Nursing Workload and Patient Safety Essay
Introduction, nurses are not overworked, nurses are overworked, both views are right or wrong.
The United States faces an increased demand for nursing professionals in hospitals and other health care facilities. On the other hand, the number of nurses graduating into the profession is not increasing in the same rate as their demand. As a result, hospitals and other health institutions have to increase the working times of the present nurses. It is now common for nurses to work extensively on overtime just to match the demand for their services. The issue causes nurses to suffer fatigue, which compromises their patient care ability. I strongly disagree with the above claim that nurses are overworked.
Nurses face various situations in the hospital that require them to make rational choices instantly. They receive training on how to deal with emergencies as well as normal health conditions. Thus, the claim of overworking nurses is false. Many people go into the nursing profession due to their passions to assist people and not for the money. Therefore, they are motivated to assist as many patients as possible.
Previously, the government trained very few nurses. However, nurse shortages prompted for a reversal of that policy (Chang, et al., 2005). The nursing selection and training is vigorous enough to eliminate any person not keen on the professional demands of nursing. Everyone who becomes a nurse knows that the job requires his or her commitment at all times. Although they enjoy day offs, leaves and normal working hours, nurses know that they should be on call always. The nature of emergencies does no give nurses the luxury of avoiding overtimes at work.
There are different aspects of nursing, apart from general nursing, which require additional skills and proficiency. These specialization demand extra commitments on the part of the nurse during training (Carayon & Gurses, 2008). Given that the specialized nurses attract a higher pay than general nurses do, the professions attract many applicants. People who have a calling on helping people would like to do so with a high pay. The high number of applicants forces institutions to use a rigorous selection process. The process ensures that only the best and most prepared for the profession eventually turn to be nurses. The demanding process prepares all nurses for what will later come when they are in the job.
Complaints saying that nurses are overworked point to their negligence at work as an effect. Some say that nurses are uncaring. People expect nurses to share emotional connections with their patients. The reality is that nurses handle many cases in a day and they cannot afford to attach themselves. This does not imply that they are uncaring. It also does not mean that they are overworked.
Just like with any other profession, nurses are free to seek medical attention when they are not feeling good. They suffer from the effects of the economy like everyone else. Some face difficulties in some areas of their lives. Different personal conditional affecting nurses cause them to deviate from properly doing their jobs. As far as the nursing job goes, its demands do not exceed the capabilities of the people who serve as nurses. Some nurses do a terrible job, and complain of being overworked. Some hospitals face budget cuts and are understaffed. However, such cases are minute and their solutions appear immediately people raise complaints. These few cases do not represent the entire situation for nurses. Nurses work normally and receive compensation whenever they do overtime. Therefore, there is no issue of overworking.
On the other hand, nurses might actually be overworked. The characteristics of bad nurses offer signs of being overwhelmed (Chang, et al., 2005). Some nurses appear to neglect basis procedures and hygiene requirements (Rauhala, et al., 2007). For example, they have hanging hair, wear dirty shoes and smoke in or around hospitals. Patients complain that nurses neglect them. Nurses have many cases to attend. They prefer to deal with the straightforward cases and leave the complicated cases for later. Unfortunately, there is no later for nurses; patients keep streaming into hospitals. Therefore, the neglected patients are a sign of nurse work overload. Some people go into the profession to earn money. If you are motivated to earn more, then work becomes too much as long as your pay does not match your expectations. A high number of dropouts from nursing degrees indicate that the process is arduous. If the training process is that difficult, then what people are training for will demand much more than the training.
Based on the above arguments for both sides, the two positions could all be right. We can say that nurses are not overworked and at the same time say that nurses are overworked. The first part is a disagreement with the claim that nurses are overworked. This part shows that money is not the main attractiveness of the nursing profession. Therefore, it is wrong to equate the amount earn with the time put to work, and then use that to claim a work overload. The argument rightfully shows that the rigorous training for nurses equips them for the demands of their jobs. Since they are well equipped to handle the situations arising in hospitals, nurses should not claim to be overworked.
The second part of the argument could also be right. It points to the signs of negligence, which may point to a work overload situation. Yes, when nurses are seeing too many patients in a day, they will prefer to work with the easy cases. Eventually this will present a pile of neglected complicated cases. During their breaks, nurses become hostile to patients, which are an indication that they are facing many demands from work (Fitzpatrick, 2006). They would not like more work demands creeping into their personal time.
Again, assuming another perspective, both arguments for and against nurse’s work overload could be wrong. Rigorous training does not necessarily prepare a person for the emergencies that appear in actual nurse work. The training mindset is different from the working mindset. Secondly, the calling to help other people has its limits. When the demand of work is overwhelming, people would demand more compensation even if they like their jobs. Similarly, claiming that the signs of negligence are indications of work overload is wrong. There are different parameters within and outside the nursing career that influence a nurse to neglect their primary work duties (Carayon & Gurses, 2008).
Overall, the issue of work overload is not important. At any time, there would be mismatches in the number of staff and patients. It is the duty of management to balance the two variables. However, as explained above, each side of the argument has a valid case point. The issue of nurse work overload depends on the perspective that one chooses.
Carayon, P., & Gurses, A. P. (2008). Nursing workload and patient safety – A human factors engineering perspective. In H. R. G (Ed.), Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: Agency for Healthcase Research and Quality.
Chang, E. M., Hancock, K. M., Johnson, A., Daly, J., & Jackson, D. (2005). Role stress in nurses: Review of related factors and strategies for moving forward. Nursing & Health Sciences, 7 (1), 57-65.
Fitzpatrick, J. J. (Ed.). (2006). Encyclopedia of Nursing Research. New York, NY: Springer Publishing Company.
Rauhala, A., Mika, K., Lisabeth, F., Marko, E., Mariana, V., Jussi, V., et al. (2007). What degree of work overload is likely to cause increased sickness absenteeism among nurses? Evidence from the RAFAELA patient classification system. Journal of Advanced Nursing, 57 (3), 286-295.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2022, April 28). Nursing Workload and Patient Safety. https://ivypanda.com/essays/nursing-workload-and-patient-safety/
"Nursing Workload and Patient Safety." IvyPanda , 28 Apr. 2022, ivypanda.com/essays/nursing-workload-and-patient-safety/.
IvyPanda . (2022) 'Nursing Workload and Patient Safety'. 28 April.
IvyPanda . 2022. "Nursing Workload and Patient Safety." April 28, 2022. https://ivypanda.com/essays/nursing-workload-and-patient-safety/.
1. IvyPanda . "Nursing Workload and Patient Safety." April 28, 2022. https://ivypanda.com/essays/nursing-workload-and-patient-safety/.
Bibliography
IvyPanda . "Nursing Workload and Patient Safety." April 28, 2022. https://ivypanda.com/essays/nursing-workload-and-patient-safety/.
- Are Australian Employees Overworked?
- The Role of Nurses and the Pressures They Face on a Daily Basis
- A Nursing Shortage Article by Marc et al.
- Iron Overload Diagnosing and Treating
- Emergency Medical Care and Nursing Overwork
- Solution to Overwhelming Amount of Work in College
- Organizational Structure in Business
- Vincent Valley Southview Clinic's Analysis
- Creating Environments for Excellence in Nursing
- Health Policy in the US Analysis
- Identifying Nursing Values and Realms of Caring
- Trends in Nursing, Leadership Styles, Career Plans
- The Responsibility of Professional Nurses
- Human Dignity in Nursing
- “The Evolution of the New Environmental Metaparadigms of Nursing” by Kleffel

Nursing workload: a concept analysis
Affiliation.
- 1 Hahn School of Nursing and Health Science, University of San Diego, San Diego, CA, USA.
- PMID: 26749124
- DOI: 10.1111/jonm.12354
Aim: The aim of the present study was to develop a comprehensive understanding of the concept 'workload' within the nursing profession in order to arrive at a clear definition of nursing workload based on the evidence in existing literature.
Background: Nursing workload is a common term used in the health literature, but often without specification of its exact meaning. Concept clarification is needed to delineate the meaning of the term 'nursing workload'.
Method: A concept analysis was conducted using Walker and Avant's method to clarify the defining attributes of nursing workload. As the subject matter was nursing focused, only one database was searched, the Cumulative Index for Nursing and Allied Health Literature (CINAHL). Articles that did not use 'workload' in the title or abstract were excluded. A model case, contrary case, related case and empirical referents were constructed to clarify the concept and to demonstrate how the workload is captured by the main attributes.
Results: The attributes of nursing workload found in the literature fall into five main categories: the amount of nursing time; the level of nursing competency; the weight of direct patient care; the amount of physical exertion; and complexity of care. The attributes were organised according to the leading antecedents, which were identified as the patient, nurse and health institution.
Implications for nursing management: Nurse managers need to address the workload issues with regard to the real nature of nursing work; this could increase nurses' productivity, nurses' satisfaction, turnover, work stress and provide sufficient staffing to patient care needs.
Conclusion: The concept analysis demonstrated clearly the complexity of the concept and its implications for practice and research. It is believed that the current concept analysis will help to provide a better understanding of nursing workload and contribute towards the standardisation of the nursing workload and the development of a valid and reliable measurement system.
Keywords: acuity; competency; complexity of care; intensity; nursing workload; staffing.
© 2016 John Wiley & Sons Ltd.
Publication types
- Attitude of Health Personnel
- Concept Formation*
- Workload / standards*
- Open access
- Published: 07 July 2023
The association between workload and quality of work life of nurses taking care of patients with COVID-19
- Hassan Babamohamadi 1 , 2 ,
- Hossein Davari 1 , 2 ,
- Abbas-Ali Safari 3 ,
- Seifollah Alaei 1 , 2 &
- Sajjad Rahimi Pordanjani 4 , 5
BMC Nursing volume 22 , Article number: 234 ( 2023 ) Cite this article
5272 Accesses
6 Citations
1 Altmetric
Metrics details
The COVID-19 epidemic has brought significant changes and complexities to nurses’ working conditions. Given the crucial role of health workers, particularly nurses, in providing healthcare services, it is essential to determine the nurses’ workload, and its association with the quality of work life (QWL) during COVID-19 epidemic, and to explain the factors predicting their QWL.
A total of 250 nurses, who provided care for patients with COVID-19 in Imam Hossein Hospital of Shahrud, and met the inclusion criteria, were considered the samples in the present cross-sectional study in 2021–2022. Data were collected using the demographic questionnaire, NASA Task Load Index (TLX), and Walton’s QWL questionnaire, which were analyzed using SPSS26 and based on descriptive and inferential statistical tests. A p-value less than 0.05 was considered significant for all cases.
The nurses’ mean scores of workload and QWL were 71.43 ± 14.15 and 88.26 ± 19.5, respectively. Pearson’s correlation test indicated a significant inverse relationship between workload and QWL ( r=-0.308, p < 0.001 ). The subscales with the highest perceived workload scores were physical demand and mental demand (14.82 ± 8.27; 14.36 ± 7.43), respectively, and the subscale with the lowest workload was overall performance (6.63 ± 6.31). The subscales with the highest scores for QWL were safety and health in working conditions and opportunity to use and develop human capabilities (15.46 ± 4.11; 14.52 ± 3.84), respectively. The subscales with the lowest scores were adequate and fair compensation, work and total living space (7.46 ± 2.38; 6.52 ± 2.47), respectively. The number of children (β = 4.61, p = 0.004), work experience (β= -0.54, p = 0.019), effort (β = 0.37, p = 0.033) and total workload (β= -0.44, p = 0.000) explained 13% of the variance of nurses’ QWL.
Conclusions
The study’s findings showed that a higher workload score is associated with nurses’ lower perception of QWL. In order to improve the QWL of nurses, reducing the physical and mental demands of their workload and strengthening overall performance is necessary. Additionally, when promoting QWL, adequate and fair compensation and the work and living space should be considered. The researchers suggest that hospital managers should make more significant efforts to develop and promote the QWL of nurses. To achieve this goal, organizations can pay attention to other influential factors, primarily by increasing organizational support.
Peer Review reports
Nurses comprise the most significant healthcare and treatment systems workforce, serving as the care team’s backbone [ 1 ]. The World Health Organization (WHO) states that there are approximately 27 million nurses worldwide, accounting for 50% of all health workers, and projects that this number will increase by 9 million by 2030 [ 2 ]. Nurses are responsible for most care and treatment measures and often must take on additional tasks beyond their primary roles [ 3 , 4 ]. Numerous studies have documented the high workload experienced by nurses [ 5 , 6 ]. Furthermore, nurses face various stressors, including unhealthy work environments, continuous fatigue, challenging workplace relationships, occupational hazards, and demanding workloads that can negatively impact their professional performance [ 7 ]. Over the past few decades, research has highlighted the stressful and demanding nature of nursing, characterized by its specialization, complexity, and the need to manage emergencies [ 8 ]. Considering the interconnectedness between caregivers and care, it is essential to prioritize the quality of care and the satisfaction of the care providers [ 9 ].
Nurses are one of the most crucial pillars of healthcare organizations in various situations, including the COVID-19 pandemic [ 10 ]. Although the severity of COVID-19 is gradually decreasing, nurses have been providing care to patients in various sectors of hospitals, including emergency departments, intensive care units, and wards, for nearly three years. One study has even suggested that 80% of the workload related to patient care and treatment in hospitals falls on the shoulders of nurses [ 11 ]. Workload refers to the total work done by an individual or team within a specific period. Although the workload is a concept that refers to the number of primary tasks assigned, it can threaten the physical and psychological safety of nurses and reduce job satisfaction while increasing job burnout [ 12 ]. Trait anxiety, psychological health, and social isolation are the primary factors affecting Turkish nurses’ quality of life during the COVID-19 pandemic [ 13 ]. Therefore, paying close attention to the factors influencing nurses’ performance and workplace, especially in critical situations, is crucial.
There are many consequences and preoccupations brought about by COVID-19, such as the severity of the disease, its unpredictability, and the lack of knowledge about the timing of the disease’s outbreak [ 14 ]. Fear and anxiety about possible infection with COVID-19 are destructive, as they can cause stress and psychological abnormalities in individuals [ 15 ]. The nature of this disease increases severe stress reactions, such as fatigue, anxiety, and depression in nurses [ 16 ]. A study indicated that among healthcare workers, nurses experienced higher anxiety about infection with COVID-19 for themselves and their families [ 9 ]. Evidence and data indicate that nursing care for COVID-19 patients is challenging and exhausting, and a high volume of services and work shift restrictions make nurses exhausted. Nurses participating in a study mentioned that patients’ higher care needs and fewer nursing personnel increased the nurses’ workload and fatigue [ 17 ]. The COVID-19 epidemic and changes in work status have significantly impacted nurses’ lives personally and professionally. In today’s interconnected world, the integration of personal and work life has resulted in work life overshadowing personal life, leading to the emergence of the quality of work life (QWL) [ 18 ]. QWL refers to the satisfaction of workers with their personal and work-related needs within their job roles [ 19 ]. Unlike in the past, where the focus was primarily on personal life, improving work life has now become a crucial social issue worldwide, with organizations and employees striving to achieve this goal [ 20 ].
QWL encompasses workplace processes, strategies, and conditions that contribute to employees’ overall job satisfaction, which, in turn, relies on favorable work conditions and organizational efficiency [ 21 ]. In order to enhance and optimize organizational efficiency, prioritizing employees’ capabilities, physical and mental health, and performance is essential [ 22 ]. The QWL and practical job performance have been recognized as critical success factors for any organization, including healthcare institutions like hospitals since 1973 [ 23 ].
By serving as an index, QWL offers valuable insights to managers regarding employees’ primary concerns, fostering a sense of ownership, self-management, security, and responsibility, thereby increasing employee productivity [ 24 ]. QWL has a direct relationship with job satisfaction but an inverse relationship with job turnover [ 25 ]. Therefore, QWL is essential in improving organizational commitment among healthcare workers [ 26 ], nurses’ performance, and care performance and outcomes [ 4 ].
Health managers, especially hospital managers, must take appropriate measures to make necessary changes in the model and contents of academic education in response to experiences related to recent events or other care conditions, such as natural crises [ 27 ], as well as management considerations. Undoubtedly, evaluating the workload and QWL of nurses is essential, despite the effective measures taken by health managers, particularly hospital managers, to recruit a new workforce, balance nurse workload, and provide suitable facilities and incentives.
The present study aimed to answer the question, “What is the relationship between the workload and the QWL of nurses providing care for patients with diseases?” Given the heterogeneous findings about workload [ 28 ] and the nurses’ QWL before the COVID-19 pandemic [ 29 ], the present study was thus conducted to determine: (1) the relationship between workload and the QWL of nurses caring for COVID-19 patients admitted to Imam Hossein Hospital, affiliated with Shahrud University of Medical Sciences, and (2) to elucidate the factors predicting their QWL.
Design, setting, and participants
The present cross-sectional study was conducted from October 10, 2021, to January 15, 2022. The city of Shahrud has three hospitals, two of which are affiliated with the university of medical sciences. Among these three hospitals, only one, Imam Hossein Hospital, serves as the designated referral center for COVID-19 patients. It has dedicated emergency units, infectious disease wards, and ICUs for their admission. In the sample, we included 250 nurses caring for COVID-19 patients admitted to Imam Hossein Hospital of Shahrud. We applied the inclusion and exclusion criteria using census sampling to select all nurses for the study.
The inclusion criteria were having at least three months of work experience caring for COVID-19 patients and expressing willingness and consent to participate in the study. We considered returning incomplete questionnaires and unwillingness to participate in research as the exclusion criteria.
Ethical considerations
Data collection began after the hospital management approved the project and obtained ethical approval (Approval: IR.SEMUMS.REC.1400.282). During the rest time of these nurses in a work shifts, the researcher explained the research objective to them and assured them that the research findings would be used only for research purposes and would be anonymous and confidential. The participating nurses completed informed consent forms to participate in the study and returned the questionnaires afterward.
Instruments and data collection
We collected data using the researcher-made demographic information questionnaire, which included questions about age, gender, marital status, clinical work experience, work shifts, and work experience in the COVID-19 unit. The NASA Task Load Index (TLX) questionnaire and Walton’s Quality of Work Life (QWL) questionnaire were employed.
The NASA Task Load Index questionnaire consists of two sections. The first section classifies the total activity workload into six subscales: Mental demand, Physical demand, Temporal demand, Overall performance, Effort, and Frustration. Each subscale ranks on a 100-point scale with 5-point steps. Individuals establish personal weights based on their perceived importance through pairwise comparisons. They then multiply these weights by the scale score of each dimension, divide them by 15, and obtain a workload score ranging from 0 to 100, representing the total workload index. Mean scores below 50 are acceptable, while scores above 50 indicate a high workload [ 30 ]. The reliability coefficient of the NASA-TLX scale has been reported as 0.746 using the test-retest method [ 31 ]. Additionally, the questionnaire’s reliability was confirmed among 30 nurses, yielding a Cronbach’s alpha of 0.847 [ 32 ]. In this study, we confirmed the reliability of the NASA-TLX through a pilot study involving ten nurses, resulting in a Cronbach’s alpha of 0.89.
Walton’s QWL questionnaire (1973) encompasses components such as Adequate and fair compensations, Safety and health in working conditions, Work and total living space, Constitutionalism in the organization of work, Career opportunities and job security, Opportunity to use and develop human capabilities, Social relevance of work life, and Social integration in the organization [ 33 ]. The questionnaire includes 35 closed-ended questions, categorized on a 5-point Likert scale. The total score of each field and all questions determines the QWL index, which ranges from a minimum of 35 to a maximum of 175. Higher scores indicate better QWL. Previous studies among Iranian hospital workers and nurses have investigated the reliability and validity of this tool, confirming its validity and reporting a reliability of 0.94 using the Cronbach’s alpha test [ 34 ]. In our pilot study involving ten nurses, we confirmed the reliability of the QWL questionnaire, which yielded a Cronbach’s alpha of 0.80.
Data analysis
We performed statistical analysis using SPSS-26 software at a significance level of 0.05. We used descriptive and inferential statistics to analyze the data. We described, classified, and compared the research data using relative and absolute frequency tables. Before analyzing the data, we used the Kolmogorov-Smirnov test to determine the normal distribution. We analyzed the collected data using an independent t-test, Pearson’s correlation coefficient, and one-way analysis of variance (ANOVA). Additionally, we utilized backward multiple linear regression analysis to examine the prediction role of workload subscales and demographic characteristics in nurses’ QWL during the COVID-19 pandemic.
Demographic characteristics of the participants
The nurses’ mean age was 32.92 years, 73.6% were females, and 69.6% were married. The nurses’ mean work experience was 8.75 years, and 15 months were related to working in COVID-19 care units. Furthermore, 92% of nurses were working in rotational shifts (Table 1 ).
The mean score of workload, Walton’s quality of work life, and their subscales
Based on the results, the participants’ mean workload and QWL were 71.43 ± 14.15 and 88.26 ± 19.50, respectively. The maximum perceived workload belonged to physical demand (14.82 ± 8.27) and mental demand (14.36 ± 7.43), and the minimum workload belonged to overall performance (6.63 ± 6.31). The maximum score of QWL subscales belonged to safety and health in working conditions (15.46 ± 4.11), and the minimum score was related to the work and total living space (6.52 ± 2.47) (Table 2 ).
Relationship between workload, the quality of work life, and demographic variables in nurses
The study of the relationship between workload and its subscales with demographic variables indicated that workload had a positive and significant correlation only with age (` r = 0.140, p = 0.027). Even though there was no difference between the workload of single and married nurses, there was a negative and significant relationship between marital status and mental demand ( r =-0.126, p = 0.046). Furthermore, there was a significant positive relationship between the number of children and temporal demand ( r = 0.155, p = 0.014). There was no statistically significant relationship between work experience and workload ( r = 0.096, p = 0.129) and no significant relationship between workload and work experience in the COVID-19 department ( r = 0.036, p = 0.568). However, a statistically significant relationship existed between work experience and temporal demand ( r = 0.179, p = 0.004).
The study of the relationship between QWL and its subscales with demographic variables indicated no statistical association between age and QWL ( p = 0.057). There was a strong positive association between age and fair compensations for the subscales of QWL ( r = 0.151, p = 0.014). Pearson’s test showed no significant relationship between marital status and the number of children with a nurse’s QWL ( p = 0.618 and p = 0.311, respectively). Regarding the subscales of the QWL, there was a significant positive correlation between fair compensations and the number of children ( r = 0.155, p = 0.014).
Furthermore, there was no significant statistical relationship between the QWL, work experience ( r =-0.078, p = 0.222), and work experience in the COVID-19 unit ( r = 0.006, p = 0.923), but there was a negative and significant relationship between fair compensations subscale and work experience ( r =-0.159, p = 0.016).
Relationship between workload, the quality of work life, and work shift in nurses
Even though the workload of night shifts was less than in the morning and afternoon, the results of the one-way analysis of variance test (ANOVA) indicated no statistically significant relationship between workload and shift work, and it was the same for the relationship between each workload subscale and work shift. The frustration score on the night shift was close to the significance level ( p = 0.059). Also, the results of One-way ANOVA indicated no significant difference between the nurses’ QWL in different shifts. There was no significant relationship between work shifts and QWL ( p = 0.933), but the nurses’ QWL was more appropriate in night shifts (Table 3 ).
The relationship between QWL and its subscales with the workload in nurses
Based on the results, there was a significant negative correlation of 0.308 between workload and QWL in nurses ( r =-0.308, p < 0.001); in other words, a higher workload decreased the QWL. Furthermore, the workload had a significant inverse relationship with all subscales of the QWL (Table 4 ).
The multivariate linear regression analysis of the effect of the demographic characteristics and workload subscales on the QWL`
A multiple linear regression model was used to investigate the predictor variables (the demographic characteristics and workload subscales) that had a significant effect on global QWL based on the backward model. To evaluate the extent of the correlation of QWL score with each predictive variable, we used backward linear regression and the ‘margins’ post- estimation command to obtain estimated marginal means and associated confidence intervals. The Kolmogorov–Smirnov test was used to test predictive variables for multicollinearity and the residuals for normal distribution. The results of the regression indicated the four predictors explained 13% of the variance ( R 2 = 0.14, F (4,244) = 10.28, p < 0.001). It was found that number of children (β = 4.61, p = 0.004), work experience (β= − 0.54, p = 0.019), Effort (β = 0.37, p = 0.033), and total workload (β = −0.44, p = 0.000) significantly predicted nurses’ QWL (Table 5 ).
The current study’s findings, which sought to ascertain the relationship between nurses’ workload and the quality of their working lives while caring for COVID-19 patients, showed that the average workload for the nurses was 71.43 ± 14.15. Consistent with the results of the present study, Pourteimour et al. (2021) reported the mean workload of nurses who took care of patients with COVID-19 in Urmia and Hamedan hospitals (67.30 ± 14.53) [ 35 ]. The results of studies by Shoja et al. (2020) and Judek et al. (2018) also confirmed this finding [ 36 , 37 ]. Based on findings of research by Bakhshi et al. in Kermanshah hospitals (2017), the mean ± standard deviation of workload score was 69.73 ± 15.26 [ 5 ], and it was 59.95 ± 16.41in a study by Jarahian et al. [ 6 ], and it was partially less than the present study. In similar studies, nurses’ mean workload was moderate to low in non-critical situations [ 38 , 39 , 40 ]. Malekpour et al. (2014) reported that nurses were responsible for 80% of tasks in health and medical centers and generally had a heavy workload [ 3 ]. The COVID-19 epidemic has significantly increased the workload for nurses, as indicated by the results. According to the findings, mental demand was identified as the dimension with the highest perceived workload, while overall performance had the lowest workload, aligning with a study by Gharagozlou et al. (2020) [ 41 ]. Shoja et al. (2020) examined the subscales of the workload questionnaire and observed increased scores for mental demand, physical demand, temporal demand, and frustration, leading them to conclude that the COVID-19 pandemic negatively affected staff workload and mental health [ 36 ]. A study conducted by Bakhshi et al. (2017) found that mental workload made the highest contribution, while the feeling of frustration had the lowest contribution [ 5 ]. Rafiee et al. (2015) conducted a study to measure the mental workload of nurses in the emergency department of a hospital and reported that the dimension of overall performance had the lowest score, while frustration had the highest score [ 42 ].
Furthermore, the nurses caring for COVID-19 patients endure high physical and mental demands. Based on the results of some studies conducted before the prevalence of COVID-19, nurses who took care of COVID-19 patients felt more frustrated and discouraged but considered their activities more effective. High and frequent workloads are two key factors leading to exhaustion and burnout [ 12 ], resulting in lower overall performance, memory, and thinking process, irritability, annoyance, and reduced learning [ 43 ]. The findings of Mohamadzadeh Tabrizis’ study show the negative impact of caring for COVID-19 patients on nurses’ quality of life [ 44 ].
This study showed that other than age, there was no link between workload and demographic factors like sex, marital status, number of children, working shifts, and years of work experience. There was a relationship between marital status, mental demand, the number of children, and temporal demand. There was no correlation between workload and work experience in the COVID-19 unit and shift work. Jarahian et al. (2018) found a correlation between workload, work experience, and the number of children. The study indicated that individuals with lower work experience and no children had lower mental workloads [ 6 ].
The findings of a study on determinants of workload indicated a significant relationship between physical workload with work experience, age, work pattern, number of shifts, and type of employment, and between temporal demand with body mass index (BMI), work experience, and type of employment [ 5 ]. Based on research by Shoja et al., the type of job, work shift, education level, and exposure to COVID-19 affected the workload score [ 36 ]. Older nurses, married individuals, and those with children might experience a higher workload due to increased work shifts and forced overtime. The higher workload, particularly regarding temporal demand, is especially evident. Establishing a balance between work life and personal/family demands is vital since research indicates that personal and professional lives often intertwine [ 4 ]. Nurses, regardless of gender or age, must work various shifts and wear protective masks in hospitals during the COVID-19 outbreak. Huang et al. (2018) confirm that nurses face high responsibility, heavy workload, intense work pressure, and the need to work in rotational shifts due to the unique nature of their profession [ 45 ].
Based on the results, the mean QWL of the nurses was 88.26 ± 19.50. In line with the findings of the present study, Nikeghbal et al. reported that the QWL of nurses who took care of patients with COVID-19 was 92.57 with a standard deviation of 13.2, which was better than the non-COVID-19 caregivers (79.43). A significant association between the two groups was revealed by the comparison ( p = 0.001) [ 46 ]. The results of Mohammadi’s study in Iran [ 29 ], and most studies in the world, show that nursing QWL is mainly at a moderate level and requires improvement interventions [ 40 , 42 , 47 ]. Some studies show an increase in depression, anxiety [ 48 ], stress, and burnout [ 49 , 50 ] among nurses during the pandemic of Coronavirus Disease.
Based on the results, the highest score of subscales belonged to safety and health in working conditions, while the lowest score belonged to work and total living space. Like Aminizadeh’s finding in pre-hospital staffs, Opportunity to use and develop human capabilities had a significant role in nurses’ QWL [ 26 ]. According to research on the relationship between job burnout, performance, and QWL, the constitutionalism in how work is organized contributed the most to the QWL score, while the social significance of work life contributed the least [ 51 ].
In a study on the relationship between the components of the QWL and job satisfaction of midwives, the results indicated that providing career opportunities and job security had the most significant contribution, and social relevance of work life in the organization had the minor contribution to the QWL in the midwives [ 52 ].
Falahi Khoshknab’s study before the COVID-19 pandemic indicated that 21% of nurses described their quality of work life (QWL) as moderate, while 67% described it as good, and 11% of nurses were delighted with their QWL [ 53 ]. In a study by Faraji et al. conducted prior to the prevalence of COVID-19, 61% of nurses had a low QWL, and even 39.7% of them wanted to leave their jobs [ 54 ]. In line with these studies, the current study, as well as Jafari’s study [ 48 ], suggests that nurses must receive adequate support to overcome workplace stressors. The findings of Shirali’s study showed job stress and low resilience as threatening factors in nurses during the care of COVID-19 patients [ 55 ]. Therefore, support for nurses should focus on both individual and organizational aspects.
Nurses’ workload has significantly increased, yet their work-life quality remains moderate. Various factors contribute to this category, and we will address some below. The present study identified a significant relationship among age, number of children, work experience, and specific aspects of QWL. Previous studies, such as those conducted by Gharagozlou et al. and Shafipour et al., found no significant relationship between QWL and demographic variables like age, gender, and marital status [ 41 , 56 ]. Dehghannayieri et al. [ 57 ] and Dargahi et al. [ 58 ] also found no significant relationship between marital status and QWL, but Khaghanizadeh [ 59 ] and Falahi Khoshknab [ 53 ] reported a significant relationship. Mohammadi et al. (2017) reported a significant correlation between the QWL and employment status, shift work, hospital, and satisfaction with the field of study ( p < 0.001) [ 29 ]. According to Gharagozlou’s study, there was no significant relationship between nurses’ QWL with the number of shifts and the number of patients in each shift, but there was a significant relationship between the QWL and overtime hours among the nurses [ 41 ]. In a study by Shafipour et al., there were significant relationships between the QWL, overtime hours, number of night shifts per month, and income level, but there was no significant relationship with the job unit [ 56 ]. A study indicated that working on the night shift negatively influences nurses’ QWL [ 60 ]. Researchers considered possible reasons for contradictions and differences in the types of sectors based on the characteristics of the participants and the study time (before and during the pandemic) in the study. The present study reported no difference among different shifts regarding QWL, but the night shift was associated with a better QWL. Researchers believe this was because most diagnostic and therapeutic procedures were carried out during the morning shift, and systemic supervision and nurses’ freedom of action were reduced during the night shift. However, the difference was not statistically significant.
Furthermore, there was a relationship between work experience and adequate and fair compensation, indicating the financial concerns of married nurses with higher experience and more children. In the present study, the Opportunity to use and develop human capabilities and safety and health in working conditions had the most significant contribution, adequate and fair compensations, and work and total living space had the minor contribution. Consistent with this finding, Jafari et al. reported that the highest contribution to the QWL was the development of human capabilities, career opportunities, and job security, but the lowest was fair compensations [ 34 ]. In a study by Dargahi et al. [ 58 ] and research in Ethiopia [ 4 ], there was a significant relationship between the monthly income level and the QWL. The QWL increased with higher total compensation. A study in Canada indicated that a higher level of income increased the QWL [ 61 ], but in a study by Nikeghbal et al., there was a significant relationship between the QWL index (adequate and fair compensations) and monthly income only in nurses who took care of COVID-19 patients [ 46 ].
The results of this study indicate a significant inverse relationship between nurses’ workload and quality of work life (QWL). In other words, a higher workload leads to a decrease in QWL. The COVID-19 pandemic has imposed difficult circumstances, and due to the intensity of the workload, nurses have had to put their own lives and the lives of their loved ones at risk while treating COVID-19 patients. The risk of infection and death from COVID-19 has caused significant psychosocial stress for nurses and other healthcare professionals [ 62 ]. In similar studies, Lai et al. [ 63 ] and Gharagozlou et al. [ 41 ] investigated the QWL and workload status using the same tools as in the present study and reported significant relationships between different dimensions of workload and QWL.
Numerous studies have indicated that a high workload endangers the quality and safety of patient care, increases errors, and ultimately prolongs hospitalization time. This situation affects the relationship between nurses, physicians, and patients [ 64 ]. In a study by Ardesatni Rostami et al. (2019) focusing on nurses in ICUs, a negative correlation was found between workload and job performance. According to the study, 75% of nurses rated their performance moderate [ 65 ]. These studies were conducted primarily before the COVID-19 pandemic, but nurses have always had to work long hours to manage their workload. Although the pandemic has further increased their workload, it has not significantly impacted the quality of their work life. Similar to the pre-COVID-19 era, the quality of work life remains predominantly dependent on organizational factors such as support and financial assistance.
The present findings indicate that an increase in the number of children and effort contributes to a high level of QWL, while work experience and total workload decrease the QWL of nurses during the COVID-19 pandemic. Consistent with these findings, Navales et al. (2021) reported a relationship between individual factors, such as older nurses, females, bachelor graduates with more dependents, more children, and job positions with more extended work experience, and nurses’ QWL in Indonesia [ 66 ]. Woon et al. (2021) found that social support from friends and significant others (such as children and spouse) predicted higher QWL. Despite the COVID-19 restrictions, encouragement regarding family and children appears to have positively influenced the quality of nurses’ work life [ 67 ].
Contrary to the findings of Gharagozlou’s study, nurses who encounter COVID-19 patients require additional effort, potentially resulting in an enhanced QWL [ 41 ]. Hence, despite the numerous adverse effects of the COVID-19 pandemic on nurses, it has also presented opportunities for provisional, organizational, and individual improvements in their quality of life.
The mental burden experienced by nurses in these job groups is significant. Several factors contribute to the creation and escalation of this burden, including consistent and uninterrupted work, work duration, job requirements (such as concentration, accuracy, and effort), physical stress-induced fatigue, age, work experience, environmental factors (such as sound and vibration), equipment usage, individual feedback on work and interpersonal interactions, overtime, and ergonomic working conditions [ 46 ]. Thus, these factors are among those that contribute to the increased workload of nurses. Furthermore, as these employees operate within a consistent and stable work environment characterized by the nature of the job and working conditions, they often have longer working hours. Consequently, this leads to physical and mental fatigue, exhaustion, burnout and ultimately diminishing their QWL. In line with the negative effect of workload on QWL, Nikeghbal et al.‘s study supported that an increased workload was associated with a decreased QWL [ 46 ].
Limitations of the study
Since we conducted this research solely on the Shahrud University of Medical Sciences nursing staff, it is essential to exercise caution when generalizing the results to other settings. We recommend conducting multicenter studies with larger sample sizes. We maintained a continuous presence in different units and shifts to address the main barriers for nurses to participate in the study, namely the lack of free time and high workload. We also followed up to increase participation in the study. Another limitation was that nurses were less focused on answering the questionnaires because they had to complete them during work hours. Some nurses hesitated to complete the questionnaires due to insufficient information from prior research. We assured the participants that they would have access to the research results. Furthermore, it is worth noting that the participants’ mental state during the questionnaire completion could also influence the research results.
Recommendations for future research
We recommend conducting multicenter studies with larger samples in settings with different cultures to identify other unrecognized effective factors in relation to workload and QWL. It is essential to carry out interventional studies, mainly focusing on nurses’ psychological empowerment and organizational support. Additionally, qualitative research is required to explain the process of QWL development and comprehend nurses’ lived experiences.
Clinical implications for nursing managers and policymakers
In order to achieve a better quality of work life (QWL), nursing managers can take active steps to improve nurses’ work conditions. These steps include reducing nurses’ workload, creating a respectful working atmosphere, considering their work experience, work shifts, and age, and ensuring adequate and fair pay. Additionally, effective measures should be taken to recruit a new workforce, balance nurses’ workload, and provide suitable facilities and incentives.
The high workload was a significant stressor for hospital staff and nurses. The nurses’ workload increased, leading to increased stress and decreased productivity, ultimately affecting their quality of life. Compared to studies before the outbreak of COVID-19, there was a partial increase in nurses’ workload, but there was no noticeable change in the quality of their work life, which remained at a moderate level. Therefore, acquiring knowledge about the influential factors for positive quality of work life (QWL) development among nurses is crucial to improve their QWL. Developing QWL in nurses can increase their loyalty to the profession and promote the quality of care and patient satisfaction while decreasing nurses’ exhaustion and burnout.
Availability of data and materials
All the data supporting the study findings are within the manuscript. Additional detailed information and raw data are available from the corresponding author upon reasonable request.
Abbreviations
World Health Organization
Quality of work life
Gerami Nejad N, Hosseini M, Mousavi Mirzaei S, Ghorbani Moghaddam Z. Association between Resilience and Professional Quality of Life among Nurses Working in Intensive Care Units. IJN. 2019;31(116):49–60.
Article Google Scholar
World Health Organization. State of the world’s nursing 2020: investing in education, jobs and leadership. Available at: https://www.who.int/publications/i/item/9789240003279 .
Malekpour F, Mohammadian Y, Malekpour AR, Mohammadpour Y, Sheikh Ahmadi A, Shakarami A. Assessment of mental workload in nursing using NASA-TLX. Nurs Midwifery J. 2014;11(11):892–99.
Google Scholar
Mosisa G, Abadiga M, Oluma A, Wakuma B. Quality of work-life and associated factors among nurses working in wollega zones public hospitals, West Ethiopia: a cross-sectional study. Int J Afr Nurs Sci. 2022;17:100466. https://doi.org/10.1016/j.ijans.2022.100466 .
Bakhshi E, Mazlomi A, Hoseini SM. Mental workload and its determinants among nurses in one hospital in Kermanshah City, Iran. J Occup Hygiene Eng (JOHE). 2017;3(4):53–60.
Jarahian Mohammady M, Sedighi A, Khaleghdoost T, Kazem Nejad E, Javadi-Pashaki N. Relationship between Nurses’ subjective workload and occupational cognitive failure in Intensive Care Units. J Crit Care Nurs (jccnursing). 2018;11(4):53–61.
Abdi F, Khaghanizade M, Sirati M. Determination of the amount burnout in nursing staff. J Behav Sci. 2008;2(1):51–9.
Chou L, Li C, Hu SC. Job stress and burnout in hospital employees: comparisons of different medical professions in a regional hospital in Taiwan. BMJ Open. 2014;4:e004185. https://doi.org/10.1136/bmjopen-2013-004185 .
Article PubMed PubMed Central Google Scholar
Nemati M, Ebrahimi B, Nemati F. Assessment of iranian nurses’ knowledge and anxiety toward COVID-19 during the current outbreak in Iran. Arch Clin Infect Dis. 2020;15(COVID–19):e102848. https://doi.org/10.5812/archcid.102848 .
Article CAS Google Scholar
Jamebozorgi M, Jafari H, Sadeghi R, Sheikhbardsiri H, Kargar M, Gharaghani MA. The prevalence of depression, anxiety, and stress among nurses during the coronavirus disease 2019: a comparison between nurses in the frontline and the second line of care delivery. Nurs Midwifery Stud. 2021;10(3):188–93. https://doi.org/10.4103/nms.nms_103_20 .
Razu SR, Yasmin T, Arif TB, Islam M, Islam SMS, Gesesew HA, Ward P. Challenges faced by healthcare professionals during the COVID-19 pandemic: a qualitative inquiry from Bangladesh. Front public health. 2021;9:647315. https://doi.org/10.3389/fpubh.2021.647315 .
Jamebozorgi MH, Karamoozian A, Bardsiri TI, Sheikhbardsiri H. Nurses burnout, resilience, and its association with socio-demographic factors during COVID-19 pandemic. Front Psychiatry. 2022;12:803506. https://doi.org/10.3389/fpsyt.2021.803506 .
Potas N, Koçtürk N, Toygar SA. Anxiety effects on quality of life during the COVID-19 outbreak: a parallel-serial mediation model among nurses in Turkey. Work. 2021;69(1):37–45. https://doi.org/10.3233/WOR-205050 .
Article PubMed Google Scholar
Bo HX, Li W, Yang Y, Wang Y, Zhang Q, Cheung T, Wu X, Xiang YT. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol Med. 2021;51(6):1052–3. https://doi.org/10.1017/S0033291720000999 .
Poursadeghiyan M, Abbasi M, Mehri A, Hami M, Raei M, Ebrahimi MH. Relationship between job stress and anxiety, depression and job satisfaction in nurses in Iran. The Soc Sci. 2016;11(9):2349–55.
Rahimian Boogar E, Nouri A, Oreizy H, Molavi H, Foroughi Mobarake A. Relationship between adult attachment styles with job satisfaction and job stress in nurses. Iran J psychiatry Clin Psychol (IJPCP). 2007;13(2):148–57.
Galehdar N, Toulabi T, Kamran A, Heydari H. Exploring nurses’ perception of taking care of patients with coronavirus disease (COVID-19): a qualitative study. Nurs Open. 2020;11(1):171–9. https://doi.org/10.1002/nop2.616 .
Shiri A, Yari AB, Dehghani M. A study of relation between Job Rotation and Staff’s Organizational Commitment (A Case Study at Ilam University). Trends Adv Sci Engin. 2012;5(1):82–6.
Yunus YM, Idris K, Rahman AA, Lai HI. The role of quality of nursing work life and turnover intention in primary healthcare services among registered nurses in Selangor. Int J Acad Res Bus Soc Sci. 2017;7(6):1201–13. https://doi.org/10.6007/IJARBSS/v7-i6/3353 .
Abrishamirad S, Kordi M, Abbasi T. A comparison of Employee’s Engagement Models with emphasis on Human Resources in Iranian Organizations. Iran J Comp Educ. 2021;4(3):1329–48. https://doi.org/10.22034/IJCE.2021.256255.1236 .
Ruževičius J. Quality of Life and of Working Life: Conceptions and research. 17th Toulon-Verona International Conference. Liverpool John Moores University. Excellence in Services. Liverpool (England). Conference Proceedings ISBN 9788890432743, August 28-29, 2014: 317-334.
Hosseini M, Sedghi Goyaghaj N, Alamadarloo A, Farzadmehr M, Mousavi A. The relationship between job burnout and job performance of clinical nurses in Shiraz Shahid Rajaei hospital (thruma) in 2016. J Clin Nurs Midwifery. 2017;6(2):59–68.
Kuzey C. Impact of Health Care Employees’ job satisfaction on Organizational Performance Support Vector Machine Approach (January 19, 2018). J Econ Financial Anal. 2018;2(1):45–68.
Abadi F, Abadi F, Nouhi E. Survey factors affecting of quality of work life in the clinical nurses. Nurs Midwifery J. 2019;16(11):832–40.
Salahat MF, Al-Hamdan ZM. Quality of nursing work life, job satisfaction, and intent to leave among jordanian nurses: a descriptive study. Heliyon. 2022;8(7):e09838. https://doi.org/10.1016/j.heliyon.2022.e09838 .
Aminizadeh M, Saberinia A, Salahi S, Sarhadi M, Jangipour Afshar P, Sheikhbardsiri H. Quality of working life and organizational commitment of iranian pre-hospital paramedic employees during the 2019 novel coronavirus outbreak. Int J Healthc Manag. 2022;15(1):36–44. https://doi.org/10.1080/20479700.2020.1836734 .
Mehryar HR, Garkaz O, Sepandi M, Taghdir M, Paryab S. How to manage emergency response of health teams to natural disasters in Iran: a systematic review. Arch Trauma Res. 2021;10(1):1–6. https://doi.org/10.4103/atr.atr_20_20 .
Stavropoulou A, Rovithis M, Sigala E, Moudatsou M, Fasoi G, Papageorgiou D, Koukouli S. Exploring nurses’ working experiences during the First Wave of COVID-19 outbreak. Healthc (Basel). 2022;10(8):1406. https://doi.org/10.3390/healthcare10081406 .
Mohammadi M, Mozaffari N, Dadkhah B, Etebari Asl F, Etebari Asl M. Study of work-related quality of life of nurses in Ardabil Province Hospitals. J Health Care (JHC). 2017;19(3):108–16.
Mohamed R, Raman M, Anderson J, McLaughlin K, Rostom A, Coderre S. Validation of the National Aeronautics and Space Administration Task load index as a tool to evaluate the learning curve for endoscopy training. Can J Gastroenterol Hepatol. 2014;28(3):155–9. https://doi.org/10.1155/2014/892476 .
Mohammadi M, Nasl Seraji J, Zeraati H. Developing and assessing the validity and reliability of a questionnaire to assess the mental workload among ICUs Nurses in one of the Tehran University of Medical Sciences hospitals, Tehran, Iran. J Sch Public Health Inst Public Health Res. 2013;11(2):87–96.
Safari S, Mohammadi-Bolbanabad H, Kazemi M. Evaluation Mental Work load in nursing critical care unit with National Aeronautics and Space Administration Task load index (NASA-TLX). J Health Syst Res. 2013;9(6):613–9.
Walton RE. Quality of working life: what is it? Sloan Management Review. 1973;15(1):11–21.
Jafari M, Habibi Houshmand B, Maher A. Relationship of occupational stress and quality of work life with turnover intention among the Nurses of Public and private hospitals in selected cities of Guilan Province, Iran, in 2016. J Health Res Commun. 2017;3(3):12–24.
Pourteimour S, Yaghmaei S, Babamohamadi H. The relationship between mental workload and job performance among iranian nurses providing care to COVID-19 patients: a cross-sectional study. J Nurs Manag. 2021;29(6):1723–32. https://doi.org/10.1111/jonm.13305 .
Shoja E, Aghamohammadi V, Bazyar H, Moghaddam HR, Nasiri K, Dashti M, Choupani A, Garaee M, Aliasgharzadeh S, Asgari A. Covid-19 effects on the workload of iranian healthcare workers. BMC Public Health. 2020;20(1):1636. https://doi.org/10.1186/s12889-020-09743-w .
Article CAS PubMed PubMed Central Google Scholar
Judek C, Verhaegen F, Belo J, Verdel T. Crisis managers’ workload assessment during a simulated crisis situation. By Malizia A, D’Arienzo M, editors. Enhancing CBRNE Safety & Security: Proceedings of the SICC 2017Conference. Spinger Nature 2018. https://doi.org/10.1007/978-3/319-91791-7_37 .
Destiani W, Mediawati AS, Permana RH. The mental workload of nurses in the role of nursing care providers. J Nurs Care. 2020;3(1):11–8. https://doi.org/10.24198/jnc.v3il.22938 .
Mohammadi M, Mazloumi A, Kazemi Z, Zeraati H. Evaluation of Mental workload among ICU Ward’s nurses. Health Promot Perspect. 2016;5(4):280–7. https://doi.org/10.15171/hpp.2015.033 .
Asamani JA, Amertil NP, Chebere M. The influence of workload levels on performance in a rural hospital. Br J Healthc Manage. 2015;21(12):577–86. https://doi.org/10.12968/bjhc.2015.21.12.577 .
Gharagozlou F, karamimatin B, Kashefi H, Nikravesh Babaei D, Bakhtyarizadeh F, Rahimi S. The relationship between quality of working life of nurses in educational hospitals of Kermanshah with their perception and evaluation of workload in 2017. Iran Occup Health (ioh). 2020;17(1):25–36.
Rafiee N, Hajimaghsoudi M, Bahrami Ma GN, Mazrooei M. Evaluation nurses’ mental work load in Emergency Department: case study. Quart J Nurse Manag. 2015;3(4):43–50.
Sorić M, Golubić R, Milosević M, Juras K, Mustajbegović J. Shift work, quality of life and work ability among croatian hospital nurses. Coll Antropol. 2013;37(2):379–84. PMID: 23940978.
PubMed Google Scholar
Mohamadzadeh Tabrizi Z, Mohammadzadeh F, Davarinia Motlagh Quchan A, Bahri N. COVID-19 anxiety and quality of life among iranian nurses. BMC Nurs. 2022;21(1):27. https://doi.org/10.1186/s12912-021-00800-2 .
Huang CLC, Wu MP, Ho CH, Wang JJ. Risks of treated anxiety, depression, and insomnia among nurses: a nationwide longitudinal cohort study. PLoS ONE. 2018;13(9):e0204224. https://doi.org/10.1371/journal.pone.0204224 .
Nikeghbal K, Kouhnavard B, Shabani A, Zamanian Z. Covid-19 Effects on the Mental workload and quality of Work Life in iranian nurses. Ann Glob Health. 2021;87(1):79. https://doi.org/10.5334/aogh.3386 .
Parra-Giordano D, Quijada Sánchez D, Grau Mascayano P, Pinto-Galleguillos D. Quality of Work Life and work process of assistance nurses. Int J Environ Res Public Health. 2022;19(11):6415. https://doi.org/10.3390/ijerph19116415 .
Jafari H, Amiri Gharaghani M. Cultural challenges: the most important challenge of COVID-19 control policies in Iran. Prehosp Disaster Med. 2020;35(4):470–1. https://doi.org/10.1017/S1049023X20000710 .
Jose S, Dhandapani M, Cyriac MC. Burnout and resilience among frontline nurses during COVID-19 pandemic: a cross-sectional study in the emergency department of a tertiary care center, North India. Indian J Crit Care Med. 2020;24(11):1081–88. https://doi.org/10.5005/jp-journals-10071-23667 .
Kishi H, Watanabe K, Nakamura S, Taguchi H, Narimatsu H. Impact of nurses’ roles and burden on burnout during the COVID-19 pandemic: Multicentre cross-sectional survey. J Nurs Manag. 2022;30(6):1922–30. https://doi.org/10.1111/jonm.13648 .
Bakhshi E, Gharagozlou F, Moradi A, Naderi MR. Quality of work life and its association with job burnout and job performance among iranian healthcare employees in Islamabad-e Gharb, 2016. J Occup Health Epidemiol. 2019;8(2):94–101.
Hadizadeh Talasaz Z, Nourani Saadoldin S, Shakeri MT. Relationship between components of quality of Work Life with Job satisfaction among midwives in mashhad, 2014. J Hayat. 2015;21(1):56–67.
Falahi Khoshknab M, Karimlou M, Rahgoy A, Fattah Moghaddam L. Quality of life and factors related to it among psychiatric nurses in the university teaching hospitals in Tehran. Hakim Res J. 2007;9(4):24–30.
Faraji O, Salehnejad G, Gahramani S, Valiee S. The relation between nurses’ quality of work life with intention to leave their job. Nurs Pract Today (NPT). 2017;4(2):103–11.
Shirali GA, Amiri A, Chanani KT, Silavi M, Mohipoor S, Rashnuodi P. Job stress and resilience in iranian nurses during the COVID-19 pandemic: a case-control study. Work. 2021;70(4):1011–20. https://doi.org/10.3233/WOR-210476 .
Shafipour V, Momeni B, YazdaniCharati J, Esmaeili R. Quality of working life and its related factors in critical care unit nurses. J Mazandaran Univ Med Sci. 2016;26(142):117–26.
Dehghannyieri N, Salehi T, Asadinoghabi A. Assessing the quality of work life, productivity of nurses and their relationship. IJNR. 2008;3(9):8.
Dargahi H, Gharib M, Goodarzi M. Quality of work life in nursing employees of Tehran University of Medical Sciences Hospitals. J Hayat. 2007;13(2):13–21.
Khaghanizadeh M, Ebadi A, Cirati nair M, Rahmani M. The study of relationship between job stress and quality of work life of nurses in military hospitals. J Mil Med. 2008;10(3):175–84.
Ebatetou E, Atipo-Galloye P, Moukassa D. Shift work: impact on nurses’ Health and Quality Life in Pointe-Noire (Congo). Open J Epidemiol. 2021;11:16–30. https://doi.org/10.4236/ojepi.2021.111002 .
Sale JE, Smoke M. Measuring quality of work-life: a participatory approach in a canadian cancer center. J Cancer Educ. 2007;22(1):62–6. https://doi.org/10.1007/BF03174378 .
Huang L, Lin G, Tang L, Yu L, Zhou Z. Special attention to nurses’ protection during the COVID-19 epidemic. Crit Care. 2020;24:120. https://doi.org/10.1186/s13054-020-2841-7 .
Lai SL, Chang J, Hsu LY. Does effect of workload on quality of work life vary with generations? Asia Pac Manage Rev. 2017;17(4):437–51. https://doi.org/10.6126/APMR.2012.17.4.06 .
Boonrod W. Quality of working life: perceptions of professional nurses at Phramongkutklao Hospital. J Med Assoc Thai. 2009;92(Suppl 1):S7-15 PMID: 21302412.
Ardesatni Rostami R, Ghasembaglu A, Bahadori M. Relationship between work load of nurses and their performance in the intensive care units of educational hospitals in Tehran. SJNMP. 2019;4(3):63–71.
Navales JV, Jallow AW, Lai CY, Liu CY, Chen SW. Relationship between quality of nursing work life and uniformed nurses’ attitudes and practices related to COVID-19 in the Philippines: a cross-sectional study. Int J Environ Res Public Health. 2021;18(19):9953. https://doi.org/10.3390/ijerph18199953 .
Woon LS, Mansor NS, Mohamad MA, Teoh SH, Leong Bin Abdullah MFI. Quality of life and its predictive factors among healthcare workers after the end of a movement lockdown: the salient roles of COVID-19 stressors, psychological experience, and social support. Front Psychol. 2021;12:652326. https://doi.org/10.3389/fpsyg.2021.652326 .
Download references
Acknowledgements
We took the present manuscript from the nursing master’s thesis, which Semnan University of Medical Sciences approved and supported. We express our gratitude to the management and nursing staff of Shahrud Hospital for their cooperation in facilitating the data collection.
We conducted this study without financial support.
Author information
Authors and affiliations.
Nursing Care Research Center, Education and Research Campus, Semnan University of Medical Sciences, Po Box: 3513138111, 5 Kilometer of Damghan Road, Semnan, Iran
Hassan Babamohamadi, Hossein Davari & Seifollah Alaei
Department of Nursing, School of Nursing and Midwifery, Semnan University of Medical Sciences, Semnan, Iran
Student Research Committee, Semnan University of Medical Sciences, Semnan, Iran
Abbas-Ali Safari
Social Determinants of Health Research Center, Semnan University of Medical Sciences, Semnan, Iran
Sajjad Rahimi Pordanjani
Department of Community Medicine, School of Medicine, Semnan University of Medical Sciences, Semnan, Iran
You can also search for this author in PubMed Google Scholar
Contributions
SA, AS, and HB conceived and designed the study. AS and HD collected, inputted, and checked the data. SR analyzed the data. SA and HB draft the manuscript. HB and SA revised the manuscript, and SA submitted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Seifollah Alaei .
Ethics declarations
Ethics approval and consent to participate.
The researchers first considered respecting participants’ rights and protecting their health and rights under the guidance of the principles outlined in the World Medical Association Declaration of Helsinki. This study strictly adheres to ethical principles. The Ethics Committee of Semnan University of Medical Sciences approved the research (IR.SEMUMS.REC.1400.282). After obtaining permission from the hospital officials, the researchers initiated data collection. Since the current study was a cross-sectional study with the only risk of participants’ privacy, the researchers introduced themselves to the nurses when conducting the survey. They provided thorough explanations regarding the study objectives and methods, the confidentiality of the data, and the voluntary nature of participation. The nurses’ questions were also addressed, and written informed consent was obtained from them to participate in the study. The researchers distributed the questionnaires among the nurses and requested them to complete and return them in the presence of the researcher.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Babamohamadi, H., Davari, H., Safari, AA. et al. The association between workload and quality of work life of nurses taking care of patients with COVID-19. BMC Nurs 22 , 234 (2023). https://doi.org/10.1186/s12912-023-01395-6
Download citation
Received : 09 March 2023
Accepted : 22 June 2023
Published : 07 July 2023
DOI : https://doi.org/10.1186/s12912-023-01395-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Quality of Work Life
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Open access
- Published: 05 June 2020
Burnout in nursing: a theoretical review
- Chiara Dall’Ora 1 ,
- Jane Ball 2 ,
- Maria Reinius 2 &
- Peter Griffiths 1 , 2
Human Resources for Health volume 18 , Article number: 41 ( 2020 ) Cite this article
241k Accesses
290 Citations
321 Altmetric
Metrics details
Workforce studies often identify burnout as a nursing ‘outcome’. Yet, burnout itself—what constitutes it, what factors contribute to its development, and what the wider consequences are for individuals, organisations, or their patients—is rarely made explicit. We aimed to provide a comprehensive summary of research that examines theorised relationships between burnout and other variables, in order to determine what is known (and not known) about the causes and consequences of burnout in nursing, and how this relates to theories of burnout.
We searched MEDLINE, CINAHL, and PsycINFO. We included quantitative primary empirical studies (published in English) which examined associations between burnout and work-related factors in the nursing workforce.
Ninety-one papers were identified. The majority ( n = 87) were cross-sectional studies; 39 studies used all three subscales of the Maslach Burnout Inventory (MBI) Scale to measure burnout. As hypothesised by Maslach, we identified high workload, value incongruence, low control over the job, low decision latitude, poor social climate/social support, and low rewards as predictors of burnout. Maslach suggested that turnover, sickness absence, and general health were effects of burnout; however, we identified relationships only with general health and sickness absence. Other factors that were classified as predictors of burnout in the nursing literature were low/inadequate nurse staffing levels, ≥ 12-h shifts, low schedule flexibility, time pressure, high job and psychological demands, low task variety, role conflict, low autonomy, negative nurse-physician relationship, poor supervisor/leader support, poor leadership, negative team relationship, and job insecurity. Among the outcomes of burnout, we found reduced job performance, poor quality of care, poor patient safety, adverse events, patient negative experience, medication errors, infections, patient falls, and intention to leave.
Conclusions
The patterns identified by these studies consistently show that adverse job characteristics—high workload, low staffing levels, long shifts, and low control—are associated with burnout in nursing. The potential consequences for staff and patients are severe. The literature on burnout in nursing partly supports Maslach’s theory, but some areas are insufficiently tested, in particular, the association between burnout and turnover, and relationships were found for some MBI dimensions only.
Peer Review reports
Introduction
The past decades have seen a growing research and policy interest around how work organisation characteristics impact upon different outcomes in nursing. Several studies and reviews have considered relationships between work organisation variables and outcomes such as quality of care, patient safety, sickness absence, turnover, and job dissatisfaction [ 1 , 2 , 3 , 4 ]. Burnout is often identified as a nursing ‘outcome’ in workforce studies that seek to understand the effect of context and ‘inputs’ on outcomes in health care environments. Yet, burnout itself—what constitutes it, what factors contribute to its development, and what the wider consequences are for individuals, organisations, or their patients—is not always elucidated in these studies.
The term burnout was introduced by Freudenberger in 1974 when he observed a loss of motivation and reduced commitment among volunteers at a mental health clinic [ 5 ]. It was Maslach who developed a scale, the Maslach Burnout Inventory (MBI), which internationally is the most widely used instrument to measure burnout [ 6 ]. According to Maslach’s conceptualisation, burnout is a response to excessive stress at work, which is characterised by feelings of being emotionally drained and lacking emotional resources—Emotional Exhaustion; by a negative and detached response to other people and loss of idealism—Depersonalisation; and by a decline in feelings of competence and performance at work—reduced Personal Accomplishment [ 7 ].
Maslach theorised that burnout is a state, which occurs as a result of a prolonged mismatch between a person and at least one of the following six dimensions of work [ 7 , 8 , 9 ]:
Workload: excessive workload and demands, so that recovery cannot be achieved.
Control: employees do not have sufficient control over the resources needed to complete or accomplish their job.
Reward: lack of adequate reward for the job done. Rewards can be financial, social, and intrinsic (i.e. the pride one may experience when doing a job).
Community: employees do not perceive a sense of positive connections with their colleagues and managers, leading to frustration and reducing the likelihood of social support.
Fairness: a person perceiving unfairness at the workplace, including inequity of workload and pay.
Values: employees feeling constrained by their job to act against their own values and their aspiration or when they experience conflicts between the organisation’s values.
Maslach theorised these six work characteristics as factors causing burnout and placed deterioration in employees’ health and job performance as outcomes arising from burnout [ 7 ].
Subsequent models of burnout differ from Maslach’s in one of two ways: they do not conceptualise burnout as an exclusively work-related syndrome; they view burnout as a process rather than a state [ 10 ].
The job resources-demands model [ 11 ] builds on the view of burnout as a work-based mismatch but differs from Maslach’s model in that it posits that burnout develops via two separate pathways: excessive job demands leading to exhaustion, and insufficient job resources leading to disengagement. Along with Maslach and Schaufeli, this model sees burnout as the negative pole of a continuum of employee’s well-being, with ‘work engagement’ as the positive pole [ 12 ].
Among those who regard burnout as a process, Cherniss used a longitudinal approach to investigate the development of burnout in early career human services workers. Burnout is presented as a process characterised by negative changes in attitudes and behaviours towards clients that occur over time, often associated with workers’ disillusionment about the ideals that had led them to the job [ 13 ]. Gustavsson and colleagues used this model in examining longitudinal data on early career nurses and found that exhaustion was a first phase in the burnout process, proceeding further only if nurses present dysfunctional coping (i.e. cynicism and disengagement) [ 14 ].
Shirom and colleagues suggested that burnout occurs when individuals exhaust their resources due to long-term exposures to emotionally demanding circumstances in both work and life settings, suggesting that burnout is not exclusively an occupational syndrome [ 15 , 16 ].
This review aims to identify research that has examined theorised relationships with burnout, in order to determine what is known (and not known) about the factors associated with burnout in nursing and to determine the extent to which studies have been underpinned by, and/or have supported or refuted, theories of burnout.
This was a theoretical review conducted according to the methodology outlined by Campbell et al. and Pare et al. [ 17 , 18 ]. Theoretical reviews draw on empirical studies to understand a concept from a theoretical perspective and highlight knowledge gaps. Theoretical reviews are systematic in terms of searching and inclusion/exclusion criteria and do not include a formal appraisal of quality. They have been previously used in nursing, but not focussing on burnout [ 19 ]. While no reporting guideline for theoretical reviews currently exists, the PRISMA-ScR was deemed to be suitable, with some modifications, to enhance the transparency of reporting for the purposes of this review. The checklist, which can be found as Additional file 2 , has been modified as follows:
Checklist title has been modified to indicate that the checklist has been adapted for theoretical reviews.
Introduction (item 3) has been modified to reflect that the review questions lend themselves to a theoretical review approach.
Selection of sources of evidence (item 9) has been modified to state the process for selecting sources of evidence in the theoretical review.
Limitations (item 20) has been amended to discuss the limitations of the theoretical review process.
Funding (item 22) has been amended to describe sources of funding and the role of funders in the theoretical review.
All changes from the original version have been highlighted.
Literature search
A systematic search of empirical studies examining burnout in nursing published in journal articles since 1975 was performed in May 2019, using MEDLINE, CINAHL, and PsycINFO. The main search terms were ‘burnout’ and ‘nursing’, using both free-search terms and indexed terms, synonyms, and abbreviations. The full search and the total number of papers identified are in Additional file 1 .
We included papers written in English that measured the association between burnout and work-related factors or outcomes in all types of nurses or nursing assistants working in a healthcare setting, including hospitals, care homes, primary care, the community, and ambulance services. Because there are different theories of burnout, we did not restrict the definition of burnout according to any specific theory. Burnout is a work-related phenomenon [ 8 ], so we excluded studies focussing exclusively on personal factors (e.g. gender, age). Our aim was to identify theorised relationships; therefore, we excluded studies which were only comparing the levels of burnout among different settings (e.g. in cancer services vs emergency departments). We excluded literature reviews, commentaries, and editorials.
Data extraction and quality appraisal
The following data were extracted from included studies: country, setting, sample size, staff group, measure of burnout, variables the relationship with burnout was tested against, and findings against the hypothesised relationships. One reviewer (MEB) extracted data from all the studies, with CDO and JEB extracting 10 studies each to check for agreement in data extraction. In line with the theoretical review methodology, we did not formally assess the quality of studies [ 19 ]. However, in Additional file 3 , we have summarised the key aspects of quality for each study, covering generalisability (e.g. a multisite study with more than 500 participants); risk of bias from common methods variance (e.g. burnout and correlates assessed with the same survey. This bias arises when there is a shared (common) variance because of the common method rather than a true (causal) association between variables); evidence of clustering (e.g. nurses nested in wards, wards nested in hospitals); and evidence of statistical adjustment (e.g. the association between burnout and correlates has been adjusted to control for potentially influencing variables). It should be noted that cells are shaded in green when the above-mentioned quality standards have been met, and in red when they have not. In the ‘Discussion’ section, we offer a reflection on the common limitations of research in the field and present a graphic summary of the ‘strength of evidence’ in Fig. 1 .
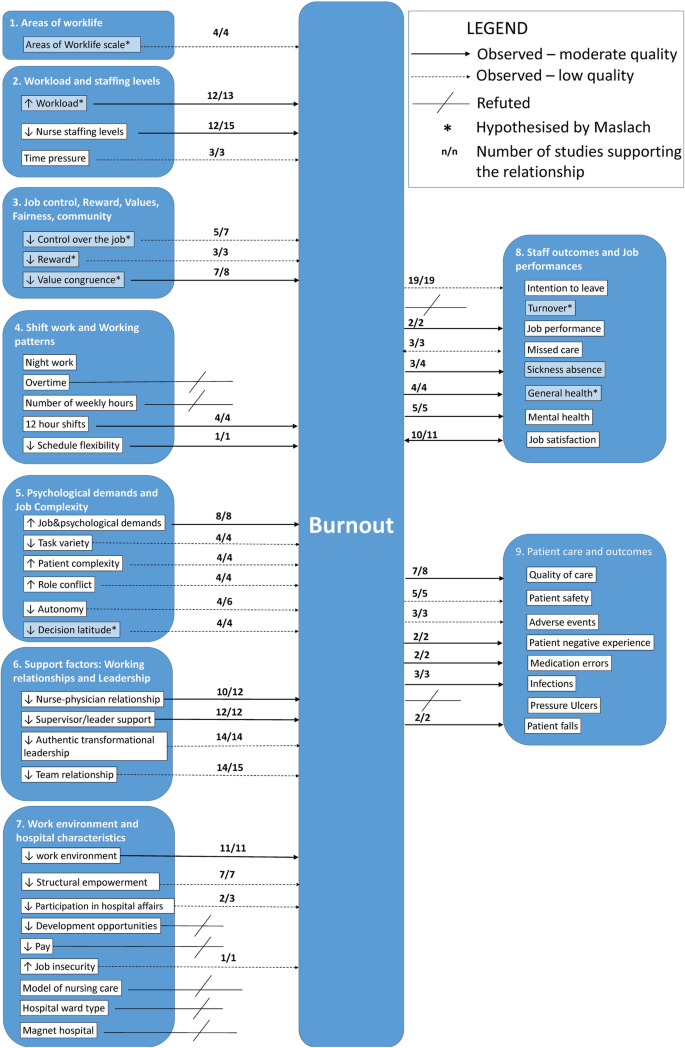
Graphical representation of strength of relationships with burnout
Data synthesis
Due to the breadth of the evidence, we summarised extracted data by identifying common categories through a coding frame. The starting point of the coding frame was the burnout multidimensional theory outlined by Maslach [ 7 ]. We then considered whether the studies’ variables fit into Maslach’s categorisation, and where they did not, we created new categories. We identified nine broad categories: (1) Areas of Worklife; (2) Workload and Staffing Levels; (3) Job Control, Reward, Values, Fairness, and Community; (4) Shift Work and Working Patterns; (5) Psychological Demands and Job Complexity; (6) Support Factors: Working Relationships and Leadership; (7) Work Environment and Hospital Characteristics; (8) Staff Outcomes and Job Performance; and (9) Patient Care and Outcomes. In the literature, categories 1–7 were treated as predictors of burnout and categories 8 and 9 as outcomes, with the exception of missed care and job satisfaction which were treated both as predictors and outcomes.
When the coding frame was finalised, CDO and MLR applied it to all studies. Where there was disagreement, a third reviewer (JEB) made the final decision.
The database search yielded 12 248 studies, of which 11 870 were rapidly excluded as either duplicates or titles and/or abstract not meeting the inclusion criteria. Of the 368 studies accessed in full text, 277 were excluded, and 91 studies were included in the review. Figure 2 presents a flow chart of the study selection.
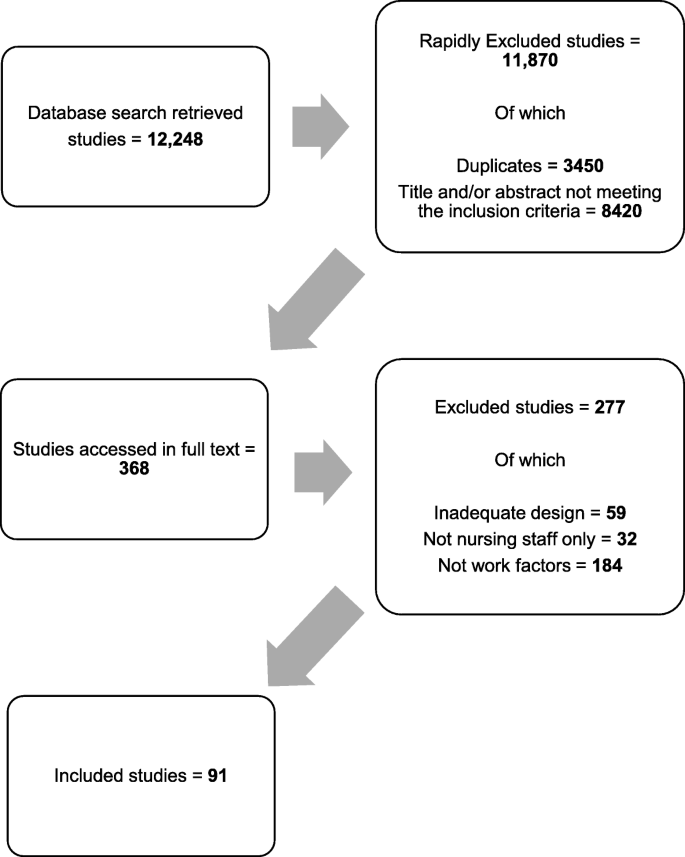
Study selection flow chart
The 91 studies identified covered 28 countries; four studies included multiple countries, and in one, the country was not reported. Most were from North America ( n = 35), Europe ( n = 28), and Asia ( n = 18).
The majority had cross-sectional designs ( n = 87, 97%); of these, 84 were entirely survey-based. Three studies were longitudinal. Most studies were undertaken in hospitals ( n = 82). Eight studies surveyed nurses at a national level, regardless of their work setting.
Sample sizes ranged from hundreds of hospitals (max = 927) with hundreds of thousands of nurses (max = 326 750) [ 20 ] to small single-site studies with the smallest sample being 73 nurses [ 21 ] (see Additional file 3 ).
The relationships examined are summarised in Table 1 .
Measures of burnout
Most studies used the Maslach Burnout Inventory Scale ( n = 81), which comprises three subscales reflecting the theoretical model: Emotional Exhaustion, Depersonalisation, and reduced Personal Accomplishment. However, less than half (47%, n = 39) of the papers measured and reported results with all three subscales. Twenty-three papers used the Emotional Exhaustion subscale only, and 11 papers used the Emotional Exhaustion and Depersonalisation subscales. In nine studies, the three MBI subscales were summed up to provide a composite score of burnout, despite Maslach and colleagues advising against such an approach [ 22 ].
Five studies used the Copenhagen Burnout Inventory (CBI) [ 23 ]. This scale consists of three dimensions of burnout: personal, work-related, and client-related. Two studies used the Malach-Pines Scale [ 24 ], and one used the burnout subscale of the Professional Quality of Life Measure (ProQoL5) scale, which posits burnout as an element of compassion fatigue [ 25 ]. Two studies used idiosyncratic measures of burnout based on items from other instruments [ 20 , 26 ].
Factors examined in relation to burnout: an overview
The studies which tested the relationships between burnout and Maslach’s six areas of worklife—workload, control, reward, community, fairness, and values—typically supported Maslach’s theory that these areas are predictors of burnout. However, some evidence is based only on certain MBI dimensions. High scores on the Areas of Worklife Scale [ 27 ] (indicating a higher degree of congruence between the job and the respondent) were associated with less likelihood of burnout, either directly [ 28 , 29 ] or through high occupational coping self-efficacy [ 30 ] and presence of civility norms and co-worker incivility [ 31 ].
The majority of studies looking at job characteristics hypothesised by the Maslach model considered workload ( n = 31) and job control and reward ( n = 10). While only a few studies ( n = 9) explicitly examined the hypothesised relationships between burnout and community, fairness, or values, we identified 39 studies that covered ‘supportive factors’ including relationships with colleagues and leadership.
A large number of studies included factors that fall outside of the Maslach model. Six main areas were identified:
Working patterns and shifts working ( n = 15)
Features inherent in the job such as psychological demand and complexity ( n = 24)
Job support from working relationships and leadership ( n = 39)
Hospital or environmental characteristics ( n = 28)
Staff outcomes and job performance ( n = 33)
Patient outcomes ( n = 17)
Individual attributes (personal or professional) ( n = 16)
Workload and staffing levels
Workload and characteristics of jobs that contribute to workload, such as staffing levels, were the most frequently examined factor in relation to burnout. Thirty studies found an association between high workload and burnout.
Of these, 13 studies looked specifically at measures of workload as a predictor of burnout. Workload was associated with Emotional Exhaustion in five studies [ 32 , 33 , 34 , 35 , 36 ], with some studies also reporting a relationship with Depersonalisation, and others Cynicism. Janssen reported that ‘mental work overload’ predicted Emotional Exhaustion [ 37 ]. Three studies concluded that workload is associated with both Emotional Exhaustion and Depersonalisation [ 38 , 39 , 40 ]. Kitaoka-Higashiguchi tested a model of burnout and found that heavy workload predicted Emotional Exhaustion, which in turn predicted Cynicism [ 41 ]. This was also observed in a larger study by Greengrass et al. who found that high workload was associated with Emotional Exhaustion, which consequently predicted Cynicism [ 42 ]. One study reported no association between workload and burnout components [ 43 ], and one study found an association between manageable workload and a composite burnout score [ 44 ].
Further 15 studies looked specifically at nurse staffing levels, and most reported that when nurses were caring for a higher number of patients or were reporting staffing inadequacy, they were more likely to experience burnout. No studies found an association between better staffing levels and burnout.
While three studies did not find a significant association with staffing levels [ 32 , 45 , 46 ], three studies found that higher patient-to-nurse ratios were associated with Emotional Exhaustion [ 47 , 48 , 49 ], and in one study, higher patient-to-nurse-ratios were associated with Emotional Exhaustion, Depersonalisation, and Personal Accomplishment [ 50 ]. One study concluded that Emotional Exhaustion mediated the relationship between patient-to-nurse ratios and patient safety [ 51 ]. Akman and colleagues found that the lower the number of patients nurses were responsible for, the lower the burnout composite score [ 52 ]. Similar results were highlighted by Faller and colleagues [ 53 ]. Lower RN hours per patient day were associated with burnout in a study by Thompson [ 20 ].
When newly qualified RNs reported being short-staffed, they were more likely to report Emotional Exhaustion and Cynicism 1 year later [ 54 ]. In a further study, low staffing adequacy was associated with Emotional Exhaustion [ 55 ]. Similarly, Leineweber and colleagues found that poor staff adequacy was associated with Emotional Exhaustion, Depersonalisation, and Personal Accomplishment [ 56 ]. Leiter and Spence Laschinger explored the relationship between staffing adequacy and all MBI subscales and found that Emotional Exhaustion mediated the relationship between staffing adequacy and Depersonalisation [ 57 ]. Time pressure was investigated in three studies, which all concluded that reported time pressure was associated with Emotional Exhaustion [ 58 , 59 , 60 ].
In summary, there is evidence that high workload is associated with Emotional Exhaustion, nurse staffing levels are associated with burnout, and time pressure is associated with Emotional Exhaustion.
Job control, reward, values, fairness, and community
Having control over the job was examined in seven studies. Galletta et al. found that low job control was associated with all MBI subscales [ 40 ], as did Gandi et al. [ 61 ]. Leiter and Maslach found that control predicted fairness, reward, and community, and in turn, fairness predicted values, and values predicted all MBI subscales [ 35 ]. Low control predicted Emotional Exhaustion only for nurses working the day shift [ 62 ], and Emotional Exhaustion was significantly related to control over practice setting [ 63 ]; two studies reported no effect of job control on burnout [ 44 , 64 ].
Reward predicted Cynicism [ 35 ] and burnout on a composite score [ 44 ]. Shamian and colleagues found that a higher score in the effort and reward imbalance scale was associated with Emotional Exhaustion, and higher scores in the effort and reward imbalance scale were associated with burnout measured by the CBI [ 65 ].
Value congruence refers to a match between the requirements of the job and people’s personal principles [ 7 ]. Value conflicts were related with a composite score of burnout [ 44 ], and one study concluded that nurses with a high value congruence reported lower Emotional Exhaustion than those with a low value congruence, and nurses with a low value congruence experienced more severe Depersonalisation than nurses with a high value congruence [ 66 ]. Low value congruence was a predictor of all three MBI dimensions [ 35 ] and of burnout measured with the Malach-Pines Burnout Scale [ 67 ]. Two studies considered social capital, defined as a social structure that benefits its members including trust, reciprocity, and a set of shared values, and they both concluded that lower social capital in the hospital-predicted Emotional Exhaustion [ 33 , 36 ]. A single study showed fairness predicted values, which in turn predicted all MBI Scales [ 35 ]. Two studies looked at community, and one found that community predicts a composite score of burnout [ 44 ], while the other found no relationships [ 35 ].
While not directly expressed in the terms described by Maslach, other studies demonstrate associations with possible causal factors, many of which are reflected in Maslach’s theory.
In summary, there is evidence that control over the job is associated with reduced burnout, and value congruence is associated with reduced Emotional Exhaustion and Depersonalisation.
Working patterns and shift work
Shift work and working patterns variables were considered by 15 studies. Overall, there was mixed evidence on the relationship between night work, number of hours worked per week, and burnout, with more conclusive results regarding the association between long shifts and burnout, and the potential protective effect of schedule flexibility.
Working night shifts was associated with burnout (composite score) [ 68 ] and Emotional Exhaustion [ 62 ], but the relationship was not significant in two studies [ 69 , 70 ]. Working on permanent as opposed to rotating shift patterns did not impact burnout [ 71 ], but working irregular shifts did impact a composite burnout score [ 72 ]. When nurses reported working a higher number of shifts, they were more likely to report higher burnout composite scores [ 68 ], but results did not generalise in a further study [ 69 ]. One study found working that overtime was associated with composite MBI score [ 73 ]. On-call requirement was not significantly associated with any MBI dimensions [ 71 ].
The number of hours worked per week was not a significant predictor of burnout according to two studies [ 25 , 53 ], but having a higher number of weekly hours was associated with Emotional Exhaustion and Depersonalisation in one study [ 70 ]. Long shifts of 12 h or more were associated with all MBI subscales [ 74 ] and with Emotional Exhaustion [ 49 , 75 ]. A study using the ProQoL5 burnout scale found that shorter shifts were protective of burnout [ 25 ].
Having higher schedule flexibility was protective of Emotional Exhaustion [ 46 ], and so was the ability to schedule days off for a burnout composite score [ 76 ]. Having more than 8 days off per month was associated with lower burnout [ 69 ]. Stone et al. found that a positive scheduling climate was protective of Emotional Exhaustion only [ 77 ].
In summary, we found an association between ≥ 12-h shifts and Emotional Exhaustion and between schedule flexibility and reduced Emotional Exhaustion.
Psychological demands and job complexity
There is evidence from 24 studies that job demands and aspects intrinsic to the job, including role conflict, autonomy, and task variety, are associated with some burnout dimensions.
Eight studies considered psychological demands. The higher the psychological demands, the higher the likelihood of experiencing all burnout dimensions [ 72 ], and high psychological demands were associated with higher odds of Emotional Exhaustion [ 62 , 78 ]. Emotional demands, in terms of hindrances, had an effect on burnout [ 67 ]. One study reported that job demands, measured with the Effort-Reward Imbalance Questionnaire, were correlated with all burnout dimensions [ 79 ], and similarly, Garcia-Sierra et al. found that demands predict burnout, measured with a composite scale of Emotional Exhaustion and Cynicism [ 80 ]. According to one study, job demands were not associated with burnout [ 73 ], and Rouxel et al. concluded that the higher the job demands, the higher the impact on both Emotional Exhaustion and Depersonalisation [ 64 ].
Four studies looked at task nature and variety, quality of job content, in terms of skill variety, skill discretion, task identity, task significance, influenced Emotional Exhaustion through intrinsic work motivation [ 37 ]. Skill variety and task significance were related to Emotional Exhaustion; task significance was also related to Personal Accomplishment [ 60 ]. Having no administrative tasks in the job was associated with a reduced likelihood to experience Depersonalisation [ 71 ]. Higher task clarity was associated with reduced levels of Emotional Exhaustion and increased Personal Accomplishment [ 58 ].
Patient characteristics/requirements were investigated in four papers. When nurses were caring for suffering patients and patients who had multiple requirements, they were more likely to experience Emotional Exhaustion and Cynicism. Similarly, caring for a dying patient and having a high number of decisions to forego life-sustaining treatments were associated with a higher likelihood of burnout (measured with a composite score) [ 76 ]. Stress resulting from patient care was associated with a composite burnout score [ 73 ]. Patient violence also had an impact on burnout, measured with CBI [ 81 ], as did conflict with patients [ 76 ].
Role conflict is a situation in which contradictory, competing, or incompatible expectations are placed on an individual by two or more roles held at the same time. Role conflict predicted Emotional Exhaustion [ 41 ], and so it did in a study by Konstantinou et al., who found that role conflict was associated with Emotional Exhaustion and Depersonalisation [ 34 ]; Levert and colleagues reported that role conflict correlated with Emotional Exhaustion, Depersonalisation, and Personal Accomplishment. They also considered role ambiguity, which correlated with Emotional Exhaustion and Depersonalisation, but not Personal Accomplishment [ 39 ]. Andela et al. investigated the impact of emotional dissonance, defined as the mismatch between the emotions that are felt and the emotions required to be displayed by organisations. They reported that emotional dissonance is a mediator between job aspects (i.e. workload, patient characteristics, and team issues) and Emotional Exhaustion and Cynicism. Rouxel et al. found that perceived negative display rules were associated with Emotional Exhaustion [ 64 ].
Autonomy related to Emotional Exhaustion and Depersonalisation [ 60 ], and in another study, it only related to Depersonalisation [ 43 ]. Low autonomy impacted Emotional Exhaustion via organisational trust [ 82 ]. Autonomy correlated with burnout [ 67 ]. There was no effect of autonomy on burnout according to two studies [ 58 , 63 ]. Low decision-making at the ward level was associated with all MBI subscales [ 77 ]. Decision latitude impacted Personal Accomplishment only [ 36 ], and in one study, it was found to be related to Emotional Exhaustion [ 78 ]. High decision latitude was associated with Personal Accomplishment [ 41 ] and low Emotional Exhaustion [ 33 ].
Overall, high job and psychological demands were associated with Emotional Exhaustion, as was role conflict. Patient complexity was associated with burnout, while task variety, autonomy, and decision latitude were protective of burnout.
Working relationships and leadership
Overall, evidence from 39 studies supports that having positive support factors and working relationships in place, including positive relationships with physicians, support from the leader, positive leadership style, and teamwork, might play a protective role towards burnout.
The quality of the relationship with physicians was investigated by 12 studies. In two studies, having negative relationships with physicians was associated with all MBI dimensions [ 77 , 83 ]; quality of nurse-physician relationship was associated with Emotional Exhaustion and Depersonalisation, but not PA [ 50 ]. Two studies found an association with Emotional Exhaustion only [ 55 , 84 ], and one concluded that quality of relationship with physicians indirectly supported PA [ 36 ]. This was also found by Leiter and Laschinger, who found that positive nurse-physician collaborations predicted Personal Accomplishment [ 57 , 85 ]. When burnout was measured with composite scores of MBI and a not validated scale, two studies reported an association with nurse-physician relationship [ 20 , 76 ], and two studies found no associations [ 56 , 63 ].
Having support from the supervisor or leader was considered in 12 studies, which found relationships with different MBI dimensions. A relationship between low support from nurse managers and all MBI subscales was observed in one study [ 77 ], while two studies reported it is a protective factor from Emotional Exhaustion only [ 58 , 83 ], and one that it was also associated with Depersonalisation [ 86 ]. Kitaoka-Higashiguchi reported an association only with Cynicism [ 41 ], and Jansen et al. found it was only associated with Depersonalisation and Personal Accomplishment [ 60 ]. Van Bogaert and colleagues found that support from managers predicted low Emotional Exhaustion and high Personal Accomplishment [ 84 ], but in a later study, it only predicted high Personal Accomplishment [ 36 ]. Regarding the relationship with the manager, it had a direct effect on Depersonalisation, and it moderated the effect of time pressure on Emotional Exhaustion and Depersonalisation [ 59 ]; a protective effect of a quality relationship with the head nurse on a composite burnout score was also reported [ 76 ]. Two studies using different burnout scales found an association between manager support and reduced burnout [ 25 , 67 ]. Low trust in the leader showed a negative impact on burnout, measured with a composite score [ 87 ]. Two further studies focused on the perceived nurse manager’s ability: authors found that it was related to Emotional Exhaustion [ 46 ], and Emotional Exhaustion and Personal Accomplishment [ 50 ].
Fourteen studies looked at the leadership style and found that it affects burnout through different pathways and mechanisms. Boamah et al. found that authentic leadership—described as leaders who have high self-awareness, balanced processing, an internalised moral perspective, and transparency—predicted higher empowerment, which in turn predicted lower levels of Emotional Exhaustion and Cynicism a year later [ 54 ]. Authentic leadership had a negative direct effect on workplace bullying, which in turn had a direct positive effect on Emotional Exhaustion [ 88 ]. Effective leadership predicted staffing adequacy, which in turn predicted Emotional Exhaustion [ 57 , 85 ]. Authentic leadership predicted all areas of worklife, which in turn predicted all MBI dimensions of burnout [ 30 ], and a similar pathway was identified by Laschiner and Read, although authentic leadership impacted Emotional Exhaustion only and it was also through civility norms and co-worker incivility [ 31 ]. Emotional Exhaustion mediated the relationship between authentic leadership and intention to leave the job [ 89 ]. ‘Leader empowering behaviour’ had an indirect effect on Emotional Exhaustion through structural empowerment [ 29 ], and empowering leadership predicted trust in the leader, which in turn was associated with burnout composite score [ 87 ]. Active management-by-exception was beneficial for Depersonalisation and Personal Accomplishment, passive laissez-faire leadership negatively affected Emotional Exhaustion and Personal Accomplishment, and rewarding transformational leadership protected from Depersonalisation [ 90 ]. Contrary to this, Madathil et al. found that transformational leadership protected against Emotional Exhaustion, but not Depersonalisation, and promoted Personal Accomplishment [ 43 ]. Transformational leadership predicted positive work environments, which in turn predicted lower burnout (composite score) [ 44 ]. Positive leadership affected Emotional Exhaustion and Depersonalisation [ 56 ] and burnout measured with a non-validated scale [ 20 ].
Teamwork and social support were also explored. Co-worker cohesion was only related to Depersonalisation [ 58 ]; team collaboration problems predicted negative scores on all MBI subscales [ 38 ], and workplace support protected from Emotional Exhaustion [ 72 ]. Similarly, support received from peers had a protective effect on Emotional Exhaustion [ 60 ]. Collegial support was related to Emotional Exhaustion and Personal Accomplishment [ 39 ], and colleague support protected from burnout [ 67 ]. Interpersonal conflict affected Emotional Exhaustion through role conflict, but co-worker support had no effect on any burnout dimensions [ 41 ], and similarly, co-worker incivility predicted Emotional Exhaustion [ 31 ], and so did bullying [ 88 ]. Poor team communication was associated with all MBI dimensions [ 40 ], staff issues predicted burnout measured with a composite score [ 73 ], and so did verbal violence from colleagues [ 68 ]. One study found that seeking social support was not associated with any of the burnout dimensions, while another study found that low social support predicted Emotional Exhaustion [ 37 ], and social support was associated with lower Emotional Exhaustion and higher Personal Accomplishment [ 21 ]. Vidotti et al. found an association between low social support and all MBI dimensions [ 62 ].
Work environment and hospital characteristics
Eleven studies were considering the work environment measured with the PES-NWI scale [ 91 ], where higher scores indicate positive work environments. Five studies comprising diverse samples and settings concluded that the better rated the work environment, the lower the likelihood of experiencing Emotional Exhaustion [ 32 , 47 , 49 , 51 , 92 ], and four studies found the same relationship, but on both Emotional Exhaustion and Depersonalisation [ 50 , 66 , 93 , 94 ]; only one study concluded there is an association between work environment and all MBI dimensions [ 95 ]. Negative work environments affected burnout (measured with a composite score) via job dissatisfaction [ 96 ]. One study looked at organisational characteristics on a single scale and found that a higher rating of organisational characteristics predicted lower Emotional Exhaustion [ 82 ]. Environmental uncertainty was related to all MBI dimensions [ 86 ].
Structural empowerment was also considered in relation to burnout: high structural empowerment led to lower Emotional Exhaustion and Cynicism via staffing levels and worklife interference [ 54 ]; in a study using a similar methodology, structural empowerment affected Emotional Exhaustion via Areas of Worklife [ 29 ]. The relationship between Emotional Exhaustion and Cynicism was moderated by organisational empowerment [ 40 ], and organisational support had a protective effect on burnout [ 67 ]. Hospital management and organisational support had a direct effect on Emotional Exhaustion and Personal Accomplishment [ 84 ]. Trust in the organisation predicted lower levels of Emotional Exhaustion [ 82 ] and of burnout measured with a composite MBI score [ 87 ].
Three studies considered whether policy involvement had an effect on burnout. Two studies on the same sample found that having the opportunity to participate in policy decisions was associated with reduced burnout (all subscales) [ 57 , 85 ], and one study did not report results for the association [ 20 ]. Emotional Exhaustion mediated the relationship between nurses’ participation in hospital affairs and their intention to leave the job [ 97 ]; a further study did not found an association between participation in hospital affairs and Emotional Exhaustion, but only with Personal Accomplishment [ 50 ]. Lastly, one study investigated participation in research groups and concluded it was associated with reduced burnout measured with a composite score [ 76 ].
There was an association between opportunity for career advancement and all MBI dimensions [ 77 ]; however, another study found that having promotion opportunities was not related to burnout [ 79 ]. Moloney et al. found that professional development was not related to burnout [ 67 ]. Two studies considered pay. In one study, no effect was found on any MBI dimension [ 73 ], and a very small study ( n = 78 nurses) reported an effect of satisfaction with pay on Emotional Exhaustion and Depersonalisation [ 34 ]. Job insecurity predicted Depersonalisation and PA [ 79 ].
When the hospital adopted nursing models of care rather than medical models of care, nurses were more likely to report high levels of Personal Accomplishment [ 57 , 85 ]. However, another study found no significant relationship [ 20 ]. Regarding ward and hospital type, Aiken and Sloane found that RNs working in specialised AIDS units reported lower levels of Emotional Exhaustion [ 98 ]; however, ward type was not found to be significantly associated with burnout in a study on temporary nurses [ 53 ]. Working in different ward settings was not associated with burnout, but working in hospitals as opposed to in primary care was associated with lower Emotional Exhaustion [ 71 ]. Working in a small hospital was associated with a lower likelihood of Emotional Exhaustion, when compared to working in a community hospital [ 63 ]. Faller’s study also concluded that working in California was a significant predictor of reduced burnout.
When the hospitals’ investment in the quality of care was considered, one study found that having foundations for quality of care was associated with reduced Emotional Exhaustion only [ 50 ], but in another study, foundations for quality of care were associated with all MBI dimensions [ 83 ]. Working in a Magnet hospital was not associated with burnout [ 53 ].
In summary, having a positive work environment (generally work environments scoring higher on the PES-NWI scale) was associated with reduced Emotional Exhaustion, and so was higher structural empowerment. However, none of the organisational characteristics at the hospital level was consistently associated with burnout.
Staff outcomes and job performance
Nineteen studies considered the impact of burnout on intention to leave. Two studies found that Emotional Exhaustion and Cynicism had a direct effect on turnover intentions [ 28 , 99 ], and four studies reported that only Emotional Exhaustion affected intentions to leave the job [ 21 , 32 , 37 , 100 ], with one of these indicating that Emotional Exhaustion affected also intention to leave the organisation [ 32 ], but one study did not replicate such findings [ 101 ] and concluded that only Cynicism was associated with intention to leave the job and nursing. Similarly, one study found that Cynicism was directly related to intention to leave [ 35 ]. A further study found that Emotional Exhaustion affected turnover intentions via job satisfaction [ 88 ], and one article reported that Emotional Exhaustion mediated the effect of authentic leadership on intention to leave [ 89 ]. Emotional Exhaustion was a mediator between nurses’ involvement with decisions and intention to leave the organisation [ 97 ]. Burnout measured on a composite score was associated with a higher intention to leave [ 96 ]. Laeeque et al. reported that burnout, captured with CBI, related to intention to leave [ 81 ]; Estryn-Behar et al. used the same scale to measure burnout and found that high burnout was associated with higher intention to leave in all countries, except for Slovakia [ 102 ]. Burnout, measured with the Malach-Pines Scale, was associated with intention to quit, and stronger associations were found for nurses who had higher perceptions of organisational politics [ 103 ]. Burnout (Malach-Pines Scale) predicted both the intention to leave the job and nursing [ 67 ]. Three studies investigated the relationship between burnout and intention to leave; one of these aggregated all job outcomes in a single variable (i.e. job satisfaction, intention to leave the hospital, applied for another job, and intention to leave nursing) and reported that Depersonalisation and Personal Accomplishment predict job outcomes [ 84 ]; they replicated a similar approach and found the same associations [ 36 ]. They later found that all MBI dimensions were associated with leaving the nursing profession [ 104 ]. Only one study in a sample of 106 nurses from one hospital found an association between Depersonalisation and turnover within 2 years [ 105 ].
Two studies looked at the effect of burnout on job performance: one found a negative association between burnout (measured with CBI) and both task performance and contextual performance [ 106 ]. Only Emotional Exhaustion was associated with self-rated and supervisor-rated job performance of 73 RNs [ 21 ]. Missed care was investigated in three studies, and it was found to be both predictor of Emotional Exhaustion [ 32 ], an outcome of burnout [ 20 , 103 ].
Four studies considered sickness absence. When RNs had high levels of Emotional Exhaustion, they were more likely to experience short-term sickness absence (i.e. 1–10 days of absence), which was obtained from hospital administrative records. Similarly, Emotional Exhaustion was associated with seven or more days of absence in a longitudinal study [ 105 ]. Emotional Exhaustion was significantly associated with reported mental health absenteeism, but not reported physical health absenteeism, and sickness absence from administrative records [ 21 ]. One study did not find any meaningful relationships between burnout and absenteeism [ 107 ].
Emotional Exhaustion was a significant predictor of general health [ 73 ], and in a further study, both Emotional Exhaustion and Personal Accomplishment were associated with perceived health [ 70 ]. Final-year nursing students who experienced health issues were more likely to develop high burnout when entering the profession [ 26 ]. When quality of sleep was treated both as a predictor and outcome of burnout, relationships were found in both instances [ 106 ].
Focussing on mental health, one study found that burnout predicted mental health problems for newly qualified nurses [ 30 ], and Emotional Exhaustion and Cynicism predicted somatisation [ 42 ]. Depressive symptoms were predictive of Emotional Exhaustion and Depersonalisation, considering therefore depression as a predictor of burnout [ 108 ]. Rudman and Gustavsson also found that having depressive mood and depressive episodes were common features of newly qualified nurses who developed or got worse levels of burnout throughout their first years in the profession [ 26 ]. Tourigny et al. considered depression as a predictor and found it was significantly related to Emotional Exhaustion [ 107 ].
Eleven studies considered job satisfaction: of these, three treated job satisfaction as a predictor of burnout and concluded that higher levels of job satisfaction were associated with a lower level of composite burnout scores [ 52 , 96 ] and all MBI dimensions [ 94 ]. According to two studies, Emotional Exhaustion and Cynicism predicted job dissatisfaction [ 54 , 101 ], while four studies reported that Emotional Exhaustion only was associated with increased odds to report job dissatisfaction [ 73 , 82 , 88 , 100 ]; one study reported that Cynicism only was associated with job dissatisfaction [ 99 ]. Rouxel et al. did not find support in their hypothesised model that Emotional Exhaustion and Depersonalisation predicted job satisfaction [ 64 ].
In summary, considering 39 studies, there is conflicting evidence on the direction of the relationship between burnout and missed care, mental health, and job satisfaction. An association between burnout and intention to leave was found, although only one small study reported an association between burnout and turnover. A moderate relationship was found for the effect of burnout on sickness absence, job performance, and general health.
Patient care and outcomes
Among the patient outcomes of burnout, quality of care was investigated by eight studies. Two studies in diverse samples and settings reported that high Emotional Exhaustion, high Depersonalisation, and low Personal Accomplishment were associated with poor quality of care [ 109 , 110 ], but one study found that only Personal Accomplishment was related to better quality of care at the last shift [ 104 ]; Emotional Exhaustion and Cynicism predict low quality of care [ 54 ]; two articles reported that Emotional Exhaustion predicts poor nurse ratings of quality of care [ 82 , 84 ]. A high burnout composite score predicted poor nurse-assessed quality of care [ 96 ]. In one instance, no associations were found between any of the burnout dimensions and quality of care [ 36 ].
Five studies considered aspects of patient safety: burnout was correlated with negative patient safety climate [ 111 ]. Emotional Exhaustion and Depersonalisation were both associated with negative patient safety grades and safety perceptions [ 112 ], and burnout fully mediated the relationship between depression and individual-level safety perceptions and work area/unit level safety perceptions [ 108 ]. Emotional Exhaustion mediated the relationship between workload and patient safety [ 51 ], and a higher composite burnout score was associated with lower patient safety ratings [ 113 ].
Regarding adverse events, high DEP and low Personal Accomplishment predicted a higher rate of adverse events [ 85 ], but in another study, only Emotional Exhaustion predicted adverse events [ 51 ]. When nurses were experiencing high levels of Emotional Exhaustion, they were less likely to report near misses and adverse events, and when they were experiencing high levels of Depersonalisation, they were less likely to report near misses [ 112 ].
All three MBI dimensions predicted medication errors in one study [ 109 ], but Van Bogaert et al. found that only high levels of Depersonalisation were associated with medication errors [ 104 ]. High scores in Emotional Exhaustion and Depersonalisation predicted infections [ 109 ]. Cimiotti et al. found that Emotional Exhaustion was associated with catheter-associated urinary tract infections and surgical site infections [ 114 ], while in another study, Depersonalisation was associated with nosocomial infections [ 104 ]. Lastly, patient falls were also explored, and Depersonalisation and low Personal Accomplishment were significant predictors in one study [ 109 ], while in a further study, only Depersonalisation was associated with patient falls [ 104 ]. There was no association between burnout and hospital-acquired pressure ulcers [ 20 ].
Considering patient experience, Vahey et al. concluded that higher Emotional Exhaustion and low Personal Accomplishment levels were associated with patient dissatisfaction [ 93 ], and Van Bogaert et al. found that Emotional Exhaustion was related to patient and family verbal abuse, and Depersonalisation was related to both patient and family verbal abuse and patient and family complaints [ 104 ].
In summary, evidence deriving from 17 studies points to a negative effect of burnout on quality of care, patient safety, adverse events, error reporting, medication error, infections, patient falls, patient dissatisfaction, and family complaints, but not on pressure ulcers.
Individual characteristics
In total, 16 studies, which had examined work characteristics related to burnout, also considered the relationship between characteristics of the individual and burnout. Relationships were tested on demographic variables, including gender, age, and family status; on personality aspects; on work-life interference; and on professional attributes including length of experience and educational level. Because our focus on burnout is as a job-related phenomenon, we have not reported results of these studies into detail, but overall evidence on demographic and personality factors was inconclusive, and having family issues and high work-life interference was associated with different burnout dimensions. Being younger and not having a bachelor’s degree were found to be associated with a higher incidence of burnout.
This review aimed to identify research that had examined theorised relationships with burnout, in order to determine what is known (and not known) about the factors associated with burnout in nursing and to determine the extent to which studies have been underpinned by, and/or have supported or refuted, theories of burnout. We found that the associations hypothesised by Maslach’s theory between mismatches in areas of worklife and burnout were generally supported.
Research consistently found that adverse job characteristics—high workload, low staffing levels, long shifts, low control, low schedule flexibility, time pressure, high job and psychological demands, low task variety, role conflict, low autonomy, negative nurse-physician relationship, poor supervisor/leader support, poor leadership, negative team relationship, and job insecurity—were associated with burnout in nursing.
However few studies used all three MBI subscales in the way intended, and nine used different approaches to measuring burnout.
The field has been dominated by cross-sectional studies that seek to identify associations with one or two factors, rarely going beyond establishing correlation. Most studies were limited by their cross-sectional nature, the use of different or incorrectly applied burnout measures, the use of common methods (i.e. survey to capture both burnout and correlates), and omitted variables in the models. The 91 studies reviewed, while highlighting the importance of burnout as a feature affecting nurses and patient care, have generally lacked a theoretical approach, or identified mechanisms to test and develop a theory on the causes and consequences of burnout, but were limited in their testing of likely mechanisms due to cross-sectional and observational designs.
For example, 19 studies showed relationships between burnout and job satisfaction, missed care, and mental health. But while some studies treated these as predictors of burnout, others handled as outcomes of burnout. This highlights a further issue that characterises the burnout literature in nursing: the simultaneity bias, due to the cross-sectional nature of the evidence. The inability to establish a temporal link means limits the inference of causality [ 115 ]. Thus, a factor such as ‘missed care’ could lead to a growing sense of compromise and ‘crushed ideals’ in nurses [ 116 ], which causes burnout. Equally, it could be that job performance of nurses experiencing burnout is reduced, leading to increased levels of ‘missed care’. Both are plausible in relation to Maslach’s original theory of burnout, but research is insufficient to determine which is most likely, and thereby develop the theory.
To help address this, three areas of development within research are proposed. Future research adopting longitudinal designs that follow individuals over time would improve the potential to understand the direction of the relationships observed. Research using Maslach’s theory should use and report all three MBI dimensions; where only the Emotional Exhaustion subscale is used, this should be explicit and it should not be treated as being synonymous to burnout. Finally, to move our theoretical understanding of burnout forward, research needs to prioritise the use of empirical data on employee behaviours (such as absenteeism, turnover) rather than self-report intentions or predictions.
Addressing these gaps would provide better evidence of the nature of burnout in nursing, what causes it and its potential consequences, helping to develop evidence-based solutions and motivate work-place change. With better insight, health care organisations can set about reducing the negative consequences of having patient care provided by staff whose work has led them to become emotionally exhausted, detached, and less able to do the job, that is, burnout.
Limitations
Our theoretical review of the literature aimed to summarise information from a large quantity of studies; this meant that we had to report studies without describing their context in the text and also without providing estimates (i.e. ORs and 95% CIs). In appraising studies, we did not apply a formal quality appraisal instrument, although we noted key omissions of important details. However, the results of the review serve to illustrate the variety of factors that may influence/result from burnout and demonstrate where information is missing. We did not consider personality and other individual variables when extracting data from studies. However, Maslach and Leiter recently reiterated that although some connections have been made between burnout and personality characteristics, the evidence firmly points towards work characteristics as the primary drivers of burnout [ 8 ].
While we used a reproducible search strategy searching MEDLINE, CINAHL, and PsycINFO, it is possible that there are studies indexed elsewhere and we did not identify them, and we did not include grey literature. It seems unlikely that these exist in sufficient quantity to substantively change our conclusions.
Patterns identified across 91 studies consistently show that adverse job characteristics are associated with burnout in nursing. The potential consequences for staff and patients are severe. Maslach’s theory offers a plausible mechanism to explain the associations observed. However incomplete measurement of burnout and limited research on some relationships means that the causes and consequences of burnout cannot be reliably identified and distinguished, which makes it difficult to use the evidence to design interventions to reduce burnout.

Availability of data and materials
Not applicable
Abbreviations
- Maslach Burnout Inventory
Copenhagen Burnout Inventory
Professional Quality of Life Measure
Dall’Ora C, Ball J, Recio-Saucedo A, Griffiths P. Characteristics of shift work and their impact on employee performance and wellbeing: a literature review. Int J Nurs Stud. 2016;57:12–27.
Article PubMed Google Scholar
Griffiths P, Ball J, Drennan J, Dall’Ora C, Jones J, Maruotti A, et al. Nurse staffing and patient outcomes: Strengths and limitations of the evidence to inform policy and practice. A review and discussion paper based on evidence reviewed for the National Institute for Health and Care Excellence Safe Staffing guideline development. Int J Nurs Stud. 2016;63:213–25.
Cummings GG, MacGregor T, Davey M, Lee H, Wong CA, Lo E, et al. Leadership styles and outcome patterns for the nursing workforce and work environment: a systematic review. Int J Nurs Stud. 2010;47(3):363–85.
Rafferty AM, Ball J, Aiken LH. Are teamwork and professional autonomy compatible, and do they result in improved hospital care? Qual Health Care. 2001;10(suppl 2):ii32-iii7.
Freudenberger HJ. Staff burn-out. J Soc Issues. 1974;30(1):159–65.
Article Google Scholar
Maslach C, Jackson SE. The measurement of experienced burnout. J Occup Behav. 1981;2(2):99–113.
Maslach C. A Multidimensional theory of burnout. In: Cooper CL, editor. Theories of Organizational Stress Oxford University Press Inc.; 1999.
Maslach C, Leiter M. Burnout. Fink G, editor. London, UK: Academic Press; 2016. 351-7 p.
Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52(1):397–422.
Article CAS PubMed Google Scholar
Ekstedt M. Burnout and sleep: Institutionen för folkhälsovetenskap/Department of Public Health Sciences; 2005.
Google Scholar
Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands-resources model of burnout. J Appl Psychol. 2001;86(3):499.
Schaufeli WB, Leiter MP, Maslach C. Burnout: 35 years of research and practice. Career Dev Int. 2009;14(2-3):204–20.
Cherniss C. Burnout in new professionals: a long-term follow-up study. J Health Hum Resour Adm. 1989;12(1):11–24.
Gustavsson JP, Hallsten L, Rudman A. Early career burnout among nurses: modelling a hypothesized process using an item response approach. Int J Nurs Stud. 2010;47(7):864–75.
Shirom A. Job-related burnout: a review. Handbook of occupational health psychology. Washington, DC, US: American Psychological Association; 2003. p. 245-264.
Melamed S, Kushnir T, Shirom A. Burnout and risk factors for cardiovascular diseases. Behav Med. 1992;18(2):53–60.
Campbell M, Egan M, Lorenc T, Bond L, Popham F, Fenton C, et al. Considering methodological options for reviews of theory: illustrated by a review of theories linking income and health. Syst Rev. 2014;3(1):114.
Article PubMed PubMed Central Google Scholar
Pare G, Trudel MC, Jaana M, Kitsiou S. Synthesizing information systems knowledge: a typology of literature reviews. Inf Manag. 2015;52(2):183–99.
Lavoie P, Michaud C, Bélisle M, Boyer L, Gosselin É, Grondin M, et al. Learning theories and tools for the assessment of core nursing competencies in simulation: a theoretical review. J Adv Nurs. 2018;74(2):239–50.
Thompson D. The examination of practice environment, burnout, and missed care on pressure ulcer prevalence rates using a complexity science framework: University of Kansas; 2014.
Parker PA, Kulik JA. Burnout, self- and supervisor-rated job performance, and absenteeism among nurses. J Behav Med. 1995;18(6):581–99.
Maslach C, Jackson SE, Leiter M. Maslach burnout inventory manual. 3rd ed. ed: Mind Garden, Inc.; 2010.
Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work Stress. 2005;19(3):192–207.
Malach-Pines A. The burnout measure, short version. Int J Stress Manag. 2005;12(1):78–88.
Hunsaker S, Chen HC, Maughan D, Heaston S. Factors that influence the development of compassion fatigue, burnout, and compassion satisfaction in emergency department nurses. J Nurs Scholarsh. 2015;47(2):186–94.
Rudman A, Gustavsson JP. Early-career burnout among new graduate nurses: a prospective observational study of intra-individual change trajectories. Int J Nurs Stud. 2011;48(3):292–306.
Leiter MP, Maslach C. Areas of worklife survey manual. Centre for Organizational Research and Development, Acadia University, Wolfville. 2006.
Boamah SA, Laschinger H. The influence of areas of worklife fit and work-life interference on burnout and turnover intentions among new graduate nurses. J Nurs Manag. 2016;24(2):E164–74.
Greco P, Laschinger HK, Wong C. Leader empowering behaviours, staff nurse empowerment and work engagement/burnout. Nurs Leadersh (Tor Ont). 2006;19(4):41–56.
Laschinger HK, Borgogni L, Consiglio C, Read E. The effects of authentic leadership, six areas of worklife, and occupational coping self-efficacy on new graduate nurses’ burnout and mental health: a cross-sectional study. Int J Nurs Stud. 2015;52(6):1080–9.
Laschinger HK, Read EA. The effect of authentic leadership, person-job fit, and civility norms on new graduate nurses’ experiences of coworker incivility and burnout. J Nurs Adm. 2016;46(11):574–80.
Flynn L, Thomas-Hawkins C, Clarke SP. Organizational traits, care processes, and burnout among chronic hemodialysis nurses. West J Nurs Res. 2009;31(5):569–82.
Kowalski C, Ommen O, Driller E, Ernstmann N, Wirtz MA, Kohler T, et al. Burnout in nurses - the relationship between social capital in hospitals and emotional exhaustion. J Clin Nurs. 2010;19(11-12):1654–63.
Konstantinou AK, Bonotis K, Sokratous M, Siokas V, Dardiotis E. Burnout evaluation and potential predictors in a Greek cohort of mental health nurses. Arch Psychiatr Nurs. 2018;32(3):449–56.
Leiter MP, Maslach C. Nurse turnover: the mediating role of burnout. J Nurs Manag. 2009;17(3):331–9.
Van Bogaert P, Kowalski C, Weeks SM, Van Heusden D, Clarke SP. The relationship between nurse practice environment, nurse work characteristics, burnout and job outcome and quality of nursing care: a cross-sectional survey. Int J Nurs Stud. 2013;50(12):1667–77.
Janssen PP, Jonge JD, Bakker AB. Specific determinants of intrinsic work motivation, burnout and turnover intentions: a study among nurses. J Adv Nurs. 1999;29(6):1360–9.
Andela M, Truchot D, Van der Doef M. Job stressors and burnout in hospitals: the mediating role of emotional dissonance. Int J Stress Manag. 2016;23(3):298–317.
Levert T, Lucas M, Ortlepp K. Burnout in psychiatric nurses: contributions of the work environment and a Sense of Coherence. S Afr J Psychol. 2000;30(2):36–43.
Galletta M, Portoghese I, Ciuffi M, Sancassiani F, Aloja E, Campagna M. Working and environmental factors on job burnout: a cross-sectional study among nurses. Clin Pract Epidemiol Ment Health. 2016;12:132–41.
Kitaoka-Higashiguchi K. Burnout as a developmental process among Japanese nurses: investigation of Leiter’s model. Jpn J Nurs Sci. 2005;2(1):9–16.
Greenglass ER, Burke RJ, Fiksenbaum L. Workload and burnout in nurses. J Community Appl Soc Psychol. 2001;11(3):211–5.
Madathil R, Heck NC, Schuldberg D. Burnout in psychiatric nursing: examining the interplay of autonomy, leadership style, and depressive symptoms. Arch Psychiatr Nurs. 2014;28(3):160–6.
Lewis HS, Cunningham CJ. Linking nurse leadership and work characteristics to nurse burnout and engagement. Nurs Res. 2016;65(1):13–23.
Lu M, Ruan H, Xing W, Hu Y. Nurse burnout in China: a questionnaire survey on staffing, job satisfaction, and quality of care. J Nurs Manag. 2015;23(4):440–7.
Dhaini SR, Denhaerynck K, Bachnick S, Schwendimann R, Schubert M, De Geest S, et al. Work schedule flexibility is associated with emotional exhaustion among registered nurses in Swiss hospitals: a cross-sectional study. Int J Nurs Stud. 2018;82:99–105.
Aiken LH, Clarke SP, Sloane DM, Lake ET, Cheney T. Effects of hospital care environment on patient mortality and nurse outcomes. J Nurs Adm. 2008;38(5):223–9.
Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–93.
Zhou W, He G, Wang H, He Y, Yuan Q, Liu D. Job dissatisfaction and burnout of nurses in Hunan, China: A cross-sectional survey. Nurs Health Sci. 2015;17(4):444–50.
Hanrahan NP, Aiken LH, McClaine L, Hanlon AL. Relationship between psychiatric nurse work environments and nurse burnout in acute care general hospitals. Issues Ment Health Nurs. 2010;31(3):198–207.
Liu X, Zheng J, Liu K, Baggs JG, Liu J, Wu Y, et al. Hospital nursing organizational factors, nursing care left undone, and nurse burnout as predictors of patient safety: a structural equation modeling analysis. Int J Nurs Stud. 2018;86:82–9.
Akman O, Ozturk C, Bektas M, Ayar D, Armstrong MA. Job satisfaction and burnout among paediatric nurses. J Nurs Manag. 2016;24(7):923–33.
Faller MS, Gates MG, Georges JM, Connelly CD. Work-related burnout, job satisfaction, intent to leave, and nurse-assessed quality of care among travel nurses. J Nurs Adm. 2011;41(2):71–7.
Boamah SA, Read EA, Spence Laschinger HK. Factors influencing new graduate nurse burnout development, job satisfaction and patient care quality: a time-lagged study. J Adv Nurs. 2017;73(5):1182–95.
Kanai-Pak M, Aiken LH, Sloane DM, Poghosyan L. Poor work environments and nurse inexperience are associated with burnout, job dissatisfaction and quality deficits in Japanese hospitals. J Clin Nurs. 2008;17(24):3324–9.
Leineweber C, Westerlund H, Chungkham HS, Lindqvist R, Runesdotter S, Tishelman C. Nurses’ practice environment and work-family conflict in relation to burn out: a multilevel modelling approach. PLoS One. 2014;9(5):e96991.
Article PubMed PubMed Central CAS Google Scholar
Leiter MP, Spence Laschinger HK. Relationships of work and practice environment to professional burnout: testing a causal model. Nurs Res. 2006;55(2):137–46.
Adali E, Priami M, Evagelou H, Mougia V, Ifanti M, Alevizopoulos G. Burnout in psychiatric nursing personnel in Greek hospitals. European Journal of Psychiatry. 2003;17(3):173–81.
Cao X, Naruse T. Effect of time pressure on the burnout of home-visiting nurses: the moderating role of relational coordination with nursing managers. Jpn J Nurs Sci. 2019;16(2):221–31.
Jansen PG, Kerkstra A, Abu-Saad HH, van der Zee J. The effects of job characteristics and individual characteristics on job satisfaction and burnout in community nursing. Int J Nurs Stud. 1996;33(4):407–21.
Gandi JC, Wai PS, Karick H, Dagona ZK. The role of stress and level of burnout in job performance among nurses. Ment Health Fam Med. 2011;8(3):181–94.
PubMed PubMed Central Google Scholar
Vidotti V, Ribeiro RP, Galdino MJQ, Martins JT. Burnout syndrome and shift work among the nursing staff. Rev Lat Am Enfermagem. 2018;26:e3022.
Shamian J, Kerr MS, Laschinger HK, Thomson D. A hospital-level analysis of the work environment and workforce health indicators for registered nurses in Ontario’s acute-care hospitals. Can J Nurs Res. 2002;33(4):35–50.
CAS PubMed Google Scholar
Rouxel G, Michinov E, Dodeler V. The influence of work characteristics, emotional display rules and affectivity on burnout and job satisfaction: a survey among geriatric care workers. Int J Nurs Stud. 2016;62:81–9.
Colindres CV, Bryce E, Coral-Rosero P, Ramos-Soto RM, Bonilla F, Yassi A. Effect of effort-reward imbalance and burnout on infection control among Ecuadorian nurses. Int Nurs Rev. 2018;65(2):190–9.
Shao J, Tang L, Wang X, Qiu R, Zhang Y, Jia Y, et al. Nursing work environment, value congruence and their relationships with nurses’ work outcomes. J Nurs Manag. 2018;26(8):1091–9.
Moloney W, Boxall P, Parsons M, Cheung G. Factors predicting registered nurses’ intentions to leave their organization and profession: a job demands-resources framework. J Adv Nurs. 2018;74(4):864–75.
Anwar MM, Elareed HR. Burnout among Egyptian nurses. Journal of Public Health-Heidelberg. 2017;25(6):693–7.
Wisetborisut A, Angkurawaranon C, Jiraporncharoen W, Uaphanthasath R, Wiwatanadate P. Shift work and burnout among health care workers. Occup Med (Lond). 2014;64(4):279–86.
Article CAS Google Scholar
Ilhan MN, Durukan E, Taner E, Maral I, Bumin MA. Burnout and its correlates among nursing staff: questionnaire survey. J Adv Nurs. 2008;61(1):100–6.
Canadas-De la Fuente GA, Vargas C, San Luis C, Garcia I, Canadas GR, De la Fuente EI. Risk factors and prevalence of burnout syndrome in the nursing profession. Int J Nurs Stud. 2015;52(1):240–9.
Bagheri Hosseinabadi M, Ebrahimi MH, Khanjani N, Biganeh J, Mohammadi S, Abdolahfard M. The effects of amplitude and stability of circadian rhythm and occupational stress on burnout syndrome and job dissatisfaction among irregular shift working nurses. J Clin Nurs. 2019;28(9-10):1868–78.
Khamisa N, Peltzer K, Ilic D, Oldenburg B. Work related stress, burnout, job satisfaction and general health of nurses: a follow-up study. Int J Nurs Pract. 2016;22(6):538–45.
Dall’Ora C, Griffiths P, Ball J, Simon M, Aiken LH. Association of 12 h shifts and nurses’ job satisfaction, burnout and intention to leave: findings from a cross-sectional study of 12 European countries. BMJ Open. 2015;5(9):e008331.
Stimpfel AW, Sloane DM, Aiken LH. The longer the shifts for hospital nurses, the higher the levels of burnout and patient dissatisfaction. Health Aff (Millwood). 2012;31(11):2501–9.
Poncet MC, Toullic P, Papazian L, Kentish-Barnes N, Timsit JF, Pochard F, et al. Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med. 2007;175(7):698–704.
Stone PW, Du Y, Gershon RR. Organizational climate and occupational health outcomes in hospital nurses. J Occup Environ Med. 2007;49(1):50–8.
Bourbonnais R, Comeau M, Vezina M, Dion G. Job strain, psychological distress, and burnout in nurses. Am J Ind Med. 1998;34(1):20–8.
Basinska BA, Wilczek-Ruzyczka E. The role of rewards and demands in burnout among surgical nurses. Int J Occup Med Environ Health. 2013;26(4):593–604.
Garcia-Sierra R, Fernandez-Castro J, Martinez-Zaragoza F. Relationship between job demand and burnout in nurses: does it depend on work engagement? J Nurs Manag. 2016;24(6):780–8.
Laeeque SH, Bilal A, Babar S, Khan Z, Rahman SU. How patient-perpetrated workplace violence leads to turnover intention among nurses: the mediating mechanism of occupational stress and burnout. J Aggress Maltreat Trauma. 2018;27(1):96–118.
Laschinger HKS, Shamian J, Thomson D. Impact of magnet hospital characteristics on nurses’ perceptions of trust, burnout, quality of care, and work satisfaction. Nurs Econ. 2001;19(5):209–19.
Li B, Bruyneel L, Sermeus W, Van den Heede K, Matawie K, Aiken L, et al. Group-level impact of work environment dimensions on burnout experiences among nurses: a multivariate multilevel probit model. Int J Nurs Stud. 2013;50(2):281–91.
Van Bogaert P, Meulemans H, Clarke S, Vermeyen K, Van de Heyning P. Hospital nurse practice environment, burnout, job outcomes and quality of care: test of a structural equation model. J Adv Nurs. 2009;65(10):2175–85.
Laschinger HKS, Leiter MP. The impact of nursing work environments on patient safety outcomes - the mediating role of burnout/engagement. J Nurs Adm. 2006;36(5):259–67.
Garrett DK, McDaniel AM. A new look at nurse burnout: the effects of environmental uncertainty and social climate. J Nurs Adm. 2001;31(2):91–6.
Bobbio A, Bellan M, Manganelli AM. Empowering leadership, perceived organizational support, trust, and job burnout for nurses: a study in an Italian general hospital. Health Care Manag Rev. 2012;37(1):77–87.
Spence Laschinger HK, Wong CA, Grau AL. The influence of authentic leadership on newly graduated nurses’ experiences of workplace bullying, burnout and retention outcomes: a cross-sectional study. Int J Nurs Stud. 2012;49(10):1266–76.
Lee HF, Chiang HY, Kuo HT. Relationship between authentic leadership and nurses’ intent to leave: the mediating role of work environment and burnout. J Nurs Manag. 2019;27(1):52–65.
Kanste O, Kyngas H, Nikkila J. The relationship between multidimensional leadership and burnout among nursing staff. J Nurs Manag. 2007;15(7):731–9.
Lake ET. Development of the practice environment scale of the Nursing Work Index. Res Nurs Health. 2002;25(3):176–88.
Nantsupawat A, Kunaviktikul W, Nantsupawat R, Wichaikhum OA, Thienthong H, Poghosyan L. Effects of nurse work environment on job dissatisfaction, burnout, intention to leave. Int Nurs Rev. 2017;64(1):91–8.
Vahey DC, Aiken LH, Sloane DM, Clarke SP, Vargas D. Nurse burnout and patient satisfaction. Med Care. 2004;42(2 Suppl):II57–66.
Klopper HC, Coetzee SK, Pretorius R, Bester P. Practice environment, job satisfaction and burnout of critical care nurses in South Africa. J Nurs Manag. 2012;20(5):685–95.
Zhang LF, You LM, Liu K, Zheng J, Fang JB, Lu MM, et al. The association of Chinese hospital work environment with nurse burnout, job satisfaction, and intention to leave. Nurs Outlook. 2014;62(2):128–37.
Liu Y, Aungsuroch Y. Factors influencing nurse-assessed quality nursing care: a cross-sectional study in hospitals. J Adv Nurs. 2018;74(4):935–45.
Marques-Pinto A, Jesus EH, Mendes A, Fronteira I, Roberto MS. Nurses’ intention to leave the organization: a mediation study of professional burnout and engagement. Span J Psychol. 2018;21:E32.
Aiken LH, Sloane DM. Effects of organizational innovations in AIDS care on burnout among urban hospital nurses. Work Occup. 1997;24(4):453–77.
Spence Laschinger HK, Leiter M, Day A, Gilin D. Workplace empowerment, incivility, and burnout: impact on staff nurse recruitment and retention outcomes. J Nurs Manag. 2009;17(3):302–11.
Dutra HS, Cimiotti JP, Guirardello EB. Nurse work environment and job-related outcomes in Brazilian hospitals. Appl Nurs Res. 2018;41:68–72.
Laschinger HK. Job and career satisfaction and turnover intentions of newly graduated nurses. J Nurs Manag. 2012;20(4):472–84.
Estryn-Behar M, Van der Heijden BI, Oginska H, Camerino D, Le Nezet O, Conway PM, et al. The impact of social work environment, teamwork characteristics, burnout, and personal factors upon intent to leave among European nurses. Med Care. 2007;45(10):939–50.
Basar U, Basim N. A cross-sectional survey on consequences of nurses’ burnout: moderating role of organizational politics. J Adv Nurs. 2016;72(8):1838–50.
Van Bogaert P, Timmermans O, Weeks SM, van Heusden D, Wouters K, Franck E. Nursing unit teams matter: impact of unit-level nurse practice environment, nurse work characteristics, and burnout on nurse reported job outcomes, and quality of care, and patient adverse events--a cross-sectional survey. Int J Nurs Stud. 2014;51(8):1123–34.
Firth H, Britton P. Burnout, absence and turnover amongst British nursing staff. J Occup Psychol. 1989;62(1):55–9.
Giorgi F, Mattei A, Notarnicola I, Petrucci C, Lancia L. Can sleep quality and burnout affect the job performance of shift-work nurses? A hospital cross-sectional study. J Adv Nurs. 2018;74(3):698–708.
Tourigny L, Baba VV, Wang XY. Burnout and depression among nurses in Japan and China: the moderating effects of job satisfaction and absence. Int J Hum Resour Manag. 2010;21(15):2741–61.
Johnson J, Louch G, Dunning A, Johnson O, Grange A, Reynolds C, et al. Burnout mediates the association between depression and patient safety perceptions: a cross-sectional study in hospital nurses. J Adv Nurs. 2017;73(7):1667–80.
Nantsupawat A, Nantsupawat R, Kunaviktikul W, Turale S, Poghosyan L. Nurse burnout, nurse-reported quality of care, and patient outcomes in Thai hospitals. J Nurs Scholarsh. 2016;48(1):83–90.
Poghosyan L, Clarke SP, Finlayson M, Aiken LH. Nurse burnout and quality of care: cross-national investigation in six countries. Res Nurs Health. 2010;33(4):288–98.
Zarei E, Khakzad N, Reniers G, Akbari R. On the relationship between safety climate and occupational burnout in healthcare organizations. Saf Sci. 2016;89:1–10.
Halbesleben JR, Wakefield BJ, Wakefield DS, Cooper LB. Nurse burnout and patient safety outcomes: nurse safety perception versus reporting behavior. West J Nurs Res. 2008;30(5):560–77.
Teng CI, Shyu YI, Chiou WK, Fan HC, Lam SM. Interactive effects of nurse-experienced time pressure and burnout on patient safety: a cross-sectional survey. Int J Nurs Stud. 2010;47(11):1442–50.
Cimiotti JP, Aiken LH, Sloane DM, Wu ES. Nurse staffing, burnout, and health care-associated infection. Am J Infect Control. 2012;40(6):486–90.
Antonakis J, Bendahan S, Jacquart P, Lalive R. On making causal claims: a review and recommendations. Leadersh Q. 2010;21(6):1086–120.
Maben J, Latter S, Clark JM. The sustainability of ideals, values and the nursing mandate: evidence from a longitudinal qualitative study. Nurs Inq. 2007;14(2):99–113.
Download references
Acknowledgements
We would like to thank Jane Lawless who performed the second screening of the provisionally included papers.
Author information
Authors and affiliations.
School of Health Sciences, and Applied Research Collaboration Wessex, Highfield Campus, University of Southampton, Southampton, SO17 1BJ, UK
Chiara Dall’Ora & Peter Griffiths
Department of Learning, Informatics, Management and Ethics, Karolinska Institutet, Tomtebodavägen 18a, 17177, Solna, Sweden
Jane Ball, Maria Reinius & Peter Griffiths
You can also search for this author in PubMed Google Scholar
Contributions
CDO led the paper write-up at all stages, designed and conducted the search strategy, completed the initial screening of papers, co-developed the coding frame, and applied the coding frame to all studies. JB conceived the review, co-developed the coding frame, applied the coding frame to all studies, and contributed substantially to drafting the paper at various stages. MR extracted all the data from studies and produced evidence tables. PG conceived the review and contributed substantially to the drafting of the paper at various stages. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Chiara Dall’Ora .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:.
MEDLINE via OVID, CINAHL with full text via EBSCO, and PsycINFO via EBSCO.
Additional file 2:
PRISMA-ScR Checklist.
Additional file 3:
Studies’ settings, sample sizes, burnout and correlates measurement, and appraisal of quality.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Dall’Ora, C., Ball, J., Reinius, M. et al. Burnout in nursing: a theoretical review. Hum Resour Health 18 , 41 (2020). https://doi.org/10.1186/s12960-020-00469-9
Download citation
Received : 04 December 2019
Accepted : 24 March 2020
Published : 05 June 2020
DOI : https://doi.org/10.1186/s12960-020-00469-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Job demands
- Practice environment
Human Resources for Health
ISSN: 1478-4491
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Call to +1 844 889-9952
Nursing Work Overload and Effect on Patient Safety
Introduction, nature of the problem, the settings where workload can be observed, effects of a nursing workload, significance of the study, video voice-over.
The primary role of the nurses is to provide an optimal care to both the inpatients and the outpatients. This form of a healthcare commitment within the highly sensitive areas often requires the nurses to remain alert and vigilant in the hospitals throughout their working durations (Carayon & Gurses, 2010). A constant problem that often threatens the safety of the patients and the concentration of the nurses is fatigue. Carayon and Gurses (2010) assert that one of the main contributing factors of nurse fatigue in a workplace is high nursing workload. This essay discusses the nature of high nursing workload, the setting in which nursing workload can be observed, its impact on the work environment and quality of care, and its impact on the patient outcomes as well as its research significance in the nursing practice.
Every work is tiring, and excess work is even more tiring. Hence, the size of a workload determines the level of fatigue. Several manageable deaths have occurred within the hospitals due to lapses in the nursing systems. According to Hughes (2001), the issue of high nursing workload has been a prevalent matter in most of the hospitals across America and in several parts of the world. A nursing work overload occurs when the nurses work on excess assignments and extra time due to understaffing, unstable work systems within the workplaces, or due to the worsened patients conditions (Hughes, 2001). A recent American research on the issues of nursing workload and patient safety revealed that the rapidly increasing national population and the patient population are overwhelming to the nurses (Carayon & Gurses, 2010). Hence, nurse workload increases with the number of patients.
In the nursing practice, a nursing workload can occur in various settings although four main scenarios can explain the manner in which a nursing workload can happen. In their recent study of the American Health Care System, Carayon and Gurses (2012) discovered that a nursing workload occurs within the unit levels, within the normal work levels, within the patient levels, and within the situational levels. The situational and patient levels are forms of workloads that form part of the job-level workload, while the job-level workload falls within the unit-level workload (Neill, 2012). This means that the problem of nursing workload is systemic and revolves around several issues such as hospital management, work arrangement, staffing, and healthcare infrastructure. Concerning emergencies, Hughes (2001) explains that nurses also face extreme pressure from the increasing numbers of patients that present serious issues.
A nursing workload affects almost all the parameters of healthcare because nurses form an important part of the healthcare system. In terms of its effect on the work environment, a nursing workload causes stress and fatigue, which are two major aspects that contribute to increased health risks, accidents, low work concentration, and practice lapses (Neill, 2012). Poor concentration at workplace, fatigue, depression, and stress, are factors that affect the mental and physical alertness of the nurses in their working environments. According to Neill (2012), the altered concentration of the nurses in the workplace affects the quality of care that the nurses can provide, and hence, the health outcomes of the patients remain affected. Hughes (2001) established that several American nurses that have contributed to unintended deaths, have faced unfair legal charges pertaining to contributory duty negligence.
In a study, Carayon and Gurses (2010) revealed that some deaths of patients are unnatural and unintended because they sometimes associate with workplace negligence. Nonetheless, so much remains unknown about the strenuous and frustrating workplace conditions of the nurses and the contribution of a nursing workload to a workplace stress (Carayon & Gurses, 2010). A nursing workload is a serious issue in the American Health Care System that needs a special attention in its research (Neill, 2012). Through giving an in-depth analysis of the issue of the nursing workload and the manner in which it affects the nursing practice within the healthcare centers, the nursing industry may reshape effectively. Practitioners and policymakers will definitely understand the vital issues that affect the nursing fraternity (Carayon & Gurses, 2010). They will also learn the manner in which they can formulate reformative policies.
Internationally, it is obvious that an acute nurse shortage seems to contribute to high nursing workloads. Nursing workload is a universal healthcare concern that seems to affects several health care centers across the world due to the overwhelming health situations, chronic health issues, nurse shortages, and poor management within the hospitals. Although the problem is eminent in several nations, there exist very few remedies for countering the problem. Nursing workload is actually a dangerous issue as it causes stress, depression, and fatigue, which are some of the major factors that affect the physical and mental alertness of the nurses in the workplaces. Several cases of deaths and injuries that involve the nurses in the hospitals are due to nursing workload, which seems to influence the behavior of the nurses in their work environments.
Updated: Jan 27th, 2024
Carayon, P., & Gurses, A. (2010). Chapter 30. Nursing Workload and Patient Safety—A Human Factors Engineering Perspective . Rockville, United States: Academic Press.
Hughes, R. (2001). Nursing workload: an unquantifiable entity. Journal of Nursing Management , 7 (6), 317-322.
Neill, D. (2012). Nursing Workload and the Changing Health Care Environment: A Review of the Literature. Administrative Issues Journal , 1 (2), 132-140.
Cite this paper
Select style
- Chicago (A-D)
- Chicago (N-B)
NursingBird. (2024, January 27). Nursing Work Overload and Effect on Patient Safety. https://nursingbird.com/nursing-work-overload-and-effect-on-patient-safety/
"Nursing Work Overload and Effect on Patient Safety." NursingBird , 27 Jan. 2024, nursingbird.com/nursing-work-overload-and-effect-on-patient-safety/.
NursingBird . (2024) 'Nursing Work Overload and Effect on Patient Safety'. 27 January.
NursingBird . 2024. "Nursing Work Overload and Effect on Patient Safety." January 27, 2024. https://nursingbird.com/nursing-work-overload-and-effect-on-patient-safety/.
1. NursingBird . "Nursing Work Overload and Effect on Patient Safety." January 27, 2024. https://nursingbird.com/nursing-work-overload-and-effect-on-patient-safety/.
Bibliography
NursingBird . "Nursing Work Overload and Effect on Patient Safety." January 27, 2024. https://nursingbird.com/nursing-work-overload-and-effect-on-patient-safety/.
- Legal and Ethical Problems of Access to Information for Nurses
- US Nursing Shortage and Means to Address It
- Nursing in Global Health Systems: Somalia
- Nursing: End-of-Life Care as an Ethical Issue
- Surveillance as a Nursing Concept
- The Subcutaneous Immunoglobulin Therapy in a Home Care Setting
- Nursing Philosophy: Personal Views on the Nursing Career
- Nursing Workloads Analysis
- Florence Nightingale’s Philosophy in Nursing
- The Holistic Care Philosophy: Concerns and Coping Patterns
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Nursing Workforce Challenges in the Postpandemic World
The United States and the rest of the world continue to grapple with the COVID-19 pandemic. Considering that nurses make up the largest segment of the U.S. healthcare workforce, they are essential to the country’s collective pandemic response. Nurses are the primary source of direct care to persons infected by COVID-19, including historically marginalized populations, and the ongoing demands placed on nurses are leading to unprecedented stress, burnout, and uncertainty about their profession. Even before the pandemic, healthcare settings were chronically understaffed and nurses were burnt out. According to a prepandemic analysis, a shortfall of more than 150,000 registered nurses was anticipated by 2020 ( Zhang et al., 2018 ). The pandemic has exacerbated the labor shortage well beyond prior forecasts, stressing an already fragile U.S. healthcare system and potentially contributing to worse patient outcomes and wider health inequities.
A 2021 integrative review examining the pre- and post-COVID-19 pandemic literature on nursing turnover found that since the pandemic’s onset, there has been a significant increase in nurse turnover intention ( Falatah, 2021 ). A 16-study synthesis of nurse burnout literature during the pandemic found high levels of emotional exhaustion and depersonalization, as well as reduced feelings of personal accomplishment ( Galanis et al., 2021 ). The same study also identified risk factors for burnout, including decreased social support, working in hospitals with inadequate and insufficient material and human resources, and increased workload ( Galanis et al., 2021 ).
The staggeringly high turnover across America’s working population due to the COVID-19 pandemic has been referred to as the “Great Resignation” ( Gahdhi & Robison, 2021 ). In addition to record-high resignations and unfilled positions, an analysis by Gallup found employee engagement—rather than an industry, role, or pay issue—to be the major risk factor for resignation ( Gahdhi & Robison, 2021 ). From September 2019 to March 2021, the proportion of U.S. employees “actively disengaged” (looking for a job or watching for opportunities) increased from 69% to 74% ( Gahdhi & Robison, 2021 ).
Studies suggest that nursing is particularly susceptible to the Great Resignation. An American Nurses Foundation (2022) survey of nearly 12,000 nurses conducted in January 2022 found that 60% of respondents younger than 35 years reported experiencing an extremely stressful, violent, or traumatic event resulting from COVID-19, and 89% reported that their organization was experiencing a staffing shortage. More than one-half of respondents felt undervalued, and nearly one quarter reported that they intended to leave their positions in the next 6 months.
Concerned about these trends, the AcademyHealth Interdisciplinary Research Group on Nursing Issues (IRGNI) has devoted its energy to supporting the development of health services research that examines the nursing workforce, shapes our understanding of the practice environment, and evaluates the workforce needs of the postpandemic world in both hospital and community settings. The collection of abstracts presented at this year’s IRGNI conference reflects this commitment. Many of these abstracts address the adverse effects of the pandemic on nurses. Stimpfel, for example, describes the impact of the first 6 months of the pandemic on nurses’ psychological health and reports high rates of depression, anxiety, and insomnia. In the study by Montgomery and Patrician, the researchers show that stress during the pandemic contributed to high rates of burnout. Similarly, Pogue et al. found that during COVID-19, registered nurses, compared to physicians and advanced practice providers, reported the highest levels of burnout, job dissatisfaction, stress, and intent to leave.
These abstracts reinforce the importance of a supportive work environment for achieving nurses’ well-being, improving patient outcomes, and reducing health inequities. Townley et al., for example, found that poorly rated primary care nurse practitioner work environments contributed to high rates of hospitalization for dually-eligible adults with chronic conditions. In a systematic review of 12 research articles, Rosenbaum and Lake reported a strong association between hospital nursing resources, such as Magnet designation, nurse staffing, and the nurse work environment, and patient satisfaction based on the Hospital Consumer Assessment of Healthcare Providers and Systems survey.
Taken together, these works call for “rebooting” the practice environment to offset the adverse effects of the pandemic on nurses and their patients, and the nursing workforce must be prepared for the postpandemic world. Investments in the practice environment may help to offset the adverse effects of the pandemic on nurses and their patients. We believe that this will require innovative models of nurse-led care; reimagined nursing-sensitive performance measures; new and sustained efforts for promoting diversity, equity, and inclusion; payment policies that reflect nurses’ value; as well as innovative organizational and institutional approaches that enable flexibility and recognize nurses’ contributions. The IRGNI looks to its members and other nursing health services researchers to open lines of inquiry that inform these new directions and improve healthcare delivery for all Americans.
We thank the contributors for their trailblazing work, and we look forward to witnessing and contributing to the innovations in practice environments to come.
A Mixed Methods Study of Individual and Work Factors Associated With Psychosocial Health of Registered Nurses During the COVID-19 Pandemic
Author: Amy Witkoski Stimpfel, PhD, RN
Research Objective: To describe the initial influence of the COVID-19 pandemic on U.S. nurses’ psychosocial health, and to identify factors associated with poor psychosocial health outcomes.
Study Design: We conducted an exploratory, descriptive study with a convergent mixed methods design (QUAN + qual) in which the quantitative data were prioritized and qualitative data were used to explain and augment findings. The quantitative data were captured in a survey of nurses’ work environments, COVID-19–related experiences, and psychosocial health outcomes using REDCap, a secure cloud-based platform. We developed separate multivariable logistic regression models for 3 psychosocial health outcomes using the Patient Health Questionnaire (PHQ-9), which is a 9-item survey measuring depressive symptom severity; the Generalized Anxiety Disorder (GAD-7) tool, which measures anxiety using 7 items; and the Insomnia Severity Index (ISI), which measures insomnia symptoms with 7 items. Qualitative data were captured in individual semi-structured interviews conducted through audio-only Zoom meetings. An interview guide based on the conceptual framework that guided this study (Work, Stress, and Health) consisted of a series of theoretically derived open-ended questions and probes. We used content analysis to process and analyze qualitative data. To integrate the quantitative and qualitative data, we used joint analysis displays.
Population Studied: Participants were recruited from June to August 2020, which was an early period of the pandemic in the United States. To capture a range of geographic locations and pandemic intensity, we used multiple sources, including regional professional nursing organization membership list servs, NIOSH (National Institute for Occupational Safety and Health) Education and Research Centers, and social media platforms. Eligibility criteria included (a) being a registered nurse, (b) currently working in the, United States, and, (c) having at least 6 months of work experience since initial nursing licensure. We administered surveys ( N = 629) and conducted semi-structured interviews ( N = 34) among a subset of nurses working across healthcare settings in 18 states.
Principal Findings: Nurses reported high rates of depressive symptoms (22%), anxiety (52%), and insomnia (55%). The only work or COVID-19–related variable that predicted poor outcomes across all three multivariable logistic regression models was shorter total sleep time before work, i.e., 5 hours of sleep or less. The integrated analysis found that disturbances to sleep were both a contributing factor to, and an outcome of, poor psychosocial health status. Throughout the individual interviews, participants described sleep as “the biggest issue I’ve had” with a mix of anxiety and insomnia co-occurring. For example, one participant said, “I had the anxiety and the constant racing of thoughts and that kind of kept me up and that didn’t let me fall asleep as well.” Anxiety and rumination about their working conditions—extreme stress, understaffing, redeployment into a COVID-19 unit, rationing/lack of personal protective equipment, high mortality—lead to difficulty initiating or maintaining sleep.
Conclusions: Nurses working during the onset of the COVID-19 pandemic faced severe work stressors affecting their psychosocial health status. Immediate attention as well as long-term follow-up are warranted for this priority workforce.
Implications for Policy or Practice: Healthcare leaders are responsible for ensuring that evidence-based interventions are being implemented within their organizations to promote and restore the psychosocial health and well-being of the nursing workforce.
Nursing Data in Large, Federal Government-Sponsored, Health-Related Surveys and Datasets: A Mapping Review
Authors: Ann Annis, PhD, MPH, RN; Crista Reaves, PhD, RN; Jessica Sender; and Sherry Bumpus, PhD, FNP-BC
Research Objective: Nursing faculty conducting research and scholarship face competing priorities, time constraints, and limited resources. Secondary big data from national databases offer new opportunities to address important issues that influence the nation’s health. However, navigating these sources can be challenging. Furthermore, the extent to which these data sources include information related to nursing practice is not known. We aimed to review and summarize a comprehensive list of federally-sponsored sources of healthcare data and determine the inclusion of nursing-sensitive data.
Study Design: We conducted a systematic mapping review of federal sources of healthcare data available for researchers. An iterative process of data collection, coding, and review was undertaken. The primary measure of interest was the availability of nursing-inclusive data. Additional key measures included the overview and purpose of the data, population of interest and sampling design, methodology of data collection, type and description of data, and cost to obtain data. Convergent synthesis analysis was used to aggregate findings.
Population Studied: We included federal government entities that collected health-related data on populations, patients, individuals, healthcare providers, or systems. We searched their websites for publicly available datasets. Data sources with active data collection within the previous 10 years, and those that collected health-related data on populations, individuals, healthcare providers, or systems were included. Among 91 data sources identified, 58 met final inclusion criteria.
Principal Findings: The 58 data sources belonged to nine government entities, with the majority (28%) managed by the Centers for Disease Control and Prevention. The primary population of interest for most sources (71%) was individuals or patients; fewer sources focused on providers (26%) and health systems (24%). More than half ( n = 34, 59%) included some data elements on healthcare providers, which included nurses. However, few ( n = 13, 22%) distinguished nurses from other healthcare providers. Data related to nurses were generally buried within measures that were nonspecific for type of provider, which prevents the calculation of metrics that directly reflect nursing practice.
Conclusions: National data sources represent a valuable resource of big data that provide insight into the nation’s health, healthcare system, and workforce. These secondary data are a feasible, cost-efficient means by which to investigate important health issues relevant to nurses. However, despite the diverse collection of nationally representative datasets available to researchers, we found that the inclusion of nursing-specific data is uncommon. More than half of the data sources we reviewed contained information on providers, yet few collected data that would permit nursing-specific analyses.
Implications for Policy or Practice: Nurses and advanced practice nurses deliver a large proportion of care in the, United States, but federal data sources do not adequately measure the role of nurses in healthcare delivery. The current drive toward value-based care requires the attribution of providers’ care to patient outcomes. However, without more granular data on providers, we are unable to produce measures that accurately reflect nursing contributions in healthcare. Our findings highlight the importance of building the capacity of big data sources to incorporate nursing-specific data, which are needed to inform policies that guide provider practice.
Better NP Practice Environments Reduce Disparities in Hospitalizations Among Dually Eligible Patients With Chronic Ambulatory Care Sensitive Conditions
Authors: Jacqueline Nikpour Townley, PhD, RN; Heather Brom, PhD, APRN; Aleigha Mason, BSN, RN; Jesse Chittams, MS; Lusine Poghosyan, PhD, MPH, RN, FAAN; and J. Margo Brooks Carthon, PhD, APRN, FAAN
Research Objective: Adults eligible for both Medicare and Medicaid, known as dually eligible patients, experience significant health disparities, including twice as many hospitalizations, significant unmet health-related social needs, and higher rates of chronic ambulatory care sensitive conditions (ACSCs), such as coronary artery disease (CAD) and diabetes, compared to Medicare-only patients. Nurse practitioners (NPs) are well-positioned to address the care needs of dually eligible patients, as NPs are increasingly providing primary care management of ACSCs and are more likely than physicians to accept Medicaid. However, NPs often work in unsupportive clinical practice environments marked by strained relationships with administrators, a lack of independent practice and support, and limited professional visibility, limiting their ability to optimally meet patients’ needs. The purpose of this study was to examine the association between the NP primary care practice environment and disparities in all-cause hospitalizations between dually eligible and Medicare-only patients with ACSCs.
Study Design: Secondary cross-sectional survey methodology was employed to collect data from primary care NPs across 460 practices in four states (Pennsylvania, New, Jersey, California, and Florida) in 2015. The Nurse Practitioner Primary Care Organizational Climate Questionnaire (NP-PCOCQ), which contains 4 subscales with high internal consistency reliability, was used to measure NP practice environment. Practice environments with all 4 mean subscale scores above the median were classified as “good.” Those with 2–3 subscales above the median were classified as “mixed” practice environments, and those with 0–1 subscales above the median were classified as “poor.” Survey data were linked to Medicare claims files through a practice identifier available in the SK&A OneKey database. Multilevel regression models accounting for patient and practice characteristics were employed, followed by pairwise comparisons to compare disparities in all-cause hospitalizations between dually eligible patients and Medicare-only patients within good, mixed, and poor NP practice environments.
Population Studied: A total of 165,200 patients (14.9% dually eligible patients and 85.1% Medicare-only beneficiaries) were included across 460 practices. Patients had an International Classifications of Diseases, 10th edition, Clinical Modification, code for CAD or diabetes as one of their top five diagnoses.
Principal Findings: The majority of patients (58.1% dually eligible, 60.1% Medicare only) received care in poor practice environments (χ 2 = 157.8, p < .001). After adjusting for patient and practice characteristics, dually eligible patients had 50% higher odds overall of being hospitalized compared to Medicare-only patients (OR 1.51, 95% CI: 1.41–1.62). Dually eligible patients in poor practice environments had the highest adjusted odds of being hospitalized compared to their Medicare-only counterparts (OR 1.51, 95% CI: 1.41–1.62). In mixed practice environments, dually eligible patients had approximately 44% higher odds of a hospitalization (OR 1.44, 95% CI: 1.23–1.67), whereas in the best practice environments, dually eligible patients had approximately 29% higher odds (OR 1.29, 95% CI: 1.14–1.45, p < .001).
Conclusions: Improving NPs’ clinical practice environment in primary care may sizably reduce disparities in hospitalizations for dually eligible patients. However, even in the best practice environments, critical disparities in hospitalizations remain.
Implications for Policy or Practice: As policymakers look to improve outcomes and reduce costs among dually eligible patients, addressing a modifiable aspect of care delivery in NPs’ clinical practice environment is a key opportunity to reduce hospitalization disparities. Further efforts are needed to address remaining disparities by understanding and meeting patients’ health-related social needs.
Understanding Relationships Between Health Access Literacy, Health Self-Efficacy, Emotional Well-being, and Meaningful Engagement With the Children’s Mental Health System During the COVID-19 Pandemic.
Authors: Suzanne Courtwright, PhD, MSN, NP, NEA-BC, and Jacqueline Jones, PhD, RN, FAAN
Research Objective: Access to adolescent mental health services is limited, leading the Children’s Hospital Association to advocate on behalf of children and teens with a written letter to leaders of the, United States Senate and House of Representatives on January 27, 2022, to invest in the pediatric mental health workforce. The COVID-19 pandemic is exacerbating the growing mental health crisis in the country’s pediatric and adolescent population. In October 2021, the Children’s Hospital Association joined the American Academy of Pediatrics and the American Academy of Child and Adolescent Psychiatry and declared a national emergency in children’s mental health, as rates of anxiety, depression, and hospitalizations for suicide attempts and self-harm have risen more than 50% from prepandemic levels. Teens with chronic conditions have 4.3 greater odds of suicidal ideation and completion than their peers, and nearly 1 in 4 teens has a chronic condition. Understanding how adolescents with chronic conditions access, utilize, and engage with the children’s mental health system is necessary to better inform allocation of investments in mental healthcare delivery models for this vulnerable but growing population. The purpose of this study is to understand how health access literacy, health self-efficacy, and emotional well-being influence meaningful engagement with the children’s mental health system during the COVID-19 pandemic.
Study Design: A convergent mixed methods design utilizing path analysis of factor variables integrated with analysis of qualitative data using interpretive phenomenology was used.
Population Studied: Adolescents aged 10–21 years with chronic conditions, defined as requiring ongoing treatment for more than 1 year, were included.
Principal Findings: Preliminary findings indicate that adolescents with chronic conditions do not access healthcare for mental help until “it gets really bad.” Establishing trust over time is an important factor for this population. For those who tried to access services, non-White participants reported more challenges to access mental health services than their White peers.
Conclusion: The preliminary results of this study highlight opportunities to improve health equity by investing in mental health resources across both micro- and macro-level systems of care.
Implications for Policy or Practice: Improving health equity for teen mental health services may begin with placing interdisciplinary providers in micro-level proximity to teens, such as in schools and community-based programs, to optimize opportunities for trusting relationships to develop. Psychiatric mental health nurse practitioners, pediatric nurse practitioners, nurse coaches, community health nurses, school nurses, and public health nurses are well poised to provide easier access to school- and community-level preventive mental health education, and services. Removing policy barriers to advanced practice in densely populated states such as New, Jersey and the northeast will only advance efforts to optimize access to care.
Complementing ICD Codes With Nurses’ EHR Documentation Can Improve the Identification of Patients With Predisposing Factors of Iatrogenic Conditions
Authors: Sarah E. Ser, MS; Urszula A. Snigurska, BSN, RN; Mattia Prosperi, PhD, MEng; Ragnhildur I. Bjarnadottir, PhD, MPH, RN; and Robert J. Lucero, PhD, MPH, RN, FAAN
Research Objective: Accurate identification of patients with predisposing factors of iatrogenic conditions is a prerequisite for implementation of targeted prevention interventions. The International Classification of Diseases (ICD) codes are frequently used as proxies for a patient’s health status. However, ICD codes are unlikely to reflect a patient’s complete hospital experience. This results in an underutilization of potentially significant clinical information, including nursing assessment data, which could be used to develop valid outcome measures as well as accurate prognostic models for point-of-care decision support. Nursing assessment data may complement ICD codes in the overall characterization of a patient’s hospital experience. This study explored complementing ICD codes with electronic health record (EHR) nursing assessment data to operationalize dysuria, a factor associated with several iatrogenic conditions.
Study Design: We conducted a descriptive observational analysis of data from an ongoing retrospective study on predictors of iatrogenic conditions. Data were extracted from the University of Florida (UF)’s Integrated Data Repository. We developed an operational definition of dysuria using ICD codes from the 9th (ICD-9) and 10th (ICD-10) editions and EHR nursing assessment data. We compared the number of patients with dysuria based on ICD codes to those captured by our operational definition.
Population Studied: Observations included 135,739 patients admitted to one of 21 medical and/or surgical nursing units of an academic medical center hospital between 2012 and 2018.
Principal Findings: Based on ICD codes and EHR nursing assessment data, we created the following operational definition of dysuria: ICD-9 Code: 788.1 (or) ICD-10 Code: R30.0 (or) ICD-10 Code: R30.9 (or) nurses’ documentation of “burning” under “genitourinary symptoms” in at least one of the simple or complex Assessment flowsheets. A total of 3,637 patients with dysuria were identified by our new operational definition, and 198 were identified with both ICD codes and nursing assessment data. Four and one-half times as many patients experienced dysuria based on the combination of ICD codes with nursing assessment data compared to only ICD codes.
Conclusions: We demonstrated that complementing ICD codes with nurses’ documentation of dysuria captured patients who would not have been identified using only ICD codes. These findings could have practical and methodological implications for understanding dysuria during hospitalization; our analysis indicates that use of nursing assessment and other nursing data should be further explored. We highlighted only one of the many possibilities for identifying patients with risk factors of iatrogenic conditions using nurse-generated data. In addition to the simple and complex assessment flowsheets, there are other flowsheets in which nurses document patients’ data, which can be used to complement ICD codes and other coded data. Additionally, although we used only structured data to formulate our operational definition of dysuria, nurses’ narrative notes can contain rich contextual information, which is not typically documented in structured fields of EHRs but may be necessary for accurate outcomes measurement and case identification.
Implications for Policy or Practice: Relying exclusively on ICD codes to identify patients with certain conditions can introduce coding bias. Nursing assessments and other sources of clinical EHR documentation data may provide a source of direct clinical information to address the bias found when using ICD codes.
Understanding Crisis Needs Among Family Caregivers of Patients in Critical Care: A Qualitative Analysis
Authors: Amanda C. Blok, PhD, MSN, RN, PHCNS-BC; Thomas S. Valley, MD, MSc; Lauren E. Weston, MPH; Jacquelyn Miller, MA; Kyra Lipman, BS; and Sarah L. Krein, PhD, RN
Research Objective: To understand met or unmet needs of family caregivers in crisis during a critical care hospitalization and examine differences by anxiety level to help inform family-centered intervention design.
Study Design: We conducted a qualitative content analysis of 40 semi-structured interviews of family caregivers of mechanically ventilated patients to understand their experiences with critical care. We specifically identified needs of family caregivers in crisis—informational and emotional processing, social support, and self-care—and factors that may influence these needs using nursing theoretical models for family management of conditions. Next, we used the Hospital Anxiety and Depression Scale (HADS) administered at the time of interview to measure anxiety and divided the sample into three groups by HADS: anxiety ( n = 15), borderline anxiety ( n = 11), and low anxiety ( n = 14). We examined similarities and differences in family member experiences and needs among the three groups.
Population Studied: Family caregivers of patients hospitalized in critical care.
Principal Findings: Most family caregivers were adult children (32%), followed by spouses (22%), parents (15%), siblings (15%), and other family (15%). Crisis needs were present in all anxiety groups, but there were differences in the extent and specifics of their needs by anxiety level. For informational processing, family caregivers with anxiety described challenges understanding medical decisions made by the clinical team, often waiting for healthcare providers to initiate conversations, while family caregivers with low anxiety valued detailed information from staff and tried to prepare other family members to prevent distress. For emotional processing, family caregivers with anxiety reported fear, a sense of responsibility to protect other family members from fear, and a preoccupation with day-to-day events that inhibited processing their emotions, whereas those with borderline and low anxiety noted that other family members and prior experiences helped them deal with their emotions. For social support, more than half of caregivers with anxiety expressed strained relationships in their social support network or felt alone, whereas those with borderline and low anxiety did not describe experiencing relationship strain. Faith communities were identified as a source of support by all anxiety groups, although the added emotional and financial support from these communities appeared more prominent among those with borderline and low anxiety. For self-care, family caregivers with anxiety reported that worry impinged on their sleep and self-care, whereas family caregivers with low anxiety prioritized sleep and self-care. Caregivers with low and borderline anxiety were better able to care for themselves due to tangible support from other family members.
Conclusions: Family caregivers of critical care patients experience crisis needs during the hospitalization, although the specific needs appear to differ by family caregiver anxiety level. Our detailed understanding of caregiver experiences can inform intervention components that address these crisis needs during a patient’s critical care hospitalization.
Implications for Policy or Practice: Critical care nurses spend the most time at the bedside with family caregivers of critical care patients. Developing interventions that address the crisis needs of family caregivers may help family caregivers to engage with nurses and further enhance the care delivery process.
COVID-Related Stressors, Burnout, Turnover Intention, and Resilience Among Nurse Leaders During the Pandemic
Authors: Aoyjai P. Montgomery, PhD, BSN, and Patricia A. Patrician, PhD, RN, FAAN
Research Objective: Even before the COVID-19 outbreak, at least one of every 10 nurses worldwide was suffering from high burnout, which contributed to high turnover rates. With the COVID-19 pandemic, anecdotal reports of overwork, burnout, and even suicide of healthcare professionals is being shared in the news and on social media. The pandemic introduced new stressors to nurse leaders, such as managing the complex staffing situation (staff shortages, reassigning nurses to cover COVID-19 units, limited bed capacity, high patient acuities, shortage of personal protective equipment), while supporting their staff nurses. Since COVID-19 began, there has been research concerning COVID-related stressors, burnout, turnover intention, and resilience among nursing staff but not among nurse leaders. Therefore, this study aimed to examine the COVID-related stressors that are most significantly related to burnout and turnover intention, investigate how resilience impacts burnout and turnover intention, and explore strategies that nurse leaders are using during this pandemic to maintain resiliency.
Study Design: This descriptive, cross-sectional study employed an electronic survey of several instruments to measure COVID-related stressors (COVID-related Stress Scales [CSS]), burnout (Copenhagen Burnout Inventory [CBI]), turnover intention (a single item), and resilience (Connor-Davidson Resilience Scale [CD-RISC-25]) among nurse leaders. The survey also included open-ended questions that were analyzed qualitatively.
Population Studied: In September 2021, 57 nurse leaders who worked in Birmingham, Alabama, hospitals, including nurse managers, directors of nursing, and other nurses who are in administrative roles, responded to the survey.
Principal Findings: The average respondent had 10.7 years of nurse leader experience, had a graduate degree (67%), and worked as nurse managers (42%) or nursing directors (37%). The CSS was positively related to all three burnout subscales (Personal, Work-Related, Client-Related Burnout) ( r = .27 to .40, p < .05) but not significantly related to intent to leave ( r = 0.17, p = .20). Resiliency was negatively related to all subscales of burnout ( r = -.53 to -.59), p < .01) and intent to leave ( r = -.32, p < .05) but not significantly related to COVID-19 stress ( r = -.07 to -.20, p > .05). The top three resiliency strategies that nurse leaders used were (a) prayer and faith, (b) social support, and (c) self-care (e.g., taking a break, exercising, promoting good nutrition). The top three recommendations that nurse leaders had for other nurse leaders were (a) disconnect/take time off, (b) positive and creative thinking, (c) self-care (e.g., exercising, resting, and stress relief).
Conclusions: Among nurse leaders, COVID-19 stress impacts burnout but does not affect resiliency and intent to leave. Nurse leaders who had higher resiliency seemed to have lower burnout and were less likely to leave their positions.
Implications for Policy or Practice: The findings of this study provide baseline data to inform the development of actionable interventions to prevent or at least reduce burnout and turnover intention. Furthermore, the resiliency strategies and recommendations from these nurse leaders should be disseminated to other nurse leaders to help them reduce burnout and turnover intention.
The Association Between Hospital Nursing Resources and Patient Satisfaction Using the HCAHPS Survey: A Systematic Review
Authors: Kathleen E. Fitzpatrick Rosenbaum, BSN, RN, NICU-RNC, CCRN; and Eileen T. Lake, PhD, RN, FAAN
Research Objective: Identifying factors that influence patient satisfaction has become a priority for healthcare system managers. The Centers for Medicare and Medicaid Services implemented Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) surveys to evaluate hospitals and incentivize them to improve patient satisfaction. Survey results are linked to hospital Medicare reimbursements, making high scores of particular interest to hospital managers and to healthcare consumers. The purpose of this systematic review was to synthesize the literature reporting the association between nursing resources (nurse education, nurse staffing, the nurse work environment, and Magnet designation) and HCAHPS scores. Our goals were to provide managers with evidence to inform their decisions and identify gaps for researchers to address.
Study Design: A systematic review was conducted searching the CINAHL and MEDLINE databases. Key terms were searched using headings and text phrases related to educational preparation, nurse work environment and nurse staffing, and Magnet designation. Chain searching was applied, and the Johns Hopkins Nursing Evidence-Based Practice: Evidence Level and Quality Guide was used to grade the evidence. Effect sizes were measured by regression coefficients when available.
Population Studied: Our inclusion criteria were (a) a nursing resource as an independent variable, (b) HCAHPS scores as a dependent variable, (c) a cross-sectional study design, and (d) U.S. empirical data published in a scientific journal. Studies meeting these criteria and published between 2006 and 2021 were examined.
Principal Findings: Twelve articles met inclusion criteria. Among these articles, 7 focused on magnet designation, 3 on nurse staffing, 2 on the nurse work environment, and 0 on nurses’ education. All but 2 studies included global HCAHPS measures. In addition, 8 studies included HCAHPS composite measures. The samples of hospitals ranged from 110 to 3,026. The years represented in the data encompassed 2005 to 2018. In 11 of the 12 studies, nursing resources were significantly associated with HCAHPS scores. Magnet designation exhibited the largest effect size of 6.33. Nurse staffing showed the most variation across studies with the largest effect size related to an additional hour of nursing care per patient day or an additional patient per nurse. Coefficients ranged between -0.24 and -1.44. Nurse staffing results showed that for every one additional patient a nurse cared for, there was a 1.44% decrease in the percentage of patients giving high ratings for willingness to recommend. The nurse work environment had a positive association with patient satisfaction; effect sizes ranged from 3.15 to 6.08, with patients much more likely to give high ratings to hospitals classified as having favorable nurse work environments.
Conclusions: For hospital managers eager to improve patient satisfaction, understanding which organizational factors are associated with patient satisfaction is of interest. Nursing resources were shown to be a lever toward high HCAHPS scores. Additional research is needed to identify the association between nurse education and HCAHPS scores.
Implications for Policy or Practice: It would behoove managers to invest in nursing resources to improve patient satisfaction and achieve high-value care. Administration should support managers’ endeavors to improve nurse staffing, foster a positive nurse work environment, and develop Magnet-like qualities.
The Association Between Nursing Home IT Maturity and UTI Among Long-Term Residents
Authors: Catherine C. Cohen, PhD, RN; Kimberly Powell, PhD, RN; Andrew W. Dick; Patricia W. Stone, PhD, RN, FAAN; and Gregory L. Alexander, PhD, RN, FAAN, FACMI
Research Objective: Urinary tract infections (UTIs) are the most common infections among nursing home (NH) residents. Improving UTI prevention and management in NHs is included in key antibiotic stewardship and infection control and prevention initiatives. NH information technology (IT) maturity (i.e., technological capability, extent to which systems are used, and degree to which different systems are integrated) could impact NHs’ ability to prevent and manage UTIs through improved integration and communication of data from multiple sources. This study aimed to explore the relationship between specific aspects of IT maturity and odds of UTI among long-stay NH residents.
Study Design: We conducted a repeated cross-sectional study combining three nationally representative data sources: (a) four annual surveys measuring IT maturity, (b) Minimum Data Set (MDS) 3.0 assessments measuring resident characteristics, and (c) Certification and Survey Provider Enhanced Reporting data identifying facility characteristics. Nonadmission MDS assessments completed within 90 days of IT survey completion were matched to survey data, including nine scales of IT maturity including three healthcare domains (resident care, clinical support, and administrative activities) and three dimensions (IT capabilities, extent of IT use, and degree of IT integration with internal/external stakeholders). The outcome was a binary indicator of UTI, which is recorded according to evidence-based criteria that includes clinical symptoms. Descriptive statistics were examined. Bivariate and multivariate regressions using NH fixed effects were conducted controlling for resident and NH characteristics. We varied assumptions to test robustness of our results.
Population Studied: Assessments of long-term residents aged 65 + years from a random sample of Medicare-certified U.S. NHs over 4 consecutive years (2013–2017) were included.
Principal Findings: Our sample included 816 NHs. These NHs had 219,730 regular NH resident assessments within 90 days of a survey, representing 80,322 unique long-term NH residents. Of these assessments, 4.1% recorded a UTI. In the multivariate analyses, maturity of administrative IT capabilities was associated with lower odds of UTI (adjusted OR 0.906, 95% CI: 0.843, 0.973). No components of this domain/dimension were individually associated with UTI, nor were any other IT maturity dimension/domain scores. These results were robust in all sensitivity analyses.
Conclusion: To our knowledge, this study was the first to determine a link between NHs’ IT maturity and health outcomes at the resident-assessment level. The finding that administrative IT capabilities are associated with decreased odds of UTI was additionally robust given healthcare facilities with better documentation systems may experience measurement bias as they are more likely to record health outcomes, such as UTI.
Implications for Policy and/or Practice: This work is timely and relevant to policy decisions at facility and public health levels, as it could shape utilization of IT in NHs. This work supports the need to include use of health IT in publicly reported national datasets. Consistent reporting of IT maturity in NHs could clarify ongoing impacts of important legislative actions such as the 21st Century Cures Act, which was enacted to accelerate the effective use of IT to support better access to healthcare information.
Nurses Insight and Psychological Reaction Toward a COVID-19 Outbreak in Bangladesh
Authors: Shanzida Khatun, PhD, MSc, RN; Fahima Khatun; Md. Shariful Islam; Khaleda Akter; and Md. Abdul Latif
Research Objective: To explore nurses’ insights and psychological reactions toward a COVID-19 outbreak in Bangladesh.
Study Design and Setting: Both the qualitative and quantitative aspects of this study were conducted at 54 settings from primary level to tertiary level hospitals.
Population Studied: A total of 800 nurses participated in the quantitative portion of the study, which used the Z-score formula, and 28 nurses participated in the qualitative portion, which used focus group discussion.
Principal Findings: The mean age of nurses was around 34 years. The mean (SD) knowledge score was 15.33 (2.60); perception, 7.41 (1.62); and Depression, Anxiety, and Stress Scale, 43.73 (30.95). Regression analysis showed that knowledge, perception, length of service, working experience at a COVID-19 ward, information from media, personal protective equipment supply, hand hygiene supply, and feeling of confidence in taking care of COVID-19 patients together explained 25% of the variance in the psychological reaction toward the COVID-19 outbreak. Five themes emerged from the focus group discussion, including “challenges for nurses of working [at] COVID-19 hospital,” “fear of becoming infected and infecting the family members,” “stress due to new context and heavy workloads,” inappropriate knowledge of wearing personal protective equipment, and lack of adequate training for nurses regarding COVID-19.
Conclusions: Further study is needed to identify the factors influencing nurses’ psychological reactions toward the COVID-19 outbreak. In addition, an intervention study will help nurses to increase their knowledge and perception of the pandemic and will help to decrease nurses’ psychological problems and increase coping related to the pandemic.
Implications for Policy or Practice: The findings of this study provide baseline information to policymakers to develop a strategy on nursing management for COVID-19 patients. This also contributes to design training programs for nurses during the outbreak.
Clarifying Nurse Practitioner Integration
Authors: Joshua Porat-Dahlerbruch, PhD, RN; Lusine Poghosyan, PhD, MPH, RN, FAAN; Nancy Blumenthal, DNP; Shoshana Ratz, MSc, RN; and Moriah Ellen, MBA, PhD
Research Objectives: Globally, healthcare systems are facing care provider shortages. These shortages are due to growing populations with increasingly complex healthcare needs, and physician supply alone cannot meet demands. These workforce needs across the world require innovative solutions. Many nations have introduced the nurse practitioner (NP) role to diminish workforce shortages. NPs bring a holistic scope of practice, which has been found to be well suited to address complex care needs. Research has shown that NPs provide safe and effective care. However, the ability to produce these results relies on successfully integrating NPs into all levels of the healthcare system. Despite the rich literature, to our knowledge, the “NP integration” concept has never been synthesized and defined. “NP integration” is described inconsistently and lacks elucidation. Without a definition of the concept, NP integration cannot be researched consistently. High-level evidence requires synthesis of findings researching the same concept. Research, therefore, cannot be synthesized to create a theory or a model to guide NP integration, which is critical for policymakers and stakeholders. This concept analysis aims to define and operationalize the concept of NP integration for research and to provide a basis for which theory on NP integration can be deduced and policy can be easily understood from the literature.
Study Design: The Walker and Avant (2019) concept analysis method was used.
Study Population: We included full-text articles, government reports, conference presentations, and abstracts, yielding 200 publications. After removing duplicates and abstract screening, 78 publications remained.
Principal Findings: Defining attributes of NP integration include process, achievable goal, introduction of the role, incorporation into organizational care models, challenging traditional ideologies, ability to function, provide high care quality, and improve outcomes, sustainability, and health system transformation. We identified facilitators and barriers affecting NP integration and multiple healthcare system levels at which NP integration occurs—macro, meso, and micro. We identified antecedents and consequences of NP integration. We synthesized findings to create an NP integration conceptual model. The analysis resulted in an operational definition of NP integration: A multilevel process of incorporating NPs into the healthcare system so that they can function to the full extent of their scope and contribute to patient, health system, and population needs.
Conclusions: This is the first research to synthesize NP integration literature to provide an operational definition and conceptual model. Moreover, most literature refers to macro (system-wide) or meso (organizational) level integration. We identified a new dimension—micro—which refers to individual interactions of NPs with other NPs, patients, physicians, nurses, and staff. NP integration is a complex process acting on multiple levels in the healthcare system. Policy intervention at all three levels is likely critical for NP integration.
Implications for Policy or Practice: These findings provide an operational definition so that research on NP integration can be conducted consistently. This research can be a basis for developing research tools assessing NP integration progress that stakeholders and policymakers can use to understand where policy intervention is necessary to improve NP integration.
Nurse Work Patterns in Long-Term Care: A Time-Motion Analysis
Authors: Yu Jin Kang, PhD, MPH, RN; Jeannie P. Cimiotti, PhD, RN, FAAN; and Karen A. Monsen, PhD, RN, FAMIA, FNAP, FAAN
Research Objective: It is well known that nurses working in the long-term care sector are short staffed and under a tremendous amount of pressure to complete nursing care in a timely manner. Multitasking is expected of these nurses, such as performing nursing tasks while communicating, but extensive multitasking should be minimized to avoid potential adverse events. Little is known about how these nurses might multitask in an effort to complete essential nursing care. The purpose of this study was to examine the workflow of licensed nurses in a skilled nursing facility and to determine how they might multitask to complete nursing care.
Study Design: An observational time-motion study was conducted at a 250-bed skilled nursing facility located in the southeastern United States. A web-based time capture application, TimeCaT, was used to collect data from September 2019 to March 2020. TimeCaT was customized to include 57 validated nursing activities based on the Omaha System. This method allowed for the collection of time-stamped workflow data that included communication and tasks—data that were not mutually exclusive. Observed nurse workflow was analyzed using χ 2 statistics and visualized with a heatmap.
Population Studied: Registered nurses (RNs, n = 4) and licensed practical nurses (LPNs, n = 7) who worked on short-term care (STC) and long-term care (LTC) units or provided wound care were included in the study. All participating nurses were full-time clinicians except one nurse who was supplied by a supplemental staffing agency. On average, one nurse was responsible for the care of 12 residents.
Principal Findings: There were 5,306 observations of multitasking episodes—an average of 35 multitasking episodes per hour. The majority of multitasking episodes occurred during care supervision (81%) and medication regimen (33%). Forty-eight percent of the episodes were related to the medication regimen among STC and LTC nurses, where communication with residents and other care team members and documentation occurred while nurses prepared medications (17%) and where communication with residents, including medication instruction, occurred while nurses administered medications (11%). A larger percentage of LTC nurses multitasked medication regimen activities when compared to STC nurses (55% vs 39%, p < 0.001) and in the morning when compared to afternoon and evening (57% vs 39% vs 48%, p < 0.001). Overall, a larger percentage of LPNs multitasked medication regimen activities when compared to RNs (51% vs 46%, p < 0.001).
Conclusions: Nurses frequently multitask during the preparation and administration of medications in a skilled nursing facility. Research is warranted to better understand the complexity of medication regimens and the factors that contribute to multitasking practice patterns. Furthermore, it is imperative that we determine whether multitasking practice patterns increase the cognitive workload of nurses and the likelihood of medication errors in skilled nursing facilities.
Implications for Policy or Practice: Healthcare administrators and policymakers should be mindful of the fact that nurses often multitask in skilled nursing facilities. This calls for policies that monitor nurse practice patterns in the long-term care sector and provide suggestions for improvement when necessary. If not, we risk the possibility of short- and long-term sequela associated with these questionable workflow patterns.
Linking Patient Safety Climate With Missed Nursing Care in Labor and Birth Units: Findings From the LaborRNs Survey
Authors: Jie Zhong, MSN; Kathleen Rice Simpson, PhD, RNC, FAAN; Joanne Spetz, PhD; Jason Fletcher, PhD; Caryl L. Gay, PhD; Gay L. Landstrom, PhD, RN, NEA-BC; and Audrey Lyndon, PhD, RNC, FAAN
Research Objective: Inpatient labor and birth settings are specialty care units with limited evidence regarding nursing care quality. Missed nursing care has been used to indicate nursing care quality in medical-surgical, intensive, and pediatric care settings. An emerging body of evidence suggests that features inherent in a better culture of safety, such as aligned organizational priorities, attention to workload, and team communication, are associated with less missed nursing care in general. The aim of this study was to explore patient safety climate and its association with the outcome of missed nursing care in labor and birth units.
Study Design and Population Studied: We recruited nurse respondents for this cross-sectional study in the United States via email distribution of an electronic survey between February 2018 and July 2019. Hospitals with labor and birth units were recruited from states with projected availability of 2018 State Inpatient Data. All registered nurses working in labor and birth units in the targeted hospitals were eligible. Measures included the Safety Climate Subscale from the Safety Attitudes Questionnaire, the Perinatal MISSCARE Survey, and nurse characteristics. The mean of individual nurse Safety Climate Subscale questions was used to measure nurses’ perception of the unit safety climate on a scale of 1–5, with a higher score indicating a better climate. The Perinatal MISSCARE Survey uses 25 items to assess the frequency at which required aspects of nursing care are delayed, unfinished, or completely missed on the respondent’s unit. The sum of missed aspects of care ranged from 0–25, with a higher score indicating more missed care. We used Kruskal-Wallis tests for bivariate analysis followed by mixed-effects linear regression models to estimate the relationships between patient safety climate and missed nursing care while accounting for clustering of nurses within hospitals.
Principal Findings: The response rate was 35%, resulting in a sample of 3,429 labor and birth registered nurses from 255 hospitals. A majority of respondents (65.7%) reported a perception of good safety climate in their units, with a mean (SD) score of 4.12 (0.73). The mean (SD) number of aspects of care occasionally, frequently, or always missed on their units was 11.04 (6.99). The adjusted mixed-effects model identified a significant association between better nurse-perceived safety climate and less missed care (-2.65; 95% CI: -2.97 to -2.34) after controlling for age and years of experience as a labor nurse. The estimates indicated each one unit increase of the mean score of nurse-perceived safety climate was associated with 2.65 fewer missed essential aspects of perinatal nursing care.
Conclusion and Implications for Policy or Practice: Our findings suggest that improving safety climate may promote nursing care quality during labor and birth through decreasing missed nursing care. Conversely, it is also possible that strategies to reduce missed care, such as staffing improvements, may improve safety climate. Safety strategies such as promoting open communication, ensuring nonpunitive response to error, incorporating perinatal safety nurses, and ongoing learning from safety events may decrease missed care in daily nursing activities.
Emergency Nursing Workforce Burnout and Job Turnover in the United States: A National Sample Survey Analysis
Authors: Allison A. Norful, PhD, RN, ANP-BC, FAAN; Kenrick Cato, PhD, RN, FAAN; Bernard P. Chang, PhD, MD; Taryn Amberson, MPH, RN, CEN, NHDP-BC; and Jessica Castner, PhD, RN, FAEN, FAAN
Research Objective: Burnout, especially in registered nurses working in emergency departments, has substantially jeopardized the nursing workforce supply and the ability to meet demands for care. Past research documenting the prevalence of burnout among emergency nurses have been limited by small sample sizes and local sampling approaches as they have been unable to capture the diversity of clinical, geographic, and demographic characteristics at a national level. Few studies have examined turnover in nurses who have left their job or are not currently working, resulting in the potential for healthy worker or survivor bias. The aims of our study were to (a) test differences in reasons for turnover or not currently working between emergency nurses and other registered nurses and (b) ascertain factors associated with burnout as a reason for turnover or not currently working among emergency nurses.
Study Design: We conducted a secondary analysis of the National Sample Survey for Registered Nurses publicly available from Health Resources and Services Administration. We excluded advanced practice nurses and respondents who were not working due to retirement. Demographic and work characteristics (e.g., sex, age, race and ethnicity, marital status, highest degree, years of experience, hours worked per week, household income, and degree enrollment) were extracted. Next, we extracted responses to 6 survey items permitting the identification of nurses who were not currently working or who recently left their position (within 2 years) and their reasons for turnover (22 response options, including “burnout”). Design weights were applied using the jackknife estimation procedure. Data were analyzed using descriptive statistics, χ 2 test, t test, unadjusted and adjusted logistic regression applying design sampling weights, and controlling for potential individual and work characteristic confounders.
Population Studied: Nationally representative sample of registered nurses (weighted N = 3,001,283) from the 50 United States and the District of Columbia. Analysis included 1,266 emergency nurses (weighted N = 217,706) and 18,589 nurses (weighted N = 2,786,879) in other settings.
Principal Findings: Seven job turnover reasons were endorsed by emergency nurses and significantly higher than reasons provided by other nurses: Insufficient staffing (11.1%, p = .011); physical demands (5.1%, p = 0.44); patient population (4.3%, p < .001); better pay elsewhere (11.5%, p = .001); career advancement/promotion (9.6%, p = .007); length of commute (5.1%, p = .012); and relocation (5%, p = .006). Increasing age and years of experience were significantly associated with decreased odds of burnout in adjusted models. Being female was associated with decreased odds of burnout when controlling for insufficient staffing, scheduling, and stressful work environment.
Conclusions: Several modifiable factors, such as insufficient staffing and better pay elsewhere, appear to be associated with job turnover. Further research should account for gender and age to better understand and mitigate burnout. Ongoing research is essential to identify priorities for risk detection and for future national-level nursing workforce policies and interventions.
Implications for Policy or Practice: Given the critical need of the emergency nursing workforce, this study provides evidence for preventive intervention and policy at the national level. Interventions to reduce burnout and job turnover may include enhancing work environments (e.g., sufficient staffing), increasing pay, and investing in the physical and psychological health of nurses. Practice and policy efforts aimed at precursors of nursing burnout as modifiable targets to reduce turnover may improve career longevity, well-being, and workforce retention.
The Impact of Pre–COVID-19 Nursing Home Infection Prevention and Control Policies on COVID- 19 Deaths
Authors: Jung A Kang, MSN, RN, AGACNP-BC, AGCNS-BC; Patricia Stone, PhD, RN, FAAN, CIC; and Andrew Dick, PhD
Research Objective: Nursing home (NH) residents have been disproportionally suffering from the COVID-19 pandemic. Therefore, it is essential to have a comprehensive NH Infection Prevention and Control (IPC) program to prevent potential infectious disease outbreaks. However, it is not known how NH IPC programs have impacted COVID-19 deaths. Therefore, the goal of this study was to examine the relationship between pre–COVID-19 NH IPC programs/policies and COVID-19 resident deaths.
Study Design: This retrospective study used publicly available data from the Centers for Disease Control and Prevention’s Long-Term Care Facility COVID-19 Module and USA Facts county-level COVID-19 data linked to a national survey of NHs in 2018. The survey included questions about NH IPC programs such as having infection preventionists certified in infection control (CIC) and outbreak preparedness policies. We used 10-week periods to separately assess the impact of NH IPC programs on the weekly resident COVID-19 deaths per 1,000 residents between May 24, 2020 and May 30, 2021. We then estimated multivariable regression models to examine the association between NH IPC programs and COVID-19 deaths controlling for facility-level characteristics and county-level COVID-19 death intensity.
Population Studied: A total of 857 NHs located in 489 counties were identified and included in this analysis. Approximately 7.5% of NHs had the infection preventionist certified in infection control. Among the outbreak preparedness policies, instructing infected staff to stay home was most common in NHs (92.4%), and use of rapid diagnostic methods for case detection was least common (49.9%).
Principal Findings: In the multivariable models, during the December 2020 peak period, NHs with CIC infection preventionists had 4.9 fewer weekly COVID-19 deaths per 1,000 residents compared to the NHs without CIC infection preventionists (β = -4.9, SE = 1.1, p < .0001). Use of rapid diagnostic methods for case detection was also associated with lower weekly COVID-19 deaths during the peak period (β = -1.25, SE = 0.43, p = .004). Cohorting infected residents together was negatively associated with weekly COVID-19 deaths during the off-peak periods (β = -2.7, SE = 0.5, p < .0001). On the other hand, instructing infected staff to stay home and closing to new admits were associated with higher weekly COVID-19 deaths, particularly during the peak periods (β = 1.03, SE = 0.52, p = .047; and β = 3.16, SE = 0.94, p = .001 respectively).
Conclusions: Most of the IPC programs had different impacts on COVID-19 deaths depending on the stage of COVID-19. The lower rate of COVID-19 deaths in NHs with CIC infection preventionists persisted throughout the pandemic periods. We also found that the use of rapid diagnostic methods for case detection was protective against COVID-19 deaths during the peak period, as was cohorting infected residents together during the off-peak period.
Implications for Policy or Practice: This study provides evidence-based policy recommendations to clinicians and policymakers to prevent future infectious disease crises in NHs. Aligning with the Centers for Disease Control and Prevention’s recommendation regarding infection preventionists, assigning one or more full-time infection preventionist with training in infection control in NHs is recommended.
U.S. Clinician Well-being Study: A Descriptive Analysis of the Work Environment and Clinician Well-being
Authors: Colleen A. Pogue, PhD, RN; Linda H. Aiken, PhD, RN, FAAN, FRCN; Kathleen F. Rosenbaum, BSN, RN, NICU-RNC, CCRN; Maura E. Dougherty, BSN, CRNA; and Matthew D. McHugh, PhD, JD, MPH, RN, FAAN
Research Objective: To determine factors associated with interdisciplinary clinician mental health and well-being in hospitals during COVID-19.
Study Design: This cross-sectional study utilized primary data collected through an electronic survey sent via hospital emails to identified clinicians between February 2021 and July 2021. Clinicians provided detailed information regarding clinician well-being (i.e., mental health, burnout, and job satisfaction) and quality of work environment (e.g., workload, autonomy, work-life balance, and interdisciplinary teamwork). Data were aggregated at the hospital level.
Population Studied: An interdisciplinary group of registered nurses (RNs) ( n = 15,738), advanced practice registered nurses and physician assistants (advanced practice providers [APPs]) ( n = 2,662), and physicians ( n = 5,336) were surveyed. Surveyed clinicians had to be working in an inpatient or ED setting. Data were collected from 60 different Magnet hospitals across the United States.
Principal Findings: Overall, findings of high clinician burnout (30%–44%), job dissatisfaction (12%–22%), and likelihood of leaving the job (23%–41%) were consistent across clinician groups and highest among nurses. A quarter of nurses experienced clinical levels of anxiety. Overall burnout levels varied widely across Magnet hospitals (25%–65%). Clinicians reported having high levels of stress at work (40%–53%) and having very little joy (7%–14%) with nurses reporting the highest levels of stress and the least joy. One-third of nurses rated their work environment as poor/fair. The quality of the work environment varied considerably across all Magnet hospitals, with as few as 5% and up to as many as 65% of hospital clinicians reporting that their work environment was poor/fair. More than half of all nurses (54%) felt there were not enough nurses to care for patients. There was less concern regarding nurse staffing among physicians and APPs, with 71% of physicians and 63% of APPs feeling that there were enough nurses to care for patients. Physicians reported high frustration with electronic health records (61%) and poor work-life balance (32%). APPs experience of well-being and perceptions of their work environment overlapped with both physicians and nurses. All clinicians stated the importance of being heard and supported by the administration and having a shared vision and values with the administration. Nearly 95% of clinicians reported good interdisciplinary working relationships and high levels of teamwork. Clinicians also rated the effectiveness of interventions to improve well-being. Across all clinicians, the most effective interventions were those that allow them time and resources to provide clinical care (e.g., improve nurse staffing levels, have breaks without interruption, reduce time spent on documentation, increase control over scheduling). There was clear agreement across clinicians on interventions they felt would not be as effective in improving well-being (e.g., resilience training, meditation rooms, wellness champion/committee).
Conclusions: Clinician burnout was high, and the quality of the work environment varied considerably across Magnet hospitals.
Implications for Policy or Practice: Opportunities to improve the work environment through empirically informed interventions are necessary to improve clinician well-being. Data suggest variation in the effectiveness of well-being interventions by clinician group, which should be taken into consideration during the development and implementation of such interventions.
The Association Between Primary Care Work Environments and Missed Opportunities for Emotional Healthcare
Authors: Eleanor Turi, BSN, RN, CCRN; Amelia Schlak, PhD, RN; Jianfang Liu, PhD; and Lusine Poghosyan, PhD, MPH, RN, FAAN
Research Objective: Nurse practitioners (NPs) are key to improving primary care delivery as they represent the fastest growing segment of the primary care workforce. Yet, poor nursing working conditions (i.e., hostile working relations, low autonomy, lack of support, and inadequate professional visibility) often challenge NP care delivery and have been linked with lower quality of care and adverse patient outcomes. These poor conditions also lead NPs to prioritize acute care needs of patients and ignore other needs such as addressing patients’ emotional well-being, which is an important and often overlooked area of health. We investigated the relationship between NP work environment and missed care around patients’ emotional health.
Study Design: This was a secondary analysis of cross-sectional survey data from 2017. The survey asked primary care NPs to complete the Errors of Care Omission Survey (EoCOS) to determine whether NPs missed opportunities for care and the NP Primary Care Organizational Climate Questionnaire (NP-PCOCQ) to assess the NP work environment. We examined the association between the NP-PCOCQ subscales (i.e., independent practice and support [IPS], NP-administrative relations [NP-AR], professional visibility [PV], and NP-physician relations [NP-PR]) and an aggregate measure of the EoCOS describing NP ability to address patients’ emotional health (EH-EoCOS; 3 items related to addressing emotional concerns of patients, discussing patients’ emotional well-being, and providing emotional support when making treatment decisions) using multilevel mixed-effects linear regression models. Higher scores on the NP-PCOCQ and the EH-EoCOS indicate a favorable work environment and that patients’ emotional health is addressed, respectively. We controlled for NP demographics and practice features.
Population Studied: A total of 397 primary care NPs in New York State across 377 primary care practices were included.
Principal Findings: In the bivariate model, higher IPS scores were positively associated with a higher EH-EoCOS score that neared statistical significance; for every 1 unit increase in IPS score, EH-EoCOS increased by 0.30 ( p = 0.059). After adjusting for NP demographics and practice features, there was a positive association between IPS score and EH-EoCOS, again that neared statistical significance (β = 0.29, p = 0.077). NP-AR (β = 0.11, p = 0.285), PV (β = 0.10, p = 0.370), and NP-PR (β = 0.22, p = 0.106) subscales were not significantly associated with EH-EoCOS.
Conclusions: Our findings suggest that NP ability to address patients’ emotional health needs is, in part, driven by the level of support for NP independent practice.
Implications for Policy or Practice: Lack of support for NP independent practice may prevent NPs from addressing patients’ emotional health, which could lead to future mental health complications among patients. NPs are uniquely prepared to deliver emotional healthcare because of their nursing education, which is grounded in holistic, person-centered care. Practices employing NPs should ensure that NPs have access to ancillary staff and support for care management to deliver care to patients. Practices should also allow NPs to manage patients independently, practicing to the full scope of their education and licensure.
Conflicts of Interest: Dr. Ghazal is a postdoctoral research fellow supported by NIH-NCI T32CA236621. Dr. Nikpour Townley is a postdoctoral fellow supported by NIH-NINR T32NR007104. Dr. Pogue is a postdoctoral fellow supported by NIH-NINR T32NR007104. Dr. Riman is a postdoctoral fellow supported by NIH-NHLBI T32HL007820. Dr. Schlak is a postdoctoral fellow supported by NIH-NINR CER2 T32NR014205.
- Pulse on the nation’s nurses survey series: COVID-19 two-year impact assessment survey American Nurses Foundation. 2022 March 1 https://www.nursingworld.org/~492857/contentassets/872ebb13c63f44f6b11a1bd0c74907c9/covid-19-two-year-impact-assessment-written-report-final.pdf [ Google Scholar ]
- Falatah R. The impact of the coronavirus disease (COVID-19) pandemic on nurses’ turnover intention: An integrative review. Nursing Reports. 2021; 11 (4):787–810. doi: 10.3390/nursrep11040075. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gahdhi V., Robison J. Gallup Workplace ; 2021 July 22. The ‘great resignation’ is really the ‘great discontent.’ https://www.gallup.com/workplace/351545/great-resignation-really-great-discontent.aspx [ Google Scholar ]
- Galanis P., Vraka I., Fragkou D., Bilali A., Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: A systematic review and meta-analysis. Journal of Advanced Nursing. 2021; 77 (8):3286–3302. https://10.1111/jan.14839. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zhang X., Tai D., Pforsich H., Lin V.W. United States registered nurse workforce report card and shortage forecast: A revisit. American Journal of Medical Quality. 2018; 33 (3):229–236. doi: 10.1177/1062860617738328. [ PubMed ] [ CrossRef ] [ Google Scholar ]
How to bridge the experience gap by supporting nurses of all tenures
From baby boomers to Gen Zers, the question of how the four generations comprising today’s workforce 1 Elka Torpey, “Millennials in the labor force, projected 2019‒29,” US Bureau of Labor Statistics, November 2020. can best work together gets a lot of attention. Personal and professional experiences, levels of training, employer expectations, and career outlook can vary across generations. In nursing, tenure is a particularly nuanced factor that adds complexity to the discussion on workforce dynamics and may be one of the more definitive features of employee experience and, ultimately, retention.
About the authors
As healthcare organizations and other stakeholders refine their strategies for bolstering the nursing workforce, it is critical to incorporate the nuanced needs and preferences of nurses at different stages of their careers. To this end, we surveyed 5,772 nurses across tenures in October 2023 as part of an ongoing research collaboration between the American Nurses Foundation (the Foundation) and McKinsey (see sidebar, “About the research collaboration between the American Nurses Foundation and McKinsey”). The survey results provide insights into opportunities to bridge the experience gap and support nurses across their career continuum.
The survey analyzed three specific nurse cohorts: early-tenure nurses (less than five years of nursing experience), midtenure nurses (five to less than 21 years), and most-tenured nurses (21 or more years). When notable differences were reported within these cohorts, the specific tenure range was also noted.
About the research collaboration between the American Nurses Foundation and McKinsey
The American Nurses Foundation (the Foundation) is a national research, educational, and philanthropic affiliate of the American Nurses Association committed to advancing the nursing profession by serving as a thought leader, catalyst for action, convener, and funding conduit. The Foundation and McKinsey have partnered to assess and report on trends related to the nursing profession. A foundational part of this effort is jointly publishing novel insights related to supporting nurses throughout their careers. The first publication from the research partnership, “ Understanding and prioritizing nurses’ mental health and well-being ,” was based on a survey conducted in April and May 2023. 1 “ Understanding and prioritizing nurses’ mental health and well-being ,” McKinsey, November 6, 2023.
This is the second publication from the research partnership and is based on a survey of 5,772 nurses across the United States, conducted in October 2023. The intent of this new research is to better understand surveyed nurses’ experiences, needs, preferences, and career intentions.
As part of the research, we asked nurses to share how much nursing experience they had based on these categories: less than two years, two to four, five to ten, 11 to 20, 21 to 30, 31 to 40, 41 to 50, and more than 50 years. Respondents were provided a disclaimer prior to completing the survey that results would be anonymous and shared only in aggregate. All survey questions were based on the experiences of the individual professional. All questions were also optional for survey respondents; therefore, the number of responses may vary by question. Additionally, publicly shared examples, tools, and healthcare systems referenced in this article are representative of actions that stakeholders are taking to address workforce challenges.
Across all experience levels, intent to leave the bedside remains high for surveyed nurses. About 30 percent of survey respondents indicated they were at least somewhat likely to leave their positions in the next six months. This is particularly acute in the early-tenure population, where a greater proportion of surveyed nurses reported considering leaving (about 45 percent) compared with midtenure (31 percent) and most-tenured nurses (27 percent).
The early-tenure population is particularly important to retain as more experienced nurses reach retirement age. Supporting and retaining midtenure and most-tenured nurses is also crucial given the critical role they play in teaching and mentoring those newer to the profession. In fact, finding creative ways to enable not only nurses nearing retirement but also those already retired to participate in direct patient care activities or coaching could help fill part of the experience void—and this cohort appears open to doing so if their needs and preferences were met.
We asked nurses who indicated they were currently or previously retired what would make them consider returning to clinical nursing. Of the 179 survey respondents, 45 percent reported that having the ability to set their own schedule would make them consider returning to clinical nursing, 34 percent wanted the ability to serve as an educator, and 31 percent wanted the ability to mentor nurses. Surveyed nurses across tenures indicated that there is a need to enact structures that would enable more robust onboarding and training for new nurses, promote team building, and create safe working environments through policies designed to prevent incivility and bullying.
Understanding the common needs of the nursing workforce as well as unique tenure-specific qualities can help hospital leaders find tangible ways to create collaborative and sustainable environments that would benefit nurses across the entirety of their careers. In this article, we explore how a positive team environment, across and between all tenures, can promote well-being and holistic employee health.
How the work environment can affect nurses
It’s no surprise that a team environment can substantially affect both health and burnout. Positive team characteristics, such as a sense of belonging, psychological safety, opportunities to learn and grow, and coworker support, were among the top indicators of an employee’s holistic health, according to a global survey conducted by the McKinsey Health Institute (MHI) across industries last year. 2 Jacqueline Brassey, Brad Herbig, Barbara Jeffery, and Drew Ungerman, “ Reframing employee health: Moving beyond burnout to holistic health ,” McKinsey Health Institute, November 2, 2023. Negative team characteristics, such as toxic workplace behavior and interpersonal conflict, were strongly linked with burnout.
MHI’s findings were reflected in the sentiments of early-tenure nurses in our survey. These respondents indicated that they were looking for a work environment where they felt supported and could learn from more-tenured nurses, but reported sometimes experiencing a negative environment, which can contribute to burnout. While in our May 2023 survey, nurses overall reported that they were indeed feeling burned out and that their mental health was suffering , nurses with less than five years of experience more often reported lower satisfaction with their roles, greater intent to leave their roles, and experiencing burnout. 3 “ Understanding and prioritizing nurses’ mental health and well-being ,” McKinsey, November 6, 2023.
In our October 2023 survey, we examined how negative sentiments after working a shift may be affecting nurses’ intent to leave. We asked nurses to select an adjective or sentiment for how they felt after they finished working a shift with each nursing tenure, including their peer group. When we compared intent to leave with the sentiments each nurse shared, there was a positive correlation between those who reported more negative sentiments and those who reported a greater intent to leave. This is particularly salient for stakeholders, as it provides a glimpse into how culture and team dynamics may affect nurses and their likelihood to stay in their current roles.
Nurses’ sentiments about working with those of different tenures
To better understand the overall nursing experience, it is important to evaluate each tenure, including the unique needs, preferences, and experiences of the nurses in each tenure, as well as where there is common ground among tenures. Not surprisingly, we found some distinct nuances to each group’s professional experience but also many commonalities to build upon.
Our joint research highlighted that nurses’ experiences working with different tenures may affect how they feel at the end of their shifts (Exhibit 1)—even though nurses are likely to tell you there is no such thing as a typical shift or day for them.
Surveyed nurses were asked to select the top sentiments they felt after working a shift. Early-tenure nurses more often reported feeling supported by midtenure nurses (29 percent) than feeling supported by most-tenured nurses (17 percent). Early-tenure nurses also more often said that they felt frustrated by their most-tenured colleagues (12 percent), compared with midtenure nurses (8 percent). Additionally, early-tenure nurses more often reported feeling intimidated by most-tenured nurses (12 percent) than by their midtenure coworkers (2 percent).
Despite these negative sentiments, however, about 75 percent of early-tenure nurse respondents reported that they agreed or strongly agreed that they enjoyed working with most-tenured nurses. More than 80 percent reported that they viewed most-tenured nurses as “a great resource to learn from” (Exhibit 2). These sentiments were consistent across early-tenure nurses with less than two years of experience and those with more than two years but less than five years of experience.
These two early-tenure nurse subsets differed, however, when reflecting on shifts with midtenure colleagues, most evidently on whether midtenure nurses “have the time and capacity to train and coach them.” About 25 percent of those with less than two years of experience reported that they disagreed or strongly disagreed, compared with about 11 percent of nurses with more than two years but less than five years of experience.
Midtenure and most-tenured nurses were fairly aligned with each other in terms of how they felt about working with early-tenure nurses. Midtenure and most-tenured nurses reported feeling hopeful, like a leader, and respected. Yet they also noted being exhausted and concerned after a shift with early-tenure nurses. In fact, only half of most-tenured and midtenure nurses reported that they got enough support from early-tenure nurses.
This response may indicate that midtenure nurses feel that early-tenure nurses entering the workforce require more support than they can provide (for example, if they are managing more complex patients while also training new joiners). Nonetheless, about 75 percent of both midtenure and most-tenured nurse respondents shared that they enjoyed working with early-tenure nurses (Exhibit 3). Greater than 70 percent of midtenure and most-tenured nurses said they felt energized or personally fulfilled by supporting early-tenure nurses in learning and developing, but more than 33 percent reported that they didn’t have the time or capacity to train or coach others.
Actions to improve collaborative work across tenures
To address the unique challenges facing each tenure and strengthen retention, it is imperative for organizations to evaluate how and where to deploy resources that best match the needs of nurses across their career continuum. To identify tactical, actionable solutions, organizations need a better understanding of what initiatives nurses think could improve the experience of a multitenure workforce and how to create environments that are more collaborative. We also looked at additional cross-cutting strategies for recruitment and retention, such as flexibility.
Ultimately, the interventions an organization chooses will depend on the makeup of its staff and the organization’s goals for its nursing pipeline. However, by using the preferences that the nurses in our survey shared, there are three potential avenues that organizations can consider.
Enhance flexibility for all
Providing schedule flexibility could be helpful not only for nurses who are currently practicing but also to potentially bring back retired nurses. Nearly a third of respondents reported that their employers didn’t offer any type of shift flexibility. Among those who worked at places offering some schedule flexibility, more than 30 percent of early-tenure nurses reported feeling neutral to very dissatisfied with the available options, and 25 percent of midtenure and most-tenured nurses reported the same.
We asked nurses to select all the flexible-schedule options that mattered the most to them (Exhibit 4). Across all tenures, nurses expressed a desire for self-scheduling (for example, everyone gets to select the days and shifts they work for the entirety of the published schedule). This was particularly important for early-tenure nurses, with 46 percent selecting this as an important scheduling option. Additionally, all nurses wanted their employers to offer variable and flexible shift lengths (for example, four, six, eight, ten, and 12 hours). Among early-tenure nurses, 36 percent selected this as a desired scheduling option, while 32 percent of midtenure nurses chose this option. Early-tenure nurses also requested flexible and variable start times (for example, 7:00 a.m., 8:00 p.m., et cetera), while midtenure and most-tenured nurses opted for hybrid working options.
Some organizations have started utilizing technology to support flexible scheduling options. For example, Providence partnered with healthcare platform CareRev to provide unclaimed shifts to nurses or care providers in nontraditional increments, such as 9:00 a.m. to 2:00 p.m., which could then free up nurses to perform daytime activities such as dropping off and picking up their kids from school. 4 “Flexible staffing models cut costs, attract workers,” Becker’s Hospital Review , January 2, 2024. Similarly, SSM Health partnered with the app ShiftMed to offer open shifts to its workforce. The partnership gave SSM Health the opportunity to pilot flexible shift options, start times, and roles and allowed them to fill more than 85 percent of their 25,000 posted shifts per quarter. 5 “How on-demand staffing benefited SSM Health,” Becker’s Hospital Review , December 28, 2023.
The exodus from the workforce of the many nurses nearing retirement age 6 Nursing workforce fact sheet, American Association of Colleges of Nursing, updated July 2023. may mean the loss of decades of expertise and institutional knowledge. Some organizations have implemented programs that provide flexibility and schedule relief to these most-tenured preretirement nurses. Indeed, being able to set their own schedule was the top response among the 1,640 respondents who identified as eligible for retirement, with 46 percent sharing that this would encourage them to consider delaying their retirement. And 45 percent of nurses who were currently or previously retired indicated that this would make them consider rejoining the workforce.
Examples of organizations that have focused on bringing nurses back to their organizations by using flexibility include Henry Ford Health and Northwestern Memorial HealthCare. Henry Ford Health focused on outreach to nurses who left the workforce during the COVID-19 pandemic. It offered flexible opportunities, including internal travel nurse programs and weekend-only options. This strategy resulted in about 25 percent of nurses returning to the organization. 7 Mackenzie Bean and Erica Carbajal, “How Henry Ford rehired 25% of nurses who left during the pandemic,” Becker’s Hospital Review , February 15, 2023. Similarly, Northwestern Memorial HealthCare concentrated on opportunities it called “knowledge worker” roles, which may be less physically demanding than a bedside position and allow nurses to participate in its innovative nursing models, including remote intensive care unit care and virtual nursing. 8 Mackenzie Bean and Erica Carbajal, “How Henry Ford rehired 25% of nurses who left during the pandemic,” Becker’s Hospital Review , February 15, 2023.
Bolster mentorship opportunities
Asking nurses how they felt after working a shift revealed a road map of what they need, as well as the barriers they encounter when nurses don’t have the time or resources to follow this plan. Early-tenure nurses indicated they wanted to learn from their midtenure and most-tenured coworkers, with 18 percent ranking formal mentorship programs as a top initiative to support a positive work environment. About 72 percent of midtenure and most-tenured nurses shared that they felt energized and fulfilled when they could teach and coach their early-tenure colleagues. However, only about 60 percent of midtenure and most-tenured nurses shared that they had adequate time or capacity to coach and teach. This can lead to sentiments of confusion, burnout, intimidation, and frustration.
Although many nurses are already feeling stretched and mentally exhausted, there may be a key group of nurses with the expertise, bandwidth, and desire to support onboarding and mentoring programs. We asked nurses who had not yet retired to select the top three things that their employers could do for them to consider staying in their role. While the ability to set their own schedule was the top response (46 percent), 27 percent reported that being able to work as a nurse educator or in a virtual-nurse capacity would be attractive.
Among nurses who have retired or were previously retired, similar sentiments were shared (Exhibit 5). More than 30 percent reported that being able to serve as an educator or focus on mentoring newer nurses would be enough to make them consider rejoining the workforce.
As a growing number of nurses reach retirement age, organizations have an opportunity to create roles that honor the expertise of these often more-tenured nurses while promoting a work environment that is collaborative and positive for early-tenure nurses. Facilities within the Mass General Brigham healthcare system piloted a formal mentoring program in which early-tenure nurses meet every two weeks for three months with more-tenured nurses. The organization considers this to be paid educational time. Reviews from the pilot show that job satisfaction increased for both new and experienced nurses. 9 “New nurse mentorship program provides ongoing connections, deepens professional investment,” Cooley Dickinson Health Care, April 15, 2022. Similarly, the AARP Center for Health Equity through Nursing is recruiting working and retired nurses for its mentorship program, which is focused on nursing students in underrepresented communities, as part of its Campaign for Action focused on health equity. 10 “Help wanted: Nurse mentors for a more diverse nurse workforce,” Campaign for Action, April 11, 2023.
In addition, adequate support for new graduates entering the workforce was indicated as the number-one contributor toward a positive work environment among all three tenure cohorts. For example, the Practice Transition Accreditation Program, an evidence-based accredited registered nurse residency and fellowship program created by the American Nurses Credentialing Center (ANCC), demonstrated an 85.3 percent retention over 12 months, compared with the industry average of 71.3 percent. 11 “ANCC PTAP accredited programs: Data gathered from PTAP accredited RN programs Oct. 2022–Sept. 2023,” American Nurses Credentialing Center; ANCC is a subsidiary of the American Nurses Association (ANA), while McKinsey’s partner for this research, American Nurses Foundation, is ANA’s research, education, and charitable affiliate.
Promote team building and safe spaces
Personal working styles in any work environment can vary greatly depending on the individual; however, in healthcare specifically, teams should work cohesively and collaboratively. When surveyed nurses were asked to choose the top three most important factors for creating a collaborative working environment, nurses across all tenures selected team building as a top initiative.
Healthcare organizations may not need to look far to find processes to support better collaboration and understanding among team members. Many organizations use after-action reviews following patient safety events to assess and reflect on what went well and what needs to be improved to prevent such future incidents. 12 Catherine Hogan et al., “Effect of after action review on safety culture and second victim experience and its implementation in an Irish hospital: A mixed methods study protocol,” PLoS One , 2021, Volume 16, Issue 11. Additionally, it may be beneficial for departments to conduct more frequent check-ins, huddles, and team-building exercises to give nurses and health professionals an opportunity to share experiences and establish norms for their working culture. Often conducted at the beginning of shifts, huddles may also allow departments to set up working models and provide a platform for staff to get to know one another more informally, which can build trust and professional collaboration.
Another example initiative that could help build a more supportive environment is the Schwartz Rounds program. It was established as a contrast to traditional patient rounding, which tends to focus on patient needs and barriers to care. Instead, the Schwartz Rounds program offers healthcare providers time and space to discuss the social and emotional issues they face while caring for patients and families. The benefits include improved teamwork, better interdisciplinary communication, and a greater appreciation for different roles and disciplines, as well as a decrease in feelings of stress and isolation.
Other actions that stakeholders can consider include establishing and enforcing policies that create space for nurses to feel safe at work. Among early-tenure and midtenure nurses, 12 percent reported that a top priority was formal policies and enforcement against bullying (Exhibit 6). Bullying, incivility, and verbal abuse can lead to a degradation of safe, quality care and affect an individual’s sense of well-being, creating an unhealthy work environment. 13 “Incivility, bullying, and workplace violence,” ANA, July 22, 2015.
Supporting nurses across their career continuum
Addressing the complexity of this multitenure, multigenerational workforce is critical to supporting the healthcare workforce and ensuring an adequate pipeline of nurses eager and engaged in the profession. Many surveyed nurses expressed positive sentiments toward their peers and colleagues but also shared structural challenges that may be preventing them from fully appreciating the potential benefits of a multitenure workforce.
Bolstering cross-tenure relationships would increase trust and collaboration among nurses, not only increasing the likelihood that they stay in the profession but also improving productivity and engagement in real time. How to address these challenges will depend on the makeup of each specific workforce, but stakeholders can start by evolving their workforce strategies to ensure that tenure-specific needs and preferences are considered.
Gretchen Berlin, RN , is a senior partner in McKinsey’s Washington, DC, office, where Faith Burns is an associate partner; Stephanie Hammer, RN , is a consultant in the Denver office; and Mhoire Murphy is a partner in the Boston office. Adriane Griffen is a vice president at the American Nurses Foundation; Amy Hanley is a program manager at the Foundation; and Kate Judge is the executive director of the Foundation.
The authors wish to thank the nurses, physicians, and staff on the front lines who are caring for patients and communities. They also wish to thank Beth Bravo, Brad Herbig, and Deirdre Keane for their contributions to this article.
This article was edited by Querida Anderson, a senior editor in the New York office.
Explore a career with us
Related articles.

Understanding and prioritizing nurses’ mental health and well-being

Nursing in 2023: How hospitals are confronting shortages

Reimagining the nursing workload: Finding time to close the workforce gap

IMAGES
VIDEO
COMMENTS
Nursing workload is affected by staffing levels and the patients' conditions, but also by the design of the nurses' work system. In this chapter, a description of different levels of workload, including situational workload, was offered, and a proposal for a human factors engineering approach aimed at reducing workload or at mitigating or balancing the impact of workload on nurses and ...
This review identifies the body of nursing workload research and establishes the need to include a subjective perception of the nurse as part of any workload measure. Keywords: nursing workload, human factors, subjective mental workload, cognitive workload T he demands in nursing and health care have received increasing attention in recent years.
Typically, papers identify time or some weighting associated with aspects of care or particular groups of patients 'on average'. However, they generally fail to report or consider variability in the underlying estimates. ... However, nursing workload below the optimal level (higher staffing) was associated with improvements in outcomes ...
Heavy workload is a source of distress to nurses, hindering their ability to provide effective patient care. Nursing evidence has established a link between heavy workload, job distress and poor performance (Kokoroko & Sanda, 2019; Li et al., 2017). We surmise that poor quality performance (due to workload factors) is negatively perceived by ...
Increased workload has effects on nurses, manifested through burnout . In the light of nursing presenteeism , which is increasing due to the lack of replacement, job insecurity, etc., there is an increase in the probability of patients suffering adverse events due to poor performance per hour worked. These result in decreased safety and quality ...
Nursing workload and its effects on the quality of nursing care is a major concern for nurse managers. Factors which mediate the relationship between workload and the quality of nursing care have not been extensively studied. This study aimed to investigate the mediating role of implicit rationing of nursing care, job satisfaction and emotional exhaustion in the relationship between workload ...
Introduction. The aim of this commentary paper is to enhance readers' understanding of research design strategies for studying nursing workloads. This paper consolidates key learnings from past nursing workload research that most influenced the research direction of the paper's authors. The current work of two Canadian health services ...
The characteristics of bad nurses offer signs of being overwhelmed (Chang, et al., 2005). Some nurses appear to neglect basis procedures and hygiene requirements (Rauhala, et al., 2007). For example, they have hanging hair, wear dirty shoes and smoke in or around hospitals. Patients complain that nurses neglect them.
Aim: The aim of the present study was to develop a comprehensive understanding of the concept 'workload' within the nursing profession in order to arrive at a clear definition of nursing workload based on the evidence in existing literature. Background: Nursing workload is a common term used in the health literature, but often without specification of its exact meaning.
Nursing workload is a common term used in the health literature, but often without specification of its exact meaning. Concept clarification is needed to delineate the meaning of the term 'nursing workload'. Method. A concept analysis was conducted using Walker and Avant's method to clarify the defining attributes of nursing workload.
The Malawi health system has taken numerous actions to reduce high nurse workloads, despite this, shortage of nurses especially in critical care settings still persists due to lack of prioritisation of critical care. Therefore, it is important to understand the effects of high nursing workload in Intensive Care Unit (ICU). This study aimed at exploring the perceptions of nurses regarding the ...
The COVID-19 epidemic has brought significant changes and complexities to nurses' working conditions. Given the crucial role of health workers, particularly nurses, in providing healthcare services, it is essential to determine the nurses' workload, and its association with the quality of work life (QWL) during COVID-19 epidemic, and to explain the factors predicting their QWL.
Nursing workload is an essential part of nursing literature. It helps estimate required staffing resources and is linked to nurse and patient outcomes, and quality of care. Despite its importance, measuring nurse workload is difficult, and the definition of its predictors is still in its infancy.
Measures of burnout. Most studies used the Maslach Burnout Inventory Scale (n = 81), which comprises three subscales reflecting the theoretical model: Emotional Exhaustion, Depersonalisation, and reduced Personal Accomplishment.However, less than half (47%, n = 39) of the papers measured and reported results with all three subscales. Twenty-three papers used the Emotional Exhaustion subscale ...
Carayon and Gurses (2010) assert that one of the main contributing factors of nurse fatigue in a workplace is high nursing workload. This essay discusses the nature of high nursing workload, the setting in which nursing workload can be observed, its impact on the work environment and quality of care, and its impact on the patient outcomes as ...
Decent Essays. 2656 Words. 11 Pages. Open Document. Hospitals nationwide are experiencing nurse shortage and increased workloads because of shorter hospital stays, fewer support resources and higher acuity in patients (Vahey, D. C., Aiken, L. H., Sloane, D. M., Clarke, S. P., & Vargas, D., 2004). Higher nurse workloads are directly associated ...
The modern health care delivery system is complex and rapidly changing and it is therefore important for nursing staff to work together to secure patient safety (Jomaa et al., 2021) and quality of care (Kalisch et al., 2007; Zeleníková et al., 2020).Teamwork and team-based care are identified as key contributors to patient safety and quality patient care (Mitchell et al., 2012; WHO, 2016).
Nursing Workload and Patient Safety Unlike physicians who spend approximately 30 to 45 minutes per day with a patient, the presence of nurses at the bedside is essential throughout the day. Apart from attending the patients, they regularly interact with families of the sick and other healthcare practitioners, such as physicians and pharmacists.
1 BACKGROUND. Nursing work is complex in nature and capturing its variegation is therefore difficult (White et al., 2015).Previous research estimated nursing workload by calculating nurse-to-patient ratios, nursing hours per patient day, or volume of nursing tasks based on patient complexity classifications (Griffiths et al., 2020).Other researchers suggested including non-patient related ...
Nursing workload measures can be categorized into four levels. Info: 3262 words (13 pages) Nursing Essay. Published: 11th Feb 2020. Reference this. Share this: Facebook Twitter LinkedIn WhatsApp. The most commonly used unit-level workload measure is the nurse-patient ratio. The nurse-patient ratio can be used to compare units and their patient ...
Furthermore, it is imperative that we determine whether multitasking practice patterns increase the cognitive workload of nurses and the likelihood of medication errors in skilled nursing facilities. Implications for Policy or Practice: Healthcare administrators and policymakers should be mindful of the fact that nurses often multitask in ...
📝 Essay description: This essay discusses the nature of high nursing workload, the setting in which nursing workload can be observed, its impact on the work...
Typically, papers identify time or some weighting associated with aspects of care or particular groups of patients 'on average'. However, they generally fail to report or consider variability in the underlying estimates. ... However, nursing workload below the optimal level (higher staffing) was associated with improvements in outcomes ...
The survey results provide insights into opportunities to bridge the experience gap and support nurses across their career continuum. The survey analyzed three specific nurse cohorts: early-tenure nurses (less than five years of nursing experience), midtenure nurses (five to less than 21 years), and most-tenured nurses (21 or more years).