles were widely distributed between journals of various disciplines, which underlines the intersectoral nature of the field. In general, articles were published in international, field-specific journals with a median impact factor of 2.3. However, it is noteworthy that over a tenth of the articles were published in journals with no impact factor whatsoever; anatomic reports appeared to be overrepresented in this subgroup. As for geographical distribution, the vast majority of articles were from European and Asian researchers. Notably, articles from American groups were less common, and only two African articles were published over the entire review period. In order to expedite the development and implementation of forensic neuropathology globally, research input is needed from medico-legal units across the world. Unfortunately, achieving this objective may prove difficult due to resource- and policy-related barriers. It would be important to ensure sufficient personnel resources, methodological expertise, access to research funding, and comprehensible research permit policies for medico-legal data.
Sample-related considerations
Sample sizes were moderate, with a median of 57 subjects; this included both cases and potential controls. Two articles appeared to lack a clear indication of sample size. Despite the relatively small sample sizes, statistical power calculations were rarely presented. In quantitative studies, power calculations guide sample collection and corroborate the statistical approach [ 152 ]. Of note is also the fact that over a half of the studies did not have a control group, which implies that most articles were descriptive in nature. A comparative design is a prerequisite for many scientifically relevant conclusions [ 153 ].
Age ranges were generally wide, which increased the generalizability of findings across age groups. However, taking into account the moderate sample sizes, the level of heterogeneity within samples may significantly increase with widening age spans. Over a quarter of studies appeared to lack a clear statement of the minimum and maximum ages of the sample; some reported standard deviations and interquartile ranges instead.
Research themes, methods, and future directions
Traumatic intracranial injury was the most common research theme. Research activity around the topic is easy to comprehend as traumatic brain injury and intracranial hemorrhages are complex and deadly entities that often present themselves to a forensic pathologist [ 2 , 21 ]. As neuropathology may have a pivotal role in a cause-of-death investigation [ 3 ] or legal proceedings [ 25 , 26 ], novel tools are needed to identify traumatic changes and estimate the age of injury. However, significant breakthroughs are yet to come.
Alongside traumatic intracranial injury, the top-three research themes included anatomy and substance abuse. Somewhat surprisingly, macroscopic and microscopic anatomy of intracranial structures were among the most popular research themes. Many of these studies reported important findings for neurosurgeons, for example, but appeared to make a minor contribution to the field of forensic neuropathology. Substance abuse, which indeed is a central medico-legal entity [ 154 ], was approached from a variety of perspectives method- and substance-wise. However, more research input will be needed to identify substance-specific markers in brain tissue and differentiate substance abuse and intoxication from other causes of death.
Neurodegenerative diseases were addressed in a handful of studies. In spite of the vast research activity in clinical neuropathology, studies in medico-legal samples are also important, as neurodegenerative diseases appear to increase the risk of unnatural deaths [ 155 ]. Providing medico-legal units with diagnostic methods that have been validated in medico-legal samples will be of utmost importance. As for sudden unexplained deaths among infants and children, studies have kept chasing potential mechanisms and biomarkers, but again, significant breakthroughs are yet to come.
Although suicide is a major and diverse entity in forensic pathology [ 156 ], only a few studies addressed the topic. Considering the obscurity behind predisposing and underlying factors, there should be a lot to achieve mechanism- and prevention-wise. Medico-legal samples may have significant translational potential in this regard. Moreover, only a few studies addressed asphyxia, drowning, hypothermia, hyperthermia, sudden unexpected death in epilepsy, and estimation of postmortem interval. Higher research activity should be directed toward these themes in order to improve postmortem diagnostics.
Immunotechniques, i.e., immunohistochemistry and immunoblotting, were commonly applied to detect potential changes in brain tissue. Genetic techniques were exploited in various approaches such as brain tissue identification and gene expression analysis. A minority of studies used conventional histology as the main method. Although a number of novel findings were reported, most were of preliminary nature and will require further validation. Macroscopic observation of intracranial structures was a common method, but the studies often merely described injury patterns or anatomic variations. The crude measurement of brain weight was also used in some studies, but these often had null findings.
Limitations of the review
This scoping review had several limitations that should be considered. First, the scope of the literature search was notably broad, and conventional search terms were covered. However, articles that used specific or uncommon terminology may have been omitted. A large number of initial hits were obtained and manually evaluated, which may have reduced the risk of omitting in-scope articles. Second, as the review focused on original articles, emerging research themes may not have been fully covered. Moreover, there is a large body of research that may not be captured in this review even though it is relevant to forensic neuropathologists (e.g., CNS infections and emerging concepts in neurodegenerative diseases). Future reviews are expected to cover these aspects. Finally, as the aim was to explore and summarize original research in the field, there were no particular restrictions on scientific rigor, and no formal bias assessment was performed.
This scoping literature review explored original research on forensic neuropathology over the years 2010–2022. A total of 122 original articles were eventually included in the synthesis. Traumatic intracranial injury was the most common research theme, immunotechniques being the most commonly applied method. Only 3–17 articles were published per year globally. Although a number of novel findings were reported, most were of preliminary nature and will require further validation. In order to reach breakthroughs and validate novel tools for routine use, more research input is urged in forensic neuropathology from researchers across the world. Interdisciplinary cooperation may be the key to increasing research activity in the field. Researchers should ensure appropriate sample sizes and make use of comparative designs whenever possible.
Knowledge of diseases and trauma related to the central nervous system has high value in forensic pathology
This scoping review explored literature on forensic neuropathology from 2010 to 2022
A total of 122 original articles were included, corresponding to 3–17 publications per year globally
4.The most common research theme was traumatic intracranial injury (24.6%), followed by anatomy (12.3%) and substance abuse (11.5%). Key methods included immunotechniques (31.1%) and macroscopic observation (21.3%)
To reach breakthroughs and validate tools for routine practice, more research input is needed from researchers across the world
Availability of data and material
This is a review of published literature. The dataset generated and analysed during the study is presented in Supplementary Table 1 .
Code availability
Not applicable.
GBD 2016 Neurology Collaborators. Global, regional, and national burden of neurological disorders, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18:459–80.
Rubiano AM, Carney N, Chesnut R, Puyana JC. Global neurotrauma research challenges and opportunities. Nature. 2015;527:S193–7.
Kalimo H, Saukko P, Graham D. Neuropathological examination in forensic context. Forensic Sci Int. 2004;146:73–81.
Bruner JM, Louis DN, McLendon R, Rosenblum MK, Archambault WT, Most S, et al. The utility of expert diagnosis in surgical neuropathology: Analysis of consultations reviewed at 5 national comprehensive cancer network institutions. J Neuropathol Exp Neurol. 2017;76:189–94.
Iacono D, Geraci-Erck M, Peng H, Bouffard JP. Symmetric bihemispheric postmortem brain cutting to study healthy and pathological brain conditions in humans. J Vis Exp. 2016;118:54602.
Trejo-Lopez JA, Yachnis AT, Prokop S. Neuropathology of Alzheimer’s disease. Neurotherapeutics. 2022;19:173–85.
Kon T, Tomiyama M, Wakabayashi K. Neuropathology of Lewy body disease: Clinicopathological crosstalk between typical and atypical cases. Neuropathology. 2020;40:30–9.
Koga S, Sekiya H, Kondru N, Ross OA, Dickson DW. Neuropathology and molecular diagnosis of synucleinopathies. Mol Neurodegener. 2021;16:83.
Lassmann H. The contribution of neuropathology to multiple sclerosis research. Eur J Neurol. 2022;29:2869–2877.
Clark HB. The neuropathology of autoimmune ataxias. Brain Sci. 2022;12:257.
Fetit R, Hillary RF, Price DJ, Lawrie SM. The neuropathology of autism: A systematic review of post-mortem studies of autism and related disorders. Neurosci Biobehav Rev. 2021;129:35–62.
Cole BL. Neuropathology of pediatric brain tumors: A concise review. Neurosurgery. 2022;90:7–15.
von Spreckelsen N, Kesseler C, Brokinkel B, Goldbrunner R, Perry A, Mawrin C. Molecular neuropathology of brain-invasive meningiomas. Brain Pathol. 2022;32:e13048.
Seilhean D. Infections of the central nervous system: Neuropathology. Rev Neurol (Paris). 2019;175:431–5.
Maiese A, Manetti AC, Bosetti C, del Duca F, la Russa R, Frati P, et al. SARS-CoV-2 and the brain: A review of the current knowledge on neuropathology in COVID-19. Brain Pathol. 2021;31:e13013.
Mavroudis I, Kazis D, Chowdhury R, Petridis F, Costa V, Balmus I-M, et al. Post-concussion syndrome and chronic traumatic encephalopathy: Narrative review on the neuropathology, neuroimaging and fluid biomarkers. Diagnostics (Basel). 2022;12:740.
Zhang L, Lucassen PJ, Salta E, Verhaert PDEM, Swaab DF. Hippocampal neuropathology in suicide: Gaps in our knowledge and opportunities for a breakthrough. Neurosci Biobehav Rev. 2022;132:542–52.
Patodia S, Somani A, Thom M. Review: Neuropathology findings in autonomic brain regions in SUDEP and future research directions. Auton Neurosci. 2021;235:102862.
McGuone D, Crandall LG, Devinsky O. Sudden unexplained death in childhood: A neuropathology review. Front Neurol. 2020;11:582051.
Zwirner J, Kulakofsky R, Fitzek A, Schröder AS, Bohnert S, Franke H, et al. Forensic biomarkers of lethal traumatic brain injury. Int J Legal Med. 2022;136:871–86.
Bertozzi G, Maglietta F, Sessa F, Scoto E, Cipolloni L, di Mizio G, et al. Traumatic brain injury: A forensic approach: A literature review. Curr Neuropharmacol. 2020;18:538–50.
Article CAS PubMed PubMed Central Google Scholar
Stewart W, Black M, Kalimo H, Graham DI. Non-traumatic forensic neuropathology. Forensic Sci Int. 2004;146:125–47.
Balestrini S, Iacono D, Devinsky O, Mcguone D, Crandall LG. Sudden unexplained death in childhood: A neuropathology review. Front Neurol. 2020;11:582051.
MacKenzie JM. Examining the decomposed brain. Am J Forensic Med Pathol. 2014;35:265–70.
Kresak JL, Zehe S, Reichard RR. What every neuropathologist needs to know: Neuropathology and the US legal system. J Neuropathol Exp Neurol. 2019;78:291–3.
Whitwell H, Milroy C, du Plessis D. Forensic Neuropathology. 2nd Ed. London: CRC Press; 2021.
Book Google Scholar
Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A, Mcewen SA. A scoping review of scoping reviews: Advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5:371–85.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:143.
Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13:141–6.
Aghakhani K, Heidari M, Ameri M, Mehrpisheh S, Memarian A. Characteristics of traumatic brain injury among accident and falling down cases. Acta Med Iran. 2015;53:652–5.
PubMed Google Scholar
Al-Sarraj S, Fegan-Earl A, Ugbade A, Bodi I, Chapman R, Poole S, et al. Focal traumatic brain stem injury is a rare type of head injury resulting from assault: A forensic neuropathological study. J Forensic Leg Med. 2012;19:144–51.
Article PubMed Google Scholar
Alvarado-Esquivel C, Mendoza-Larios LA, García-Dolores F, Sánchez-Anguiano LF, Antuna-Salcido EI, Hernández-Tinoco J, et al. Association between Toxoplasma gondii infection in brain and a history of depression in suicide decedents: A cross-sectional study. Pathogens. 2021;10:1313.
Ambrose N, Waters KA, Rodriguez ML, Bailey K, Machaalani R. Neuronal apoptosis in the brainstem medulla of sudden unexpected death in infancy (SUDI), and the importance of standardized SUDI classification. Forensic Sci Med Pathol. 2018;14:42–56.
Article CAS PubMed Google Scholar
An J-L, Ishida Y, Kimura A, Kondo T. Immunohistochemical examination of intracerebral aquaporin-4 expression and its application for differential diagnosis between freshwater and saltwater drowning. Int J Legal Med. 2011;125:59–65.
Bartschat S, Fieguth A, Könemann J, Schmidt A, Bode-Jänisch S. Indicators for acute hypoxia-An immunohistochemical investigation in cerebellar Purkinje-cells. Forensic Sci Int. 2012;223:165–70.
Bauer M, Deigendesch N, Wittig H, Scheurer E, Lenz C. Tissue sample analysis for post mortem determination of brain edema. Forensic Sci Int. 2021;323:110808.
Bauer M, Gerlach K, Scheurer E, Lenz C. Analysis of different post mortem assessment methods for cerebral edema. Forensic Sci Int. 2020;308:110164.
Bohnert S, Georgiades Kosmas, ·, Monoranu C-M, Bohnert · Michael, Büttner A, Ondruschka B. Quantitative evidence of suppressed TMEM119 microglial immunohistochemistry in fatal morphine intoxications. Int J Legal Med. 2021;135:2315–22.
Article PubMed PubMed Central Google Scholar
Bohnert S, Seiffert A, Trella S, Bohnert M, Distel L, Ondruschka B, et al. TMEM119 as a specific marker of microglia reaction in traumatic brain injury in postmortem examination. Int J Legal Med. 2020;134:2167–76.
Bright FM, Byard RW, Vink R, Paterson DS. Medullary serotonin neuron abnormalities in an Australian cohort of sudden infant death syndrome. J Neuropathol Exp Neurol. 2017;76:864–73.
Bruno-Mascarenhas MA, Ramesh VG, Venkatraman S, Mahendran J v., Sundaram S. Microsurgical anatomy of the superior sagittal sinus and draining veins. Neurol India. 2017;65:794–800.
Campell ZK, Kwon I, Finley SJ, Lee Y, Javan GT. Talin: A potential protein biomarker in postmortem investigations. J Forensic Leg Med. 2016;44:188–91.
Castellani RJ, Smith M, Bailey K, Perry G, Dejong JL. Neuropathology in consecutive forensic consultation cases with a history of remote traumatic brain injury. J Alzheimers Dis. 2019;72:683–91.
Cavdar S, Solmaz B, Tanis Ö, Guler O, Dalcik H, Aydogmus E, et al. Anatomic variations of the human falx cerebelli and its association with occipital venous sinuses. Br J Neurosurg. 2021;35:306–12.
Chatzopoulos K, Treeck B van, Venable E, Serla V, Wirth T, Amirahmadi F, et al. Formalin pigment artifact deposition in autopsy tissue: predisposing factors, patterns of distribution and methods for removal. Forensic Sci Med Pathol. 2020;16:435–41.
Chen Z, Mu J, Chen X, Dong H. Sudden unexplained nocturnal death syndrome in Central China (Hubei): A 16-year retrospective study of autopsy cases. Medicine (Baltimore). 2016;95:1–6.
Cheshire EC, Biggs MJP, Hollingbury FE, Fitzpatrick-Swallow VL, Prickett TRA, Malcomson RDG. Frequency of macroscopic intradural hemorrhage with and without subdural hemorrhage in early childhood autopsies. Forensic Sci Med Pathol. 2019;15:184–90.
Chindemi C, Cirielli V, Cima L, Danzi O, Raniero D, Tagliaro F, et al. Autophagy pathways in drug abusers after forensic autopsy: LC3B, ph-mTOR and p70S6K analysis. Med Sci Law. 2019;59:49–56.
Chung U, Seo J-S, Kim Y-H, Hoon Son G, Hwang J-J. Quantitative analyses of postmortem heat shock protein mRNA profiles in the occipital lobes of human cerebral cortices: Implications in cause of death. Mol Cells. 2012;34:473–80.
Cirielli V, Cima L, Chindemi C, Danzi O, Ghimenton C, Eccher A, et al. Cortical expression of the polysialylated isoform of the neural cell adhesion molecule on brain tissue to recognize drug-related death. Am J Forensic Med Pathol. 2018;39:8–13.
Danusso R, Alfonsi G, Ferrero S, Lavezzi AM, Lattuada D. Mitochondrial DNA content: A new potential biomarker for sudden infant death syndrome. Pediatr Res. 2022;92:1282–1287.
Darke S, Duflou J, Forensic Pathologist C, Torok M, Officer R, Prolov T, et al. Toxicology, circumstances and pathology of deaths from acute alcohol toxicity. J Forensic Leg Med. 2013;20:1122–5.
Darke S, Lappin J, Kaye S, Duflou J. Clinical characteristics of fatal methamphetamine-related stroke: A national study. J Forensic Sci. 2018;63:735–9.
Davceva N, Janevska V, Ilievski B, Petrushevska G, Popeska Z. The occurrence of acute subdural haematoma and diffuse axonal injury as two typical acceleration injuries. J Forensic Leg Med. 2012;19:480–4.
Davceva N, Janevska V, Ilievski B, Spasevska J, Jovanovic R. The importance of the detail forensic-neuropathological examination in the determination of the diffuse brain injuries. Soud Lek. 2012;57:2–6.
CAS PubMed Google Scholar
del Bigio MR, Phillips SM. Retroocular and subdural hemorrhage or hemosiderin deposits in pediatric autopsies. J Neuropathol Exp Neurol. 2017;76:313–22.
Delteil C, Kolopp M, Capuani C, Humez S, Boucekine M, Leonetti G, et al. Histological dating of subarachnoid hemorrhage and retinal hemorrhage in infants. Forensic Sci Int. 2019;303:109952.
Delteil C, Humez S, Boucekine M, Jouvet A, Hedouin V, Fanton L, et al. Histological dating of subdural hematoma in infants. Int J Legal Med. 2019;133:539–46.
Du SH, Tan XH, Zhao R, Zhao D, Xue Y, Wang HJ, et al. Molecular pathology of cerebral TNF-α, IL-1β, iNOS and Nrf2 in forensic autopsy cases with special regard to deaths due to environmental hazards and intoxication. Forensic Sci Med Pathol. 2017;13:409–16.
Du Y, Xu J-T, Jin H-N, Zhao R, Zhao D, Du S-H, et al. Increased cerebral expressions of MMPs, CLDN5, OCLN, ZO1 and AQPs are associated with brain edema following fatal heat stroke. Sci Rep. 2017;7:1691.
Elliott JA, Vink R, Jensen L, Byard RW. Brain weight-body weight ratio in sudden infant death syndrome revisited. Med Sci Law. 2012;52:207–9.
Erbay L, Karhdag R, Oruc M, Cigremis Y, Celbis O. Association of BDNF/TRKB and NGF/TRKA levels in postmortem brain with major depression and suicide. Psychiatr Danub. 2021;33:491–8.
Esen Melez İ, Arslan M, Melez D, Şanli AN, Koç S. Sudden unexpected death in epilepsy: A retrospective autopsy study of 112 epileptic patients. Arch Neuropsychiatry. 2017;54:225–33.
Florou C, Zorilă A, Zorilă M, Marinescu M, Andrei C, Păvăloiu R, et al. Clinico-statistical and morphological aspects of severe traumatic brain injuries. Rom J Morphol Embryol. 2016;57:391–400.
Flugt A, Frost L, Søndergaard C, Milidou I. Lethal abusive head trauma in infancy in Denmark from 2000 to 2011. Dan Med J. 2021;68:AO8200604.
Google Scholar
Folkerth RD, Nunez J, Georgievskaya Z, McGuone D. Neuropathologic examination in sudden unexpected deaths in infancy and childhood: Recommendations for highest diagnostic yield and cost-effectiveness in forensic settings. Acad Forensic Pathol. 2017;7:182–99.
Funabashi KS, Barcelos D, Visoná I, e Silva SM, Almeida ML, e Sousa PO, et al. DNA extraction and molecular analysis of non-tumoral liver, spleen, and brain from autopsy samples: The effect of formalin fixation and paraffin embedding. Pathol Res Pract. 2012;208:584–91.
García Corredor N, Forero Porras P, Ballesteros Acuña L. Morphological evaluation of the distal medial striated artery. A study with cadaverous material. Colomb Med (Cali). 2020;51:e204440.
Gholamzadeh S, Zarenezhad M, Montazeri M, Zareikordshooli M, Sadeghi G, Malekpour A, et al. Statistical analysis of organ morphometric parameters and weights in South Iranian adult autopsies. Medicine (Baltimore). 2017;96:e6447.
Gielda L, Rigg S. Extraction of amplifiable DNA from embalmed human cadaver tissue. BMC Res Notes. 2017;10:737.
Girela-López E, Beltran-Aroca CM, Dye A, Gill JR. Epidemiology and autopsy findings of 500 drowning deaths. Forensic Sci Int. 2022;330:111137.
Hanson E, Ballantyne J. Human organ tissue identification by targeted RNA deep sequencing to aid the investigation of traumatic injury. Genes (Basel). 2017;8:319.
Haque MA, Khalil M, Khalil M, Sultana SZ, Mannan S, Rahman M, et al. Morphometry of Purkinje cell body of cerebellum in Bangladeshi cadaver. Mymensingh Med J Bangladesh. 2010;19:504–9.
CAS Google Scholar
Haque MA, Khalil M, Sultana SZ, Mannan S, Uddin MM, Hossain M, et al. Morphometric study of dentate nucleus of cerebellum in Bangladeshi cadaver. Mymensingh Med J Bangladesh. 2015;24:25–33.
Hashemi R, Mahmoodi R, Amirjamshidi A. Variations in the anatomy of the Willis’ circle: A 3-year cross-sectional study from Iran (2006–2009). Are the distributions of variations of circle of Willis different in different populations? Result of an anatomical study and review of literature. Surg Neurol Int. 2013;4:65.
Helm K, Matzenauer C, Neuhuber F, Monticelli F, Meyer H, Pittner S, et al. Suitability of specific soft tissue swabs for the forensic identification of highly decomposed bodies. Int J Legal Med. 2021;135:1319–27.
Hu Y, Tian L, Ma K, Han L, Li W, Hu L, et al. ER stress-related protein, CHOP, may serve as a biomarker of mechanical asphyxia: a primary study. Int J Legal Med. 2022;136:1091–104.
Ishikawa T, Yoshida C, Michiue T, Große Perdekamp M, Pollak S, Maeda H. Immunohistochemistry of catecholamines in the hypothalamic-pituitary-adrenal system with special regard to fatal hypothermia and hyperthermia. Leg Med (Tokyo). 2010;12:121–7.
Jack E, Haas E, Haddix TL. Evaluation of the presence and distribution of leptomeningeal inflammation in SIDS/SUDI cases and comparison with a hospital-based cohort. Childs Nerv Syst. 2019;35:2391–7.
Jack E, Fennelly NK, Haddix T. The inflammatory cellular constituents of foetal and infant leptomeninges: A survey of hospital-based autopsies without trauma. Childs Nerv Syst. 2014;30:911–7.
Johnson MM, David JA, Michelhaugh SK, Schmidt CJ, Bannon MJ. Increased heat shock protein 70 gene expression in the brains of cocaine-related fatalities may be reflective of postdrug survival and intervention rather than excited delirium. J Forensic Sci. 2012;57:1519–23.
Karayel F, Turan A, Sav A, Pakis I, Akyildiz E, Ersoy G. Methanol intoxication. Am J Forensic Med Pathol. 2010;31:34–6.
Article Google Scholar
Kibayashi K, Shimada R, Nakao KI, Ro A. Analysis of pituitary lesions in fatal closed head injury. Am J Forensic Med Pathol. 2012;33:206–10.
Kinney HC, Cryan JB, Haynes RL, Paterson DS, Haas EA, Othon, et al. Dentate gyrus abnormalities in sudden unexplained death in infants: Morphological marker of underlying brain vulnerability. Acta Neuropathol. 2015;129:65–80.
Kobek M, Jankowski Z, Szala J, Gąszczyk-Ozarowski Z, Pałasz A, Skowronek R. Time-related morphometric studies of neurofilaments in brain contusions. Folia Neuropathol. 2016;54:50–8.
Krohn M, Drebler J, Bauer M, Schober K, Franke H, Ondruschka B. Immunohistochemical investigation of S100 and NSE in cases of traumatic brain injury and its application for survival time determination. J Neurotrauma. 2015;32:430–40.
Krywanczyk A, Bundock EA. Quantifying macrophages and hemosiderin in pediatric dura mater. J Forensic Sci. 2018;63:902–5.
Krzyzanowska M, Steiner J, Karnecki K, Kaliszan M, Brisch R, Wiergowski M, et al. Decreased ribosomal DNA transcription in dorsal raphe nucleus neurons differentiates between suicidal and non-suicidal death. Eur Arch Psychiatry Clin Neurosci. 2016;266:217–24.
Kurtulus Dereli A, Demırci GN, Dodurga Y, Özbal S, Cankurt U, Boz B, et al. Evaluation of human pineal gland acetylserotonin O-methyltransferase immunoreactivity in suicide: A preliminary study. Med Sci Law. 2018;58:233–8.
Lech T, Sadlik J. Zinc in postmortem body tissues and fluids. Biol Trance Elem Res. 2011;142:11–7.
Article CAS Google Scholar
Leitner DF, McGuone D, William C, Faustin A, Askenazi M, Snuderl M, et al. Blinded review of hippocampal neuropathology in sudden unexplained death in childhood reveals inconsistent observations and similarities to explained paediatric deaths. Neuropathol Appl Neurobiol. 2022;e12746.
Lesnikova I, Schreckenbach MN, Kristensen MP, Papanikolaou LL, Hamilton-Dutoit S. Usability of immunohistochemistry in forensic samples with varying decomposition. Am J Forensic Med Pathol. 2018;39:185–91.
Liang Y, Tong F, Huang F, Liu Y, Zhu L, le Grange JM, et al. Pathological changes induced by phosphine poisoning: A study on 8 children. Int J Legal Med. 2020;134:217–28.
Lier J, Ondruschka B, Bechmann I, Dreßler J. Fast microglial activation after severe traumatic brain injuries. Int J Legal Med. 2020;134:2187–93.
Lindenbergh A, van den Berge M, Oostra R-J, Cleypool C, Bruggink A, Kloosterman A, et al. Development of a mRNA profiling multiplex for the inference of organ tissues. Int J Legal Med. 2013;127:891–900.
Lundesgaard Eidahl JM, Opdal SH, Rognum TO, Stray-Pedersen A. Postmortem evaluation of brain edema: An attempt with measurements of water content and brain-weight-to-inner-skull-circumference ratio. J Forensic Leg Med. 2019;64:1–6.
Matoba K, Hyodoh H, Murakami M, Matoba T, Saito A, Feng F, et al. Freezing preparation for macroscopic forensic investigation in putrefied brain. Leg Med (Tokyo). 2017;26:6–10.
Mehrpour O, Sheikhazadi A, Hasan Ghadyani M, Hooshyar H. Brain weight of Iranian population; The first report. J Forensic Leg Med. 2010;17:426–31.
Mohd Saman SA, Jothee S, Nor FM, Shafie MS. The pattern of injuries among motorcyclists in fatal road traffic accidents: An autopsy-based study. Am J Forensic Med Pathol. 2021;42:141–6.
Molina D, Vance K, Coleman M, Hargrove V. Testing an age-old adage: Can autopsy findings be of assistance in differentiating opioid versus cardiac deaths? J Forensic Sci. 2020;65:112–6.
Mori S, Takahashi S, Hayakawa A, Saito K, Takada A, Fukunaga T. Fatal intracranial aneurysms and dissections causing subarachnoid hemorrhage: An epidemiological and pathological analysis of 607 legal autopsy cases. J Stroke Cerebrovasc Dis. 2018;27:486–93.
Mubbunu L, Bowa K, Petrenko V, Silitongo M. Correlation of internal organ weights with body weight and body height in normal adult Zambians: A case study of Ndola Teaching Hospital. Anat Res Int. 2018;2018:4687538.
Naue J, Sänger T, Hoefsloot HCJ, Lutz-Bonengel S, Kloosterman AD, Verschure PJ. Proof of concept study of age-dependent DNA methylation markers across different tissues by massive parallel sequencing. Forensic Sci Int Genet. 2018;36:152–9.
Nishida N, Yoshida K, Hata Y, Arai Y, Kinoshita K. Pathological features of preclinical or early clinical stages of corticobasal degeneration: a comparison with advanced cases. Neuropathol Appl Neurobiol. 2015;41:893–905.
Nyasa C, Mwakikunga A, Tembo LH, Dzamalala C, Ihunwo AO. Anatomical variations and morphometric properties of the circulus arteriosus cerebri in a cadaveric Malawian population. Folia Morphol (Warsz). 2021;80:820–6.
Oerter S, Förster C, Bohnert M. Validation of sodium/glucose cotransporter proteins in human brain as a potential marker for temporal narrowing of the trauma formation. Int J Legal Med. 2019;133:1107–14.
Olczak M, Poniatowski Ł, Kwiatkowska M, Samojłowicz D, Tarka S, Wierzba-Bobrowicz T. Immunolocalization of dynein, dynactin, and kinesin in the cerebral tissue as a possible supplemental diagnostic tool for traumatic brain injury in postmortem examination. Folia Neuropathol. 2019;57:51–62.
Olczak M, Chutorański D, Kwiatkowska M, Samojłowicz D, Tarka S, Wierzba-Bobrowicz T. Bystin (BYSL) as a possible marker of severe hypoxic-ischemic changes in neuropathological examination of forensic cases. Forensic Sci Med Pathol. 2018;14:26–30.
Pelletier DE, Andrew TA. Common findings and predictive measures of opioid overdoses. Acad Forensic Pathol. 2017;7:91–8.
Pelletti G, Garagnani M, Barone R, Boscolo-Berto R, Rossi F, Morotti A, et al. Validation and preliminary application of a GC–MS method for the determination of putrescine and cadaverine in the human brain: a promising technique for PMI estimation. Forensic Sci Int. 2019;297:221–7.
Preusse-Prange A, Modrow J-H, Schwark T, von Wurmb-Schwark N. Detection of constitutive and inducible HSP70 proteins in formalin fixed human brain tissue. Forensic Sci Int. 2014;235:62–7.
Priemer DS, Folkerth RD. Dementia in the forensic setting: Diagnoses obtained using a condensed protocol at the Office of Chief Medical Examiner, New York City. J Neuropathol Exp Neurol. 2021;80:724–30.
Rao M, Singh D, Vashista R, Sharma S. Dating of acute and subacute subdural haemorrhage: A histo-pathological study. J Clin Diagn Res. 2016;10:HC01–7.
Rebollo-Soria MC, Arregui-Dalmases C, Sánchez-Molina D, Velázquez-Ameijide J, Galtés I. Injury pattern in lethal motorbikes-pedestrian collisions, in the area of Barcelona, Spain. J Forensic Leg Med. 2016;43:80–4.
Romero Tirado M, Pampin JMB, Gómez RG. Dating of traumatic brain injury in forensic cases using immunohistochemical markers (I): Neurofilaments and β-amyloid precursor protein. Am J Forensic Med Pathol. 2018;39:201–7.
Rungruangsak K, Poriswanish N. Pathology of fatal diffuse brain injury in severe non-penetrating head trauma. J Forensic Leg Med. 2021;82:102226.
Sadat-Shirazi MS, Soltani H, Nikpour N, Haghshenas M, Khalifeh S, Mokri A, et al. Alteration of orexin-A and PKCα in the postmortem brain of pure-opioid and multi-drug abusers. Neuropeptides. 2020;83:102074.
Sadat-Shirazi M-S, Zarrindast M-R, Ashabi G. Oxidative stress enzymes are changed in opioid abusers and multidrug abusers. J Clin Neurosci. 2020;72:365–8.
Sadat-Shirazi MS, Zarrindast MR, Daneshparvar H, Ziaie A, Fekri M, Abbasnezhad E, et al. Alteration of dopamine receptors subtypes in the brain of opioid abusers: A postmortem study in Iran. Neurosci Lett. 2018;687:169–76.
Sakai K, Fukuda T, Iwadate K. Immunohistochemical analysis of the ubiquitin proteasome system and autophagy lysosome system induced after traumatic intracranial injury: Association with time between the injury and death. Am J Forensic Med Pathol. 2014;35:38–44.
Samsuwan J, Muangsub T, Yanatatsaneejit P, Mutirangura A, Kitkumthorn N. Combined bisulfite restriction analysis for brain tissue identification. Forensic Sci Int. 2018;286:42–5.
Sauer E, Extra A, Caché P, Courts C. Identification of organ tissue types and skin from forensic samples by microRNA expression analysis. Forensic Sci Int Genet. 2017;28:99–110.
Schober K, Ondruschka B, Dreßler J, Abend M. Detection of hypoxia markers in the cerebellum after a traumatic frontal cortex injury: A human postmortem gene expression analysis. Int J Legal Med. 2015;129:701–7.
Shaha KK, Joe AE. Electrocution-related mortality: A retrospective review of 118 deaths in Coimbatore, India, between January 2002 and December 2006. Med Sci Law. 2010;50:72–4.
Sheikhazadi A, Shahabeddin Sadr S, Hasan Ghadyani M, Kazem Taheri S, Asghar Manouchehri A, Nazparvar B, et al. Study of the normal internal organ weights in Tehran’s population. J Forensic Leg Med. 2010;17:78–83.
Siddiqi H, Tahir M, Lone K. Variations in cerebral arterial circle of Willis in adult Pakistani population. J Coll Physicians Surg Pak. 2013;23:615–9.
Sultana N, Khalil M, Khan MK, Kabir A, Farjan S, Ismatsara M, et al. Variation in the position and diameter of basilar artery in different ages of Bangladeshi people. Mymensingh Med J. 2018;27:504–7.
Takayama M, Kashiwagi M, Matsusue A, Waters B, Hara K, Ikematsu N, et al. Quantification of immunohistochemical findings of neurofibrillary tangles and senile plaques for a diagnosis of dementia in forensic autopsy cases. Leg Med (Tokyo). 2016;22:82–9.
Takayama M, Kashiwagi M, Matsusue A, Waters B, Hara K, Ikematsu N, et al. Quantification of neuropathological findings by image data for the diagnosis of dementia in forensic autopsy cases. J Med Invest. 2016;63:114–8.
Tolescu S, Zorila M, Serbanescu M, Kamal K, Zorila G, Dumitru I, et al. Severe traumatic brain injury (TBI)-A seven-year comparative study in a Department of Forensic Medicine. Rom J Morphol Embryol. 2020;61:95–103.
Tong F, Wu R, Huang W, Yang Y, Zhang L, Zhang B, et al. Forensic aspects of homicides by insulin overdose. Forensic Sci Int. 2017;278:9–15.
Trautz F, Franke H, Bohnert S, Hammer N, Müller W, Stassart R, et al. Survival-time dependent increase in neuronal IL-6 and astroglial GFAP expression in fatally injured human brain tissue. Sci Rep. 2019;9:11771.
Trautz F, Dreßler J, Stassart R, Müller W, Ondruschka B. Proposals for best-quality immunohistochemical staining of paraffin-embedded brain tissue slides in forensics. Int J Legal Med. 2018;132:1103–9.
van den Berge M, Wiskerke D, Gerretsen R, Tabak J, Sijen T. DNA and RNA profiling of excavated human remains with varying postmortem intervals. Int J Legal Med. 2016;130:1471–80.
Vasović L, Trandafilović M, Jovanović I, Ugrenović S, Vlajković S. Vertebral and/or basilar dolichoectasia in human adult cadavers. Acta Neurochir. 2012;154:1477–88.
Wang Q, Ishikawa T, Michiue T, Zhu B-L, Guan D-W, Maeda H. Molecular pathology of brain matrix metalloproteases, claudin5, and aquaporins in forensic autopsy cases with special regard to methamphetamine intoxication. Int J Legal Med. 2014;128:469–74.
Wang Q, Ishikawa T, Michiue T, Zhu B-L, Guan D-W, Maeda H. Molecular pathology of brain edema after severe burns in forensic autopsy cases with special regard to the importance of reference gene selection. Int J Legal Med. 2013;127:881–9.
Wang Q, Ishikawa T, Michiue T, Zhu B-L, Guan D-W, Maeda H. Stability of endogenous reference genes in postmortem human brains for normalization of quantitative real-time PCR data: Comprehensive evaluation using geNorm, NormFinder, and BestKeeper. Int J Legal Med. 2012;126:943–52.
Wang Q, Ishikawa T, Michiue T, Zhu B-L, Guan D-W, Maeda H. Quantitative immunohistochemical analysis of human brain basic fibroblast growth factor, glial fibrillary acidic protein and single-stranded DNA expressions following traumatic brain injury. Forensic Sci Int. 2012;221:142–51.
Wang Q, Ishikawa T, Michiue T, Zhu B-L, Guan D-W, Maeda H. Evaluation of human brain damage in fatalities due to extreme environmental temperature by quantification of basic fibroblast growth factor (bFGF), glial fibrillary acidic protein (GFAP), S100b and single-stranded DNA (ssDNA) immunoreactivities. Forensic Sci Int. 2012;219:259–64.
Wong B, Ong BB, Milne N. The source of haemorrhage in traumatic basal subarachnoid haemorrhage. J Forensic Leg Med. 2015;29:18–23.
Yarid NA, Harruff RC. Globus pallidus necrosis unrelated to carbon monoxide poisoning: Retrospective analysis of 27 cases of basal ganglia necrosis. J Forensic Sci. 2015;60:1484–7.
Yoshida K, Hata Y, Ichimata S, Nishida N. Tau and amyloid-β pathology in Japanese forensic autopsy series under 40 years of age: Prevalence and association with APOE genotype and suicide risk. J Alzheimers Dis. 2019;72:641–52.
Yoshida K, Hata Y, Kinoshita K, Takashima S, Tanaka K, Nishida N. Incipient progressive supranuclear palsy is more common than expected and may comprise clinicopathological subtypes: A forensic autopsy series. Acta Neuropathol. 2017;133:809–23.
Yoshida C, Ishikawa T, Michiue T, Quan L, Maeda H. Postmortem biochemistry and immunohistochemistry of chromogranin A as a stress marker with special regard to fatal hypothermia and hyperthermia. Int J Legal Med. 2011;125:11–20.
Zedler B, Flaig B, Ackermann H, Parzeller M, Bratzke H. Brain weight in completed suicide and other cases of death-comparison of recent and previous studies. Int J Legal Med. 2014;128:295–301.
Zhang Z, Gong Q, Feng X, Zhang D, Quan L. Astrocytic clasmatodendrosis in the cerebral cortex of methamphetamine abusers. Forensic Sci Res. 2017;2:139–44.
Zhang H, Zhang P, Ma K, Lv Y, Li W, Luo C, et al. The selection of endogenous genes in human postmortem tissues. Sci Justice. 2013;53:115–20.
Zhuo L, Zhang Y, Zielke HR, Levine B, Zhang X, Chang L, et al. Sudden unexpected death in epilepsy: Evaluation of forensic autopsy cases. Forensic Sci Int. 2012;223:171–5.
Zorilă A, Zorilă M, Marinaş M, Ţolescu R, Zorilă G, Florou C, et al. Evaluation of brain injuries in children deceased due to head trauma. Rom J Morphol Embryol. 2017;58:1417–28.
Zwirner J, Scholze M, Neil Waddell J, Ondruschka B, Hammer N. Mechanical properties of human dura mater in tension-An analysis at an age range of 2 to 94 years. Sci Rep. 2019;9:16655.
Wade A. Fear or favour? Statistics in pathology. J Clin Pathol. 2000;53:16–8.
Grimes DA, Schulz KF. Compared to what? Finding controls for case-control studies. Lancet. 2005;365:1429–33.
Büttner A. Review: The neuropathology of drug abuse. Neuropathol Appl Neurobiol. 2011;37:118–34.
An JH, Lee KE, Jeon HJ, Son SJ, Kim SY, Hong JP. Risk of suicide and accidental deaths among elderly patients with cognitive impairment. Alzheimers Res Ther. 2019;11:32.
Byard RW, Austin A. The role of forensic pathology in suicide. Forensic Sci Med Pathol. 2010;7:1–2.
Download references
Open Access funding provided by University of Helsinki including Helsinki University Central Hospital.
Author information
Authors and affiliations.
Department of Forensic Medicine, Faculty of Medicine, University of Helsinki, P.O. Box 21, Helsinki, FI-00014, Finland
Petteri Oura, Antti Hakkarainen & Antti Sajantila
Forensic Medicine Unit, Finnish Institute for Health and Welfare, P.O. Box 30, Helsinki, FI-00271, Finland
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization and methodology: PO and AS. Formal analysis and investigation: PO and AS. Writing—original draft preparation: PO, AH, and AS. Writing—review and editing: PO, AH, and AS. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Petteri Oura .
Ethics declarations
Ethics approval, consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (PDF 396 KB)
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Oura, P., Hakkarainen, A. & Sajantila, A. Forensic neuropathology in the past decade: a scoping literature review. Forensic Sci Med Pathol (2023). https://doi.org/10.1007/s12024-023-00672-9
Download citation
Accepted : 22 June 2023
Published : 13 July 2023
DOI : https://doi.org/10.1007/s12024-023-00672-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Neuropathology
- Meta-level attribute
- Research theme
- Methodology
- Medico-legal
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 23 August 2022
Prognostic risk factors for moderate-to-severe exacerbations in patients with chronic obstructive pulmonary disease: a systematic literature review
- John R. Hurst 1 ,
- MeiLan K. Han 2 ,
- Barinder Singh 3 ,
- Sakshi Sharma 4 ,
- Gagandeep Kaur 3 ,
- Enrico de Nigris 5 ,
- Ulf Holmgren 6 &
- Mohd Kashif Siddiqui 3
Respiratory Research volume 23 , Article number: 213 ( 2022 ) Cite this article
6408 Accesses
20 Citations
42 Altmetric
Metrics details
Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity and mortality worldwide. COPD exacerbations are associated with a worsening of lung function, increased disease burden, and mortality, and, therefore, preventing their occurrence is an important goal of COPD management. This review was conducted to identify the evidence base regarding risk factors and predictors of moderate-to-severe exacerbations in patients with COPD.
A literature review was performed in Embase, MEDLINE, MEDLINE In-Process, and the Cochrane Central Register of Controlled Trials (CENTRAL). Searches were conducted from January 2015 to July 2019. Eligible publications were peer-reviewed journal articles, published in English, that reported risk factors or predictors for the occurrence of moderate-to-severe exacerbations in adults age ≥ 40 years with a diagnosis of COPD.
The literature review identified 5112 references, of which 113 publications (reporting results for 76 studies) met the eligibility criteria and were included in the review. Among the 76 studies included, 61 were observational and 15 were randomized controlled clinical trials. Exacerbation history was the strongest predictor of future exacerbations, with 34 studies reporting a significant association between history of exacerbations and risk of future moderate or severe exacerbations. Other significant risk factors identified in multiple studies included disease severity or bronchodilator reversibility (39 studies), comorbidities (34 studies), higher symptom burden (17 studies), and higher blood eosinophil count (16 studies).
Conclusions
This systematic literature review identified several demographic and clinical characteristics that predict the future risk of COPD exacerbations. Prior exacerbation history was confirmed as the most important predictor of future exacerbations. These prognostic factors may help clinicians identify patients at high risk of exacerbations, which are a major driver of the global burden of COPD, including morbidity and mortality.
Chronic obstructive pulmonary disease (COPD) is the third leading cause of death worldwide [ 1 ]. Based upon disability-adjusted life-years, COPD ranked sixth out of 369 causes of global disease burden in 2019 [ 2 ]. COPD exacerbations are associated with a worsening of lung function, and increased disease burden and mortality (of those patients hospitalized for the first time with an exacerbation, > 20% die within 1 year of being discharged) [ 3 ]. Furthermore, patients with COPD consider exacerbations or hospitalization due to exacerbations to be the most important disease outcome, having a large impact on their lives [ 4 ]. Therefore, reducing the future risk of COPD exacerbations is a key goal of COPD management [ 5 ].
Being able to predict the level of risk for each patient allows clinicians to adapt treatment and patients to adjust their lifestyle (e.g., through a smoking cessation program) to prevent exacerbations [ 3 ]. As such, identifying high-risk patients using measurable risk factors and predictors that correlate with exacerbations is critical to reduce the burden of disease and prevent a cycle of decline encompassing irreversible lung damage, worsening quality of life (QoL), increasing disease burden, high healthcare costs, and early death.
Prior history of exacerbations is generally thought to be the best predictor of future exacerbations; however, there is a growing body of evidence suggesting other demographic and clinical characteristics, including symptom burden, airflow obstruction, comorbidities, and inflammatory biomarkers, also influence risk [ 6 , 7 , 8 , 9 ]. For example, in the prospective ECLIPSE observational study, the likelihood of patients experiencing an exacerbation within 1 year of follow-up increased significantly depending upon several factors, including prior exacerbation history, forced expiratory volume in 1 s (FEV 1 ), St. George’s Respiratory Questionnaire (SGRQ) score, gastroesophageal reflux, and white blood cell count [ 9 ].
Many studies have assessed predictors of COPD exacerbations across a variety of countries and patient populations. This systematic literature review (SLR) was conducted to identify and compile the evidence base regarding risk factors and predictors of moderate-to-severe exacerbations in patients with COPD.
- Systematic literature review
A comprehensive search strategy was designed to identify English-language studies published in peer-reviewed journals providing data on risk factors or predictors of moderate or severe exacerbations in adults aged ≥ 40 years with a diagnosis of COPD (sample size ≥ 100). The protocol is summarized in Table 1 and the search strategy is listed in Additional file 1 : Table S1. Key biomedical electronic literature databases were searched from January 2015 until July 2019. Other sources were identified via bibliographic searching of relevant systematic reviews.
Study selection process
Implementation and reporting followed the recommendations and standards of the Preferred Reporting Items for Systematic reviews and Meta-analyses (PRISMA) statement [ 10 ]. An independent reviewer conducted the first screening based on titles and abstracts, and a second reviewer performed a quality check of the excluded evidence. A single independent reviewer also conducted the second screening based on full-text articles, with a quality check of excluded evidence performed by a second reviewer. Likewise, data tables of the included studies were generated by one reviewer, and another reviewer performed a quality check of extracted data. Where more than one publication was identified describing a single study or trial, data were compiled into a single entry in the data-extraction table to avoid double counting of patients and studies. One publication was designated as the ‘primary publication’ for the purposes of the SLR, based on the following criteria: most recently published evidence and/or the article that presented the majority of data (e.g., journal articles were preferred over conference abstracts; articles that reported results for the full population were preferred over later articles providing results of subpopulations). Other publications reporting results from the same study were designated as ‘linked publications’; any additional data in the linked publications that were not included in the primary publication were captured in the SLR. Conference abstracts were excluded from the SLR unless they were a ‘linked publication.’
Included studies
A total of 5112 references (Fig. 1 ) were identified from the database searches. In total, 76 studies from 113 publications were included in the review. Primary publications and ‘linked publications’ for each study are detailed in Additional file 1 : Table S2, and study characteristics are shown in Additional file 1 : Table S3. The studies included clinical trials, registry studies, cross-sectional studies, cohort studies, database studies, and case–control studies. All 76 included studies were published in peer-reviewed journals. Regarding study design, 61 of the studies were observational (34 retrospective observational studies, 19 prospective observational studies, four cross-sectional studies, two studies with both retrospective and prospective cohort data, one case–control study, and one with cross-sectional and longitudinal data) and 15 were randomized controlled clinical trials.
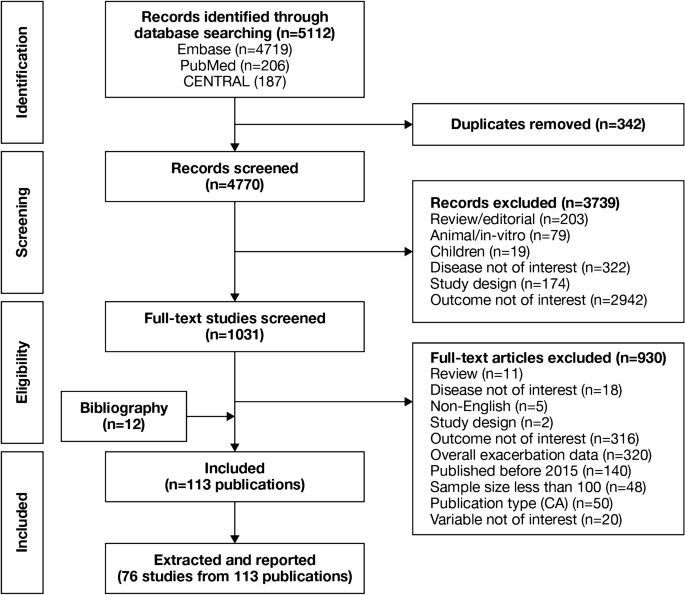
PRISMA flow diagram of studies through the systematic review process. CA conference abstract, CENTRAL Cochrane Central Register of Controlled Trials, PRISMA Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Of the 76 studies, 16 were conducted in North America (13 studies in the USA, two in Canada, and one in Mexico); 26 were conducted in Europe (seven studies in Spain, four in the UK, three in Denmark, two studies each in Bulgaria, the Netherlands, and Switzerland, and one study each in Sweden, Serbia, Portugal, Greece, Germany, and France) and 17 were conducted in Asia (six studies in South Korea, four in China, three in Taiwan, two in Japan, and one study each in Singapore and Israel). One study each was conducted in Turkey and Australia. Fifteen studies were conducted across multiple countries.
The majority of the studies (n = 54) were conducted in a multicenter setting, while 22 studies were conducted in a single-center setting. The sample size among the included studies varied from 118 to 339,389 patients.
Patient characteristics
A total of 75 studies reported patient characteristics (Additional file 1 : Table S4). The mean age was reported in 65 studies and ranged from 58.0 to 75.2 years. The proportion of male patients ranged from 39.7 to 97.6%. The majority of included studies (85.3%) had a higher proportion of males than females.
Exacerbation history (as defined per each study) was reported in 18 of 76 included studies. The proportion of patients with no prior exacerbation was reported in ten studies (range, 0.1–79.5% of patients), one or fewer prior exacerbation in ten studies (range, 46–100%), one or more prior exacerbation in eight studies (range, 18.4–100%), and two or more prior exacerbations in 12 studies (range, 6.1–55.0%).
Prognostic factors of exacerbations
A summary of the risk factors and predictors reported across the included studies is provided in Tables 2 and 3 . The overall findings of the SLR are summarized in Figs. 2 and 3 .
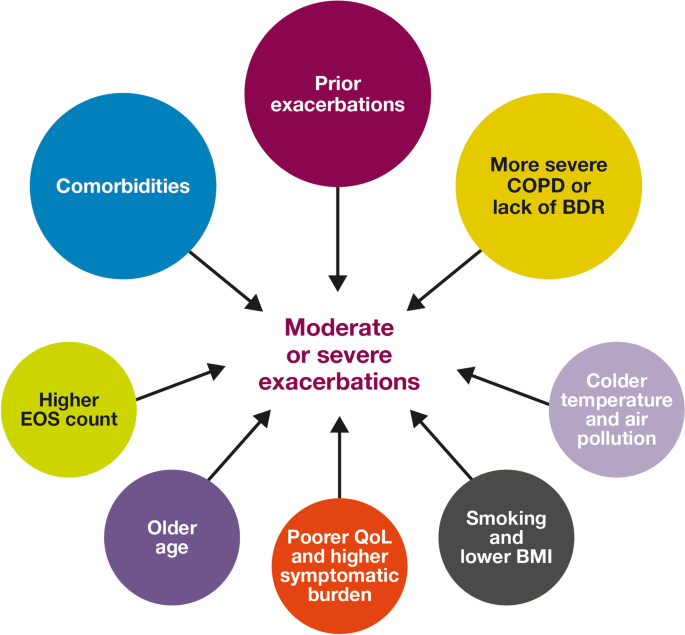
Risk factors for moderate-to-severe exacerbations in patients with COPD. Factors with > 30 supporting studies shown as large circles; factors with ≤ 30 supporting studies shown as small circles and should be interpreted cautiously. BDR bronchodilator reversibility, BMI body mass index, COPD chronic obstructive pulmonary disease, EOS eosinophil, QoL quality of life
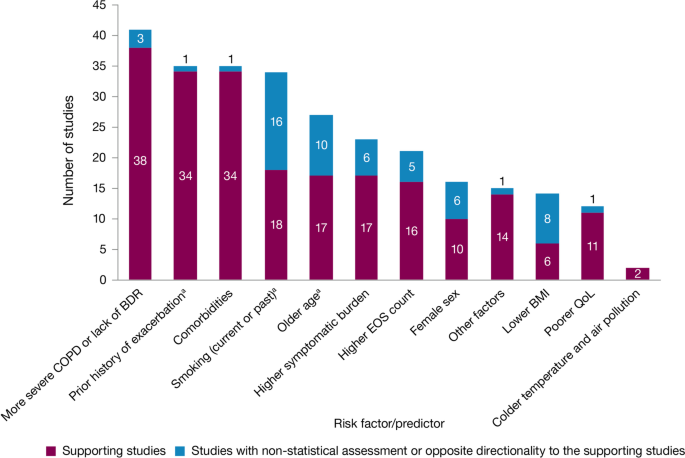
Summary of risk factors for exacerbation events. a Treatment impact studies removed. BDR bronchodilator reversibility, BMI body mass index, COPD chronic obstructive pulmonary disease, EOS eosinophil, QoL quality of life
Exacerbation history within the past 12 months was the strongest predictor of future exacerbations. Across the studies assessing this predictor, 34 out of 35 studies (97.1%) reported a significant association between history of exacerbations and risk of future moderate-to-severe exacerbations (Table 3 ). Specifically, two or more exacerbations in the previous year or at least one hospitalization for COPD in the previous year were identified as reliable predictors of future moderate or severe exacerbations. Even one moderate exacerbation increased the risk of a future exacerbation, with the risk increasing further with each subsequent exacerbation (Fig. 4 ). A severe exacerbation was also found to increase the risk of subsequent exacerbation and hospitalization (Fig. 5 ). Patients experiencing one or more severe exacerbations were more likely to experience further severe exacerbations than moderate exacerbations [ 11 , 12 ]. In contrast, patients with a history of one or more moderate exacerbations were more likely to experience further moderate exacerbations than severe exacerbations [ 11 , 12 ].
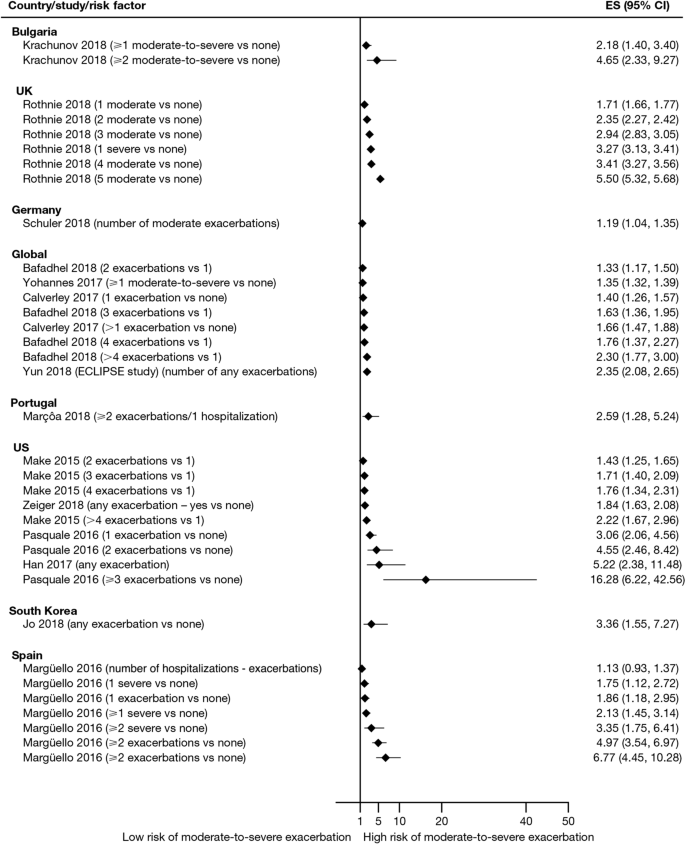
Exacerbation history as a risk factor for moderate-to-severe exacerbations. Yun 2018 included two studies; the study from which data were extracted (COPDGene or ECLIPSE) is listed in parentheses. CI confidence interval, ES effect size
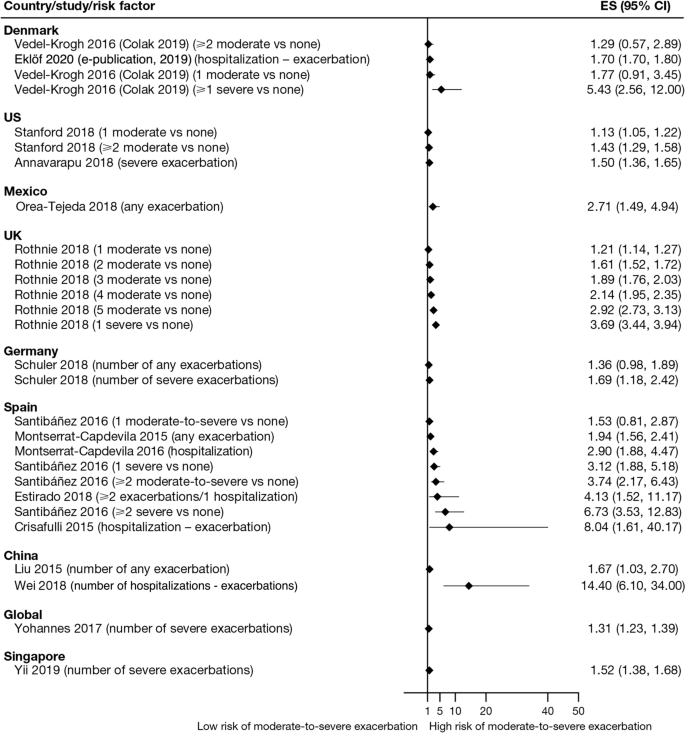
Exacerbation history as a risk factor for severe exacerbations. Where data have been extracted from a linked publication rather than the primary publication, the linked publication is listed in parentheses. CI confidence interval, ES , effect size
Overall, 35 studies assessed the association of comorbidities with the risk of exacerbation. All studies except one (97.1%) reported a positive association between comorbidities and the occurrence of moderate-to-severe exacerbations (Table 3 ). In addition to the presence of any comorbidity, specific comorbidities that were found to significantly increase the risk of moderate-to-severe exacerbations included anxiety and depression, cardiovascular comorbidities, gastroesophageal reflux disease/dyspepsia, and respiratory comorbidities (Fig. 6 ). Comorbidities that were significant risk factors for severe exacerbations included cardiovascular, musculoskeletal, and respiratory comorbidities, diabetes, and malignancy (Fig. 7 ). Overall, the strongest association between comorbidities and COPD readmissions in the emergency department was with cardiovascular disease. The degree of risk for both moderate-to-severe and severe exacerbations also increased with the number of comorbidities. A Dutch cohort study found that 88% of patients with COPD had at least one comorbidity, with hypertension (35%) and coronary heart disease (19%) being the most prevalent. In this cohort, the comorbidities with the greatest risk of frequent exacerbations were pulmonary cancer (odds ratio [OR] 1.85) and heart failure (OR 1.72) [ 7 ].
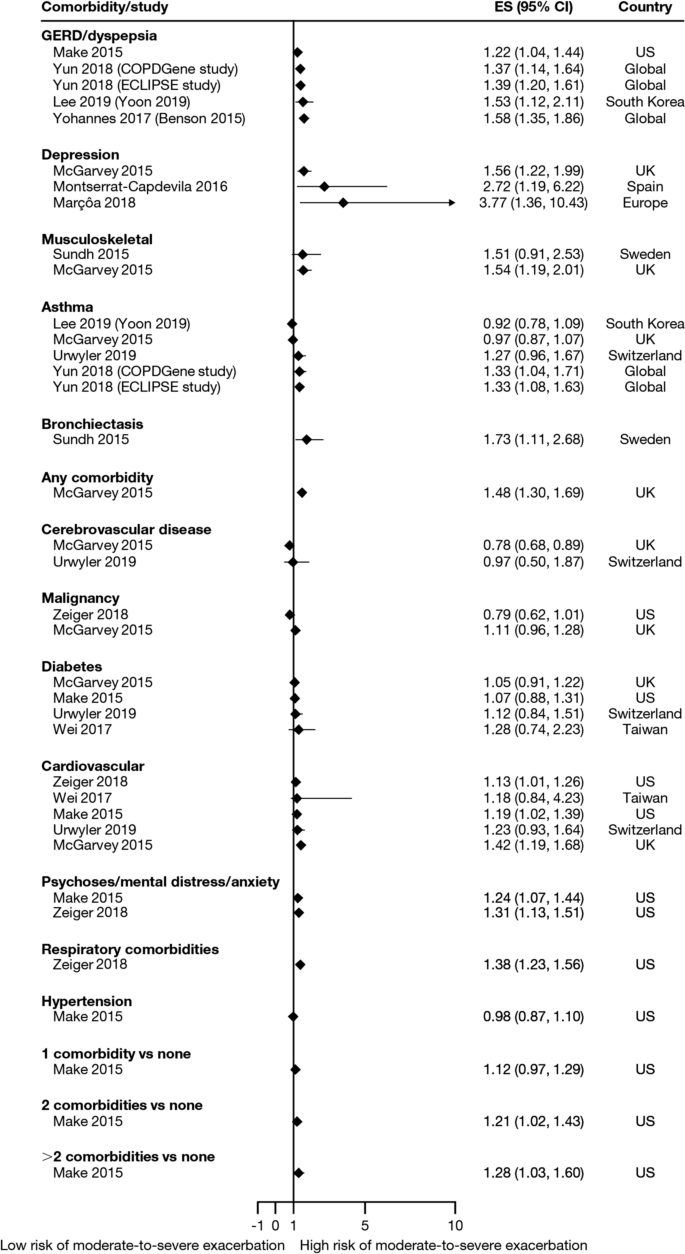
Comorbidities as risk factors for moderate-to-severe exacerbations. Yun 2018 included two studies; the study from which data were extracted (COPDGene or ECLIPSE) is listed in parentheses. Where data have been extracted from a linked publication rather than the primary publication, the linked publication is listed in parentheses. CI confidence interval, ES effect size, GERD gastroesophageal disease
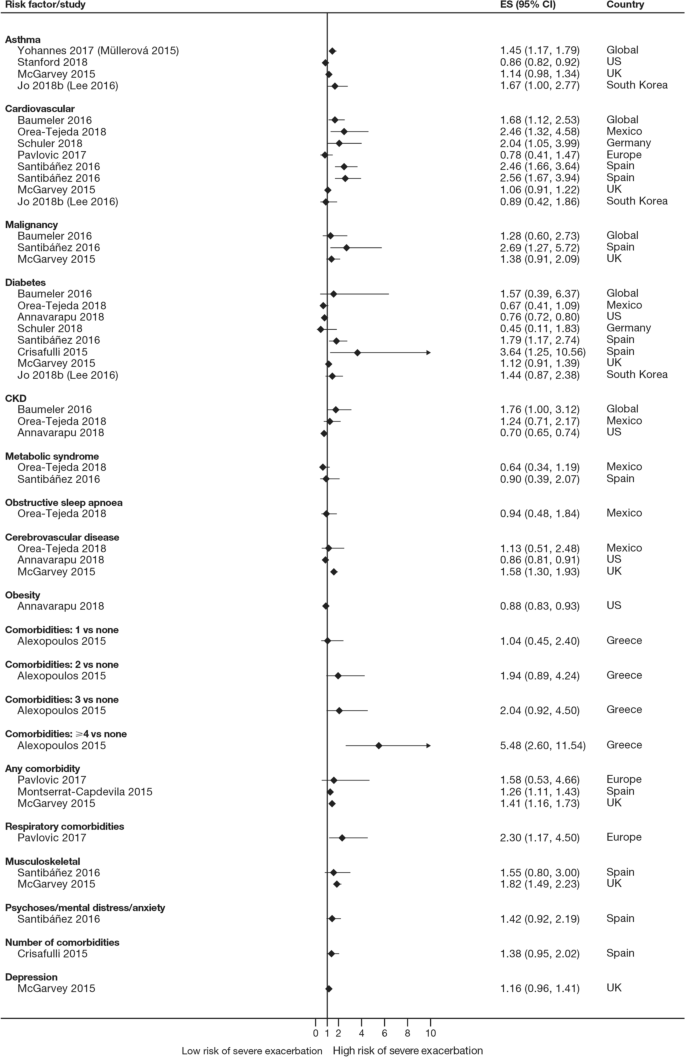
Comorbidities as risk factors for severe exacerbations. Where data have been extracted from a linked publication rather than the primary publication, the linked publication is listed in parentheses. CI confidence interval, CKD , chronic kidney disease, ES effect size
The majority of studies assessing disease severity or bronchodilator reversibility (39/41; 95.1%) indicated a significant positive relation between risk of future exacerbations and greater disease severity, as assessed by greater lung function impairment (in terms of lower FEV 1 , FEV 1 /forced vital capacity ratio, or forced expiratory flow [25–75]/forced vital capacity ratio) or more severe Global Initiative for Chronic Obstructive Lung Disease (GOLD) class A − D, and a positive relationship between risk of future exacerbations and lack of bronchodilator reversibility (Table 3 , Figs. 8 and 9 ).
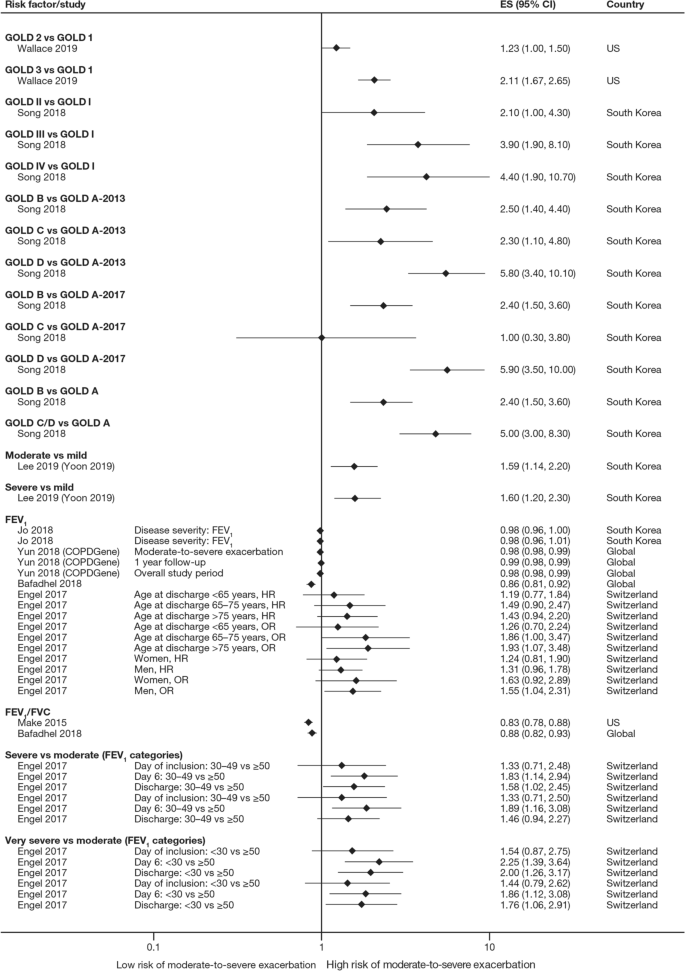
Disease severity as a risk factor for moderate-to-severe exacerbations. Yun 2018 included two studies; the study from which data were extracted (COPDGene or ECLIPSE) is listed in parentheses. Where data have been extracted from a linked publication rather than the primary publication, the linked publication is listed in parentheses. CI confidence interval, ES effect size, FEV 1 f orced expiratory volume in 1 s, FVC , forced vital capacity, GOLD Global Initiative for Obstructive Lung Disease, HR hazard ratio, OR odds ratio
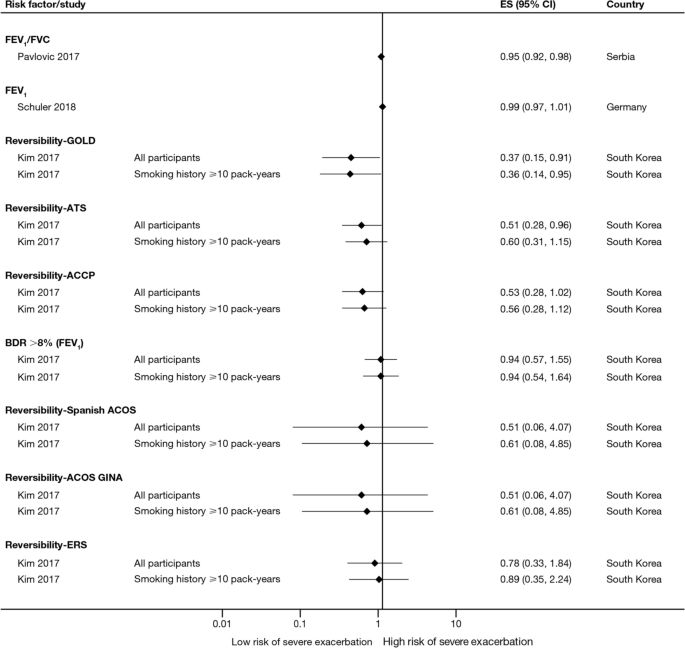
Disease severity and BDR as risk factors for severe exacerbations. ACCP American College of Chest Physicians, ACOS Asthma-COPD overlap syndrome, ATS American Thoracic Society, BDR bronchodilator reversibility, CI confidence interval, ERS European Respiratory Society, ES effect size, FEV 1 forced expiratory volume in 1 s, FVC forced vital capacity, GINA Global Initiative for Asthma, GOLD Global Initiative for Obstructive Lung Disease
Of 21 studies assessing the relationship between blood eosinophil count and exacerbations (Table 3 ), 16 reported estimates for the risk of moderate or severe exacerbations by eosinophil count. A positive association was observed between higher eosinophil count and a higher risk of moderate or severe exacerbations, particularly in patients not treated with an inhaled corticosteroid (ICS); however, five studies reported a significant positive association irrespective of intervention effects. The risk of moderate-to-severe exacerbations was observed to be positively associated with various definitions of higher eosinophil levels (absolute counts: ≥ 200, ≥ 300, ≥ 340, ≥ 400, and ≥ 500 cells/mm 3 ; % of blood eosinophil count: ≥ 2%, ≥ 3%, ≥ 4%, and ≥ 5%). Of note, one study found reduced efficacy of ICS in lowering moderate-to-severe exacerbation rates for current smokers versus former smokers at all eosinophil levels [ 13 ].
Of 12 studies assessing QoL scales, 11 (91.7%) studies reported a significant association between the worsening of QoL scores and the risk of future exacerbations (Table 3 ). Baseline SGRQ [ 14 , 15 ], Center for Epidemiologic Studies Depression Scale (for which increased scores may indicate impaired QoL) [ 16 ], and Clinical COPD Questionnaire [ 17 , 18 ] scores were found to be associated with future risk of moderate and/or severe COPD exacerbations. For symptom scores, six out of eight studies assessing the association between moderate-to-severe or severe exacerbations with COPD Assessment Test (CAT) scores reported a significant and positive relationship. Furthermore, the risk of moderate-to-severe exacerbations was found to be significantly higher in patients with higher CAT scores (≥ 10) [ 15 , 19 , 20 , 21 ], with one study demonstrating that a CAT score of 15 increased predictive ability for exacerbations compared with a score of 10 or more [ 18 ]. Among 15 studies that assessed the association of modified Medical Research Council (mMRC) scores with the risk of moderate-to-severe or severe exacerbation, 11 found that the risk of moderate-to-severe or severe exacerbations was significantly associated with higher mMRC scores (≥ 2) versus lower scores. Furthermore, morning and night symptoms (measured by Clinical COPD Questionnaire) were associated with poor health status and predicted future exacerbations [ 17 ].
Of 36 studies reporting the relationship between smoking status and moderate-to-severe or severe exacerbations, 22 studies (61.1%) reported a significant positive association (Table 3 ). Passive smoking was also significantly associated with an increased risk of severe exacerbations (OR 1.49) [ 20 ]. Of note, three studies reported a significantly lower rate of moderate-to-severe exacerbations in current smokers compared with former smokers [ 22 , 23 , 24 ].
A total of 14 studies assessed the association of body mass index (BMI) with the occurrence of frequent moderate-to-severe exacerbations in patients with COPD. Six out of 14 studies (42.9%) reported a significant negative association between exacerbations and BMI (Table 3 ). The risk of moderate and/or severe COPD exacerbations was highest among underweight patients compared with normal and overweight patients [ 23 , 25 , 26 , 27 , 28 ].
In the 29 studies reporting an association between age and moderate or severe exacerbations, more than half found an association of older age with an increased risk of moderate-to-severe exacerbations (58.6%; Table 3 ). Four of these studies noted a significant increase in the risk of moderate-to-severe or severe exacerbations for every 10-year increase in age [ 25 , 26 , 29 , 30 ]. However, 12 studies reported no significant association between age and moderate-to-severe or severe exacerbation risk.
Sixteen out of 33 studies investigating the impact of sex on exacerbation risk found a significant association (48.5%; Table 3 ). Among these, ten studies reported that female sex was associated with an increased risk of moderate-to-severe exacerbations, while six studies showed a higher exacerbation risk in males compared with females. There was some variation in findings by geographic location and exacerbation severity (Additional file 2 : Figs. S1 and S2). Notably, when assessing the risk of severe exacerbations, more studies found an association with male sex compared with female sex (6/13 studies vs 1/13 studies, respectively).
Both studies evaluating associations between exacerbations and environmental factors reported that colder temperature and exposure to major air pollution (NO 2 , O 3 , CO, and/or particulate matter ≤ 10 μm in diameter) increased hospital admissions due to severe exacerbations and moderate-to-severe exacerbation rates [ 31 , 32 ].
Four studies assessed the association of 6-min walk distance with the occurrence of frequent moderate-to-severe exacerbations (Table 3 ). One study (25.0%) found that shorter 6-min walk distance (representing low physical activity) was significantly associated with a shortened time to severe exacerbation, but the effect size was small (hazard ratio 0.99) [ 33 ].
Five out of six studies assessing the relationship between race or ethnicity and exacerbation risk reported significant associations (Table 3 ). Additionally, one study reported an association between geographic location in the US and exacerbations, with living in the Northeast region being the strongest predictor of severe COPD exacerbations versus living in the Midwest and South regions [ 34 ].
Overall, seven studies assessed the association of biomarkers with risk of future exacerbations (Table 3 ), with the majority identifying significant associations between inflammatory biomarkers and increased exacerbation risk, including higher C-reactive protein levels [ 8 , 35 ], fibrinogen levels [ 8 , 30 ], and white blood cell count [ 8 , 15 , 16 ].
This SLR has identified several demographic and clinical characteristics that predict the future risk of COPD exacerbations. Key factors associated with an increased risk of future moderate-to-severe exacerbations included a history of prior exacerbations, worse disease severity and bronchodilator reversibility, the presence of comorbidities, a higher eosinophil count, and older age (Fig. 2 ). These prognostic factors may help clinicians identify patients at high risk of exacerbations, which are a major driver of the burden of COPD, including morbidity and mortality [ 36 ].
Findings from this review summarize the existing evidence, validating the previously published literature [ 6 , 9 , 23 ] and suggesting that the best predictor of future exacerbations is a history of exacerbations in the prior year [ 8 , 11 , 12 , 13 , 14 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 26 , 29 , 34 , 35 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 ]. In addition, the effect size generally increased with the number of prior exacerbations, with a stronger effect observed with prior severe versus moderate exacerbations. This effect was observed across regions, including in Europe and North America, and in several global studies. This relationship represents a vicious circle, whereby one exacerbation predisposes a patient to experience future exacerbations and leading to an ever-increasing disease burden, and emphasizes the importance of preventing the first exacerbation event through early, proactive exacerbation prevention. The finding that prior exacerbations tended to be associated with future exacerbations of the same severity suggests that the severity of the underlying disease may influence exacerbation severity. However, the validity of the traditional classification of exacerbation severity has recently been challenged [ 61 ], and further work is required to understand relationships with objective assessments of exacerbation severity.
In addition to exacerbation history, disease severity and bronchodilator reversibility were also strong predictors for future exacerbations [ 8 , 14 , 16 , 18 , 19 , 20 , 22 , 23 , 24 , 26 , 28 , 29 , 33 , 37 , 40 , 43 , 44 , 45 , 46 , 48 , 50 , 51 , 52 , 56 , 59 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 ]. The association with disease severity was noted in studies that used GOLD disease stages 1–4 and those that used FEV 1 percent predicted and other lung function assessments as continuous variables. Again, this risk factor is self-perpetuating, as evidence shows that even a single moderate or severe exacerbation may almost double the rate of lung function decline [ 79 ]. Accordingly, disease severity and exacerbation history may be correlated. Margüello et al. concluded that the severity of COPD could be associated with a higher risk of exacerbations, but this effect was partly determined by the exacerbations suffered in the previous year [ 23 ]. It should be noted that FEV 1 is not recommended by GOLD for use as a predictor of exacerbation risk or mortality alone due to insufficient precision when used at the individual patient level [ 5 ].
Another factor that should be considered when assessing individual exacerbation risk is the presence of comorbidities [ 7 , 14 , 16 , 18 , 19 , 20 , 21 , 22 , 24 , 25 , 26 , 27 , 28 , 30 , 33 , 34 , 35 , 40 , 41 , 44 , 45 , 46 , 47 , 48 , 51 , 52 , 53 , 54 , 56 , 58 , 59 , 63 , 64 , 73 , 74 , 76 , 77 , 80 , 81 , 82 , 83 , 84 , 85 ]. Comorbidities are common in COPD, in part due to common risk factors (e.g., age, smoking, lifestyle factors) that also increase the risk of other chronic diseases [ 7 ]. Significant associations were observed between exacerbation risk and comorbidities, such as anxiety and depression, cardiovascular disease, diabetes, and respiratory comorbidities. As with prior exacerbations, the strength of the association increased with the number of comorbidities. Some comorbidities that were found to be associated with COPD exacerbations share a common biological mechanism of systemic inflammation, such as cardiovascular disease, diabetes, and depression [ 86 ]. Furthermore, other respiratory comorbidities, including asthma and bronchiectasis, involve inflammation of the airways [ 87 ]. In these patients, optimal management of comorbidities may reduce the risk of future COPD exacerbations (and improve QoL), although further research is needed to confirm the efficacy of this approach to exacerbation prevention. As cardiovascular conditions, including hypertension and coronary heart disease, are the most common comorbidities in people with COPD [ 7 ], reducing cardiovascular risk may be a key goal in reducing the occurrence of exacerbations. For other comorbidities, the mechanism for the association with exacerbation risk may be related to non-biological factors. For example, in depression, it has been suggested that the mechanism may relate to greater sensitivity to symptom changes or more frequent physician visits [ 88 ].
There is now a growing body of evidence reporting the relationship between blood eosinophil count and exacerbation risk [ 8 , 13 , 14 , 20 , 37 , 48 , 52 , 56 , 59 , 60 , 62 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 ]. Data from many large clinical trials (SUNSET [ 89 ], FLAME [ 96 ], WISDOM [ 98 ], IMPACT [ 13 ], TRISTAN [ 99 ], INSPIRE [ 99 ], KRONOS [ 91 ], TRIBUTE [ 48 ], TRILOGY [ 52 ], TRINITY [ 56 ]) have also shown relationships between treatment, eosinophil count, and exacerbation rates. Evidence shows that eosinophil count, along with other effect modifiers (e.g., exacerbation history), can be used to predict reductions in exacerbations with ICS treatment. Identifying patients most likely to respond to ICS should contribute to personalized medicine approaches to treat COPD. One challenge in drawing a strong conclusion from eosinophil counts is the choice of a cut-off value, with a variety of absolute and percentage values observed to be positively associated with the risk of moderate-to-severe exacerbations. The use of absolute counts may be more practical, as these are not affected by variations in other immune cell numbers; however, there is a lack of consensus on this point [ 100 ].
Across the studies examined, associations between sex and the risk of moderate and/or severe exacerbations were variable [ 14 , 16 , 18 , 20 , 21 , 22 , 23 , 24 , 26 , 27 , 28 , 29 , 37 , 40 , 42 , 44 , 45 , 46 , 47 , 48 , 51 , 52 , 56 , 58 , 59 , 63 , 73 , 74 , 77 , 80 , 83 , 84 , 85 ]. A greater number of studies showed an increased risk of exacerbations in females compared with males. In contrast, some studies failed to detect a relationship, suggesting that country-specific or cultural factors may play a role. A majority of the included studies evaluated more male patients than female patients; to further elucidate the relationship between sex and exacerbations, more studies in female patients are warranted. Over half of the studies that assessed the relationship between age and exacerbation risk found an association between increasing age and increasing risk of moderate-to-severe COPD exacerbations [ 14 , 16 , 18 , 20 , 21 , 22 , 23 , 24 , 26 , 27 , 28 , 29 , 33 , 40 , 42 , 44 , 45 , 47 , 51 , 52 , 54 , 56 , 63 , 73 , 74 , 77 , 80 , 83 , 85 ].
Our findings also suggested that patients with low BMI have greater risk of moderate and/or severe exacerbations. The mechanism underlying this increased risk in underweight patients is poorly understood; however, loss of lean body mass in patients with COPD may be related to ongoing systemic inflammation that impacts skeletal muscle mass [ 101 , 102 , 103 ].
A limitation of this SLR, that may have resulted in some studies with valid results being missed, was the exclusion of non-English-language studies and the limitation by date; however, the search strategy was otherwise broad, resulting in the review of a large number of studies. The majority of studies captured in this SLR were from Europe, North America, and Asia. The findings may therefore be less generalizable to patients in other regions, such as Africa or South America. Given that one study reported an association between geographic location within different regions of the US and exacerbations [ 34 ], it is plausible that risk of exacerbations may be impacted by global location. As no formal meta-analysis was planned, the assessments are based on a qualitative synthesis of studies. A majority of the included studies looked at exposures of certain factors (e.g., history of exacerbations) at baseline; however, some of these factors change over time, calling into question whether a more sophisticated statistical analysis should have been conducted in some cases to consider time-varying covariates. Our results can only inform on associations, not causation, and there are likely bidirectional relationships between many factors and exacerbation risk (e.g., health status). Finally, while our review of the literature captured a large number of prognostic factors, other variables such as genetic factors, lung microbiome composition, and changes in therapy over time have not been widely studied to date, but might also influence exacerbation frequency [ 104 ]. Further research is needed to assess the contribution of these factors to exacerbation risk.
This SLR captured publications up to July 2019. However, further studies have since been published that further support the prognostic factors identified here. For example, recent studies have reported an increased risk of exacerbations in patients with a history of exacerbations [ 105 ], comorbidities [ 106 ], poorer lung function (GOLD stage) [ 105 ], higher symptomatic burden [ 107 ], female sex [ 105 ], and lower BMI [ 106 , 108 ].
In summary, the literature assessing risk factors for moderate-to-severe COPD exacerbations shows that there are associations between several demographic and disease characteristics with COPD exacerbations, potentially allowing clinicians to identify patients most at risk of future exacerbations. Exacerbation history, comorbidities, and disease severity or bronchodilator reversibility were the factors most strongly associated with exacerbation risk, and should be considered in future research efforts to develop prognostic tools to estimate the likelihood of exacerbation occurrence. Importantly, many prognostic factors for exacerbations, such as symptom burden, QoL, and comorbidities, are modifiable with optimal pharmacologic and non-pharmacologic treatments or lifestyle modifications. Overall, the evidence suggests that, taken together, predicting and reducing exacerbation risk is an achievable goal in COPD.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Body mass index
COPD Assessment Test
Chronic obstructive pulmonary disease
Forced expiratory volume in 1 s
Global Initiative for Chronic Obstructive Lung Disease
Inhaled corticosteroid
Modified Medical Research Council
Quality of life
St. George’s Respiratory Questionnaire
World Health Organization. The top 10 causes of death. 2018. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death . Accessed 22 Jul 2020.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. 2020;396:1204–22.
Article Google Scholar
Hurst JR, Skolnik N, Hansen GJ, Anzueto A, Donaldson GC, Dransfield MT, Varghese P. Understanding the impact of chronic obstructive pulmonary disease exacerbations on patient health and quality of life. Eur J Intern Med. 2020;73:1–6.
Article PubMed Google Scholar
Zhang Y, Morgan RL, Alonso-Coello P, Wiercioch W, Bała MM, Jaeschke RR, Styczeń K, Pardo-Hernandez H, Selva A, Ara Begum H, et al. A systematic review of how patients value COPD outcomes. Eur Respir J. 2018;52:1800222.
Global Initiative for Chronic Obstructive Lung Disease. 2022 GOLD Report. Global strategy for the diagnosis, management and prevention of COPD. 2022. https://goldcopd.org/2022-gold-reports-2/ . Accessed 02 Feb 2022.
Müllerová H, Shukla A, Hawkins A, Quint J. Risk factors for acute exacerbations of COPD in a primary care population: a retrospective observational cohort study. BMJ Open. 2014;4: e006171.
Article PubMed PubMed Central Google Scholar
Westerik JAM, Metting EI, van Boven JFM, Tiersma W, Kocks JWH, Schermer TR. Associations between chronic comorbidity and exacerbation risk in primary care patients with COPD. Respir Res. 2017;18:31.
Vedel-Krogh S, Nielsen SF, Lange P, Vestbo J, Nordestgaard BG. Blood eosinophils and exacerbations in chronic obstructive pulmonary disease. The Copenhagen General Population Study. Am J Respir Crit Care Med. 2016;193:965–74.
Hurst JR, Vestbo J, Anzueto A, Locantore N, Müllerová H, Tal-Singer R, Miller B, Lomas DA, Agusti A, Macnee W, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363:1128–38.
Article CAS PubMed Google Scholar
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Çolak Y, Afzal S, Marott JL, Nordestgaard BG, Vestbo J, Ingebrigtsen TS, Lange P. Prognosis of COPD depends on severity of exacerbation history: a population-based analysis. Respir Med. 2019;155:141–7.
Rothnie KJ, Müllerová H, Smeeth L, Quint JK. Natural history of chronic obstructive pulmonary disease exacerbations in a general practice-based population with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;198:464–71.
Pascoe S, Barnes N, Brusselle G, Compton C, Criner GJ, Dransfield MT, Halpin DMG, Han MK, Hartley B, Lange P, et al. Blood eosinophils and treatment response with triple and dual combination therapy in chronic obstructive pulmonary disease: analysis of the IMPACT trial. Lancet Respir Med. 2019;7:745–56.
Yun JH, Lamb A, Chase R, Singh D, Parker MM, Saferali A, Vestbo J, Tal-Singer R, Castaldi PJ, Silverman EK, et al. Blood eosinophil count thresholds and exacerbations in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2018;141:2037-2047.e10.
Yoon HY, Park SY, Lee CH, Byun MK, Na JO, Lee JS, Lee WY, Yoo KH, Jung KS, Lee JH. Prediction of first acute exacerbation using COPD subtypes identified by cluster analysis. Int J Chron Obstruct Pulmon Dis. 2019;14:1389–97.
Article CAS PubMed PubMed Central Google Scholar
Yohannes AM, Mulerova H, Lavoie K, Vestbo J, Rennard SI, Wouters E, Hanania NA. The association of depressive symptoms with rates of acute exacerbations in patients with COPD: results from a 3-year longitudinal follow-up of the ECLIPSE cohort. J Am Med Dir Assoc. 2017;18:955-959.e6.
Tsiligianni I, Metting E, van der Molen T, Chavannes N, Kocks J. Morning and night symptoms in primary care COPD patients: a cross-sectional and longitudinal study. An UNLOCK study from the IPCRG. NPJ Prim Care Respir Med. 2016;26:16040.
Jo YS, Yoon HI, Kim DK, Yoo CG, Lee CH. Comparison of COPD Assessment Test and Clinical COPD Questionnaire to predict the risk of exacerbation. Int J Chron Obstruct Pulmon Dis. 2018;13:101–7.
Marçôa R, Rodrigues DM, Dias M, Ladeira I, Vaz AP, Lima R, Guimarães M. Classification of Chronic Obstructive Pulmonary Disease (COPD) according to the new Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2017: comparison with GOLD 2011. COPD. 2018;15:21–6.
Han MK, Quibrera PM, Carretta EE, Barr RG, Bleecker ER, Bowler RP, Cooper CB, Comellas A, Couper DJ, Curtis JL, et al. Frequency of exacerbations in patients with chronic obstructive pulmonary disease: an analysis of the SPIROMICS cohort. Lancet Respir Med. 2017;5:619–26.
Yii ACA, Loh CH, Tiew PY, Xu H, Taha AAM, Koh J, Tan J, Lapperre TS, Anzueto A, Tee AKH. A clinical prediction model for hospitalized COPD exacerbations based on “treatable traits.” Int J Chron Obstruct Pulmon Dis. 2019;14:719–28.
McGarvey L, Lee AJ, Roberts J, Gruffydd-Jones K, McKnight E, Haughney J. Characterisation of the frequent exacerbator phenotype in COPD patients in a large UK primary care population. Respir Med. 2015;109:228–37.
Margüello MS, Garrastazu R, Ruiz-Nuñez M, Helguera JM, Arenal S, Bonnardeux C, León C, Miravitlles M, García-Rivero JL. Independent effect of prior exacerbation frequency and disease severity on the risk of future exacerbations of COPD: a retrospective cohort study. NPJ Prim Care Respir Med. 2016;26:16046.
Engel B, Schindler C, Leuppi JD, Rutishauser J. Predictors of re-exacerbation after an index exacerbation of chronic obstructive pulmonary disease in the REDUCE randomised clinical trial. Swiss Med Wkly. 2017;147: w14439.
PubMed Google Scholar
Benson VS, Müllerová H, Vestbo J, Wedzicha JA, Patel A, Hurst JR. Evaluation of COPD longitudinally to identify predictive surrogate endpoints (ECLIPSE) investigators. Associations between gastro-oesophageal reflux, its management and exacerbations of chronic obstructive pulmonary disease. Respir Med. 2015;109:1147–54.
Santibáñez M, Garrastazu R, Ruiz-Nuñez M, Helguera JM, Arenal S, Bonnardeux C, León C, García-Rivero JL. Predictors of hospitalized exacerbations and mortality in chronic obstructive pulmonary disease. PLoS ONE. 2016;11: e0158727.
Article PubMed PubMed Central CAS Google Scholar
Jo YS, Kim YH, Lee JY, Kim K, Jung KS, Yoo KH, Rhee CK. Impact of BMI on exacerbation and medical care expenses in subjects with mild to moderate airflow obstruction. Int J Chron Obstruct Pulmon Dis. 2018;13:2261–9.
Alexopoulos EC, Malli F, Mitsiki E, Bania EG, Varounis C, Gourgoulianis KI. Frequency and risk factors of COPD exacerbations and hospitalizations: a nationwide study in Greece (Greek Obstructive Lung Disease Epidemiology and health ecoNomics: GOLDEN study). Int J Chron Obstruct Pulmon Dis. 2015;10:2665–74.
PubMed PubMed Central Google Scholar
Liu D, Peng SH, Zhang J, Bai SH, Liu HX, Qu JM. Prediction of short term re-exacerbation in patients with acute exacerbation of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015;10:1265–73.
Müllerová H, Maselli DJ, Locantore N, Vestbo J, Hurst JR, Wedzicha JA, Bakke P, Agusti A, Anzueto A. Hospitalized exacerbations of COPD: risk factors and outcomes in the ECLIPSE cohort. Chest. 2015;147:999–1007.
de Miguel-Díez J, Hernández-Vázquez J, López-de-Andrés A, Álvaro-Meca A, Hernández-Barrera V, Jiménez-García R. Analysis of environmental risk factors for chronic obstructive pulmonary disease exacerbation: a case-crossover study (2004–2013). PLoS ONE. 2019;14: e0217143.
Krachunov II, Kyuchukov NH, Ivanova ZI, Yanev NA, Hristova PA, Borisova ED, Popova TP, Pavlov PS, Nikolova PT, Ivanov YY. Impact of air pollution and outdoor temperature on the rate of chronic obstructive pulmonary disease exacerbations. Folia Med (Plovdiv). 2017;59:423–9.
Article CAS Google Scholar
Baumeler L, Papakonstantinou E, Milenkovic B, Lacoma A, Louis R, Aerts JG, Welte T, Kostikas K, Blasi F, Boersma W, et al. Therapy with proton-pump inhibitors for gastroesophageal reflux disease does not reduce the risk for severe exacerbations in COPD. Respirology. 2016;21:883–90.
Annavarapu S, Goldfarb S, Gelb M, Moretz C, Renda A, Kaila S. Development and validation of a predictive model to identify patients at risk of severe COPD exacerbations using administrative claims data. Int J Chron Obstruct Pulmon Dis. 2018;13:2121–30.
Crisafulli E, Torres A, Huerta A, Méndez R, Guerrero M, Martinez R, Liapikou A, Soler N, Sethi S, Menéndez R. C-reactive protein at discharge, diabetes mellitus and ≥1 hospitalization during previous year predict early readmission in patients with acute exacerbation of chronic obstructive pulmonary disease. COPD. 2015;12:311–20.
Bollmeier SG, Hartmann AP. Management of chronic obstructive pulmonary disease: a review focusing on exacerbations. Am J Health Syst Pharm. 2020;77:259–68.
Bafadhel M, Peterson S, De Blas MA, Calverley PM, Rennard SI, Richter K, Fagerås M. Predictors of exacerbation risk and response to budesonide in patients with chronic obstructive pulmonary disease: a post-hoc analysis of three randomised trials. Lancet Respir Med. 2018;6:117–26.
Calverley PM, Anzueto AR, Dusser D, Mueller A, Metzdorf N, Wise RA. Treatment of exacerbations as a predictor of subsequent outcomes in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:1297–308.
Calverley PM, Tetzlaff K, Dusser D, Wise RA, Mueller A, Metzdorf N, Anzueto A. Determinants of exacerbation risk in patients with COPD in the TIOSPIR study. Int J Chron Obstruct Pulmon Dis. 2017;12:3391–405.
Eklöf J, Sørensen R, Ingebrigtsen TS, Sivapalan P, Achir I, Boel JB, Bangsborg J, Ostergaard C, Dessau RB, Jensen US, et al. Pseudomonas aeruginosa and risk of death and exacerbations in patients with chronic obstructive pulmonary disease: an observational cohort study of 22 053 patients. Clin Microbiol Infect. 2020;26:227–34.
Estirado C, Ceccato A, Guerrero M, Huerta A, Cilloniz C, Vilaró O, Gabarrús A, Gea J, Crisafulli E, Soler N, Torres A. Microorganisms resistant to conventional antimicrobials in acute exacerbations of chronic obstructive pulmonary disease. Respir Res. 2018;19:119.
Fuhrman C, Moutengou E, Roche N, Delmas MC. Prognostic factors after hospitalization for COPD exacerbation. Rev Mal Respir. 2017;34:1–18.
Krachunov I, Kyuchukov N, Ivanova Z, Yanev NA, Hristova PA, Pavlov P, Glogovska P, Popova T, Ivanov YY. Stability of frequent exacerbator phenotype in patients with chronic obstructive pulmonary disease. Folia Med (Plovdiv). 2018;60:536–45.
Make BJ, Eriksson G, Calverley PM, Jenkins CR, Postma DS, Peterson S, Östlund O, Anzueto A. A score to predict short-term risk of COPD exacerbations (SCOPEX). Int J Chron Obstruct Pulmon Dis. 2015;10:201–9.
Montserrat-Capdevila J, Godoy P, Marsal JR, Barbé F. Predictive model of hospital admission for COPD exacerbation. Respir Care. 2015;60:1288–94.
Montserrat-Capdevila J, Godoy P, Marsal JR, Barbé F, Galván L. Risk factors for exacerbation in chronic obstructive pulmonary disease: a prospective study. Int J Tuberc Lung Dis. 2016;20:389–95.
Orea-Tejeda A, Navarrete-Peñaloza AG, Verdeja-Vendrell L, Jiménez-Cepeda A, González-Islas DG, Hernández-Zenteno R, Keirns-Davis C, Sánchez-Santillán R, Velazquez-Montero A, Puentes RG. Right heart failure as a risk factor for severe exacerbation in patients with chronic obstructive pulmonary disease: prospective cohort study. Clin Respir J. 2018;12:2635–41.
Papi A, Vestbo J, Fabbri L, Corradi M, Prunier H, Cohuet G, Guasconi A, Montagna I, Vezzoli S, Petruzzelli S, et al. Extrafine inhaled triple therapy versus dual bronchodilator therapy in chronic obstructive pulmonary disease (TRIBUTE): a double-blind, parallel group, randomised controlled trial. Lancet. 2018;391:1076–84.
Lipson DA, Barnhart F, Brealey N, Brooks J, Criner GJ, Day NC, Dransfield MT, Halpin DMG, Han MK, Jones CE, et al. Once-daily single-inhaler triple versus dual therapy in patients with COPD. N Engl J Med. 2018;378:1671–80.
Pasquale MK, Xu Y, Baker CL, Zou KH, Teeter JG, Renda AM, Davis CC, Lee TC, Bobula J. COPD exacerbations associated with the modified Medical Research Council scale and COPD assessment test among Humana Medicare members. Int J Chron Obstruct Pulmon Dis. 2016;11:111–21.
Schuler M, Wittmann M, Faller H, Schultz K. Including changes in dyspnea after inpatient rehabilitation improves prediction models of exacerbations in COPD. Respir Med. 2018;141:87–93.
Singh D, Papi A, Corradi M, Pavlišová I, Montagna I, Francisco C, Cohuet G, Vezzoli S, Scuri M, Vestbo J. Single inhaler triple therapy versus inhaled corticosteroid plus long-acting β 2 -agonist therapy for chronic obstructive pulmonary disease (TRILOGY): a double-blind, parallel group, randomised controlled trial. Lancet. 2016;388:963–73.
Søgaard M, Madsen M, Løkke A, Hilberg O, Sørensen HT, Thomsen RW. Incidence and outcomes of patients hospitalized with COPD exacerbation with and without pneumonia. Int J Chron Obstruct Pulmon Dis. 2016;11:455–65.
Stanford RH, Nag A, Mapel DW, Lee TA, Rosiello R, Schatz M, Vekeman F, Gauthier-Loiselle M, Merrigan JFP, Duh MS. Claims-based risk model for first severe COPD exacerbation. Am J Manag Care. 2018;24:e45–53.
Stanford RH, Lau MS, Li Y, Stemkowski S. External validation of a COPD risk measure in a commercial and medicare population: the COPD treatment ratio. J Manag Care Spec Pharm. 2019;25:58–69.
Vestbo J, Papi A, Corradi M, Blazhko V, Montagna I, Francisco C, Cohuet G, Vezzoli S, Scuri M, Singh D. Single inhaler extrafine triple therapy versus long-acting muscarinic antagonist therapy for chronic obstructive pulmonary disease (TRINITY): a double-blind, parallel group, randomised controlled trial. Lancet. 2017;389:1919–29.
Wei X, Ma Z, Yu N, Ren J, Jin C, Mi J, Shi M, Tian L, Gao Y, Guo Y. Risk factors predict frequent hospitalization in patients with acute exacerbation of COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:121–9.
Whalley D, Svedsater H, Doward L, Crawford R, Leather D, Lay-Flurrie J, Bosanquet N. Follow-up interviews from The Salford Lung Study (COPD) and analyses per treatment and exacerbations. NPJ Prim Care Respir Med. 2019;29:20.
Zeiger RS, Tran TN, Butler RK, Schatz M, Li Q, Khatry DB, Martin U, Kawatkar AA, Chen W. Relationship of blood eosinophil count to exacerbations in chronic obstructive pulmonary disease. J Allergy Clin Immunol Pract. 2018;6:944-954.e945.
Vogelmeier CF, Kostikas K, Fang J, Tian H, Jones B, Morgan CL, Fogel R, Gutzwiller FS, Cao H. Evaluation of exacerbations and blood eosinophils in UK and US COPD populations. Respir Res. 2019;20:178.
Celli BR, Fabbri LM, Aaron SD, Agusti A, Brook R, Criner GJ, Franssen FME, Humbert M, Hurst JR, O’Donnell D, et al. An updated definition and severity classification of COPD exacerbations: the Rome proposal. Am J Respir Crit Care Med. 2021;204:1251–8.
Adir Y, Hakrush O, Shteinberg M, Schneer S, Agusti A. Circulating eosinophil levels do not predict severe exacerbations in COPD: a retrospective study. ERJ Open Research. 2018;4:00022–2018.
Bartels W, Adamson S, Leung L, Sin DD, van Eeden SF. Emergency department management of acute exacerbations of chronic obstructive pulmonary disease: factors predicting readmission. Int J Chron Obstruct Pulmon Dis. 2018;13:1647–54.
Kim V, Zhao H, Regan E, Han MK, Make BJ, Crapo JD, Jones PW, Curtis JL, Silverman EK, Criner GJ, COPDGene Investigators. The St. George’s Respiratory Questionnaire definition of chronic bronchitis may be a better predictor of COPD exacerbations compared with the classic definition. Chest. 2019;156:685–95.
Abston E, Comellas A, Reed RM, Kim V, Wise RA, Brower R, Fortis S, Beichel R, Bhatt S, Zabner J, et al. Higher BMI is associated with higher expiratory airflow normalised for lung volume (FEF25-75/FVC) in COPD. BMJ Open Respir Res. 2017;4: e000231.
Emura I, Usuda H, Satou K. Appearance of large scavenger receptor A-positive cells in peripheral blood: a potential risk factor for severe exacerbation of chronic obstructive pulmonary disease. Pathol Int. 2019;69:187–92.
Erol S, Sen E, Gizem Kilic Y, Yousif A, Akkoca Yildiz O, Acican T, Saryal S. Does the 2017 revision improve the ability of GOLD to predict risk of future moderate and severe exacerbation? Clin Respir J. 2018;12:2354–60.
Han MZ, Hsiue TR, Tsai SH, Huang TH, Liao XM, Chen CZ. Validation of the GOLD 2017 and new 16 subgroups (1A–4D) classifications in predicting exacerbation and mortality in COPD patients. Int J Chron Obstruct Pulmon Dis. 2018;13:3425–33.
Huang TH, Hsiue TR, Lin SH, Liao XM, Su PL, Chen CZ. Comparison of different staging methods for COPD in predicting outcomes. Eur Resp J. 2018;51:1700577.
Jung YH, Lee DY, Kim DW, Park SS, Heo EY, Chung HS, Kim DK. Clinical significance of laryngopharyngeal reflux in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015;10:1343–51.
CAS PubMed PubMed Central Google Scholar
Kim J, Kim WJ, Lee CH, Lee SH, Lee MG, Shin KC, Yoo KH, Lee JH, Lim SY, Na JO, et al. Which bronchodilator reversibility criteria can predict severe acute exacerbation in chronic obstructive pulmonary disease patients? Respir Res. 2017;18:107.
Kobayashi S, Hanagama M, Ishida M, Sato H, Ono M, Yamanda S, Yamada M, Aizawa H, Yanai M. Clinical characteristics and outcomes in Japanese patients with COPD according to the 2017 GOLD classification: the Ishinomaki COPD Network Registry. Int J Chron Obstruct Pulmon Dis. 2018;13:3947–55.
Lee SH, Lee JH, Yoon HI, Park HY, Kim TH, Yoo KH, Oh YM, Jung KS, Lee SD, Lee SW. Change in inhaled corticosteroid treatment and COPD exacerbations: an analysis of real-world data from the KOLD/KOCOSS cohorts. Respir Res. 2019;20:62.
Pavlovic R, Stefanovic S, Lazic Z, Jankovic S. Factors associated with the rate of COPD exacerbations that require hospitalization. Turk J Med Sci. 2017;47:134–41.
Song JH, Lee CH, Um SJ, Park YB, Yoo KH, Jung KS, Lee SD, Oh YM, Lee JH, Kim EK, Kim DK. Clinical impacts of the classification by 2017 GOLD guideline comparing previous ones on outcomes of COPD in real-world cohorts. Int J Chron Obstruct Pulmon Dis. 2018;13:3473–84.
Sundh J, Johansson G, Larsson K, Lindén A, Löfdahl CG, Sandström T, Janson C. The phenotype of concurrent chronic bronchitis and frequent exacerbations in patients with severe COPD attending Swedish secondary care units. Int J Chron Obstruct Pulmon Dis. 2015;10:2327–34.
Urwyler P, Hussein NA, Bridevaux PO, Chhajed PN, Geiser T, Grendelmeier P, Zellweger LJ, Kohler M, Maier S, Miedinger D, et al. Predictive factors for exacerbation and reexacerbation in chronic obstructive pulmonary disease: an extension of the Cox model to analyze data from the Swiss COPD cohort. Multidiscip Respir Med. 2019;14:7.
Wallace AE, Kaila S, Bayer V, Shaikh A, Shinde MU, Willey VJ, Napier MB, Singer JR. Health care resource utilization and exacerbation rates in patients with COPD stratified by disease severity in a commercially insured population. J Manag Care Spec Pharm. 2019;25:205–17.
Halpin DMG, Decramer M, Celli BR, Mueller A, Metzdorf N, Tashkin DP. Effect of a single exacerbation on decline in lung function in COPD. Respir Med. 2017;128:85–91.
Bade BC, DeRycke EC, Ramsey C, Skanderson M, Crothers K, Haskell S, Bean-Mayberry B, Brandt C, Bastian LA, Akgün KM. Sex differences in veterans admitted to the hospital for chronic obstructive pulmonary disease exacerbation. Ann Am Thorac Soc. 2019;16:707–14.
Iyer AS, Bhatt SP, Dransfield M, Kinney G, Holm K, Wamboldt FS, Hanania N, Martinez C, Regan E, Foreman MG, et al. Psychological distress prospectively predicts severe exacerbations in smokers with and without airflow limitation—a longitudinal follow-up study of the COPDGene cohort [abstract]. Am J Respir Crit Care Med. 2017. https://doi.org/10.1164/ajrccm-conference.2017.195.1_MeetingAbstracts.A4709 .
Diamond M, Zhao H, Armstrong HF, Morrison M, Bailey KL, Carretta EE, Criner GJ, Han MK, Bleeker E, Cooper CB, et al. Anxiety and depression, either alone or in combination, are associated with respiratory exacerbations in smokers with and without COPD [abstract]. Am J Respir Crit Care Med. 2017;195:1615–31.
Google Scholar
Lau CS, Siracuse BL, Chamberlain RS. Readmission After COPD Exacerbation Scale: determining 30-day readmission risk for COPD patients. Int J Chron Obstruct Pulmon Dis. 2017;12:1891–902.
Pikoula M, Quint JK, Nissen F, Hemingway H, Smeeth L, Denaxas S. Identifying clinically important COPD sub-types using data-driven approaches in primary care population based electronic health records. BMC Med Inform Decis Mak. 2019;19:86.
Wei YF, Tsai YH, Wang CC, Kuo PH. Impact of overweight and obesity on acute exacerbations of COPD—subgroup analysis of the Taiwan Obstructive Lung Disease cohort. Int J Chron Obstruct Pulmon Dis. 2017;12:2723–9.
Barnes PJ, Celli BR. Systemic manifestations and comorbidities of COPD. Eur Resp J. 2009;33:1165–85.
Polverino E, Dimakou K, Hurst J, Martinez-Garcia MA, Miravitlles M, Paggiaro P, Shteinberg M, Aliberti S, Chalmers JD. The overlap between bronchiectasis and chronic airway diseases: state of the art and future directions. Eur Respir J. 2018;52:1800328.
Xu W, Collet JP, Shapiro S, Lin Y, Yang T, Platt RW, Wang C, Bourbeau J. Independent effect of depression and anxiety on chronic obstructive pulmonary disease exacerbations and hospitalizations. Am J Respir Crit Care Med. 2008;178:913–20.
Chapman KR, Hurst JR, Frent SM, Larbig M, Fogel R, Guerin T, Banerji D, Patalano F, Goyal P, Pfister P, et al. Long-term triple therapy de-escalation to indacaterol/glycopyrronium in patients with chronic obstructive pulmonary disease (SUNSET): a randomized, double-blind, triple-dummy clinical trial. Am J Respir Crit Care Med. 2018;198:329–39.
Couillard S, Larivée P, Courteau J, Vanasse A. Eosinophils in COPD exacerbations are associated with increased readmissions. Chest. 2017;151:366–73.
Ferguson GT, Rabe KF, Martinez FJ, Fabbri LM, Wang C, Ichinose M, Bourne E, Ballal S, Darken P, DeAngelis K, et al. Triple therapy with budesonide/glycopyrrolate/formoterol fumarate with co-suspension delivery technology versus dual therapies in chronic obstructive pulmonary disease (KRONOS): a double-blind, parallel-group, multicentre, phase 3 randomised controlled trial. Lancet Respir Med. 2018;6:747–58.
Ko FWS, Chan KP, Ngai J, Ng SS, Yip WH, Ip A, Chan TO, Hui DSC. Blood eosinophil count as a predictor of hospital length of stay in COPD exacerbations. Respirology. 2019;25:259–66.
MacDonald MI, Osadnik CR, Bulfin L, Hamza K, Leong P, Wong A, King PT, Bardin PG. Low and high blood eosinophil counts as biomarkers in hospitalized acute exacerbations of COPD. Chest. 2019;156:92–100.
Müllerová H, Hahn B, Simard EP, Mu G, Hatipoğlu U. Exacerbations and health care resource use among patients with COPD in relation to blood eosinophil counts. Int J Chron Obstruct Pulmon Dis. 2019;14:683–92.
Bafadhel M, Greening NJ, Harvey-Dunstan TC, Williams JEA, Morgan MD, Brightling CE, Hussain SF, Pavord ID, Singh SJ, Steiner MC. Blood eosinophils and outcomes in severe hospitalised exacerbations of COPD. Chest. 2016;150:320–8.
Roche N, Chapman KR, Vogelmeier CF, Herth FJF, Thach C, Fogel R, Olsson P, Patalano F, Banerji D, Wedzicha JA. Blood eosinophils and response to maintenance chronic obstructive pulmonary disease treatment. Data from the FLAME trial. Am J Respir Crit Care Med. 2017;195:1189–97.
Vestbo J, Vogelmeier CF, Small M, Siddall J, Fogel R, Kostikas K. Inhaled corticosteroid use by exacerbations and eosinophils: a real-world COPD population. Int J Chron Obstruct Pulmon Dis. 2019;14:853–61.
Watz H, Tetzlaff K, Wouters EFM, Kirsten A, Magnussen H, Rodriguez-Roisin R, Vogelmeier C, Fabbri LM, Chanez P, Dahl R, et al. Blood eosinophil count and exacerbations in severe chronic obstructive pulmonary disease after withdrawal of inhaled corticosteroids: a post-hoc analysis of the WISDOM trial. Lancet Respir Med. 2016;4:390–8.
Pavord ID, Lettis S, Locantore N, Pascoe S, Jones PW, Wedzicha JA, Barnes NC. Blood eosinophils and inhaled corticosteroid/long-acting beta-2 agonist efficacy in COPD. Thorax. 2016;71:118–25.
Singh D. Predicting corticosteroid response in chronic obstructive pulmonary disease. Blood eosinophils gain momentum. Am J Respir Crit Care Med. 2017;196:1098–100.
Vestbo J, Prescott E, Almdal T, Dahl M, Nordestgaard BG, Andersen T, Sørensen TIA, Lange P. Body mass, fat-free body mass, and prognosis in patients with chronic obstructive pulmonary disease from a random population sample: findings from the Copenhagen City Heart Study. Am J Respir Crit Care Med. 2006;173:79–83.
Agustí AGN, Noguera A, Sauleda J, Sala E, Pons J, Busquets X. Systemic effects of chronic obstructive pulmonary disease. Eur Respir J. 2003;21:347–60.
Agustí AGN, Sauleda J, Miralles C, Gomez C, Togores B, Sala E, Batle S, Busquets X. Skeletal muscle apoptosis and weight loss in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2002;166:485–9.
Labaki WW, Martinez FJ. Time to understand the infrequency of the frequent exacerbator phenotype in COPD. Chest. 2018;153:1087–8.
Hartley BF, Barnes NC, Lettis S, Compton CH, Papi A, Jones P. Risk factors for exacerbations and pneumonia in patients with chronic obstructive pulmonary disease: a pooled analysis. Respir Res. 2020;21:5.
Kim Y, Kim YJ, Kang YM, Cho WK. Exploring the impact of number and type of comorbidities on the risk of severe COPD exacerbations in Korean Population: a Nationwide Cohort Study. BMC Pulm Med. 2021;21:151.
Mackay AJ, Kostikas K, Roche N, Frent SM, Olsson P, Pfister P, Gupta P, Patalano F, Banerji D, Wedzicha JA. Impact of baseline symptoms and health status on COPD exacerbations in the FLAME study. Respir Res. 2020;21:93.
Smulders L, van der Aalst A, Neuhaus EDET, Polman S, Franssen FME, van Vliet M, de Kruif MD. Decreased risk of COPD exacerbations in obese patients. COPD. 2020;17:485–91.
Battisti WP, Wager E, Baltzer L, Bridges D, Cairns A, Carswell CI, Citrome L, Gurr JA, Mooney LA, Moore BJ, et al. Good publication practice for communicating company-sponsored medical research: GPP3. Ann Intern Med. 2015;163:461–4.
Putcha N, Barr RG, Han M, Woodruff PG, Bleecker ER, Kanner RE, Martinez FJ, Tashkin DP, Rennard SI, Breysse P, et al. Understanding the impact of passive smoke exposure on outcomes in COPD [abstract]. Am J Respir Crit Care Med. 2015;191:411–20.
Wu Z, Yang D, Ge Z, Yan M, Wu N, Liu Y. Body mass index of patients with chronic obstructive pulmonary disease is associated with pulmonary function and exacerbations: a retrospective real world research. J Thorac Dis. 2018;10:5086–99.
Download references
Acknowledgements
Medical writing support, under the direction of the authors, was provided by Julia King, PhD, and Sarah Piggott, MChem, CMC Connect, McCann Health Medical Communications, funded by AstraZeneca in accordance with Good Publication Practice (GPP3) guidelines [ 109 ].
This study was supported by AstraZeneca.
Author information
Authors and affiliations.
UCL Respiratory, University College London, London, WC1E 6BT, UK
John R. Hurst
Division of Pulmonary and Critical Care, University of Michigan, Ann Arbor, MI, USA
MeiLan K. Han
Formerly of Parexel International, Mohali, India
Barinder Singh, Gagandeep Kaur & Mohd Kashif Siddiqui
Parexel International, Mohali, India
Sakshi Sharma
Formerly of AstraZeneca, Cambridge, UK
Enrico de Nigris
AstraZeneca, Gothenburg, Sweden
Ulf Holmgren
You can also search for this author in PubMed Google Scholar
Contributions
The authors have made the following declaration about their contributions. JRH and MKH made substantial contributions to the interpretation of data; BS, SS, GK, and MKS made substantial contributions to the acquisition, analysis, and interpretation of data; EdN and UH made substantial contributions to the conception and design of the work and the interpretation of data. All authors contributed to drafting or critically revising the article, have approved the submitted version, and agree to be personally accountable for their own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. All authors read and approved the final manuscript.
Corresponding author
Correspondence to John R. Hurst .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
JRH reports consulting fees from AstraZeneca; speaker fees from AstraZeneca, Chiesi, Pfizer, and Takeda; and travel support from GlaxoSmithKline and AstraZeneca. MKH reports assistance with conduction of this research and publication from AstraZeneca; personal fees from Aerogen, Altesa Biopharma, AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, DevPro, GlaxoSmithKline, Integrity, Medscape, Merck, Mylan, NACE, Novartis, Polarean, Pulmonx, Regeneron, Sanofi, Teva, Verona, United Therapeutics, and UpToDate; either in kind research support or funds paid to the institution from the American Lung Association, AstraZeneca, Biodesix, Boehringer Ingelheim, the COPD Foundation, Gala Therapeutics, the NIH, Novartis, Nuvaira, Sanofi, and Sunovion; participation in Data Safety Monitoring Boards for Novartis and Medtronic with funds paid to the institution; and stock options from Altesa Biopharma and Meissa Vaccines. BS, GK, and MKS are former employees of Parexel International. SS is an employee of Parexel International, which was funded by AstraZeneca to conduct this analysis. EdN is a former employee of AstraZeneca and previously held stock and/or stock options in the company. UH is an employee of AstraZeneca and holds stock and/or stock options in the company.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file1: table s1..
Search strategies. Table S2. List of included studies with linked publications. Table S3. Study characteristics across the 76 included studies. Table S4. Clinical characteristics of the patients assessed across the included studies.
Additional file 2: Fig. S1.
Sex (male vs female) as a risk factor for moderate-to-severe exacerbations. Fig. S2. Sex (male vs female) as a risk factor for severe exacerbations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hurst, J.R., Han, M.K., Singh, B. et al. Prognostic risk factors for moderate-to-severe exacerbations in patients with chronic obstructive pulmonary disease: a systematic literature review. Respir Res 23 , 213 (2022). https://doi.org/10.1186/s12931-022-02123-5
Download citation
Received : 02 March 2022
Accepted : 20 July 2022
Published : 23 August 2022
DOI : https://doi.org/10.1186/s12931-022-02123-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Exacerbations
- Comorbidities
- Hospitalization
Respiratory Research
ISSN: 1465-993X
- General enquiries: [email protected]
- Open access
- Published: 21 June 2022
Fluid challenge in critically ill patients receiving haemodynamic monitoring: a systematic review and comparison of two decades
- Antonio Messina 1 , 2 ,
- Lorenzo Calabrò 1 ,
- Luca Pugliese 1 ,
- Aulona Lulja 1 ,
- Alexandra Sopuch 1 ,
- Daniela Rosalba 3 ,
- Emanuela Morenghi 1 , 2 ,
- Glenn Hernandez 4 ,
- Xavier Monnet 5 , 6 , 7 &
- Maurizio Cecconi 1 , 2
Critical Care volume 26 , Article number: 186 ( 2022 ) Cite this article
11k Accesses
30 Citations
36 Altmetric
Metrics details
Introduction
Fluid challenges are widely adopted in critically ill patients to reverse haemodynamic instability. We reviewed the literature to appraise fluid challenge characteristics in intensive care unit (ICU) patients receiving haemodynamic monitoring and considered two decades: 2000–2010 and 2011–2021.
We assessed research studies and collected data regarding study setting, patient population, fluid challenge characteristics, and monitoring. MEDLINE, Embase, and Cochrane search engines were used. A fluid challenge was defined as an infusion of a definite quantity of fluid (expressed as a volume in mL or ml/kg) in a fixed time (expressed in minutes), whose outcome was defined as a change in predefined haemodynamic variables above a predetermined threshold.
We included 124 studies, 32 (25.8%) published in 2000–2010 and 92 (74.2%) in 2011–2021, overall enrolling 6,086 patients, who presented sepsis/septic shock in 50.6% of cases. The fluid challenge usually consisted of 500 mL (76.6%) of crystalloids (56.6%) infused with a rate of 25 mL/min. Fluid responsiveness was usually defined by a cardiac output/index (CO/CI) increase ≥ 15% (70.9%). The infusion time was quicker (15 min vs 30 min), and crystalloids were more frequent in the 2011–2021 compared to the 2000–2010 period.
Conclusions
In the literature, fluid challenges are usually performed by infusing 500 mL of crystalloids bolus in less than 20 min. A positive fluid challenge response, reported in 52% of ICU patients, is generally defined by a CO/CI increase ≥ 15%. Compared to the 2000–2010 decade, in 2011–2021 the infusion time of the fluid challenge was shorter, and crystalloids were more frequently used.
Fluid administration in the intensive care unit (ICU) is one of the most common and disputed interventions triggered at the bedside by several clinical variables [ 1 , 2 ].
Fluid therapy aims to increase stroke volume (SV) and cardiac output (CO) to optimise systemic blood flow and tissue perfusion. As with any therapeutic intervention, the final clinical effect elicited may vary because of a complex interplay between the patient's intrinsic conditions and the therapy itself.
Fluid responsiveness can occur only if both ventricles work on the ascending, steep part of the Frank–Starling curve, i.e. in cases where CO is preload dependent [ 3 , 4 ]. Preload dependency is assessed using a diagnostic test performed by infusing a fixed aliquot of fluid, the fluid challenge [ 5 , 6 , 7 ]. From a clinical perspective, this approach also allows titration of fluid administration (when the patient becomes no longer responsive to the fluid challenge) and reduces the risk of fluid overload, which worsens the outcome of ICU patients [ 8 , 9 ].
Several variables defining the characteristics of the fluid challenge have been further investigated in studies adopting continuous haemodynamic monitoring, showing that the amount of fluids given, the rate of administration, and the threshold adopted to define fluid responsiveness impact the outcome of a fluid challenge [ 10 , 11 , 12 ]. Moreover, despite conflicting results on shock reversal efficacy between crystalloids and colloids, crystalloids are now recommended as the first-line fluid type in patients with septic shock, being inexpensive and widely available. Also, the administration of colloids compared to crystalloids has not demonstrated any clear benefit in the literature [ 13 , 14 ].
However, neither the nature, mode of administration, and method to assess the effectiveness of the fluid challenge are standardised in current clinical practice, and the definition of fluid challenge responsiveness is also variable among studies [ 15 , 16 , 17 , 18 ].
Whether or not these findings have modified the modalities of fluid challenge and the definition of fluid responsiveness in published studies is uncertain. To address this issue, we systematically reviewed existing literature from the year 2000. We appraised the characteristics of fluid challenges in critically ill patients (i.e., amount and kind of fluid administration, time of infusion, hemodynamic variables, and thresholds for fluid responsiveness) enrolled in research studies receiving continuous haemodynamic monitoring and assessed the relationship between the reported fluid responsiveness and predefined independent variables. Secondarily, we compared data from studies published in 2011–2021 versus those published in 2000–2010.
Material and methods
We adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis-Protocols (PRISMA-P) guidelines (Additional file 1 : Table S1). The study protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO) in November 2021 (CRD42021284761).
Search strategy
A systematic literature search was performed, including the following databases: PUBMED®, EMBASE®, and the Cochrane Controlled Clinical trials register. The following keywords and their related MeSh terms were used: “fluid challenge”, “fluid responsiveness”, “stroke volume variation”, “pulse pressure variation”, “dynamic indices OR indexes”, “passive leg raising”, OR “passive leg raising test”, “functional haemodynamic test OR tests”. Included papers were also examined to identify other studies of interest missed during the primary search.
Study selection and inclusion criteria
Articles enrolling at least 20 adult critically ill patients, written in English and published from 1st January 2000 to 31st December 2021 in indexed scientific journals, were considered. Editorials, commentaries, letters to the editor, opinion articles, reviews, and meeting abstracts were excluded. Studies enrolling paediatric or obstetric populations were excluded. References of selected papers, review articles, commentaries, and editorials on this topic were also reviewed to identify other studies of interest missed during the primary search. When multiple publications of the same research group/centre described potentially overlapping cohorts, the most recent publications were selected.
A fluid challenge was defined as an infusion of a definite quantity of fluid (expressed as a volume in mL or ml/kg) in a fixed time (expressed in minutes), whose outcome was defined as a change in one of the following haemodynamic variables above a predetermined threshold: CO, cardiac index (CI), SV, SV index (SVI), or surrogate of SV, i.e., velocity–time integral (VTI) in the left ventricular outflow tract and aortic blood flow (ABF), as assessed by transthoracic, transoesophageal echocardiography or oesophageal Doppler. We included studies adopting both a specific (i.e., Ringer lactate, saline, etc.) and a broad definition (i.e., crystalloids, colloids, etc.) of the fluid used for the fluid challenge. Studies adopting changes in systemic arterial pressure to define fluid responsiveness were excluded. Finally, we considered the predefined clinical reasons and triggers to start fluid challenge infusion.
Data extraction
Three couples of examiners independently evaluated titles and abstracts. The articles were then subdivided into three subgroups: “included” and “excluded” (if the two examiners agreed with the selection) or “uncertain” (in case of disagreement). In the case of “uncertain” classification, discrepancies were resolved by further examination performed by one of the three expert authors (A.M., X.M., or M.C.). We used a standardised electronic spreadsheet (Microsoft Excel, V 14.4.1; Microsoft, Redmond, WA) to extract data from all included studies, recording: the study setting (type of study, geographical area and time, where and when the study was carried out, and sample size), patient characteristics (gender, age, reason for admission, underlying diseases, ICU scores of severity, mode of ventilation, and inotropic/vasopressor support), criteria for haemodynamic instability, fluid challenge characteristics, pre- and post-fluid challenge haemodynamic variables. When necessary, the corresponding authors of the included studies were contacted to obtain missing data related to trial demographics, methods, and outcomes (Additional file 1 : Table S2).
Statistical analysis
Statistical analysis was conducted on the summary statistics described in the selected articles (e.g., means, medians, proportions) and, therefore, the statistical unit of observation for all the selected variables was the single study and not the patient. Due to the discrepancy between the overall patients enrolled in the trials over the two considered decaders, the comparisons were not weighted for study size.
Fluid challenge was the exposure variable, and clinical and haemodynamic characteristics were considered outcome variables. Descriptive statistics of individual studies used different statistical indicators for central tendency and variability, such as means and standard deviations (i.e., age, tidal volume, fluid responders, severity scores), whereas absolute and relative frequencies were adopted for qualitative variables. To show one indicator for the quantitative variables, we collected means with standard deviations (SD) or medians and inter-quartile ranges (IQR).
Student's t test or Mann–Whitney test in case of parametric or nonparametric distributions, respectively, were used to assess the difference in mean values between responders and non-responders.
Statistical analyses were conducted using GraphPad PRISM® 8 (GraphPad Software Inc., San Diego, CA, USA) and STATA®15 (StataCorp, College Station, TX, USA). For all comparisons, we considered p values < 0.05 significant.
The electronic search identified 3,963 potentially relevant studies. Figure 1 and Additional file 1 : Table S3 provide a detailed description of the selection process flow. After evaluating 160 full-text manuscripts, the inclusion criteria were met by 124 studies, 32 (25.8%) published in the period 2000–2010 and 92 (74.2%) in the period 2011–2021. Ten studies (8.1%) required revision by senior examiners because of disagreement regarding inclusion criteria between the initial examiners. We did not find any further relevant publications by reviewing the bibliography of the selected studies.
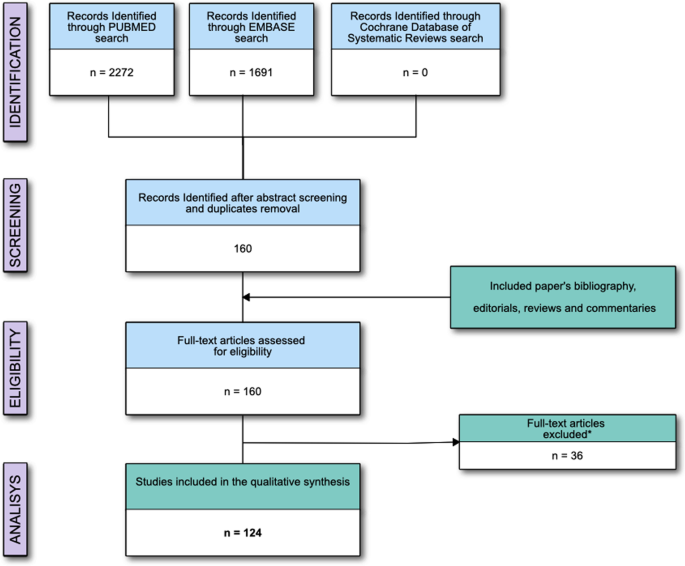
Flow of the studies; *Reasons for studies' exclusion are reported in the Supplementary materials
The general characteristics of the patients are reported in Table 1 . We included 6,086 patients, with a median (IQR) of 38 (30–59) patients enrolled in each study. Six studies (4.8%) [ 20 , 21 , 22 , 23 , 24 , 25 ] were retrospective, while the others were prospective. The median (IQR) period of enrolment [reported in 66 (52.8%) studies] was 12 (6–18) months. At baseline, 2,985 (49.0%) patients received norepinephrine, 179 (2.9%) dopamine, 416 (6.8%) dobutamine, and 177 (2.8%) epinephrine.
The reliability of a functional haemodynamic test in predicting fluid responsiveness was assessed in 46 (37.1%) studies. Comparing the two considered decades, no difference was found in the rate of FC administration [17 min (17–33) vs. 33 min (17–50); p = 0.39), in the percentage of fluid responders [52% (43–67) vs. 53% (45–60); p = 0.91], in the percentage of studies adopting crystalloids over colloids [63.6% vs. 67.9%; p = 1.00), or in the threshold of increase in CO or surrogates adopted to define fluid responsiveness (10% over 15%) [18.2% vs. 24.1%; p = 1.00).
Forty-four studies (35.4%) investigated the reliability of a dynamic index in predicting fluid responsiveness. Comparing the two considered decades, no differences were found in the rate of FC administration [17 min (17–25) vs. 29 min (13–33) p = 0.42), or in the rate of fluid responders [53% (41–62) vs. 50% (44–56) p = 0.81), or in the threshold of increase in CO or surrogates adopted to define fluid responsiveness (10% over 15%) (78.5% vs. 66.67 p = 0.42), as compared to studies in the decade 2000–2010. On the contrary, in the decade 2010-2021 we adopted more frequently crystalloids (21.4% vs. 60.0% p = 0.024).
Fluid challenge characteristics and haemodynamic monitoring
Overall, the included studies infused 6,333 fluid challenges. The median (IQR) proportion of fluid responders was 52 (44–62)% (Table 2 ).
In 19 studies (15.3%), the volume of the fluid challenge was reported in mL/kg, with a median (IQR) of 7 (6–8) mL/kg (Table 2 ). A fixed volume of 500 mL was administered in 95 (76.6)% of the included studies. The median (IQR) of the dispensed volume of fluid was 500 (500–500) mL, infused in a median (IQR) of 18 (11–30) min. Then, the median (IQR) infusion rate was 25 (17–33) mL/min.
CO/CI was used as target variables in 78 (62.9%) studies, while SV/SVI was used in 40 (32.2%) studies. The other six studies (4.8%) adopted SV surrogates (ABF in 4 studies and VTI in two studies). In 88 (70.9%) studies, the threshold adopted to define the fluid responsiveness was an increase of the considered variable ≥ 15% from baseline (Table 2 ).
Three studies (2.4%) [ 25 , 26 , 27 ] did not report the type of fluid used for the fluid challenge. Among the others, crystalloids were used in 68 (56.6)% studies, colloids in 52 (43.3) %, and blood in one (0.8)% (Table 2 ).
The majority of the studies [49 (39.5%)] used transpulmonary thermodilution/dye dilution calibrated haemodynamic monitoring; 22 (17.7%) studies adopted the pulmonary artery catheter monitoring. Echocardiography (either transthoracic or transoesophageal) was used in 31 (25.0)% of studies, and 5 (4.0%) used oesophageal doppler monitoring. Uncalibrated pulse wave analysis monitoring was used in the other 14 (11.2)% studies (Table 2 ). Finally, bioreactance was adopted in three studies (2.4%). Haemodynamic pre–post-fluid challenge variables in responders and non-responders populations are reported in Table 3 .
Trigger of fluid challenge administration.
Hypotension (i.e., systolic or mean arterial pressure below a fixed value or reduced by a fixed percentage from baseline) was used in 68 (62.4)% of studies. Oliguria (i.e. a drop in urine output below 0.5 mL/h for 2 or 3 consecutive hours) was used in 54 (49.5)% studies, skin mottling or peripheral hypoperfusion in 47 (43.1)% studies, tachycardia (i.e. an increase in heart rate above 100–110 beats/min) in 43 (39.4)%, the need for initiating the infusion or reducing the dose of vasoactive drugs in 41 (37.6)% studies, an increase in blood lactate in 34 (31.2)% studies, a diagnosis of sepsis/septic shock in 12 (11.0)% studies, and renal or hepatic dysfunction in seven (6.4)% studies. Fifteen studies (12.1%) did not report any trigger to start fluid challenge administration.
Comparison of publication periods 2011–2021 versus 2000–2010
The comparison between the 2000–2010 and 2011–2021 decades is reported in Table 4 . The percentage of fluid responders (52% for both the decades) and the volume infused (500 mL) were comparable. On the contrary, the infusion time was lower in the last decade (a median of 15 (10–30) min vs 30 (15–30) min, p = 0.03). Crystalloids were used in 61.9% of studies published between 2011–2021 and 34.3% in the 2000–2010 decade ( p = 0.007) (Figs. 2 and S1 in the Additional file 1 ).
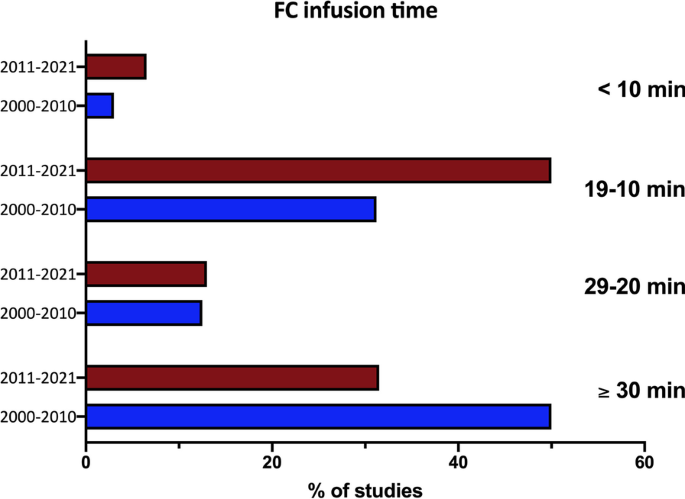
Percentage of studies in the two decades adopting different infusion timings. Fluid challenge, fluid challenge
CO/CI was used in 67% of the studies published in 2011–2021 and in 60% of those published in 2000–2010 ( p = 0.51). The threshold adopted was an increase in CO or surrogates ≥ 15% in 67.4% of the studies of the 2011–2021 decade and in 81.2% of the studies published in 2000–2010 ( p = 0.17) (Additional file 1 : Figure S1).
The results of this review, including research studies investigating the fluid challenge effect in critically ill adult patients receiving haemodynamic monitoring, may be summarised as follows: 1) fluid challenge is usually performed infusing a bolus of 500 mL of fluid, most often a crystalloid, in less than 20 min; 2) the response to fluid challenge is usually defined as a CI or CO increase ≥ 15% as compared to baseline; 3) positive response to fluid challenge is reported in about 50% of ICU patients; 4) the most common trigger for fluid challenge administration is usually the occurrence of hypotension, followed by oliguria and clinical signs of hypoperfusion; 5) the comparison between the 2000–2010 and 2011–2021 decades of publication showed no difference in the percentage of fluid responders (52% on average for both the decades), the volume infused (500 ml), and the criteria defining fluid responsiveness. On the contrary, compared to the 2000–2010 decade, in the period 2011–2021, the fluid challenge infusion time was lower, and crystalloids were more frequently used.
Fluid challenge characteristics
Among the included studies, the fluid challenge usually consisted of a median volume of 500 mL administered over a 20-min period and defined as a positive response by an increase ≥ 15% of CO or surrogate. These characteristics and responsiveness definition are to be considered good practice, for the response of CO to a fluid bolus is poorly followed by the simultaneous changes in arterial pressure [ 28 , 29 ] or heart rate [ 30 ]. However, this is not the case in clinical practice, where the fluid challenge effect is often assessed by a rise in arterial blood pressure [ 16 ].
Interestingly, 500 mL was also the median volume fluid challenge used in the FENICE study (an observational study including 311 centres across 46 countries) [ 16 ], whereas a fluid challenge of 250 mL is usually adopted in high-risk surgical patients undergoing goal-directed therapy optimisation [ 31 ]. The use of large volumes for fluid challenge optimisation should be balanced to the detrimental risk of fluid overload [ 9 ], primarily if safety limits (i.e. , increase in CVP) dynamically indicate fluid non-responsiveness are rarely used [ 19 ]. Since fluid challenge volume should be at least 4 mL/kg [ 32 ], smaller fluid challenge volumes may be considered for repetitive tests.
Moreover, the FENICE study reported a median of 24 min of infusion time and a rate of 17 mL/min [ 16 ]. Hence, the volume and rate of administration seem comparable between clinical and research settings. On the contrary, the infusion time was lower in the last decade (a median of 15 min vs 30 min, p = 0.03), indicating a trend towards the increase in the infusion rate in more recent studies. This global inception cohort study evaluated the clinical use of the fluid challenge in daily practice, whereas our review considered only research papers adopting the fluid challenge as a part of a protocol, limiting the comparison with the results of the FENICE. Moreover, in contrast with a previous metanalysis, including ICU studies up to 2014 [ 19 ], crystalloids are used in most studies. Crystalloids have been used in two-thirds of the studies from 2011 to 2021, compared to one-third from 2000 to 2010. These data indicate an alignment between research studies, recent guidelines, and metanalyses [ 13 , 14 ].
Limitations
Limitations of our review have to be considered when extrapolating the results to clinical practice. First, the present study does not report any outcome endpoints. A recent large randomised-controlled trial showed no difference in mortality rate among ICU patients receiving different fluid bolus infusion rates [ 33 ]. However, the faster rate adopted in this study (5.5 mL/min) is below the median rate found in the studies included in the present review (25 mL/min) [ 33 ]. The administration of aliquots of fluids at a slow rate should not probably be indicated as a fluid challenge. Moreover, all the included studies are research papers whose aim was to evaluate the haemodynamic changes after the fluid challenge infusion or assess the reliability of indexes or functional haemodynamic tests in predicting the response to a fluid challenge. We did not include studies on the fluid challenge clinical use in ICU patients.
Another potential source of bias is related to the different haemodynamic monitorings used to assess fluid challenge responsiveness. When considering the median cut-off value identifying responders from non-responders, the accuracy of measurement of the changes in CO, or its surrogates, is undoubtedly relevant. Additionally, the reliability of different monitorings in tracking the dynamic trends of CO may not be consistent and may be below the boundaries of accuracy and precision of the Critchley–Critchley criteria [ 34 ]. Hence, the reproducibility of CO measurements obtained by the different monitoring systems may be limited. Moreover, cut-off values and measurement techniques potentially induce heterogeneity in response to the fluid challenge administration. As confirmed, responders ranged from 23 to 100% across the included studies (Table 2 ). The use of echocardiography is associated with high proportions of fluid responders compared to other haemodynamic monitoring devices. The operator-dependent bias may affect the evaluation of SV changes after fluid challenge.
We excluded studies in which the fluid challenge response has been assessed without haemodynamic monitoring and, hence assessing changes in systemic arterial pressures, potentially limiting the whole comparability of the technique in the two considered decades. Finally, the overall number of patients enrolled in the trials of the two considered decades was considerably different. This could bias the comparisons between the two groups if weighted for study size.
This systematic review, including research studies on fluid challenge use in critically ill adult patients receiving haemodynamic monitoring, showed a positive response in 52% of the patients. This test was usually performed infusing a bolus of 500 mL fluid, more often a crystalloid, in less than 20 min, and fluid responsiveness was generally indicated as a CI or CO increase ≥ 15% compared to baseline. Fluid challenge administration is usually triggered by hypotension. In the 2011–2021, the infusion time was shorter, and crystalloids were more frequently used than in the 2000–2010 decade.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Cardiac index
Stroke volume index
Cardiac output
Stroke volume
Intensive care unit
Central venous pressure
Velocity–time integral in the left ventricular outflow tract
Aortic blood flow
Myburgh JA, Mythen MG. Resuscitation fluids. N Engl J Med. 2013;369:1243–51.
Article CAS PubMed Google Scholar
Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, et al. Consensus on circulatory shock and hemodynamic monitoring. Task force of the european society of intensive care medicine. Intensive Care Med. 2014;40:1795–815.
Article PubMed PubMed Central Google Scholar
Vincent JL, De Backer D. Circulatory shock. N Engl J Med. 2013;369:1726–34.
Magder S. Bench-to-bedside review: an approach to hemodynamic monitoring–guyton at the bedside. Crit Care. 2012;16:236.
Cecconi M, Parsons AK, Rhodes A. What is a fluid challenge? Curr Opin Crit Care. 2011;17:290–5.
Article PubMed Google Scholar
Marik PE, Monnet X, Teboul JL. Hemodynamic parameters to guide fluid therapy. Ann Intensive Care. 2011;1:1.
Monnet X, Marik PE, Teboul JL. Prediction of fluid responsiveness: an update. Ann Intensive Care. 2016;6:111.
Hjortrup PB, Haase N, Bundgaard H, Thomsen SL, Winding R, Pettila V, et al. Restricting volumes of resuscitation fluid in adults with septic shock after initial management: the classic randomised, parallel-group, multicentre feasibility trial. Intensive Care Med. 2016;42:1695–705.
Marik PE, Linde-Zwirble WT, Bittner EA, Sahatjian J, Hansell D. Fluid administration in severe sepsis and septic shock, patterns and outcomes: An analysis of a large national database. Intensive Care Med. 2017;43:625–32.
Messina A, Palandri C, De Rosa S, Danzi V, Bonaldi E, Montagnini C, et al.: Pharmacodynamic analysis of a fluid challenge with 4 mL kg(-1) over 10 or 20 min: A multicenter cross-over randomized clinical trial. J Clin Monit Comput 2021
Aya HD, Rhodes A, Chis Ster I, Fletcher N, Grounds RM, Cecconi M. Hemodynamic effect of different doses of fluids for a fluid challenge: a quasi-randomized controlled study. Crit Care Med. 2017;45:e161–8.
Messina A, Sotgiu G, Saderi L, Cammarota G, Capuano L, Colombo D, et al.: Does the definition of fluid responsiveness affect passive leg raising reliability? A methodological ancillary analysis from a multicentric study. Minerva Anestesiol 2021
Lewis SR, Pritchard MW, Evans DJ, Butler AR, Alderson P, Smith AF, et al. Colloids versus crystalloids for fluid resuscitation in critically ill people. Cochrane Database Syst Rev. 2018;8:CD000567.
PubMed Google Scholar
Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47:1181–247.
Finfer S, Liu B, Taylor C, Bellomo R, Billot L, Cook D, et al. Resuscitation fluid use in critically ill adults: an international cross-sectional study in 391 intensive care units. Crit Care. 2010;14:R185.
Cecconi M, Hofer C, Teboul JL, Pettila V, Wilkman E, Molnar Z, et al. Fluid challenges in intensive care: The fenice study: a global inception cohort study. Intensive Care Med. 2015;41:1529–37.
Messina A, Longhini F, Coppo C, Pagni A, Lungu R, Ronco C, et al.: Use of the fluid challenge in critically ill adult patients: a systematic review. Anesth Analg 2017
Messina A, Dell’Anna A, Baggiani M, Torrini F, Maresca GM, Bennett V, et al. Functional hemodynamic tests: A systematic review and a metanalysis on the reliability of the end-expiratory occlusion test and of the mini-fluid challenge in predicting fluid responsiveness. Crit Care. 2019;23:264.
Messina A, Longhini F, Coppo C, Pagni A, Lungu R, Ronco C, et al. Use of the fluid challenge in critically ill adult patients: a systematic review. Anesth Analg. 2017;125:1532–43.
Vaquer S, Chemla D, Teboul JL, Ahmad U, Cipriani F, Oliva JC, et al. Volume infusion markedly increases femoral dp/dtmax in fluid-responsive patients only. Crit Care Med. 2020;48:1487–93.
Monge Garcia MI, Guijo Gonzalez P, Gracia Romero M, Gil Cano A, Oscier C, Rhodes A, et al. Effects of fluid administration on arterial load in septic shock patients. Intensive Care Med. 2015;41:1247–55.
Osman D, Ridel C, Ray P, Monnet X, Anguel N, Richard C, et al. Cardiac filling pressures are not appropriate to predict hemodynamic response to volume challenge. Crit Care Med. 2007;35:64–8.
Velissaris D, Pierrakos C, Scolletta S, De Backer D, Vincent JL. High mixed venous oxygen saturation levels do not exclude fluid responsiveness in critically ill septic patients. Crit Care. 2011;15:R177.
Hu B, Xiang H, Liang H, Yu L, Xu T, Yang JH, et al. Assessment effect of central venous pressure in fluid resuscitation in the patients with shock: a multi-center retrospective research. Chin Med J (Engl). 2013;126:1844–9.
Google Scholar
De Santis P, De Fazio C, Franchi F, Bond O, Vincent JL, Creteur J, et al.: Incoherence between systemic hemodynamic and microcirculatory response to fluid challenge in critically ill patients. J Clin Med 2021;10
Cecconi M, Aya HD, Geisen M, Ebm C, Fletcher N, Grounds RM, et al. Changes in the mean systemic filling pressure during a fluid challenge in postsurgical intensive care patients. Intensive Care Med. 2013;39:1299–305.
Pranskunas A, Koopmans M, Koetsier PM, Pilvinis V, Boerma EC. Microcirculatory blood flow as a monitoring to select icu patients eligible for fluid therapy. Intensive Care Med. 2013;39:612–9.
Monnet X, Letierce A, Hamzaoui O, Chemla D, Anguel N, Osman D, et al. Arterial pressure allows monitoring the changes in cardiac output induced by volume expansion but not by norepinephrine. Crit Care Med. 2011;39:1394–9.
Pierrakos C, Velissaris D, Scolletta S, Heenen S, De Backer D, Vincent JL. Can changes in arterial pressure be used to detect changes in cardiac index during fluid challenge in patients with septic shock? Intensive Care Med. 2012;38:422–8.
Ait-Hamou Z, Teboul JL, Anguel N, Monnet X. How to detect a positive response to a fluid bolus when cardiac output is not measured? Ann Intensive Care. 2019;9:138.
Messina A, Pelaia C, Bruni A, Garofalo E, Bonicolini E, Longhini F, et al.: Fluid challenge during anesthesia: A systematic review and meta-analysis. Anesth Analg 2018
Aya HD, Ster IC, Fletcher N, Grounds RM, Rhodes A, Cecconi M. Pharmacodynamic analysis of a fluid challenge. Crit Care Med. 2016;44:880–91.
Zampieri FG, Machado FR, Biondi RS, Freitas FGR, Veiga VC, Figueiredo RC, et al. Effect of slower vs faster intravenous fluid bolus rates on mortality in critically ill patients: the basics randomized clinical trial. JAMA. 2021;326:830–8.
Critchley LA, Critchley JA. A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput. 1999;15:85–91.
Mahjoub Y, Touzeau J, Airapetian N, Lorne E, Hijazi M, Zogheib E, et al. The passive leg-raising maneuver cannot accurately predict fluid responsiveness in patients with intra-abdominal hypertension. Crit Care Med. 2010;38:1824–9.
Preau S, Dewavrin F, Soland V, Bortolotti P, Colling D, Chagnon JL, et al. Hemodynamic changes during a deep inspiration maneuver predict fluid responsiveness in spontaneously breathing patients. Cardiol Res Pract. 2012;2012: 191807.
Feissel M, Michard F, Faller JP, Teboul JL. The respiratory variation in inferior vena cava diameter as a guide to fluid therapy. Intensive Care Med. 2004;30:1834–7.
Caille V, Jabot J, Belliard G, Charron C, Jardin F, Vieillard-Baron A. Hemodynamic effects of passive leg raising: an echocardiographic study in patients with shock. Intensive Care Med. 2008;34:1239–45.
Marik PE, Levitov A, Young A, Andrews L. The use of bioreactance and carotid doppler to determine volume responsiveness and blood flow redistribution following passive leg raising in hemodynamically unstable patients. Chest. 2013;143:364–70.
Mahjoub Y, Benoit-Fallet H, Airapetian N, Lorne E, Levrard M, Seydi AA, et al. Improvement of left ventricular relaxation as assessed by tissue doppler imaging in fluid-responsive critically ill septic patients. Intensive Care Med. 2012;38:1461–70.
Wyffels PA, Durnez PJ, Helderweirt J, Stockman WM, De Kegel D. Ventilation-induced plethysmographic variations predict fluid responsiveness in ventilated postoperative cardiac surgery patients. Anesth Analg. 2007;105:448–52.
Wu Y, Zhou S, Zhou Z, Liu B. A 10-second fluid challenge guided by transthoracic echocardiography can predict fluid responsiveness. Crit Care. 2014;18:R108.
Jozwiak M, Depret F, Teboul JL, Alphonsine JE, Lai C, Richard C, et al. Predicting fluid responsiveness in critically ill patients by using combined end-expiratory and end-inspiratory occlusions with echocardiography. Crit Care Med. 2017;45:e1131–8.
Fellahi JL, Fischer MO, Rebet O, Massetti M, Gerard JL, Hanouz JL. A comparison of endotracheal bioimpedance cardiography and transpulmonary thermodilution in cardiac surgery patients. J Cardiothorac Vasc Anesth. 2012;26:217–22.
Monnet X, Osman D, Ridel C, Lamia B, Richard C, Teboul JL. Predicting volume responsiveness by using the end-expiratory occlusion in mechanically ventilated intensive care unit patients. Crit Care Med. 2009;37:951–6.
Smorenberg A, Cherpanath TGV, Geerts BF, de Wilde RBP, Jansen JRC, Maas JJ, et al. A mini-fluid challenge of 150ml predicts fluid responsiveness using modelflow(r) pulse contour cardiac output directly after cardiac surgery. J Clin Anesth. 2018;46:17–22.
Monnet X, Bleibtreu A, Ferre A, Dres M, Gharbi R, Richard C, et al. Passive leg-raising and end-expiratory occlusion tests perform better than pulse pressure variation in patients with low respiratory system compliance. Crit Care Med. 2012;40:152–7.
Muller L, Toumi M, Bousquet PJ, Riu-Poulenc B, Louart G, Candela D, et al. An increase in aortic blood flow after an infusion of 100 ml colloid over 1 minute can predict fluid responsiveness: The mini-fluid challenge study. Anesthesiology. 2011;115:541–7.
Chen YH, Lai YJ, Huang CY, Lin HL, Huang CC. Effects of positive end-expiratory pressure on the predictability of fluid responsiveness in acute respiratory distress syndrome patients. Sci Rep. 2021;11:10186.
Article CAS PubMed PubMed Central Google Scholar
Monge Garcia MI, Gil Cano A, Diaz Monrove JC. Arterial pressure changes during the valsalva maneuver to predict fluid responsiveness in spontaneously breathing patients. Intensive Care Med. 2009;35:77–84.
Natalini G, Rosano A, Taranto M, Faggian B, Vittorielli E, Bernardini A. Arterial versus plethysmographic dynamic indices to test responsiveness for testing fluid administration in hypotensive patients: a clinical trial. Anesth Analg. 2006;103:1478–84.
Messina A, Romano SM, Ozdemirkan A, Persona P, Tarquini R, Cammarota G, et al.: Multivariable haemodynamic approach to predict the fluid challenge response: a multicentre cohort study. Eur J Anaesthesiol 2020
Mahjoub Y, Pila C, Friggeri A, Zogheib E, Lobjoie E, Tinturier F, et al. Assessing fluid responsiveness in critically ill patients: False-positive pulse pressure variation is detected by doppler echocardiographic evaluation of the right ventricle. Crit Care Med. 2009;37:2570–5.
Taccheri T, Gavelli F, Teboul JL, Shi R, Monnet X. Do changes in pulse pressure variation and inferior vena cava distensibility during passive leg raising and tidal volume challenge detect preload responsiveness in case of low tidal volume ventilation? Crit Care. 2021;25:110.
Fischer MO, Coucoravas J, Truong J, Zhu L, Gerard JL, Hanouz JL, et al. Assessment of changes in cardiac index and fluid responsiveness: a comparison of nexfin and transpulmonary thermodilution. Acta Anaesthesiol Scand. 2013;57:704–12.
Kaur KB, Nakra M, Mangal V, Singh S, Taank P, Marwah V. Comparative evaluation of stroke volume variation and inferior vena cava distensibility index for prediction of fluid responsiveness in mechanically ventilated patients. Ann Card Anaesth. 2021;24:327–32.
PubMed PubMed Central Google Scholar
Vistisen ST, Struijk JJ, Larsson A. Automated pre-ejection period variation indexed to tidal volume predicts fluid responsiveness after cardiac surgery. Acta Anaesthesiol Scand. 2009;53:534–42.
Biasucci DG, Cina A, Calabrese M, Antoniucci ME, Cavaliere C, Bevilacqua F, et al. Size and shape of the inferior vena cava before and after a fluid challenge: a pilot study. Minerva Anestesiol. 2019;85:514–21.
Kupersztych-Hagege E, Teboul JL, Artigas A, Talbot A, Sabatier C, Richard C, et al. Bioreactance is not reliable for estimating cardiac output and the effects of passive leg raising in critically ill patients. Br J Anaesth. 2013;111:961–6.
Gavaud A, Nguyen LS, Caubel A, Grillet G, Donal E, Belliard G. Respiratory variability of pulmonary velocity-time integral as a new gauge of fluid responsiveness for mechanically ventilated patients in the icu. Crit Care Med. 2019;47:e310–6.
Monge Garcia MI, Gil Cano A, Diaz Monrove JC. Brachial artery peak velocity variation to predict fluid responsiveness in mechanically ventilated patients. Crit Care. 2009;13:R142.
Depret F, Jozwiak M, Teboul JL, Alphonsine JE, Richard C, Monnet X. Esophageal doppler can predict fluid responsiveness through end-expiratory and end-inspiratory occlusion tests. Crit Care Med. 2019;47:e96–102.
Lakhal K, Ehrmann S, Benzekri-Lefevre D, Runge I, Legras A, Dequin PF, et al. Brachial cuff measurements of blood pressure during passive leg raising for fluid responsiveness prediction. Ann Fr Anesth Reanim. 2012;31:e67-72.
Messina A, Colombo D, Barra FL, Cammarota G, De Mattei G, Longhini F, et al. Sigh maneuver to enhance assessment of fluid responsiveness during pressure support ventilation. Crit Care. 2019;23:31.
Soubrier S, Saulnier F, Hubert H, Delour P, Lenci H, Onimus T, et al. Can dynamic indicators help the prediction of fluid responsiveness in spontaneously breathing critically ill patients? Intensive Care Med. 2007;33:1117–24.
Vistisen ST, Krog MB, Elkmann T, Vallentin MF, Scheeren TWL, Solling C. Extrasystoles for fluid responsiveness prediction in critically ill patients. J Intensive Care. 2018;6:52.
Fellahi JL, Fischer MO, Dalbera A, Massetti M, Gerard JL, Hanouz JL. Can endotracheal bioimpedance cardiography assess hemodynamic response to passive leg raising following cardiac surgery? Ann Intensive Care. 2012;2:26.
Xu B, Yang X, Wang C, Jiang W, Weng L, Hu X, et al. Changes of central venous oxygen saturation define fluid responsiveness in patients with septic shock: a prospective observational study. J Crit Care. 2017;38:13–9.
Preau S, Bortolotti P, Colling D, Dewavrin F, Colas V, Voisin B, et al. Diagnostic accuracy of the inferior vena cava collapsibility to predict fluid responsiveness in spontaneously breathing patients with sepsis and acute circulatory failure. Crit Care Med. 2017;45:e290–7.
Lakhal K, Ehrmann S, Runge I, Benzekri-Lefevre D, Legras A, Dequin PF, et al. Central venous pressure measurements improve the accuracy of leg raising-induced change in pulse pressure to predict fluid responsiveness. Intensive Care Med. 2010;36:940–8.
Machare-Delgado E, Decaro M, Marik PE. Inferior vena cava variation compared to pulse contour analysis as predictors of fluid responsiveness: a prospective cohort study. J Intensive Care Med. 2011;26:116–24.
Oliveira-Costa CD, Friedman G, Vieira SR, Fialkow L. Pulse pressure variation and prediction of fluid responsiveness in patients ventilated with low tidal volumes. Clinics (Sao Paulo). 2012;67:773–8.
Article Google Scholar
Monnet X, Julien F, Ait-Hamou N, Lequoy M, Gosset C, Jozwiak M, et al. Lactate and venoarterial carbon dioxide difference/arterial-venous oxygen difference ratio, but not central venous oxygen saturation, predict increase in oxygen consumption in fluid responders. Crit Care Med. 2013;41:1412–20.
Monnet X, Chemla D, Osman D, Anguel N, Richard C, Pinsky MR, et al. Measuring aortic diameter improves accuracy of esophageal doppler in assessing fluid responsiveness. Crit Care Med. 2007;35:477–82.
Monnet X, Jabot J, Maizel J, Richard C, Teboul JL. Norepinephrine increases cardiac preload and reduces preload dependency assessed by passive leg raising in septic shock patients. Crit Care Med. 2011;39:689–94.
Ishihara H, Hashiba E, Okawa H, Saito J, Kasai T, Tsubo T. Neither dynamic, static, nor volumetric variables can accurately predict fluid responsiveness early after abdominothoracic esophagectomy. Perioper Med (Lond). 2013;2:3.
Muller L, Louart G, Bousquet PJ, Candela D, Zoric L, de La Coussaye JE, et al. The influence of the airway driving pressure on pulsed pressure variation as a predictor of fluid responsiveness. Intensive Care Med. 2010;36:496–503.
Monge Garcia MI, Gil Cano A, Gracia Romero M, Monterroso Pintado R, Perez Madueno V, Diaz Monrove JC. Non-invasive assessment of fluid responsiveness by changes in partial end-tidal co2 pressure during a passive leg-raising maneuver. Ann Intensive Care. 2012;2:9.
Muller L, Louart G, Bengler C, Fabbro-Peray P, Carr J, Ripart J, et al. The intrathoracic blood volume index as an indicator of fluid responsiveness in critically ill patients with acute circulatory failure: a comparison with central venous pressure. Anesth Analg. 2008;107:607–13.
Luzi A, Marty P, Mari A, Conil JM, Geeraerts T, Lepage B, et al. Noninvasive assessment of hemodynamic response to a fluid challenge using femoral doppler in critically ill ventilated patients. J Crit Care. 2013;28:902–7.
Heenen S, De Backer D, Vincent JL. How can the response to volume expansion in patients with spontaneous respiratory movements be predicted? Crit Care. 2006;10:R102.
Dong ZZ, Fang Q, Zheng X, Shi H. Passive leg raising as an indicator of fluid responsiveness in patients with severe sepsis. World J Emerg Med. 2012;3:191–6.
De Backer D, Heenen S, Piagnerelli M, Koch M, Vincent JL. Pulse pressure variations to predict fluid responsiveness: influence of tidal volume. Intensive Care Med. 2005;31:517–23.
Jabot J, Teboul JL, Richard C, Monnet X. Passive leg raising for predicting fluid responsiveness: importance of the postural change. Intensive Care Med. 2009;35:85–90.
Le Dorze M, Huche F, Coelembier C, Rabuel C, Payen D. Impact of fluid challenge increase in cardiac output on the relationship between systemic and cerebral hemodynamics in severe sepsis compared to brain injury and controls. Ann Intensive Care. 2018;8:74.
Préau S, Saulnier F, Dewavrin F, Durocher A, Chagnon JL. Passive leg raising is predictive of fluid responsiveness in spontaneously breathing patients with severe sepsis or acute pancreatitis. Crit Care Med. 2010;38:819–25.
Wu J, Wang Z, Wang T, Yu T, Yuan J, Zhang Q, et al. Evaluation of the fluid responsiveness in patients with septic shock by ultrasound plus the passive leg raising test. J Surg Res. 2018;224:207–14.
Monnet X, Rienzo M, Osman D, Anguel N, Richard C, Pinsky MR, et al. Passive leg raising predicts fluid responsiveness in the critically ill. Crit Care Med. 2006;34:1402–7.
Si X, Cao DY, Chen J, Wu JF, Liu ZM, Xu HL, et al. Effect of systolic cardiac function on passive leg raising for predicting fluid responsiveness: a prospective observational study. Chin Med J (Engl). 2018;131:253–61.
Pouska J, Tegl V, Astapenko D, Cerny V, Lehmann C, Benes J. Impact of intravenous fluid challenge infusion time on macrocirculation and endothelial glycocalyx in surgical and critically ill patients. Biomed Res Int. 2018;2018:8925345.
Article PubMed PubMed Central CAS Google Scholar
Monnet X, Guerin L, Jozwiak M, Bataille A, Julien F, Richard C, et al. Pleth variability index is a weak predictor of fluid responsiveness in patients receiving norepinephrine. Br J Anaesth. 2013;110:207–13.
Xu J, Peng X, Pan C, Cai S, Zhang X, Xue M, et al. Fluid responsiveness predicted by transcutaneous partial pressure of oxygen in patients with circulatory failure: a prospective study. Ann Intensive Care. 2017;7:56.
Loupec T, Nanadoumgar H, Frasca D, Petitpas F, Laksiri L, Baudouin D, et al. Pleth variability index predicts fluid responsiveness in critically ill patients. Crit Care Med. 2011;39:294–9.
Soussi S, Vallee F, Roquet F, Bevilacqua V, Benyamina M, Ferry A, et al. Measurement of oxygen consumption variations in critically ill burns patients: are the fick method and indirect calorimetry interchangeable? Shock. 2017;48:532–8.
Monnet X, Dres M, Ferre A, Le Teuff G, Jozwiak M, Bleibtreu A, et al. Prediction of fluid responsiveness by a continuous non-invasive assessment of arterial pressure in critically ill patients: comparison with four other dynamic indices. Br J Anaesth. 2012;109:330–8.
Mallat J, Lemyze M, Meddour M, Pepy F, Gasan G, Barrailler S, et al. Ratios of central venous-to-arterial carbon dioxide content or tension to arteriovenous oxygen content are better markers of global anaerobic metabolism than lactate in septic shock patients. Ann Intensive Care. 2016;6:10.
Huang CC, Fu JY, Hu HC, Kao KC, Chen NH, Hsieh MJ, et al. Prediction of fluid responsiveness in acute respiratory distress syndrome patients ventilated with low tidal volume and high positive end-expiratory pressure. Crit Care Med. 2008;36:2810–6.
Khwannimit B, Bhurayanontachai R. Prediction of fluid responsiveness in septic shock patients: comparing stroke volume variation by flotrac/vigileo and automated pulse pressure variation. Eur J Anaesthesiol. 2012;29:64–9.
Hamimy W, Mukhtar A, Zaghloul A, Salem M. Comparing transesophageal doppler corrected systolic flow time versus central venous pressure as a guide for fluid resuscitation in septic shock. Egypt J Anaesthesia. 2019;32:181–7.
Fischer MO, Pelissier A, Bohadana D, Gerard JL, Hanouz JL, Fellahi JL. Prediction of responsiveness to an intravenous fluid challenge in patients after cardiac surgery with cardiopulmonary bypass: a comparison between arterial pulse pressure variation and digital plethysmographic variability index. J Cardiothorac Vasc Anesth. 2013;27:1087–93.
Liu Y, Wei LQ, Li GQ, Yu X, Li GF, Li YM. Pulse pressure variation adjusted by respiratory changes in pleural pressure, rather than by tidal volume, reliably predicts fluid responsiveness in patients with acute respiratory distress syndrome. Crit Care Med. 2016;44:342–51.
Kramer A, Zygun D, Hawes H, Easton P, Ferland A. Pulse pressure variation predicts fluid responsiveness following coronary artery bypass surgery. Chest. 2004;126:1563–8.
Guerin L, Teboul JL, Persichini R, Dres M, Richard C, Monnet X. Effects of passive leg raising and volume expansion on mean systemic pressure and venous return in shock in humans. Crit Care. 2015;19:411.
Yazigi A, Khoury E, Hlais S, Madi-Jebara S, Haddad F, Hayek G, et al. Pulse pressure variation predicts fluid responsiveness in elderly patients after coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth. 2012;26:387–90.
Airapetian N, Maizel J, Alyamani O, Mahjoub Y, Lorne E, Levrard M, et al. Does inferior vena cava respiratory variability predict fluid responsiveness in spontaneously breathing patients? Crit Care. 2015;19:400.
Wyler von Ballmoos M, Takala J, Roeck M, Porta F, Tueller D, Ganter CC, et al. Pulse-pressure variation and hemodynamic response in patients with elevated pulmonary artery pressure: a clinical study. Crit Care. 2010;14:R111.
Messina A, Colombo D, Cammarota G, De Lucia M, Cecconi M, Antonelli M, et al. Patient-ventilator asynchrony affects pulse pressure variation prediction of fluid responsiveness. J Crit Care. 2015;30:1067–71.
Michard F, Boussat S, Chemla D, Anguel N, Mercat A, Lecarpentier Y, et al. Relation between respiratory changes in arterial pulse pressure and fluid responsiveness in septic patients with acute circulatory failure. Am J Respir Crit Care Med. 2000;162:134–8.
Cecconi M, Monge Garcia MI, Gracia Romero M, Mellinghoff J, Caliandro F, Grounds RM, et al. The use of pulse pressure variation and stroke volume variation in spontaneously breathing patients to assess dynamic arterial elastance and to predict arterial pressure response to fluid administration. Anesth Analg. 2015;120:76–84.
Lakhal K, Ehrmann S, Benzekri-Lefevre D, Runge I, Legras A, Dequin PF, et al. Respiratory pulse pressure variation fails to predict fluid responsiveness in acute respiratory distress syndrome. Crit Care. 2011;15:R85.
Soliman RA, Samir S, el Naggar A, El Dehely K. Stroke volume variation compared with pulse pressure variation and cardiac index changes for prediction of fluid responsiveness in mechanically ventilated patients. The Egypt J Crit Care Med. 2015;3:9–16.
Muller L, Bobbia X, Toumi M, Louart G, Molinari N, Ragonnet B, et al. Respiratory variations of inferior vena cava diameter to predict fluid responsiveness in spontaneously breathing patients with acute circulatory failure: Need for a cautious use. Crit Care. 2012;16:R188.
Nunes TS, Ladeira RT, Bafi AT, de Azevedo LC, Machado FR, Freitas FG. Duration of hemodynamic effects of crystalloids in patients with circulatory shock after initial resuscitation. Ann Intensive Care. 2014;4:25.
Giraud R, Siegenthaler N, Gayet-Ageron A, Combescure C, Romand JA, Bendjelid K. Scvo(2) as a marker to define fluid responsiveness. J Trauma. 2011;70:802–7.
CAS PubMed Google Scholar
Lakhal K, Ehrmann S, Perrotin D, Wolff M, Boulain T. Fluid challenge: Tracking changes in cardiac output with blood pressure monitoring (invasive or non-invasive). Intensive Care Med. 2013;39:1953–62.
Suehiro K, Rinka H, Ishikawa J, Fuke A, Arimoto H, Miyaichi T. Stroke volume variation as a predictor of fluid responsiveness in patients undergoing airway pressure release ventilation. Anaesth Intensive Care. 2012;40:767–72.
Perner A, Faber T. Stroke volume variation does not predict fluid responsiveness in patients with septic shock on pressure support ventilation. Acta Anaesthesiol Scand. 2006;50:1068–73.
Smorenberg A, Lust EJ, Beishuizen A, Meijer JH, Verdaasdonk RM, Groeneveld AB. Systolic time intervals vs invasive predictors of fluid responsiveness after coronary artery bypass surgery. Eur J Cardiothorac Surg. 2013;44:891–7.
Monnet X, Picard F, Lidzborski E, Mesnil M, Duranteau J, Richard C, et al. The estimation of cardiac output by the nexfin device is of poor reliability for tracking the effects of a fluid challenge. Crit Care. 2012;16:R212.
Schnell D, Camous L, Guyomarc’h S, Duranteau J, Canet E, Gery P, et al. Renal perfusion assessment by renal doppler during fluid challenge in sepsis. Crit Care Med. 2013;41:1214–20.
Yonis H, Bitker L, Aublanc M, Perinel Ragey S, Riad Z, Lissonde F, et al. Change in cardiac output during trendelenburg maneuver is a reliable predictor of fluid responsiveness in patients with acute respiratory distress syndrome in the prone position under protective ventilation. Crit Care. 2017;21:295.
Xiao-ting W, Hua Z, Da-wei L, Hong-min Z, Huai-wu H, Yun L, et al. Changes in end-tidal co2 could predict fluid responsiveness in the passive leg raising test but not in the mini-fluid challenge test: a prospective and observational study. J Crit Care. 2015;30:1061–6.
Elsayed AI, Selim KA, Zaghla HE, Mowafy HE, Fakher MA. Comparison of changes in ppv using a tidal volume challenge with a passive leg raising test to predict fluid responsiveness in patients ventilated using low tidal volume. Indian J Crit Care Med. 2021;25:685–90.
Biais M, Vidil L, Sarrabay P, Cottenceau V, Revel P, Sztark F. Changes in stroke volume induced by passive leg raising in spontaneously breathing patients: Comparison between echocardiography and vigileo/flotrac device. Crit Care. 2009;13:R195.
Bataille B, de Selle J, Moussot PE, Marty P, Silva S, Cocquet P. Machine learning methods to improve bedside fluid responsiveness prediction in severe sepsis or septic shock: an observational study. Br J Anaesth. 2021;126:826–34.
Mallat J, Meddour M, Durville E, Lemyze M, Pepy F, Temime J, et al. Decrease in pulse pressure and stroke volume variations after mini-fluid challenge accurately predicts fluid responsiveness. Br J Anaesth. 2015;115:449–56.
Maizel J, Airapetian N, Lorne E, Tribouilloy C, Massy Z, Slama M. Diagnosis of central hypovolemia by using passive leg raising. Intensive Care Med. 2007;33:1133–8.
Kumar N, Malviya D, Nath SS, Rastogi S, Upadhyay V. Comparison of the efficacy of different arterial waveform-derived variables (pulse pressure variation, stroke volume variation, systolic pressure variation) for fluid responsiveness in hemodynamically unstable mechanically ventilated critically ill patients. Indian J Crit Care Med. 2021;25:48–53.
Lamia B, Ochagavia A, Monnet X, Chemla D, Richard C, Teboul JL. Echocardiographic prediction of volume responsiveness in critically ill patients with spontaneously breathing activity. Intensive Care Med. 2007;33:1125–32.
Braun F, Proenca M, Wendler A, Sola J, Lemay M, Thiran JP, et al. Noninvasive measurement of stroke volume changes in critically ill patients by means of electrical impedance tomography. J Clin Monit Comput. 2020;34:903–11.
Silva E, De Backer D, Creteur J, Vincent JL. Effects of fluid challenge on gastric mucosal pco2 in septic patients. Intensive Care Med. 2004;30:423–9.
Huette P, Abou-Arab O, Longrois D, Guinot PG. Fluid expansion improve ventriculo-arterial coupling in preload-dependent patients: a prospective observational study. BMC Anesthesiol. 2020;20:171.
Cecconi M, Monti G, Hamilton MA, Puntis M, Dawson D, Tuccillo ML, et al. Efficacy of functional hemodynamic parameters in predicting fluid responsiveness with pulse power analysis in surgical patients. Minerva Anestesiol. 2012;78:527–33.
Mohammad Abdelfattah WoM, Saad-eldeen Elgammal S, Mohammad Elsayed K, Said Mowafy SM, Mohammad Abdalla R. Distensibility index of inferior vena cava and pulse pressure variation as predictors of fluid responsiveness in mechanically ventilated shocked patients. J Emerg Med Trauma Acute Care 2020;2020
Georges D, de Courson H, Lanchon R, Sesay M, Nouette-Gaulain K, Biais M. End-expiratory occlusion maneuver to predict fluid responsiveness in the intensive care unit: an echocardiographic study. Crit Care. 2018;22:32.
Jacquet-Lagreze M, Bouhamri N, Portran P, Schweizer R, Baudin F, Lilot M, et al. Capillary refill time variation induced by passive leg raising predicts capillary refill time response to volume expansion. Crit Care. 2019;23:281.
Monnet X, Bataille A, Magalhaes E, Barrois J, Le Corre M, Gosset C, et al. End-tidal carbon dioxide is better than arterial pressure for predicting volume responsiveness by the passive leg raising test. Intensive Care Med. 2013;39:93–100.
Beurton A, Teboul JL, Girotto V, Galarza L, Anguel N, Richard C, et al. Intra-abdominal hypertension is responsible for false negatives to the passive leg raising test. Crit Care Med. 2019;47:e639–47.
Monnet X, Rienzo M, Osman D, Anguel N, Richard C, Pinsky MR, et al. Esophageal doppler monitoring predicts fluid responsiveness in critically ill ventilated patients. Intensive Care Med. 2005;31:1195–201.
Roger C, Zieleskiewicz L, Demattei C, Lakhal K, Piton G, Louart B, et al. Time course of fluid responsiveness in sepsis: the fluid challenge revisiting (fcrev) study. Crit Care. 2019;23:179.
Biais M, Cottenceau V, Stecken L, Jean M, Ottolenghi L, Roullet S, et al. Evaluation of stroke volume variations obtained with the pressure recording analytic method. Crit Care Med. 2012;40:1186–91.
Mukhtar A, Awad M, Elayashy M, Hussein A, Obayah G, El Adawy A, et al. Validity of mini-fluid challenge for predicting fluid responsiveness following liver transplantation. BMC Anesthesiol. 2019;19:56.
Trifi A, Abdellatif S, Daly F, Nasri R, Touil Y, Ben Lakhal S. Ultrasound stroke volume variation induced by passive leg raising and fluid responsiveness: An observational cohort study. Med Intensiva (Engl Ed). 2019;43:10–7.
Article CAS Google Scholar
Michard F, Alaya S, Zarka V, Bahloul M, Richard C, Teboul JL. Global end-diastolic volume as an indicator of cardiac preload in patients with septic shock. Chest. 2003;124:1900–8.
Giraud R, Abraham PS, Brindel P, Siegenthaler N, Bendjelid K. Respiratory changes in subclavian vein diameters predicts fluid responsiveness in intensive care patients: a pilot study. J Clin Monit Comput. 2018;32:1049–55.
Download references
Acknowledgements
We are thankful to Dr. Katerina Negri for the linguistic revision of this manuscript.
This work has not been funded by an external source.
Author information
Authors and affiliations.
Department of Anesthesia and Intensive Care Medicine, Humanitas Clinical and Research Center—IRCCS, Via Alessandro Manzoni, 56, 20089, Rozzano, Milano, Italy
Antonio Messina, Lorenzo Calabrò, Luca Pugliese, Aulona Lulja, Alexandra Sopuch, Emanuela Morenghi & Maurizio Cecconi
Department of Biomedical Sciences, Humanitas University, Pieve Emanuele, Milano, Italy
Antonio Messina, Emanuela Morenghi & Maurizio Cecconi
Università del Piemonte Orientale, Vercelli, Italy
Daniela Rosalba
Departamento de Medicina Intensiva, Facultad de Medicina, Pontificia Universidad Católica de Chile, Diagonal Paraguay 362, Santiago, Chile
Glenn Hernandez
Hôpitaux Universitaires Paris-Sud, Hôpital de Bicêtre, Medical Intensive Care Unit, Le Kremlin-Bicêtre, F-94270, Paris, France
Xavier Monnet
Université Paris-Saclay, AP-HP, Service de médecine intensive-réanimation, Hôpital de Bicêtre, Paris, France
DMU CORREVE, Inserm UMR S_999, FHU SEPSIS, Groupe de Recherche Clinique CARMAS, Le Kremlin-Bicêtre, Paris, France
You can also search for this author in PubMed Google Scholar
Contributions
AM designed the study, performed data analysis, and drafted the manuscript; EM: helped in data analysis and manuscript preparation; LC, LP, AL, AS, and DR substantially contributed to data collection and interpretation; MC, XM, and GE substantially contributed to data interpretation and manuscript draft. All the authors approved the final version of the paper and agreed to be accountable for all aspects of the work, thereby ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Correspondence to Antonio Messina .
Ethics declarations
Humans ethics statement, adult consent to participate written and human accordance statement.
Not applicable.
Consent for publication
Competing interests.
Dr. Messina received travel expenses and registration for meetings, congresses, and courses and lecture fees from Vygon, Edwards, Philips, and Getinge. Xavier Monnet is a member of the medical advisory board of Pulsion Medical Systems (Getinge), and has given lectures for Baxter. Prof. Cecconi is a consultant of Edwards Lifesciences (Directed Systems Consultancy).
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
. Table S1. PRISMA-DTA checklist. Table S2. Extracted data in each study assessed for eligibility. Table S3. Full-text articles excluded, not fitting eligibility criteria. Table S4. Studies on functional haemodynamic tests or dynamic indexes of fluid responsiveness. Figure S1. Characteristics of fluid challenge administration and monitoring along the considered years.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Messina, A., Calabrò, L., Pugliese, L. et al. Fluid challenge in critically ill patients receiving haemodynamic monitoring: a systematic review and comparison of two decades. Crit Care 26 , 186 (2022). https://doi.org/10.1186/s13054-022-04056-3
Download citation
Received : 01 April 2022
Accepted : 07 June 2022
Published : 21 June 2022
DOI : https://doi.org/10.1186/s13054-022-04056-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Fluid challenge
- Fluid bolus
- Fluid responsiveness
- Critically ill patients
Critical Care
ISSN: 1364-8535
- Submission enquiries: [email protected]
- Open supplemental data
- Reference Manager
- Simple TEXT file
People also looked at
Case report article, graded exercise with motion style acupuncture therapy for a patient with failed back surgery syndrome and major depressive disorder: a case report and literature review.

- 1 Department of Acupuncture and Moxibustion, Jaseng Korean Medicine Hospital, Seoul, Republic of Korea
- 2 Jaseng Spine and Joint Research Institute, Jaseng Medical Foundation, Seoul, Republic of Korea
Effective treatment of failed back surgery syndrome (FBSS) remains challenging despite urgent medical attention requirements. Depression is a contributing factor to the development and poor prognosis of FBSS, and vice versa. We report the case of a patient with FBSS and major depressive disorder (MDD) treated with graded exercise combined with motion-style acupuncture therapy (MSAT). A 53-year-old male veteran who had undergone lumbar discectomy and laminectomy with instrumented fusion was admitted to the hospital with re-current back pain and radiative pain in the left leg. The effects of failed surgery triggered MDD as a comorbidity. After a six-week routine treatment without remarkable improvement, a three-week program of graded exercise with MSAT was applied. The numeric rating scale (NRS) and short form-36 (SF-36) were used to assess low back pain with radiating leg pain, and daily functioning levels, respectively. The voluntary walking distance of the patients was measured. To analyze the therapeutic effects and other applications of the intervention, we surveyed clinical trials using MSAT or graded exercise therapy (GET). Three weeks of graded exercise with MSAT reduced physical and mental functional disabilities (SF-36, physical component: 15.0 to 37.2, mental component: 21.9 to 30.1) as well as the intensity of low back pain and/or radiative leg pain (NRS: 50 to 30). Furthermore, as the therapeutic intensity gradually increased, there was a significant corresponding increase in daily walking distance (mean daily walking distance, the first week vs. baseline, second, and third week, 3.05 ± 0.56: 2.07 ± 0.79, 4.27 ± 0.96, and 4.72 ± 1.04 km, p = 0.04, p = 0.02, and p = 0.003, respectively). Three randomized controlled trials of GET were included, all showing statistically significant antidepressant effects in the diseased population. Graded exercise with MSAT may be an effective rehabilitative therapy for patients with FBSS and MDD who have impaired daily routines.
1 Introduction
Failed back surgery syndrome (FBSS) is a post-spinal surgery condition characterized by persistent or recurrent spinal pain and/or radiating pain in the lower extremities ( 1 ). The incidence of FBSS is estimated to range from 10 to 40% after lumbar laminectomy, with or without instrumented fusion ( 2 ). Recently, owing to the increased demand for lumbar surgeries to treat degenerative spinal diseases, that is, an approximately 140% increase from 2004 to 2015 in the United States and 2-fold increase from 1997 to 2018 in Finland, FBSS requires medical attention ( 3 , 4 ). Patients with FBSS exhibit debilitated mental and physical functions and experience a lower health-related quality of life (QoL) than patients with cancer or stroke ( 5 ). The estimated annual cost of medical and productivity losses ranges from US $22,403 to US $26,170 per patient in Washington State ( 6 ).
Factors contributing to the development of FBSS include recurrent spinal disease, postoperative infection, nerve injury, and psychological disorders such as depression ( 1 ). Psychiatric problems are frequently encountered in cases of medically unexplainable pain with a challenging pathophysiology. Patients with FBSS have a significantly higher risk of developing mental disorders ( 7 ). According to the National Inpatient Sample database, the incidence of comorbid depression in hospitalized patients with FBSS was estimated to be 23% in 2015, and this was dominant in the working-age population ( 8 ). Moreover, chronic pain and mood disorders mutually contribute to a poor prognosis ( 9 ). Given the absence of an established treatment for FBSS accompanied by the unexplainable pain, not even with depression, the development of valid therapeutic approaches for FBSS with depressive disorder is imperatively required.
Acupuncture and exercise therapy are commonly recommended as effective non-pharmacological treatments for chronic low back pain (LBP) ( 10 ). The mechanism of pain relief provided by acupuncture involves neuronal modulation within the central nervous system (CNS) through peripheral stimuli ( 11 ). A modification of acupuncture, motion-style acupuncture therapy (MSAT), wherein acupuncture is combined with coordinated motion, demonstrated a decent analgesic effect on chronic LBP in spinal degenerative disorders such as herniated intervertebral disc (HIVD) ( 12 , 13 ). MSAT reinforces the stimuli to invade tissues using the targeted muscles. In contrast, graded exercise therapy (GET) is a type of physical training in which the intensity of exercise is gradually increased ( 14 ). GET strengthens physical capacity and provides psychological encouragement by demonstrating objective improvements in patient performance ( 15 ). GET has been shown to be effective in ameliorating the conditions of patients with cancer with comorbid mental disabilities such as depression, anxious mood, and catastrophizing ( 16 ). The respective therapeutic effects of MSAT and exercise for LBP or depressive mood are widely recognized; however, the clinical application and synergies of combining these treatments are novel for pain or mental disorders. Considering the pain-relief effect and neuronal activity improvement provided by acupuncture, we hypothesized that MSAT with simultaneous GET would improve both physical and mental health in chronic pain with depressive disorder.
Herein, we evaluated the effect of GET with MSAT in a patient with FBSS and major depressive disorder (MDD). We also undertook a literature review of clinical trials that used MSAT or GET for depressive mood therapy in a diseased population to corroborate the findings of the case study and further clinical applicability.
2 Case presentation
2.1 patient characteristics and medical history.
A 53-year-old Asian male veteran was admitted to Jaseng Hospital of Korean Medicine on October 7, 2022, presenting complaints of LBP and numbness in the left shin and hallux, which initially manifested 3 years prior. His anthropometric measurements include a height of 168.3 cm, weight of 65.2 kg, and a body mass index (BMI) of 23.0, positioning him on the border between normal and overweight classifications. Over the past 3 years since the onset of pain, he has maintained a sedentary lifestyle, engaging in less than 30 min of walking per day. He adheres to non-smoking and non-drinking habits and reports no comorbidities or significant familial history of underlying diseases. The range of motion (ROM) of the lumbar spine was limited only in flexion/extension, measuring 70/10 degrees respectively, and a negative straight leg raise test was observed. The blood and urine analyses conducted upon admission, which encompassed a complete blood count, glucose/lipid metabolic panel, liver and kidney function tests, and inflammatory markers, did not reveal any remarkable findings.
In his medical history, the patient had been diagnosed with L4–5 HIVD and had undergone discectomy and laminectomy with instrumented fusion in September 2021. Before diagnosis and surgery, he received no treatment other than arbitrary analgesic administration when the pain was severe. Although the surgery was successful with no abnormal findings on magnetic resonance imaging (MRI) or computed tomography (CT), the patient had no symptomatic changes in the lower back or lower extremities ( Figure 1B ). Subsequently, he had to be discharged from the army because of disturbance in his activities of daily living, which had become strikingly worse than before becoming diseased. Moreover, following two ineffective functional intramuscular stimulation (FIMS) treatments, the patient developed helplessness and hopelessness. This triggered depression, manifesting as sleep disturbance, reduced appetite, pessimism regarding his symptoms, and a subsequent attempted suicide. Later that year, he was diagnosed with MDD. Four admissions for integrative medicine treatment, before and after the diagnosis of MDD, did not indicate any pain management strategies ( Figure 1A ).
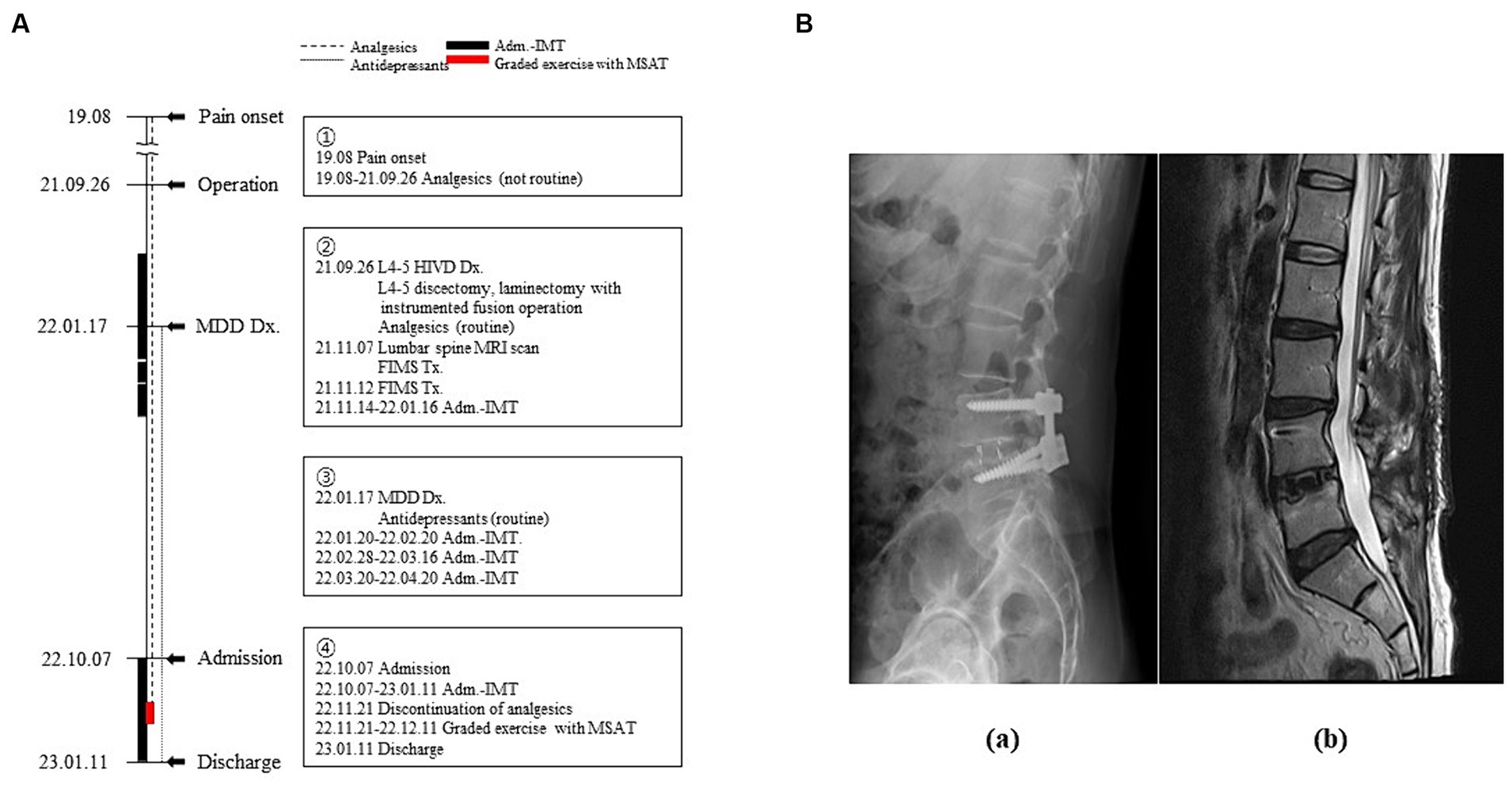
Figure 1 . Timeline of the patient’s medical history. (A) Timeline of the medical events between the onset of the pain and the current treatment period. Narrative demonstrations of the timeline are in the boxes. (B) Radiological images of the lumbar spine (a: lateral view of X-ray image, b: Sagittal section of T2-weighted magnetic resonance image). Adm, admission; Dx, diagnosis; FIMS, functional intramuscular stimulation; HIVD, herniated intervertebral disc; IMT, integrative medicine treatment; MDD, major depressive disorder; MRI, magnetic resonance imaging; MSAT, motions style acupuncture therapy; Tx, treatment.
2.2 Diagnosis and treatment
The diagnosis of FBSS was determined based on the persistent LBP with left radiative pain and numbness that existed despite surgery being performed in 2021. Furthermore, MDD was diagnosed in accordance with the Diagnostic and Statistical Manual of mental disorders-5 ( 17 ).
Routine treatments, as standardized by practice guideline ( 18 ), included acupuncture with electronic stimulus, pharmacopuncture, herbal medicine, analgesics, and psychopharmacotherapy which were prescribed and administered, since his admission in October 2022, by the psychiatric clinics that had confirmed the diagnosis of MDD ( Supplementary Table 1 ). Since the 6-week routine treatment did not provide remarkable improvement, graded exercise with MSAT was additionally performed after excluding analgesics from the routine treatment. It was prospectively employed with the expectation of curative effects on debilitating pain and depressive mood by referring to its successful application in patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) ( 19 ).
MSAT is a physical restoration technique performing the specific movements with needles inserted into the muscles associated with restricted motion ( 12 ). The treatment method used in this case combines the characteristics of MSAT, usually employed as a one-off treatment, with GET, which gradually increases the distance and weight. The acupoints utilized were both sides of LR3, ST36, and BL25. These points were chosen to stimulate muscles associated with walking pain (BL25: erector spinae, ST36: tibialis anterior) as well as brain activities related to pain perception and emotional processing (LR3) ( 20 ). Needles measuring 0.25 × 30 (DongBang Co., Seoul, Korea) were used. With the needles retained at the acupoints, the patient was instructed to walk at a pace of one step per second, while carrying 0–2 sandbags, each weighing 800 g. ( 21 ). Exercise was performed on weekdays for 3 weeks. The number of exercise sets (50 m per set) and sandbags were gradually increased based on the patient’s exercise performance under the physician’s judgment. The rest intervals between sets are 30 s.
2.3 Course of symptom and physical performance
The numeric rating scale (NRS) for LBP and radiating leg pain was recorded at baseline and every end of weekly treatments. Also, daily functioning levels was assessed with short form-36 (SF-36) at baseline and the end of the intervention ( 22 ). In addition, spontaneous daily walking distances, except for intervention-associated steps, were measured using a Samsung Health Pedometer (Samsung Electronics Co., Suwon, Korea).
As shown in Figure 2A , 3 weeks of graded exercise with MSAT reduced the intensity of LBP and radiative leg pain (NRS: 50 to 30), as well as improved both physical and mental health (SF-36, physical component: 15.0 to 37.2; mental component: 21.9 to 30.1). Furthermore, the physical function of the SF-36, which includes general activities of daily living including walking, climbing stairs, and carrying objects, showed improvement. However, his emotional state, particularly in feeling blue, nervous, and worn out, still persisted, as evidenced by the SF-36 mental component scores.
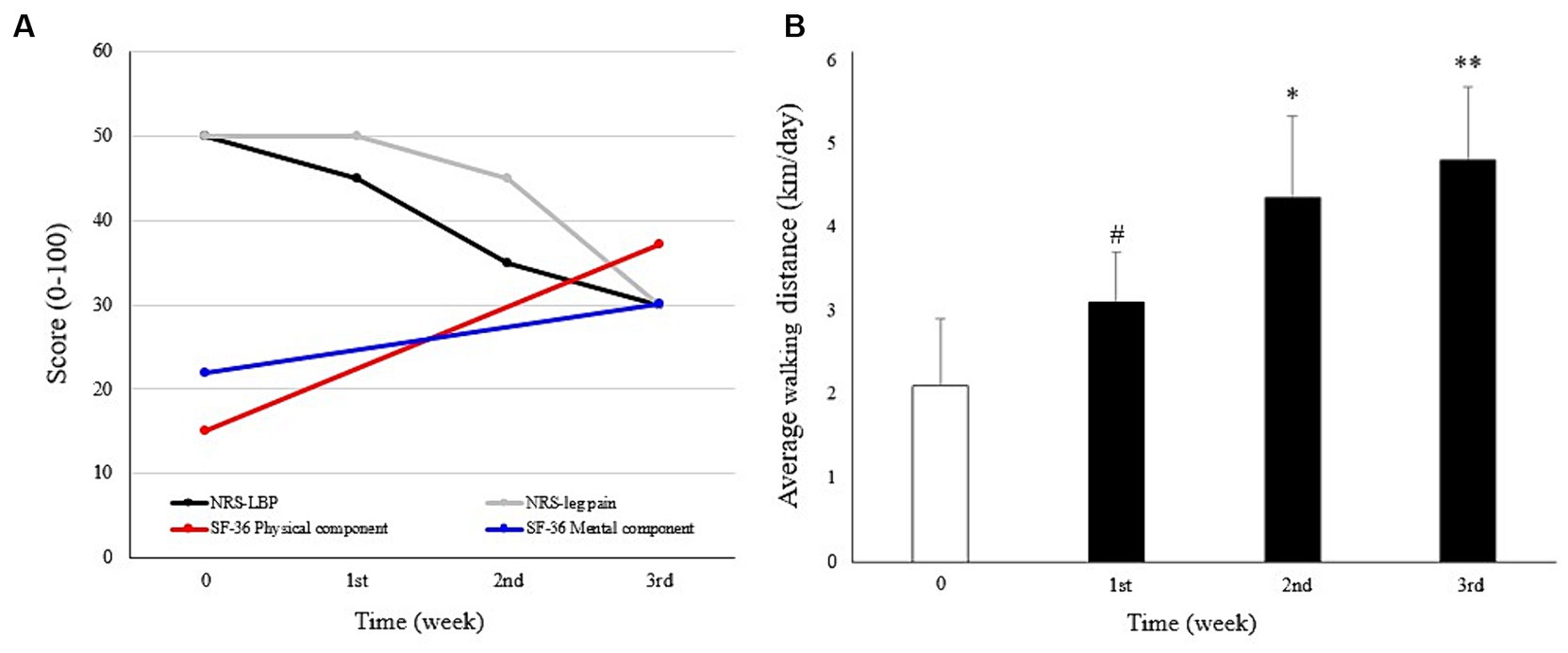
Figure 2 . Course of symptoms. (A) Changes in low back pain (LBP), leg pain, physical and mental health scores, measured using the numeric rating scale (NRS) and Short Form-36 (SF-36), respectively. (B) Mean daily walking distances were calculated at baseline (Week 0, before the intervention) and the first to third week during which the intervention was applied, with gradually increased exercise intensity. # p < 0.05, compared with baseline. * p < 0.05; ** p < 0.01 compared with the first week. Mann–Whitney U test was used to analyze statistical significance.
The intensity of the intervention was gradually escalated. During the initial week of treatment, the patient executed two sets (100 m) daily without the use of sandbags. Subsequently, in the second week, the regimen progressed to three sets with the addition of one sandbag (800 g), and by the third week, the patient advanced to four sets while incorporating two sandbags.
Similarly, the vitality and physical function of the patient improved as daily walking distance increased. An immediate increase in the distance was shown in the first week (3.05 ± 0.56 km compared to that of the previous week at 2.07 ± 0.79 km, p = 0.04). This improving pattern was maintained in the following 2 weeks as well (4.27 ± 0.96 and 4.72 ± 1.04 km compared to the distance in the first week, p = 0.02 and p = 0.003, respectively) in accordance with gradually intensified exercise ( Figure 2B ). No adverse events were observed during the treatment.
2.4 Literature review
A literature survey was conducted using a single database: PubMed, up to December 2024, to identify clinical trials that employed MSAT or GET to treat depressive mood as a symptom in diseased populations. The inclusion criteria were as follows: (1) studies following a randomized controlled trial (RCT) design and assessed the effects of MSAT or GET, (2) studies being conducted on participants who were diseased adults, and (3) studies that evaluated changes in depressive mood using a relevant measuring tool. The search term used was “(motion style acupuncture or graded exercise therapy) and (depression) and (randomized controlled trial),” and references were screened by examining their titles, abstracts, and full texts.
Out of the total of 123 surveyed initial articles, none included RCTs assessing the MSAT for its antidepressant effect. Consequently, three RCTs with GET were reviewed, and the characteristics of the trials are summarized in Table 1 . Two RCTs were conducted on patients with ME/CFS and presented statistically significant improvements in depressive mood and fatigue following therapy ( 23 , 25 ). The antidepressant effect of GET was also demonstrated in another RCT that included patients with chronic neck pain ( 24 ).
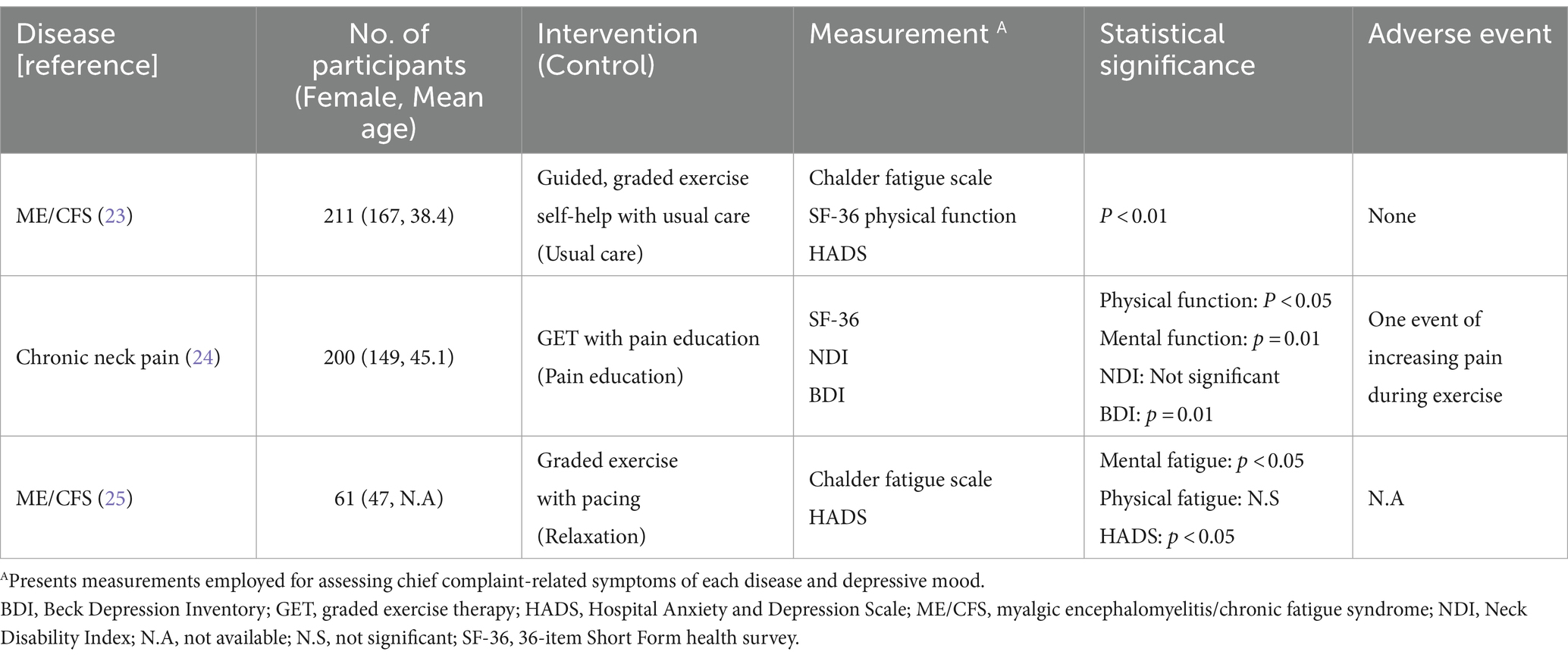
Table 1 . Characteristics of the studies in the literature review.
3 Discussion
Pain commonly accompanies depressive symptoms ( 26 ). Greater pain severity and refractory treatment outcomes are associated with more depressive symptoms and worse depression outcomes ( 27 ). In our case, the patient had a negative and hopeless mood, exacerbated by impairments on his daily living, such as restricted mobility, driven by ineffective therapeutic interventions. This involved the conservative and symptomatic management for medically unexplainable pain he had been undergoing without abnormal findings on MRI or CT. Accumulating evidence suggests that spinal cord stimulation can reduce pain and improve physical function in patients with FBSS but would not affect mental health ( 28 ). Despite 1.5 months of routine care, including paravertebral electroacupuncture, depressive symptoms and pain persisted in our patient ( Supplementary Table S1 ). However, we demonstrated how we used GET and MSAT to improve pain outcomes as well as physical and mental function in a patient with FBSS and MDD.
Acupuncture is recommended as an effective nonpharmacological intervention for the treatment of chronic LBP ( 10 ). Needling of abnormally strained muscles, known as trigger points, can ameliorate spasticity and pain in patients with LBP ( 29 ). MSAT reinforces the stimulus quantity of acupuncture by moving the needled muscles. It promotes the pain-relief effect of therapy such that the patient gradually expands their limited ROM, leading to restored physical function ( 13 ). The analgesic effect of MSAT in this case, which is not achieved through conventional acupuncture, may arise from the release of instrumented surgery-derived hyper-strained tissues by activating muscles involved in gait cycles. The selected acupoints, BL25 and ST36, were strategically chosen due to their proximity to primary pain regions and their involvement in locomotion. Additionally, the pain regulation effect of acupuncture includes the modulation of neuronal activity in the CNS ( 11 ). The peripheral stimulus-derived opioids 5-hydroxytryptamine (5-HT) and norepinephrine in the CNS are believed to regulate inflammatory and neuropathic pain ( 30 , 31 ). A study using electroencephalography suggested that pain improvement following electrocutaneous treatment in patients with FBSS was associated with increased cerebral activity, primarily in the anterior cingulate gyrus, which participates in pain and emotion processing ( 32 , 33 ). Likewise, the acupoint LR3 employed in this case is recognized for its modulatory effects on pain perception and emotional functions ( 20 ). By increasing the peripheral stimulus, MSAT may provide a greater analgesic effect with neuronal modulation in the CNS than conventional acupuncture therapy ( Figure 2A ).
Exercise has been used in musculoskeletal reinforcement and psychological therapy ( 15 ). Regarding chronic pain, exercise therapy is a nonpharmacological and noninvasive approach recommended by the Centers for Disease Control and Prevention ( 34 ). Activation of the deep trunk muscles by exercise and performing of complex functional tasks is recommended as an effective noninvasive treatment for chronic LBP ( 35 ). In our patient, exercise with MSAT focused on the trunk muscles via acupuncture and slow walking while maintaining the body’s balance. Gradually increasing the intensity and repeating the processes provided cardiovascular training and muscle strengthening. In addition, aerobic exercise has been shown to have a positive mood regulation effect in patients with depression ( 36 ). Cardiovascular exercise is believed to promote 5-HT metabolism in the CNS and reconfigure the brain structure in patients with depression, thereby improving neuroprocessing and delaying cognitive degradation ( 37 ). Therefore, the graded exercise technique used may have contributed to mood regulation and pain control in our case ( Figure 2A ).
During the exercise, the physician closely guided and corrected the posture of the patient in a step-by-step manner and encouraged him to perform more tasks by demonstrating the results of what had been achieved objectively. Thus, the physician provided not only exercise feedback but also mental support. Cognitive behavior therapy, a type of mental support intervention, has been applied to chronic pain, including LBP, in which aberrant pain perception caused by heightened interoceptive awareness is a common clinical feature ( 38 , 39 ). Likewise, the GET also has psychological benefits as it provides patients with confidence through a gradual increase in physical performance. In this context, cognitive behavior therapy and GET are recommended interventions for debilitating mental symptoms such as those of in ME/CFS ( 19 ). Therefore, it can be suggested that the mental-supportive features of graded exercise with MSAT might have motivated our patient to increase spontaneous activities ( Figure 2B ).
We prospectively adopted MSAT combined with GET as a therapeutic approach for a patient with FBSS and MDD, expecting amelioration of the low mood and pain. As a positive outcome was observed in this case, we analyzed its clinical utility by surveying RCTs to evaluate the antidepressant effects of MSAT or GET in diseased participants. All three RCTs we reviewed employed GET; the results demonstrated statistically significant improvements in the patients’ depression scores on the Beck Depression Inventory (BDI) or Hospital Anxiety and Depression Scale (HADS), compared with the scores of those in the control group ( Table 1 ). Regarding the two RCTs for ME/CFS, unlike the overall positive outcomes of mental function scores in both trials, the results for physical fatigue were not aligned in the same positive direction ( 23 , 25 ). Similarly, psychological impairment was significantly improved by GET in another RCT among patients with chronic neck pain, whereas the physical function in the neck measured by the Neck Disability Index was not ( 24 ). This might be due to the immoderate application on the patient vulnerable for excision, and one adverse event of increasing pain was reported. In fact, one survey on patients with ME/CFS reported that approximately 79% of respondents experienced their health worsening due to the GET ( 40 ). This implies that the clinical adoption of the GET requires the intensity of tasks to be adjusted considering the patient’s physical capacity and the possibility of increased pain. Regarding FBSS, moderate exercise enhances daily living, strength, and fearlessness in patients ( 41 ). Therefore, we hypothesized that MSAT assisted in providing adequate exercise intensity and pain control in our patient. The results of the case study and literature review indicate that graded exercise with MSAT may offer effective rehabilitation for individuals suffering from depression induced by pain disorders, and vice versa, facilitating a resumption of their daily activities.
This case study has several limitations. First, follow-up data were not available after the patient was discharged from the hospital, which can induce uncertainty regarding therapeutic effects and its generalizability, such as the Hawthorne effect. Second, routine integrative Korean medicine treatments were used previously and simultaneously with the intervention, which could have induced synergistic therapeutic effects. Third, depression-specific scales such as the BDI or the HADS were not used for evaluating the depressive status of the patient. While our primary focus lay in functional rehabilitation utilizing the SF-36, employing measurements specialized for MDD could provide more explicit assessments of mental status. The SF-36 survey is originally intended for measuring the QoL of patients, and we employed it considering the etiological history of this case, where restrictions in daily living, closely related to QoL, resulting from failed surgery caused depression. Nonetheless, to our knowledge, this is the first report of successful treatment of FBSS and MDD, unresponsive to usual medications, by employing graded exercise with MSAT. Further, there were no adverse events noted in the patient. However, to facilitate the clinical use of this intervention, further well-designed clinical trials on its efficacy and safety are warranted.
Data availability statement
The original data presented in the study are included in the article/ Supplementary material , further inquiries can be directed to the corresponding author.
Ethics statement
The ethical review and approval of this study were waived by the Institutional Review Board of Jaseng Hospital of Korean Medicine, Seoul, Korea (IRB file No. JASENG 2023–12-002) for the study design: a single case study with literature review. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the minor(s)’ legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author contributions
D-YK: Conceptualization, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. I-HH: Conceptualization, Writing – review & editing. J-YK: Supervision, Visualization, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1376680/full#supplementary-material
1. Baber, Z, and Erdek, MA. Failed back surgery syndrome: current perspectives. J Pain Res . (2016) 9:979–87. doi: 10.2147/JPR.S92776
PubMed Abstract | Crossref Full Text | Google Scholar
2. Chan, C-W, and Peng, P. Failed back surgery syndrome. Pain Med . (2011) 12:577–606. doi: 10.1111/j.1526-4637.2011.01089.x
3. Martin, BI, Mirza, SK, Spina, N, Spiker, WR, Lawrence, B, and Brodke, DS. Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the United States, 2004 to 2015. Spine . (2019) 44:369–76. doi: 10.1097/BRS.0000000000002822
4. Ponkilainen, VT, Huttunen, TT, Neva, MH, Pekkanen, L, Repo, JP, and Mattila, VM. National trends in lumbar spine decompression and fusion surgery in Finland, 1997–2018. Acta Orthop . (2021) 92:199–203. doi: 10.1080/17453674.2020.1839244
5. Taylor, RS, and Taylor, RJ. The economic impact of failed back surgery syndrome. Br J Pain . (2012) 6:174–81. doi: 10.1177/2049463712470887
6. Hollingworth, W, Turner, JA, Welton, NJ, Comstock, BA, and Deyo, RA. Costs and cost-effectiveness of spinal cord stimulation (SCS) for failed back surgery syndrome: an observational study in a workers' compensation population. Spine . (2011) 36:2076–83. doi: 10.1097/BRS.0b013e31822a867c
7. Stanton, E, Fresquez, Z, Muehlbauer, EJ, Wang, JC, and Buser, Z. Onset of mental disorders in patients who developed failed back surgery syndrome. Eur Spine J . (2022) 31:2612–8. doi: 10.1007/s00586-022-07334-4
8. Orhurhu, V, Urits, I, Olusunmade, M, Owais, K, Jones, M, Galasso, A, et al. Trends of co-morbid depression in hospitalized patients with failed back surgery syndrome: an analysis of the nationwide inpatient sample. Pain Ther . (2018) 7:217–26. doi: 10.1007/s40122-018-0104-y
9. Thase, ME. Managing medical comorbidities in patients with depression to improve prognosis. J Clin Psychiatry . (2016) 77:22–7. doi: 10.4088/JCP.14077su1c.04
Crossref Full Text | Google Scholar
10. Chou, R, Deyo, R, Friedly, J, Skelly, A, Hashimoto, R, Weimer, M, et al. Nonpharmacologic therapies for low back pain: a systematic review for an American College of Physicians clinical practice guideline. Ann Intern Med . (2017) 166:493–505. doi: 10.7326/M16-2459
11. Chen, T, Zhang, WW, Chu, Y-X, and Wang, Y-Q. Acupuncture for pain management: molecular mechanisms of action. Am J Chin Med . (2020) 48:793–811. doi: 10.1142/S0192415X20500408
12. Kim, D, Lee, YJ, and Ha, I-H. A scoping review of clinical research on motion style acupuncture treatment. Perspect Integr Med . (2023) 2:65–76. doi: 10.56986/pim.2023.06.001
13. Shin, J-S, Ha, I-H, Lee, J, Choi, Y, Kim, M-R, Park, B-Y, et al. Effects of motion style acupuncture treatment in acute low back pain patients with severe disability: a multicenter, randomized, controlled, comparative effectiveness trial. Pain . (2013) 154:1030–7. doi: 10.1016/j.pain.2013.03.013
14. Fulcher, KY, and White, PD. Randomised controlled trial of graded exercise in patients with the chronic fatigue syndrome. BMJ . (1997) 314:1647–52. doi: 10.1136/bmj.314.7095.1647
15. Penedo, FJ, and Dahn, JR. Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Curr Opin Psychiatry . (2005) 18:189–93. doi: 10.1097/00001504-200503000-00013
16. Lahousse, A, Reynebeau, I, Nijs, J, Beckwée, D, Van Wilgen, P, Fernández-De-Las-Peñas, C, et al. The effect of psychologically informed practice with behavioural graded activity in cancer survivors: systematic review and meta-analysis. J Cancer Surviv . (2023):1–46. doi: 10.1007/s11764-022-01270-4
17. American Psychiatric Association, D., and Association, A.P. Diagnostic and statistical manual of mental disorders: DSM-5 . WashingtonDC: American Psychiatric Association (2013).
Google Scholar
18. Song, YK. Korean medicine clinical practice guideline for post-operative treatment of spinal disorders . Republic of Korea: National Institute for Korean Medicine Development (2021).
19. White, PD, Goldsmith, KA, Johnson, AL, Potts, L, Walwyn, R, Decesare, JC, et al. Comparison of adaptive pacing therapy, cognitive behaviour therapy, graded exercise therapy, and specialist medical care for chronic fatigue syndrome (PACE): a randomised trial. Lancet . (2011) 377:823–36. doi: 10.1016/S0140-6736(11)60096-2
20. Rao, Y, Ge, L, and Wu, J. A systematic review and coordinate-based meta-analysis of fMRI studies on acupuncture at LR 3. Front Neurosci . (2024) 18:1341567. doi: 10.3389/fnins.2024.1341567
21. Hwangbo, S.-Y., Kim, Y.-J., Shin, D.G., An, S.-J., Choi, H., Lee, Y., et al. Effectiveness and safety of progressive loading–motion style acupuncture treatment for acute low Back pain after traffic accidents: a randomized controlled trial. Healthcare . (2023). 11:2939. doi: 10.3390/healthcare11222939
22. Ware, JE Jr. SF-36 health survey update. Spine . (2000) 25:3130–9. doi: 10.1097/00007632-200012150-00008
23. Clark, LV, Pesola, F, Thomas, JM, Vergara-Williamson, M, Beynon, M, and White, PD. Guided graded exercise self-help plus specialist medical care versus specialist medical care alone for chronic fatigue syndrome (GETSET): a pragmatic randomised controlled trial. Lancet . (2017) 390:363–73. doi: 10.1016/S0140-6736(16)32589-2
24. Ris, I, Søgaard, K, Gram, B, Agerbo, K, Boyle, E, and Juul-Kristensen, B. Does a combination of physical training, specific exercises and pain education improve health-related quality of life in patients with chronic neck pain? A randomised control trial with a 4-month follow up. Man Ther . (2016) 26:132–40. doi: 10.1016/j.math.2016.08.004
25. Wallman, KE, Morton, AR, Goodman, C, Grove, R, and Guilfoyle, AM. Randomised controlled trial of graded exercise in chronic fatigue syndrome. Med J Aust . (2004) 180:444–8. doi: 10.5694/j.1326-5377.2004.tb06019.x
26. Ishak, WW, Wen, RY, Naghdechi, L, Vanle, B, Dang, J, Knosp, M, et al. Pain and depression: a systematic review. Harv Rev Psychiatry . (2018) 26:352–63. doi: 10.1097/HRP.0000000000000198
27. Bair, MJ, Robinson, RL, Katon, W, and Kroenke, K. Depression and pain comorbidity: a literature review. Arch Intern Med . (2003) 163:2433–45. doi: 10.1001/archinte.163.20.2433
28. Kurt, E, Noordhof, RK, Van Dongen, R, Vissers, K, Henssen, D, and Engels, Y. Spinal cord stimulation in failed back surgery syndrome: An integrative review of quantitative and qualitative studies. Neuromodulation Technol Neural Interface . (2022) 25:657–70. doi: 10.1016/j.neurom.2021.11.013
29. Liu, H, Li, Y-P, Hou, M-J, Huang, W-J, Chen, X-L, Gao, Z, et al. Effect of trigger point acupuncture on pain and functional activity in patients with chronic non-specific low back pain: a randomised controlled trial. Acupunct Med . (2023) 41:130–41. doi: 10.1177/09645284221107685
30. Xiao, L-Y, Wang, X-R, Ye, Y, Yang, J-W, Cao, Y, Ma, S-M, et al. Applications of acupuncture therapy in modulating plasticity of central nervous system. Neuromodulation Technol Neural Interface . (2018) 21:762–76. doi: 10.1111/ner.12724
31. Zhang, R, Lao, L, Ren, K, and Berman, BM. Mechanisms of acupuncture–electroacupuncture on persistent pain. Anesthesiology . (2014) 120:482–503. doi: 10.1097/ALN.0000000000000101
32. Lee, CH, Kim, HS, Kim, Y-S, Jung, S, Yoon, CH, and Kwon, O-Y. Cerebral current-source distribution associated with pain improvement by non-invasive painless signaling therapy in patients with failed back surgery syndrome. Korean J Pain . (2021) 34:437–46. doi: 10.3344/kjp.2021.34.4.437
33. Vogt, BA. Pain and emotion interactions in subregions of the cingulate gyrus. Nat Rev Neurosci . (2005) 6:533–44. doi: 10.1038/nrn1704
34. Qaseem, A, Wilt, TJ, McLean, R, Forciea, MA, Clinical Guidelines Committee of the American College of PhysiciansDenberg, TD, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med . (2017) 166:514–30. doi: 10.7326/M16-2367
35. Saragiotto, BT, Maher, CG, Yamato, TP, Costa, LO, Menezes Costa, LC, Ostelo, RW, et al. Motor control exercise for chronic non-specific low-back pain. Cochrane Database Syst Rev . (2016) CD012004. doi: 10.1002/14651858.CD012004
36. Kok, RM, and Reynolds, CF. Management of depression in older adults: a review. JAMA . (2017) 317:2114–22. doi: 10.1001/jama.2017.5706
37. Zhao, JL, Jiang, WT, Wang, X, Cai, ZD, Liu, ZH, and Liu, GR. Exercise, brain plasticity, and depression. CNS Neurosci Ther . (2020) 26:885–95. doi: 10.1111/cns.13385
38. Thoma, N, Pilecki, B, and Mckay, D. Contemporary cognitive behavior therapy: a review of theory, history, and evidence. Psychodynamic Psychiatry . (2015) 43:423–61. doi: 10.1521/pdps.2015.43.3.423
39. Turner, JA. Educational and behavioral interventions for back pain in primary care. Spine . (1996) 21:2851–7. doi: 10.1097/00007632-199612150-00010
40. Bjørkum, T, and Wang, C. Patients' experience with treatment of chronic fatigue syndrome. Tidsskrift for den Norske laegeforening . (2009) 129:1214–6. doi: 10.4045/tidsskr.09.35791
41. Miller, B, Gatchel, RJ, Lou, L, Stowell, A, Robinson, R, and Polatin, PB. Interdisciplinary treatment of failed back surgery syndrome (FBSS): a comparison of FBSS and non-FBSS patients. Pain Pract . (2005) 5:190–202. doi: 10.1111/j.1533-2500.2005.05304.x
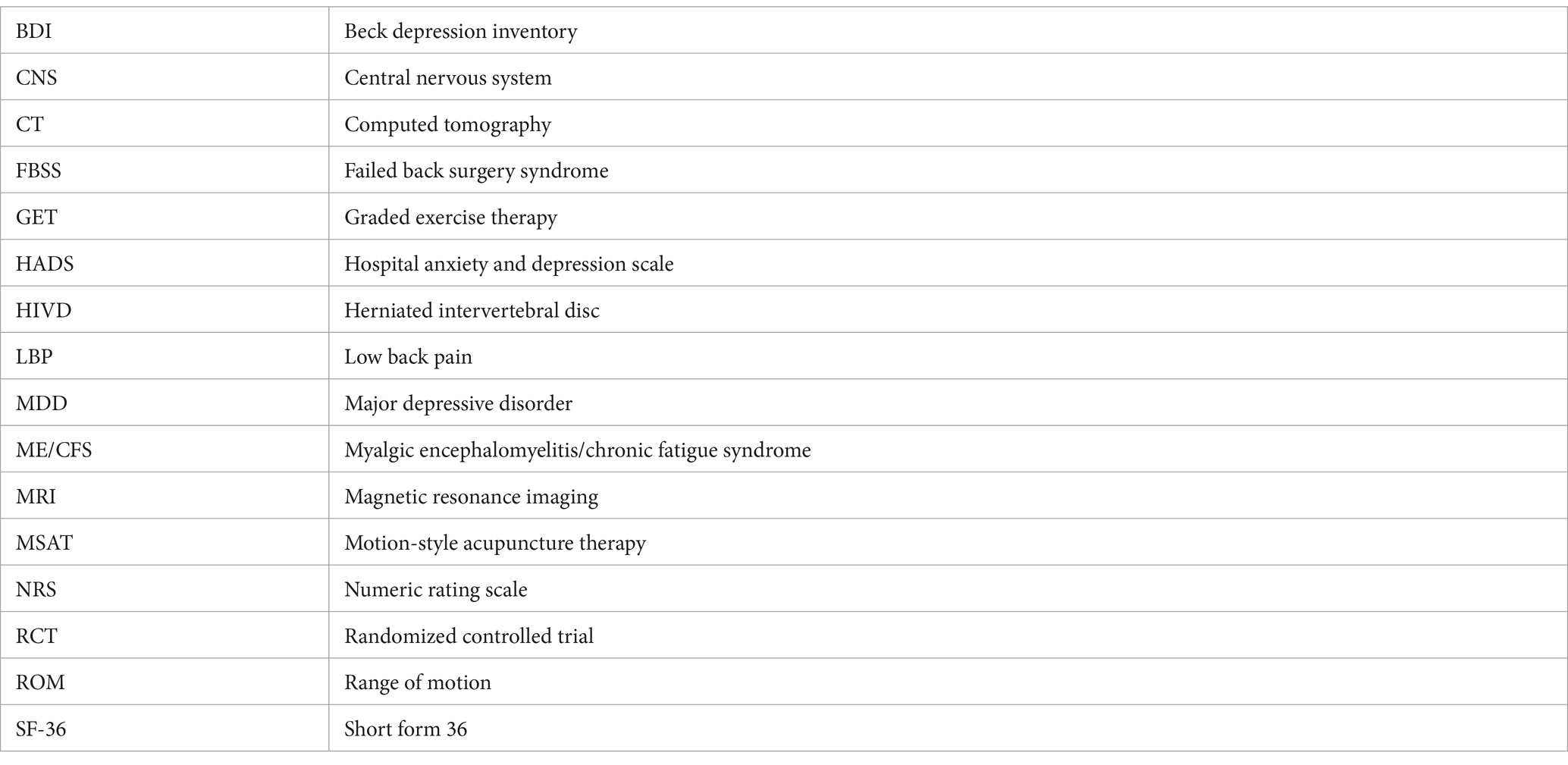
Keywords: failed back surgery syndrome, major depressive disorder, rehabilitation therapy, motion-style acupuncture therapy, graded exercise therapy
Citation: Kim D-Y, Ha I-H and Kim J-Y (2024) Graded exercise with motion style acupuncture therapy for a patient with failed back surgery syndrome and major depressive disorder: a case report and literature review. Front. Med . 11:1376680. doi: 10.3389/fmed.2024.1376680
Received: 26 January 2024; Accepted: 19 March 2024; Published: 08 April 2024.
Reviewed by:
Copyright © 2024 Kim, Ha and Kim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ju-Yeon Kim, [email protected]
This article is part of the Research Topic
Rehabilitation and Alternative Medicine in the Healthcare for Chronic Rheumatic Pain Disorders

IMAGES
VIDEO
COMMENTS
Examples of literature reviews. Step 1 - Search for relevant literature. Step 2 - Evaluate and select sources. Step 3 - Identify themes, debates, and gaps. Step 4 - Outline your literature review's structure. Step 5 - Write your literature review.
A literature review is a document or section of a document that collects key sources on a topic and discusses those sources in conversation with each other (also called synthesis).The lit review is an important genre in many disciplines, not just literature (i.e., the study of works of literature such as novels and plays).
A literature review is a review and synthesis of existing research on a topic or research question. A literature review is meant to analyze the scholarly literature, make connections across writings and identify strengths, weaknesses, trends, and missing conversations. A literature review should address different aspects of a topic as it ...
A literature review is a survey of scholarly sources on a specific topic. It provides an overview of current knowledge, allowing you to identify relevant theories, methods, and gaps in the existing research. There are five key steps to writing a literature review: Search for relevant literature. Evaluate sources. Identify themes, debates and gaps.
Literature reviews are in great demand in most scientific fields. Their need stems from the ever-increasing output of scientific publications .For example, compared to 1991, in 2008 three, eight, and forty times more papers were indexed in Web of Science on malaria, obesity, and biodiversity, respectively .Given such mountains of papers, scientists cannot be expected to examine in detail every ...
Example: Predictors and Outcomes of U.S. Quality Maternity Leave: A Review and Conceptual Framework: 10.1177/08948453211037398 ; Systematic review: "The authors of a systematic review use a specific procedure to search the research literature, select the studies to include in their review, and critically evaluate the studies they find." (p. 139).
1. Outline and identify the purpose of a literature review. As a first step on how to write a literature review, you must know what the research question or topic is and what shape you want your literature review to take. Ensure you understand the research topic inside out, or else seek clarifications.
A literature review serves two main purposes: 1) To show awareness of the present state of knowledge in a particular field, including: seminal authors. the main empirical research. theoretical positions. controversies. breakthroughs as well as links to other related areas of knowledge. 2) To provide a foundation for the author's research.
Literature review is an essential feature of academic research. Fundamentally, knowledge advancement must be built on prior existing work. To push the knowledge frontier, we must know where the frontier is. By reviewing relevant literature, we understand the breadth and depth of the existing body of work and identify gaps to explore.
The characteristics of a literature review are then presented along with identifying three main types of literature reviews (systematic, integrated, scoping) along with checklists for each to help aid researchers in their planning stages. Because one essential component of a literature review involves synthesizing the data (literature), we ...
Literature reviews can take two major forms. The most prevalent one is the "literature review" or "background" section within a journal paper or a chapter in a graduate thesis. This section synthesizes the extant literature and usually identifies the gaps in knowledge that the empirical study addresses (Sylvester, Tate, & Johnstone, 2013).
The integrative literature review is a particularly broad form of studying the field of existing literature because it can encompass a broad array of scholarly literature— empirical, non-empirical, conceptual, theoretical—to address a particular phenomenon (Kennedy, 2007). The historic literature review reconstructs, constructs, or ...
A sophisticated literature review (LR) can result in a robust dissertation/thesis by scrutinizing the main problem examined by the academic study; anticipating research hypotheses, methods and results; and maintaining the interest of the audience in how the dissertation/thesis will provide solutions for the current gaps in a particular field.
A literature review can broadly be described as a more or less systematic way of collecting and synthesizing previous research (Baumeister & Leary, 1997; Tranfield, Denyer, & Smart, 2003). ... Techniques can also be used to discover which study-level or sample characteristics have an effect on the phenomenon being studied, ...
"A type of review that has as its primary objective the identification of the size and quality of research in a topic area in order to inform subsequent review" (Booth et al., 2012, p. 269). Characteristics: Main purpose is to map out and categorize existing literature, identify gaps in literature—great for informing policy-making
The first level, exhaustive coverage, means the reviewer intends to be comprehensive in the presentation of works relevant to the topic under consideration. ii. The second type of coverage also ...
Literature review: Generic term: published materials that provide examination of recent or current literature. ... Analysis may characterise both literatures and look for correlations between characteristics or use gap analysis to identify aspects absent in one literature but missing in the other: Overview: Generic term: summary of the [medical ...
University of Arusha. A literature review is a documentation of a comprehensive review of publish and unpublished work from second source of data in the area of specific of the researcher. The ...
Characteristics of an effective literature review In addition to fulfilling the purposes outlined above, an effective literature review provides a critical overview of existing research by. Outlining important research trends. Assessing strengths and weaknesses (of individual studies as well the existing research as a whole). Identifying ...
A literature review is a scholarly paper that presents the current knowledge including substantive findings as well as theoretical and methodological contributions to a particular topic. Literature
This systematic literature review intends to examine research articles on job characteristics and work engagement (WE) from 2017 to 2021 that were retrieved from publicly available databases.
Narrative reviews have many strengths. They are flexible and practical, and ideally provide a readable, relevant synthesis of a diverse literature. Narrative reviews are often helpful for teaching or learning about a topic because they deliver a general overview. They are also useful for setting the stage for future research, as they offer an ...
Background It is uncertain if patient's characteristics are associated with complaints and claims against doctors. Additionally, evidence for the effectiveness of remedial interventions on rates of complaints and claims against doctors has not been synthesised. Methods We conducted a rapid review of recent literature to answer: Question 1 "What are the common characteristics and ...
This scoping literature review explored literature on forensic neuropathology from January 1, 2010, until February 12, 2022. The aims were to (1) analyze the volume of research on the topic, (2) describe meta-level attributes and sample characteristics, and (3) summarize key research themes and methods.
Systematic literature review. A comprehensive search strategy was designed to identify English-language studies published in peer-reviewed journals providing data on risk factors or predictors of moderate or severe exacerbations in adults aged ≥ 40 years with a diagnosis of COPD (sample size ≥ 100).
This literature review provides a comprehensive overview of triple-negative breast cancer (TNBC) and explores innovative targeted therapies focused on specific hallmarks of cancer cells, aiming to revolutionize breast cancer treatment. TNBC, characterized by its lack of expression of estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2 ...
Fluid challenges are widely adopted in critically ill patients to reverse haemodynamic instability. We reviewed the literature to appraise fluid challenge characteristics in intensive care unit (ICU) patients receiving haemodynamic monitoring and considered two decades: 2000-2010 and 2011-2021. We assessed research studies and collected data regarding study setting, patient population ...
We also undertook a literature review of clinical trials that used MSAT or GET for depressive mood therapy in a diseased population to corroborate the findings of the case study and further clinical applicability. 2 Case presentation 2.1 Patient characteristics and medical history. A 53-year-old Asian male veteran was admitted to Jaseng ...