Editor's Choice: AI Tools to Improve Access to Reliable Health Information
- Original Investigation Non–High-Density Lipoprotein Cholesterol Levels From Childhood to Adulthood and Cardiovascular Disease Events Feitong Wu, PhD; David R. Jacobs, PhD; Stephen R. Daniels, MD, PhD; et al cme

Just Published
- Serious Bleeding in Patients With Atrial Fibrillation Using Diltiazem With Apixaban or Rivaroxaban Wayne A. Ray, PhD; et al. Original Investigation online first has active quiz Wayne A. Ray, PhD; et al.
- Leave of Absence and Medical Student GME Placement by Race and Ethnicity Mytien Nguyen, MS; et al. Research Letter online first Mytien Nguyen, MS; et al.
- Non–HDL-C Levels From Childhood to Adulthood and CVD Events Feitong Wu, PhD; et al. Original Investigation online first has active quiz Feitong Wu, PhD; et al.
- Manufacturer Payments to Cardiologists and Use of Devices Sanket S. Dhruva, MD, MHS; et al. Research Letter online first Sanket S. Dhruva, MD, MHS; et al.
- Acetaminophen Use During Pregnancy and Children’s Risk of Autism, ADHD, and Intellectual Disability Viktor H. Ahlqvist, PhD; et al. Original Investigation has active quiz Viktor H. Ahlqvist, PhD; et al.
- Protecting Privacy of Pregnant and LGBTQ+ Research Participants Ellen Wright Clayton, MD, JD; et al. Viewpoint online first free access Ellen Wright Clayton, MD, JD; et al.
- Assessing the Real-World Effectiveness of Immunizations for Respiratory Syncytial Virus Fatimah S. Dawood, MD; et al. Viewpoint online first free access Fatimah S. Dawood, MD; et al.
- Good Enough Lauren Rissman, MD A Piece of My Mind online first free access Lauren Rissman, MD
- Including Pregnant and Lactating Women in Clinical Research Margaret Foster Riley, JD Viewpoint online first free access Margaret Foster Riley, JD
- Trading Places, Becoming One Rafael Campo, MD, MA Editor's Note free access Rafael Campo, MD, MA
- Does This Infant Have a Dislocated Hip? Abhinav Singh, BMBS, MSc; et al. The Rational Clinical Examination online first has active quiz has multimedia Abhinav Singh, BMBS, MSc; et al.
- Tilt Table Testing William P. Cheshire, MD; et al. JAMA Diagnostic Test Interpretation online first has active quiz William P. Cheshire, MD; et al.
- Does This Patient Have Alcohol Use Disorder? Evan Wood, MD, PhD; et al. The Rational Clinical Examination has active quiz Evan Wood, MD, PhD; et al.
- Systemic Lupus Erythematosus Caroline H. Siegel, MD, MS; et al. Review online first has active quiz has multimedia Caroline H. Siegel, MD, MS; et al.
- Risk Assessment and Prevention of Falls in Older Community-Dwelling Adults Cathleen S. Colón-Emeric, MD, MHS; et al. Review online first has active quiz has multimedia Cathleen S. Colón-Emeric, MD, MHS; et al.
Latest from the USPSTF
- USPSTF Recommendation: Primary Care Interventions to Prevent Child Maltreatment
- USPSTF Recommendation: Screening for Speech and Language Delay and Disorders
- USPSTF Recommendation: Screening and Preventive Interventions for Oral Health in Adults
- 41,538 Views Brain Waves Appear to Wash Out Waste During Sleep
- 32,110 Views Prostate-Specific Antigen Screening and 15-Year Prostate Cancer Mortality
- 30,169 Views Provision of Medications for Self-Managed Abortion Before and After the Dobbs Decision
- 28,819 Views Study Provides Insight Into ME/CFS
- 27,066 Views Industry Payments to US Physicians by Specialty and Product Type
- 26,961 Views Effect of Tirzepatide on Maintenance of Weight Reduction
- 23,892 Views Acetaminophen Use During Pregnancy and Children’s Risk of Autism, ADHD, and Intellectual Disability
- 22,710 Views Questions Surround Blood Tests That Claim to Screen for Multiple Cancers
- 22,238 Views Stroke Risk After COVID-19 Bivalent Vaccination in US Older Adults
- 21,946 Views Systemic Lupus Erythematosus
- 717 Citations Antibody Response to 2-Dose SARS-CoV-2 mRNA Vaccine Series in Solid Organ Transplant Recipients
- 652 Citations Strengthening the Reporting of Observational Studies in Epidemiology Using Mendelian Randomization
- 609 Citations Pancreatic Cancer
- 598 Citations Updated Guidance on the Reporting of Race and Ethnicity in Medical and Science Journals
- 591 Citations USPSTF Recommendation: Screening for Colorectal Cancer
- 511 Citations Effect of 2 Inactivated SARS-CoV-2 Vaccines on Symptomatic COVID-19 Infection in Adults
- 456 Citations The Leading Causes of Death in the US for 2020
- 444 Citations Effect of Intermediate- vs Standard-Dose Anticoagulation on Outcomes of Patients With COVID-19
- 440 Citations Association Between IL-6 Antagonists and Mortality Among Patients Hospitalized for COVID-19
- 409 Citations Association Between 3 Doses of mRNA COVID-19 Vaccine and Symptomatic Infection Caused by Omicron and Delta Variants
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- PRO Courses Guides New Tech Help Pro Expert Videos About wikiHow Pro Upgrade Sign In
- EDIT Edit this Article
- EXPLORE Tech Help Pro About Us Random Article Quizzes Request a New Article Community Dashboard This Or That Game Popular Categories Arts and Entertainment Artwork Books Movies Computers and Electronics Computers Phone Skills Technology Hacks Health Men's Health Mental Health Women's Health Relationships Dating Love Relationship Issues Hobbies and Crafts Crafts Drawing Games Education & Communication Communication Skills Personal Development Studying Personal Care and Style Fashion Hair Care Personal Hygiene Youth Personal Care School Stuff Dating All Categories Arts and Entertainment Finance and Business Home and Garden Relationship Quizzes Cars & Other Vehicles Food and Entertaining Personal Care and Style Sports and Fitness Computers and Electronics Health Pets and Animals Travel Education & Communication Hobbies and Crafts Philosophy and Religion Work World Family Life Holidays and Traditions Relationships Youth
- Browse Articles
- Learn Something New
- Quizzes Hot
- This Or That Game New
- Train Your Brain
- Explore More
- Support wikiHow
- About wikiHow
- Log in / Sign up
- Education and Communications
- College University and Postgraduate
- Academic Writing
- Research Papers
How to Write a Medical Research Paper
Last Updated: February 5, 2024 Approved
This article was co-authored by Chris M. Matsko, MD . Dr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017. wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 89% of readers who voted found the article helpful, earning it our reader-approved status. This article has been viewed 201,912 times.
Writing a medical research paper is similar to writing other research papers in that you want to use reliable sources, write in a clear and organized style, and offer a strong argument for all conclusions you present. In some cases the research you discuss will be data you have actually collected to answer your research questions. Understanding proper formatting, citations, and style will help you write and informative and respected paper.
Researching Your Paper

- Pick something that really interests you to make the research more fun.
- Choose a topic that has unanswered questions and propose solutions.

- Quantitative studies consist of original research performed by the writer. These research papers will need to include sections like Hypothesis (or Research Question), Previous Findings, Method, Limitations, Results, Discussion, and Application.
- Synthesis papers review the research already published and analyze it. They find weaknesses and strengths in the research, apply it to a specific situation, and then indicate a direction for future research.

- Keep track of your sources. Write down all publication information necessary for citation: author, title of article, title of book or journal, publisher, edition, date published, volume number, issue number, page number, and anything else pertaining to your source. A program like Endnote can help you keep track of your sources.
- Take detailed notes as you read. Paraphrase information in your own words or if you copy directly from the article or book, indicate that these are direct quotes by using quotation marks to prevent plagiarism.
- Be sure to keep all of your notes with the correct source.
- Your professor and librarians can also help you find good resources.

- Keep all of your notes in a physical folder or in a digitized form on the computer.
- Start to form the basic outline of your paper using the notes you have collected.
Writing Your Paper

- Start with bullet points and then add in notes you've taken from references that support your ideas. [1] X Trustworthy Source PubMed Central Journal archive from the U.S. National Institutes of Health Go to source
- A common way to format research papers is to follow the IMRAD format. This dictates the structure of your paper in the following order: I ntroduction, M ethods, R esults, a nd D iscussion. [2] X Research source
- The outline is just the basic structure of your paper. Don't worry if you have to rearrange a few times to get it right.
- Ask others to look over your outline and get feedback on the organization.
- Know the audience you are writing for and adjust your style accordingly. [3] X Research source

- Use a standard font type and size, such as Times New Roman 12 point font.
- Double-space your paper.
- If necessary, create a cover page. Most schools require a cover page of some sort. Include your main title, running title (often a shortened version of your main title), author's name, course name, and semester.

- Break up information into sections and subsections and address one main point per section.
- Include any figures or data tables that support your main ideas.
- For a quantitative study, state the methods used to obtain results.

- Clearly state and summarize the main points of your research paper.
- Discuss how this research contributes to the field and why it is important. [4] X Research source
- Highlight potential applications of the theory if appropriate.
- Propose future directions that build upon the research you have presented. [5] X Research source
- Keep the introduction and discussion short, and spend more time explaining the methods and results.

- State why the problem is important to address.
- Discuss what is currently known and what is lacking in the field.
- State the objective of your paper.
- Keep the introduction short.

- Highlight the purpose of the paper and the main conclusions.
- State why your conclusions are important.
- Be concise in your summary of the paper.
- Show that you have a solid study design and a high-quality data set.
- Abstracts are usually one paragraph and between 250 – 500 words.

- Unless otherwise directed, use the American Medical Association (AMA) style guide to properly format citations.
- Add citations at end of a sentence to indicate that you are using someone else's idea. Use these throughout your research paper as needed. They include the author's last name, year of publication, and page number.
- Compile your reference list and add it to the end of your paper.
- Use a citation program if you have access to one to simplify the process.

- Continually revise your paper to make sure it is structured in a logical way.
- Proofread your paper for spelling and grammatical errors.
- Make sure you are following the proper formatting guidelines provided for the paper.
- Have others read your paper to proofread and check for clarity. Revise as needed.
Expert Q&A

- Ask your professor for help if you are stuck or confused about any part of your research paper. They are familiar with the style and structure of papers and can provide you with more resources. Thanks Helpful 0 Not Helpful 0
- Refer to your professor's specific guidelines. Some instructors modify parts of a research paper to better fit their assignment. Others may request supplementary details, such as a synopsis for your research project . Thanks Helpful 0 Not Helpful 0
- Set aside blocks of time specifically for writing each day. Thanks Helpful 0 Not Helpful 0

- Do not plagiarize. Plagiarism is using someone else's work, words, or ideas and presenting them as your own. It is important to cite all sources in your research paper, both through internal citations and on your reference page. Thanks Helpful 4 Not Helpful 2
You Might Also Like

- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3178846/
- ↑ http://owl.excelsior.edu/research-and-citations/outlining/outlining-imrad/
- ↑ http://china.elsevier.com/ElsevierDNN/Portals/7/How%20to%20write%20a%20world-class%20paper.pdf
- ↑ http://intqhc.oxfordjournals.org/content/16/3/191
- ↑ http://www.ruf.rice.edu/~bioslabs/tools/report/reportform.html#form
About This Article

To write a medical research paper, research your topic thoroughly and compile your data. Next, organize your notes and create a strong outline that breaks up the information into sections and subsections, addressing one main point per section. Write the results and discussion sections first to go over your findings, then write the introduction to state your objective and provide background information. Finally, write the abstract, which concisely summarizes the article by highlighting the main points. For tips on formatting and using citations, read on! Did this summary help you? Yes No
- Send fan mail to authors
Reader Success Stories
Joshua Benibo
Jun 5, 2018
Did this article help you?

Dominic Cipriano
Aug 16, 2016
Obiajulu Echedom
Apr 2, 2017
Noura Ammar Alhossiny
Feb 14, 2017
Dawn Daniel
Apr 20, 2017

Featured Articles

Trending Articles

Watch Articles

- Terms of Use
- Privacy Policy
- Do Not Sell or Share My Info
- Not Selling Info
Get all the best how-tos!
Sign up for wikiHow's weekly email newsletter
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 11 August 2020
Improving the accuracy of medical diagnosis with causal machine learning
- Jonathan G. Richens ORCID: orcid.org/0000-0001-8755-2286 1 ,
- Ciarán M. Lee 1 , 2 &
- Saurabh Johri ORCID: orcid.org/0000-0002-8240-2075 1
Nature Communications volume 11 , Article number: 3923 ( 2020 ) Cite this article
92k Accesses
186 Citations
931 Altmetric
Metrics details
- Predictive medicine
An Author Correction to this article was published on 31 March 2021
A Publisher Correction to this article was published on 16 September 2020
This article has been updated
Machine learning promises to revolutionize clinical decision making and diagnosis. In medical diagnosis a doctor aims to explain a patient’s symptoms by determining the diseases causing them. However, existing machine learning approaches to diagnosis are purely associative, identifying diseases that are strongly correlated with a patients symptoms. We show that this inability to disentangle correlation from causation can result in sub-optimal or dangerous diagnoses. To overcome this, we reformulate diagnosis as a counterfactual inference task and derive counterfactual diagnostic algorithms. We compare our counterfactual algorithms to the standard associative algorithm and 44 doctors using a test set of clinical vignettes. While the associative algorithm achieves an accuracy placing in the top 48% of doctors in our cohort, our counterfactual algorithm places in the top 25% of doctors, achieving expert clinical accuracy. Our results show that causal reasoning is a vital missing ingredient for applying machine learning to medical diagnosis.
Similar content being viewed by others
A novel method for causal structure discovery from EHR data and its application to type-2 diabetes mellitus
Xinpeng Shen, Sisi Ma, … Gyorgy J. Simon

Theory and rationale of interpretable all-in-one pattern discovery and disentanglement system
Andrew K. C. Wong, Pei-Yuan Zhou & Annie E.-S. Lee
Second opinion needed: communicating uncertainty in medical machine learning
Benjamin Kompa, Jasper Snoek & Andrew L. Beam
Introduction
Providing accurate and accessible diagnoses is a fundamental challenge for global healthcare systems. In the US alone an estimated 5% of outpatients receive the wrong diagnosis every year 1 , 2 . These errors are particularly common when diagnosing patients with serious medical conditions, with an estimated 20% of these patients being misdiagnosed at the level of primary care 3 and one in three of these misdiagnoses resulting in serious patient harm 1 , 4 .
In recent years, artificial intelligence and machine learning have emerged as powerful tools for solving complex problems in diverse domains 5 , 6 , 7 . In particular, machine learning assisted diagnosis promises to revolutionise healthcare by leveraging abundant patient data to provide precise and personalised diagnoses 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 . Despite significant research efforts and renewed commercial interest, diagnostic algorithms have struggled to achieve the accuracy of doctors in differential diagnosis 17 , 18 , 19 , 20 , 21 , 22 , 23 , where there are multiple possible causes of a patients symptoms.
This raises the question, why do existing approaches struggle with differential diagnosis? All existing diagnostic algorithms, including Bayesian model-based and Deep Learning approaches, rely on associative inference—they identify diseases based on how correlated they are with a patients symptoms and medical history. This is in contrast to how doctors perform diagnosis, selecting the diseases which offer the best causal explanations for the patients symptoms. As noted by Pearl, associative inference is the simplest in a hierarchy of possible inference schemes 24 , 25 , 26 . Counterfactual inference sits at the top of this hierarchy, and allows one to ascribe causal explanations to data. Here, we argue that diagnosis is fundamentally a counterfactual inference task. We show that failure to disentangle correlation from causation places strong constraints on the accuracy of associative diagnostic algorithms, sometimes resulting in sub-optimal or dangerous diagnoses. To resolve this, we present a causal definition of diagnosis that is closer to the decision making of clinicians, and derive counterfactual diagnostic algorithms to validate this approach.
We compare the accuracy of our counterfactual algorithms to a state-of-the-art associative diagnostic algorithm and a cohort of 44 doctors, using a test set of 1671 clinical vignettes. In our experiments, the doctors achieve an average diagnostic accuracy of 71.40%, while the associative algorithm achieves a similar accuracy of 72.52%, placing in the top 48% of doctors in our cohort. However, our counterfactual algorithm achieves an average accuracy of 77.26%, placing in the top 25% of the cohort and achieving expert clinical accuracy. These improvements are particularly pronounced for rare diseases, where diagnostic errors are more common and often more serious, with the counterfactual algorithm providing a better diagnosis for 29.2% of rare and 32.9% of very-rare diseases compared to the associative algorithm.
Importantly, the counterfactual algorithm achieves these improvements using the same disease model as the associative algorithm—only the method for querying the model has changed. This backwards compatibility is particularly important as disease models require significant resources to learn 20 . Our algorithms can thus be applied as an immediate upgrade to existing Bayesian diagnostic models, even those outside of medicine 27 , 28 , 29 , 30 .
Associative diagnosis
Here, we outline the basic principles and assumptions underlying the current approach to algorithmic diagnosis. We then detail scenarios where this approach breaks down due to causal confounding, and propose a set of principles for designing diagnostic algorithms that overcome these pitfalls. Finally, we use these principles to propose two diagnostic algorithms based on the notions of necessary and sufficient causation.
Since its formal definition 31 , model-based diagnosis has been synonymous with the task of using a model θ to estimate the likelihood of a fault component D given findings \({\mathcal{E}}\) 32 ,
In medical diagnosis D represents a disease or diseases, and findings \({\mathcal{E}}\) can include symptoms, tests outcomes and relevant medical history. In the case of diagnosing over multiple possible diseases, e.g., in a differential diagnosis, potential diseases are ranked in terms of their posterior. Model-based diagnostic algorithms are either discriminative, directly modelling the conditional distribution of diseases D given input features \({\mathcal{E}}\) ( 1 ), or generative, modelling the prior distribution of diseases and findings and using Bayes rule to estimate the posterior,
Examples of discriminative diagnostic models include neural network and deep learning models 8 , 10 , 15 , 33 , 34 , whereas generative models are typically Bayesian networks 18 , 19 , 21 , 22 , 27 , 35 , 36 .
How does this approach compare to how doctors perform diagnosis? It has long been argued that diagnosis is the process of finding causal explanations for a patient’s symptoms 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 . For example 37 , concludes “The generation of hypotheses is by habitual abduction. The physician relies on her knowledge of possible causes that explain the symptoms”. Likewise 48 defines diagnosis as “the investigation or analysis of the cause or nature of a condition, situation, or problem”. That is, given the evidence presented by the patient, a doctor attempts to determine the diseases that are the best explanation—the most likely underlying cause—of the symptoms presented. We propose the following causal definition of diagnosis,
The identification of the diseases that are most likely to be causing the patient’s symptoms, given their medical history .
Despite the wealth of literature placing causal reasoning at the centre of diagnosis, to the best of our knowledge there are no existing approaches to model-based diagnosis that employ modern causal analysis techniques 49 , 50 .
It is well known that using the posterior to identify causal relations can lead to spurious conclusions in all but the simplest causal scenarios—a phenomenon known as confounding 51 . For example, Fig. 1 a shows a disease D which is a direct cause of a symptom S . In this scenario, D is a plausible explanation for S , and treating D could alleviate symptom S . In Fig. 1 b, variable R is a confounder for D and S , for example R could be a genetic factor which increases a patients chance of developing disease D and experiencing symptom S . Although D and S can be strongly correlated in this scenario, P ( D = T ∣ S = T ) ≫ P ( D = T ) (where D = T denotes the presence of D ), D cannot have caused symptom S and so would not constitute a reasonable diagnosis. In general, diseases are related to symptoms by both directed and common causes that cannot be simply disentangled, as shown in Fig. 1 c). The posterior ( 1 ) does not differentiate between these different scenarios and so is insufficient for assigning a diagnosis to a patient’s symptoms in all but the simplest of cases, and especially when there are multiple possible causes for a patient’s symptoms.
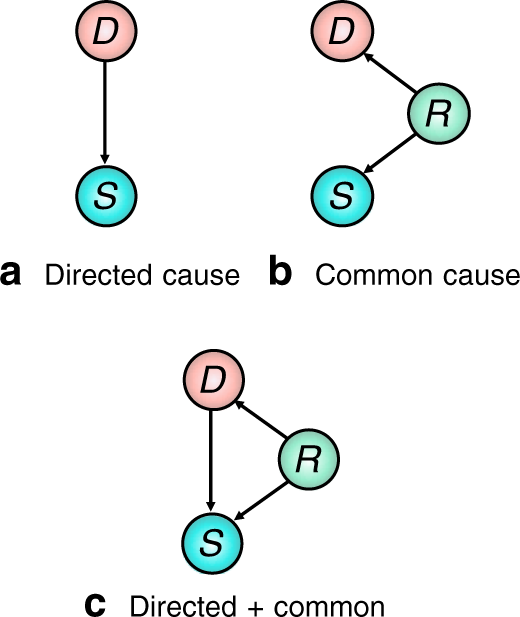
a Disease D is a direct cause of symptom S , b D does not cause symptom S , but they are correlated by a latent common cause R , c D is a direct cause of S and a latent common cause R is present.
Example 1: An elderly smoker reports chest pain, nausea, and fatigue. A good doctor will present a diagnosis that is both likely and relevant given the evidence (such as angina). Although this patient belongs to a population with a high prevalence of emphysema, this disease is unlikely to have caused the symptoms presented and should not be put forward as a diagnosis. Emphysema is positively correlated with the patient’s symptoms, but this is primarily due to common causes 52 .
Example 2: Ref. 53 found that asthmatic patients who were admitted to hospital for pneumonia were more aggressively treated for the infection, lowering the sub-population mortality rate. An associative model trained on this data to diagnose pneumonia will learn that asthma is a protective risk factor—a dangerous conclusion that could result in a less aggressive treatment regime being proposed for asthmatics, despite the fact that asthma increases the risk of developing pneumonia. In this example, the confounding factor is the unobserved level of care received by the patient.
Real-world examples of confounding, such as Examples 1 and 2, have lead to increasing calls for causal knowledge to be properly incorporated into decision support algorithms in healthcare 54 .
Principles for diagnostic reasoning
An alternative approach to associative diagnosis is to reason about causal responsibility (or causal attribution)—the probability that the occurrence of the effect S was in fact brought about by target cause D 55 . This requires a diagnostic measure \({\mathcal{M}}(D,{\mathcal{E}})\) for ranking the likelihood that a disease D is causing a patient’s symptoms given evidence \({\mathcal{E}}\) . We propose the following three minimal desiderata that should be satisfied by any such diagnostic measure,
The likelihood that a disease D is causing a patient’s symptoms should be proportional to the posterior likelihood of that disease \({\mathcal{M}}(D,{\mathcal{E}})\propto P(D=T| {\mathcal{E}})\) (consistency),
A disease D that cannot cause any of the patient’s symptoms cannot constitute a diagnosis, \({\mathcal{M}}(D,{\mathcal{E}})=0\) (causality),
Diseases that explain a greater number of the patient’s symptoms should be more likely (simplicity).
The justification for these desiderata is as follows. Desideratum i) states that the likelihood that a disease explains the patient’s symptoms is proportional to the likelihood that the patient has the disease in the first place. Desideratum ii) states that if there is no causal mechanism whereby disease D could have generated any of the patient’s symptoms (directly or indirectly), then D cannot constitute causal explanation of the symptoms and should be disregarded. Desideratum iii) incorporates the principle of Occam’s razor—favouring simple diagnoses with few diseases that can explain many of the symptoms presented. Note that the posterior only satisfies the first desiderata, violating the last two.
Counterfactual diagnosis
To quantify the likelihood that a disease is causing the patient’s symptoms, we employ counterfactual inference 56 , 57 , 58 . Counterfactuals can test whether certain outcomes would have occurred had some precondition been different. Given evidence \({\mathcal{E}}=e\) we calculate the likelihood that we would have observed a different outcome \({\mathcal{E}}=e^{\prime}\) , counter to the fact \({\mathcal{E}}=e\) , had some hypothetical intervention taken place. The counterfactual likelihood is written \(P({\mathcal{E}}=e^{\prime} \ | \ {\mathcal{E}}=e,{\rm{do}}(X\ =\ x))\) where do( X = x ) denotes the intervention that sets variable X to the value X = x , as defined by Pearl’s calculus of interventions 49 (see Supplementary Note 3 for formal definitions).
Counterfactuals provide us with the language to quantify how well a disease hypothesis D = T explains symptom evidence S = T by determining the likelihood that the symptom would not be present if we were to intervene and ‘cure’ the disease by setting do( D = F ), given by the counterfactual probability P ( S = F ∣ S = T , do( D = F )). If this probability is high, D = T constitutes a good causal explanation of the symptom. Note that this probability refers to two contradictory states of S and so cannot be represented as a standard posterior 49 , 59 . In Supplementary Note 3 we describe how these counterfactual probabilities are calculated.
Inspired by this example, we propose two counterfactual diagnostic measures, which we term the expected disablement and expected sufficiency. We show in Theorem 1 at the end of this section that both measures satisfy all three of our desiderata.
Definition 1 (Expected disablement) The expected disablement of disease D is the number of present symptoms that we would expect to switch off if we intervened to cure D ,
where \({\mathcal{E}}\) is the factual evidence and \({{\mathcal{S}}}_{+}\) is the set of factual positively evidenced symptoms. The summation is calculated over all possible counterfactual symptom evidence states \({\mathcal{S}}^{\prime}\) and \({{\mathcal{S}}}_{+}^{\prime}\) denotes the positively evidenced symptoms in the counterfactual symptom state. do ( D = F ) denotes the counterfactual intervention setting D → F . \(\left|{{\mathcal{S}}}_{+}\setminus {{\mathcal{S}}}_{+}^{\prime} \right|\) denotes the cardinality of the set of symptoms that are present in the factual symptom evidence but are not present in the counterfactual symptom evidence.
The expected disablement derives from the notion of necessary cause 50 , whereby D is a necessary cause of S if S = T if and only if D = T . The expected disablement therefore captures how well disease D alone can explain the patient’s symptoms, as well as the likelihood that treating D alone will alleviate the patient’s symptoms.
Definition 2 (expected sufficiency) The expected sufficiency of disease D is the number of positively evidenced symptoms we would expect to persist if we intervene to switch off all other possible causes of the patient’s symptoms,
where the summation is over all possible counterfactual symptom evidence states \({\mathcal{S}}^{\prime}\) and \({{\mathcal{S}}}_{+}^{\prime}\) denotes the positively evidenced symptoms in the counterfactual symptom state. \({\mathsf{Pa}}({{\mathcal{S}}}_{+})\setminus D\) denotes the set of all direct causes of the set of positively evidenced symptoms excluding disease D , and \({do}({\mathsf{Pa}}({{\mathcal{S}}}_{+})\setminus D=F)\) denotes the counterfactual intervention setting all \({\mathsf{Pa}}({{\mathcal{S}}}_{+}^{\prime} \setminus D)\to F\) . \({\mathcal{E}}\) denotes the set of all factual evidence. \(\left|{{\mathcal{S}}}_{+}^{\prime} \right|\) denotes the cardinality of the set of present symptoms in the counterfactual symptom evidence.
The expected sufficiency derives from the notion of sufficient cause 50 , whereby D is a sufficient cause of S if the presence of D can cause subsequent occurrence of S but, as S can have multiple causes, the presence of S does not imply the prior occurrence of D . Note the use of sufficiency here is in line with 60 and does not refer to the INUS conditions \cite{mackie1974cement}. Typically, diseases are sufficient causes of symptoms (see Supplementary Note 4 for further discussion). By performing counterfactual interventions to remove all possible causes of the symptoms (both diseases and exogenous influences), the only remaining cause is D and so we isolate its effect as a sufficient cause in our model. If we cannot assume that a disease is a sufficient cause of its symptoms, the expected disablement should be used. See Supplementary Note 8 for comparison of the expected disablement and sufficiency to other counterfactual measures. See Supplementary Note 9 for comparisons of the expected disablement and sufficiency and the posterior in some simple diagnostic models.
Theorem 1 (Diagnostic properties of expected disablement and expected sufficiency). Expected disablement and expected sufficiency satisfy the three desiderata .
The proof is provided in Supplementary Notes 5 and 7 .
Structural causal models for diagnosis
We now introduce the statistical disease models we use to test the diagnostic measures outlined in the previous sections. We then derive simplified expressions for the expected disablement and sufficiency in these models.
The disease models we use in our experiments are Bayesian Networks (BNs) that model the relationships between hundreds of diseases, risk factors and symptoms. BNs are widely employed as diagnostic models as they are interpretable and explicitly encode causal relations between variables—a prerequisite for causal and counterfactual analysis 49 . These models typically represent diseases, symptoms and risk factors as binary nodes that are either on (true) or off (false). We denote true and false with the standard integer notation 1 and 0 respectively.
A BN is specified by a directed acyclic graph (DAG) and a joint probability distribution over all nodes which factorises with respect to the DAG structure. If there is a directed arrow from node X to Y , then X is said to be a parent of Y , and Y to be a child of X . A node Z is said to be an ancestor of Y if there is a directed path from Z to Y . A simple example BN is shown in Fig. 2 a, which depicts a BN modelling diseases, symptoms, and risk factors (the causes of diseases).
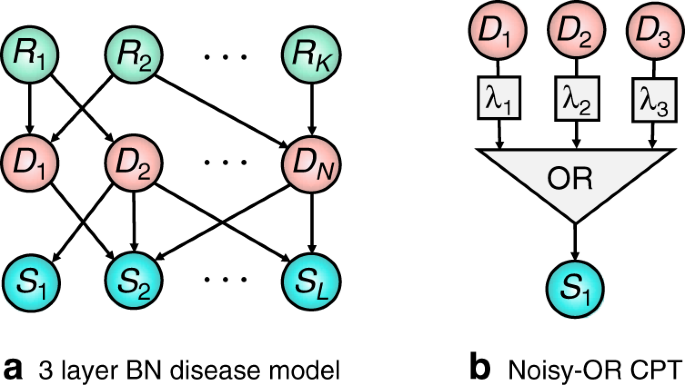
a Three-layer Bayesian network representing risk factors R i , diseases D j and symptoms S k . b noisy-OR CPT. S is the Boolean OR function of its parents, each with an independent probability λ i of being ignored, removing them from the OR function.
BN disease models have a long history going back to the INTERNIST-1 18 , Quick Medical Reference (QMR) 19 , 20 , and PATHFINDER 21 , 22 systems, with many of the original systems corresponding to noisy-OR networks with only disease and symptom nodes, known as BN2O networks 36 . Recently, three-layer BNs as depicted in Fig. 2 a have replaced these two layer models 23 . These models make fewer independence assumptions and allow for disease risk factors to be included. While our results will be derived for these models, they can be simply extended to models with more or less complicated dependencies 19 , 61 .
In the field of causal inference, BNs are replaced by the more fundamental Structural Causal Models (SCMs), also referred to as Functional Causal Models and Structural Equation Models 59 , 62 . SCMs are widely applied and studied, and their relation to other approaches, such as probabilistic graphical models and BNs, is well understood 49 , 63 . The key characteristic of SCMs is that they represent each variable as deterministic functions of their direct causes together with an unobserved exogenous ‘noise’ term, which itself represents all causes outside of our model. That the state of the noise term is unknown induces a probability distribution over observed variables. For each variable Y , with parents in the model X , there is a noise term u Y , with unknown distribution P ( u Y ) such that Y = f ( x , u Y ) and \(P(Y=y| X=x)={\sum }_{{u}_{Y}:f(x,{u}_{Y}) = y}P({U}_{Y}={u}_{Y})\) .
By incorporating knowledge of the functional dependencies between variables, SCMs enable us to determine the response of variables to interventions (such as treatments). Note that counterfactuals cannot in general be identified from data alone, and require modelling assumptions such as knowledge of the underlying structural equations 58 , 64 . As we now show, existing diagnostic BNs such as BN2O networks 36 are naturally represented as SCMs.
Noisy-OR twin diagnostic networks
When constructing disease models it is common to make additional modelling assumptions beyond those implied by the DAG structure. The most widely used of these correspond to ‘noisy-OR’ models 19 . Noisy-OR models are routinely used for modelling in medicine, as they reflect basic intuitions about how diseases and symptoms are related 65 , 66 . In addition, they support efficient inference 67 and learning 68 , 69 , and allow for large BNs to be described by a number of parameters that grows linearly with the size of the network 68 , 70 . Under the noisy-OR assumption, a parent D i activates its child S (causing S = 1) if (i) the parent is on, D i = 1, and (ii) the activation does not randomly fail. The probability of failure, conventionally denoted as \({\lambda }_{{D}_{i},S}\) , is independent from all other model parameters. The ‘OR’ component of the noisy-OR states that the child is activated if any of its parents successfully activate it. Concretely, the value s of S is the Boolean OR function ∨ of its parents activation functions, s = ∨ i f ( d i , u i ), where the activation functions take the form \(f({d}_{i},{u}_{i})={d}_{i}\wedge {\bar{u}}_{i}, \wedge\) denotes the Boolean AND function, d i ∈ {0, 1} is the state of a given parent D i and u i ∈ {0, 1} is a latent noise variable ( \({\bar{u}}_{i}:= 1-{u}_{i}\) ) with a probability of failure \(P({u}_{i}=1)={\lambda }_{{D}_{i},S}\) . The noisy-OR model is depicted in Fig. 1 b. Intuitively, the noisy-OR model captures the case where a symptom only requires a single activation to switch it on, and ‘switching on’ a disease will never ‘switch off’ a symptom. For further details on noisy-OR disease modelling see Supplementary Note 2 .
We now derive expressions for the expected disablement and expected sufficiency for these models using twin-networks method for computing counterfactuals introduced in 64 , 71 . This method represents real and counterfactual variables together in a single SCM—the twin network—from which counterfactual probabilities can be computed using standard inference techniques. This approach greatly amortizes the inference cost of calculating counterfactuals compared to abduction 49 , 72 , which is intractable for large SCMs. We refer to these diagnostic models as twin diagnostic networks, see Supplementary Note 3 for further details.
Theorem 2 For 3-layer noisy-OR BNs (formally described in Supplementary Notes 2 and 3 , the expected sufficiency and expected disablement of disease D k are given by
where for the expected sufficiency
and for the expected disablement
where \({{\mathcal{S}}}_{\pm }\) denotes the positive and negative symptom evidence, \({\mathcal{R}}\) denotes the risk-factor evidence, and \({\lambda }_{{D}_{k},S}\) is the noise parameter for D k and S .
The proof is provided by Theorem 2 in Supplementary Note 4 and by Theorem 4 in Supplementary Note 6 .
Experiments
Here we outline our experiments comparing the expected disablement and sufficiency to posterior inference using the models outlined in the previous section. We introduce our test set which includes a set of clinical vignettes and a cohort of doctors. We then evaluate our algorithms across several diagnostic tasks.
Diagnostic model and datasets
One approach to validating diagnostic algorithms is to use electronic health records (EHRs) 8 , 9 , 10 , 11 , 12 . A key limitation of this approach is the difficulty in defining the ground truth diagnosis, where diagnostic errors result in mislabeled data. This problem is particularly pronounced for differential diagnoses because of the large number of candidate diseases and hence diagnostic labels, incomplete or inaccurate recording of case data, high diagnostic uncertainty and ambiguity, and biases such as the training and experience of the clinician who performed the diagnosis.
To resolve these issues, a standard method for assessing doctors is through the examination of simulated diagnostic cases or clinical vignettes 73 . A clinical vignette simulates a typical patient’s presentation of a disease, containing a non-exhaustive list of evidence including symptoms, medical history, and basic demographic information such as age and birth gender 23 . This approach is often more robust to errors and biases than real data sets such as EHRs, as the task of simulating a disease given its known properties is simpler than performing a differential diagnosis, and has been found to be effective for evaluating human doctors 73 , 74 , 75 , 76 and comparing the accuracy of doctors to symptom checker algorithms 17 , 23 , 77 , 78 .
We use a test set of 1671 clinical vignettes, generated by a separate panel of doctors qualified at least to the level of general practitioner (equivalent to board certified primary care physicians). The vignettes are generated independently of the assumptions underlying our disease model. Where possible, symptoms and risk factors match those in our disease model. However, to avoid biasing our study the vignettes include any additional clinical information as case notes, which are available to the doctors in our experiments. Each vignette is authored by a single doctor and then verified by multiple doctors to ensure that it represents a realistic diagnostic case. See Supplementary Note 10 for an example vignette. For each vignette the true disease is masked and the algorithm returns a diagnosis in the form of a full ranking of all modelled diseases using the vignette evidence. The disease ranking is computed using the posterior for the associative algorithm, and the expected disablement or expected sufficiency for the counterfactual algorithms. Doctors provide an independent differential diagnosis in the form of a partially ranked list of candidate diseases.
In all experiments the counterfactual and associative algorithms use identical disease models to ensure that any difference in diagnostic accuracy is due to the ranking query used. The disease model used is a three-layer noisy-OR diagnostic BN as described above and in Supplementary Note 2 . The BN is parameterised by a team of doctors and epidemiologists 23 , 78 . The model is specified independently of the test set of vignettes. The prior probabilities of diseases and risk factors are obtained from epidemiological data, and conditional probabilities are obtained through elicitation from multiple independent medical sources and doctors. The expected disablement and expected sufficiency are calculated using Theorem 2.
Counterfactual vs associative rankings
Our first experiment compares the diagnostic accuracy of ranking diseases using the posterior ( 1 ), expected disablement and expected sufficiency ( 5 ). For each of the 1671 vignettes the top- k ranked diseases are computed, with k = 1, …20, and the top- k accuracy is calculated as fraction of the 1671 diagnostic vignettes where the true disease is present in the k -top ranking. The results are presented in Fig. 3 . The expected disablement and expected sufficiency give almost identical accuracies for all k on our test set, and for the sake of clarity we present the results for the expected sufficiency alone. The reasons for the similarity of these two measures on our test set is discussed in Supplementary Note 9 . A complete table of results is present in the Supplementary Table 1 .
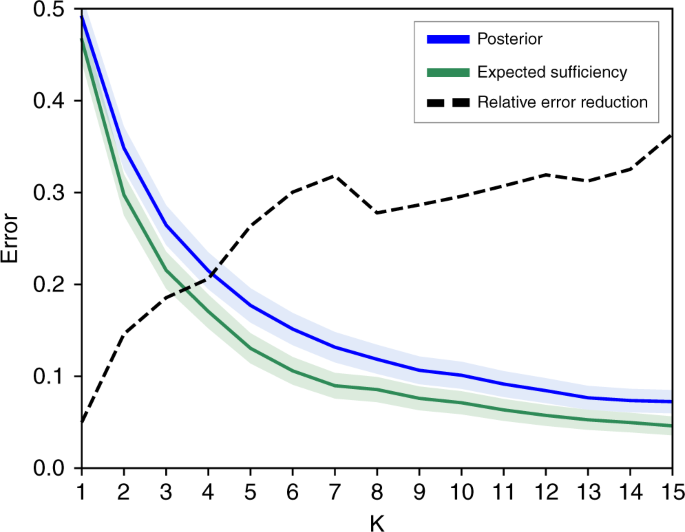
Figure shows the top k error (1—accuracy) of the counterfactual (green line) and associative (blue line) algorithms over all 1671 vignettes vs k . Shaded regions give 95% confidence intervals. The black dashed line shows the relative reduction in error when switching from the associative to counterfactual algorithm, given by 1 − e c / e a where e a is the error rate of the associative algorithm, and e c is the error rate of the counterfactual algorithm. Results shown for k = 1, …15, for complete results see the supplementary table 1 .
For k = 1, returning the top ranked disease, the counterfactual algorithm achieves a 2.5% higher accuracy than the associative algorithm. For k > 1 the performance of the two algorithms diverge, with the counterfactual algorithm giving a large reduction in the error rate over the associative algorithm. For k > 5, the counterfactual algorithm reduces the number of misdiagnoses by ~30% compared to the associative algorithm. This suggests that the best candidate disease is reasonably well identified by the posterior, but the counterfactual ranking is significantly better at identifying the next most likely diseases. These secondary candidate diseases are especially important in differential diagnosis for the purposes of triage and determining optimal testing and treatment strategies.
A simple method for comparing two rankings is to compare the position of the true disease in the rankings. Across all 1671 vignettes we found that the counterfactual algorithm ranked the true disease higher than the associative algorithm in 24.7% of vignettes, and lower in only 1.9% of vignettes. On average the true disease is ranked in position 3.16 ± 4.4 by the counterfactual algorithm, a substantial improvement over 3.81 ± 5.25 for the associative algorithm (see Table 1 ).
In Table 1 we stratify the vignettes by the prior incidence rates of the true disease by very common, common, uncommon, rare and very rare. While the counterfactual algorithm achieves significant improvements over the associative algorithm for both common and rare diseases, the improvement is particularly large for rare and very-rare diseases, achieving a higher ranking for 29.2% and 32.9% of these vignettes respectively. This improvement is important as rare diseases are typically harder to diagnose and include many serious conditions where diagnostic errors have the greatest consequences.
Comparing to doctors
Our second experiment compares the counterfactual and associative algorithms to a cohort of 44 doctors. Each doctor is assigned a set of at least 50 vignettes (average 159), and returns an independent diagnosis for each vignette in the form of a partially ranked list of k diseases, where the size of the list k is chosen by the doctor on a case-by-case basis (average diagnosis size is 2.58 diseases). For a given doctor, and for each vignette diagnosed by the doctor, the associative and counterfactuals algorithms are supplied with the same evidence (excluding the free text case description) and each returns a top- k diagnosis, where k is the size of the diagnosis provided by the doctor. Matching the precision of the doctor for every vignette allows us to compare the accuracy of the doctor and the algorithms without constraining the doctors to give a fixed number of diseases for each diagnosis. This is important as doctors will naturally vary the size k of their diagnosis to reflect their uncertainty in the diagnostic vignette.
The complete results for each of the 44 doctors, and for the posterior, expected disablement, and expected sufficiency ranking algorithms are included in the Supplementary Table 3 . Figure 4 compares the accuracy of each doctor to the associative and counterfactual algorithms. Each point gives the average accuracy for one of the 44 doctors, calculated as the proportion of vignettes diagnosed by the doctor where the true disease is included in the doctor’s differential. This is plotted against the accuracy that the corresponding algorithm achieved when diagnosing the same vignettes and returning differentials of the same size as that doctor.
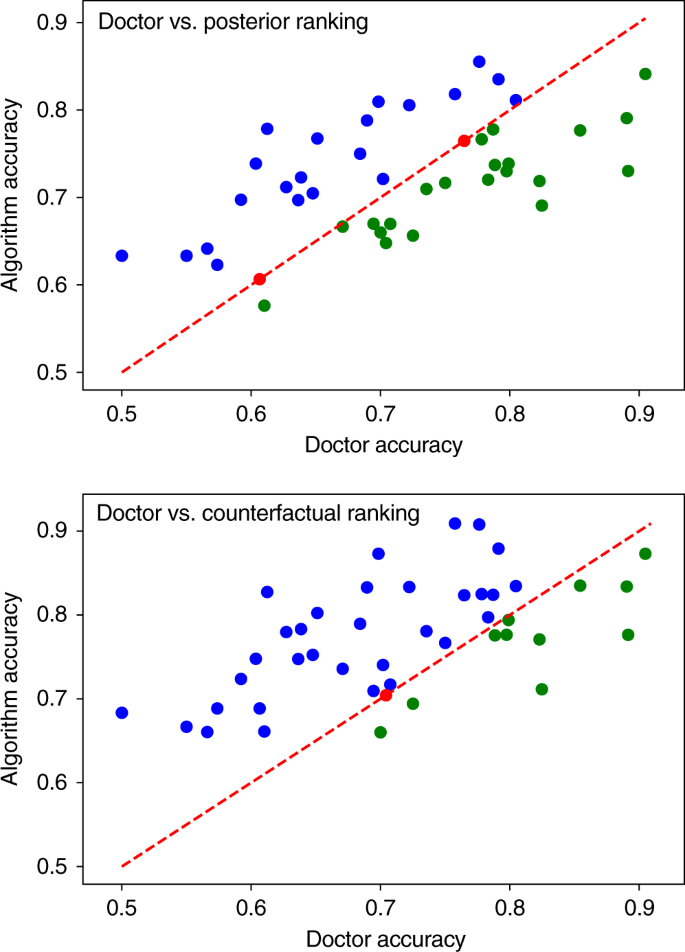
Figure shows the mean accuracy for each of the 44 doctors, compared to the posterior ranking (top) and expected sufficiency ranking (bottom) algorithms. The line y = x gives a reference for comparing the accuracy of each doctor to the algorithm shadowing them. Points above the line correspond to doctors who achieved a lower accuracy than the algorithm (blue), points on the line are doctors that achieved the same accuracy as the algorithm (red), and below the line are doctors that achieved higher accuracy than the algorithm (green). The linear correlation can be explained by the variation in the difficulty of the sets of vignettes diagnosed by each doctor. Sets of easier/harder vignettes results in higher/lower doctor and algorithm accuracy scores. As the results for the expected disablement and expected sufficiency are almost identical, we show only the results for the expected sufficiency. Complete results are listed in the Supplementary Table 3 . All figures generated using matplotlib version 3.2.1.
Doctors tend to achieve higher accuracies in case sets involving simpler vignettes—identified by high doctor and algorithm accuracies. Conversely, the algorithm tends to achieve higher accuracy than the doctors for more challenging vignettes—identified by low doctor and algorithm accuracies. This suggests that the diagnostic algorithms are complimentary to the doctors, with the algorithm performing better on vignettes where doctor error is more common and vice versa.
Overall, the associative algorithm performs on par with the average doctor, achieving a mean accuracy across all trails of 72.52 ± 2.97% vs 71.4 ± 3.01% for doctors. The algorithm scores higher than 21 of the doctors, draws with 2 of the doctors, and scores lower than 21 of the doctors. The counterfactual algorithm achieves a mean accuracy of 77.26 ± 2.79%, considerably higher than the average doctor and the associative algorithm, placing it in the top 25% of doctors in the cohort. The counterfactual algorithm scores higher than 32 of the doctors, draws with 1, and scores a lower accuracy than 12 (see Table 2 ).
In summary, we find that the counterfactual algorithm achieves a substantially higher diagnostic accuracy than the associative algorithm. We find the improvement is particularly pronounced for rare diseases. While the associative algorithm performs on par with the average doctor, the counterfactual algorithm places in the upper quartile of doctors.
Poor access to primary healthcare and errors in differential diagnoses represent a significant challenge to global healthcare systems 1 , 2 , 3 , 4 , 79 , 80 . If machine learning is to help overcome these challenges, it is important that we first understand how diagnosis is performed and clearly define the desired output of our algorithms. Existing approaches have conflated diagnosis with associative inference. While the former involves determining the underlying cause of a patient’s symptoms, the latter involves learning correlations between patient data and disease occurrences, determining the most likely diseases in the population that the patient belongs to. While this approach is perhaps sufficient for simple causal scenarios involving single diseases, it places strong constraints on the accuracy of these algorithms when applied to differential diagnosis, where a clinician chooses from multiple competing disease hypotheses. Overcoming these constraints requires that we fundamentally rethink how we define diagnosis and how we design diagnostic algorithms.
We have argued that diagnosis is fundamentally a counterfactual inference task and presented a causal definition of diagnosis. We have derived two counterfactual diagnostic measures, expected disablement and expected sufficiency, and a class of diagnostic models—twin diagnostic networks—for calculating these measures. Using existing diagnostic models we have demonstrated that ranking disease hypotheses by these counterfactual measures greatly improves diagnostic accuracy compared to standard associative rankings. While the associative algorithm performed on par with the average doctor in our cohort, the counterfactual algorithm places in the top 25% of doctors in our cohort—achieving expert clinical accuracy. The improvement is particularly pronounced for rare and very-rare diseases, where diagnostic errors are typically more common and more serious, with the counterfactual algorithm ranking the true disease higher than the associative algorithm in 29.2% and 32.9% of these cases respectively. Importantly, this improvement comes ‘for free’, without requiring any alterations to the disease model. Because of this backward compatibility our algorithm can be used as an immediate upgrade for existing Bayesian diagnostic algorithms including those outside of the medical setting 27 , 28 , 29 , 30 , 81 .
Whereas other approaches to improving clinical decision systems have focused on developing better model architectures or exploiting new sources of data, our results demonstrate a new path towards expert-level clinical decision systems—changing how we query our models to leverage causal knowledge. Our results add weight to the argument that machine learning methods that fail to incorporate causal reasoning will struggle to surpass the capabilities of human experts in certain domains 24 .
Our results present the first evidence of the superiority of counterfactual over associative reasoning in a complex real-world task. The question of how to incorporate causal and counterfactual reasoning into other machine learning methods beyond structural causal models, for example in Deep Learning for image classification 82 , 83 and deep generative models 84 , 85 , 86 , is an active area research. We hope that the results presented in our article will further motivate this area of research, by presenting a new application for improving diagnostic accuracy using counterfactual inference.
While we have focused on comparing our algorithms to doctors, future experiments could determine the effectiveness of these algorithms as clinical support systems—guiding doctors by providing a second opinion diagnosis. Given that our algorithm appears to be complimentary to human doctors, performing better on vignettes that doctors struggle to diagnose, it is likely that the combined diagnosis of doctor and algorithm will be more accurate than either alone.
The proofs and further exposition of our disease models and inference methods are contained in Supplementary Information . In Supplementary Note A and B we address the preliminaries and framework within which we derive our proofs, introducing the framework of structural causal models, defining noisy-OR networks as structural causal models, and detailing their assumptions with respect to disease modelling. In Supplementary Note C we introduce counterfactual inference in structural causal models and the twin-networks inference scheme, and derive the twin networks used to compute the expected disablement and sufficiency. In Supplementary Note D we derived the expression for the expected sufficiency and in Supplementary Note E we prove that it satisfies our desiderata. In Supplementary Note F we derived the expression for the expected disablement and in Supplementary Note E we prove that it satisfies our desiderata. In Supplementary Note J we provide an example of the clinical vignettes used in our experiments. In Supplementary Note K we provide our full experimental results.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The data that support the findings of this study are available on https://github.com/babylonhealth/counterfactual-diagnosis . Any features of the vignettes not used to generate the methods or results of the study have been removed or de-identified prior to sharing. Accredited researchers may request access to the complete clinical dataset for the purpose of checking the validity of the clinical vignettes used in the study by contacting the corresponding author. Access will be vetted by the Babylon Health access committee and will take place within the Babylon health intranet and under a non-disclosure agreement.
Code availability
The code used to generate results shown in this study is available at https://github.com/babylonhealth/counterfactual-diagnosis 87 .
Change history
31 march 2021.
A Correction to this paper has been published: https://doi.org/10.1038/s41467-021-21494-9
16 September 2020
A Correction to this paper has been published: https://doi.org/10.1038/s41467-020-18310-1
Singh, H., Meyer, A. N. & Thomas, E. J. The frequency of diagnostic errors in outpatient care: estimations from three large observational studies involving us adult populations. BMJ Qual. Saf. 23 , 727–731 (2014).
Article PubMed PubMed Central Google Scholar
Singh, H., Schiff, G. D., Graber, M. L., Onakpoya, I. & Thompson, M. J. The global burden of diagnostic errors in primary care. BMJ Qual. Saf. 26 , 484–494 (2017).
Article PubMed Google Scholar
Graber, M. L. The incidence of diagnostic error in medicine. BMJ Qual. Saf. 22 , ii21–ii27 (2013).
Singh, H. et al. Types and origins of diagnostic errors in primary care settings. JAMA Intern. Med. 173 , 418–425 (2013).
Silver, D. et al. Mastering the game of go without human knowledge. Nature 550 , 354 (2017).
Article ADS CAS PubMed Google Scholar
Brown, N. & Sandholm, T. Superhuman ai for multiplayer poker. Science eaay2400, (2019).
Tomašev, N. et al. A clinically applicable approach to continuous prediction of future acute kidney injury. Nature 572 , 116 (2019).
Article ADS PubMed PubMed Central CAS Google Scholar
Liang, H. et al. Evaluation and accurate diagnoses of pediatric diseases using artificial intelligence. Nat. Med. 1 , 433–438 (2019).
Article CAS Google Scholar
Topol, E. J. High-performance medicine: the convergence of human and artificial intelligence. Nat. Med. 25 , 44 (2019).
Article CAS PubMed Google Scholar
De Fauw, J. et al. Clinically applicable deep learning for diagnosis and referral in retinal disease. Nat. Med. 24 , 1342 (2018).
Article PubMed CAS Google Scholar
Yu, K.-H., Beam, A. L. & Kohane, I. S. Artificial intelligence in healthcare. Nat. Biomed. Eng. 2 , 719 (2018).
Jiang, F. et al. Artificial intelligence in healthcare: past, present and future. Stroke Vasc. Neurol. 2 , 230–243 (2017).
Esteva, A. et al. A guide to deep learning in healthcare. Nat. Med. 25 , 24 (2019).
Zhang, Z. et al. Pathologist-level interpretable whole-slide cancer diagnosis with deep learning. Nat. Mach. Intell. 1 , 236–245 (2019).
Article Google Scholar
Litjens, G. et al. Deep learning as a tool for increased accuracy and efficiency of histopathological diagnosis. Sci. Rep. 6 , 26286 (2016).
Article ADS CAS PubMed PubMed Central Google Scholar
Buchard, A. et al. Learning medical triage from clinicians using deep q-learning. Preprint at https://arxiv.org/abs/2003.12828 (2020).
Semigran, H. L., Levine, D. M., Nundy, S. & Mehrotra, A. Comparison of physician and computer diagnostic accuracy. JAMA Intern. Med. 176 , 1860–1861 (2016).
Miller, R. A., McNeil, M. A., Challinor, S. M., Masarie, F. E. Jr & Myers, J. D. The internist 1 quick medical reference project status report. West. J. Med. 145 , 816 (1986).
CAS PubMed PubMed Central Google Scholar
Shwe, M. A. et al. Probabilistic diagnosis using a reformulation of the internist-1/qmr knowledge base. Methods Inf. Med. 30 , 241–255 (1991).
Miller, R. A history of the internist-1 and quick medical reference (qmr) computer-assisted diagnosis projects, with lessons learned. Yearb. Med. Inform. 19 , 121–136 (2010).
Heckerman, D. E., Horvitz, E. J. & Nathwani, B. N. Toward normative expert systems: Part i the pathfinder project. Methods Inf. Med. 31 , 90–105 (1992).
Razzaki, S. et al. A comparative study of artificial intelligence and human doctors for the purpose of triage and diagnosis. Preprint at https://arxiv.org/abs/1806.10698 (2018).
Pearl, J. Theoretical impediments to machine learning with seven sparks from the causal revolution. Preprint at https://arxiv.org/abs/1801.04016 (2018).
Greenland, S. For and against methodologies: some perspectives on recent causal and statistical inference debates. Eur. J. Epidemiol. 32 , 3–20 (2017).
Gigerenzer, G. & Marewski, J. N. Surrogate science: the idol of a universal method for scientific inference. J. Manag. 41 , 421–440 (2015).
Google Scholar
Cai, B., Huang, L. & Xie, M. Bayesian networks in fault diagnosis. IEEE Trans. Ind. Inform. 13 , 2227–2240 (2017).
Yongli, Z., Limin, H. & Jinling, L. Bayesian networks-based approach for power systems fault diagnosis. IEEE Trans. Power Deliv. 21 , 634–639 (2006).
Dey, S. & Stori, J. A bayesian network approach to root cause diagnosis of process variations. Int. J. Mach. Tools Manuf. 45 , 75–91 (2005).
Cai, B. et al. Multi-source information fusion based fault diagnosis of ground-source heat pump using bayesian network. Appl. Energy 114 , 1–9 (2014).
Article ADS Google Scholar
Reiter, R. A theory of diagnosis from first principles. Artif. Intell. 32 , 57–95 (1987).
Article MathSciNet MATH Google Scholar
de Kleer, J. Using crude probability estimates to guide diagnosis. Artif. Intell. 45 , 381–391 (1990).
Liu, S. et al. Early diagnosis of alzheimer’s disease with deep learning. In 2014 IEEE 11th international symposium on biomedical imaging (ISBI) , 1015–1018 (IEEE, 2014).
Wang, D., Khosla, A., Gargeya, R., Irshad, H. & Beck, A. H. Deep learning for identifying metastatic breast cancer. Preprint at https://arxiv.org/abs/1606.05718 (2016).
Kahn, C. E. Jr, Roberts, L. M., Shaffer, K. A. & Haddawy Construction of a bayesian network for mammographic diagnosis of breast cancer. Computers Biol. Med. 27 , 19–29 (1997).
Morris, Q. Recognition networks for approximate inference in bn20 networks. In Proc. Seventeenth Conference on Uncertainty in Artificial Intelligence (eds Breese, J. & Koller, D.) 370–377 (Seattle, Washington, USA, Morgan Kaufmann Publishers Inc., 2001).
Stanley, D. E. & Campos, D. G. The logic of medical diagnosis. Perspect. Biol. Med. 56 , 300–315 (2013).
Thagard. How Scientists Explain Disease (Princeton University Press, 2000).
Qiu, R.-Z. Models of explanation and explanation in medicine. Int. Stud. Philos. Sci. 3 , 199–212 (1989).
Cournoyea, M. & Kennedy, A. G. Causal explanatory pluralism and medically unexplained physical symptoms. J. Evaluation Clin. Pract. 20 , 928–933 (2014).
Kirmayer, L. J., Groleau, D., Looper, K. J. & Dao, M. D. Explaining medically unexplained symptoms. Can. J. Psychiatry 49 , 663–672 (2004).
Ledley, R. S. & Lusted, L. B. Reasoning foundations of medical diagnosis. Science 130 , 9–21 (1959).
Article ADS CAS PubMed MATH Google Scholar
Westmeyer, H. The diagnostic process as a statistical-causal analysis. Theory Decis. 6 , 57–86 (1975).
Article MATH Google Scholar
Rizzi, D. A. Causal reasoning and the diagnostic process. Theor. Med. 15 , 315–333 (1994).
Benzi, M. Medical diagnosis and actual causation. LPS-Log. Philos. Sci. 9 , 365–372 (2011).
Patil, R. S., Szolovits & Schwartz, W. B. Causal understanding of patient illness in medical diagnosis. IJCAI 81 , 893–899 (1981).
Davis, R. In Readings in Qualitative Reasoning about Physical Systems . (eds Weld, D.S. & de Kleer, J.) 535–541 (Elsevier, 1990).
Merriam-Webster, I. Merriam-Webster’s Medical Dictionary (Merriam-Webster, 1995).
Pearl, J. Causality (Cambridge University Press, 2009).
Halpern, J. Y. Actual Causality (MiT Press, 2016).
Pearl, J. Comment understanding simpson’s paradox. Am. Statistician 68 , 8–13 (2014).
Greenland, S. et al. Causal diagrams for epidemiologic research. Epidemiology 10 , 37–48 (1999).
Cooper, G. F. et al. Predicting dire outcomes of patients with community acquired pneumonia. J. Biomed. Inform. 38 , 347–366 (2005).
Ghassemi, M., Naumann, T., Schulam, Beam, A. L. & Ranganath, R. Opportunities in machine learning for healthcare. Preprint at https://arxiv.org/abs/1806.00388 (2018).
Waldmann, M. The Oxford Handbook of Causal Reasoning (Oxford University Press, 2017).
Shpitser, I. & Pearl, J. Effects of treatment on the treated: Identification and generalization. In Proc. Twenty-fifth Conference on Uncertainty in Artificial Intelligence (eds Bilmes, J. & Ng, A.Y.) 514–521 (Montreal, Quebec, Canada, AUAI Press, 2009).
Morgan, S. L. & Winship, C. Counterfactuals and Causal Inference (Cambridge University Press, 2015).
Pearl, J. et al. Causal inference in statistics: an overview. Stat. Surv. 3 , 96–146 (2009).
Peters, J., Janzing, D. & Schölkopf, B. Elements of Causal Inference-Foundations and Learning Algorithms (The MIT Press, 2017).
Pearl, J. Probabilities of causation: three counterfactual interpretations and their identification. Synthese 121 , 93–149 (1999).
Heckerman, E. & Nathwani, N. Toward normative expert systems: part ii probability-based representations for efficient knowledge acquisition and inference. Methods Inf. Med. 31 , 106–116 (1992).
Lee, C. M. & Spekkens, R. W. Causal inference via algebraic geometry: feasibility tests for functional causal structures with two binary observed variables, J. Causal Inference 5 (2015).
Lauritzen, S. L. Graphical Models , 17 (Clarendon Press, 1996).
Shpitser, I. & Pearl, J. What counterfactuals can be tested. Preprint at https://arxiv.org/abs/1206.5294 (2012).
Nikovski, D. Constructing bayesian networks for medical diagnosis from incomplete and partially correct statistics. IEEE Transactions Knowledge Data Eng. 12 , 509–516 (2000).
Rish, I., Brodie, M. & Ma, S. Accuracy vs. efficiency trade-offs in probabilistic diagnosis. AAAI/IAAI 560–566 (2002).
Heckerman, D. A tractable inference algorithm for diagnosing multiple diseases. Machine Intelligence Pattern Recognition 10 , 163–171 (1990).
Halpern, Y. & Sontag, D. Unsupervised learning of noisy-or bayesian networks. Preprint at https://arxiv.org/abs/1309.6834 (2013).
Arora, S., Ge, R., Ma, T. & Risteski, A. Provable learning of noisy-or networks. In Proc. 49th Annual ACM SIGACT Symposium on Theory of Computing (ed Hatami, H.) 1057–1066 (Montreal, Canada, ACM, 2017).
Oniśko, A., Druzdzel, M. J. & Wasyluk, H. Learning bayesian network parameters from small data sets: application of noisy-or gates. Int. J. Approx. Reasoning 27 , 165–182 (2001).
Balke, A. & Pearl, J. Counterfactual probabilities: Computational methods, bounds and applications. In Proc. Tenth International Conference on Uncertainty in Artificial Intelligence (eds Lopez de Mantaras, R. & Poole, D.) 46–54 (Seattle, Washington, Morgan Kaufmann Publishers Inc., 1994).
Perov, Y. et al. Multiverse: causal reasoning using importance sampling in probabilistic programming. Paper presented at Symposium on Advances in Approximate Bayesian Inference , Vancouver, (Canada, 2020).
Peabody, J. W. et al. Measuring the quality of physician practice by using clinical vignettes: a prospective validation study. Ann. Intern. Med. 141 , 771–780 (2004).
Veloski, J., Tai, S., Evans, A. S. & Nash, D. B. Clinical vignette-based surveys: a tool for assessing physician practice variation. Am. J. Med. Qual. 20 , 151–157 (2005).
Converse, L., Barrett, K., Rich, E. & Reschovsky, J. Methods of observing variations in physicians’ decisions: the opportunities of clinical vignettes. J. Gen. Intern. Med. 30 , 586–594 (2015).
Article PubMed Central Google Scholar
Dresselhaus, T. R., Peabody, J. W., Luck, J. & Bertenthal, D. An evaluation of vignettes for predicting variation in the quality of preventive care. J. Gen. Intern. Med. 19 , 1013–1018 (2004).
Semigran, H. L., Linder, J. A., Gidengil, C. & Mehrotra, A. Evaluation of symptom checkers for self diagnosis and triage: audit study. BM J 351 , h3480 (2015).
Middleton, K. et al. Sorting out symptoms: design and evaluation of the’babylon check’automated triage system. Preprint at https://arxiv.org/abs/1606.02041 (2016).
Higgs, J., Jones, M. A., Loftus, S. & Christensen, N. Clinical Reasoning in the Health Professions E-Book (Elsevier Health Sciences, 2008).
Liberman, A. L. & Newman-Toker, D. E. Symptom-disease pair analysis of diagnostic error (spade): a conceptual framework and methodological approach for unearthing misdiagnosis-related harms using big data. BMJ Qual. Saf. 27 , 557–566 (2018).
Romessis, C. & Mathioudakis, K. Bayesian network approach for gas path fault diagnosis. J. Eng. Gas. Turbines Power 128 , 64–72 (2006).
Badgeley, M. A. et al. Deep learning predicts hip fracture using confounding patient and healthcare variables. NPJ Digital Med. 2 , 1–10 (2019).
Janizek, J. D., Erion, G., DeGrave, A. J. & Lee, S.-I. An adversarial approach for the robust classification of pneumonia from chest radiographs. In Proceedings of the ACM Conference on Health, Inference, and Learning (ed Ghassemi, M.) (Toronto, ON, Canada, 2020).
Gowal, S. et al. Achieving robustness in the wild via adversarial mixing with disentangled representations. Preprint at https://arxiv.org/abs/1912.03192 (2019).
Besserve, M., Sun, R. & Schölkopf, B. Counterfactuals uncover the modular structure of deep generative models. Preprint at https://arxiv.org/abs/1812.03253 (2018).
Kocaoglu, M., Snyder, C., Dimakis, A. G. & Vishwanath, S. Causalgan: Learning causal implicit generative models with adversarial training. Preprint at https://arxiv.org/abs/1709.02023 (2017).
Richens, J. G., Lee, C. M. & Johri, S. Improving the accuracy of medical diagnosis with causal machine learning. Zenodo , https://doi.org/10.5281/zenodo.4575649 (2021).
Download references
Acknowledgements
The authors would like to thank Kostis Gourgoulias, Chris Lucas, Yura Perov, Adam Baker and Albert Buchard for discussions. The authors would like to thank Peter Spirtes for valuable suggestions for the manuscript.
Author information
Authors and affiliations.
Babylon Health, 60 Sloane Ave, Chelsea, London, SW3 3DD, UK
Jonathan G. Richens, Ciarán M. Lee & Saurabh Johri
University College London, Gower St, Bloomsbury, London, WC1E 6BT, UK
Ciarán M. Lee
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the original idea for the project. J.G.R. conceived the project and acted as project leader. J.G.R. and C.M.L. wrote the first draft of the paper and the revised versions with input from S.J. Proofs, experiments, code, tables, and figures contributed by J.G.R. All authors discussed the content and contributed to editing the manuscript.
Corresponding author
Correspondence to Jonathan G. Richens .
Ethics declarations
Competing interests.
All the authors in the article are employees of Babylon Health.
Additional information
Peer review information Nature Communications thanks Michael Hofler, Peter Spirtes and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, reporting summary, peer review file, source data, source data, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Richens, J.G., Lee, C.M. & Johri, S. Improving the accuracy of medical diagnosis with causal machine learning. Nat Commun 11 , 3923 (2020). https://doi.org/10.1038/s41467-020-17419-7
Download citation
Received : 13 March 2020
Accepted : 26 June 2020
Published : 11 August 2020
DOI : https://doi.org/10.1038/s41467-020-17419-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
The bio-exposome: intracellular processes, stress physiology and the environment.
- Helen Minnis
- Anne-Laura van Harmelen
- Paul G. Shiels
Nature Mental Health (2024)
Improving generalization of machine learning-identified biomarkers using causal modelling with examples from immune receptor diagnostics
- Milena Pavlović
- Ghadi S. Al Hajj
- Geir K. Sandve
Nature Machine Intelligence (2024)
Diagnostic capabilities of ChatGPT in ophthalmology
- Asaf Shemer
- Michal Cohen
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
Explainable Artificial Intelligence Multimodal of Autism Triage Levels Using Fuzzy Approach-Based Multi-criteria Decision-Making and LIME
- A. S. Albahri
- Shahad Sabbar Joudar
- Iman Mohamad Sharaf
International Journal of Fuzzy Systems (2024)
Machine learning model for the prediction of gram-positive and gram-negative bacterial bloodstream infection based on routine laboratory parameters
BMC Infectious Diseases (2023)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

How to Write Better Medical Papers
- © 2019
- Michael Hanna 0
Mercury Medical Research & Writing, New York, USA
You can also search for this author in PubMed Google Scholar
Assists clinicians and researchers in writing papers for publication in peer-reviewed scientific journals in medicine, health, and life sciences
A step-by-step guide from analyzing the data to writing each part of the manuscript to revising and publishing the paper
Includes careful referencing and an extensive annotated bibliography to guide readers to further resources in the vast literature on medical scientific writing
131k Accesses
6 Citations
9 Altmetric
This is a preview of subscription content, log in via an institution to check access.
Access this book
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Other ways to access
Licence this eBook for your library
Institutional subscriptions
Table of contents (60 chapters)
Front matter, introduction.
Michael Hanna
The Ethical Foundations of Medical Scientific Writing
Ethics of conducting research, searching the literature, the elevator speech, the outline, envision your readers, ethics of data analysis, data preparation, statistics: general principles, statistics: common mistakes, presentation: figures versus tables versus text, figures: general guidance.
- medical writing
- scientific writing
- medical research
- statistical analysis
- research ethics
About this book
This book guides medical researchers through all stages of transforming their scientific data and ideas into a published paper. Many researchers in medicine, including the life sciences and health sciences, struggle to get their research written and published. Manuscripts are typically rejected and/or sent back for revisions several times before ever being published. One reason for this is that researchers have not received much instruction in the specific subjects and skills needed to write and publish scientific medical papers: research methodology, ethics, statistics, data visualization, writing, revising, and the practicalities of publishing.
Authors and Affiliations
Mercury medical research & writing, new york, usa, about the author.
Michael Hanna, PhD, is an independent Medical Writer and Research Consultant from New York City. He has over a decade of experience consulting on study design, conducting literature reviews, performing statistical analysis, and writing and editing scientific papers across the spectrum of medical specialties. He has lectured widely in Europe and North America on medical writing and has mentored many researchers and medical residents on scientific writing.
Michael Hanna earned a doctoral degree in Clinical Psychology from the University of Cologne, Germany, and completed a post-doctoral fellowship at Cornell University’s medical school in New York City. Previously, he earned a Master’s degree in Psychology from the University of Paris VIII and a Bachelor’s degree in Neuroscience and in French Studies from Wesleyan University in Middletown, CT, USA.
Prior to becoming a professional Medical Writer and Research Consultant, Michael Hanna taught at the University Hospital of Aachen, Germany. He also acquired clinical and scientific experience at the University of Cologne, Germany; the Raymond Poincaré Hospital in Paris, France; and other specialized clinics in America and Europe. He is fluent in German, French, and Spanish.
Bibliographic Information
Book Title : How to Write Better Medical Papers
Authors : Michael Hanna
DOI : https://doi.org/10.1007/978-3-030-02955-5
Publisher : Springer Cham
eBook Packages : Medicine , Medicine (R0)
Copyright Information : Springer Nature Switzerland AG 2019
Softcover ISBN : 978-3-030-02954-8 Published: 29 March 2019
eBook ISBN : 978-3-030-02955-5 Published: 20 March 2019
Edition Number : 1
Number of Pages : XI, 335
Number of Illustrations : 8 illustrations in colour
Topics : Internal Medicine , Primary Care Medicine
- Publish with us
Policies and ethics
- Find a journal
- Track your research
AMBOSS Blog
- Student Life
How to Write and Publish Clinical Research in Medical School
From working hard on the USMLE® exams to holding leadership positions in a specialty’s academic society, there are many ways medical students can work towards matching into the residency of their choice. One such activity that looks great on residency applications is finding clinical research opportunities in medical school to write and publish papers. No one knows this better than Dr. Eve Bowers.
An Otolaryngology resident at the University of Miami/Jackson Memorial Hospital, Eve became an expert in writing, submitting, and publishing manuscripts during her final years in medical school. Check out Eve’s blog post below to get valuable insights on how to get published in medical school.
As medical students, we’re told that research is important and that publications are “good”, and even “necessary to match ” into residency, but we often aren’t given the tools we need to turn ideas into manuscripts. This is especially true given our rigorous schedules.
When I looked through my CV, I saw I had a few abstracts and presentations, but no manuscripts. I wanted to write, but publishing seemed like just checking another resume box. On top of that, I didn’t know where to begin.
My writing journey started with a case report I nervously picked up during my surgery clerkship . Then, over ten months of typing, editing, and sending unanswered emails, I went from writing 0 to ten manuscripts. The process was sometimes painful but mostly gratifying (yes, research can be gratifying), and you can do it, too.
To make finding, starting, and publishing high-quality research articles a little bit easier and a lot more enjoyable, check out my five tips for publishing clinical research in medical school.
1. Build your network to find publication opportunities in medical school
When looking for projects, finding great mentors is often more useful than finding the perfect project. This is especially true when starting out. Use your time on clerkships to identify attending and resident mentors who you trust to support your budding author ambitions.
At this stage, residents especially are your friends . When you demonstrate follow-through and receptiveness to feedback, you will be given more research opportunities. Don’t be shy about asking mentors for tasks if you can juggle multiple projects, but don’t bite off more than you can chew. It’s important to communicate honestly and be transparent about the amount of time you have.
2. Kickstarting your research during medical school: start small
If you have no research experience, start with a case report. Volunteer to write an article about an interesting case you saw in the operating room or clinic. It’s much easier and more rewarding to write about patients you have experience with, and case reports are a great way to demonstrate your writing ability to more senior authors.
Pro tip : Try to figure out as much as you can independently by using published reports as blueprints before asking for help. Nevertheless, don’t be afraid to seek guidance when you need it! If you approach a mentor with a problem, come prepared with 2-3 realistic solutions or examples of how you tried to figure it out on your own.
3. Know the criteria for writing a clinical research paper
Before you begin, ask your mentor where they would like to submit the completed work. Each journal has specific standards, styles, and submission criteria. For guidance, look to papers previously published in that journal.
As far as annotations and citations are concerned, download and learn how to use Endnote or Zotero right now! You’ll save days of work formatting your references.
Additionally, consider creating folders and spreadsheets to keep track of projects. Set goals and timelines for yourself from the beginning, and block off dedicated time to conduct a literature review, analyze data, and write.
Pro tip : If you are the first author and overseeing a large team, improve communication and efficiency by making everyone’s roles and expectations very clear to the group via email.
4. Follow up with your mentor
Sometimes you’ll send your mentor a draft, but she won’t get back to you with edits and feedback in a reasonable timeframe. Surprisingly, many projects do not get past this point because of insufficient persistence. Here’s what to do if this happens:
- Politely nudge your mentor with follow-up emails and schedule a meeting to discuss in person or via Zoom.
- Set deadlines and give specific reasons why the paper needs to be submitted. Some reasons could include, “I need this submission for my residency application ” or “this is a requirement for my school.”
- Ask your co-author resident and/or fellow to advocate for edits and submission.
Whatever happens, don’t give up at this point. You’ve put in the work, and persistence makes or breaks a successful student-author.
5. Write about the medical topics that you love
Writing is fun when you focus on subjects you’re really passionate about. You also don’t have to stay within your institution: feel free to branch out if you come across an interesting research opportunity at a different program. A little cold email can go a long way!
If your goal is quantity, you can increase output by asking around about “productive” research mentors and sticking to topics related to clinical practice or medical education. However, my advice is to never let relatively quick publication opportunities compromise the quality of your work. Remember — every paper you write gets easier and more enjoyable, and your work will be truly important to advancing the field you care about. Good luck!

About the Author : Eve is an Otolaryngology Resident at the University of Miami/Jackson Memorial Hospital. She attended medical school at the University of Pittsburgh School of Medicine and undergrad at the University of Pennsylvania. She is passionate about medical education, mentorship, and increasing minority and female leadership in surgical fields. For more tips and tricks, follow her on Twitter and Instagram !
For more information on residency applications, check out the AMBOSS Residency Applications Clerkship Survival Guide.

Related posts you might like
Amboss apps: for medical students during clinical rotations.
No matter the specialty, the clinical clerkship period is full of challenging moments critical to ...
On the Wards: The Unwritten Rules of Clerkship Etiquette
You’re kicking off your clerkships this year, and there’s plenty to sink your teeth into as you ...
5 Tips To Survive And Thrive During Clinical Rotations
Last updated: August 10, 2021. Clinical rotations are an exciting time. Finally, after countless ...
Join Our Mailing List
And get updates on new posts and news about AMBOSS sent directly to your inbox.
All-in-one resource for residents and medical students.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- How to get involved in...
How to get involved in research as a medical student
- Related content
- Peer review
- Anna Kathryn Taylor , final year medical student 1 ,
- Sarah Purdy , professor of primary care and associate dean 1
- 1 Faculty of Health Sciences, University of Bristol, UK
Participating in research gives students great skills and opportunities. Anna Taylor and Sarah Purdy explain how to get started
This article contains:
-How to get involved with research projects
-Questions to ask yourself before starting research
-What can you get published? Research output
-Advice for contacting researchers
-Different types of research explained
-Stages of research projects
Students often go into medicine because of a desire to help others and improve patients’ physical and mental wellbeing. In the early years of medical school, however, it can seem as if you are not making much difference to patient care. Involvement in research can provide exciting opportunities to work as part of a team, improve career prospects, and most importantly add to the evidence base, leading to better outcomes for patients.
Research is usually multidisciplinary, including clinical academics (medical doctors who spend part of their working life doing research), nurses, patients, scientists, and researchers without a medical background. Involvement in such a team can improve your communication skills and expand your understanding of how a multidisciplinary team works.
Participating in research can also help you to develop skills in writing and critical appraisal through the process of publishing your work. You may be able to present your work at conferences—either as a poster or an oral presentation—and this can provide valuable points for job applications at both foundation programme and core training level. This is particularly important if you are considering a career in academia. You will also develop skills in time management, problem solving, and record keeping. You might discover an area of medicine in which you are keen to carry out further work. For some people, getting involved in research as a medical student can be the first step in an academic career.
Kyla Thomas, National Institute for Health Research clinical lecturer in public health at the University of Bristol, says, “my first baby steps into a clinical academic career started with a research project I completed as a medical student. That early involvement in research opened my eyes to a whole new world of opportunities that I never would have considered.
“Importantly, participating in undergraduate research sets students apart from their colleagues. Applying for foundation posts is a competitive process and it is a definite advantage if you have managed to obtain a peer reviewed publication.”
Getting involved with research projects
Although it is possible to do research at medical school, it is important to be realistic about how much free time you have. It might be possible to set up your own research project, but this will require substantial planning in terms of writing research protocols, gaining ethical approval, and learning about new research methodologies. Other opportunities for research that make less demands on your time include:
Intercalated degrees—these often have time set aside for research in a specific area, so it is important to choose your degree according to what you might like to do for your dissertation (for example, laboratory-based work in biochemistry, or qualitative research in global health. Some subjects may have options in both qualitative and quantitative research).
Student selected components or modules can provide a good opportunity to be involved in an ongoing study or research project. If you have a long project period, you might be able to develop your own small project.
Electives and summer holidays can also provide dedicated time for research, either within the United Kingdom or in another country. They can allow you to become established in a research group if you’re there for a few weeks, and can lead to a longstanding relationship with the research group if you continue to work with them over your medical school career.
If you don’t know what to do, contacting the Student Audit and Research in Surgery (STARSurg), 1 the National Student Association of Medical Research (NSAMR), 2 or your medical school’s research society may be a good place to start.
The INSPIRE initative, 3 coordinated by the Academy of Medical Sciences, gives support and grants to help students take part in research. Some UK medical schools have small grants for elective and summer projects, and organise taster days for students to get an idea of different research areas.
You may also be able to access other grants or awards to support your research. Some of the royal colleges, such as the Royal College of General Practitioners and the Royal College of Psychiatrists, offer bursaries to students doing research in their holidays or presenting at conferences. Other national organisations, such as the Medical Women’s Federation, offer bursaries for elective projects.
Box 1: Questions to ask yourself before starting research
What are you interested in? There is no point getting involved in a project area that you find boring.
How much time do you have available? It is crucial to think about this before committing to a project, so that your supervisor can give you an appropriate role.
What do you want to get out of your research experience? Do you want a brief insight into research? Or are you hoping for a publication or presentation?
Do you know any peers or senior medical students who are involved in research? Ask them about their experiences and whether they know of anyone who might be willing to include you in a project.
Box 2: Research output
Publication —This is the “gold standard” of output and usually consists of an article published in a PubMed ID journal. This can lead to your work being cited by another researcher for their paper, and you can get up to two extra points on foundation programme applications if you have published papers with a PubMed ID.
Not all research will get published, but there are other ways to show your work, such as presenting at conferences:
Oral presentation —This involves giving a short talk about your research, describing the background, methods, and results, then talking about the implications of your findings.
Poster presentation —This involves creating a poster, usually A1 or A2 in size, summarising the background, methods, and results of your research. At a conference, presenters stand by their poster and answer questions from other delegates.
Contacting researchers
Most universities have information about their research groups on their websites, so spend some time exploring what studies are being carried out and whether you are interested in one of the research topics.
When contacting a member of the research group, ask if they or someone else within their team would be willing to offer you some research experience. Be honest if you don’t have any prior experience and about the level of involvement you are looking for, but emphasise what it is about their research that interests you and why you want to work with them. It’s important to have a flexible approach to what they offer you—it may not initially sound very exciting, but it will be a necessary part of the research process, and may lead to more interesting research activity later.
Another way to make contact with researchers is at university talks or lectures. It might be intimidating to approach senior academics, but if you talk to them about your interest they will be more likely to remember you if you contact them later on.
Box 3: What can students offer research teams?—Views from researchers
“Medical students come to research with a ‘fresh eyes’ perspective and a questioning mindset regarding the realities of clinical practice which, as a non-medic myself, serves to remind me of the contextual challenges of implementing recommendations from our work.”
Alison Gregory, senior research associate, Centre for Academic Primary Care, University of Bristol, UK.
“Enthusiasm, intelligence, and a willingness to learn new skills to solve challenges—bring those attributes and you’ll be valuable to most research teams.”
Tony Pickering, consultant anaesthetist and Wellcome Trust senior research fellow, University of Bristol, UK.
Box 4: Different types of research
Research aims to achieve new insights into disease, investigations, and treatment, using methodologies such as the ones listed below:
Qualitative research —This can be used to develop a theory and to explain how and why people behave as they do. 4 It usually involves exploring the experience of illness, therapeutic interventions, or relationships, and can be compiled using focus groups, structured interviews, consultation analysis, 5 or ethnography. 6
Quantitative research —This aims to quantify a problem by generating numerical data, and may test a hypothesis. 7 Research projects can use chemicals, drugs, biological matter, or even computer generated models. Quantitative research might also involve using statistics to evaluate or compare interventions, such as in a randomised controlled trial.
Epidemiological research —This is the study of the occurrence and distribution of disease, the determinants influencing health and disease states, and the opportunities for prevention. It often involves the analysis of large datasets. 4
Mixed methods research —This form of research incorporates both quantitative and qualitative methodologies.
Systematic reviews —These provide a summary of the known evidence base around a particular research question. They often create new data by combining other quantitative (meta-analysis) or qualitative (meta-ethnography) studies. They are often used to inform clinical guidelines.
Box 5: Stages of research projects
Project conception—Come up with a hypothesis or an objective for the project and form the main research team.
Write the research protocol—Produce a detailed description of the methodology and gain ethical approval, if needed.
Carry out the methodology by collecting the data.
Analyse the data.
Decide on the best way to disseminate your findings—for example, a conference presentation or a publication—and where you will do this.
Write up your work, including an abstract, in the format required by your chosen journal or conference.
Submit . For conference abstracts, you may hear back swiftly whether you have been offered the chance to present. Publication submissions, however, must be peer reviewed before being accepted and it can take over a year for a paper to appear in print.
Originally published as: Student BMJ 2017;25:i6593
Competing interests: AKT received grant money from INSPIRE in 2013.
Provenance and peer review: Not commissioned; externally peer reviewed.
- ↵ STARSurg. Student Audit and Research in Surgery. 2016. www.starsurg.org .
- ↵ NSAMR. National Student Association of Medical Research. 2016. www.nsamr.org .
- ↵ The Academy of Medical Sciences. About the INSPIRE initiative. 2016. www.acmedsci.ac.uk/careers/mentoring-and-careers/INSPIRE/about-INSPIRE/ .
- ↵ Ben-Shlomo Y, Brookes ST, Hickman M. Lecture Notes: Epidemiology, Evidence-based Medicine and Public Health. 6th ed . Wiley-Blackwell, 2013 .
- ↵ gp-training.net. Consultation Theory. 2016. www.gp-training.net/training/communication_skills/consultation/consultation_theory.htm .
- ↵ Reeves S, Kuper A, Hodges BD. Qualitative research methodologies: ethnography. BMJ 2008 ; 337 : a1020 . doi:10.1136/bmj.a1020 pmid:18687725 . OpenUrl FREE Full Text
- ↵ Porta M. A Dictionary of Epidemiology. 5th ed . Oxford University Press, 2008 .
- Open access
- Published: 09 April 2024
Preparing medical students for their educational task as physicians: important, desirable and unexplored territory
- Bas PH ter Brugge 1 ,
- Lena Sophia Fegg 2 &
- Marjo Wijnen-Meijer 2 , 3
BMC Medical Education volume 24 , Article number: 391 ( 2024 ) Cite this article
138 Accesses
Metrics details
Physicians engage in educational activities in daily practice and take over an important role in providing information and transferring knowledge to patients and medical students. Therefore, it is important to focus on methods to develop teaching skills during medical school. Peer-teaching is a teaching method that is connected to different positive learning outcomes. This study aims to investigate the perspective of medical students regarding teaching as a core competency of physicians and peer-teaching as an opportunity to acquire educational skills. The study also aims to examine to what extent medical students are prepared for their teaching role at medical schools.
This cross-sectional study was performed by an online survey amongst Dutch medical students from all medical schools across all years of study. In total, 2666 medical students filled out the survey. The survey was part of the annual online survey of the Dutch medical advocacy group (DeGeneeskundestudent) amongst all medical students in the fall of 2017. The data were analysed with descriptive statistics and statistical tests (chi-squared-test and binomial test).
The results show that 49% of medical students see teaching as one of the core tasks of a physician. However, only 25% feel well prepared by their medical school for this teaching role. Instead, there are many students who gain experiences and teaching skills on their own outside medical schools. 64% of the respondents agrees that senior medical students can educate junior medical students well.

Conclusions
Implementing peer-teaching in the curricular of medical schools could be an effective teaching method to prepare medical students for their future teaching role. It is important that medical schools focus on enhancing educational quality and designing learning environments for best learning outcomes to better prepare medical students for professional life.
Peer Review reports
The teaching role of physicians is a core competency in the new Dutch Medical Training Framework: “Physicians contribute as academics to the application, spread, translation and proliferation of knowledge in practice through lifelong learning, training others, evaluating evidence and contributing to scientific research” [ 1 ]. Every physician must be able to “create a safe learning environment”, “provide a teaching activity” and “constructively evaluate teaching activities to improve education” [ 1 ]. After all, every physician engages in educational activities in one way or another. It has been shown that a general practitioner spends up to 20% of his consultation time on patient education and a medical specialist up to 10% of his time on supervising residents or medical students [ 2 , 3 ]. Physicians play an important role in providing information and transferring knowledge to patients and medical students. Therefore, parallel to clinical skills the acquisition of educational skills should begin in medical school and continue throughout postgraduate training [ 4 ].
Educational skills are best developed by doing it yourself [ 5 , 6 ]. Peer-teaching, i.e. students teaching other students, is a method for medical students to practice teaching in a controlled environment [ 6 ]. In some medical faculties, both in the Netherlands and other countries, peer-teaching is a regular part of medical school [ 7 , 8 ]. To develop medical students’ teaching skills, peer-teaching programmes, teaching workshops, and community outreach programmes are used [ 9 ]. Many medical schools in the United States offer formal students-as-teachers (SAT) programmes, where students are assigned educational roles such as peer mentors, teaching assistants or contributing to the development of a curriculum design. These programmes benefit the students’ teaching skills, improve their clinical knowledge and communication- and professional skills. Peer-teachers can benefit from peer-teaching experiences in many ways. Teaching offers a chance to identify personal strengths and weaknesses by preparing complex medical knowledge, organizing classes, enhancing public speaking skills, giving- and receiving feedback, working in a team and leading near-peer students [ 6 , 7 , 8 , 10 , 11 ]. By actively participating in their training the medical students’ intrinsic motivation is improved [ 12 , 13 ].
In a recent non-randomized controlled trial by Veloso et al. (2019), it was shown that medical students who taught Basic Life Support skills to community health professionals had a better theoretical and practical performance in Basic Life Support, than medical students who didn’t teach these skills [ 14 ]. Peer-teaching is further supported by studies that have found no difference in medical students’ academic achievements when taught by peer-teachers or faculty staff. While peer-teachers are considered less knowledgeable than faculty staff, students actually feel more at ease asking questions and, due to peer-teachers being regarded as more approachable, they are better understood and guided in comprehending difficult topics [ 11 , 14 , 15 , 16 ]. A final reason for implementation of peer -teaching programmes is the rise in student numbers. Peer-teachers offer a solution to overcome the strained teaching capacity of faculty staff [ 11 , 17 ].
There is evidence that former peer-teaching physicians become more engaged in educational activities. A study by Kloek et al. (2016) indicated that these physicians themselves highly appreciated the teaching internship and are likely committed to building an educational career in their future professional life [ 18 ].
Unfortunately, little is known about the perspective of medical students regarding teaching as a physician and peer-teaching. This perspective is relevant to facilitate the introduction of peer-teaching by medical schools and better prepare medical students for their future teaching role as a physician. It is relevant to assess medical students’ perspective on the teaching role of physicians and their educational activities during medical school. Therefore, this study aims to gain insight into medical students´ opinion on teaching as a physician and peer teaching by answering the following research questions:
To what extent do medical students consider teaching a core competency of a physician?
How and to what extent are medical students prepared for teaching as a physician during medical school?
Study design and participants
This study has a cross-sectional design and is performed by an online survey amongst medical students.
The research population comprised of Dutch medical students from all medical schools across all years of study. In the Netherlands, there are eight medical schools that offer a six-year undergraduate medical training. The undergraduate program is divided in a three year Bachelor, with mostly theoretical education, and a three year Master, with both theoretical educations and clerkships.
The survey started with a general section on gender, university and study-phase. Next, five questions asked for the participants view regarding (the preparation for) teaching as a physician and peer-teaching (see Tables 1 and 2 ). The questions were grounded in literature [ 17 ]. Four questions were answered on a five-point Likert scale (strongly agree- strongly disagree), in which answer option 3 means “neutral” and for the question “older students can teach younger year medical students well” also “no experience”. The final question was a binary question (yes/no).
The survey was part of the annual online survey of the Dutch medical advocacy group (DeGeneeskundestudent) amongst all medical students in the fall of 2017. Participants voluntarily filled out the questionnaire and informed consent was given for anonymous use of the data.
Data analysis
Before data-analysis we excluded the following participants. Participants with an abbreviated medical study were excluded because they had already finished a wide range of different previous bachelor-studies. Participants who had not filled out the general section were excluded as well. The results were analysed with SPSS version 25. The general section was analysed with descriptive statistics. The study population was compared with available national data on medical students regarding gender, study-phase and university [ 19 , 20 ]. The questions on the participants view answered on a Likert scale were dichotomised to agree (strongly agree-agree) and disagree (strongly disagree-disagree). In the analysis, we left out the responses to category 3 to get an impression of students’ positive or negative attitude towards peer-teaching and, regarding question 2, to avoid bias from people who have no experience with it giving an opinion. The results were analysed with descriptive statistics. The participants view according to different gender, study-phase or university was analysed with a chi-squared-test or binomial test. The binary question on the participants view was analysed with descriptive statistics. The participants view according to different gender, study-phase or university was analysed with a chi-squared-test. The outcome of all tests was significant if p < 0.05.
Respondents´ characteristics
The respondents´ characteristics are shown in Table 3 . A total of 2666 medical students filled out the survey. The percentage of male respondents was lower than the national average, 23% versus 34%, as well as the percentage of master students, 47% versus 53%. The percentage of respondents from the University of Amsterdam (UvA), Vrije Universiteit (VU) and Rotterdam was slightly lower than the national average, while the percentage of respondents from Groningen, Leiden and Nijmegen was higher than the national average. The distribution of respondents across years of study is similar to the distribution in the overall population.
View on teaching as a physician and peer-teaching
The results on teaching as a physician and peer-teaching are shown in Tables 1 and 2 . Significant results are highlighted in the paragraph below.
Teaching as a physician
49% of the respondents agrees that teaching is a core responsibility of a physician, while 22% of the respondents disagrees. Male respondents agree more often than female respondents, 58% versus 47%, as well as respondents in the master phase than respondents in the bachelor phase, 64% versus 35%. Agreement of respondents from different universities was between 43% and 56%.
- Peer-teaching
64% of the respondents agrees that senior medical students can educate junior medical students well, while 13% of the respondents disagrees. Respondents in the master phase disagree more often than respondents in the bachelor phase, 13% versus 11%. Agreement of respondents from different universities was between 53% and 75%.
View on preparation for teaching as a physician
The results on preparation for teaching as a physician by the formal education and respondents’ own experience are shown in Tables 1 and 2 . Table 4 shows the respondents own experience with teaching. Significant results are highlighted in the paragraph below.
Formal education
27% of the respondents agrees that the medical education prepares them well for teaching as a physician, while 39% disagrees. Male respondents agree more often than female respondents, 36% versus 24%. Respondents in the master phase disagree more often than respondents in the bachelor phase, 46% versus 33%. Agreement of respondents from different universities was between 19% and 33%.
Own experience
48% of the respondents agrees that their own experience with teaching prepares them well for teaching as a physician, while 22% disagrees. Male respondents agree more often than female respondents, 62% versus 44%. Respondents in the master phase agree more often than respondents in the bachelor phase, 56% versus 40%. Agreement of respondents from different universities was between 39% and 56%.
52% of the respondents have teaching experience. Male respondents more often have experience than female respondents, 59% versus 51%, as well as respondents in the master phase than the bachelor phase, 63% versus 42%. The percentage of respondents from different universities with teaching experience varies between 44% and 60%.
Of the respondents with teaching experience, 13% have experience as peer-teacher, 11% as part of the formal education and 37% outside the formal education. Male respondents have more experience than female respondents with teaching outside the formal education, 42% versus 36%, and as peer-teacher, 16% versus 12%. Respondents in the master phase have more experience in all manners of teaching than respondents in the bachelor phase. The percentage of respondents from different universities with teaching experience varies, as peer-teacher (4 − 17%), as part of the curriculum (6 − 21%) and outside the formal education (33-45%).
Half of medical students feel that teaching is one of the core tasks of a physician. Unfortunately, only 25% feel well prepared by their medical school for this teaching role. This is in line with the literature that students would benefit from more preparation in this area [ 21 , 22 ]. It is striking that students who are more advanced in their studies feel less prepared than students who are at the beginning of medical school. The explanation for this may be that older students have more insight into the complexity of the teaching task because they have more experience with the physicians who teach or have had some experience of this themselves. It is contradictory that on the one hand students are aware of their later teaching role and responsibility but on the other hand do not feel adequately prepared for this role. A core task of physicians is to provide knowledge, experiences and skills to different learning groups, e.g. to medical students, patients and other professionals and should therefore be a relevant part of medical education programs.
Almost half of the students feel well prepared for their later teaching role from their own experience. They look for teaching opportunities themselves in anatomy or skills courses or as a secondary job [ 23 ]. They agree that their own experience with teaching prepares them well for teaching as a physician. This finding highlights the importance of providing appropriate learning opportunities during medical education. Students engaging as peer-teachers have the chance to gain extracurricular experiences that are relevant not only for professional practice but also to strengthen soft skills and interdisciplinary competencies. Teaching experiences are beneficial in many ways, increase teaching skills, intensify knowledge, increase organizational and communication skills and enhance leading and speaking skills that are relevant for daily practice [ 6 , 7 , 8 , 10 , 11 , 24 ].
A large majority of medical students think that older students are good at teaching younger ones. At some universities, students have a more positive image of peer-teaching than at others. It is useful to find out whether these faculties use peer-teaching more as a teaching method.
Thus, medical students’ own views on peer-teaching do not seem to be an impediment to using peer-teaching to learn the role of a teacher. This is also in line with the literature on peer-teaching showing different advantages of learning from other students [ 11 , 25 ]. First, peer-teachers are closer to the student in experience. Therefore, they can better understand what the students find difficult and they also understand the knowledge level of the students better, compared to, for example, medical specialists [ 15 ]. In addition, peer-teachers can create a safe educational climate in which mistakes are allowed and questions can be asked, because peer-teacher are perceived as less threatening [ 15 ]. Peer-teachers and students both can profit from peer-teaching settings.
The use of students as teachers can improve teaching capacities and is also connected to economic aspects. To secure high standards in the quality of education in medical schools, peer-teaching programs should be accompanied by training and supervision [ 11 , 17 ].
A strength of this research project is that it is a cross-section of all Dutch universities and all study years. Therefore, the results give a good picture of the opinion of Dutch medical students. Furthermore, the study focuses on the perspective of medical students. This perspective can be beneficial for gaining insights into medical students’ opinions and for designing adequate learning environments in medical schools. A limitation is that due to the nature of the survey, questionnaires with multiple choice questions, it only provides a global picture. Furthermore, male and bachelor students participated significantly less, which may distort the results. Future research can focus on a comparison between universities with and without formal education in the study program in the area of teaching skills. Furthermore, follow-up research should focus on assessing gender differences. Interviews or focus groups can also provide insight into the motivation and argumentation of the students to gain deeper insights into students’ perceptions. Additionally, further research should also include medical teachers, professionals at medical schools, experts and physicians to gain multiple perspectives. It is also important to focus on the effectiveness of peer-teaching programs in comparison to other learning methods, particularly from a long-term perspective. As teaching skills are a core competence of physicians for daily practice, assessing learning opportunities and methods for physicians in the context of continuing education should also be taken into account.
Many medical students see teaching as a core task of physicians and are aware of their later teaching role. However, a large proportion of them, especially the students in the last phase of their studies, feel that their medical school program has not adequately prepared them for this role. Instead, there are many students who gain experiences and teaching skills on their own initiative outside medical schools. Preparing medical students for their educational tasks and supporting them in the acquisition of teaching skills should be an essential part of their education. The majority of medical students think that senior students can educate junior medical students well. Therefore, implementing peer-teaching in the curricular of medical schools could be an effective teaching method for learning success. In a broader context, preparing medical students for their teaching role can be beneficial for the patient-medicine relationship and the provision of knowledge and health competency for patients. This study and the literature show that peer teaching, combined with good supervision and feedback, is a good way to prepare medical students for the future teaching role. It is important that medical schools focus on enhancing educational quality and designing beneficial and positive learning environments for best learning outcomes to better prepare medical students for professional life.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to data protection guidelines of the institution but are available from the corresponding author on reasonable request.
Abbreviations
students-as-teachers
Universiteit van Amsterdam
Vrije Universiteit
Nederlandse Federatie van Universitair Medische Centra (NFU). Dutch Medical Training Framework 2020. Utrecht. 2020;1–82.
Yawn B, Goodwin MA, Zyzanski SJ, Stange KC. Time use during acute and chronic illness visits to a family physician. Fam Pract. 2003;20:474–7. https://doi.org/10.1093/fampra/cmg425 .
Article Google Scholar
Westbrook J, Ampt A, Kearny L, Rob M. All in a day’s work: an observational study to quantify how and with whom doctors on hospital wards spend their time. Med J Australia. 2008;188:506–9. https://doi.org/10.5694/j.1326-5377.2008.tb01762.x .
Haber R, Bardach N, Vedanthan R, Gillum L, Haber L, Dhaliwal G. Preparing fourth-year medical students to teach during internship. J Gen Intern Med. 2006;21(5):518–20. https://doi.org/10.1111/j.1525-1497.2006.00441.x .
Ericsson KA, Krampe RTh, Tesch-Römer C. The role of deliberate practice in the acquisition of expert performance. Psychol Rev. 1993;3:363–406. https://doi.org/10.1037/0033-295X.100.3.363 .
Ralhan S, Bhogal P, Bhatnagar G, Young J, Green M. Effective teaching skills– how to become a better medical educator. BMJ. 2012;344:e765. https://doi.org/10.1136/bmj.e765 .
Dandavino M, Snell L, Wiseman J. Why medical students should learn how to teach. Med Teach. 2007;29(6):558–65. https://doi.org/10.1080/01421590701477449 .
Habboush Y, Stoner A, Torres C, Beidas S. Implementing a clinical-educator curriculum to enrich internal medicine residents ´teaching capacity. BMC Med Educ. 2019;19(1):459. https://doi.org/10.1186/s12909-019-1888-0 .
Marton G, McCullough B, Ramnanan C. A review of teaching skills development programmes for medical students. Med Educ. 2015;49(2):149–60. https://doi.org/10.1111/medu.12571 .
Soriano R, Blatt B, Coplit L, CichoskiKelly E, Kosowicz L, Newman L, et al. Teaching Medical Students how to teach: a National Survey of Students-as-teachers Programs in U.S. Medical Schools. Acad Med. 2010;85(11):1725–31. https://doi.org/10.1097/ACM.0b013e3181f53273 .
Bene KL, Bergus G. When learners become teachers: a review of peer teaching in medical student education. Fam Med. 2014;46(10):783–7.
Google Scholar
Nshimiyimana A, Cartledge P. Peer-teaching at the University of Rwanda - a qualitative study based on self-determination theory. BMC Med Educ. 2020;20(1):230. https://doi.org/10.1186/s12909-020-02142-0 .
Blanco M, Maderer A, Oriel A, Epstein S. How we launched a developmental student-as-teacher (SAT) program for all medical students. Med Teach. 2014;36(5):385–89. https://doi.org/10.3109/0142159X.2014.886770 .
Veloso S, Pereira G, Vasconcelos N, Senger M, de Faria R. Learning by teaching basic life support: a non-randomized controlled trial with medical students. BMC Med Educ. 2019;19(1):67. https://doi.org/10.1186/s12909-019-1500-7 .
Ten Cate O. A teaching rotation and a student teaching qualification for senior medical students. Med Teach. 2007;29(6):566–71. https://doi.org/10.1080/01421590701468729 .
Ten Cate O, Durning S. Dimensions and psychology of peer-teaching in medical education. Med Teach. 2007. https://doi.org/10.1080/01421590701583816 . 546– 52.
Burgess A, McGregor D. Peer teaching training for health professional students: a systematic review of formal programs. BMC Med Educ. 2018;18(1):263. https://doi.org/10.1186/s12909-018-1356-2 .
Kloek AT, Van Zijl ACM, Ten Cate OTJ. How a teaching rotation in medical school affects graduates´ subsequent careers. Perspective Med Educ. 2016;5:325–31. https://doi.org/10.1007/s40037-016-0302-4 .
Nationaal overzicht master studies. www.universitairemasters.nl/aantal-studenten/gezondheidszorg/ . Accessed 14 Aug 2018 [in Dutch].
Nationaal overzicht bachelor studies. www.universitaire.bachelors.nl/aantal-studenten/gezondheidszorg/ . Accessed 14 Aug 2018 [in Dutch].
Wenlock RD, Bath MF, Bashford T, Kohler K, Hutchinson PJ. The global variation of medical student engagement in teaching: implications for medical electives. PLoS ONE. 2020;15(2):e0229338. https://doi.org/10.1371/journal.pone.0229338 .
Nagji A, Leslie K, Wong E, Myhe D, Young M, Chan M. Something’s missing from my education: using a cross sectional survey to examine the needs and interest of Canadian medical students relating to their roles as teachers and educators. Can Med Educ J. 2017;8(3):e21–9.
Ocel JJ, Palmer BA, Wittich CM, Carmichael SW, Pawlina W. Outcomes of the gross and developmental anatomy teaching assistant experience. Clin Anat. 2003;16(6):526–30. https://doi.org/10.1002/ca.10193 .
Nelson AJ, Nelson SV, Linn AM, Raw LE, Kildea HB, Tonkin AL. Tomorrow’s educators… today? Implementing near-peer teaching for medical students. Med Teach. 2013;35(2):156–9. https://doi.org/10.3109/0142159X.2012.737961 .
Bulte C, Betts A, Garner K, Durning S. Student teaching: views of student near-peer teachers and learners. Med Teach. 2007;29(6):583–90. https://doi.org/10.1080/01421590701583824 .
Download references
Acknowledgements
The authors would like to thank all the students who participated in the survey.
Author information
Authors and affiliations.
Vilente, Doorwerth, Netherlands
Bas PH ter Brugge
School of Medicine and Health, Technical University of Munich, TUM Medical Education Center, Munich, Germany
Lena Sophia Fegg & Marjo Wijnen-Meijer
Institute of Medical Education, Medical Faculty and University Hospital Carl Gustav Carus, TUD Dresden University of Technology, Fetscherstraße 74, 01307, Dresden, Germany
Marjo Wijnen-Meijer
You can also search for this author in PubMed Google Scholar
Contributions
BtB, LSF and MWM designed and run the study and collected the data. BtB and MWM analysed the data and drafted the manuscript. All authors contributed to the critical revision of the manuscript and read and approved the submitted version.
Corresponding author
Correspondence to Marjo Wijnen-Meijer .
Ethics declarations
Ethics approval and consent to participate.
The survey was anonymous and voluntary. All students received information on the nature, purpose and procedure of the survey and their right to withhold or revoke their consent at any time. Participants voluntarily filled out the questionnaire and informed consent was given for anonymous use of the data. Ethical approval was obtained in 2017 from the Ethical Review Board of the Dutch Association for Medical Education.
All methods were carried out in accordance with Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
ter Brugge, B.P., Fegg, L.S. & Wijnen-Meijer, M. Preparing medical students for their educational task as physicians: important, desirable and unexplored territory. BMC Med Educ 24 , 391 (2024). https://doi.org/10.1186/s12909-024-05328-y
Download citation
Received : 26 May 2023
Accepted : 19 March 2024
Published : 09 April 2024
DOI : https://doi.org/10.1186/s12909-024-05328-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical students
- Educational skills
- Competencies
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Lyubertsy Study on Mortality Rate in Patients After Cerebral Stroke or Transient Ischemic Attack (LIS-2). Design and Medical Treatment Estimation

2015, Rational Pharmacotherapy in Cardiology
Related Papers
Rational Pharmacotherapy in Cardiology
Sergey Martsevich
Cardiovascular Therapy and Prevention
N. Kutishenko
Aim. As a part of the LIS Study (Lyubertsy Study of mortality in patients after acute myocardial infarction), to assess the patients’ demographic characteristics, specifics of the clinical course and treatment of coronary heart disease (CHD) and other cardiovascular pathology, as well as the risk factor (RF) prevalence before acute myocardial infarction (AMI). Material and methods. The study included all patients (n=1133) who, within the three-year study period, developed AMI and were admitted to Lyubertsy clinics (Moscow Region). Results. The study population included 54,5 % men and 45,5 % women. Mean age of male and female AMI patients was, respectively, 60,1±0,5 and 71,4±0,4 yeas. Approximately 35 % of all participants were working-age men. The majority of the patients had several RFs, among which arterial hypertension (AH) was the most prevalent (76 %). Over 30 % of the patients did not have pre-existing CHD before AMI. Prior to AMI, pharmaceutical treatment was rare; antiplatel...
Stroke; a journal of cerebral circulation
Harold Adams
The Bulletin of Contemporary Clinical Medicine
liton ahmed
Michael Martinov
Fiona Webster
RELATED PAPERS
Revista Cenário
Leandro Brusadin
Italian Journal of Pediatrics
FRANCESCO CLEMENTI
Anales del Seminario de Historia de la Filosofía
Ricardo da Costa
Farah Bariroh
Angewandte Chemie International Edition
Dermot Henry
Arlete Fonseca de Andrade
Alex bautista
The Spine Journal
kavitha kanesalingam
Tiskarstvo 08
maja rudolf
Govor = Speech
Ana Bonetti
Music and the Moving Image
Biochimica et Biophysica Acta (BBA) - General Subjects
MINDY KENDRICK
Research, Society and Development
Ana Carolina Oliveira Santos
Primapersona 22
Fabrizio Mangiameli
Current atherosclerosis reports
Applied Mathematics and Computation
Nanophotonics
Byung Gil Jeong
Journal of Wildlife Diseases
dale Rollins
International Journal of Plant Protection
Dr.Shamarao Jahagirdar
AIP Advances
Michael Farle
JOSE FERNANDO MIRANDA
Circulation
David Strelow
Fernando Paolicchi
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
The Effects of Medical Debt Relief: Evidence from Two Randomized Experiments
Two in five Americans have medical debt, nearly half of whom owe at least $2,500. Concerned by this burden, governments and private donors have undertaken large, high-profile efforts to relieve medical debt. We partnered with RIP Medical Debt to conduct two randomized experiments that relieved medical debt with a face value of $169 million for 83,401 people between 2018 and 2020. We track outcomes using credit reports, collections account data, and a multimodal survey. There are three sets of results. First, we find no impact of debt relief on credit access, utilization, and financial distress on average. Second, we estimate that debt relief causes a moderate but statistically significant reduction in payment of existing medical bills. Third, we find no effect of medical debt relief on mental health on average, with detrimental effects for some groups in pre-registered heterogeneity analysis.
We are grateful to seminar and conference participants at Harvard Business School, Northwestern Kellogg Strategy, University of Chicago Health, Stanford Institute for Economic Policy Research, University of Duisburg-Essen, University of Wisconsin–Madison, Chicago Booth Finance, Waseda University, NBER Economics of Health, NBER Household Finance, the AEA Health Economics Research Organization Session, and BYU Finance for helpful comments. We thank Constantine Yannelis and Tal Gross for thoughtful discussions of the paper and Will Dobbie, Zack Cooper, Amy Finkelstein, Paul Goldsmith-Pinkham, and Matt Notowidigdo for thoughtful comments. The experiments reported in this study are listed in the AEA RCT Registry (#0003332, #0003664, and #0007426) and were approved by Stanford IRB (#57138). We gratefully acknowledge J-PAL North America, the National Institutes of Health (R01 AG066890-01A1), and the National Institute on Aging (T32-AG000186) for financial support and RIP Medical Debt for their partnership on the study. We thank Julie Gasparac, Laurie Imhof, and Nithya Rajendran at NORC at the University of Chicago for survey implementation, and Jinglin Wang, Bruno Mauricio Escobar Izquierdo, Zahra Thabet, and Eleanor Jenke for superb research assistance. Wesley Yin is currently serving in the Office of Management and Budget (OMB), and completed the work on this article prior to joining OMB. The views expressed in this article are those of the authors themselves, and do not necessarily represent the view of the United States or OMB. The views expressed herein are those of the authors and do not necessarily reflect the views of the National Bureau of Economic Research.
MARC RIS BibTeΧ
Download Citation Data
Working Groups
Mentioned in the news, more from nber.
In addition to working papers , the NBER disseminates affiliates’ latest findings through a range of free periodicals — the NBER Reporter , the NBER Digest , the Bulletin on Retirement and Disability , the Bulletin on Health , and the Bulletin on Entrepreneurship — as well as online conference reports , video lectures , and interviews .

- COVID-19 and your mental health
Worries and anxiety about COVID-19 can be overwhelming. Learn ways to cope as COVID-19 spreads.
At the start of the COVID-19 pandemic, life for many people changed very quickly. Worry and concern were natural partners of all that change — getting used to new routines, loneliness and financial pressure, among other issues. Information overload, rumor and misinformation didn't help.
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020.
Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19. And you're not alone if you've coped with the stress in less than healthy ways, such as substance use.
But healthier self-care choices can help you cope with COVID-19 or any other challenge you may face.
And knowing when to get help can be the most essential self-care action of all.
Recognize what's typical and what's not
Stress and worry are common during a crisis. But something like the COVID-19 pandemic can push people beyond their ability to cope.
In surveys, the most common symptoms reported were trouble sleeping and feeling anxiety or nervous. The number of people noting those symptoms went up and down in surveys given over time. Depression and loneliness were less common than nervousness or sleep problems, but more consistent across surveys given over time. Among adults, use of drugs, alcohol and other intoxicating substances has increased over time as well.
The first step is to notice how often you feel helpless, sad, angry, irritable, hopeless, anxious or afraid. Some people may feel numb.
Keep track of how often you have trouble focusing on daily tasks or doing routine chores. Are there things that you used to enjoy doing that you stopped doing because of how you feel? Note any big changes in appetite, any substance use, body aches and pains, and problems with sleep.
These feelings may come and go over time. But if these feelings don't go away or make it hard to do your daily tasks, it's time to ask for help.
Get help when you need it
If you're feeling suicidal or thinking of hurting yourself, seek help.
- Contact your healthcare professional or a mental health professional.
- Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline , available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential.
If you are worried about yourself or someone else, contact your healthcare professional or mental health professional. Some may be able to see you in person or talk over the phone or online.
You also can reach out to a friend or loved one. Someone in your faith community also could help.
And you may be able to get counseling or a mental health appointment through an employer's employee assistance program.
Another option is information and treatment options from groups such as:
- National Alliance on Mental Illness (NAMI).
- Substance Abuse and Mental Health Services Administration (SAMHSA).
- Anxiety and Depression Association of America.
Self-care tips
Some people may use unhealthy ways to cope with anxiety around COVID-19. These unhealthy choices may include things such as misuse of medicines or legal drugs and use of illegal drugs. Unhealthy coping choices also can be things such as sleeping too much or too little, or overeating. It also can include avoiding other people and focusing on only one soothing thing, such as work, television or gaming.
Unhealthy coping methods can worsen mental and physical health. And that is particularly true if you're trying to manage or recover from COVID-19.
Self-care actions can help you restore a healthy balance in your life. They can lessen everyday stress or significant anxiety linked to events such as the COVID-19 pandemic. Self-care actions give your body and mind a chance to heal from the problems long-term stress can cause.
Take care of your body
Healthy self-care tips start with the basics. Give your body what it needs and avoid what it doesn't need. Some tips are:
- Get the right amount of sleep for you. A regular sleep schedule, when you go to bed and get up at similar times each day, can help avoid sleep problems.
- Move your body. Regular physical activity and exercise can help reduce anxiety and improve mood. Any activity you can do regularly is a good choice. That may be a scheduled workout, a walk or even dancing to your favorite music.
- Choose healthy food and drinks. Foods that are high in nutrients, such as protein, vitamins and minerals are healthy choices. Avoid food or drink with added sugar, fat or salt.
- Avoid tobacco, alcohol and drugs. If you smoke tobacco or if you vape, you're already at higher risk of lung disease. Because COVID-19 affects the lungs, your risk increases even more. Using alcohol to manage how you feel can make matters worse and reduce your coping skills. Avoid taking illegal drugs or misusing prescriptions to manage your feelings.
Take care of your mind
Healthy coping actions for your brain start with deciding how much news and social media is right for you. Staying informed, especially during a pandemic, helps you make the best choices but do it carefully.
Set aside a specific amount of time to find information in the news or on social media, stay limited to that time, and choose reliable sources. For example, give yourself up to 20 or 30 minutes a day of news and social media. That amount keeps people informed but not overwhelmed.
For COVID-19, consider reliable health sources. Examples are the U.S. Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
Other healthy self-care tips are:
- Relax and recharge. Many people benefit from relaxation exercises such as mindfulness, deep breathing, meditation and yoga. Find an activity that helps you relax and try to do it every day at least for a short time. Fitting time in for hobbies or activities you enjoy can help manage feelings of stress too.
- Stick to your health routine. If you see a healthcare professional for mental health services, keep up with your appointments. And stay up to date with all your wellness tests and screenings.
- Stay in touch and connect with others. Family, friends and your community are part of a healthy mental outlook. Together, you form a healthy support network for concerns or challenges. Social interactions, over time, are linked to a healthier and longer life.
Avoid stigma and discrimination
Stigma can make people feel isolated and even abandoned. They may feel sad, hurt and angry when people in their community avoid them for fear of getting COVID-19. People who have experienced stigma related to COVID-19 include people of Asian descent, health care workers and people with COVID-19.
Treating people differently because of their medical condition, called medical discrimination, isn't new to the COVID-19 pandemic. Stigma has long been a problem for people with various conditions such as Hansen's disease (leprosy), HIV, diabetes and many mental illnesses.
People who experience stigma may be left out or shunned, treated differently, or denied job and school options. They also may be targets of verbal, emotional and physical abuse.
Communication can help end stigma or discrimination. You can address stigma when you:
- Get to know people as more than just an illness. Using respectful language can go a long way toward making people comfortable talking about a health issue.
- Get the facts about COVID-19 or other medical issues from reputable sources such as the CDC and WHO.
- Speak up if you hear or see myths about an illness or people with an illness.
COVID-19 and health
The virus that causes COVID-19 is still a concern for many people. By recognizing when to get help and taking time for your health, life challenges such as COVID-19 can be managed.
- Mental health during the COVID-19 pandemic. National Institutes of Health. https://covid19.nih.gov/covid-19-topics/mental-health. Accessed March 12, 2024.
- Mental Health and COVID-19: Early evidence of the pandemic's impact: Scientific brief, 2 March 2022. World Health Organization. https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1. Accessed March 12, 2024.
- Mental health and the pandemic: What U.S. surveys have found. Pew Research Center. https://www.pewresearch.org/short-reads/2023/03/02/mental-health-and-the-pandemic-what-u-s-surveys-have-found/. Accessed March 12, 2024.
- Taking care of your emotional health. Centers for Disease Control and Prevention. https://emergency.cdc.gov/coping/selfcare.asp. Accessed March 12, 2024.
- #HealthyAtHome—Mental health. World Health Organization. www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---mental-health. Accessed March 12, 2024.
- Coping with stress. Centers for Disease Control and Prevention. www.cdc.gov/mentalhealth/stress-coping/cope-with-stress/. Accessed March 12, 2024.
- Manage stress. U.S. Department of Health and Human Services. https://health.gov/myhealthfinder/topics/health-conditions/heart-health/manage-stress. Accessed March 20, 2020.
- COVID-19 and substance abuse. National Institute on Drug Abuse. https://nida.nih.gov/research-topics/covid-19-substance-use#health-outcomes. Accessed March 12, 2024.
- COVID-19 resource and information guide. National Alliance on Mental Illness. https://www.nami.org/Support-Education/NAMI-HelpLine/COVID-19-Information-and-Resources/COVID-19-Resource-and-Information-Guide. Accessed March 15, 2024.
- Negative coping and PTSD. U.S. Department of Veterans Affairs. https://www.ptsd.va.gov/gethelp/negative_coping.asp. Accessed March 15, 2024.
- Health effects of cigarette smoking. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm#respiratory. Accessed March 15, 2024.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed March 15, 2024.
- Your healthiest self: Emotional wellness toolkit. National Institutes of Health. https://www.nih.gov/health-information/emotional-wellness-toolkit. Accessed March 15, 2024.
- World leprosy day: Bust the myths, learn the facts. Centers for Disease Control and Prevention. https://www.cdc.gov/leprosy/world-leprosy-day/. Accessed March 15, 2024.
- HIV stigma and discrimination. Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/basics/hiv-stigma/. Accessed March 15, 2024.
- Diabetes stigma: Learn about it, recognize it, reduce it. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/features/diabetes_stigma.html. Accessed March 15, 2024.
- Phelan SM, et al. Patient and health care professional perspectives on stigma in integrated behavioral health: Barriers and recommendations. Annals of Family Medicine. 2023; doi:10.1370/afm.2924.
- Stigma reduction. Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/od2a/case-studies/stigma-reduction.html. Accessed March 15, 2024.
- Nyblade L, et al. Stigma in health facilities: Why it matters and how we can change it. BMC Medicine. 2019; doi:10.1186/s12916-019-1256-2.
- Combating bias and stigma related to COVID-19. American Psychological Association. https://www.apa.org/topics/covid-19-bias. Accessed March 15, 2024.
- Yashadhana A, et al. Pandemic-related racial discrimination and its health impact among non-Indigenous racially minoritized peoples in high-income contexts: A systematic review. Health Promotion International. 2021; doi:10.1093/heapro/daab144.
- Sawchuk CN (expert opinion). Mayo Clinic. March 25, 2024.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and coronavirus
- COVID-19 and pets
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- COVID-19 drugs: Are there any that work?
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 travel advice
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to measure your respiratory rate
- How to take your pulse
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related information
- Mental health: What's normal, what's not - Related information Mental health: What's normal, what's not
- Mental illness - Related information Mental illness
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- International edition
- Australia edition
- Europe edition

Gender medicine ‘built on shaky foundations’, Cass review finds
Analysis finds most research underpinning clinical guidelines, hormone treatments and puberty blockers to be low quality
Review of gender services has major implications for mental health services
The head of the world’s largest review into children’s care has said that gender medicine is “built on shaky foundations”.
Dr Hilary Cass, the paediatrician commissioned to conduct a review of the services provided by the NHS to children and young people questioning their gender identity, said that while doctors tended to be cautious in implementing new findings in emerging areas of medicine, “quite the reverse happened in the field of gender care for children”.
Cass commissioned the University of York to conduct a series of analyses as part of her review.
Two papers examined the quality and development of current guidelines and recommendations for managing gender dysphoria in children and young people. Most of the 23 clinical guidelines reviewed were not independent or evidence based, the researchers found.
A third paper on puberty blockers found that of 50 studies, only one was of high quality.
Similarly, of 53 studies included in a fourth paper on the use of hormone treatment, only one was of sufficiently high quality, with little or only inconsistent evidence on key outcomes.
Here are the main findings of the reviews:
Clinical guidelines
Increasing numbers of children and young people experiencing gender dysphoria are being referred to specialist gender services. There are various guidelines outlining approaches to the clinical care of these children and adolescents.
In the first two papers, the York researchers examined the quality and development of published guidelines or clinical guidance containing recommendations for managing gender dysphoria in children and young people up to the age of 18.
They studied a total of 23 guidelines published in different countries between 1998 and 2022. All but two were published after 2010.

Most of them lacked “an independent and evidence-based approach and information about how recommendations were developed”, the researchers said.
Few guidelines were informed by a systematic review of empirical evidence and they lack transparency about how their recommendations were developed. Only two reported consulting directly with children and young people during their development, the York academics found.
“Healthcare services and professionals should take into account the poor quality and interrelated nature of published guidance to support the management of children and adolescents experiencing gender dysphoria/incongruence,” the researchers wrote.
Writing in the British Medical Journal (BMJ) , Cass said that while medicine was usually based on the pillars of integrating the best available research evidence with clinical expertise, and patient values and preferences, she “found that in gender medicine those pillars are built on shaky foundations”.
She said the World Professional Association of Transgender Healthcare (WPATH) had been “highly influential in directing international practice, although its guidelines were found by the University of York’s appraisal to lack developmental rigour and transparency”.
In the foreword to her report, Cass said while doctors tended to be cautious in implementing new findings “quite the reverse happened in the field of gender care for children”.
In one example, she said a single Dutch medical study, “suggesting puberty blockers may improve psychological wellbeing for a narrowly defined group of children with gender incongruence”, had formed the basis for their use to “spread at pace to other countries”. Subsequently, there was a “greater readiness to start masculinising/feminising hormones in mid-teens”.
She added: “Some practitioners abandoned normal clinical approaches to holistic assessment, which has meant that this group of young people have been exceptionalised compared to other young people with similarly complex presentations. They deserve very much better.”
Both papers repeatedly pointed to a key problem in this area of medicine: a dearth of good data.
She said: “Filling this knowledge gap would be of great help to the young people wanting to make informed choices about their treatment.”
Cass said the NHS should put in place a “full programme of research” looking at the characteristics, interventions and outcomes of every young person presenting to gender services, with consent routinely sought for enrolment in a research study that followed them into adulthood.
Gender medicine was “an area of remarkably weak evidence”, her review found, with study results also “exaggerated or misrepresented by people on all sides of the debate to support their viewpoint”.
Alongside a puberty blocker trial, which could be in place by December, there should be research into psychosocial interventions and the use of the masculinising and feminising hormones testosterone and oestrogen, the review found.
Hormone treatment
Many trans people who seek medical intervention in their transition opt to take hormones to masculinise or feminise their body, an approach that has been used in transgender adults for decades.
“It is a well-established practice that has transformed the lives of many transgender people,” the Cass review notes, adding that while these drugs are not without long-term problems and side-effects, for many they are dramatically outweighed by the benefits.
For birth-registered females, the approach means taking testosterone, which brings about changes including the growth of facial hair and a deepening of the voice, while for birth-registered males, it involves taking hormones including oestrogen to promote changes including the growth of breasts and an increase in body fat. Some of these changes may be irreversible.
However, in recent years a growing proportion of adolescents have begun taking these cross-sex, or gender-affirming, hormones, with the vast majority who are prescribed puberty blockers subsequently moving on to such medication.
This growing take-up among young people has led to questions over the impact of these hormones in areas ranging from mental health to sexual functioning and fertility.
Now researchers at the University of York have carried out a review of the evidence, comprising an analysis of 53 previously published studies, in an attempt to set out what is known – and what is not – about the risks, benefits and possible side-effects of such hormones on young people.
All but one study, which looked at side-effects, were rated of moderate or low quality, with the researchers finding limited evidence for the impact of such hormones on trans adolescents with respect to outcomes, including gender dysphoria and body satisfaction.
The researchers noted inconsistent findings around the impact of such hormones on growth, height, bone health and cardiometabolic effects, such as BMI and cholesterol markers. In addition, they found no study assessed fertility in birth-registered females, and only one looked at fertility in birth-registered males.
“These findings add to other systematic reviews in concluding there is insufficient and/or inconsistent evidence about the risks and benefits of hormone interventions in this population,” the authors write.
However, the review did find some evidence that masculinising or feminising hormones might help with psychological health in young trans people. An analysis of five studies in the area suggested hormone treatment may improve depression, anxiety and other aspects of mental health in adolescents after 12 months of treatment, with three of four studies reporting an improvement around suicidality and/or self-harm (one reported no change).
But unpicking the precise role of such hormones is difficult. “Most studies included adolescents who received puberty suppression, making it difficult to determine the effects of hormones alone,” the authors write, adding that robust research on psychological health with long-term follow-up was needed.
The Cass review has recommended NHS England should review the current policy on masculinising or feminising hormones, advising that while there should be the option to provide such drugs from age 16, extreme caution was recommended, and there should be a clear clinical rationale for not waiting until an individual reached 18.
Puberty blockers
Treatments to suppress puberty in adolescents became available through routine clinical practice in the UK a decade ago.
While the drugs have long been used to treat precocious puberty – when children start puberty at an extremely young age – they have only been used off-label in children with gender dysphoria or incongruence since the late 1990s. The rationale for giving puberty blockers, which originated in the Netherlands, was to buy thinking time for young people and improve their ability to smooth their transition in later life.
Data from gender clinics reported in the Cass review showed the vast majority of people who started puberty suppression went on to have masculinising or feminising hormones, suggesting that puberty blockers did not buy people time to think.
To understand the broader effects of puberty blockers, researchers at the University of York identified 50 papers that reported on the effects of the drugs in adolescents with gender dysphoria or incongruence. According to their systematic review, only one of these studies was high quality, with a further 25 papers regarded as moderate quality. The remaining 24 were deemed too weak to be included in the analysis.
Many of the reports looked at how well puberty was suppressed and the treatment’s side-effects, but fewer looked at whether the drugs had their intended benefits.
Of two studies that investigated gender dysphoria and body satisfaction, neither found a change after receiving puberty blockers. The York team found “very limited” evidence that puberty blockers improved mental health.
Overall, the researchers said “no conclusions” could be drawn about the impact on gender dysphoria, mental and psychosocial health or cognitive development, though there was some evidence bone health and height may be compromised during treatment.
Based on the York work, the Cass review finds that puberty blockers offer no obvious benefit in helping transgender males to help their transition in later life, particularly if the drugs do not lead to an increase in height in adult life. For transgender females, the benefits of stopping irreversible changes such as a deeper voice and facial hair have to be weighed up against the need for penile growth should the person opt for vaginoplasty, the creation of a vagina and vulva.
In March, NHS England announced that children with gender dysphoria would no longer receive puberty blockers as routine practice. Instead, their use will be confined to a trial that the Cass review says should form part of a broader research programme into the effects of masculinising and feminising hormones.
- Transgender
- Young people

Veteran trans campaigner: ‘Cass review has potential for positive change’

Cass review must be used as ‘watershed moment’ for NHS gender services, says Streeting

‘This isn’t how good scientific debate happens’: academics on culture of fear in gender medicine research

Five thousand children with gender-related distress awaiting NHS care in England

Ban on children’s puberty blockers to be enforced in private sector in England

What Cass review says about surge in children seeking gender services

Adult transgender clinics in England face inquiry into patient care

‘Children are being used as a football’: Hilary Cass on her review of gender identity services

Thousands of children unsure of gender identity ‘let down by NHS’, report finds

Most viewed
Oral-History : Yury Gulyaev
- 1 About Yury Gulyaev
- 2 About the Interview
- 3 Copyright Statement
- 4.1 The Early Days
- 4.2 Education, Diploma and PhD
- 4.3 Dissertation under guidance of Prof. V.L. Bonch-Bruevich
- 4.4 Soviet Union after Stalin
- 4.5 The invention of the Interdigital transducer in 1965
- 4.6 Becoming Head of Laboratory in Fryazino
- 4.7 Bleustein-Gulyaev waves
- 4.8 Other types of acoustic waves
- 4.9 SAW devices fabrication in Soviet Union
- 4.10 Future developments in the field of acoustic wave technology
- 4.11 Friends and awards
- 4.12 The Saratov Institute
- 4.13 Carbone Nanotubes
- 4.14 Research in the area of medicine
- 5 References
About Yury Gulyaev
Yury Gulyaev was born on 18 September 1935 in Tomilino, a suburb of Moscow near the satellite town of Lyubertsy. He graduated from Moscow Institute of Physics and Technology, MIPT (1958), and was awarded Ph.D. (1962) and D.Sci. (1970) Degrees. He is a Professor and Head Chair of Solid State Electronics, Radiophysics and Applied Information Technologies (since 1971), Corresponding Member of Acad. Sci. USSR since 1979, Full Member (Academician) of Ac. Sci. USSR and Russian Academy of Sciences (RAS) since 1984, now in the Division of Nanotechnologies and Information technologies of RAS. Starting in 1960 he worked at the Institute of Radio-engineering and Electronics (IRE) Ac. Sci. USSR (later RAS) as a Researcher, Senior Researcher and Head of the Department. He served as Deputy Director since 1972, Director of IRE RAS since 1988, and Scientific Supervisor of IRE RAS since 2004. Gulyaev is the author of more than 500 scientific papers and 11 monographs, and has more than 60 patents. For his scientific work, he was awarded the State Prize of the USSR in 1974 and 1984 and the State Prize of Russia in 1993 and 2006 for his works on Surface Acoustic Waves Devices. In 1995, he was awarded the A.S. Popov Gold Medal of RAS for his works in the field of radio-engineering and electronics. In 1979 Gulyaev was awarded the Europhysics Prize of European Physical Society. In 2006, he was awarded the prestigious IEEE Rayleigh Award for his work on physics and technology of SAW devices for information processing. In 1989-1991 Gulyaev was elected People’s Deputy of the USSR (Member of USSR Parliament) and the Chairman of the Subcommittee on Telecommunications and Informatics of the Committee on Transport, Telecommunications and Informatics of the Supreme Soviet of the USSR. Gulyaev was the President of IEEE Russian Section from 1988-2016, and is an IEEE Life Fellow . He is the President of Russian and International Unions of Scientific and Engineering Associations (RUSEA and IUSEA), Chairman of A.S. Popov Russian Science and Technology Society for Radioengineering, Electronics and Communications. Gulyaev is the Chairman of the Russian URSI (International Union of Radio Science) Committee.
About the Interview
Yury Gulyaev An Interview conducted by Victor Plessky, and Clemens Ruppel, Gorgier/Switzerland, July 13, 2017.
Interview #784 for the IEEE History Center, the Institute of Electrical and Electronics Engineers, Inc.
Copyright Statement
This manuscript is being made available for research purposes only. All literary rights in the manuscript including the right to publish, are reserved to the IEEE History Center. No part of the manuscript may be quoted for publication without the written permission of the Director of the IEEE History Center.
Request for permission to quote for publication should be addressed to the IEEE History Center Oral History Program, IEEE History Center, 445 Hoes Lane, Piscataway, NJ 08854 USA or [email protected]. It should include identification of the specific passages to be quoted, anticipated use of the passage, and identification of the user.
It is recommended that this oral history be cited as follows:
Yury Gulyaev, an oral history conducted by Victor Plessky, and Clemens Ruppel, Gorgier/Switzerland, July 13, 2017
INTERVIEWEE: Yury Gulyaev
INTERVIEWERS: Victor Plessky, and Clemens Ruppel
DATE: July 13, 2017
PLACE: Gorgier/Switzerland
The Early Days
Yury, you were born in 1935 near Moscow. Please tell us a little bit about your early days!
I was born on September 18, 1935 in the suburb of Moscow, called Tomilino near satellite town Lyubertsy, Moscow region. My father, Vasiliy Sergeevich Gulyaev, worked as an economist in the Ministry of Finances of the USSR. My mother, Eugenia Dmitrievna Anisimova, a medical doctor, worked at a local policlinic. We lived in a small private house (with 0,3 hectare of land) that was built in 1933 on the money of my grandfather. At the beginning of the Second World War in 1941 my father and mother were mobilized to the army. I was sent to my grandparents, to a small village named Gulyaevo (22 houses) on the bank of the Vyatka river near the Urals. In 1943, I have entered in an elementary (8 classes) school in the big village Shurma (23 km from Gulyaevo), where my mother worked in the hospital as a military doctor. She got a house where we lived. After the first week in the 1st class of the school I was transferred to the 2nd class, as I could already read, write and count. In 1945, my father was demobilized from the army and returned to Gulyaevo since he was not able to work at the Ministry of Finances due to heavy wounds.
Please tell us more about your home village Gulyaevo!
I should tell some words about Gulyaevo village. It was a small village of 22 houses (families), and everybody had last name “Gulyaev”. As far as I know all the villagers before the end of serfdom in Russia in 1861 were serfs of the landlord, named Gulyaev. Therefore, after serfdom abolition all of them have kept that last name. Besides all of them were quite rich peoples. For example, my grandfather owned a big house with about 2 ha of land, 1 horse, 2 cows, several pigs, sheep and chicken. To grow harvest of wheat, potatoes, vegetables, etc. my grandfather used hired labor from poorer neighbor villages. In Russian terms, he could be called a “kulak”. The other families in Gulyaevo were equally rich and in fact quite good friends. So, nobody tried to write negative reports on each other because of envy. This explains the fact that during the Stalin repressive crackdowns in the 30ies nobody from Gulyaevo suffered. In the course of collectivization of the agriculture Gulyaevo’s inhabitants formed a collective farm or “kolkhoz’, where everybody had a certain position. For example, my grandfather became the head of the cattle-yard as he had some veterinary education. During the Second World War, almost all men of the age from 18 up to 50 years old were taken to the army and the majority of them were killed. So, in the 40ies and 50ies the welfare at Gulyaevo was quite poor, the household management was performed mainly by women, old men and children.
My farther became the head of Gulyaevo collective farm (“kolkhoz”) as he had agricultural education and as many working age men from Gulyaevo were killed in the war. In 1950, the health of my father significantly improved due to fascinating nature of Gulyaevo (river, forest, fishing, etc.). I graduated from the last 8th class of the school and all of our family returned to Tomilino (Moscow region). In that time, our family consisted of father, mother, me and 2 my brothers: Boris (born 1941) and Valeriy (born in 1948). About their present positions, I will tell later. In September 1950, I entered the 9th class of the middle school (10 classes) in an adjacent Lyubertsy town and graduated from it in 1952. Entering that school, I was afraid that it would be more difficult to study there due to the nearness to Moscow and higher requirements. However, in reality it turned out that it was easier to study in this school. The point is that in Shurma’s elementary school, the teachers on physics, mathematics and literature were professors in exile and the level of teaching of mentioned subjects was very high!
Education, Diploma and PhD
Please tell us how you decided to study physics.
After finishing school, I decided to enter journalistic department of the Lomonosov Moscow State University (MSU). Why journalistic?
The point is that in Lyubertsy’s middle school the Russian language and literature were taught by an excellent teacher and a wonderful person Dr. A. Lapitsky, to whom all of us indebted and respected. His lessons were extremely interesting. Therefore, it is quite understandable that my favourite subject was literature. I myself wrote several booklets of poetry and prose although never shared it with anybody and it had never been published. However, I was interested in other subjects: physics, mathematics, history, etc. I had an excellent score on all subjects that we studied. At home I carried out experiments in a new highly developing branch of physics: radio physics. For example, I constructed and made a radio receiver in accordance with Dr. Momot ideas, that was able to receive the signals of jammed stations including the Voice of America. Nevertheless, I have chosen the journalistic department. But the God decided it in another way!
To enter the Journalistic Department of the MSU, we, me and my classmate and friend Rail Safarov, came to Mokhovaya Street in the center of Moscow, where it is located up to now. However, our documents were not accepted since we had only certificates regarding graduation from the school, but not yet formal Diplomas (which have been given to us later). At the moment when we were thinking what to do, one tall young man (later we found out that he was 2nd year student of Moscow Institute of Physics and Technology (MIPT), assisting at entrance exams) and said that our desire to get into MSU Journalistic Department is at least stupid. Maximum on what we can hope it is the Chief Editor position at some regional newspaper in province. And he added: by the way in the same corridor there is Entrance Exams Commission of MIPT, or so called PhysTech, and physics is the most perspective science with brilliant future. We have thought once more and submitted documents to PhysTech commission, where they accepted us even without Diplomas. Thus, my coming to physics was to certain degree accidental. We have passed entrance exams with highest marks «5» and were accepted to PhysTech in spite of competition 13:1. Thus, in 1952 I was accepted to Radiophysical Department of Moscow Institute of Physics and Technology (PhysTech).
When and why did you start with sports?
As award for entering to the High School my father bought me the voucher to spend one month at resort near Moscow, where I soon understood, to my regret, that I was not attractive as a man: very small (1,64 m) and weak. The girls didn't pay attention on me and I was very sorry with this circumstance. So, I got into sport exercises especially in swimming and running. Later at PhysTech I continued regular sport training in swimming, boxing and heavy athletics. Suddenly I have started to grow and after 1st year of studies my height was already 1,78 m. So, during 1 year I have grown up by 14 cm and got rid of my complex of infantility!
Studying physics in Moscow is a little bit different to what I know. Please tell us about the system at PhysTech!
In the beginning of the first year of study my pendulum moved to the other side: in the first semester of the 1st year I practically did not visit lectures and seminars and was completely busy with sport and girls, but before Winter exams I remembered that always at the school I had highest marks (5) and it is not good to fall down to lower level. So about one month before exams I started seriously study physics, mathematics and English (at school I studied German) using textbooks. Later when I understood who were higher level scientist who made lectures to us I deeply regretted that I didn’t listen their lectures. For example, general physics was presented by Prof. G.S. Landsberg, who discovered combination light scattering independently from Raman, Mathematical analysis was given by Prof. F.R. Gantmakher, famous mathematician in the matrix theory.
Nevertheless, the first exam session I passed with only the high (5) marks as all the other sessions during my training at the PhysTech.
However, one subject I studied regularly from the beginning: it was English. As I already mentioned at the school I studied German, but at the Institute it becomes clear that for the future work English language is much more important. Since I didn’t know English at all, I started training at so called “retarded” group (for beginners or for those who knew English weakly), but with very good teacher Vera Belokryltseva. After one year training, she provided the level of my English enough to join the advanced group (who studied English from the beginning at the school) where she also was a teacher. After completing of my training in the PhysTech I was speaking and writing in English fluently as majority of PhysTech graduates! I always remember her with the feeling of great gratitude.
So, my everyday life at PhysTech began. A few words about education system at PhysTech: it has official name “PhysTech System”. Main feature of this system is that only 1st year students have training at main MIPT Campus in Dolgoprudny city, 30 km from Moscow. There they have training in general subjects: mathematics, general physics, chemistry, foreign language (by choice), drawing, sport, etc. with corresponding practical training. Starting from the 2nd year some part of education is performed at affiliated chairs, so called “bases”, which are usually at the institutes of Russian Academy of Sciences or at high-level industrial enterprises. There students have lectures and practical seminars in special subjects, concerning with their future professional activity. After 4th year education is almost 100% at the bases. Usually after graduation with diploma of engineer-physicist between 5th and 6th year of training student stays at the base for work as a scientist. The best students are recommended to continue education for next three years for candidate of science degree (some analog of PhD, but a little bit more) either at PhysTech itself or at the base. Later, in the case of success, researcher could get D.Sc. degree, usually 5-10 years after candidate degree, already been well known specialist. Of course, there are exceptions: for example, one of the creators of the Russian Atomic and hydrogen bombs Prof. Ya.B. Zeldovich received D.Sc. degree not having even Diploma about graduation from the school!
So, on the 2nd year of training in 1953 I was directed to the base, high level industrial institute, that specialized in radars and radio navigation devices development, to antennas department. But after half a year I understood that it is not very interesting direction for me and passed to the newly opened semiconductor department headed by one of the leaders of semiconductor physics and technology in USSR Prof. S.G. Kalashnikov. This was the time of rapid growth of semiconductor industry in the World and investigations at Kalashnikov’s department were made on high international level. I can tell here some sad story. Two Kalashnikov’s co-workers have seen the influence of current through one contact on the current through adjacent contact on the surface of semiconductor, i.e. point transistor effect 3 month before discovery of the transistor. But Kalashnikov decided that it is influence of some dirt at the surface and asked them to clean the surface to avoid this effect. During the time of cleaning of the surface famous Nobel paper by Bardeen and Brattain on invention of the point transistor was published. Thus, Russia didn’t get this Nobel Prize, but it was so closely!
In January 1955, whole Kalashnikov’s department was moved to newly created Institute of Radio- engineering and Electronics of the USSR Academy of Sciences (Now IRE RAS), where I work already for 62 years. Here I got acquainted with outstanding physicist-theoretician Victor Bonch-Bruevich, who worked part time in Kalashnikov’s department. He suggested me to work with him in the field of semiconductors theory. When I have agreed, he said me that we depart for two years. During that period, I should pass through all (or part) famous Landau theoretical minimum. I knew that it is very heavy task and it is the condition for work in Landau School, but I decided to do it. After three months of preparations during day and night to first exams (in Mathematics). I called Landau and said that my name is Yury Gulyaev and I want to start passing through his theoretical minimum exams. He answered: “So far, I am not interested to know your name. Come to my room at the Institute of Physical Problems on Tuesday next week at 10 o’clock”, and he gave me the address. I came at appointed time. The door was opened by very beautiful young woman (as I knew later it was his wife Kora). She accompanied me to completely empty room: only table and two chairs. She suggested tea or coffee. Soon Landau entered, proposed three problems for solving from the field of differential and integral calculations and disappeared not asking me about anything. During about 3 hours when I was solving these problems (not using any textbooks or materials because of their absence) Kora came three times bringing coffee. Finally, I said her that I am ready. Landau came and almost not asking me questions in 5 minutes understood that I solved problems correctly. Then he smiled and asked about my name and about educational institution, where I have training. I answered that I’m PhysTech student with the base at IRE RAS. He said that he is very glad that at PhysTech (of which he was one of creators) there are good students. Then he said that next exam (mechanics) I should pass to E.M. Lifshits, when I will be ready. I left his apartment being enchanted by personal contact with one of the greatest scientists in the World. In 2 years, I had passed 5 exams (from 9) and Bonch-Bruevich said me that this is enough, since I’m going to work in the theory of solid state, not in nuclear physics. My diploma work was devoted to some corrections to Conwell-Weisscopf formula for scattering of electrons on impurities in semiconductors when Born approximation is not valid. When I brought the paper about this work for publication in a journal and asked Bonch-Bruevich to sign it as co-author, he became angry and rejected to sign. He said: “I never sign the papers about research, in which I didn’t take essential participation. And this is the case, so maximum what I can allow you, to express my gratitude for discussion on the theme”. This was a good lesson to me for the future. My paper was published in the beginning of 1959 in the first issue of newly created journal “ Solid State Physics” under only my name. [1]
During PhysTech years I was quite deeply involved into sport: swimming, boxing and weightlifting, but not in politics. However, as one of the best students I was delegated to 7th November 1952 demonstration on Red Square. For the first (and the last) time I have seen Stalin alive. When he died on 5th of March 1953 I was between the first people who passed near his coffin in the Hall of Columns (Moscow). At that day, many people died or were injured in huge crowds moved to see Stalin coffin. My parents were quite anti-stalinists (but never spoke about it outside of home). So, this funerals for me were more sporting event rather than some political action.
Dissertation under guidance of Prof. V.L. Bonch-Bruevich
What came next after graduation in 1958?
After graduation from PhysTech I was recommended to continue education for the next three years either at PhysTech or at the base. I preferred the base and in 1958 became the PhD student at IRE Academy of Sci USSR under guidance of Prof. V.L. Bonch-Bruevich. Topic of my dissertation was the consideration of some questions of recombination of carriers in semiconductors, in particular recombination on dislocations. It the same time I continued swimming almost professionally: I was member of All-Union sport team “Burevestnik” in swimming and was going to get highest sport title “Master of Sport”. In 1958, I got married. My wife was a student in economics. In 1959, we have got a son. My postgraduate student’s stipend was not enough to keep the family, so I was compelled to stop big sport and started to make money by teaching: training of young scholars to join PhysTech, Lomonosov MSU and Moscow Institute of Physics and Engineering (MIPE). I have got a state license and was giving private lessons. Our life became more or less normal.
Soviet Union after Stalin
When Nikita Khrushchev came into office many thing changed in your life!
In general, our life in Soviet Union after famous speech by Nikita Khrushchev at the XXth Congress of CPSU with denunciation of Stalin ‘s purges was drastically changed. Nobody now was afraid that at night any car could come and take off him to jail, everybody could speak freely in the streets, etc. So, all of us felt the wind of freedom: it was called “Khrushchev thaw”. In 1960, I joined IRE Acad. Sci. USSR as Junior Researcher and in 1962 successfully defended my Candidate of Science dissertation. The main achievements of my dissertation work were the theory of “impact recombination” of carriers in semiconductors (inverse process of so called “ impact ionization”) and the theory of carriers recombination on dislocations. [2] [3]
Soon the possibility to go to England for temporal work in certain University during one year was opened. To do this it was necessary to pass through some competition including knowledge in English. Together with 30 young specialists, I was recommended and in July 1962 was invited to be Assistant Professor in Manchester University at Physical Department headed by Lord Brian Flowers, one of the creators of the British atomic bomb. In practice, I was working with Prof. Samuel F. Edwards (later Sir Sam) on the theory of electronic properties of heavy doped semiconductors with the application of Feynman path integrals technic.
It was wonderful year in my life. For the first time I was abroad in completely different World and where? In the cradle of capitalism, in England. Besides of the interesting work in outstanding team of physicists I again started sport training and was a member of swimming team of Manchester University, showing on 100-yard distance 3rd time in the team (the first result had a bronze medalist of previous Olympics!). During this year, Edwards and me published 2 papers in Proc. of Royal Soc. and Proc. of Phys. Soc., [4] [5] [6] where we developed steepest descent method for Feinman continual integrals and obtained general expression for conductivity of disordered heavily doped semiconductor which later, by other authors, was used in the theory of semiconductor lasers. The paper [4] is cited in mathematical textbooks and is one of the most cited my works.
When coming back to Moscow, you start working in the area of acoustic waves!
After returning to the USSR, I became interested in the problem of conversion of the energy of d.c. current to the energy of high frequency oscillations (microwaves) by solid state devices. Of course, there have been known and quickly developing transistors, but they at that time couldn’t work at microwave frequencies 100 mHz-100 GHz or more. So, everybody was seeking for mew physical phenomena. One of such phenomena was amplification of acoustic waves in piezoelectric semiconductor CdS, experimentally observed by Hudson, McFee and D.L. White [7] in 1961. Theoretically, this effect has been predicted by Tolpygo and Uritsky [8] and independently by Weinreich [9] in 1956. This effect opened possibility of creation of solid state analog of famous vacuum travelling wave tube (TWT). However, soon it became clear that to realize this device with the use of known piezoelectric semiconductors (CdS, ZnO, etc.) practically is not possible as mobility of electrons in such materials is very low, so one should use very high driving voltages and crystals burn out.
Thinking of this problem I came to idea to use for amplification surface acoustic waves (SAW). SAW travelling along the surface of piezoelectric is accompanied with the wave of electric field over the surface. By this field, SAW can interact with electrons in adjacent to surface material (metal, semiconductor, etc.) and vice versa, electric fields in adjacent material can interact with SAW travelling along the surface of the piezoelectric. If, for example, adjacent material is semiconductor in which exists supersonic drift of electrons in the direction of SAW propagation, then SAW will be amplified – already in full analogy with TWT. Only now one can use as adjacent material non-piezoelectric semiconductor with high mobility of electrons. This idea and corresponding calculation of amplification coefficient I presented in 1963 to Bonch-Bruevich seminar. Bonch-Bruevich immediately estimated the physical sense and practical value of this idea and suggested me to report it at the most prestigious in Moscow seminar of acad. V.L. Ginzburg. When in 1964 I claimed for the report at this seminar, I was said that there is a big queue and to the seminar there is presented a report on the same topic by Ginzburg’s post-graduate student Vladislav Pustovoit (with whom I was not acquainted). So, they put our reports at the same seminar. The idea in both reports was the same, only we used different calculation methods. The results of course were the same. After the seminar Ginzburg advised us to join together and apply first for the patent on new device and then for joint publication. Finally, we sent the article to Journal of Experimental and Theoretical Physics (JETP) where it was published in Dec. 1964. [10]
The invention of the Interdigital transducer in 1965
A revolution in the development in SAW technology happen in 1965!
In the next year, 1965, American scientists R.M. White and F.W. Voltmer suggested further development of the idea of SAW interaction with the electric fields and electrons in adjacent to the surface conducting material – interaction with periodic grating of metallic electrodes on the surface of piezoelectric – interdigital transducer.<refname="refnum10">R.M. White, F.W. Voltmer, Appl. Phys.Lett., 1965, 17, 314</ref> This brilliant work opened possibility of direct effective way to excitation and detection of SAW. In fact, it was some kind of so called “travelling wave antenna’ used for excitation and detection of electromagnetic waves . [11] Our work [10] and work of White and Voltmer<refname="refnum10"/> were as far as I know the first publications on the use of SAW in microwave electronics. Both ideas were experimentally realized in 1968 – 70 in several works. [12] [13] [14] In our work [15] there was suggested the idea and developed the theory of SAW amplification by the electron beam propagating near the surface of piezoelectric dielectric. Later this effect was experimentally obtained in the work. [16]
First applications for SAW technology was signal processing?
Next fundamental step in the problem of signal processing with the help of SAW have been done in 1969 by Tancrell et al, [17] where they suggested a dispersive delay line with an interdigital transducer with periodicity of electrodes changing gradually from one end to another end of a transducer. Hartemann and Dieulesaint, [18] Kovalev and Yakovkin [19] and Tancrell and Holland [20] suggested to make “weighting” of electrodes (different overlapping of electrode length) for formation of required frequency curve of the transducer, in particular for reduction of the side lobes of the compressed pulse. It allowed to create on the basis of SAW famous Kallman filter with arbitrary amplitude-frequency curve (AFC). For to avoid the parasitic effects in SAW filters Yu.V. Gulyaev at al [21] and independently D. Malocha et al [22] suggested so called “capacitive tap weighting” of electrodes in interdigital transducer. This construction of transducer is much more flexible for formation of required AFC and allows to make SAW filters with better quality.
Eric Ash [23] proposed a grating structure (analog of Bragg reflector for light) for reflecting of SAW and made the first SAW resonator. Also, he invented SAW waveguide. [24] Ted Paige et al. [25] invented the multistrip coupler. Gordon Kino at al [26] proposed an analog convolver computing analogically the convolution of two different signals.
Kiel Ingebrigtsen [27] proposed phenomenological method for calculation of SAW devices characteristics. It was based on introduction of so called “effective dielectric constant” obtained from the measurements of SAW velocity on free and metallized (when piezoelectric fields are shortened) surfaces of piezoelectric. Ingebrigtsen’s method if widely used in calculations and construction of SAW devices even in complicated cases.
I would say that the years 1962-1975 could be called the “golden years” of a new branch of physics and technology which got the name “acoustoelectronics”. This term first appeared at the Sendai symposium 1968 (Japan) and in narrow sense meant investigations of phenomena connected with interaction of high frequency acoustic waves (ultrasound with frequencies higher than 1MHz) with electrons and electric fields in various solids -- piezo electrics, ferro-electrics, non-piezoelectric dielectrics, metals, etc. These ultrasonic waves (both bulk and surface) occurred to be very good new tool for investigation of electronic and mechanical properties of solids. Now under term “acoustoelectronics” one understands all phenomena in solids connected with participation of high frequency (over 1 MHz) acoustic waves. Sometimes these phenomena are called “ microwave acoustics”. There appeared a lot of publications both theoretical and experimental, in USA, USSR, England, France, Japan, Germany etc.in this field.
Becoming Head of Laboratory in Fryazino
In 1965, you moved to Fryazino!
In 1965, I moved to Fryazino part of our Institute (30 km from Moscow) where I became the Head of Laboratory dealing with the investigations of electronic properties of semiconductors. In fact, we studied electro physical properties of semiconductors and acoustoelectronic phenomena. It was not big laboratory – 5 candidates of science (PhD) and about 5-6 postgraduate and undergraduate students, mainly from PhysTech. Nevertheless during 12 years (1965-1977) we published more than 50 papers in leading journals – JETP, JETP Letters, FTT (soviet physics-solid state), FTP (Physics and Technology of Semiconductors), Physics Letters, Transactions of IEEE on Sonics and Ultrasonics etc. Among the main our achievements during these years there are prediction and theoretical investigation of a new class of kinetic phenomena in semiconductors connected with the drag of electrons by acoustic waves: acousto-magneto-electric (AME) effect, [28] acousto-thermal effects, [29] [30] Peltier effect due to drag of electrons through contact of two materials, [30] acoustoelectric effect in semiconductors with “hot” electrons, heated by the acoustic wave, [31] acousto-magneto-thermal effect, [32] acousto-concentration effect and acousto-luminescence [33] etc.
There were predicted giant quantum oscillations of acoustic wave absorption coefficient in quantizing magnetic field, [34] developed theory of acoustoelectric effect on SAW in semiconductors including “ transverse” acoustoelectric effect, [35] later experimentally found by Kmita and Medved. [36] There was created the analytical nonlinear theory of acoustic wave absorption and amplification at arbitrary large amplitude, [37] developed nonlinear theory of acousto-optic phenomena in conducting and active solids. [38] In the works of Auld et al [39] and Gulyaev and Plessky [40] it was shown that along the periodically rough surface of any solid there can propagate pure shear SAW – in analogy with slow electromagnetic waves in slowing comb structures. These waves are used today to decrease the losses in delay lines and filters and to increase Q-factor of SAW resonators.
Could you told me was there the registration of discoveries in the Soviet Union?
Yes, in Soviet Union at that time there existed a rule to register and certificate on the State level “ discoveries” in science, similar to certification of patents. So, mine with Eric Epstein theoretical prediction and experimental observation of AME effect by Korolyuk and Roy [41] were registered as our “discovery”. The referee of our work was famous scientist M.A. Leontovich (“boundary conditions by Leontovich” are well known in electrodynamics). He knew me personally, so he “opened himself” and said to me: “You know that I am against State registration and certification of discoveries. Scientists themselves know, is this work a discovery or not. But this your work is indeed good and as there is a rule to register discoveries, I wrote positive conclusion on that work”. That was enough for corresponding Committee to award us with the Diploma for discovery No 133.
What about the team in Fryazino?
Almost all members of my Fryazino team became well known scientists: doctors, professors, including previous postgraduate students. Two of them: Alexandr Bugaev and Sergei Nikitov were elected members of the Russian Academy of Sciences. Several of my pupils live and work abroad: Victor Plessky, one of the leading world scientists in the theory of SAW devices, now works in Switzerland, Alexander Kozorezov is outstanding scientist, professor of physics at Leicester University (England), specialist in solid state theory; Boris Elenkrieg now is in Canada, specialist in electrical engineering and microwave technique; Andrey Matlashov is a scientist in the field of biomedical radio electronics in Los-Alamos (USA), etc. I have very good relations with all of them, visit them, exchange with them scientific ideas and problems.
Bleustein-Gulyaev waves
Could you please detail the history of Bleustein-Gulyaev waves?!
Now I would like to tell the story about the discovery (suggestion, theory and experiment) of principally new acoustic phenomena – pure shear surface acoustic waves in piezoelectric crystals, called “Bleustein-Gulyaev waves” (BG waves). When in 1967 I began to prepare my D.Sc. thesis (dissertation), I wrote down a general system of equations describing acoustic waves propagation in piezoelectric crystals (dielectrics, semiconductors) taking into account the symmetry of the crystals, piezo-effect, electrostriction, interaction of acoustic waves with electrons via piezo-effect and via deformation potential etc. When solving this system of equations, in addition to bulk acoustic waves I found a solution which corresponds to the known Rayleigh SAW modernized due to the presence of piezo-effect and the interaction with free electrons via both the piezo-effect and the deformation potential. This wave generally has two components of mechanical displacements – longitudinal, in the direction of the wave propagation, and transverse, perpendicular to the surface. Of course, in anisotropic crystals the directions of mechanical displacements may be at certain angles with respect to the propagation direction and to the normal to the surface.
During careful investigation of the general solution of the system of equation mentioned above I suddenly noticed that at certain symmetry of the crystals (for example, Cv) there is another exact solution in the form of pure shear SAW with mechanical displacement parallel to the surface and perpendicular to the direction of the wave propagation. For some symmetries of crystals (for example, for cubic crystals) such solution doesn’t exist. In dielectrics without piezo effect this wave turns to a usual shear bulk acoustic wave, i.e. the surface character of this new SAW is due to presence of piezo effect. In piezoelectric semiconductors, the surface character of the wave may be changed due to the interaction of the electrons with the acoustic wave. In May 1967 I reported these results at the Bonch-Bruevich seminar in IRE. Bonch-Bruevich was very skeptical: he said: "This is classics". I’m sure that this solution is in textbooks, you should better go to the library and read books more attentively. I advise you to forget about this wave and continue to work on non-linear theory of acoustoelectronic interaction”. So, I did, and returned to the question about this wave only at the end of 1968, when I went to Lenin library, looked through all textbooks on acoustics and… didn’t found this wave! I came again to Bonch- Bruevich and asked what to do. He said: “To be funny in science is possible only once, after this everybody will consider you not to be serious." Publish, if you want, but this is a big risk”. In spite of his opinion, I’ve sent the paper for publication to JETP Letters on Oct.17, 1968. It was published in January 1969 issue of the journal. [42] In February 1969 in Journal Appl.Phys. Lett, Dec.1968 I found the paper by J. Bleustein [43] on the same Shear SAW with the same result, besides it was only for piezodielectrics. I immediately looked to the date of submission of Bleustein’s paper and found that it was 20 days (!) later than the date of submission of my paper. [42] So, it is obvious that two works [42] and [43] were made independently – my paper was submitted for publication earlier, but his paper, due to shorter time of publications in Appl. Phys. Lett., was published earlier. If in spite of skepticism of Bonch-Bruevich I submitted my paper in May 1967 then my paper would be published much earlier, say in August 1967. But it happened what happened! In summer 1969, being at the Conference on Sonics and Ultrasonics in Aviemore (Scotland) I met young handsome scientist and engineer Charles Maerfeld. He told me that his colleague Pierre Tournois and him are doing experiments on observations of so called “Bleustein waves”. I said him that I know about Bleustein paper, but that I predicted and made the theory of these shear SAW earlier than Bleustein. At that time, the January 1969 issue of JETP Lett. with my paper was already translated and published in English.
Next year, 1970, I have been working for a half of the year in USA at Berkeley University with Prof. R.M. White and at Ultrasonics Symposium at New Hampshire I again met Maerfeld and Tournois, who presented the report on experimental observation and amplification of, as they called them, “Bleustein-Gulyaev Shear Surface Acoustic Waves”. [44] It was an excellent example of scientific purity and delicacy! I’m very grateful to them for this. After their paper, everywhere – in articles, textbooks, etc. these waves are called Bleustein-Gulyaev waves, or BGW.
Other types of acoustic waves
What about Maerfeld-Tournois waves?
Here I should say, that approximately at the same time BGW were observed also in CdS by scientists from parallel to my group laboratory in our Institute IRE, A.I. Morozov and M.I. Zemlyanitzyn. [45] But they even didn’t inform me about their experiments, so I consider C. Maerfeld, F. Gires and P. Tournois as pioneers in experimental observation of new phenomenon in acoustics – existence of shear surface acoustic waves in piezoelectric materials. C. Maerfeld and P. Tournois themselves predicted the existence of another new shear surface acoustic wave, which under certain conditions can propagate along the interface of two different media, in some sense counterpart of Stoneley waves, which are called “Maerfeld-Tournois waves”. [46] Various types of surface acoustic waves in inhomogeneous media are described in our book. [47] Other types of shear surface acoustic waves in solids are described in my review paper. [48]
Now I want to notice that there exists and is widely investigated a wide class of so called “quasi BGW”, the “ almost shear” waves, whose surface character is provided by the piezo-effect. The point is, as I already told, that the BG wave is exact solution of the system of acoustic waves propagation equations only for certain symmetries of the crystals and for certain cuts and propagation directions. If you change some of these conditions, say change a little bit the cut of the crystal, the BG wave will be no more the exact solution, it becomes a little bit “ leaky” and besides shear mechanical displacement will have some other displacements, so will be “quasi shear wave”. But in some cases the piezoelectric properties of these “quasi BGW” improve, the velocity also changes in necessary way, so in spite of some “leakage” these waves may be better for applications in SAW devices. It happens for some cuts of LiNbO3, LiTaO3, where “leaky” SAW, used in SAW filters, by their structure are mainly shear SAW with strong piezoelectric coefficient, and are quite close to BGW. [49] [50]
SAW devices fabrication in Soviet Union
Let’s talk about the development of SAW devices fabrication in the Soviet Union!
In 1970-1990 wide investigations of the physical phenomena connected with the interaction of SAW with electric fields and electrons in piezoelectric dielectrics and semiconductors and in layered structures piezoelectric-semiconductor were carried out in Europe, USA, USSR, Japan, Germany and in other countries. It led to intensive development of acoustoelectric devices for various radio-electronic systems of information processing and for telecommunications (see for example an excellent review paper by D. Morgan [51] and the book [52] ).
At the beginning of 70th there started a wide production of SAW devices – band pass and dispersive filters, delay lines (including dispersive), resonators and generators, coding-decoding devices, fast Fourier transformers, digital Nykwist filters, frequency synthesizers, convolution and correlation devices, sensors etc. Many firms took part in this production such as Murata, Kyoto Ceramics, Fujitsu, Hitachi, NEC, Samsung, SAWTEK, Thompson CSF, Vectron, Motorola, Siemens, EPCOS and others. We in the Soviet Union organized production of SAW filters for TV-Secam in Cherkassy (Ukraine) and Minsk (Belorussia), both now it is out of Russian Federation. Today in Russia SAW devices are produced by Morion, Butis-M, Phonon, ONIIP and some other not big firms.
At the end of the 70th I with my coworkers, besides the USSR authors certificates and patents, had 15 foreign patents of the USA, Great Britain, France, Japan and Germany for SAW filters with capacitive tap weighed electrodes. [21] In connection with the existing rules in the USSR at that time all the patents belonged to the State as they had been received during the work for the state budget. So, the USSR was the owner of the patents and it had rights to sell them. For example, the State (Ministry of trade) sold our patent to the Japanese firm “ Murata”. We received a single-time reward for three authors. Another patent was used in “Samsung” and three members of my team went for 6 months to Seoul to help in the organization of production of TV filters there.
Unfortunately, today in Russia there is no production of national TV sets, automobile radios, radio broadcasting receivers, cellular telephones etc. So, there is no need in wide scale production of SAW filters and other acoustoelectronic devices in Russia, what is very sad!
Future developments in the field of acoustic wave technology
What do you expect in future development of SAW technology?
What future I see for acoustoelectronic devices (in particular for SAW devices)? I will point out several directions, which are already seen:
- First of all – it will be SAW RFID tags, after the improvements (better reception sensitivity, solution of “collision” problems, etc.) they can be widely used everywhere – from commodity goods to planes, rockets, weapons, trains, automobiles etc. – up to personality identification.
- Use in acoustoelectronic devices bulk acoustic waves of very high frequency (more than 3GHz), where Rayleigh SAW has big losses in the surface layer due to polishing treatment. These BAW filters will be used in clocks, telecommunications, cellular phones navigation systems (GPS type), measurements and control technique, rocket and space technologies, etc. The alternative to it – the use of Bleustein-Gulyaev waves or ”quasi BGW”, which penetrate to a solid much deeper and so the surface treatment is less harmful.
- Development of SAW sensors. Today they are already used for identification of gases, vapors and liquids. The improvements of constructions, using various new types of SAW, BAW and plate modes (see for example, [53] [54] [55] ) will allow to use these sensors for detection of poisons and narcotics.
- Already mentioned amplifier of SAW by supersonic drift of electrons in layered structures piezoelectric-semiconductor of the TWT type. [10] This amplifier has the advantage with respect to transistor amplifier – it’s input and output are electrically completely isolated from each other.
- So-called “acousto-injection transistor” [56] [57] where signal amplification is connected with modulation of conductivity between collector electrodes due to the bunching of electrons by the acoustic wave.
- Charge coupling devices (CCD) connected with the charge transfer by the acoustic wave. [58] [59]
- Convolvers and correlators based on transverse acoustoelectric effect of SAW. [35] [36] Due to their much higher efficiently in comparison with the convolvers on piezodielectrics, one may hope for their wide use for pattern recognition and other information processing.
- One more application of transverse AE effect is a device for reading images with the help of a short acoustic pulse, propagating in layered structure piezoelectric-photosensitive semiconductor. This pulse produces local transverse AE effect [35] in accordance with local conductivity. It is a solid-state analog of the famous “videkon” where reading of conductive profile is executed by the electronic beam in vacuum.
Friends and awards
What about friends and awards?
For a more detailed history of acoustoelectronics development in the world in 60th and 70th years see our review paper with my friend and colleague the outstanding scientist and engineer Fred. S. Hickernell [60] who unfortunately passed away a few years ago.
In general, I should say that in my experience of scientific work all colleagues with whom I worked (including, of course, my pupils) become usually my quite close friends, partly because I never was envious to successes of my colleagues and always was happy when my pupils and friends had some good achievements. Maybe it goes up to main life principle of my father – “Don’t be a scoundrel and work hard” –which he accepted from peasants of his native village Gulyaevo and inculcated upon me in my childhood. I was lucky: in each field of science where I worked, I always had good friends-colleagues. There are so many of them that I cannot give here all the names. I can only name (in arbitrary order) several scientists of the old generation, who were the founders of acousto-electronics such as Vladislav Pustovoit, Vadim Gurevich, Igor Yakovkin, Igor Victorov, Sergey Bogdanov, Vitaliy Ljamov, Sergey Karinskiy, Vladimir Shevchik, Nikolay Sinitsyn, Yury Zyuryukin, Edgar Semenov, Peter Zilberman, Eric Epstein, Anatoly Morozov, Valery Proklov, Georgy Mansfeld, Sergey Ivanov, Vladimir Anisimkin, Anatoly Kmita, Alexander Medved’, Alexander Bagdasaryan (USSR), Dick White, Cal Quate, John Shaw, Gerry Farnell, Bert Auld, Gordon Kino, Ken Lakin, Don White, Henry Spector, Art Oliner, Pankaj Das, Wen Wang, Clinton Hartmann (USA), Eric Ash, Ted Paige, Jeff Collins, Richard De La Rue (Great Britain), Pierre Tournois, Charles Maerfeld, Eugene Dieulesaint, Philippe Nosier, Gerard Quentin (France), Nobuo Mikoshiba, Kasuo Ioshida, Jun-Ichi Nishizawa, Tetsuo Sasaki, Kimio Shiosaki, Sumio Hamakawa (Japan), Kjell Ingbrigtsen, Helge Engan (Norway),Clemens Ruppel (Germany), etc.. Many of them unfortunately already passed away… I also can name my direct pupils who contributed a lot into development of acoustoelectronics, such as (in arbitrary order) Alexander Bugaev, Gennady Shkerdin, Victor Plessky, Sergey Nikitov, Iosif Kotelyansky, Alexander Kozorezov, Natalia Polzikova and younger colleagues, such as Victor Orlov, Sergey Alexeev, Natalia Naumenko, Iren Kuznetsova, etc.
In the other fields of science in which I worked, I also have many friends-colleagues such as Nikolai Sinitsyn, my co-author in the discovery of strong electron emission from carbon nanotubes or Peter Zilberman, my co-author in the field of magneto-electronics and spintronics, or Vladimir Cherepenin with whom I work now investigating influence of strong pulsed electric fields on various media. Vladimir Cherepenin and Yury Maslennikov are also my close colleagues in the investigations in the field of biomedical radio-electronics.
During my long life in science (about 60 years!) I had more than 80 postgraduate students, majority of whom received PhD and about 25 of them became D. Sci. and professors in Physics. I consider this as one of my main achievements in science.
In 1979 five European scientists E. Ash, J. Collins, Yu. Gulyaev, K. Ingebrigtsen and E. Paige were awarded by the prestigious Europhysics Prize of European Physical Society for the development of physical foundations of Surface Acoustic Wave Devices (see fig.1). In 2006, I received IEEE Rayleigh Award for my works on physics and technology of SAW Devices for information processing. For my works in the field of acoustoelectronics I was awarded by the State Prize of the USSR (twice, in 1974 and 1984) and of Russia (twice, in 1993 and 2006).
What other research directions did you follow?
Another interest at that time was so called spin-wave electronics. The point is that system of atom spins in magnetic materials is in some sense “lighter” than the system of atoms themselves, so spin-wave devices should work at higher frequencies than their acoustic wave analogs, which are based on the motion of heavy atoms. In 1965 I predicted existence of so called “second spin waves” in ferromagnets [61] (analog of “second sound” in liquid helium, predicted by L.D. Landau) – the waves of spin-wave density. I developed the hydrodynamic theory of these waves, which later was confirmed in the works of physicists from Ural school.
Later with P.E. Zilberman, E.M. Epstein, V.P. Plessky, S.A. Nikitov and our coworkers we developed kinetic theory of spin-wave interaction with free electrons in ferrites, layered structures ferrite-semiconductor and in periodic structures at the surface of ferromagnets. On this basis, there could be developed high frequency (and with high Q-factor) filters and delay lines at microwave frequencies. We performed wide investigations of the phenomena connected with spin-oriented currents (this direction is called “spintronics’) [62] [63] [64] and experimentally observed terahertz electromagnetic radiation due to spin injection in ferromagnets. [65] [66] Together with V.P. Plessky and S.A. Nikitov we introduced a new type of metamaterials – “magnonic crystals” – a periodic medium with the period equal to the length of spin wave (analog of known “photonic” and “ phononic” crystals). [67] [68] Now these magnetic metamaterials are widely investigated as new materials for information processing.
The third direction of my scientific work since 1980 was vacuum microelectronics based on the phenomenon of “cold” electrons emission to vacuum from micro tips, made of molybdenum and other materials. These works have been carried out in Saratov division of our Institute which I organized in 1977–79 in accordance with the proposal of academician N.N. Semenov (Nobel Laureate in chemistry, who was born in Saratov) and 1st secretary of communist party of Saratov region V. Gusev, also chemist by education. There were objective reasons for creation of IRE division in Saratov as here was historically excellent classical University with strong radio-electronic department and many high levels industrial enterprises in the field of microwave electronics, some of which were transferred from Moscow and Leningrad during the Second World War. Indeed, Saratov was intellectual center of low Volga region. In 1977, the representative delegation of the Academy of Sciences of the USSR headed by Vice-President of the Academy, director of our institute Academician V.A. Kotel’nikov came to Saratov and as the result Presidium of Academy of Sciences of the USSR decided to create Saratov’s Scientific Center of the Academy of Sciences of the USSR, consisting of several Institutes in different scientific directions – precise mechanics, biology, agriculture and radio-electronics. The organization of the Center was entrusted to me, as I already was closely working with the scientists from Saratov University in the field of acoustoelectronics and microwave acoustics since early 60th.
The Saratov Institute
Yury, IRE had several Institutes in different locations. One was the Saratov Institute.
One of the Institutes of Saratov Centre was the Division of our Institute of Radioengeneering and Electronics Ac.Sci. USSR (SIRE Ac.Sci USSR).
In 1977-1985 I was spending large part of my time in Saratov carrying out both administrative and scientific work. In Saratov’s industrial enterprises there was organized production of microwave acoustic delay lines both on BAW and SAW including dispersive ones on SAW and compression filters on SAW on the technical level, similar to filters made at that time, say, at Thomson CSF. Existing at that time in the World so called “cold war” accelerated the production of those components. In Saratov division of our Institute I organized excellent group of scientists and engineers (educated in Saratov University and in Saratov Polytechnic Institute), who were by their qualification on the best world level. Level of the other Saratov’s Institutes was also very high, not lower than in Moscow or Leningrad. My Deputy head of Saratov Scientific Center Prof. A.F. Rezchikov, who helped me in creation of the Center, headed excellent Institute of Precise Mechanics and Control Systems whose works were very important for the whole country.
At that time, due continuing “cold war”, Saratov Institutes besides agricultural and biological were secret. They could not receive the foreign colleagues, their publications in open journals were sent to print through the Institutes of similar profile in Moscow or Leningrad. For example, our Institute of Radioengineering and Electronics (IRE) had Divisions in Fryazino and Saratov (and later in Ulyanovsk), which by number of scientists were comparable with central Institute in Moscow. But all publications were sent strictly from the Central Institute. Our foreign colleagues were surprised with such outstanding productivity of our scientists!
Saratov in general was closed city for foreigners as during the Second World War to Saratov there were evacuated many military industrial enterprises and some of them didn’t return to previous places. Even touristic ships with foreigners who travelled along Volga river in 60th and 70th didn’t stop in Saratov!
All of this changed with Gorbachev’s “perestroika”, but about it – later.
Carbone Nanotubes
Tell us a little bit about the discovery of carbon nanotubes!
In 1991, there was discovered a new allotropic state of carbon – so called nanotubes. It was further development of known “fullerene” state – ball-like molecules of many C atoms, for example C60. First considerations on topological possibility of existence of carbon nanotubes I’ve heard in 1991 from Prof. Leonid Chernozatonsky, my friend at the Institute of Chemical Physics of RAS, the teacher of my wife Irina Ermolaeva. He called them “tubelenes”. [69] Experimentally these carbon nanotubes were obtained practically simultaneously in 1991 by Iijima [70] in electrical arc discharge and by Chernozatonsky et al [71] by laser sputtering of graphite source. The experimentalist in the team [71] there was Zoya Kosakovskaya, a brilliant scientist and engineer, beautiful and pleasant woman, later from our Institute. I immediately (in 1991) sent her experimental results to Kroto, Nobel Prize Laureate for discovery of fullerenes, and he promised to put it into his survey paper which he was writing for journal “Nature”.
As since 1980 I was involved at Saratov in vacuum microelectronics research I’ve got the idea, that carbon nanotube could be the effective and reliable source of electron emission to vacuum. Indeed, the diameter of nanotube (or the thickness of its wall) is of the size of one atom, so it is very sharp tip. If, due to very strong electric field some atoms of carbon will fly away, the sharpness of the nanotube will not be worse – in difference from used before the molybdenum tips, which after flying away some atoms become blunter. I said this idea to the head of my experimental group in Saratov Division of IRE Prof. Nikolay Sinitsyn- known specialist in microwave electronics in general and microwave microelectronics in particular. He immediately organized the experiment and (O, glory!) indeed obtained very strong electron auto emission from carbon nanotube tips. In April 1993, we submitted our report to the International Conference in Grenoble. [72]
It was the first publication on auto emission of electrons from carbon nanotubes and foundation of a new direction in vacuum microelectronics. Today there are hundreds of publications all over the World on that subject, and many devices already have been done. For example, there are already constructed micro vacuum diode and triode, where distance between cathode (carbon nanotube) and anode is less than mean free path of electron at atmospheric pressure. It means that it doesn’t need to be pumped out! There are made already micro vacuum integrated circuits, which can work under the conditions of very strong radiation or lightning, at high temperatures, etc. – in contrary to usual semiconductor IC. The other advantage is very high working frequency as the electrons there are free and don’t collide with atoms. [73] [74] I continue to work actively in vacuum micro and nanoelectronics, investigating, in particular, possibilities of creation the new types of bright displays.
The research project “extrasenses”
How did you get involved in the “strange” research project “extrasenses”?
In 1977 Acad. Yu. B. Kobzarev outstanding scientist in the field of electrodynamics and statistical radio physics, who was a Head of the Department at our Institute, invited me to visit at home Acad. I.K. Kikoin, one of the creators of Russian atomic bomb. Also, there were invited Acad. A.N. Tikhonov, famous mathematician, the author of “Tikhonov’s regularization method”, Prof. V.B. Braginsky from MSU, outstanding physicist - experimentalist in the field of gravitational waves. Prof. G.D. Mansfeld from my Lab, brilliant experimentalist in the field of acoustoelectronics, and some other people. There was invited a woman from Leningrad Ninel Kulagina with her husband and medical doctor. She was declared to be so called “extrasens”, person, who has some unusual abilities: telepathy, introvision, telekinesis (replacement of objects without touching them) etc.
Here I should say, that at that time (the end of Brezhnev’s “stagnation” period in the USSR, end of 70th – beginning of 80th) that kind of people became very popular, as USSR people didn’t know where to go. The idea of Communism was exhausted but alternative ideology was not suggested. So, various extrasenses, wizards, exorcists, shamans, healers, astrologists, witches were flourishing and scrambling people’s brains. The “super – true” scientists considered all of this just as a rubbish and didn’t want to pay attention on it. But some scientists wanted to go deeper and understand if there is something that it is worth to study (for not to” throw out a child with water from the basin”). That was the goal of the meeting at Acad. Kikoin’s home mentioned above.
Somebody put light objects (pieces of smashed paper, cup of the pen) on the glass over the table and asked Mrs. Kulagina to move them without touching. She tried with big strain and … nothing happened, the objects didn’t move. She said immediately that she is influenced by the children’s eyes from photographs of Kikoin grandchildren under the glass over the table. So, the table glass was covered by newspaper. She repeated the efforts and finally the objects started to move (!), both to her and out of her depending on her hands position. All of us, spectators, were in great shock! Acad. Tikhonov even tried to measure with the ruler the path which the object travelled. It was about 25 cm. We kept our eyes very attentively on her hands and the objects and didn’t notice any threads or the other devices. It seemed that it was not a trick! But what it was? All of us were the scientists and didn’t believe to any miracles! Everybody started to propose explanations of what we have seen.
My idea was that there is some kind of chemical emanation from her hands as she always kept opened palms over the objects as if she was throwing down some substance from her palms on the objects. The motion of the objects more or less followed the movements of her palms, as if there was some interaction between palms and the objects. The other effect which she made was strong etching at the skin of anybody when she touched some area of skin with the palm of her hand. Prof. Braginsky even got noticeable burn of his hand from her touch. During all the experiments medical doctor measured her pulse and blood pressure. It reached by times very high level: 200 heart bits per minute and 270 mm Hg blood pressure. At the end she was completely exhausted. We returned home in deep thoughts what all of it could be. Anyway, I was interested to understand what I’ve seen: is it really some phenomenon or very clever trick? I made some inquiries about Kulagina and learned that some experiments with her already have been done by Acad. Rem Khokhlov, Rector of MSU. Unfortunately Khokhlov at that time already died, but eyewitnesses said that Kulagina could decline and scatter the laser beam! We decided to repeat his experiments. We made from cartoon the vertical tube 10 cm in diameter with 2 pairs of holes along the diameter, one pair over another by 5 cm, and let laser beam to pass through these pairs of holes. At the bottom of this tube we put small piezoelectric transducer (receiver of sound).
We invited Kulagina to come to Moscow again and asked her to move this transducer inside the tube. When Kulagina put her palms over upper opening of the tube and started moving the transducer we saw that laser beams began to tremble and scatter, one after another, and piezo-transducer registered sound flips. It looks like some “clouds” were falling down from her palms with certain velocity, scattered the laser beams and then produced sound flips, registered by the transducer. Knowing distance between laser beams we easily calculated the velocity of ‘clouds” and found that it was approximately equal to velocity of water drops, freely falling down in the atmosphere. So it became more or less clear to us that the picture of the “phenomenon” was the following: she somehow could throw out from her palms the perspiration clouds which have electric charge. These clouds on its way down scatter the laser beams and falling on the transducer produce sound flips. The transducer becomes electrically charged and Kulagina’s palms, which are also charged, could move the object (transducer), not touching it, by usual electromotive force.
It is well known that Human skin (including palms) usually is electrically charged due to friction of our feet upon the floor, ground, etc. Part of this charge Kulagina can throw out with the perspiration to the object, which thus becomes charged. Indeed we noticed that her palms after the experiments were very wet. Thus, so called “ telekinesis” is explained simply by electromotive forces! We even made the device which we called the “ witchescope” for direct measurements of the electric charge which Kulagina was throwing out of her palms. It consisted of 2 metallic plates parallel to each other with the distance between them about 5 cm. These plates were switched into a circuit consisting from the electric battery, ampermeter and voltmeter joined together by wires. In absence of Kulagina the current in the circuit was equal to zero and the voltmeter showed the voltage of the battery. When Kulagina started to throw out the clouds of her charged perspiration (in fact, clouds of some kind of electrolyte) into the space between the plates, there appears a current which is measured by the ampermeter. Knowing the sizes of the plates and current’s value one can easily calculate the amount of electric charge between the plates. It occurred to be quite enough to provide necessary electromotive force for “ telekinesis”.
The question is why she had so abundant perspiration from her palms. May be it is her physiological peculiarity. Everybody knows that some people are sweating more than another. But we even had the idea, that maybe she, before the experiments, rubbed into her palms some chemicals. This could explain the etching by her palms mentioned above: so simple! Anyway, from delicacy we didn’t investigate these experiments in such details. Unfortunately, Mrs. Kulagina soon died and we had no possibility to continue the experiments. We learned that some other people were showing similar type of “telekinesis”, but they rejected to be investigated scientifically. So our experiments with “telekinesis” were completed.
I reported the results of our experiments with Mrs. Kulagina to our Director, Acad. V.A. Kotel’nikov (He also was Vice-President of Ac.Sci. USSR) and, by his advice, to the President of Ac.Sci. USSR, Acad. A.P. Alexandrov and to the Seminar at the Institute for Physical Problems Ac. Sci. USSR. All of them accepted our possible explanation of “telekinesis”. But the question about physiological mechanism of such an abundant charged Human perspiration (even if it is due to artificial rubbing into the palms of some chemicals) was not solved up to the end. However, the positive result of this story for me was the appearance of the interest to study Human physiological functions by radiophysical methods. I should say that so far all the experiments with
Kulagina have been performed unofficially, mainly in my home. But soon there appeared the occasion which helped to transfer our experiments to official laboratory.
At the end of 1980 the Head of the State Committee on Science and Technology (SCST) Acad. G.I. Marchuk invited Acad. Evgeny Velikhov, who was at that period Vice –President of the Ac. Sci. USSR on Physics, and me, as Deputy Director of the Institute, whose activity was connected with the receiving and processing of weak signals during our investigations of Space and Planets by radars and sputniks. For example, our Institute participated in radar investigations of the planet Venus. We made the first map of Venus relief in spite of clouds in its atmosphere always covering the surface of the planet. American scientists performed the similar radar mapping of Venus one year later. I together with American colleagues reported about these achievements through the American CNN Television. Also my experiments with Kulagina were quite known and Acad. Marchuk knew about them. He said to us that the General Secretary of the Communist Party of the Soviet Union Mr. Leonid Brezhnev asked him to clear up the situation with a woman of Assyrian origin named “Djuna”, who performs treatment of several top leaders of the USSR and himself (with positive effect!) using methods not approved by official medicine. Marchuk asked us to organize some investigations of Djuna’s “healing” abilities from the point of view of physics. We agreed to try.
Research in the area of medicine
Later in your career you started to look into medical topics, and use highly sensitive sensors, which were developed for the project “extrasenses”!
I decided to consider more wide problem: to use the possibilities of our Institute for reception and processing of weak signals, coming out from any Human body due to life activity. I had in mind electric and magnetic fields, electromagnetic radiation of various frequencies, brain waves, heart beating, breathing, microwaves, heat (IR radiation), light (“aura”), acoustic radiation and chemical content of the micro-atmosphere around a human body (Fig.2). The idea was that if these signals are measurable and are modulated by life functions then they could be used for noninvasive diagnostics of a Human body.
I organized a new laboratory in the Institute called “ELDIS” (Electronic Diagnostic Systems) and invited to work very good experimental physicist Edward Godik from our Institute and a group of postgraduate and undergraduate PhysTech Students (including both of my sons, Andy and Michael, also PhysTech Students). Together with Godik we worked out the Program of investigations of the physical fields and radiations mentioned above, from any Human. We’ve got some grants from the government to buy necessary equipment and rented a part of a small old house in a quiet street of Moscow (for less electromagnetic noise from the street transport). Finally, in 1981 we created a unique completely computerized measuring complex for precise measurements of electric and magnetic fields (changing in space and time), infrared, microwave, optic and acoustic radiations and for the analysis of the micro-atmosphere around a human. For example, the dynamic IR thermography system gives temperature distribution over the Human skin with the accuracy higher than 0.01o C. The dynamic radio thermography system gives 3D temperature distribution inside a Human body with accuracy higher, than 0.1o C at the depth up to 10 cm. The dynamic system for measuring magnetic fields of muscles, heart and brain, based on SQIDS in combination of the second order gradientometer has sensitivity 10FT/ Hz1/2 within the band up to 100Hz. This measuring complex allowed us to monitor the behavior of various organs of a Human body and the Human as a whole in the norm and with various pathologies.
On that basis there was developed a set of new types of noninvasive medical diagnostics. [75] [76] [77] [78] . Some devices from this complex are produced by the industry and are used in many clinics: IR cameras, magneto- cardiographs, electric impedance mammographs etc. invented by us device against falling asleep of a person fulfilling dangerous work, based on so called “skin-galvanic effect”, [79] is used by the engine-drivers on all railways in Russia.
Finally, I should say that all of these diagnostic devices are completely noninvasive and relatively cheap. For example, electric impedance mammograph gives practically the same knowledge about woman breast pathologies as X-ray mammograph, but it is absolutely harmless and is about 20 times cheaper. I hope that this computerized diagnostic complex will be a part of future preventive individual medicine equipment.
A few words about Djuna who, unfortunately, recently passed away. We have not found any difference of the fields and radiations from her body in comparison with any of us. But she had unusually high sensitivity of her organs of feelings. For example, she felt difference in temperature of two objects 0.20C with her fingertips, while for average person this figure is 0.40C. She had very quick reaction on every word or motion of a person to whom she was speaking or putting questions. Besides of this she was high level specialist in massage and, in our opinion, quite good psychotherapeut. We come to conclusion that all of it plus known effect “placebo” perfectly explains her “healing” abilities.
Yury, I know that you have spent a lot of time for the social activity: in Gorbachev Parliament, for example. Could you tell some words about it?
All the scientific and technical achievements, described above, were mainly obtained in the Soviet Union period, even before Gorbachev’s “Perestroika” (i.e. before 1985). The Soviet Union had quite a militarized economics. Therefore, since Stalin period physics, mathematics, chemistry and technical sciences were in favor as they obviously have direct relation to military power of the country. I wouldn’t say this about biology, genetics and cybernetics which were considered as “bourgeois sciences”, contradicting Marxist-Leninist ideology and they were damped. It was very stupid, as future development have shown that these sciences are no less important even for military power of the state. Many outstanding biologists and geneticists were under repressions, put into jails and executed, as famous biologist and geneticist Acad. Nickolai Vavilov. Even some physicists, chemists and engineers, if they do not strictly follow communist party ideology, were repressed: put into to so called “Sharashkas”, some kind of jails where prisoners were doing science. Some very great physicists and engineers like L.D. Landau, S.P. Korolev, A.N. Tupolev have been in Sharashkas. Great Russian writer A.I. Solzhenitsyn also was working in Sharashka on speech recognition problems. But in the whole the financing and other support of physical, chemical and technical sciences was quite good. On one month’s salary of junior researcher it was possible to buy a suit, shoes, shirts and feed the family. Very important role in this there had the existence of “cold war”.
With Gorbachev’s Perestroika’ everything drastically changed. Of course, there were many positive things: freedom of speech, press publications, appearance of books and movies, which earlier were not possible, free television with criticism with respect to anybody, even Gorbachev and later Yeltsin, and, which is especially important for scientists, freedom to travel to foreign countries and personally communicate with close colleagues. But on the other hand, as USA and Western countries now were not considered as the enemies of the Soviet Union, “cold war” ended (unfortunately, temporarily!), the expenses on military related sciences dropped down very much. By the way, my colleagues from abroad told me about the same situation in USA, England, France, etc. In the Soviet Union many military technical Institutes were closed or tried to transfer to civil production. The difference between the West and the Soviet Union was that if the Western military enterprises always actively participated in civil production, in the Soviet Union it was on much lower scale. As high technology military industries dropped down there were no big need in the academic fundamental science. So on one hand the financing of the academic institutions by itself was reduced and from the other hand, it became very difficult to find contracts with the industry. The situation became even worse after falling down the Soviet Union in the Autumn of 1991. Financing of our Institute of Radioengineering and Electronics, for example, immediately dropped down by 20 times. At that time I was already the Director of the Institute and main task for me was the survival of the Institute.
Coming a little bit back in time, in 1979 I was elected the Corresponding Member of the Academy of Sciences of the USSR. After 5 years in 1984 at the age of 49 years old, I was elected a Full Member (Academician) of Ac. Sc. USSR. In 1987, our Director Academician V.A. Kotel’nikov suggested me to became the Director of the Institute and I was elected to this position. In the situation of those days I decided to find for the high physical and technical potential of the Institute some civil applications. They were: the new methods of medical diagnostics and curing, ecology of our country and the Planet Earth as a whole, fundamental works in low dimension systems electronics and in vacuum microelectronics, material sciences including metamaterials, generation and investigation of super strong pulsed electromagnetic fields and their interaction with the various media, including gold and platinum containing ores and even Human organism, etc.
In the Spring of 1989 I was elected as People’s Deputy (Member of Parliament) to Gorbachev’s Parliament. It was called “The Meeting of People’s Deputies of the USSR”. These elections have been partly from regions of the country and partly from the social organizations. I was elected from the social organization “The Union of
Scientific and Engineering Associations of the USSR” (USEA of the USSR). This organization had a quote of 16 representatives in the Parliament. For the comparison, I can say that the Academy of Sciences of the USSR had comparable number - 25 representatives. Soon after elections to the Parliament I was elected to be the President of the USEA. In the Parliament I was appointed the Chairman of Subcommittee on Telecommunication and Informatics of the Committee of Transport, Telecommunications and Informatics of the Supreme Soviet of the USSR.
In the beginning of my work in the Parliament Mr. Gorbachev asked me to create in the main Hall of the Kremlin Palace (with 6000 seats!) the machine for electronic confidential voting for the delegates. With the help of Phillips Company we did it. So before opening of every Parliament General Session Gorbachev asked me to explain to delegates how to use my machine, as it was very new for everybody.
The first thing that I decided to do at this high position was to create the complex Program of development of the telecommunications systems in the USSR and, in general, informatization of the USSR. At that time in the USSR in average there were only 9 telephones per 100 inhabitants (for comparison, in the African Republic of Zimbabwe there were 13 telephones per 100 peoples and in the USA and England there were about 90 telephones per 100 inhabitants). All of these telephones were stationary with wire connections. Era of cellular phones at that time only just started. The principle of cellular telephone was proposed by Bell Telephone Company in the USA in 1940, and it reminds the principle of estafeta (relay) in sport when one runner passes the stick to the other runner and the team overtakes the distance faster than it would be one sportsman. But it couldn’ t be realized in practice, as for duplex communications the mobile equipment was as big and heavy as at the main station. Only after the invention and development of SAW compact filters and effective solid state compact amplifiers in 80th the cellular phone could be placed into lady’s sac or men’s pocket.
As far as I know the first countries which started to produce and sale cellular stations and mobile telephones were Scandinavian countries (for example, Finnish system NMT-450) and then France with their GSM technology, England, USA and the other countries. In the USSR in 1989 there were no cellular telephones at all and they even were unknown to majority of population. My idea was to work out the Program based on 4 main directions:
- Transition to digital telecommunication systems (at that time we in the USSR had mainly analog systems).
- Wide use of fiber optic communication lines especially for long and principal lines (at that time fiber optic communications in the USSR just started).
- Much wider use of the satellite (sputnik)g communication lines as our country USSR has very big territory and in some parts, is very weakly inhabited.
- Wide use of cellular communications. This was especially important as in the USSR more than half of apartments had no cables for landline phones and using of cellular telephones in spite of their high price would be economically more profitable than to establish wire lines.
I organized the working group of the specialists in telecommunications problems and we worked out this Program taking into account the real situation in various regions of our great country. In 1989-1991 I have published several papers on the various aspects of this Program in the Soviet press and abroad. For example, in 1990 I presented at London Congress on Cellular Telephony the report under the title “Will Cellular Save the Soviet Union?”, in which on real examples I was proving the economical profit of cellular telephony for the USSR. I took participation in the first three Davos Economic Forums where I represented telecommunications part of the USSR delegation. At the end of 1989 I organized the tender between foreign and Soviet companies for installation and production of cellular telephone systems in the USSR. From 11 companies-participants the winner was Finnish company «Nokia» with their system NMT-450. So on 10th of October 1989 in Moscow there was the first ring of cellular phone. Era of cellular communications started in the Soviet Union and later in Russia.
During 3 years (1989-1991) of my work in Gorbachev's Parliament I was deeply involved into routine parliamentary work: meetings, adopting new laws and making corrections to old laws, supporting or not supporting the appointments of Ministers and Directors of the main enterprises in the field of telecommunications and informatics, etc. In this period I almost had no time for research.
But I should admit here that this new type of activity in the Parliament was very interesting and pleasant for me. There were several reasons for that. The first is that due to free elections to Gorbachev's Parliament (may be for the first time in the whole history of Russia, including Tsarist period and Communist Soviet Union) there were elected many outstanding personalities from the intellectual elite of the Country like Academicians: Andrey Sakharov, Vitaly Ginzburg, Zhores Alferov, Evgeny Velikhov, Yury Ryzhov, Yury Ossipian, Igor Gorynin,
Evgeny Primakov, Georgy Arbatov, Nikolai Petrakov, Leonid Abalkin, Professors: Svyatoslav Fedorov (ophthalmologist), Anatoliy Sobchak, Tel’man Gdlyan, Galina Starovoitova (lawyers), Alexander Lebed' ( General); economists Gavriil Popov and Yuri Boldyrev, politicians Boris Yeltsin and Alexander Yakovlev, astronaut-engineers Victor Gorbatko and Rector of Bauman University Prof. Alexey Eliseev, priest Pitirim, etc. With almost all of them I was acquainted personally in various circumstances and had close political views on the desired future of our Country. We all worked for the sake of making the Soviet Union as the democratic country.
One of the first decrees by our Parliament was the abolition from the USSR Constitution, one of the main positions about the leading role of Communist Party in our society. Of course, me and all mentioned above people's deputies voted for this decree! In the Soviet Union General Secretary of the Communist Party was the real head of the state. At that time on this position was Mikhail Gorbachev. In the new situation after acceptance of this decree the structure of high power in Soviet Union was changed and Gorbachev was elected as the first (and the last!) President of the Soviet Union.
Unfortunately, the economic policy of Gorbachev’s government was far from optimal. Governmental counsellors were suggesting one program after another, like the sad memory 500 days Program for getting out from crisis. The industry was not working, ruble was falling down with respect to USA dollar, the shelfs at the shops were empty. At the regions of the USSR there started upraising of the people, firstly in Georgia, then in Baltic Republics, who wanted to go out from the Soviet Union. These attempts were damped by the military force. It dropped down the authority of the Central Government and Gorbachev personally. At that critical moment in August 1991 Gorbachev went for the vacations to the Black sea resort and there occurred the coup-d’ état in Moscow, headed by the conservative part of Gorbachev’s governing elite. They formed governing organ SCCS (State Committee on Critical Situation), in Russian “G.K.Ch.P.” and claimed the necessity to save the previous Soviet Union with not too much of so called “Western democracy”.
At that time in Russian Federation, which is the biggest part of the Soviet Union, there was already its own leader, Boris Yeltsin, with his Russian Parliament. As Moscow is inside the Russian Federation, so Yeltsin formally had the rights to command by the Russian military troops there. On 19th August 1991 SCCS Head, Vice-President of Gorbachev’s Parliament Gennady Yanaev gave order to Defense Minister of the USSR General Yazov to move the troops including groups of tanks from the Moscow suburbs to Moscow White House, where Yeltsin’s Parliament was sitting. But Yeltsin called to Yazov and convinced him to give the order to tanks group officers not to shoot to anybody. So General Lebed’, the commander of tanks group rejected to shoot to the White House. At that time, the Moscovites, who already felt the wind of freedom, made the barricades around the White House for defense of Yeltsin’s Parliament and government. Finally, everything ended without a single tank shot, but unfortunately, 3 young boys died under armored infantry carrier, trying to stop it. This was unforgettable nights and days from 19th up to 21th August. My wife Irina and me were visiting the White House to join the defenders of Yeltsin’s democracy. and we all had been very happy with Yeltsin’s victory.
Next morning Yeltsin gave his famous speech from the tank tower promising to the country the freedom and flourishment. In one of the next days Gorbachev came back to Moscow after his vacations and found completely different country. He already did not have any real power. All members of SCCS were arrested and put to jail. After some time of coexistence of the Soviet Union with Gorbachev as the formal Head, the President, and New Russia with President Yeltsin as real power in Russia, in October 1991 the three Heads of Russia, Ukraine and Byelorussia at Byelorussian resort signed the agreement of decomposition of the USSR into a group of independent States with the boundaries between them as they were at that moment. These three Heads, Yeltsin, Kravchuk, and Shushkevich suggested to the Heads of the other Republics of the Soviet Union to join the agreement and all of them did it with pleasure. The Soviet Union was already doomed. With the Soviet Union it’ s Parliament stopped to exist. So my active political life came to the end.
When Yeltsin came to power in New Russia in 1991, you were only 56 years old. What have you been doing after coming back to academic activity?
I came back to my work in the Academy of Sciences as Director of our Institute. My Program of Informatization of the Soviet Union, described above, in the main part concerning Russian Federation (Russia) was accepted by new (Yeltsin’s) Parliament and is now practically realized in Russia. Today for 145 mio.
population of Russia there are more than 200 mio. of cellular phones! All the other directions of the Program also are developing on average international level.
In the Academy of Sciences itself there happened some significant changes at that time. I will tell about it in more detail.
In the Soviet Union, there were existed several Academies: the Ac.Sci. USSR, which was mainly consisted of the members living on the territory of the Russian Federation with a few members from the other USSR Republics, and a bit low level Academies in Republics Ukraine, Byelorussia, Kazakhstan, Georgia, etc.
After August 1991 events all the Republics became the independent States. Therefore, their Academies of Sciences became the National Academies. In Russian Federation there was no Academy of Sciences as the Ac.Sci. USSR was always unofficially considered as Russian Academy of Sciences. In Russia there existed (even in tsarist period) the group of scientists who were in opposition to the Academy because they were not elected to the Academy by various reasons, mainly due to their not very high level as scientists. Now these people, using the situation, came to Boris Yeltsin and reminded him that in the other Republics there exist Academies of Sciences, but in Russia there is no one. So, they said, let us create a new Academy of Sciences in Russia. In this case, Ac.Sci. USSR should be demolished as reminder of hated Soviet Union. Yeltsin agreed and gave them 150 vacancies for election of members of new Academy. We in Ac.Sci. USSR were just shocked with this President's decision and started to fight against it. Our foreign colleagues, for example from the USA National Academy, Royal Society, Max Plank Institute etc., have written the letters of support to Ac. Sci. USSR.
However, our opponents made crucial mistake. They proposed as the President of new Russian Academy of Sciences Academician of the Ac. Sci. USSR Yury Osipov, mathematician from Ekaterinburg, the native city of President Yeltsin. Academician Yury Osipov, outstanding scientist, was, of course, against demolition of Ac. Sci. USSR, as all of us, and at the same time he was acquainted with Boris Yeltsin from the period, when he was the 1st Secretary of the Communist Party of the Ekaterinburg region. On November 21, 1991, a group of academicians of Ac. Sci. USSR have met with Yeltsin at the airport Vnukovo, when he was going to fly abroad and was in a good humor. They reminded him about the great merits of the Ac. Sci. USSR in the main achievements of USSR during the latest years such as atomic project, rockets, space flights and investigations, etc., in which the Ac. Sci. USSR had outstanding role. They pointed out that Ac. Sci. USSR in fact was almost 99% Russian Academy of Sciences and proposed him just only to change the name of the Ac. Sci. USSR to “ Russian Academy of Sciences” (RAS), as the Academy was called between 1724-1925.
Yeltsin found their arguments reasonable, suggested to use those 150 vacancies for elections of new deserving members and signed proposed text as a decree. So since the 21th November 1991 our Academy of Sciences is called the Russian Academy of Sciences (RAS).
In December 1991 Yury Osipov was elected as the President of the New Old Russian Academy of Sciences. I was elected as the Member of the Presidium (governing body) of the Russian Academy of Sciences and was appointed as responsible person for the relations between the Academy and the Ministry on Telecommunications and Informatics of Russia. So again I had a lot of administrative work, but also much more time for research.
My main interests there were the investigations in the field of carbon nanotubes electron emission devices, spintronics and biomedical radio-electronics, as I already described earlier. Also, I was interested to study the influence of strong pulsed electric field on various media, in particular on gold and platinum containing ores. [80] [81]
Economics of Russia after “shock therapy” of 1992-1993 showed some increase, but after default in 1998 dropped down again. All that time the financing of the Academy Institutes was low, although some growth took place. Our opponents outside of the Academy were not quiet. The point is that the Academy of Sciences of the USSR had a lot of high level property: good buildings in the central parts of Moscow, Leningrad, Ekaterinburg, Novosibirsk, etc., advanced expensive equipment, special hospitals and resorts, etc. All of these belongings were not yet privatized. For many organizations, including our opponents, this Academy’s property was very desirable piece.
So in June 2013 we suddenly learned that there is prepared a project of law about liquidation of Russian Academy of Sciences and transferring of all academic institutes (about 550) to some new State institution called Federal Agency of Scientific Organizations (FASO),( in Russian FANO). Nobody new (and nobody knows now!) who was the author of this law. President of RAS Acad. Vladimir Fortov was informed about this project just several hours before the Meeting of the Government, the member of which he was. Of course, he and some members of the Government objected, but it was too late. The project with some small corrections was submitted
to Duma (Russian Parliament) for consideration and adopting. At the next day, all the World knew about this event: “Russian Academy of Sciences, one of the best scientific Centre in the World, created by Peter the Great about 300 years ago is going to be liquidated! This is a great shock for all World science!” That was the reaction of Russian and International Scientific Community. There was a big meeting (several thousand peoples) in front of the building of the Presidium RAS at Leninskiy Prospect in Moscow and extraordinary Meeting of the Presidium RAS itself, similar meetings in Leningrad (which was renamed back as Saint Petersburg), in Ekaterinburg, in Novosibirsk, etc. As the result, the final decision on that project by Duma was postponed until the Autumn. During all the summer, there were a lot of meetings, publications in Press, TV programs, Internet publications, etc. I personally wrote a big open letter to the President of Russia Vladimir Putin (he inherited Yeltsin in 2000) in which I presented to him many considerations against adoption of this law. This letter was placed at the Academy’s website for a month or longer period. Many outstanding scientists wrote analogous letters to Putin, to the Government, to Duma, etc. Foreign Academic people from USA National Academy of Science, Royal Society, Max Plank Institute, etc. also supported Russian Academy of Sciences.
Of course, such a pressure had some effect, but it was not able to change intended decision. On 18th September 2013 (at my Birthday!) the project was approved by the State Duma and became the law. In accordance with this law Russian Academy of Sciences was not liquidated (as it was planned!) but it was reorganized like Academic society (to certain aspect similar to NAS USA, Royal Society, etc.) The Institutes were taken off from the Academy and economically submitted to FASO, so budget financing of the Institutes was made through FASO. The Role of RAS was to determine directions of research in the Institutes and to provide expertize of all scientific and technical projects in the country. But it is known that “who pays for the girl, he is dancing with her”. So up to now this principle of “two keys” is not working properly. Apparently, it takes time to establish this new system.
In new structure RAS –FASO on the position of the Director of the Institute can be elected persons only below 65 years old. In July 2014 my last 5 years term as the Director of IRE RAS ended and I was retired from the Director position (I was Director of the Institute for 27 years). I was elected as the Scientific Supervisor of the IRE RAS. So, I have now only scientific duties, consisting of supervising the research directions in the Institute. Of course, as usual, I’m doing my personal work as physicist- theoretician in the field of Solid State Physics. So my scientific career continues.
What about your social activity?
In the Soviet Union there existed the Union of Scientific and Engineering Associations of the USSR (USEA USSR). It was successor of the Russian Technical Society, founded in 1866. After decomposition of the Soviet Union USEA of the USSR was transformed to the Union of Scientific and Engineering Associations of the countries from which USSR was consisted. It was called the International Union of Scientific and Engineering Associations (IUSEA). One of the members of IUSEA was RUSEA- Russian Union of Scientific and Engineering Associations. So I was elected in 1991 as the President of both IUSEA and RUSEA. In fact, they are the Unions of Engineers of both - previous USSR and Russia. There is quite a big amount of social work. IUSEA is a member of International Engineering organization WFEO (World Federation of Engineering Organizations). RUSEA is a Member of European Engineering Organization FEANI. The aim of IUSEA and RUSEA is to join in all aspects to the World engineering organizations in education, standards of engineers, reeducation of engineers in connection with scientific and technical tendencies, etc. We in Russia organize competition for the best engineer of Russia with Prizes and Diplomas, competition for All Russian Prize to young engineers “The Hope of Russia”, do some work to improve the conditions of work of engineers, help international contacts of Russian engineers, organizing of the International Conferences, etc. In the frames of RUSEA I am also the President of A.S. Popov Scientific and Engineering Society for Radioengineering, Electronics and Telecommunications, which is Russian analog of IEEE.
On international level I am the President of Russian division of URSI (International Radio Science Union), and Past President of the Russian section of IEEE (I organized this section in 1988 and was its President until 2016). So in spite of my age 81 years I am working hard and, in general, with big pleasure.
Some words about my family. My wife, Ermolaeva Irina Vasilievna, PhD, State Prize of Russia Laureate in Physics, now retired. My elder son, Andrey, born in 1959, is an electrical engineer, he works at Moscow’s
Division of Swedish firm “Scania”. My junior son, Michael, born in 1966, also is an electrical engineer, now in business, he is the owner of not big firm, which deals with computerization of aluminium industry. As I already mentioned, I have two brothers, both electrical engineers and both retired. I also have one granddaughter and two grandsons.
In conclusion, I would like to express my sincere gratitude to my colleagues and friends Victor Plessky and Clemens Ruppel for their initiative, insistence and hard work with this Interview.
- ↑ Yu.V. Gulyaev, FTT, 1959, 1, 422
- ↑ V.L. Bonch-Bruevich, Yu.V. Gulyaev, FTT, 1960, 2, 465
- ↑ Yu.V. Gulyaev, FTT, 1962, 4, 1285
- ↑ 4.0 4.1 S.F. Edwards, Yu.V. Gulyaev, Proc. Roy.SocA., 1964, 279, 229
- ↑ S.F. Edwards, Yu.V. Gulyaev, Proc. Roy.SocA., 1964, 279, 229
- ↑ S.F. Edwards, Yu.V. Gulyaev, Proc. Phys.Soc, 1964, 83, 495
- ↑ A.R. Hudson, J.H. McFee, D.L. White, Phys.Rev.Lett., 1961, 7, 237
- ↑ K.B. Tolpygo, Z.F. Uritsky, JETP, 1956, 30, 929
- ↑ G. Weinreich, Phys.Rev., 1956, 104, 321
- ↑ 10.0 10.1 10.2 Yu.V. Gulyaev, V.I. Pustovoit, JETP, 1964, 47, 2251
- ↑ C.H. Walter, Traveling Wave Antennas (in Russian, 1970)
- ↑ K. Yoshida, M. Yamanishi, Jap.J.Appl.Phys., 1968, 7, 1143
- ↑ J.H. Collins, K.M. Lakin, C.F. Quate, H.J. Shaw, Appl. Phys.Lett., 1968, 13, 314
- ↑ Yu.V. Gulyaev at al., FTT (Sov.Phys.- Solid State), 1970, 12, 2595
- ↑ Yu.V. Gulyaev, P.E. Zilberman, FTT, 1965, 7, 2772
- ↑ K. Yamanouchi, K. Shibayama, Proc. 6th Int. Congress on Acoustics, Tokyo, Japan, 1968, p. H-117.
- ↑ R.H. Tancrell, M.B. Schultz, H.H. Barrett, L. Davies, M.G. Holland, IEEE Proc., 1969, 57, issue 6
- ↑ P. Hartemann, E. Dieulesaint, Electr.Lett., 1969, 5, 219
- ↑ A. Kovalev and I. Yakovkin, R&E,1971, 16, 321
- ↑ R.H. Tancrell, and M.G. Holland, Proc. IEEE, 1971, 59, 393
- ↑ 21.0 21.1 Yu.V. Gulyaev, A.M.Kmita, A.S. Bagdasarian, JTP Lett.,1979, 5, 11, 697-701; Patents of 1977: USSR № 726648, USA №4162415, №4185218; GB №2003353; Japan №1069686; France №7821723; Germany №2831584, №283158
- ↑ D.C. Malocha, B.J. Hunsinger, IEEE Trans, Sonics, Ultrasonics, 1977, SU-24, 293
- ↑ E.A. Ash, Proc. IEEE, GMTT, 1970, 385
- ↑ E.A. Ash, Proc. IEEE Symp MTT, 1967
- ↑ F.G. Marshall and E.G.S. Paige, Electr Lett, 1971, 7, 460
- ↑ M. Luukkala and G.S. Kino, Appl. Phys.Lett, 1971, 18, 393
- ↑ K. Ingebrigtsen, J.Appl.Phys., 1969, 40, 2681
- ↑ E.M. Epstein, Yu.V. Gulyaev, FTT (Soviet Physics- Solid State), 1967, 9, 376
- ↑ Yu.V. Gulyaev, E.M. Epstein, JETP Lett6, 1966, 3, 410
- ↑ 30.0 30.1 Yu.V. Gulyaev, FTT, 1966, 8, 3366
- ↑ A.S. Bugaev, Yu.V. Gulyaev, G.N. Shkerdin, FTT, 1970, 12, 2054
- ↑ Yu.V. Gulyaev, E.M. Epstein, FTT, 1967, 9, 864
- ↑ Yu.V. Gulyaev, FTT, 1967, 9, 431
- ↑ Yu.G. Bachinin, Yu.V. Gulyaev, JETP, 1971, 60, 1036; FTT, 1971, 13, 829
- ↑ 35.0 35.1 Yu.V. Gulyaev et all, FTT, 1970, 12, 2595
- ↑ 36.0 36.1 A.M. Kmita, A.V. Medved’, JETP Letters, 1971, 14, 455
- ↑ Yu.V. Gulyaev, Phys. Lett, 1969, 30A, 260; 1969, IEEE Trans on Sonics and Ultrasonics,1970, SU-17, 111
- ↑ Yu.V. Gulyaev, G.N. Shkerdin, Radiotechnika and Electronika (R& E), 1974, 19, 3288; JETP, 1979, 77, pp.1396-1406
- ↑ B.A. Auld et al., Electron Lett, 1976, 2, 650
- ↑ Yu.V. Gulyaev, V.P. Plessky, FTP Lett, 1977, 3, 220
- ↑ A. Korolyuk, N. Roy, FTT, 1972, 14, 260
- ↑ 42.0 42.1 42.2 Yu,V, Gulyaev, JETP Lett, 1969, 9, 63
- ↑ 43.0 43.1 J.L. Bleustein, Appl Phys Lett, 1968, 13, 412
- ↑ C. Maerfeld, F. Gires, P. Tournois, Appl Phys Lett, 1970, 18, 269
- ↑ A.I. Morozov, M.A. Zemlyanitsyn, FTP Lett, 1970, 12, 396
- ↑ C. Maerfeld, P. Tournois, Appl Phys Lett, 1971
- ↑ S. Biryukov, Yu. Gulyaev, V. Krylov, V. Plessky, Surface acoustic waves in inhomogeneous media. Springer Science & Business Media, 2012, 20
- ↑ Yu.V. Gulyaev, IEEE Trans Ultrason.Ferroelectr. Freq. Control, 1998, 45, 935
- ↑ K. Hashimoto, Surface acoustic wave devices in telecommunications, Berlin, Springer, 2000
- ↑ D. Morgan, Surface Acoustic Wave Fields, Amsterdam, Elsevier, 2007
- ↑ D. Morgan, IEEE Int Freq Control Symp., May 1988
- ↑ O. Balysheva, V. Grigorievsky, Yu. Gulyaev, V. Dmitriev, G. Mansfeld, under edit. of Yu. Gulyaev, Moscow, “Radiotekhnika”, 2012, pp.576 (in Russian)
- ↑ V.I. Anisimkin, et al., Electron Lett, 1988, 34, 1360
- ↑ I.V. Anisimkin, V.I. Anisimkin, Yu.V. Gulyaev, 2000, Proc. Of IEEE, Int. Symp. Ultrasonics,1, p.713
- ↑ I.V. Anisimkin, IEEE, Intrn Symp Ultrasonic, 2003, 2, 1326
- ↑ Yu.V. Gulyaev, Patent USSR, 1971, #401271,
- ↑ Yu.V. Gulyaev, G.D. Mansfeld, G.A. Orlova, Electr. Lett., 1981, 17, 12
- ↑ Yu.V. Gulyaev, Patent USSR, Nov. 1971
- ↑ A. Siegert, Patent Osterreich, Dec 1971
- ↑ Yu.V. Gulyaev and F.S. Hickernell, Acoustoelectronics: History, Modern State and New Ideas for a New Era”, IEEE Ultrasonics Symp., 2004, 1, 182-190
- ↑ Yu.V. Gulyaev, JETP Lett, 2, 3, 1965
- ↑ Yu.V. Gulyaev, P.E. Zilbermann, R&E, 23, 898, 1978
- ↑ R.J. Eliott, E.M. Epstein, Yu.V. Gulyaev, P.E. Zilbermann, J. of Magnetism and Magnetization, 271, 83, 2004
- ↑ Yu, V. Gulyaev, P.E. Zilbermann, A.I. Panas, E.M. Epstein, UFN (Soviet Physics - Uspekhi), 179, 359, 2009
- ↑ Yu, V. Gulyaev, P.E. Zilbermann, I.V. Malikov, F.M. Mikhailov, A.I.Panas, S.G. Chigarev, E.M. Epstein, JETP Lett, 93, 289, 2011
- ↑ Yu, V. Gulyaev, P.E. Zilbermann, I.V. Malikov, F.M. Mikhailov, S.G. Chigarev, E.M. Epstein, R&E, 57, 372, 2012
- ↑ Yu.V. Gulyaev, S.A. Nikitov, V.P. Plessky, FTT, 1981, 23, 1231;
- ↑ Yu.V. Gulyaev, S.A. Nikitov, Sov. Phys- Doklady, 2001, 380, 469
- ↑ L.A. Chernozatonsky, 1991, Private Comm.; Physics Lett, 1992, A166, 55.
- ↑ S. Iijima, Nature, 1991, 354, 56
- ↑ 71.0 71.1 Z. Ya. Kozakovskaya, L.A. Chernozatonsky, E.A. Fedorov, JETP Lett, 1992, 56, 26
- ↑ Yu. V. Gulyaev, L.A. Chernozatontsev, Z. Ya. Kozakovskaya, N.I. Sinitsyn, G.V. Torgashev, Yu. F. Zakharchenko, Revus “Le Vide les Conches Minces”, Supplement N271-Mars-Apr 1994 (Submitted in 1993)
- ↑ Yu.V. Gulyaev, et al., J. of Vacuum Sci and Tech, B, 13, Mar-Apr, 1996
- ↑ Yu. V. Gulyaev, Vestnik RAS, 2003, 73, 389
- ↑ Yu. V. Gulyaev, E.E. Godik, Vestnik Acad. Sci. USSR, Ser. Phys, 1983, 8, 118
- ↑ E.E. Godik, Yu.V. Gulyaev, IEEE Engineering in Medicine and Biology, 1991, 10, 21
- ↑ Yu.V. Gulyaev, A.G. Markov, L.G. Koreneva, P.V. Zakharov, Dynamical infrared thermography in Humans, IEEE, Engineering in Medicine and Biology Magazine, 1995, 14 (6), pp.766-771
- ↑ V.A. Cherepenin, Yu.V. Gulyaev, A.V. Korzhenevsky, S.A. Sapetsky, T.S. Tuykin, Physiological Measurements 2012, 33, 849
- ↑ R.F. Musin, V.A. Morozov, E.E. Godik, Yu.V. Gulyaev, Biophysics, 1985, 30, 309
- ↑ V.A.Chanturia, Yu.V. Gulyaev, V.D .Lunin, I.Zh. Bunin, V.A. Cherepenin, DAN, 1999, 366 ,680.
- ↑ V.A. Vdovin, Yu.V. Gulyaev, V.A. Chanturia, V.A. Cherepenin, R&E, 2005, 50 (9), 1129
- Computing and electronics
- Engineering fundamentals
- Fields, waves & electromagnetics
Prestigious cancer research institute has retracted 7 studies amid controversy over errors

Seven studies from researchers at the prestigious Dana-Farber Cancer Institute have been retracted over the last two months after a scientist blogger alleged that images used in them had been manipulated or duplicated.
The retractions are the latest development in a monthslong controversy around research at the Boston-based institute, which is a teaching affiliate of Harvard Medical School.
The issue came to light after Sholto David, a microbiologist and volunteer science sleuth based in Wales, published a scathing post on his blog in January, alleging errors and manipulations of images across dozens of papers produced primarily by Dana-Farber researchers . The institute acknowledged errors and subsequently announced that it had requested six studies to be retracted and asked for corrections in 31 more papers. Dana-Farber also said, however, that a review process for errors had been underway before David’s post.
Now, at least one more study has been retracted than Dana-Farber initially indicated, and David said he has discovered an additional 30 studies from authors affiliated with the institute that he believes contain errors or image manipulations and therefore deserve scrutiny.
The episode has imperiled the reputation of a major cancer research institute and raised questions about one high-profile researcher there, Kenneth Anderson, who is a senior author on six of the seven retracted studies.
Anderson is a professor of medicine at Harvard Medical School and the director of the Jerome Lipper Multiple Myeloma Center at Dana-Farber. He did not respond to multiple emails or voicemails requesting comment.
The retractions and new allegations add to a larger, ongoing debate in science about how to protect scientific integrity and reduce the incentives that could lead to misconduct or unintentional mistakes in research.
The Dana-Farber Cancer Institute has moved relatively swiftly to seek retractions and corrections.
“Dana-Farber is deeply committed to a culture of accountability and integrity, and as an academic research and clinical care organization we also prioritize transparency,” Dr. Barrett Rollins, the institute’s integrity research officer, said in a statement. “However, we are bound by federal regulations that apply to all academic medical centers funded by the National Institutes of Health among other federal agencies. Therefore, we cannot share details of internal review processes and will not comment on personnel issues.”
The retracted studies were originally published in two journals: One in the Journal of Immunology and six in Cancer Research. Six of the seven focused on multiple myeloma, a form of cancer that develops in plasma cells. Retraction notices indicate that Anderson agreed to the retractions of the papers he authored.
Elisabeth Bik, a microbiologist and longtime image sleuth, reviewed several of the papers’ retraction statements and scientific images for NBC News and said the errors were serious.
“The ones I’m looking at all have duplicated elements in the photos, where the photo itself has been manipulated,” she said, adding that these elements were “signs of misconduct.”
Dr. John Chute, who directs the division of hematology and cellular therapy at Cedars-Sinai Medical Center and has contributed to studies about multiple myeloma, said the papers were produced by pioneers in the field, including Anderson.
“These are people I admire and respect,” he said. “Those were all high-impact papers, meaning they’re highly read and highly cited. By definition, they have had a broad impact on the field.”
Chute said he did not know the authors personally but had followed their work for a long time.
“Those investigators are some of the leading people in the field of myeloma research and they have paved the way in terms of understanding our biology of the disease,” he said. “The papers they publish lead to all kinds of additional work in that direction. People follow those leads and industry pays attention to that stuff and drug development follows.”
The retractions offer additional evidence for what some science sleuths have been saying for years: The more you look for errors or image manipulation, the more you might find, even at the top levels of science.
Scientific images in papers are typically used to present evidence of an experiment’s results. Commonly, they show cells or mice; other types of images show key findings like western blots — a laboratory method that identifies proteins — or bands of separated DNA molecules in gels.
Science sleuths sometimes examine these images for irregular patterns that could indicate errors, duplications or manipulations. Some artificial intelligence companies are training computers to spot these kinds of problems, as well.
Duplicated images could be a sign of sloppy lab work or data practices. Manipulated images — in which a researcher has modified an image heavily with photo editing tools — could indicate that images have been exaggerated, enhanced or altered in an unethical way that could change how other scientists interpret a study’s findings or scientific meaning.
Top scientists at big research institutions often run sprawling laboratories with lots of junior scientists. Critics of science research and publishing systems allege that a lack of opportunities for young scientists, limited oversight and pressure to publish splashy papers that can advance careers could incentivize misconduct.
These critics, along with many science sleuths, allege that errors or sloppiness are too common , that research organizations and authors often ignore concerns when they’re identified, and that the path from complaint to correction is sluggish.
“When you look at the amount of retractions and poor peer review in research today, the question is, what has happened to the quality standards we used to think existed in research?” said Nick Steneck, an emeritus professor at the University of Michigan and an expert on science integrity.
David told NBC News that he had shared some, but not all, of his concerns about additional image issues with Dana-Farber. He added that he had not identified any problems in four of the seven studies that have been retracted.
“It’s good they’ve picked up stuff that wasn’t in the list,” he said.
NBC News requested an updated tally of retractions and corrections, but Ellen Berlin, a spokeswoman for Dana-Farber, declined to provide a new list. She said that the numbers could shift and that the institute did not have control over the form, format or timing of corrections.
“Any tally we give you today might be different tomorrow and will likely be different a week from now or a month from now,” Berlin said. “The point of sharing numbers with the public weeks ago was to make clear to the public that Dana-Farber had taken swift and decisive action with regard to the articles for which a Dana-Farber faculty member was primary author.”
She added that Dana-Farber was encouraging journals to correct the scientific record as promptly as possible.
Bik said it was unusual to see a highly regarded U.S. institution have multiple papers retracted.
“I don’t think I’ve seen many of those,” she said. “In this case, there was a lot of public attention to it and it seems like they’re responding very quickly. It’s unusual, but how it should be.”
Evan Bush is a science reporter for NBC News. He can be reached at [email protected].
The Scientific Research Institute of the Russian Customs Academy
Nadezhda Lipatova
Director of the Institute
NADEZHDA LIPATOVA,
Leading Researcher of the Russian Customs Academy, Candidate of Technical Sciences, Senior Researcher (Associate Professor)
140009, Lyubertsy, Moscow Region
Komsomolskij prospect, 4
Tel.: +7(495) 500-13-90
E-mail: [email protected]
General information
The Research Institute of the Russian Customs Academy was established in 2014. The Institute is a structural unit of the Russian Customs Academy, carrying out scientific and research activities within the framework of the statutory activities of the Academy.
The main activities of the institute are:
- implementation of fundamental, searchable, applied, research and developmental works on customs activity issues;
- participation in scientific and technical programs, competitions, grants and other forms of scientific research conducted by ministries and departments in order to carry out accreditation indicators for the Academy;
- preparation of scientific papers: monographs, articles, reports, textbooks and other types of scientific works;
- formation of issues of the journal «Bulletin of the Russian Customs Academy», – a peer-reviewed scientific periodical edition on economic and legal sciences;
- preparation of information and analytical materials for the leadership of the Academy, for meetings and Boards of the Federal Customs Service of Russia, for the Academy website, for the media.
History reference
Term of Reference
Institute page
Information about the Heads of a Research institute
Additional information
Subdivisions of the Research Institute:
Department of Scientific and Information Research in Customs
Head of Department: Tamara Mikhailenko,
Doctor of Philology, Professor.
Tel .: 8 (495) 500-13-01
Scientific editors of the magazine “Herald of the Russian Customs Academy”
E-mail: [email protected]
Department of Economic and Legal Studies in Customs
Head of Department: Vladimir Novikov,
Doctor of Economics, professor.
Tel .: +7 (498) 602-39-64
Department of the Study of Problems in the Theory and Practice of Customs Control, Trade Nomenclature, Expertise and Trade Restrictions
Head of Department: Kozhuhanov Nikolai
Ph.D., associate professor
Tel. : +7 (498) 602-39-10
E-mail: [email protected]
Department of the Study of Customs Problems of the Development of Eurasian Integration
Head of department: Gladkov Andrey
Tel.: +7 (498) 602-39-62
E-mail: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Australas Med J
- v.5(8); 2012
Doctors and Medical Science
Are practicing medical doctors up to date on the latest advances in their field? Is published research valid and reliable? Why are doctors seldom involved in research? The aim of this editorial is to explore some of these complex issues.
Prescribing habits and therapeutic advance
Patients may believe that their doctor is a source of impartial and up to date information in his or her field but how do doctors keep up to date? Gabbayay and Le May reported the following:
‘…clinicians rarely accessed, appraised, and used explicit evidence directly from research or other formal sources; rare exceptions were where they might consult such sources after dealing with a case that had particularly challenged them. Instead, they relied on what we have called “mindlines,” collectively reinforced, internalised tacit guidelines, which were informed by brief reading, but mainly by their interactions with each other…opinion leaders, patients…pharmaceutical representatives and by other sources of largely tacit knowledge that built on their early training and their own and their colleagues' experience’ . 1
Are doctors who prescribe the latest drugs more likely to be up to date? General practitioners for example have been found to be reactive and opportunistic recipients of new drug information, and rarely report undertaking an active information search. The decision to initiate a new drug is heavily influenced by advertising, endorsement by colleagues and hospital consultants. 2 Furthermore new medications offer little, if any, incremental value over existing therapies. The combination of inadequate information about the potential side effects of new drugs plus their limited value strongly argues against their early use except in exceptional circumstances. 3
It is telling that drug companies are spending billions every year promoting their products. 4 It is also notable that many new drugs are withdrawn within a very short time of their launch. 5 Worryingly, there is sometimes a relative lack of urgency when a drug is clearly shown to be harming patients. For example 19.8 million patients were prescribed five questionable drugs before action was taken to remove them from the market. This included painkillers, anti-histamines, drugs used to treat obesity and anti-hypertensive drugs. Not one of these were lifesaving nor, in many cases, were they the only drugs available for that indication.In another case physicians prescribed a new painkiller to 2.5 million patients with acute pain, even though many well-tested similar drugs were available and the drug was known to elevate liver enzymes. Similarly the rationale for not withdrawing an anti-histamine from the market as soon as researchers clearly identified it as causing deaths has not been explained. 6 It is surprising that the drug was not removed from the market when the adverse effects were identified, but only after the manufacturer had developed a new product to substitute for it.
For some relatively rare conditions practicing doctors may know little more than they knew when they first qualified. 7 Physicians who have been in practice for a long time may be at greatest risk of being out of date in their recommendations and practice. Therefore, this group of physicians may need support to be kept abreast of research. 8 Older physicians also seem less likely to adopt newly proven therapies and may be less receptive to new standards of care. 9 - 10 So what is the role of so-called peer reviewed publication?
Publication and medical science
It is estimated that there are 1.29 papers published in the peer reviewed medical literature every minute. 11 Even if a doctor were able to keep up with this volume of reading, it is said that much of what is published is flawed. Richard Smith, former editor of the British Medical Journal (BMJ), is quoted as saying that only 5% of published papers reached minimum standards of scientific soundness and clinical relevance, and in most journals the figure was less than 1%. 12
In the period from 2000–2010 a total of 788 papers have been retracted, i.e. expunged from the public record. 13 Approximately three-quarters of these papers had been withdrawn because of a serious error; the rest of the retractions were attributed to fraud (data fabrication or falsification). The fakes were more likely to appear in leading publications with a high “impact factor”. The impact factor is a proxy measure of how often research is cited in other peer reviewed journals. More than half (53%) of the faked research papers had been written by a first author who was a “repeat offender”. This was the case in only one in five (18%) of the erroneous papers. 13 At about the same time it was estimated that the number of articles published between 1950 and 2004 that ought to be retracted should have been as many as 100,000 and at least 10,000. 14 The authors further conclude that although high impact journals tend to have fewer undetected flawed articles than their lower-impact peers, even the most vigilant journals potentially host papers that should be retracted. 14
Retraction or not, one would like to think that doctors are able to spot flawed papers and, better still, are unlikely to have their clinical practice misled by poor science or glossy leaflets for new and untested treatments. Let us start with the first question: do doctors read research papers? Here is a quote from a doctor writing in the BMJ:
‘The volume of statistical argument [in research papers] also seems part of the same disingenuous process. How many doctors have a clue what it means? Of all the areas of mathematics, probability, and its inscrutable daughter statistics, are the most slippery to grasp. Yet authors routinely drop large chunks of this extremely difficult stuff into papers that are supposed to be there to illuminate practice for doctors. But most doctors, including myself, don’t understand it’. 15
What is the point of publishing research papers that cannot be absorbed by the target audience? One author suggested a possible answer:
‘Authors are eager to get their names in print not because they are bursting to tell us something but for more solemn reasons. Another paper means another line on a curriculum vitae, another step towards a job or a research grant.’ 16
Publishers and medical science
Journals rely on ‘peers’ to decide which papers merit publication and which should be jettisoned. The process of peer review is recognised to be flawed. 17 The quality of the reviews varies. There may be divergent views expressed in the review and it is sometimes difficult to determine why an editor rejects or indeed accepts a submission without concluding that the editor’s biases have played a significant role in that decision. In many cases, especially in niche areas a competitor who may or may not declare a conflict of interest may be invited to review the paper. If the identity of the reviewer is kept from the authors, the reviewer is free to recommend rejection or publication without fear of recrimination in what is known as “blind” peer review. In very specialised topics the identity of authors can be very hard to conceal from an expert in the field at the time of review. Secondly publishing is a powerful, prestigious and lucrative business. No journal yet has taken up a long-standing suggestion to remove the names of authors from published papers. This would ensure that papers are published only for the sake of disseminating information. However to do so would be to make the journal much less attractive to authors and therefore advertisers and other cash cows. 18
To fully appreciate the value of journal articles to their target audience, namely university researchers, and their host institutions one might consider the value of a paper in a highly-rated journal (impact factor >40) compared to one in a more modestly rated one (impact factor <2). A paper in the high impact journal may have an Eigenfactor score of 0.67. The Eigenfactor score calculation is based on the number of times articles from the journal published in the past five years have been cited in the year. 19 A paper published in a ‘lesser’ journal has a Eigenfactor score of 0.003. Naturally a university dean would be impressed with work cited frequently rather than seldom. But what is even more likely is that the academic with the paper in a so-called high impact journal will be more likely to be successful on grant applications and be invited to speak at national and international conferences. All of which may attract postgraduate students, competitive grants and lucrative collaborations. In Australia, for example, universities who employ academics who publish on a predetermined list of journals are more likely to be rewarded with a larger share of government grants and subsidies. 20
That is not to say that publication in the high impact journals means living happily ever after. The reputation of a top rated medical journal was damaged by a controversy involving its response to problems with research on a drug used to treat pain. 21 A study was published in the journal in 2000 which noted an increase in myocardial infarction amongst those using the drug. 21 Concerns about the robustness of that study were raised with the journal in August 2001. At the same time both the US Food and Drug Administration and another major journal also cast doubt on the interpretation of the data that had been published in the journal. However it was not until 2005 that the journal published concern about the original study. During that five-year period funded reprints of the original article were used to promote the offending drug.
Publishing and profit
Most journals are peer reviewed by an unpaid army of academics and editors. The journals may then be sold to libraries. An annual subscription to some journals may be over $20,000. Publishers make substantial profits. Here is a list of published subscription rates for various top-rated journals:
A major publisher of medical journals is a global company based in Amsterdam, employing more than 7,000 people in 24 countries. It claims a global community of 7,000 journal editors, 70,000 editorial board members, 300,000 reviewers and 600,000 authors. In July 2010 the company posted interim profit results with a revenue of almost 3 billion GBP and adjusted profits of 758 million GBP in the six months ending 30 June. 22 This is also the company that was reported to have been paid an undisclosed sum by a pharmaceutical company to produce several volumes of a publication that had the look of a peer-reviewed medical journal, but contained only reprinted or summarised articles, most of which presented data favourable to its products with no disclosure of company sponsorship. 23
Doctors and research
Despite the fact that doctors are key to delivering health care they are seldom involved in research and far less often cited as leaders on research teams. The relationship between the research organisations and doctors is the key to understanding their limited involvement in innovation. ‘Good’ research is a painstaking science in which clearly defined research questions are articulated, appropriate methods are applied, data is efficiently collected and appropriate analysis is conducted to craft conclusions that take into account the limitations and strengths of the study. Seldom, if ever, does a single study, no matter how large, offer robust conclusions that will lead to change in practice. The design and execution of high quality research requires expertise which takes many years of further training and experience. The acquisition of these skills may take doctors out of clinics and at a significant personal opportunity cost.
The subject of clinical research, i.e. patients, must give informed consent before they can be included in a study. This is more complicated than working with uncomplaining rats in a sanitised laboratory. In practice limited control over research subjects means that most clinical research cannot be generalised and is therefore less likely to be published in high impact journals. Most research is also conducted at universities, directly or indirectly. Universities and medical schools have to generate a surplus income to grow in size and influence. Very little research in primary care or public health has a commercial value, therefore to profit from clinical research universities rely on government funding. The government agenda may be driven by political imperative. Therefore a government minister unveiling shiny new machines makes for a far more voter friendly photo opportunity than one launching a more efficient way to rehabilitate people with mental illness or manage incontinence in general practice.
Therefore funding is heavily weighted towards biomedical sciences. Here the focus is on cure rather than prevention or more efficient service delivery. Genetic research, nano particles and the study of prions, is therefore more likely to get generously funded than research on system design that would allow people to die in comfort in their own homes.
In 2010 the Australian National Health and Medical Research Council divided its research funding so that 39% of the funds were awarded to preventive medicine and public health. At the same time the majority of government funding on health care in practice is on so-called primary care services. 24 For universities the return on investment does not favour clinical research, so that laboratory-based research on a cure for cancer makes a far more compelling case than research involving therapists in the community or models of disease self-management. And yet, in the scheme of things, research in how to deliver an equitable health service is going to make more of an impression on the community in the short term than research on a cure for cancer that may be 20 years away.
Academics understand that universities are financially rewarded for adopting this paradigm by a system that is driven by priorities related to a return on investment. Given the competitive nature of those who enrol in medical school this is a considerable disincentive and drives clinicians out of research. As if that was not sufficient disincentive, there are major challenges to recruiting participants in clinical practice. 25 Patients do not seek help from doctors only to spend most of their consultation negotiating an opportunity to participate in research that may or may not benefit them directly. When the patient is paying for the doctor’s time, as is the case in many countries, doctors have no incentive to introduce distractions to that consultation. In reality many of the patients in clinical practice are excluded from research designs which usually favour young, articulate, English speaking, literate, relatively healthy people and not those living with the conditions for whom the evidence has apparently been generated. 26
Doctors are not generally actively involved in research, they may not critically appraise research articles and their knowledge of recent advances in their field may be out of date. For example there are cases of doctors continuing to prescribe drugs that have been reported to cause harm. A vast number of research papers are published every year and most of these have significant limitations and some poor science may even be published in the most influential journals. Publishers and manufacturers of pharmaceuticals have sometimes colluded in ways that do not necessarily benefit patients. The need for specialist research skills as well as research funding structures mean that those most closely involved with patients neither lead research nor participate in research projects. Much of the most generously funded research is aimed at long-term commercial goals rather than to benefit patients.
PEER REVIEW
Not commissioned. Externally peer reviewed.
CONFLICTS OF INTEREST
The author is the editor in chief of the AMJ
Please cite this paper as: Jiwa M. Doctors and Medical Science AMJ 2012, 5, 8, 462-467. http//dx. doi.org/10.4066/AMJ. 2012.1491

IMAGES
VIDEO
COMMENTS
The New England Journal of Medicine (NEJM) is a weekly general medical journal that publishes new medical research and review articles, and editorial opinion on a wide variety of topics of ...
Study Provides Insight Into ME/CFS. 22,600. 22,224. Stroke Risk After COVID-19 Bivalent Vaccination in US Older Adults. Explore the latest in medicine including the JNC8 blood pressure guideline, sepsis and ARDS definitions, autism science, cancer screening guidelines, and.
WRITING PROMPTS: 1. Summarise what the paper is about in two to three sentences: Example: "This is an interview study of 53 people living with metastatic cancer about their perspective on physicians' use of the computer during follow-up visits. The findings are similar to other studies the authors cite (basically, most patients don't seem to mind when doctors are using the computer).
Writing a medical research paper is similar to writing other research papers in that you want to use reliable sources, write in a clear and organized style, and offer a strong argument for all conclusions you present. ... With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award ...
Your success in getting published shouldn't start with a complete paper. It should start right when you conceptualize your research. Edward Livingston, MD, deputy editor of clinical content for the Journal of the American Medical Association (JAMA), said it all begins with asking the right questions."Re-examine what's in front of you," Dr. Livingston told physicians in training at a ...
Methods. Thirteen semi-structured interviews of English-speaking medical doctors of any specialty were conducted. Recruitment was achieved through the authors' network; contacting authors of relevant research papers; and Bond University's General Practitioner recruitment program.
A clinician should continuously strive to increase knowledge by reviewing and critiquing papers, thoughtfully considering how to integrate new data into practice. This is the essence of evidence-based medicine (EBM).[1] When new clinical queries arise, one should seek answers in the published literature. The ability to read a scientific or medical manuscript remains vitally important ...
High impact medical journal. Champion of better research, clinical practice & healthcare policy since 1840. For GPs, hospital doctors, educators, policymakers.
Overall, the associative algorithm performs on par with the average doctor, achieving a mean accuracy across all trails of 72.52 ± 2.97% vs 71.4 ± 3.01% for doctors. The algorithm scores higher ...
The main goal of this article is to identify the main dimensions of a model proposal for increasing the potential of big data research in Healthcare for medical doctors' (MDs') learning, which appears as a major issue in continuous medical education and learning. The paper employs a systematic literature review of main scientific databases (PubMed and Google Scholar), using the VOSviewer ...
preclinical medical research, and they attributed these problems in large part to poor training of researchers and poor quality of research reporting [4]. Several other lead-ers in medical science have also discussed the extent and gravity of irreproducible preclinical research [5-8]. Clinical research also has its own laundry list of problems.
Every clinician is responsible for evaluating their own practice, and to do that in a robust and meaningful way you need to use the tools of research. We all need to be able to critically review research done by others. For example, the guidelines used in everyday clinical practice are based on meta-analyses and systematic reviews.
To make finding, starting, and publishing high-quality research articles a little bit easier and a lot more enjoyable, check out my five tips for publishing clinical research in medical school. 1. Build your network to find publication opportunities in medical school. When looking for projects, finding great mentors is often more useful than ...
Participating in research gives students great skills and opportunities. Anna Taylor and Sarah Purdy explain how to get started ### This article contains: Students often go into medicine because of a desire to help others and improve patients' physical and mental wellbeing. In the early years of medical school, however, it can seem as if you are not making much difference to patient care.
Getting started with medical research? What future doctors must know. Oct 18, 2022 . 3 MIN READ. By. Brendan Murphy , Senior News Writer. Print Page. For medical students and residents, conducting research offers an opportunity to make a major impact. Getting started, however, can be one of the more daunting aspects of pursuing a research project.
The teaching role of physicians is a core competency in the new Dutch Medical Training Framework: "Physicians contribute as academics to the application, spread, translation and proliferation of knowledge in practice through lifelong learning, training others, evaluating evidence and contributing to scientific research" [].Every physician must be able to "create a safe learning ...
Abstract. Effective doctor-patient communication is a central clinical function in building a therapeutic doctor-patient relationship, which is the heart and art of medicine. This is important in the delivery of high-quality health care. Much patient dissatisfaction and many complaints are due to breakdown in the doctor-patient relationship.
Academia.edu is a platform for academics to share research papers. Lyubertsy Study on Mortality Rate in Patients After Cerebral Stroke or Transient Ischemic Attack (LIS-2). Design and Medical Treatment Estimation
First, we find no impact of debt relief on credit access, utilization, and financial distress on average. Second, we estimate that debt relief causes a moderate but statistically significant reduction in payment of existing medical bills. Third, we find no effect of medical debt relief on mental health on average, with detrimental effects for ...
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020. Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19.
Last modified on Wed 10 Apr 2024 01.00 EDT. The head of the world's largest review into children's care has said that gender medicine is "built on shaky foundations". Dr Hilary Cass, the ...
Medical research is of high value to clinicians and society. In modern-day practice, the continued growth of knowledge has added richness to the medical world and challenges medical professionals to stay afloat. ... They were also more likely to publish their completed research papers or present their abstracts at conferences (n = 7/12, 58% ...
Yury Gulyaev was born on 18 September 1935 in Tomilino, a suburb of Moscow near the satellite town of Lyubertsy. He graduated from Moscow Institute of Physics and Technology, MIPT (1958), and was awarded Ph.D. (1962) and D.Sci. (1970) Degrees. He is a Professor and Head Chair of Solid State Electronics, Radiophysics and Applied Information ...
Dr. John Chute, who directs the division of hematology and cellular therapy at Cedars-Sinai Medical Center and has contributed to studies about multiple myeloma, said the papers were produced by ...
Doctor of Philology, Professor. Tel .: 8 (495) 500-13-01. Scientific editors of the magazine "Herald of the Russian Customs Academy" E-mail: [email protected]. Term of Reference. Department of Economic and Legal Studies in Customs. Head of Department: Vladimir Novikov, Doctor of Economics, professor. Tel .: +7 (498) 602-39-64
Artificial intelligence (AI) is a powerful and disruptive area of computer science, with the potential to fundamentally transform the practice of medicine and the delivery of healthcare. In this review article, we outline recent breakthroughs in the application of AI in healthcare, describe a roadmap to building effective, reliable and safe AI ...
The aquifer in coal limestone is a backup source of water supply in Moscow. The horizon lies at a depth of 20-50 m and is separated from the aquifer in Quaternary sediments (upper, shallow) Jurassic clay. There are areas - hydrogeological windows, on which as a result of erosion activity, clay is absent or their thickness decreases to 1-2 m or permeability increases. Since 2013, monitoring of ...
Publishers and medical science. Journals rely on 'peers' to decide which papers merit publication and which should be jettisoned. The process of peer review is recognised to be flawed. 17 The quality of the reviews varies. There may be divergent views expressed in the review and it is sometimes difficult to determine why an editor rejects or indeed accepts a submission without concluding ...