
New cause of diabetes discovered, offering potential target for new classes of drugs to treat the disease
Researchers at Case Western Reserve University and University Hospitals have identified an enzyme that blocks insulin produced in the body -- a discovery that could provide a new target to treat diabetes.
Their study, published Dec. 5 in the journal Cell, focuses on nitric oxide, a compound that dilates blood vessels, improves memory, fights infection and stimulates the release of hormones, among other functions. How nitric oxide performs these activities had long been a mystery.
The researchers discovered a novel "carrier" enzyme (called SNO-CoA-assisted nitrosylase, or SCAN) that attaches nitric oxide to proteins, including the receptor for insulin action.
They found that the SCAN enzyme was essential for normal insulin action, but also discovered heightened SCAN activity in diabetic patients and mice with diabetes. Mouse models without the SCAN enzyme appeared to be shielded from diabetes, suggesting that too much nitric oxide on proteins may be a cause of such diseases.
"We show that blocking this enzyme protects from diabetes, but the implications extend to many diseases likely caused by novel enzymes that add nitric oxide," said the study's lead researcher Jonathan Stamler, the Robert S. and Sylvia K. Reitman Family Foundation Distinguished Professor of Cardiovascular Innovation at the Case Western Reserve School of Medicine and president of Harrington Discovery Institute at University Hospitals. "Blocking this enzyme may offer a new treatment."
Given the discovery, next steps could be to develop medications against the enzyme, he said.
The research team included Hualin Zhou and Richard Premont, both from Case Western Reserve School of Medicine and University Hospitals, and students Zack Grimmett and Nicholas Venetos from the university's Medical Science Training Program.
Many human diseases, including Alzheimer's, cancer, heart failure and diabetes, are thought to be caused or accelerated by nitric oxide binding excessively to key proteins. With this discovery, Stamler said, enzymes that attach the nitric oxide become a focus.
With diabetes, the body often stops responding normally to insulin. The resulting increased blood sugar stays in the bloodstream and, over time, can cause serious health problems. Individuals with diabetes, the Centers for Disease Control reports, are more likely to suffer such conditions as heart disease, vision loss and kidney disease.
But the reason that insulin stops working isn't well understood.
Excessive nitric oxide has been implicated in many diseases, but the ability to treat has been limited because the molecule is reactive and can't be targeted specifically, Stamler said.
"This paper shows that dedicated enzymes mediate the many effects of nitric oxide," he said. "Here, we discover an enzyme that puts nitric oxide on the insulin receptor to control insulin. Too much enzyme activity causes diabetes. But a case is made for many enzymes putting nitric oxide on many proteins, and, thus, new treatments for many diseases."
- Diseases and Conditions
- Hormone Disorders
- Chronic Illness
- Alzheimer's
- Huntington's Disease
- Disorders and Syndromes
- Nitrous oxide
- Diabetes mellitus type 1
- Diabetes mellitus type 2
- Drug discovery
- Nitrogen oxide
Story Source:
Materials provided by Case Western Reserve University . Note: Content may be edited for style and length.
Journal Reference :
- Hua-Lin Zhou, Zachary W. Grimmett, Nicholas M. Venetos, Colin T. Stomberski, Zhaoxia Qian, Precious J. McLaughlin, Puneet K. Bansal, Rongli Zhang, James D. Reynolds, Richard T. Premont, Jonathan S. Stamler. An enzyme that selectively S-nitrosylates proteins to regulate insulin signaling . Cell , 2023; DOI: 10.1016/j.cell.2023.11.009
Cite This Page :
Explore More
- Long Snouts Protect Foxes Diving Into Snow
- Promising Experimental Type 1 Diabetes Drug
- Giant, Prehistoric Salmon Had Tusk-Like Teeth
- Plants On the Menu of Ancient Hunter-Gatherers
- Unexpected Differences in Binary Stars: Origin
- Flexitarian: Invasive Species With Veggies
- T. Rex Not as Smart as Previously Claimed
- Asteroid Ryugu and Interplanetary Space
- Mice Think Like Babies
- Ancient Maya Blessed Their Ballcourts
Trending Topics
Strange & offbeat.

- April 24, 2024 | Quantum Computing Meets Genomics: The Dawn of Hyper-Fast DNA Analysis
- April 24, 2024 | Scientists Turn to Venus in the Search for Alien Life
- April 24, 2024 | NASA Astronauts Enter Quarantine As Boeing Starliner Test Flight Approaches
- April 23, 2024 | Peeking Inside Protons: Supercomputers Reveal Quark Secrets
- April 23, 2024 | A Cheaper and More Sustainable Lithium Battery: How LiDFOB Could Change Everything
Beyond Blood Sugar Control: New Target for Curing Diabetes Unveiled
By Helmholtz Munich March 22, 2024
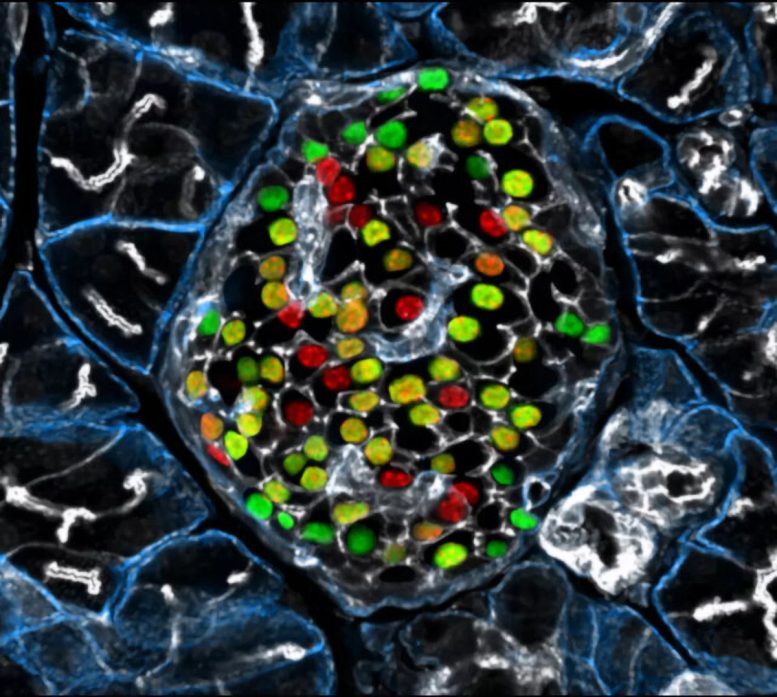
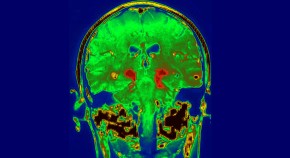
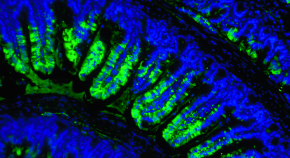
Targeting the inceptor receptor could lead to breakthrough treatments for diabetes by protecting beta cells and improving blood sugar control, with German research institutions leading this promising discovery. Insulin-producing beta cells in the islet of Langerhans. Credit: Helmholtz Munich | Erik Bader
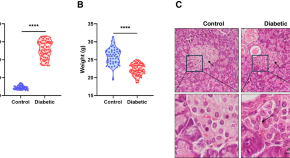
Research focusing on the insulin -inhibitory receptor, known as inceptor, has revealed promising paths for protecting beta cells, providing optimism for therapy that directly addresses diabetes. A groundbreaking study involving mice with obesity caused by diet shows that eliminating inceptor improves glucose management. This finding encourages further investigation into inceptor as a potential therapeutic target for treating type 2 diabetes.
These findings, led by Helmholtz Munich in collaboration with the German Center for Diabetes Research, the Technical University of Munich, and the Ludwig-Maximilians-University Munich, drive advancements in diabetes research.
Targeting Inceptor to Combat Insulin Resistance in Beta Cells
Insulin resistance, often linked to abdominal obesity, presents a significant healthcare dilemma in our era. More importantly, the insulin resistance of beta cells contributes to their dysfunction and the transition from obesity to overt type 2 diabetes. Currently, all pharmacotherapies, including insulin supplementation, focus on managing high blood sugar levels rather than addressing the underlying cause of diabetes: beta cell failure or loss. Therefore, research into beta cell protection and regeneration is crucial and holds promising prospects for addressing the root cause of diabetes, offering potential avenues for causal treatment.
With the recent discovery of inceptor, the research group of beta cell expert Prof. Heiko Lickert has uncovered an interesting molecular target. Upregulated in diabetes, the insulin-inhibitory receptor inceptor may contribute to insulin resistance by acting as a negative regulator of this signaling pathway. Conversely, inhibiting the function of the inceptor could enhance insulin signaling – which in turn is required for overall beta cell function, survival, and compensation upon stress.
In collaboration with Prof. Timo Müller, an expert in molecular pharmacology in obesity and diabetes, the researchers explored the effects of inceptor knock-out in diet-induced obese mice. Their study aimed to determine whether inhibiting inceptor function could also enhance glucose tolerance in diet-induced obesity and insulin resistance, both critical pre-clinical stages in the progression toward diabetes. The results were now published in Nature Metabolism .
Removing Inceptor Improves Blood Sugar Levels in Obese Mice
The researchers delved into the effects of removing inceptor from all body cells in diet-induced obese mice. Interestingly, they found that mice lacking inceptor exhibited improved glucose regulation without experiencing weight loss, which was linked to increased insulin secretion in response to glucose. Next, they investigated the distribution of inceptor in the central nervous system and discovered its widespread presence in neurons. Deleting inceptor from neuronal cells also improved glucose regulation in obese mice. Ultimately, the researchers selectively removed the inceptor from the mice’s beta cells, resulting in enhanced glucose control and a slight increase in beta cell mass.
Research for Inceptor-Blocking Drugs
“Our findings support the idea that enhancing insulin sensitivity through targeting inceptor shows promise as a pharmacological intervention, especially concerning the health and function of beta cells,” says Timo Müller. Unlike intensive early-onset insulin treatments, utilizing inceptor to enhance beta cell function offers promise in alleviating the detrimental effects on blood sugar and metabolism induced by diet-induced obesity. This approach avoids the associated risks of hypoglycemia-associated unawareness and unwanted weight gain typically observed with intensive insulin therapy.
“Since inceptor is expressed on the surface of pancreatic beta cells, it becomes an accessible drug target. Currently, our laboratory is actively researching the potential of several inceptor-blocking drug classes to enhance beta cell health in pre-diabetic and diabetic mice. Looking forward, inceptor emerges as a novel and intriguing molecular target for enhancing beta cell health, not only in prediabetic obese individuals but also in patients diagnosed with type 2 diabetes,” explains Heiko Lickert.
Reference: “Global, neuronal or β cell-specific deletion of inceptor improves glucose homeostasis in male mice with diet-induced obesity” by Gerald Grandl, Gustav Collden, Jin Feng, Sreya Bhattacharya, Felix Klingelhuber, Leopold Schomann, Sara Bilekova, Ansarullah, Weiwei Xu, Fataneh Fathi Far, Monica Tost, Tim Gruber, Aimée Bastidas-Ponce, Qian Zhang, Aaron Novikoff, Arkadiusz Liskiewicz, Daniela Liskiewicz, Cristina Garcia-Caceres, Annette Feuchtinger, Matthias H. Tschöp, Natalie Krahmer, Heiko Lickert and Timo D. Müller, 28 February 2024, Nature Metabolism . DOI: 10.1038/s42255-024-00991-3
More on SciTechDaily

Quantum Breakthrough Reveals Superconductor’s Hidden Nature

Novel Molecules Discovered to Combat Asthma and COVID-Related Lung Diseases

Orbital Engineering, Yale Engineers Change Electron Trajectories

Finding and Erasing Quantum Computing Errors in Real-Time

“Glow-in-the-Dark” Proteins: The Future of Viral Disease Detection?
A black hole – a million times as bright as our sun – offers potential clue to reionization of universe.

Risk Factors for Falls in Older Americans Identified – A Growing Public Health Concern

Common Fireworks Emit Toxic Metals Into the Air – Damage Human Cells and Animal Lungs
1 comment on "beyond blood sugar control: new target for curing diabetes unveiled".
Interesting study and hopefully another tool which will apply to diabetic patients.
Leave a comment Cancel reply
Email address is optional. If provided, your email will not be published or shared.
Save my name, email, and website in this browser for the next time I comment.
Cornell Chronicle
- Architecture & Design
- Arts & Humanities
- Business, Economics & Entrepreneurship
- Computing & Information Sciences
- Energy, Environment & Sustainability
- Food & Agriculture
- Global Reach
- Health, Nutrition & Medicine
- Law, Government & Public Policy
- Life Sciences & Veterinary Medicine
- Physical Sciences & Engineering
- Social & Behavioral Sciences
- Coronavirus
- News & Events
- Public Engagement
- New York City
- Photos of the Week
- Big Red Sports
- Freedom of Expression
- Student Life
- University Statements
- Around Cornell
- All Stories
- In the News
- Expert Quotes
- Cornellians
Large-scale study reveals new genetic details of diabetes
By wynne parry weill cornell medicine.
In experiments of unprecedented scale, investigators at Weill Cornell Medicine and the National Institutes of Health have revealed new aspects of the complex genetics behind Type 2 diabetes. Through these discoveries, and by providing a template for future studies, this research furthers efforts to better understand and ultimately treat this common metabolic disease.
Previous studies have generally examined the influence of individual genes. In research described Oct. 18 in Cell Metabolism, senior co-author Shuibing Chen , the Kilts Family Professor of Surgery at Weill Cornell Medicine, working alongside senior co-author Dr. Francis Collins , a senior investigator at the Center for Precision Health Research within the National Human Genome Research Institute of the U.S. National Institutes of Health, took a more comprehensive approach. Together, they looked at the contribution of 20 genes in a single effort.
“It’s very difficult to believe all these diabetes-related genes act independently of each other,” Chen said. By using a combination of technologies, the team examined the effects of shutting each down. By comparing the consequences for cell behavior and genetics, she said, “we found some common themes.”
As with other types of diabetes, Type 2 diabetes occurs when sugar levels in the blood are too high. In Type 2 diabetes, this happens in part because specialized cells in the pancreas, known as β-cells, don’t produce enough insulin, a hormone that tells cells to take sugar out of the blood for use as an energy source. Over time, high levels of blood sugar damage tissues and cause other problems, such as heart and kidney disease. According to the United States Centers for Disease Control and Prevention, nearly 9% of adults in the United States have been diagnosed with Type 2 diabetes.
Both genetic and environmental factors, such as obesity and chronic stress, can increase risk for it. Yet evaluating the role of the genetic contributors alone is a massive project. So far, researchers have identified more than 290 locations within the genome where changes to DNA can raise the likelihood of developing the disease. Some of these locations fall within known genes, but most are found in regions that regulate the expression of nearby genes.
For the new research, the team focused on 20 genes clearly identified as contributors. They began their investigation by using the gene editing system CRISPR-Cas9 to shut down these genes, one at a time, within 20 sets of identical stem cells.
These stem cells had the potential to generate any kind of mature cell, but the researchers coaxed them into becoming insulin-producing β-cells. They then examined the effects of losing each gene on five traits related to insulin production and the health of β-cells. They also documented the accompanying changes in gene expression and the accessibility of DNA for expression.
To make sense of the massive amount of data they collected, the team developed their own computational models to analyze it, leading to several discoveries: By comparing the effects of all 20 mutations on β-cells, they identified four additional genes, each representing a newly discovered pathway that contributes to insulin production. They also found that, of the original 20 genes, only one, called HNF4A, contributed to all five traits, apparently by acting as a master controller that regulates the activity of other genes. In one specific example, they explained how a small variation, located in a space between genes, contributes to the risk of diabetes by interfering with HNF4A’s ability to regulate nearby genes.
Ultimately, this study and others like it hold the promise of benefiting patients, Collins said. “We need to understand all the genetic and environmental factors involved so we can do a better job of preventing diabetes, and to develop new ideas about how to effectively treat it.”
Collins and Chen note that their approach may have relevance beyond diabetes, to other common diseases, such as Alzheimer’s, Parkinson’s and Crohn’s disease, that involve many genetic factors.
The work reported in this newsroom story was supported in part by the United States’ National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases and the American Diabetes Association.
Many Weill Cornell Medicine physicians and scientists maintain relationships and collaborate with external organizations to foster scientific innovation and provide expert guidance. The institution makes these disclosures public to ensure transparency. For this information, see the profile for Shuibing Chen .
Wynne Parry is a freelance writer for Weill Cornell Medicine.
Media Contact
Krystle lopez.
Get Cornell news delivered right to your inbox.
You might also like

Gallery Heading
These New Developments Could Make Living With Type 2 Diabetes More Manageable

E xperts often talk about the “burden” of a disease or illness. The word acts as a tidy container for all the unpleasantness people with that condition may experience—from their symptoms, to the cost of their care, to the restrictions imposed on their lifestyle, to the health complications that may arise. For people with Type 2 diabetes , this burden can be high.
Routine management of Type 2 diabetes often involves major changes to one’s diet and physical activity . And for many, especially those taking insulin to manage their blood sugar, the disease can necessitate daily blood-glucose monitoring, a process that entails pricking a finger to draw blood and then dabbing that blood onto a glucose monitor’s test strip. Doing this several times a week—month after month—can present overlapping challenges. According to a 2013 survey in the journal Diabetes Spectrum, people find finger-prick glucose monitoring to be painful, and the results can be confusing or unhelpful.
“Patients don’t want to prick their fingers, and they come in all the time and say, ‘I’m tired of this,’” says Dr. Francisco Pasquel, a diabetes specialist and associate professor of medicine at Emory University School of Medicine in Atlanta.
But relief is on the way. Continuous glucose monitors, or CGMs, are small devices-—often about the size of a quarter-—that use a small under-the-skin needle to continuously monitor blood-glucose levels. This information can be transmitted—in some cases wirelessly and automatically—to a smartphone app or other device. “You can look at glucose levels for a single point in time, but you can also look at trends in values over time,” says Dr. Roy Beck, medical director of the nonprofit Jaeb Center for Health Research in Tampa. Beck’s work has found that continuous glucose monitoring may provide a number of benefits for people with Type 2 diabetes.
These monitors are just one of several new advancements in Type 2 diabetes care and management. From connected technologies to new drug treatments, medical science is making steady and sometimes life-changing progress in the treatment of this condition. Here, experts describe some of the latest and greatest developments.
Continuous glucose monitors
People with Type 1 diabetes typically have to check their blood-sugar levels on a daily basis, or even multiple times each day. Because testing is such a big part of managing that disease, the research on continuous glucose monitors started with these patients. That work has shown that CGMs provide multiple benefits, including reduced hemoglobin A1C (HbA1c) levels, which is an important measure of healthy blood glucose. Continuous glucose monitors are now being studied in people with Type 2 diabetes, and research points to multiple benefits.
For a study published in 2021 in the Journal of the American Medical Association, Beck and his colleagues compared continuous glucose monitoring to standard finger-prick tests among people with Type 2 diabetes who were using insulin. They found that continuous monitoring was associated with a significantly greater drop in HbA1c. They also found that continuous monitoring helped people avoid risky and severe drops in blood sugar (a.k.a. hypoglycemia). “It’s pretty clear that there’s a benefit for people with Type 2 diabetes who are using insulin,” he says.
More than 90% of people with diabetes have Type 2 diabetes, and Beck says that roughly 30% of these people are using insulin. In other words, there are many people with Type 2 diabetes who stand to benefit from continuous glucose monitoring. However, use of these monitors is still mostly confined to people with Type 1 diabetes. “Use is slowly increasing in Type 2 patients, but I think it’s still too low considering this is a non-pharmacological approach”—something many people prefer because it avoids the side effects of medications—“that can help people,” he says.
Even for people with Type 2 diabetes who are not taking insulin, Beck says that continuous glucose monitoring could be helpful. “There’s a need for more studies to prove it, but it makes sense that it would likely have benefits,” he says. For example, monitoring blood sugar in real time could help people make diet or lifestyle changes that reduce their risks for long-term health complications. “Normally, blood glucose following a meal shouldn’t go above 140 [mg/dL],” he says. But based on factors like diet, meal timing, and exercise habits, someone with Type 2 diabetes may experience post-meal blood-sugar spikes that surpass 200 or even 300 mg/dL. These spikes could cause few symptoms or short-term consequences, Beck says, but over time they can contribute to the development of common diabetes-related complications such as kidney failure, heart disease, or diabetic retinopathy (an eye condition that can cause blurry vision or blindness). “The first time people use these continuous monitors, it can be a real eye-opener,” he adds. “I think they could be most helpful for self-management, and Type 2 diabetes is a disease where self-management through diet and exercise can make a huge difference.”
Other experts second this. “Patients using these devices can receive a graph of their glucose values over time, which helps them understand the effects of nutrition on glucose control, or how they could modify their exercise to make improvements,” says Dr. Ilias Spanakis, an associate professor of medicine in the division of endocrinology, diabetes, and nutrition at the University of Maryland School of Medicine.
For patients who are reliant on insulin to manage their blood glucose, combining continuous glucose monitors with insulin pumps—devices that automatically inject insulin as needed—could also lead to major improvements. “Smart algorithms that connect the two can automatically adjust glucose based on glucose values,” Spanakis says. This is already possible, and it’s likely to become much more commonplace, he adds.
For many people with diabetes, continuous glucose monitoring could provide a safer and simpler path forward.
Read More: The Link Between Type 2 Diabetes and Psychiatric Disorders
Bariatric surgery for Type 2 diabetes
Historically, bariatric (weight-loss) surgery has been used primarily to help people manage severe obesity, which the U.S. Centers for Disease Control and Prevention defines as a BMI of 40 or higher. Many people who are severely obese also have diabetes, and research has found that these surgical procedures can help reduce the burden of Type 2 diabetes or even send it into remission.
A 2018 study from researchers at the University of Oklahoma found that Roux-en-Y gastric bypass surgery, a common bariatric procedure, vastly outperformed typical medical management techniques—such as diet changes, doctor’s visits, and prescription drugs—among people with Type 2 diabetes. Surgery led to diabetes remission in roughly 28% of patients, compared with a remission rate of just 4% among the non-surgery group, according to the study results. More research has found that bariatric surgery may effectively send Type 2 diabetes into remission.
“Surgery does not just lead to weight loss, but also to an improvement in glycemic control, which happens even before the weight loss occurs,” says Emory’s Pasquel, who has published work on the benefits of bariatric surgery for people with Type 2 diabetes. Exactly how the surgery does this isn’t well understood, he says. However, bariatric surgery affects appetite, food intake, caloric absorption, and multiple neuroendocrine pathways—all of which could contribute to its beneficial actions for people with Type 2 diabetes.
In the future, Pasquel says these procedures are likely to become more commonplace even for people with Type 2 diabetes who are not severely obese.
More from TIME
New pharmaceutical drugs.
There are a lot of different diabetes drugs on the market, each with its own risks and benefits. But experts say two types are emerging as potential “game changers” when it comes to Type 2 diabetes treatment.
Glucagon-like peptide 1 (GLP-1) is a hormone released in the gut during digestion—one that plays a role in blood-sugar homeostasis. A class of drugs known as GLP-1 receptor agonists can interact with GLP-1 receptors in ways that lower appetite, slow digestion, and provide other benefits for people with Type 2 diabetes. These GLP-1 drugs aren’t new. But Pasquel says the latest versions are different in that they work on two different receptors, not one. “Recent evidence shows that activating both receptors has a remarkable impact on weight loss and glycemic control,” he says. Especially for people with Type 2 diabetes who are at high risk for heart or arterial disease, he says that these new drugs seem to be a big upgrade over previous medications.
A second category of drug has also emerged as a standout in the treatment of Type 2 diabetes. Known as sodium-glucose cotransporter-2 (SGLT-2) inhibitors, these drugs help the kidneys remove sugar from a person’s blood. Not only does this improve blood-sugar control in people with Type 2 diabetes, but it also helps protect them from heart failure and kidney disease—two common and serious complications. Pasquel says these drugs are so effective that they’re now being used in people with heart failure or kidney disease who do not have Type 2 diabetes.
Read More: The Truth About Fasting and Type 2 Diabetes
Emerging ways to think about weight loss
Experts have long understood that weight loss can help people reduce their Type 2 diabetes symptoms and risks . This recognition has led to research on a number of weight-loss diets . More research is needed, but some of the latest studies suggest that fasting plans—in particular, intermittent fasting—may be particularly beneficial for people with Type 2 diabetes.
Intermittent fasting involves cutting out calorie-containing foods and drinks for an extended period of time—anywhere from 12 hours to two days depending on the approach a person chooses. A 2019 research review in the journal Nutrients found that intermittent fasting promotes weight loss, increases insulin sensitivity, and reduces insulin levels in the blood. All of this is helpful for people with Type 2 diabetes. “Essentially, fasting is doing what we prescribe diabetes medications to do, which is to improve insulin sensitivity,” says Benjamin Horne, director of cardiovascular and genetic epidemiology at Intermountain Healthcare in Utah.
It’s not yet clear which form of intermittent fasting is best. But Horne says that time-restricted eating—a type of fasting that involves squeezing all the day’s calories into single six- or eight-hour feeding windows—is leading the pack, largely because patients are able to stick with it.
There are more new advancements in Type 2 diabetes care. The interventions described here—from continuous glucose monitors to novel drugs—are some of the most promising, but they have company. It’s safe to say that, looking ahead, more people with Type 2 diabetes will be able to effectively manage or mitigate their symptoms.
More Must-Reads From TIME
- The 100 Most Influential People of 2024
- Coco Gauff Is Playing for Herself Now
- Scenes From Pro-Palestinian Encampments Across U.S. Universities
- 6 Compliments That Land Every Time
- If You're Dating Right Now , You're Brave: Column
- The AI That Could Heal a Divided Internet
- Fallout Is a Brilliant Model for the Future of Video Game Adaptations
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at [email protected]
Featured Topics
Featured series.
A series of random questions answered by Harvard experts.
Explore the Gazette
Read the latest.

How old is too old to run?

America’s graying. We need to change the way we think about age.

Can we talk?
“When my son was diagnosed [with Type 1], I knew nothing about diabetes. I changed my research focus, thinking, as any parent would, ‘What am I going to do about this?’” says Douglas Melton.
Kris Snibbe/Harvard Staff Photographer
Breakthrough within reach for diabetes scientist and patients nearest to his heart
Harvard Correspondent
100 years after discovery of insulin, replacement therapy represents ‘a new kind of medicine,’ says Stem Cell Institute co-director Douglas Melton, whose children inspired his research
When Vertex Pharmaceuticals announced last month that its investigational stem-cell-derived replacement therapy was, in conjunction with immunosuppressive therapy, helping the first patient in a Phase 1/2 clinical trial robustly reproduce his or her own fully differentiated pancreatic islet cells, the cells that produce insulin, the news was hailed as a potential breakthrough for the treatment of Type 1 diabetes. For Harvard Stem Cell Institute Co-Director and Xander University Professor Douglas Melton, whose lab pioneered the science behind the therapy, the trial marked the most recent turning point in a decades-long effort to understand and treat the disease. In a conversation with the Gazette, Melton discussed the science behind the advance, the challenges ahead, and the personal side of his research. The interview was edited for clarity and length.
Douglas Melton
GAZETTE: What is the significance of the Vertex trial?
MELTON: The first major change in the treatment of Type 1 diabetes was probably the discovery of insulin in 1920. Now it’s 100 years later and if this works, it’s going to change the medical treatment for people with diabetes. Instead of injecting insulin, patients will get cells that will be their own insulin factories. It’s a new kind of medicine.
GAZETTE: Would you walk us through the approach?
MELTON: Nearly two decades ago we had the idea that we could use embryonic stem cells to make functional pancreatic islets for diabetics. When we first started, we had to try to figure out how the islets in a person’s pancreas replenished. Blood, for example, is replenished routinely by a blood stem cell. So, if you go give blood at a blood drive, your body makes more blood. But we showed in mice that that is not true for the pancreatic islets. Once they’re removed or killed, the adult body has no capacity to make new ones.
So the first important “a-ha” moment was to demonstrate that there was no capacity in an adult to make new islets. That moved us to another source of new material: stem cells. The next important thing, after we overcame the political issues surrounding the use of embryonic stem cells, was to ask: Can we direct the differentiation of stem cells and make them become beta cells? That problem took much longer than I expected — I told my wife it would take five years, but it took closer to 15. The project benefited enormously from undergraduates, graduate students, and postdocs. None of them were here for 15 years of course, but they all worked on different steps.
GAZETTE: What role did the Harvard Stem Cell Institute play?
MELTON: This work absolutely could not have been done using conventional support from the National Institutes of Health. First of all, NIH grants came with severe restrictions and secondly, a long-term project like this doesn’t easily map to the initial grant support they give for a one- to three-year project. I am forever grateful and feel fortunate to have been at a private institution where philanthropy, through the HSCI, wasn’t just helpful, it made all the difference.
I am exceptionally grateful as well to former Harvard President Larry Summers and Steve Hyman, director of the Stanley Center for Psychiatric Research at the Broad Institute, who supported the creation of the HSCI, which was formed specifically with the idea to explore the potential of pluripotency stem cells for discovering questions about how development works, how cells are made in our body, and hopefully for finding new treatments or cures for disease. This may be one of the first examples where it’s come to fruition. At the time, the use of embryonic stem cells was quite controversial, and Steve and Larry said that this was precisely the kind of science they wanted to support.
GAZETTE: You were fundamental in starting the Department of Stem Cell and Regenerative Biology. Can you tell us about that?
MELTON: David Scadden and I helped start the department, which lives in two Schools: Harvard Medical School and the Faculty of Arts and Science. This speaks to the unusual formation and intention of the department. I’ve talked a lot about diabetes and islets, but think about all the other tissues and diseases that people suffer from. There are faculty and students in the department working on the heart, nerves, muscle, brain, and other tissues — on all aspects of how the development of a cell and a tissue affects who we are and the course of disease. The department is an exciting one because it’s exploring experimental questions such as: How do you regenerate a limb? The department was founded with the idea that not only should you ask and answer questions about nature, but that one can do so with the intention that the results lead to new treatments for disease. It is a kind of applied biology department.
GAZETTE: This pancreatic islet work was patented by Harvard and then licensed to your biotech company, Semma, which was acquired by Vertex. Can you explain how this reflects your personal connection to the research?
MELTON: Semma is named for my two children, Sam and Emma. Both are now adults, and both have Type 1 diabetes. My son was 6 months old when he was diagnosed. And that’s when I changed my research plan. And my daughter, who’s four years older than my son, became diabetic about 10 years later, when she was 14.
When my son was diagnosed, I knew nothing about diabetes and had been working on how frogs develop. I changed my research focus, thinking, as any parent would, “What am I going to do about this?” Again, I come back to the flexibility of Harvard. Nobody said, “Why are you changing your research plan?”
GAZETTE: What’s next?
MELTON: The stem-cell-derived replacement therapy cells that have been put into this first patient were provided with a class of drugs called immunosuppressants, which depress the patient’s immune system. They have to do this because these cells were not taken from that patient, and so they are not recognized as “self.” Without immunosuppressants, they would be rejected. We want to find a way to make cells by genetic engineering that are not recognized as foreign.
I think this is a solvable problem. Why? When a woman has a baby, that baby has two sets of genes. It has genes from the egg, from the mother, which would be recognized as “self,” but it also has genes from the father, which would be “non-self.” Why does the mother’s body not reject the fetus? If we can figure that out, it will help inform our thinking about what genes to change in our stem cell-derived islets so that they could go into any person. This would be relevant not just to diabetes, but to any cells you wanted to transplant for liver or even heart transplants. It could mean no longer having to worry about immunosuppression.
Share this article
You might like.
No such thing, specialist says — but when your body is trying to tell you something, listen

Experts say instead of disability, focus needs to shift to ability, health, with greater participation, economically and socially

Study finds that conversation – even online – could be an effective strategy to help prevent cognitive decline and dementia
When math is the dream
Dora Woodruff was drawn to beauty of numbers as child. Next up: Ph.D. at MIT.
Seem like Lyme disease risk is getting worse? It is.
The risk of Lyme disease has increased due to climate change and warmer temperature. A rheumatologist offers advice on how to best avoid ticks while going outdoors.
Three will receive 2024 Harvard Medal
In recognition of their extraordinary service
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Diabetes articles from across Nature Portfolio
Diabetes describes a group of metabolic diseases characterized by high blood sugar levels. Diabetes can be caused by the pancreas not producing insulin (type 1 diabetes) or by insulin resistance (cells do not respond to insulin; type 2 diabetes).

Macrophage vesicles in antidiabetic drug action
Thiazolidinediones (TZDs) are potent insulin-sensitizing drugs, but their use is accompanied by adverse side-effects. Rohm et al. now report that TZD-stimulated macrophages release miR-690-containing vesicles that improve insulin sensitization and bypass unwanted side-effects.
- Rinke Stienstra
- Eric Kalkhoven
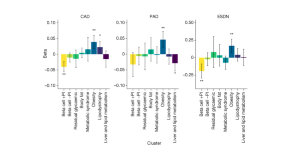
Genetic risk variants lead to type 2 diabetes development through different pathways
The largest genome-wide association study for type 2 diabetes so far, which included several ancestry groups, led to the identification of eight clusters of genetic risk variants. The clusters capture different biological pathways that contribute to the disease, and some clusters are associated with vascular complications.
Related Subjects
- Diabetes complications
- Diabetes insipidus
- Gestational diabetes
- Type 1 diabetes
- Type 2 diabetes
Latest Research and Reviews
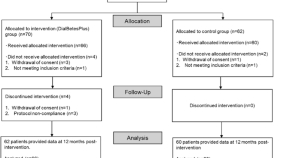
Effectiveness of DialBetesPlus, a self-management support system for diabetic kidney disease: Randomized controlled trial
- Mitsuhiko Nara
- Kazuhiko Ohe
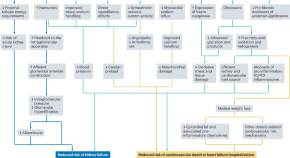
Applications of SGLT2 inhibitors beyond glycaemic control
Here, the authors discuss the beneficial effects of sodium–glucose cotransporter 2 (SGLT2) inhibitors for a range of clinical outcomes beyond glucose lowering, including kidney and cardiovascular protection. They also discuss the need for implementation and adherence initiatives to help translate the benefits of these agents into real-world clinical outcomes.
- Daniel V. O’Hara
- Carolyn S. P. Lam
- Meg J. Jardine
Novel PLGA-encapsulated-nanopiperine promotes synergistic interaction of p53/PARP-1/Hsp90 axis to combat ALX-induced-hyperglycemia
- Rishita Dey
- Sudatta Dey
- Asmita Samadder
Butyrate and iso-butyrate: a new perspective on nutrition prevention of gestational diabetes mellitus
- Weiling Han
- Guanghui Li
Nicotinamide Mononucleotide improves oocyte maturation of mice with type 1 diabetes
- Fucheng Guo
- Xiaoling Zhang
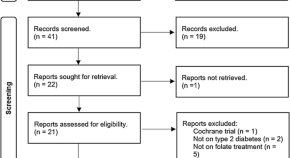
Folic acid supplementation on inflammation and homocysteine in type 2 diabetes mellitus: systematic review and meta-analysis of randomized controlled trials
- Kabelo Mokgalaboni
- Given. R. Mashaba
- Sogolo. L. Lebelo
News and Comment

Repurposing a diabetes drug to treat Parkinson’s disease
In a multicenter clinical trial, patients with early-stage Parkinson’s disease treated with lixisenatide, a drug currently used for the treatment of diabetes, showed improvement in their motor scores compared with those on placebo.
- Sonia Muliyil

A novel system for non-invasive measurement of blood levels of glucose
- Olivia Tysoe
Diabetes drug slows development of Parkinson’s disease
The drug, which is in the same family as blockbuster weight-loss drugs such as Wegovy, slowed development of symptoms by a small but statistically significant amount.
Metformin acts through appetite-suppressing metabolite: Lac-Phe
- Shimona Starling
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- U.S. Department of Health & Human Services

- Virtual Tour
- Staff Directory
- En Español
You are here
Nih research matters.
November 7, 2023
Intermittent fasting for weight loss in people with type 2 diabetes
At a glance.
- People with obesity and type 2 diabetes lost more weight using daily periods of fasting than by trying to restrict calories over a six-month period.
- Blood sugar levels lowered in people in both groups, and no serious side effects were observed.

Around 1 in 10 Americans live with type 2 diabetes, a disease in which levels of blood glucose, or blood sugar, are too high. Diabetes can lead to serious health issues such as heart disease, nerve damage, and eye problems.
Excess weight is a major risk factor for the development of type 2 diabetes, and weight loss is often recommended for those with excess weight and type 2 diabetes. Calorie restriction—reducing overall calorie intake—is a mainstay of most weight loss programs. But such regimens are very difficult to stick with over the long term.
Time-restricted eating, also called intermittent fasting, has emerged as an alternative weight loss paradigm. In this approach, the time of day during which food can be eaten is restricted, but the amount or types of food are not. Small studies have suggested that intermittent fasting is safe and promotes weight loss in people with type 2 diabetes. But these studies only tracked participants for a short period of time. They also didn’t compare the approach with traditional calorie restriction.
In a new clinical trial, an NIH-funded research team led by Dr. Krista Varady from the University of Illinois Chicago compared fasting and calorie restriction for weight loss and blood-sugar reduction. They recruited 75 people with obesity and type 2 diabetes. Of these, 70 were either Hispanic or non-Hispanic Black—two groups in the U.S. with an especially high prevalence of diabetes. The participants were randomly assigned to one of three diet groups for six months.
The fasting group could eat anything they wanted, but only between the hours of noon and 8 pm. The second group worked with a dietitian to reduce their calories by 25% of the amount needed to maintain their weight. A control group did not change their diet at all. All groups received education on healthy food choices and monitored their blood glucose closely during the study. The results were published on October 27, 2023, in JAMA Network Open .
After six months, participants in the fasting group lost an average of 3.6% percent of their body weight compared to those in the control group. In comparison, people in the calorie-restriction group did not lose a significant amount of weight compared to the control group.
Both groups had similarly healthy decreases in their average blood glucose levels. Both also had reductions in waist circumference. No serious side effects, including time outside of a safe blood glucose range, were seen in either treatment group. People in the fasting group reported that their diet was easier to adhere to than calorie restriction.
“Our study shows that time-restricted eating might be an effective alternative to traditional dieting for people who can’t do the traditional diet or are burned out on it,” Varady says. “For many people trying to lose weight, counting time is easier than counting calories.”
Some medications used to treat type 2 diabetes need adjustment for time-restricted eating. Therefore, people considering intermittent fasting should speak with a doctor before changing their eating pattern.
—by Sharon Reynolds
Related Links
- Research in Context: Obesity and Metabolic Health
- Calorie Restriction and Human Muscle Function
- Popular Diabetes Drugs Compared in Large Trial
- Diabetes Control Worsened Over the Past Decade
- Fasting Increases Health and Lifespan in Male Mice
- Factors Contributing to Higher Incidence of Diabetes for Black Americans
- Diabetes Increasing in Youths
- Benefits of Moderate Weight Loss in People with Obesity
- To Fast or Not to Fast: Does When You Eat Matter?
- Managing Diabetes: New Technologies Can Make It Easier
- Type 2 Diabetes
References: Effect of Time-Restricted Eating on Weight Loss in Adults With Type 2 Diabetes: A Randomized Clinical Trial. Pavlou V, Cienfuegos S, Lin S, Ezpeleta M, Ready K, Corapi S, Wu J, Lopez J, Gabel K, Tussing-Humphreys L, Oddo VM, Alexandria SJ, Sanchez J, Unterman T, Chow LS, Vidmar AP, Varady KA . JAMA Netw Open . 2023 Oct 2;6(10):e2339337. doi: 10.1001/jamanetworkopen.2023.39337. PMID: 37889487.
Funding: NIH’s National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK); University of Illinois.
Connect with Us
- More Social Media from NIH
Type 2 Diabetes Research At-a-Glance
The ADA is committed to continuing progress in the fight against type 2 diabetes by funding research, including support for potential new treatments, a better understating of genetic factors, addressing disparities, and more. For specific examples of projects currently funded by the ADA, see below.
Greg J. Morton, PhD
University of Washington
Project: Neurocircuits regulating glucose homeostasis
“The health consequences of diabetes can be devastating, and new treatments and therapies are needed. My research career has focused on understanding how blood sugar levels are regulated and what contributes to the development of diabetes. This research will provide insights into the role of the brain in the control of blood sugar levels and has potential to facilitate the development of novel approaches to diabetes treatment.”
The problem: Type 2 diabetes (T2D) is among the most pressing and costly medical challenges confronting modern society. Even with currently available therapies, the control and management of blood sugar levels remains a challenge in T2D patients and can thereby increase the risk of diabetes-related complications. Continued progress with newer, better therapies is needed to help people with T2D.
The project: Humans have special cells, called brown fat cells, which generate heat to maintain optimal body temperature. Dr. Morton has found that these cells use large amounts of glucose to drive this heat production, thus serving as a potential way to lower blood sugar, a key goal for any diabetes treatment. Dr. Morton is working to understand what role the brain plays in turning these brown fat cells on and off.
The potential outcome: This work has the potential to fundamentally advance our understanding of how the brain regulates blood sugar levels and to identify novel targets for the treatment of T2D.
Tracey Lynn McLaughlin, MD
Stanford University
Project: Role of altered nutrient transit and incretin hormones in glucose lowering after Roux-en-Y gastric bypass surgery
“This award is very important to me personally not only because the enteroinsular axis (gut-insulin-glucose metabolism) is a new kid on the block that requires rigorous physiologic studies in humans to better understand how it contributes to glucose metabolism, but also because the subjects who develop severe hypoglycemia after gastric bypass are largely ignored in society and there is no treatment for this devastating and very dangerous condition.”
The problem: Roux-en-Y gastric bypass (RYGB) surgery is the single-most effective treatment for type 2 diabetes, with persistent remission in 85% of cases. However, the underlying ways by which the surgery improves glucose control is not yet understood, limiting the ability to potentially mimic the surgery in a non-invasive way. Furthermore, a minority of RYGB patients develop severe, disabling, and life-threatening low-blood sugar, for which there is no current treatment.
The project: Utilizing a unique and rigorous human experimental model, the proposed research will attempt to gain a better understanding on how RYGB surgery improves glucose control. Dr. McLaughlin will also test a hypothesis which she believes could play an important role in the persistent low-blood sugar that is observed in some patients post-surgery.
The potential outcome: This research has the potential to identify novel molecules that could represent targets for new antidiabetic therapies. It is also an important step to identifying people at risk for low-blood sugar following RYGB and to develop postsurgical treatment strategies.
Rebekah J. Walker, PhD
Medical College of Wisconsin
Project: Lowering the impact of food insecurity in African Americans with type 2 diabetes
“I became interested in diabetes research during my doctoral training, and since that time have become passionate about addressing social determinants of health and health disparities, specifically in individuals with diabetes. Living in one of the most racially segregated cities in the nation, the burden to address the needs of individuals at particularly high risk of poor outcomes has become important to me both personally and professionally.”
The problem: Food insecurity is defined as the inability to or limitation in accessing nutritionally adequate food and may be one way to address increased diabetes risk in high-risk populations. Food insecure individuals with diabetes have worse diabetes outcomes and have more difficulty following a healthy diet compared to those who are not food insecure.
The project: Dr. Walker’s study will gather information to improve and then will test an intervention to improve blood sugar control, dietary intake, self-care management, and quality of life in food insecure African Americans with diabetes. The intervention will include weekly culturally appropriate food boxes mailed to the participants and telephone-delivered diabetes education and skills training. It will be one of the first studies focused on the unique needs of food insecure African American populations with diabetes using culturally tailored strategies.
The potential outcome: This study has the potential to guide and improve policies impacting low-income minorities with diabetes. In addition, Dr. Walker’s study will help determine if food supplementation is important in improving diabetes outcomes beyond diabetes education alone.
Donate Today and Change Lives!
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
How to Thrive as You Age
A cheap drug may slow down aging. a study will determine if it works.

Allison Aubrey

A drug taken by millions of people to control diabetes may do more than lower blood sugar.
Research suggests metformin has anti-inflammatory effects that could help protect against common age-related diseases including heart disease, cancer, and cognitive decline.
Scientists who study the biology of aging have designed a clinical study, known as The TAME Trial, to test whether metformin can help prevent these diseases and promote a longer healthspan in healthy, older adults.
Michael Cantor, an attorney, and his wife Shari Cantor , the mayor of West Hartford, Connecticut both take metformin. "I tell all my friends about it," Michael Cantor says. "We all want to live a little longer, high-quality life if we can," he says.
Michael Cantor started on metformin about a decade ago when his weight and blood sugar were creeping up. Shari Cantor began taking metformin during the pandemic after she read that it may help protect against serious infections.

Shari and Michael Cantor both take metformin. They are both in their mid-60s and say they feel healthy and full of energy. Theresa Oberst/Michael Cantor hide caption
Shari and Michael Cantor both take metformin. They are both in their mid-60s and say they feel healthy and full of energy.
The Cantors are in their mid-60s and both say they feel healthy and have lots of energy. Both noticed improvements in their digestive systems – feeling more "regular" after they started on the drug,
Metformin costs less than a dollar a day, and depending on insurance, many people pay no out-of-pocket costs for the drug.
"I don't know if metformin increases lifespan in people, but the evidence that exists suggests that it very well might," says Steven Austad , a senior scientific advisor at the American Federation for Aging Research who studies the biology of aging.
An old drug with surprising benefits
Metformin was first used to treat diabetes in the 1950s in France. The drug is a derivative of guanidine , a compound found in Goat's Rue, an herbal medicine long used in Europe.
The FDA approved metformin for the treatment of type 2 diabetes in the U.S. in the 1990s. Since then, researchers have documented several surprises, including a reduced risk of cancer. "That was a bit of a shock," Austad says. A meta-analysis that included data from dozens of studies, found people who took metformin had a lower risk of several types of cancers , including gastrointestinal, urologic and blood cancers.
Austad also points to a British study that found a lower risk of dementia and mild cognitive decline among people with type 2 diabetes taking metformin. In addition, there's research pointing to improved cardiovascular outcomes in people who take metformin including a reduced risk of cardiovascular death .
As promising as this sounds, Austad says most of the evidence is observational, pointing only to an association between metformin and the reduced risk. The evidence stops short of proving cause and effect. Also, it's unknown if the benefits documented in people with diabetes will also reduce the risk of age-related diseases in healthy, older adults.
"That's what we need to figure out," says Steve Kritchevsky , a professor of gerontology at Wake Forest School of Medicine, who is a lead investigator for the Tame Trial.
The goal is to better understand the mechanisms and pathways by which metformin works in the body. For instance, researchers are looking at how the drug may help improve energy in the cells by stimulating autophagy, which is the process of clearing out or recycling damaged bits inside cells.

Shots - Health News
Scientists can tell how fast you're aging. now, the trick is to slow it down.

You can order a test to find out your biological age. Is it worth it?
Researchers also want to know more about how metformin can help reduce inflammation and oxidative stress, which may slow biological aging.
"When there's an excess of oxidative stress, it will damage the cell. And that accumulation of damage is essentially what aging is," Kritchevsky explains.
When the forces that are damaging cells are running faster than the forces that are repairing or replacing cells, that's aging, Kritchevsky says. And it's possible that drugs like metformin could slow this process down.
By targeting the biology of aging, the hope is to prevent or delay multiple diseases, says Dr. Nir Barzilai of Albert Einstein College of Medicine, who leads the effort to get the trial started.
The ultimate in preventative medicine
Back in 2015, Austad and a bunch of aging researchers began pushing for a clinical trial.
"A bunch of us went to the FDA to ask them to approve a trial for metformin,' Austad recalls, and the agency was receptive. "If you could help prevent multiple problems at the same time, like we think metformin may do, then that's almost the ultimate in preventative medicine," Austad says.
The aim is to enroll 3,000 people between the ages of 65 and 79 for a six-year trial. But Dr. Barzilai says it's been slow going to get it funded. "The main obstacle with funding this study is that metformin is a generic drug, so no pharmaceutical company is standing to make money," he says.
Barzilai has turned to philanthropists and foundations, and has some pledges. The National Institute on Aging, part of the National Institutes of Health, set aside about $5 million for the research, but that's not enough to pay for the study which is estimated to cost between $45 and $70 million.
The frustration over the lack of funding is that if the trial points to protective effects, millions of people could benefit. "It's something that everybody will be able to afford," Barzilai says.
Currently the FDA doesn't recognize aging as a disease to treat, but the researchers hope this would usher in a paradigm shift — from treating each age-related medical condition separately, to treating these conditions together, by targeting aging itself.
For now, metformin is only approved to treat type 2 diabetes in the U.S., but doctors can prescribe it off-label for conditions other than its approved use .
Michael and Shari Cantor's doctors were comfortable prescribing it to them, given the drug's long history of safety and the possible benefits in delaying age-related disease.
"I walk a lot, I hike, and at 65 I have a lot of energy," Michael Cantor says. I feel like the metformin helps," he says. He and Shari say they have not experienced any negative side effects.
Research shows a small percentage of people who take metformin experience GI distress that makes the drug intolerable. And, some people develop a b12 vitamin deficiency. One study found people over the age of 65 who take metformin may have a harder time building new muscle.

Millions of women are 'under-muscled.' These foods help build strength
"There's some evidence that people who exercise who are on metformin have less gain in muscle mass, says Dr. Eric Verdin , President of the Buck Institute for Research on Aging. That could be a concern for people who are under-muscled .
But Verdin says it may be possible to repurpose metformin in other ways "There are a number of companies that are exploring metformin in combination with other drugs," he says. He points to research underway to combine metformin with a drug called galantamine for the treatment of sarcopenia , which is the medical term for age-related muscle loss. Sarcopenia affects millions of older people, especially women .
The science of testing drugs to target aging is rapidly advancing, and metformin isn't the only medicine that may treat the underlying biology.
"Nobody thinks this is the be all and end all of drugs that target aging," Austad says. He says data from the clinical trial could stimulate investment by the big pharmaceutical companies in this area. "They may come up with much better drugs," he says.
Michael Cantor knows there's no guarantee with metformin. "Maybe it doesn't do what we think it does in terms of longevity, but it's certainly not going to do me any harm," he says.
Cantor's father had his first heart attack at 51. He says he wants to do all he can to prevent disease and live a healthy life, and he thinks Metformin is one tool that may help.
For now, Dr. Barzilai says the metformin clinical trial can get underway when the money comes in.

7 habits to live a healthier life, inspired by the world's longest-lived communities
This story was edited by Jane Greenhalgh
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

New research directions on disparities in obesity and type 2 diabetes
Pamela l. thornton.
1. Division of Diabetes, Endocrinology, and Metabolic Diseases; National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institutes of Health, Bethesda, MD.
Shiriki K. Kumanyika
2. Drexel University Dornsife School of Public Health, Philadelphia, PA.
Edward W. Gregg
3. Epidemiology and Statistics Branch, Division of Diabetes Translation, Centers for Disease Control and Prevention (CDC), Atlanta, GA. Current Affiliation: Imperial College London, School of Public Health, Epidemiology and Biostatistics, South Kensington Campus, London, UK.
Maria R. Araneta
4. University of California San Diego Department of Family Medicine and Public Health, La Jolla, CA.
Monica L. Baskin
5. University of Alabama at Birmingham Department of Medicine Division of Preventive Medicine, Birmingham, AL.
Marshall H. Chin
6. University of Chicago Medicine, Chicago.

Carlos J. Crespo
7. Oregon Health and Science University and Portland State University joint School of Public Health, Portland, OR.
Mary de Groot
8. Indiana University School of Medicine, Indianapolis, IN.
David O. Garcia
9. University of Arizona Mel and Enid Zuckerman College of Public Health, Department of Health Promotion Sciences, Tucson, AZ.
Debra Haire-Joshu
10. Washington University in St. Louis, School of Medicine and The Brown School, St. Louis, MO.
Michele Heisler
11. University of Michigan Medical School, Ann Arbor, MI.
Felicia Hill-Briggs
12. Johns Hopkins School of Medicine and Welch Center for Prevention, Epidemiology & Clinical Research, Baltimore, MD.
Joseph A. Ladapo
13. David Geffen School of Medicine at the University of California, Los Angeles, Los Angeles, CA.
Nangel M. Lindberg
14. Kaiser Permanente Center for Health Research, Portland, OR.
Spero M. Manson
15. Colorado School of Public Health, Aurora, CO.
David G. Marrero
16. University of Arizona Health Sciences, Phoenix, AZ.
Monica E. Peek
Alexandra e. shields.
17. Harvard/MGH Center on Genomics, Vulnerable Populations, and Health Disparities, Mongan Institute, Mass. General Hospital and Department of Medicine, Harvard Medical School, Boston, MA.
Deborah F. Tate
18. University of North Carolina Gillings School of Global Public Health, Chapel Hill, NC.
Carol M. Mangione
19. David Geffen School of Medicine at the University of California, and UCLA Fielding School of Public Health, Los Angeles, Los Angeles, CA.
The authors of this manuscript provided substantial contributions to its conception by submitting workshop presentations and data described in the manuscript. They also participated in the major revisions of the manuscript’s intellectual content and approved the final version of the submitted manuscript. P.L.T. and S.K.K. designed the manuscript and developed the initial draft; E.W.G. codrafted the epidemiology section; A.E.S. codrafted the psychosocial/socioecological stress section; M.E.P. and M.H.C. drafted Box 1 ; and D.H.-J. drafted Box 2. All authors contributed to the revision of Table 1 .
Obesity and type 2 diabetes disproportionately impact U.S. racial and ethnic minority communities and low-income populations. Improvements in implementing efficacious interventions to reduce the incidence of type 2 diabetes are underway (i.e., National Diabetes Prevention Program), but challenges in effectively scaling-up successful interventions and reaching at-risk populations remain. In October 2017, the National Institutes of Health convened a workshop to understand how to (1) address socioeconomic and other environmental conditions that perpetuate disparities in the burden of obesity and type 2 diabetes; (2) design effective prevention and treatment strategies that are accessible, feasible, culturally relevant, and acceptable to diverse population groups; and (3) achieve sustainable health improvement approaches in communities with the greatest burden of these diseases. Common features of guiding frameworks to understand and address disparities and promote health equity were described. Promising research directions were identified in numerous areas, including study design, methodology, and core metrics; program implementation and scalability; the integration of medical care and social services; strategies to enhance patient empowerment; and understanding and addressing the impact of psychosocial stress on disease onset and progression in addition to factors that support resiliency and health.
Introduction
Obesity and type 2 diabetes are national epidemics that disproportionately impact certain populations in the United States (i.e., disparity populations). Specifically, Alaska Native, American Indian, Asian American, Native Hawaiian and Pacific Islander, non-Hispanic Black, 1 and Hispanic adults bear a disproportionate burden of illness related to these conditions compared to non-Hispanic Whites, 1 , 2 as do those with low socioeconomic status, living in rural areas, and identifying as LGBTQ. 3 Large efficacy trials have demonstrated that lifestyle change and/or medication (i.e., metformin) can prevent or delay progression of prediabetes to type 2 diabetes. 4
Efforts to scale-up and spread efficacious interventions are underway (e.g., National Diabetes Prevention Program), 5 but our knowledge of evidence-based strategies that specifically reduce diabetes-related disparities is limited. Innovative approaches, including strategies to improve available interventions and promote their long-term, wide-spread implementation among those at greatest risk are needed. A central challenge in improving population health is translating research conducted under the best case scenarios of well-resourced randomized controlled trials into real world scenarios, which requires addressing environmental, economic, and social factors that affect individuals’ engagement in and response to these interventions. 6
Workshop overview
The workshop entitled Enhancing Opportunities in Addressing Obesity and Type 2 Diabetes Disparities, was convened at the National Institutes of Health (NIH) in Bethesda, Maryland on October 24–25, 2017 to inform research opportunities for reducing disparities in these two conditions. The workshop was co-sponsored by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), the National Cancer Institute (NCI), and the NIH Office of Disease Prevention (ODP), and organized in coordination with representatives of six NIH Institutes/Offices. 2 Opening remarks by Dr. Griffin Rodgers, the NIDDK Director, and Dr. Eliseo Pérez-Stable, Director of the National Institute on Minority Health and Health Disparities (NIMHD), emphasized the importance of the workshop in identifying focal points for the next generation of high impact studies designed to reduce disparities in the burden of obesity and diabetes through elucidating the social contextual mechanisms of disease etiology, and facilitating lifestyle behavior changes, healthcare system interventions, and partnered community-based programs. Many questions remain, including how best to (1) address the socioeconomic and other environmental influences that have historically and currently affected the same minority populations and under-resourced and rural communities that bear a disproportionate burden of illness; (2) design prevention and treatment strategies to be accessible, feasible, culturally-relevant, and acceptable to at-risk communities; and (3) achieve sustainable health improvement strategies in communities that have the greatest burden of these chronic diseases.
More than 80 participants attended the workshop, including academic researchers and healthcare leaders with expertise in epidemiology, healthcare systems, primary care, behavioral interventions, public health, cultural adaptation of interventions, behavioral economics, health policy and administration, and implementation science. During the 2-day workshop, expert presentations facilitated rigorous discussion and helped identify promising research directions.
Epidemiologic overview
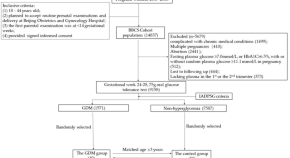
Epidemiological trends illustrate how the obesity and diabetes epidemics have grown in recent decades and the consequent adverse impact on population health. Figure 1 shows marked disparities in diabetes prevalence by race/ethnicity, education, and income. 7 Prevalence of diagnosed and undiagnosed diabetes is highest in non-Hispanic Black and Mexican Adults and notably higher in all three ethnic minority groups when compared with Whites. Based on Indian Health Service data, the prevalence of diagnosed diabetes among American Indians/Alaska Natives is 15%, higher than in the other ethnic minority populations. 8

Prevalence of total diabetes (diagnosed and undiagnosed diabetes) in the U.S. adult population, aged ≥20 years, 2011–2016. NHW, non-Hispanic White; NHB, non-Hispanic Black; MA, Mexican American; HS, high school education; PIR, poverty income ratio. Source: Unpublished data, National Health and Nutrition Examination Survey. 7
Figure 1 also shows the inverse gradients in diabetes prevalence with education and poverty. Figure 2 depicts striking geographic variations in diabetes and obesity prevalence. Evidence indicates that area-level poverty is the strongest single predictor of being a high-risk county. 9 The specific factors explaining why high poverty counties are at such excess risk, and what works to reduce this risk, need to be elucidated. In under-resourced communities, the importance of neighborhood context as a constraint on access to resources and options for healthy eating and active living has been well-documented, 10 , 11 , 12 yet we lack sufficient surveillance data to adequately identify modifiable risk factors in the highest risk neighborhoods.

Diagnosed Diabetes (%): Low (<9.0), Mid (9.0–13.9), High (>13.9); Obesity (%): Low (<29.1), Mid (29.1–36.0), High (>36.0). Estimates are percentages at the county-level; natural breaks were used to create categories using 2016 data.
The effects of education, income, and other indices of SES among people with or at risk for diabetes are often mediated by behavioral risk factors, including dietary patterns, levels of physical activity, and smoking. 13 For example, Siegel et al . 10 reported that, in a nationally-representative survey, higher education was associated with meeting diet-related diabetes prevention goals for intake of vegetables, whole grains, meats, and healthy oils. Lower SES has historically been associated with worse glycemic control among adults with type 2 diabetes, particularly younger adults. 14 , 15 Quality of diabetes care and preventive care practices to forestall diabetes-related complications vary according to disparities in access to care. 16 For example, even among insured populations, Latinos are less likely to receive regular care and less likely to meet HbA1c targets. 17 , 18 Lack of access to care in non-Hispanic Blacks is associated with not meeting blood pressure targets. 19
Although there have been encouraging reductions in most diabetes complications in the United States, with some improvements across all affected groups, disparities remain. They are observed most clearly in non-Hispanic Blacks, who have substantially higher rates of end-stage renal disease (ESRD), amputation, and stroke; 20 and in Hispanics and Asian Americans who have elevated ESRD complications. 21 , 22 Within these groups, men have notably higher rates of lower extremity amputation and myocardial infarction than women. The pattern of disparities in complications according to markers of social class and education does not appear to be consistent.
There have been successes in reducing diabetes-related complications through improvements in medical technology and care, cardiovascular risk factor management and glycemic control, self-management, and policy approaches (e.g., policy changes that have decreased smoking rates or improved access to health insurance and care). 23 , 24 Yet, there has been little success in reducing disparities. Reducing the disparities gap in diabetes and obesity incidence and outcomes requires tackling the social and environmental influences (e.g., neighborhood poverty, access to quality care, psychosocial stressors) known to affect disease etiology and exacerbate disparities. Diverse methods for assessing the effectiveness of interventions to reduce disparities and increase knowledge regarding the pathways and mechanisms through which social disadvantage translates into increased risk of disease are also needed.
Definitions and guiding frameworks
The concepts of health equity and social determinants of health (SDoH) were central to the workshop dialogue. According to the World Health Organization, “‘Health equity’ or ‘equity in health’ implies that ideally everyone should have a fair opportunity to attain their full health potential and that no one should be disadvantaged from achieving this potential.” 25 Improving health equity is a stated U.S. national priority and is inextricably linked to the goal of eliminating health disparities. 26 The concept of equity involves “the absence of avoidable, unfair, or remediable differences among groups of people, whether those groups are defined socially, economically, demographically or geographically or by other means of stratification”. 25 A large body of research demonstrates that such public health goals cannot be realized without addressing the underlying SDoH, which include environmental, economic, and social factors that significantly contribute to disparities and thus warrant much more attention. 27
Several frameworks useful for understanding and addressing health disparities and health equity issues in obesity and diabetes prevention and care were presented. These included a novel healthcare and community systems-oriented model for assessing policy and social/environmental factors influencing health equity, informed by joint analyses of health equity issues affecting ethnic minority populations in the United States and Aotearoa/New Zealand. 28 This model depicts the way government and private policies impact the healthcare system, the integration of healthcare system and social services, and the relevant SDoH, and consequently health equity (e.g., related to race/ethnicity, SES or socioeconomic deprivation)—all set within a larger context of history, culture, and values. Other notable models discussed for conceptualizing health equity issues included: the Robert Wood Johnson Foundation’s “Finding Answers” framework; 29 the Getting to Equity in Obesity Prevention research and action framework; 30 the Three-Axis Model of Health Inequity; 31 the Consolidated Framework for Implementation Research; 32 and behavioral change models involving beliefs, knowledge, social norms, environmental factors, and self-efficacy, and intrinsic and extrinsic motivation. 33 , 34 The NIMHD Research Framework 35 along with the Patient-Centered Outcomes Research Institute (PCORI) perspectives were also featured as valuable resources that illustrate funding agencies’ strategic priorities.
A theme that emerged from these presentations is that, despite sharing common features among health equity frameworks, there is value in having different frameworks for guidance within the policy, practice, and community contexts relevant to prevention and treatment. Some frameworks are designed to explain causes of disparities while others are designed to show where and how solutions to disparities could and should focus. Most frameworks—including those that focus primarily on healthcare delivery systems—acknowledge the importance of community contexts as key health determinants. Other common features among the frameworks were:
- Prominent recognition of the fundamental roles of “race,” ethnicity, SES, gender, and geography in determining health.
- Emphasis on the need to tailor conceptual frameworks according to different health domains and contextual levels.
For example, with respect to the latter, causes rooted in inequitable social structures or inadequate social protections suggest high-level policy solutions, whereas causes related to risky behaviors may point to policy-oriented and individually or family-oriented interventions and the proximal contextual factors influencing these behaviors. Causes of inequities rooted in healthcare system processes could trigger solutions involving regulatory or financing agencies, institutions involved in provider training, and system-level policy mandates addressing ongoing provider training and quality improvement. Regardless, virtually all frameworks emphasize the need for mutually reinforcing interventions at multiple levels, through socioecological models using the traditional concentric circles or other formats, to represent interrelationships among individual, community, neighborhood and/or healthcare- and policy-level influences.
Bridging interventions in healthcare settings to broader community contexts
Interventions in healthcare settings to address obesity and type 2 diabetes-related disparities involve complex considerations at the patient-, provider-, healthcare system and policy-levels. Novel implementation approaches that take account of individuals’ social contexts are necessary for full and sustained achievement of healthy lifestyle behaviors. Although a clinical perspective is considered foundational for diabetes treatment, the traditional clinical context is too narrow to accommodate broader influences on health disparities.
Perspectives and pragmatic lessons
Research agencies, such as PCORI, have shown a growing interest in simultaneously improving healthcare systems and addressing health disparities. Healthcare system interventions designed primarily for populations who face relatively few barriers to accessing care or adhering to medical recommendations may be less effective or even totally ineffective when implemented for patient populations whose access to care and barriers to participation are more challenging. Barriers to quality care and better outcomes that have been documented in the literature include: high and increasing out-of-pocket costs; time or distance factors or lack of transportation which limit access to care; absence of zoning laws and other policies that prevent exposure to adverse neighborhood conditions; unmet social needs; lack of language access, low health literacy, or cultural factors that influence communication; and implicit or explicit racial/ethnic or other biases among healthcare providers, other staff, or other healthcare system issues. 36 – 40
The many ways that unmet social needs influence the effectiveness of treatments was a key workshop theme. As healthcare systems move toward value-based purchasing, models such as accountable care organizations and sharing of costs and savings with payors have increased incentives to address patients’ health-related social needs, or unmet basic needs, to improve patient outcomes. Several of the frameworks discussed suggest ways to remove barriers and mitigate the adverse effects of social needs on treatment effectiveness. Medical interventions that consider social context and patients’ social risk profiles to inform care or directly intervene on SDoH should also consider patient empowerment strategies. Shared-decision making (SDM) or informed care, wherein patients participate as full partners in the medical encounter and select a medical option that suits their values and priorities, was deemed critical. SDM improves outcomes such as patient satisfaction and maintaining treatment regimens; however, certain at-risk groups, such as African Americans, experience SDM less often than Whites, 41 which may exacerbate health disparities. A workshop presentation exemplifies how the integration of medical and social care can improve patient outcomes (see Box 1 ). 34 , 42 – 54
Promising approaches for medical and social care integration
The Improving Diabetes Care and Outcomes on the South Side of Chicago program (known as the South Side Diabetes Project) is a multi-site, multi-targeted intervention designed to address the multiple factors that drive diabetes disparities among low-income racial minorities. The University of Chicago research team works with four federally qualified health centers (FQHCs), each of which is part of a large network of health centers, an academic internal medicine/primary care practice, and an academic endocrinology/diabetes clinic. The intervention is built on the Chronic Care Model and has four key pillars: patient education and empowerment (e.g., culturally tailored skills training in patient/provider communication and shared decision-making), healthcare provider training, quality improvement (QI)/health systems change, and community connections to local resources for diabetes self-management. 34 , 42 – 54 The research team utilized evidence-based strategies to develop the programs, and the intervention has improved patient experience, patient skills and health behaviors, processes within health systems, and diabetes-related health outcomes, including hemoglobin HbA1c, HDL cholesterol, and foot care. 43 – 45 , 50 – 54
The health system and community components of the intervention integrate to provide seamless support for patients’ diabetes management. For example, physicians can write ‘prescriptions’ for healthy food (with an accompanying voucher or coupon) at a neighborhood Farmer’s Market or a participating Walgreens’ store. 47 Once there, patients receive tours of the healthy food items, participate in cooking demonstrations, and are exposed to other hands-on skills training to support healthy lifestyles. Patients who completed the diabetes education classes were more likely to participate in the community-based programs the team has created (e.g., grocery store tours, community exercise programs) than other patients in the health centers. Thus, there may be a greater opportunity to promote sustained behavioral changes among diabetes patients when health system changes (including patient education) are combined with community-based support programs. 49
The South Side Diabetes program has been able to meet people where they are and provide the education, skills and tools they need when they are ready for it, utilizing the infrastructure of the health system and community to support the process. The project continues to expose patients to the various clinical and community components of the intervention and evaluates long-term outcomes as guided by the project’s multi-level/multi-sectoral framework. (See Fig. 1 in Ref. 126 ).
Making the business case for promising interventions
A sound business case is a critical step for supporting the adoption, dissemination, and spread of promising interventions, yet this aspect of interventions is rarely addressed in research. Analyses of costs, who bears them, and who benefits from the investment are recommended to promote sustained investments by payors and avoid the discontinuation of high-value effective interventions, as observed in previous prevention efforts. 55 Without an equity lens, most current payment mechanisms do not support or incentivize the provision of tailored care approaches necessary to reduce disparities. A key factor is the period in which the return on investment (ROI) is expected. Private insurers or agencies with clients that incur high costs may fear losing them before ROI occurs. For example, there is potential for loss of ROI because of relocations, job and insurance changes, or temporal gaps in coverage due to lack of affordability or strict health insurance eligibility criteria.
Addressing social determinants in community and neighborhood contexts
Workshop participants discussed research on three types of interventions to address social determinants of health in community and neighborhood contexts. Two types represent compensatory interventions that provide supports that enable individuals to fill gaps and access otherwise inaccessible or unavailable resources to overcome influences of negative SDoH. 6 The third type concerns root cause 27 , 56 oriented interventions designed to change underlying structures/systems rather than compensate for them.
Community Health Worker (CHW) programs
Community Health Worker (CHW) interventions represent a key compensatory strategy to address gaps in healthcare system access, communication and navigation, and the integration of social and healthcare needs. 6 CHWs are trained, frontline public health workers or extended healthcare team members, who often share characteristics (community, culture, and language) with their clients (individuals or families). 3 They typically garner trust and provide cultural mediation among community members, healthcare systems, and social services; and deliver culturally relevant and accessible program content, informal counseling, coaching, and advocacy for clients to ensure their needs are met. 57 – 59 Models of care vary, as CHWs may work alone or as part of delivery teams to conduct a range of activities effective for preventing and managing chronic diseases, promoting the use of primary care and follow-up care, reducing unnecessary utilization, and providing outreach and navigation to social and community services. 60 CHWs and lay persons who complete training as Diabetes Prevention Program (DPP) lifestyle coaches are being tested on a national scale for effectiveness in achieving DPP-related lifestyle change and behavioral outcomes among people at increased risk for type 2 diabetes. 61 Interventions engaging CHWs can improve glycemic control and weight-related outcomes among people at increased risk for type 2 diabetes, be cost effective, and thus are deemed to play an important role in reducing health disparities, improving minority health, and enhancing health equity when implemented in under-resourced communities. 60
Remotely delivered Intervention formats
The increasing use of internet, mobile phones/smart phones, and social media in the highly digitized economy of the 21st century has enabled tests of remotely delivered approaches to expand reach of and access to effective prevention and treatment programs. The potential convenience and enhanced options for people with limited access, including some in racial/ethnic minority populations, low-income populations and rural populations, 62 foretell substantial gains for prevention and treatment. The literature on effectiveness of remotely delivered approaches to treat obesity is promising, but the effects specific to minority populations are understudied. A systematic review of eHealth interventions for weight management shows interventions for the prevention and treatment of adult obesity have generally been effective compared to usual care or controls but with modest weight losses. 63 Few studies had 50% or more participants from racial or ethnic minority groups or outcomes reported by race. 63 Subsequent studies have demonstrated the acceptability and feasibility of remotely delivered obesity programs and suggest strategies to enhance recruitment of African Americans and Hispanics. 64 A trial with predominantly Hispanic women participating in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) program found that an internet-based weight loss program in addition to WIC resulted in significantly greater weight loss over 12 months compared with the WIC program alone. 65
Intervening on neighborhood contexts
Physical, or built , environments can profoundly shape health and health behaviors related to eating and physical activity. Relevant interventions include: making improvements to physical infrastructures (safe/walkable neighborhoods, recreational facilities, convenient transportation choices, access to healthy foods), and complementary policy and messaging strategies. Such strategies require a systems approach, with coordinated action by multiple sectors and disciplines (e.g., community stakeholders, economists, urban and regional planners, social scientists) within and outside of the biomedical-behavioral fields. Moving to Opportunity, a randomized social experiment offers convincing evidence of the impact of one’s neighborhood environment on diabetes and obesity. 66 Neighborhood change was effected by affording women with children the opportunity to move from a neighborhood with high poverty rates to a neighborhood with lower poverty rates. Moving was associated with lower obesity and diabetes biomarkers and reductions in prevalence of obesity and diabetes. 66
Improving community engagement and cultural relevance
Efforts to maximize effectiveness of interventions targeting obesity and diabetes in racial/ethnic minority, rural or other under-resourced communities further underscore the significance of social context and cultural relevance. Presenters discussed their experiences working with Black Americans, Hispanic Americans, Asian Americans, and American Indians and Alaska Natives (AI/AN).
Theoretical and conceptual frameworks
Two complementary cultural adaptation frameworks are widely used in this arena. Resnicow et al . differentiate between adaptations of surface or deep structure . 67 Surface structure adaptions are relatively superficial, such as, matching intervention components to observable characteristics of the population group of interest, while deep structure adaptations incorporate elements of the relevant core values and key cultural practices of community members. 67 Kreuter et al. describe five specific types of cultural tailoring: peripheral tailoring is similar to Resnicow’s surface structure; evidential tailoring refers to using data showing relevance of the problem; linguistic tailoring refers to using the preferred language(s); constituent tailoring involving approaches base adaptations on information obtained through direct engagement with members of the population of interest; and sociocultural tailoring— similar to deep structure — incorporates relevant core values and sociocultural perspectives and other health determinants. 68 Examples from The Special Diabetes Program for Indians (SDPI) underscores the anthropological perspective on culture, that is, deep structure. Culturally influenced explanatory models of illness and how symptoms are interpreted may differ markedly from the views of health providers, 69 which was an implicit or explicit theme across many workshop presentations.
Definitions of culture in practice
Counseling for obesity and diabetes-related behavior changes addresses similar variables for all populations: for example, dietary patterns and food preferences, body image, physical activity, and sedentary behavior. What is referred to as “cultural” encompasses a broad array of social and environmental contexts: the nature and level of desired and available family and social support; natural and built physical environments that affect food access and options for physical activity; economic factors; and various logistical challenges that influence whether people can achieve the intended level of intervention attendance. At any given level of motivation, these factors shape or interact with health-related knowledge, norms, values, and beliefs to influence behavior or behavior change. Thus, cultural adaptations must consider ways to help people navigate challenges they encounter in attempting to following recommendations for weight loss or diabetes self-management during and after a program. A common theme was that effective interventions must be grounded in a deep understanding of both culture and contextual variables, both how these variables interact with each other and how they affect individuals and communities. Intersections among various influences were also stressed. For example, understanding how obesity and diabetes management in Black women in the Deep South (e.g., rural Alabama and Mississippi) may be influenced not only by race and gender, but also by regional, rural, and economic factors. 70 , 71
For Asian Americans, the definition of obesity itself is problematic. Current guidelines and practice lead to underdiagnosis of obesity among Asian Americans by clinicians and national surveys. Obesity as assessed by body mass index (BMI) may lead Asian Americans to also underestimate their obesity-related risks. Diabetes prevalence in Asian Americans is higher than would be expected based on their average BMI levels, and is more similar to that in Black and Hispanic Americans than in Whites ( Fig. 1 ). 72
BMI is particularly inadequate for reflecting risks related to body fatness and body fat distribution in diverse Asian American populations. If risk is not recognized, there is insufficient triggering of preventive and treatment interventions. In 2015, the American Diabetes Association revised the BMI cut point for diabetes screening among Asian Americans to BMI≥ 23 kg/m 2 . 73 Awareness and implementation of these revised guidelines among clinicians and Asian American communities have not been evaluated, but reinforces the need to adapt health messaging to the culture of Asian Americans. 73 , 74
For example, Filipino Americans with normal BMI have significantly more visceral adipose tissue (by computed tomography) compared to clinically obese African Americans, 75 while South Asians have excess hepatic fat accumulation. 76 Differences in diabetes prevalence among Asian American subgroups emphasize the importance of disaggregating Asian American subgroups; diabetes prevalence in California was highest among Pacific Islanders, Filipinos, and South Asians (from India, Pakistan, Bangladesh, Sri Lanka) compared to groups often perceived to be at highest risk for diabetes, including non-Hispanic Blacks, Hispanics and Native Americans. 77 Diabetes risk was 50% higher among Southeast Asians, Japanese, Vietnamese, Koreans, and Chinese Americans compared with White populations, with onset of diabetes occurring at lower BMI levels. 77 Understanding the unique pathophysiology of type 2 diabetes, including regional fat distribution, in specific Asian American communities, is urgently needed to inform effective interventions in this rapidly growing population. Raising awareness of body composition and metabolic profiles in subgroups of Asian Americans is also needed to improve interventions aimed at reducing diabetes within these communities.
Success stories and promising approaches
While culturally and contextually adapted interventions constitute a relatively small portion of the evidence base regarding obesity and diabetes interventions, all presenters provided evidence of successful approaches. For example, the potential value and practicality of using individually tailored, small changes approaches to prevent excess weight gain in Black women was noted. 78 Among Hispanic women, preintervention educational approaches that provide basic information on diabetes, food measurement or nutrition facilitate intervention uptake and improve success in behavioral weight loss programs. 79
Because of its scope and special features, the SDPI was highlighted as an exemplar of cultural and contextual adaptations. The successes of this program attest to the value of: having a year-long process for strategic planning and increasing community readiness; building upon cultural strengths and traditions; incorporating family in the intervention process; emphasizing collective as well as individual support; and ongoing reinforcement of core principles for success among families, providers, and in the community at large. 80 , 81
Psychosocial and socioecological stress as an emerging theme
Increasingly, epidemiological research investigating factors associated with risk of chronic diseases such as diabetes and obesity is focusing on understanding the underlying biological pathways or mechanisms through which social disadvantage “gets under the skin” to increase risk of disease, thus potentially identifying new leverage points for intervention. The importance of identifying biomarkers to elucidate mechanisms through which stressors increase risk of disease was also presented. Psychosocial stress, which includes diverse stressors at the individual and community levels (e.g., physical and sexual abuse, neighborhood-level poverty, work stress, discrimination), has been shown to increase individuals’ risk of many chronic diseases. For example, self-reported experiences of discrimination has been associated with increased visceral fat in women, 82 and increased risk of type 2 diabetes independent of obesity or behavioral and psychosocial factors. 83 Stress at work and home, financial stress, depression, and perceived ability to control life circumstances have been associated with increased risk of acute myocardial infarction. 84 Because certain psychosocial stressors (e.g., exposure to violence, social position, trauma) are disproportionately experienced by poor and minority communities in the United States, 85 investigating the underlying mechanisms through which such stressors operate to increase risk of disease is a critical piece of the puzzle in eliminating disparities in the burden of illness. 86
Dysregulation of the stress pathway is one way in which adverse psychosocial exposures becomes embodied. Human experiments show that both emotional and physical stressors trigger the central stress response and neuroendocrine systems, which can result in a cascade of hormonal changes linked to increased risk of obesity, metabolic syndrome, and poor glycemic control. 87 While animal models have illuminated some of the key mechanisms at play, it is impossible to use these to model the diverse stressors faced by humans. Key variables for future studies include inherited and acquired personal characteristics (e.g., physiology/genetic, personality type, past trauma, perceptions of the stress) and characteristics of the stressor (e.g., severity, duration, frequency). DNA methylation provides a valuable platform for investigating the impact of various psychosocial stressors on risk of disease. Altered DNA methylation in hypothalamic–pituitary–adrenal axis (i.e., stress related) genes has been associated with increased risk of hypertension, certain cancers, and post-traumatic stress disorders. 88 Telomere length is another valuable biomarker for exploring the role of psychosocial stress in disease. Telomeres contribute to cell senescence and longevity, and measures of psychosocial stress have been associated with accelerated telomere shortening. 89
Research is also beginning to focus on positive psychosocial factors thought to support resiliency and health. Mind-body stress-reduction interventions such as the Relaxation Response Resiliency (3RP) Program or meditation, for example, have been shown to enhance expression of genes associated with favorable energy metabolism, insulin secretion, and telomere maintenance; 90 , 91 and suggest a positive benefit for cardiovascular health and reducing blood glucose levels. 92 , 93 Religion and spirituality have emerged as potentially important sources of resiliency for minority and low-income communities, 94 and may be particularly important for African American and Hispanic/Latino communities who report higher levels of religious and spiritual beliefs and practices than White and Asian American populations. 95 In a recent national study of African American women in the United States; for example, those who used religion or spirituality to cope with stress were significantly less likely to develop hypertension, and this protective effect was greater among those with the highest levels of perceived stress. 96 The same impact of religious coping on risk of hypertension was not found in a national sample of White women. 97 Social support has also been shown to buffer the adverse effects of stress on one’s health, with evidence from randomized controlled trials and experimental studies showing that various facets of social support improve diabetes control (HbA1c) and diabetes-related physical activity, weight loss, and quality of life. 98 – 100
Evidence in the areas of socioecological and psychosocial stress is long-standing and provides emerging opportunities to improve obesity and diabetes prevention and treatment. Future challenges include modeling the complexity of these interactions as well as determining any differences in patterns of stress across and within different racial/ethnic and socioeconomic groups. Equally important are studies investigating positive resources for resiliency, which may help identify and prioritize additional areas for intervention. Ultimately, there is a need to identify and better understand effective strategies to minimize the adverse effects of psychosocial stress on diabetes and obesity outcomes and remove, where possible, the adverse stressors that disproportionately impact minority and other underserved populations.
Frameworks for understanding mental health and diabetes distress
Mental health conditions such as depression and diabetes-related distress are known risk factors for obesity and type 2 diabetes. 101 Depression can induce neuroendocrine reactivity and metabolic consequences resulting in obesity and type 2 diabetes. 87 , 102 Evidence from epidemiological studies show that depression is both a risk factor for diabetes as well as a comorbid condition of diabetes. Depression is up to twice as common among individuals with diabetes compared to those without the condition; 103 , 104 and has consistently been associated with higher risk of diabetes complications, 105 poorer quality of life, 106 and increased risk of mortality. 107 , 108 Pharmacological treatments, such as antidepressant use, are associated with the risk of incident type 2 diabetes among adults 102 , 109 , 110 and youth; 111 and the use of antipsychotic drugs is associated with high fasting blood glucose and diabetes-related complications. 109 Additionally, cultural misunderstandings and clinician bias have resulted in prescribing more and higher doses of antipsychotic medications to African Americans compared with Whites, possibly without awareness of the potential higher sensitivity of some African Americans to certain psychotropic medication, causing more severe side effects (e.g., delirium). 112 Clinicians are cautioned to avoid under or overtreatment for mental health conditions by examining patient-specific drug sensitivities and by taking cultural factors into account. Given the potential for adverse side effects of drugs used to treat mental illness and evidence that culture and ethnic factors influence provider bias, 112 studies of appropriate prescribing and diagnostic accuracy are urgent research needs.
Diabetes-related distress, another psychosocial condition, refers to unique often hidden “emotional distress in diabetes that emphasizes the demanding experience of diabetes and requires diabetes-specific measurement and treatment approaches” (p. 236) 113 and “the spectrum of patient experience when managing a severe, demanding chronic disease like diabetes” (p. 259). 114 Diabetes distress is considered common and persistent over time, 114 with higher rates among ethnic diverse patients than non-Hispanic Whites. 115 Diabetes-related distress is associated with diabetes self-care and elevated HbA1c, which in turn increases the risk for the development of diabetes complications, 116 , 117 but this consideration may not be reflected in current healthcare practice.
Research translation: challenges and opportunities
A cross-cutting discussion focused on the central challenges of moving from efficacy studies (i.e., the best-case scenarios that provide convincing evidence of what can work) to demonstrating effectiveness in terms of what works in diverse and particularly under-resourced communities. A concern—and frustration—related to repeated observations that research findings from efficacy studies are not reaching populations at large, especially higher risk populations, in ways that fulfill the promise inherent in this research 118 was frequently voiced by workshop participants. The relevance of models typically used in efficacy studies to effectiveness research in real-world settings was questioned based on differences in both participant and intervention characteristics. Workshop participants’ views on this problem echoed several themes from the discussion about community engagement and cultural relevance as well as other sessions, framing the issues as contrasts between efficacy and effectiveness research. Overall, workshop participants emphasized that better translation science and efforts are needed, and this reflects a broader concern in the field. 118
Population characteristics and circumstances
Even when participants from high-risk populations are included in efficacy studies, the screening and selection into these studies achieve a certain level of homogeneity on variables related to the ability to participate. Because unbiased interpretation of efficacy trials requires achievement of the intended intervention dose and high participant retention, extraordinary measures may be taken to mitigate circumstances that constrain the necessary level and quality of participation. By contract, recognizing and allowing for heterogeneity on variables such as cultural perspectives, attitudes and behaviors, and socioeconomic circumstances, neighborhoods, built environments and resources (transportation, etc.) among these population groups become critical in community-based research if the research findings are to be meaningful in practice. Factors related to healthcare access, delivery patterns and out-of-pocket costs must be considered inasmuch as they determine the context for adoption and maintenance of health behavior changes. The rise of high deductible health plans and limited benefits have decreased the affordability of healthcare especially for employed persons with limited incomes. 119 For people who are not U.S. citizens, immigration-related factors related to employment or fear of deportation may be an important overlay influencing program participation or use of healthcare. 120 These factors, if not recognized or understood, can lead to inappropriate assumptions, e.g., that low motivation, rather than practical issues or preferences, is the main reason for lower participation rates or suboptimal behavioral outcomes.
Intervention characteristics
The time and logistical demands of attending a series of classes or counseling sessions can be prohibitive, particularly given competing demands on time or other practical constraints as noted above. Possible ways to address this include data collection to better understand these constraints, combined with testing more flexible ways of delivering interventions. A distinction was made between achieving flexibility versus reducing participant burden by limiting the dose (e.g., minimal models for lifestyle intervention). The content or frequency needed to achieve the optimal effect of interventions is not always clear. One approach that might increase the feasibility and sustainability of interventions would be linking them to ongoing, community services (e.g., linking to commercial weight loss programs which are more consumer or client oriented, and sustainable, than researcher-designed approaches). One example is the aforementioned remote intervention linked to WIC 65 that embeds interventions in federal or state-funded programs which reach low-income populations to expand dissemination efforts across diverse populations in settings that are integral to people’s daily lives. Box 2 highlights an example of linking nutrition and physical activity counseling to services provided by a national parent support organization. 121 – 123 Such approaches may allow for the needed dose of interventions to be achieved over a longer period, or intermittently, compared to the typical approach of providing a high, front-end dose within a concentrated period.
Promising approaches for delivering and scaling-up obesity prevention programs: translations in underserved communities nationwide
Two studies conducted in St. Louis Missouri, which embedded weight loss counseling based on the principles of the Diabetes Prevention Program (DPP) within a national home visiting program, showed substantial promise for obesity prevention with widespread reach. The home visiting program, Parents as Teachers National Center, Inc. (hereafter referred to as parents as teachers or PAT), trains and coordinates the services of parent-educators who promote early development, learning, and school readiness through ongoing support to families with children from prenatal through kindergarten ( https://parentsasteachers.org/ ). Families can receive up to 25 home visits annually, depending on need. Importantly, PAT uses a resource network to provide comprehensive services to families and children (e.g., unmet basic needs such as housing, food) to ensure optimal early development, health and children’s school readiness and success. PAT is located in all 50 states and reaches over 225,000 children annually.
The Healthy Eating and Active Living Taught at Home (HEALTH) Study was designed as a 2-year randomized study to assess the impact of a DPP-derived lifestyle weight loss intervention embedded within the PAT curriculum. 121 PAT + HEALTH was compared with PAT only (usual care) in a cohort of 179 ethnically and socioeconomically diverse women with overweight or obesity (BMI ≥25) and a pre-school child at home. Women in PAT + HEALTH were more likely than those in usual care to achieve 5% weight loss at 24 months (11% vs 26%, p =0.01), with a 4.7-kg weight difference ( p =0.002). Notably, the weight difference between groups was attributed to the intervention group’s maintenance of a modest loss of weight versus the control group continuing to gain weight, indicating the value of this strategy for reversing obesity trends by preventing weight gain overtime.
Similarly, the LifeMoms–Washington University Program compared the PAT curriculum to the PAT + Lifestyle intervention, conducted with pregnant and post-partum African American women with overweight or obesity, living with significant socioeconomic disadvantage (e.g., Medicaid recipients or living in low-income neighborhoods, 90 percent reporting household incomes of less than $25,000 annually, and approximately half being single parents). By 12 months postpartum, the PAT + Lifestyle group had gained less weight (2.5 kg vs. 5.7 kg; P = 0.01) and were more likely to return to their baseline weight (38.0% vs. 21.5%; P = 0.01) than those receiving the PAT curriculum. 122 , 123
The scalability of these embedded lifestyle interventions offers the potential to partner with existing national programs like PAT and leverage infrastructure to reach underserved mothers who have extensive barriers to care for widespread intervention dissemination, reach, and impact.
Additionally, greater use of telephone or digital technology to deliver or tailor interventions 64 was discussed as having a high potential because many high-risk populations are heavy users of web- or cell-technologies. 124 However, limitations on broadband access were noted as a potential issue to be resolved for rural populations. 125
Promising research directions to address obesity and type 2 diabetes disparities consider at the person-, community/neighborhood-, and system-levels, and are guided by frameworks to promote health equity (see Table 1 ). Translating lifestyle interventions for diverse communities requires research to demonstrate the effectiveness of interventions that are affordable, accessible, convenient, and sensitive to socioecological contexts, and offer equitable access to these interventions. The adoption of health equity approaches in intervention design (e.g., engagement and recruitment, implementation strategies) are needed. The ultimate goal of investments in this research would be to promote individuals’ engagement in evidenced-based interventions and help population groups reduce exposure to or overcome the effects of practical and stress-related challenges in their physical, sociocultural, and economic environments.
Promising research directions for obesity and type 2 diabetes
Intervening on the SDoH can improve health inequity by removing systemic barriers, thereby addressing root causes of obesity and diabetes-related disparities, and helping individuals overcome contextual challenges related to prevention and self-care. Novel research approaches could account for community realities and resources and treat neighborhoods as focal points for intervening on the compelling geographic variations in health. Implementation efforts can also leverage national and state-wide programs to expand reach of evidence-based interventions to diverse communities and intergenerational households. Importantly, high-impact research opportunities that leverage health equity approaches may identify ways to interrupt the intergenerational consequences of obesity and diabetes; and more effectively treat individual, families and communities that are currently affected to support reaching their highest health potential.
Acknowledgements
Additional substantial contributions to the development of this manuscript were made by Dr. Joseph Selby who provided a scientific presentation and contributed to rigorous participant deliberations at the workshop that informed Table 1 . M. Austin Argentieri affiliated with the Harvard/MGH Center on Genomics, Vulnerable Populations, and Health Disparities assisted with coediting the psychosocial/socioecological stress section and technical editing. The authors wish to acknowledge the contributions of the NIDDK for initiating and co-funding the workshop effort, the trans-NIH workshop organizing committee for substantial contributions to the workshop program; and the National Cancer Institute Division of Cancer Control and Population Sciences, and the NIH Office of Disease Prevention for cosponsoring the workshop with travel support for presenters. The authors also acknowledge and appreciate contributions of Dr. Griffin Rodgers, director of the NIDDK, and Dr. Eliseo Pérez-Stable, director of the NIMHD, for their presentations to set the tone of the workshop deliberations.
The workshop was co-funded/co-sponsored by the NIDDK, NCI, and ODP.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institutes of Health, the National Institute of Diabetes and Digestive and Kidney Diseases, or any other institution mentioned in the manuscript.
Competing interests
M.H.C. is a consultant to the Patient-Centered Outcomes Research Institute and a member of the National Advisory Council to the National Institute on Minority Health and Health Disparities. M.D.G. is a faculty consultant to the Lifescan Diabetes Institute and Eli Lilly, Co. C.M.M. is a member of the U.S. Preventive Services Task Force. This article does not necessarily represent the views and policies of the U.S. Preventive Services Task Force. D.F.T. is a member of the WW Scientific Advisory Board.
1 Also referred to in this manuscript as African American or non-Hispanic Black based on the data source.
2 National Institute of Diabetes and Digestive and Kidney Diseases; the National Cancer Institute; the NIH Office of Disease Prevention; National Heart, Lung, and Blood Institute; National Institute on Minority Health and Health Disparities; and NIH Office of Behavioral and Social Sciences Research.
3 Community Health Workers are also known by a variety of names, including community health aide, promotora/promotores de salud, and patient navigator.
Diabetes in Young People Is on the Rise

Both type 1 and type 2 diabetes affect kids and teens. Stay up to date on the latest research.
How is diabetes in kids and teens projected to increase in 40 years? New research shows what might be coming.
What’s important about this study?
Both type 1 and type 2 diabetes can develop at any age. This study shows how both types of diabetes are projected to increasingly affect kids and teens in the next 40 years. It also emphasizes the importance of diabetes prevention (when possible) and management.
What did this study examine?
Researchers used data from 2002 to 2017 to study the increasing rate of young people under age 20 with type 1 or type 2 diabetes. They then used mathematical models based on this trend to predict how diabetes in this age group will increase by 2060.
What are the terms to know?
- Type 1 diabetes is when the body does not produce enough insulin, the hormone that balances blood sugar levels. There is no known way to prevent type 1 diabetes at this time.
- Type 2 diabetes is when the body loses the ability over time to use insulin. In some people, type 2 diabetes can be prevented or delayed through lifestyle changes, such as healthy eating and being physically active.
- Incidence refers to the number of people diagnosed with a condition over a certain timeframe. Incidence in this study is measured in two ways: constant incidence , when the rate of new diabetes cases stays the same, and increasing incidence, when the rate of new cases continues to increase based on past growth trends.
What were the results?
- Constant incidence: If the rate of new cases stays the same, type 1 diabetes cases would remain about the same. Type 2 diabetes cases would increase about 70%. Total diabetes cases would increase about 12%.
- Increasing incidence: If the rate of new cases continues to trend upwards, type 1 diabetes cases would increase about 65%, and type 2 diabetes cases would increase about 700%. Total diabetes cases would increase by about 147%.
Diabetes Projections for Young People Aged less than 20 Years
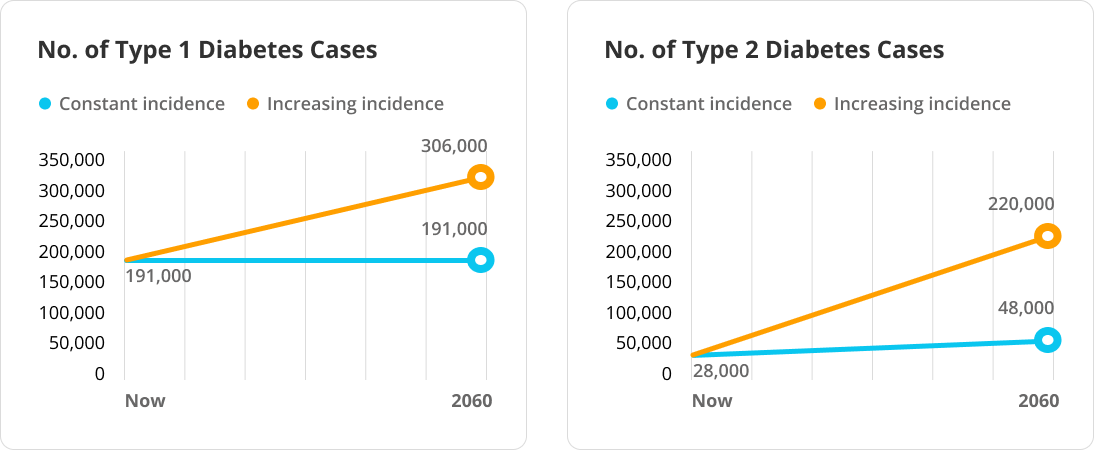
- Researchers also examined data by race and ethnicity and predicted higher increases in diabetes cases among young people who were Black, Hispanic or Latino, Asian or Pacific Islander, and American Indian or Alaska Native compared to young people who were White. This finding reinforces CDC’s actions to advance health equity .
- Researchers created a hypothetical model that decreased the annual incidence of diabetes by 2% through prevention efforts. This model reduced the increase of young people with diabetes to 294,000, compared to an increase up to 526,000 without prevention efforts.
What is the main message?
In both scenarios presented in this study, researchers expect diabetes in young people to increase over the next 40 years. This study highlights the importance of diabetes prevention efforts where possible for kids and teens.
- Projections of Type 1 and Type 2 Diabetes Burden in the U.S. Population Aged <20 Years Through 2060: The SEARCH for Diabetes in Youth Study
- Prevent type 2 diabetes
- Kids with type 1 diabetes
- Teens with type 1 diabetes
- Managing diabetes at school
- More Research Summaries
To receive updates about diabetes topics, enter your email address:
- Diabetes Home
- State, Local, and National Partner Diabetes Programs
- National Diabetes Prevention Program
- Native Diabetes Wellness Program
- Chronic Kidney Disease
- Vision Health Initiative
- Heart Disease and Stroke
- Overweight & Obesity
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Patient Care & Health Information
- Diseases & Conditions
- Type 2 diabetes
Type 2 diabetes is usually diagnosed using the glycated hemoglobin (A1C) test. This blood test indicates your average blood sugar level for the past two to three months. Results are interpreted as follows:
- Below 5.7% is normal.
- 5.7% to 6.4% is diagnosed as prediabetes.
- 6.5% or higher on two separate tests indicates diabetes.
If the A1C test isn't available, or if you have certain conditions that interfere with an A1C test, your health care provider may use the following tests to diagnose diabetes:
Random blood sugar test. Blood sugar values are expressed in milligrams of sugar per deciliter ( mg/dL ) or millimoles of sugar per liter ( mmol/L ) of blood. Regardless of when you last ate, a level of 200 mg/dL (11.1 mmol/L ) or higher suggests diabetes, especially if you also have symptoms of diabetes, such as frequent urination and extreme thirst.
Fasting blood sugar test. A blood sample is taken after you haven't eaten overnight. Results are interpreted as follows:
- Less than 100 mg/dL (5.6 mmol/L ) is considered healthy.
- 100 to 125 mg/dL (5.6 to 6.9 mmol/L ) is diagnosed as prediabetes.
- 126 mg/dL (7 mmol/L ) or higher on two separate tests is diagnosed as diabetes.
Oral glucose tolerance test. This test is less commonly used than the others, except during pregnancy. You'll need to not eat for a certain amount of time and then drink a sugary liquid at your health care provider's office. Blood sugar levels then are tested periodically for two hours. Results are interpreted as follows:
- Less than 140 mg/dL (7.8 mmol/L ) after two hours is considered healthy.
- 140 to 199 mg/dL (7.8 mmol/L and 11.0 mmol/L ) is diagnosed as prediabetes.
- 200 mg/dL (11.1 mmol/L ) or higher after two hours suggests diabetes.
Screening. The American Diabetes Association recommends routine screening with diagnostic tests for type 2 diabetes in all adults age 35 or older and in the following groups:
- People younger than 35 who are overweight or obese and have one or more risk factors associated with diabetes.
- Women who have had gestational diabetes.
- People who have been diagnosed with prediabetes.
- Children who are overweight or obese and who have a family history of type 2 diabetes or other risk factors.
After a diagnosis
If you're diagnosed with diabetes, your health care provider may do other tests to distinguish between type 1 and type 2 diabetes because the two conditions often require different treatments.
Your health care provider will test A1C levels at least two times a year and when there are any changes in treatment. Target A1C goals vary depending on age and other factors. For most people, the American Diabetes Association recommends an A1C level below 7%.
You also receive tests to screen for complications of diabetes and other medical conditions.
More Information
- Glucose tolerance test
Management of type 2 diabetes includes:
- Healthy eating.
- Regular exercise.
- Weight loss.
- Possibly, diabetes medication or insulin therapy.
- Blood sugar monitoring.
These steps make it more likely that blood sugar will stay in a healthy range. And they may help to delay or prevent complications.
Healthy eating
There's no specific diabetes diet. However, it's important to center your diet around:
- A regular schedule for meals and healthy snacks.
- Smaller portion sizes.
- More high-fiber foods, such as fruits, nonstarchy vegetables and whole grains.
- Fewer refined grains, starchy vegetables and sweets.
- Modest servings of low-fat dairy, low-fat meats and fish.
- Healthy cooking oils, such as olive oil or canola oil.
- Fewer calories.
Your health care provider may recommend seeing a registered dietitian, who can help you:
- Identify healthy food choices.
- Plan well-balanced, nutritional meals.
- Develop new habits and address barriers to changing habits.
- Monitor carbohydrate intake to keep your blood sugar levels more stable.
Physical activity
Exercise is important for losing weight or maintaining a healthy weight. It also helps with managing blood sugar. Talk to your health care provider before starting or changing your exercise program to ensure that activities are safe for you.
- Aerobic exercise. Choose an aerobic exercise that you enjoy, such as walking, swimming, biking or running. Adults should aim for 30 minutes or more of moderate aerobic exercise on most days of the week, or at least 150 minutes a week.
- Resistance exercise. Resistance exercise increases your strength, balance and ability to perform activities of daily living more easily. Resistance training includes weightlifting, yoga and calisthenics. Adults living with type 2 diabetes should aim for 2 to 3 sessions of resistance exercise each week.
- Limit inactivity. Breaking up long periods of inactivity, such as sitting at the computer, can help control blood sugar levels. Take a few minutes to stand, walk around or do some light activity every 30 minutes.
Weight loss
Weight loss results in better control of blood sugar levels, cholesterol, triglycerides and blood pressure. If you're overweight, you may begin to see improvements in these factors after losing as little as 5% of your body weight. However, the more weight you lose, the greater the benefit to your health. In some cases, losing up to 15% of body weight may be recommended.
Your health care provider or dietitian can help you set appropriate weight-loss goals and encourage lifestyle changes to help you achieve them.
Monitoring your blood sugar
Your health care provider will advise you on how often to check your blood sugar level to make sure you remain within your target range. You may, for example, need to check it once a day and before or after exercise. If you take insulin, you may need to check your blood sugar multiple times a day.
Monitoring is usually done with a small, at-home device called a blood glucose meter, which measures the amount of sugar in a drop of blood. Keep a record of your measurements to share with your health care team.
Continuous glucose monitoring is an electronic system that records glucose levels every few minutes from a sensor placed under the skin. Information can be transmitted to a mobile device such as a phone, and the system can send alerts when levels are too high or too low.
Diabetes medications
If you can't maintain your target blood sugar level with diet and exercise, your health care provider may prescribe diabetes medications that help lower glucose levels, or your provider may suggest insulin therapy. Medicines for type 2 diabetes include the following.
Metformin (Fortamet, Glumetza, others) is generally the first medicine prescribed for type 2 diabetes. It works mainly by lowering glucose production in the liver and improving the body's sensitivity to insulin so it uses insulin more effectively.
Some people experience B-12 deficiency and may need to take supplements. Other possible side effects, which may improve over time, include:
- Abdominal pain.
Sulfonylureas help the body secrete more insulin. Examples include glyburide (DiaBeta, Glynase), glipizide (Glucotrol XL) and glimepiride (Amaryl). Possible side effects include:
- Low blood sugar.
- Weight gain.
Glinides stimulate the pancreas to secrete more insulin. They're faster acting than sulfonylureas. But their effect in the body is shorter. Examples include repaglinide and nateglinide. Possible side effects include:
Thiazolidinediones make the body's tissues more sensitive to insulin. An example of this medicine is pioglitazone (Actos). Possible side effects include:
- Risk of congestive heart failure.
- Risk of bladder cancer (pioglitazone).
- Risk of bone fractures.
DPP-4 inhibitors help reduce blood sugar levels but tend to have a very modest effect. Examples include sitagliptin (Januvia), saxagliptin (Onglyza) and linagliptin (Tradjenta). Possible side effects include:
- Risk of pancreatitis.
- Joint pain.
GLP-1 receptor agonists are injectable medications that slow digestion and help lower blood sugar levels. Their use is often associated with weight loss, and some may reduce the risk of heart attack and stroke. Examples include exenatide (Byetta, Bydureon Bcise), liraglutide (Saxenda, Victoza) and semaglutide (Rybelsus, Ozempic, Wegovy). Possible side effects include:
SGLT2 inhibitors affect the blood-filtering functions in the kidneys by blocking the return of glucose to the bloodstream. As a result, glucose is removed in the urine. These medicines may reduce the risk of heart attack and stroke in people with a high risk of those conditions. Examples include canagliflozin (Invokana), dapagliflozin (Farxiga) and empagliflozin (Jardiance). Possible side effects include:
- Vaginal yeast infections.
- Urinary tract infections.
- Low blood pressure.
- High cholesterol.
- Risk of gangrene.
- Risk of bone fractures (canagliflozin).
- Risk of amputation (canagliflozin).
Other medicines your health care provider might prescribe in addition to diabetes medications include blood pressure and cholesterol-lowering medicines, as well as low-dose aspirin, to help prevent heart and blood vessel disease.
Insulin therapy
Some people who have type 2 diabetes need insulin therapy. In the past, insulin therapy was used as a last resort, but today it may be prescribed sooner if blood sugar targets aren't met with lifestyle changes and other medicines.
Different types of insulin vary on how quickly they begin to work and how long they have an effect. Long-acting insulin, for example, is designed to work overnight or throughout the day to keep blood sugar levels stable. Short-acting insulin generally is used at mealtime.
Your health care provider will determine what type of insulin is right for you and when you should take it. Your insulin type, dosage and schedule may change depending on how stable your blood sugar levels are. Most types of insulin are taken by injection.
Side effects of insulin include the risk of low blood sugar — a condition called hypoglycemia — diabetic ketoacidosis and high triglycerides.
Weight-loss surgery
Weight-loss surgery changes the shape and function of the digestive system. This surgery may help you lose weight and manage type 2 diabetes and other conditions related to obesity. There are several surgical procedures. All of them help people lose weight by limiting how much food they can eat. Some procedures also limit the amount of nutrients the body can absorb.
Weight-loss surgery is only one part of an overall treatment plan. Treatment also includes diet and nutritional supplement guidelines, exercise and mental health care.
Generally, weight-loss surgery may be an option for adults living with type 2 diabetes who have a body mass index (BMI) of 35 or higher. BMI is a formula that uses weight and height to estimate body fat. Depending on the severity of diabetes or the presence of other medical conditions, surgery may be an option for someone with a BMI lower than 35.
Weight-loss surgery requires a lifelong commitment to lifestyle changes. Long-term side effects may include nutritional deficiencies and osteoporosis.
People living with type 2 diabetes often need to change their treatment plan during pregnancy and follow a diet that controls carbohydrates. Many people need insulin therapy during pregnancy. They also may need to stop other treatments, such as blood pressure medicines.
There is an increased risk during pregnancy of developing a condition that affects the eyes called diabetic retinopathy. In some cases, this condition may get worse during pregnancy. If you are pregnant, visit an ophthalmologist during each trimester of your pregnancy and one year after you give birth. Or as often as your health care provider suggests.
Signs of trouble
Regularly monitoring your blood sugar levels is important to avoid severe complications. Also, be aware of symptoms that may suggest irregular blood sugar levels and the need for immediate care:
High blood sugar. This condition also is called hyperglycemia. Eating certain foods or too much food, being sick, or not taking medications at the right time can cause high blood sugar. Symptoms include:
- Frequent urination.
- Increased thirst.
- Blurred vision.
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS). This life-threatening condition includes a blood sugar reading higher than 600 mg/dL (33.3 mmol/L ). HHNS may be more likely if you have an infection, are not taking medicines as prescribed, or take certain steroids or drugs that cause frequent urination. Symptoms include:
- Extreme thirst.
- Drowsiness.
- Dark urine.
Diabetic ketoacidosis. Diabetic ketoacidosis occurs when a lack of insulin results in the body breaking down fat for fuel rather than sugar. This results in a buildup of acids called ketones in the bloodstream. Triggers of diabetic ketoacidosis include certain illnesses, pregnancy, trauma and medicines — including the diabetes medicines called SGLT2 inhibitors.
The toxicity of the acids made by diabetic ketoacidosis can be life-threatening. In addition to the symptoms of hyperglycemia, such as frequent urination and increased thirst, ketoacidosis may cause:
- Shortness of breath.
- Fruity-smelling breath.
Low blood sugar. If your blood sugar level drops below your target range, it's known as low blood sugar. This condition also is called hypoglycemia. Your blood sugar level can drop for many reasons, including skipping a meal, unintentionally taking more medication than usual or being more physically active than usual. Symptoms include:
- Irritability.
- Heart palpitations.
- Slurred speech.
If you have symptoms of low blood sugar, drink or eat something that will quickly raise your blood sugar level. Examples include fruit juice, glucose tablets, hard candy or another source of sugar. Retest your blood in 15 minutes. If levels are not at your target, eat or drink another source of sugar. Eat a meal after your blood sugar level returns to normal.
If you lose consciousness, you need to be given an emergency injection of glucagon, a hormone that stimulates the release of sugar into the blood.
- Medications for type 2 diabetes
- GLP-1 agonists: Diabetes drugs and weight loss
- Bariatric surgery
- Endoscopic sleeve gastroplasty
- Gastric bypass (Roux-en-Y)
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Careful management of type 2 diabetes can reduce the risk of serious — even life-threatening — complications. Consider these tips:
- Commit to managing your diabetes. Learn all you can about type 2 diabetes. Make healthy eating and physical activity part of your daily routine.
- Work with your team. Establish a relationship with a certified diabetes education specialist, and ask your diabetes treatment team for help when you need it.
- Identify yourself. Wear a necklace or bracelet that says you are living with diabetes, especially if you take insulin or other blood sugar-lowering medicine.
- Schedule a yearly physical exam and regular eye exams. Your diabetes checkups aren't meant to replace regular physicals or routine eye exams.
- Keep your vaccinations up to date. High blood sugar can weaken your immune system. Get a flu shot every year. Your health care provider also may recommend the pneumonia vaccine. The Centers for Disease Control and Prevention (CDC) also recommends the hepatitis B vaccination if you haven't previously received this vaccine and you're 19 to 59 years old. Talk to your health care provider about other vaccinations you may need.
- Take care of your teeth. Diabetes may leave you prone to more-serious gum infections. Brush and floss your teeth regularly and schedule recommended dental exams. Contact your dentist right away if your gums bleed or look red or swollen.
- Pay attention to your feet. Wash your feet daily in lukewarm water, dry them gently, especially between the toes, and moisturize them with lotion. Check your feet every day for blisters, cuts, sores, redness and swelling. Contact your health care provider if you have a sore or other foot problem that isn't healing.
- Keep your blood pressure and cholesterol under control. Eating healthy foods and exercising regularly can go a long way toward controlling high blood pressure and cholesterol. Take medication as prescribed.
- If you smoke or use other types of tobacco, ask your health care provider to help you quit. Smoking increases your risk of diabetes complications. Talk to your health care provider about ways to stop using tobacco.
- Use alcohol sparingly. Depending on the type of drink, alcohol may lower or raise blood sugar levels. If you choose to drink alcohol, only do so with a meal. The recommendation is no more than one drink daily for women and no more than two drinks daily for men. Check your blood sugar frequently after drinking alcohol.
- Make healthy sleep a priority. Many people with type 2 diabetes have sleep problems. And not getting enough sleep may make it harder to keep blood sugar levels in a healthy range. If you have trouble sleeping, talk to your health care provider about treatment options.
- Caffeine: Does it affect blood sugar?
Alternative medicine
Many alternative medicine treatments claim to help people living with diabetes. According to the National Center for Complementary and Integrative Health, studies haven't provided enough evidence to recommend any alternative therapies for blood sugar management. Research has shown the following results about popular supplements for type 2 diabetes:
- Chromium supplements have been shown to have few or no benefits. Large doses can result in kidney damage, muscle problems and skin reactions.
- Magnesium supplements have shown benefits for blood sugar control in some but not all studies. Side effects include diarrhea and cramping. Very large doses — more than 5,000 mg a day — can be fatal.
- Cinnamon, in some studies, has lowered fasting glucose levels but not A1C levels. Therefore, there's no evidence of overall improved glucose management.
Talk to your health care provider before starting a dietary supplement or natural remedy. Do not replace your prescribed diabetes medicines with alternative medicines.
Coping and support
Type 2 diabetes is a serious disease, and following your diabetes treatment plan takes commitment. To effectively manage diabetes, you may need a good support network.
Anxiety and depression are common in people living with diabetes. Talking to a counselor or therapist may help you cope with the lifestyle changes and stress that come with a type 2 diabetes diagnosis.
Support groups can be good sources of diabetes education, emotional support and helpful information, such as how to find local resources or where to find carbohydrate counts for a favorite restaurant. If you're interested, your health care provider may be able to recommend a group in your area.
You can visit the American Diabetes Association website to check out local activities and support groups for people living with type 2 diabetes. The American Diabetes Association also offers online information and online forums where you can chat with others who are living with diabetes. You also can call the organization at 800-DIABETES ( 800-342-2383 ).
Preparing for your appointment
At your annual wellness visit, your health care provider can screen for diabetes and monitor and treat conditions that increase your risk of diabetes, such as high blood pressure, high cholesterol or a high BMI .
If you are seeing your health care provider because of symptoms that may be related to diabetes, you can prepare for your appointment by being ready to answer the following questions:
- When did your symptoms begin?
- Does anything improve the symptoms or worsen the symptoms?
- What medicines do you take regularly, including dietary supplements and herbal remedies?
- What are your typical daily meals? Do you eat between meals or before bedtime?
- How much alcohol do you drink?
- How much daily exercise do you get?
- Is there a history of diabetes in your family?
If you are diagnosed with diabetes, your health care provider may begin a treatment plan. Or you may be referred to a doctor who specializes in hormonal disorders, called an endocrinologist. Your care team also may include the following specialists:
- Certified diabetes education specialist.
- Foot doctor, also called a podiatrist.
- Doctor who specializes in eye care, called an ophthalmologist.
Talk to your health care provider about referrals to other specialists who may be providing care.
Questions for ongoing appointments
Before any appointment with a member of your treatment team, make sure you know whether there are any restrictions, such as not eating or drinking before taking a test. Questions that you should regularly talk about with your health care provider or other members of the team include:
- How often do I need to monitor my blood sugar, and what is my target range?
- What changes in my diet would help me better manage my blood sugar?
- What is the right dosage for prescribed medications?
- When do I take the medications? Do I take them with food?
- How does management of diabetes affect treatment for other conditions? How can I better coordinate treatments or care?
- When do I need to make a follow-up appointment?
- Under what conditions should I call you or seek emergency care?
- Are there brochures or online sources you recommend?
- Are there resources available if I'm having trouble paying for diabetes supplies?
What to expect from your doctor
Your health care provider is likely to ask you questions at your appointments. Those questions may include:
- Do you understand your treatment plan and feel confident you can follow it?
- How are you coping with diabetes?
- Have you had any low blood sugar?
- Do you know what to do if your blood sugar is too low or too high?
- What's a typical day's diet like?
- Are you exercising? If so, what type of exercise? How often?
- Do you sit for long periods of time?
- What challenges are you experiencing in managing your diabetes?
- Professional Practice Committee: Standards of Medical Care in Diabetes — 2020. Diabetes Care. 2020; doi:10.2337/dc20-Sppc.
- Diabetes mellitus. Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/diabetes-mellitus-dm. Accessed Dec. 7, 2020.
- Melmed S, et al. Williams Textbook of Endocrinology. 14th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Dec. 3, 2020.
- Diabetes overview. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/all-content. Accessed Dec. 4, 2020.
- AskMayoExpert. Type 2 diabetes. Mayo Clinic; 2018.
- Feldman M, et al., eds. Surgical and endoscopic treatment of obesity. In: Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 11th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed Oct. 20, 2020.
- Hypersmolar hyperglycemic state (HHS). Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/hyperosmolar-hyperglycemic-state-hhs. Accessed Dec. 11, 2020.
- Diabetic ketoacidosis (DKA). Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/diabetic-ketoacidosis-dka. Accessed Dec. 11, 2020.
- Hypoglycemia. Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/hypoglycemia. Accessed Dec. 11, 2020.
- 6 things to know about diabetes and dietary supplements. National Center for Complementary and Integrative Health. https://www.nccih.nih.gov/health/tips/things-to-know-about-type-diabetes-and-dietary-supplements. Accessed Dec. 11, 2020.
- Type 2 diabetes and dietary supplements: What the science says. National Center for Complementary and Integrative Health. https://www.nccih.nih.gov/health/providers/digest/type-2-diabetes-and-dietary-supplements-science. Accessed Dec. 11, 2020.
- Preventing diabetes problems. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/all-content. Accessed Dec. 3, 2020.
- Schillie S, et al. Prevention of hepatitis B virus infection in the United States: Recommendations of the Advisory Committee on Immunization Practices. MMWR Recommendations and Reports. 2018; doi:10.15585/mmwr.rr6701a1.
- Diabetes prevention: 5 tips for taking control
- Hyperinsulinemia: Is it diabetes?
Associated Procedures
News from mayo clinic.
- Mayo study uses electronic health record data to assess metformin failure risk, optimize care Feb. 10, 2023, 02:30 p.m. CDT
- Mayo Clinic Minute: Strategies to break the heart disease and diabetes link Nov. 28, 2022, 05:15 p.m. CDT
- Mayo Clinic Q and A: Diabetes risk in Hispanic people Oct. 20, 2022, 12:15 p.m. CDT
- The importance of diagnosing, treating diabetes in the Hispanic population in the US Sept. 28, 2022, 04:00 p.m. CDT
- Mayo Clinic Minute: Managing Type 2 diabetes Sept. 28, 2022, 02:30 p.m. CDT
Products & Services
- A Book: The Essential Diabetes Book
- A Book: The Mayo Clinic Diabetes Diet
- Assortment of Health Products from Mayo Clinic Store
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
WATCH TV LIVE
Common Diabetes Drug May Slow Aging
By Lynn C. Allison | Tuesday, 23 April 2024 05:00 PM EDT
Research suggests that a medication commonly used to control Type 2 diabetes may help protect against age-related chronic diseases and promote longevity. A series of nationwide test trials will be launched to evaluate whether men and women taking metformin, a popular, low-cost diabetes drug, experience a delay in development or progression of age-related diseases such as cancer, dementia, and heart disease.
The Targeting Aging with Metformin (TAME) Trial will be conducted at 14 leading research institutions across the U.S. and will involve more than 3,000 participants between the ages of 65 and 79, according to the American Federation for Aging Research .
Special: Is Your Liver Health the REAL Fountain of Youth? More …
Metformin is an FDA-approved drug that has been used in the treatment of diabetes for more than 60 years. Animal studies have already shown that the drug delays aging, and the scientists hope to find that it also influences fundamental aging factors in humans. The TAME Trial is targeting metformin for its research because the drug has already been proven to be safe and inexpensive. Researchers are hoping that the Food and Drug Administration (FDA) will consider aging as a treatable indication, like diabetes and heart disease. They are proposing a broad category of aging that would include chronic conditions associated with aging that could be treated with metformin if the trial is successful.
According to NPR , metformin costs less than a dollar a day and may incur no out-of-pocket expenses for those with insurance. Steven N. Austad Ph.D., senior scientific director of the American Federation for Aging Research, says, “I don’t know if metformin increases lifespan in people, but the evidence that exists suggests it very well might.”
Studies have shown that the drug reduces the risk of certain types of cancer, including gastrointestinal, urologic and blood cancers. Austad said that a British study found a lower risk of dementia and cognitive decline among people who took metformin for Type 2 diabetes. There is also evidence that the drug improves cardiovascular outcomes, including a reduced risk of cardiovascular death, says NPR.
Special: Your Liver Holds the Key to Unlocking Age-Defying Health, Energy, and Longevity! More Here …
The TAME Trial that is being coordinated by researchers at Wake Forest University School of Medicine hopes to find answers as to why these benefits occur and if they are restricted to people with diabetes. The goal is to uncover how the mechanisms work in the body and if metformin can help reduce inflammation and oxidative stress, which slows biological aging.
For now, the FDA has approved metformin only to treat Type 2 diabetes, but doctors can prescribe it off-label for other conditions, says Harvard Health . Some examples include prediabetes, gestational diabetes, and polycystic ovary syndrome (PCOS). It can also be used to lessen weight gain in people who take antipsychotic medication.
The study is estimated to cost between $45 and $70 million, and researchers are having a difficult time raising funds. Because metformin is a generic drug, no pharmaceutical company stands to make any money if the results prove successful. The metformin trial will get underway once the money comes in, says Dr. Nir Barzilai, director of the Institute of Aging Research at Albert Einstein College of Medicine, who is leading the effort to get the trial started.
© 2024 NewsmaxHealth. All rights reserved.
Sign up for Newsmax’s Daily Newsletter
Receive breaking news and original analysis - sent right to your inbox.

- Health News
- Brain Health
- Natural Health
- Diet & Fitness
The information presented on this website is not intended as specific medical advice and is not a substitute for professional medical treatment or diagnosis. Read Newsmax Terms and Conditions of Service .
Newsmax, Moneynews, Newsmax Health, and Independent. American. are registered trademarks of Newsmax Media, Inc. Newsmax TV, and Newsmax World are trademarks of Newsmax Media, Inc.
- OU Homepage
- The University of Oklahoma
Researchers Earn $2.3 Million Grant to Study Generational Cycle of Maternal Obesity, Liver Disease

Project includes testing an antioxidant for improving metabolic health
OKLAHOMA CITY, OKLA. – Research increasingly suggests that when a woman with obesity becomes pregnant, a process of “fetal reprogramming” increases the risk that her baby will face problems like obesity, Type 2 diabetes and liver disease earlier in life.
To better understand how that reprogramming occurs, University of Oklahoma researchers recently earned a $2.3 million grant from the National Institutes of Health. They also will study whether an antioxidant called PQQ given to the mother can lower the risk of future metabolic problems for her offspring.
“Today in the United States, more than 40% of women of childbearing age are overweight or obese,” said OU College of Medicine researcher Karen Jonscher, Ph.D., who is leading the work of the grant with Dean Myers, Ph.D. “Research has shown that people whose mothers were obese during pregnancy have a higher risk for developing metabolic dysfunction-associated steatotic liver disease, a fatty liver disease that becomes progressively worse and can result in the need for a transplant. However, in offspring, it happens earlier in life and with more severe problems. The whole process seems to be accelerated in children who are born to mothers with obesity.”
Much of America’s obesity problem is attributed to eating a “Western-style” diet that is heavy on fats. However, even if a woman with obesity eats healthier during pregnancy, her offspring still face a higher risk of disease. Jonscher and Myers believe the key may be what is happening in the placenta — the interface between mother and fetus.
Obesity is essentially a low-grade, chronic inflammatory disease. Fat cells cause inflammation, which means the body’s white blood cells are in a constant state of activation and can damage other cells and tissues. Cholesterol and triglyceride levels rise, and blood pressure increases. Jonscher hypothesizes that the inflammation in pregnant women with obesity prompts the placenta to send a signal to the fetus’s stem cells, telling them to reprogram themselves to become more susceptible to the inflammation’s harmful effects.
“There is even some evidence that inflammation changes how nutrients are transported to the fetus so that fat is preferentially transported rather than the building blocks of proteins,” said Jonscher, an associate professor of biochemistry and physiology.
With the grant, Jonscher and Myers will try to prove that hypothesis. In addition, they will test an antioxidant called pyrroloquinoline quinone, or PQQ, for its ability to block or reverse fetal reprogramming. PQQ, found in fruits and vegetables, has anti-inflammatory properties, but if a person doesn’t eat a healthy diet, they are less likely to have adequate levels of PQQ.
In their preliminary studies in a preclinical research model, the researchers found that when PQQ is given to obese mothers, their offspring are protected from fatty liver disease in adulthood. Because women are generally advised not to take weight loss drugs during pregnancy due to potential harm to the fetus, the researchers hope PQQ is both safe and effective.
“Based on the data we have gathered so far, we believe that PQQ will create a healthier pregnancy,” Myers said. “The mother may still have a high body mass index, but PQQ appears able to lower inflammation and improve cholesterol and lipid levels. If we can improve the mother's health, we are also improving the function of the placenta, which will protect the fetus in a positive way. And if we can protect the placenta, nutrient transport will be improved with more amino acids and protein building blocks reaching the fetus instead of fats, as well as better oxygen flow.”
Myers, who is a professor in the Department of Obstetrics and Gynecology, often talks with his clinical colleagues who are caring for women with obesity during their pregnancies. Exercising and eating a healthy diet can be difficult for all people, pregnant or not, and physicians need another tool to help women become more metabolically healthy while pregnant.
“Our goal is to create a less-inflamed, healthier placenta,” he said. “Hopefully, PQQ will help the mother, too, because women with obesity who are pregnant have an increased risk for gestational diabetes. If our research with this grant is successful, we hope to move PQQ into clinical trials in a few years.”
About the University of Oklahoma
Founded in 1890, the University of Oklahoma is a public research university located in Norman, Oklahoma. As the state’s flagship university, OU serves the educational, cultural, economic and health care needs of the state, region and nation. OU was named the state’s highest-ranking university in U.S. News & World Report’s most recent Best Colleges list . For more information about the university, visit ou.edu .
Recent News
Understanding disaster response: nsf career award supports ou engineer’s research on information sharing.
Arif Sadri, Ph.D., an assistant professor in the Gallogly College of Engineering at the University of Oklahoma, has received a CAREER award from the National Science Foundation to study how communities communicate during disasters like storms, floods, tornadoes and earthquakes. His project, funded by multiple NSF programs, seeks to improve disaster preparedness, response and recovery efforts.

University of Oklahoma Receives $4M Grant for Supply Chain Resiliency Research
The University of Oklahoma has received a nearly $4 million congressional appropriation for supply chain risk management research from the 448th Supply Chain Management Wing of the U.S. Air Force Sustainment Center.

OU Student Named Pulitzer Reporting Fellow
Maddy Keyes, a senior from the Gaylord College of Journalism and Mass Communication, has been chosen as a Pulitzer Center Reporting Fellow to explore the ecological grief caused by climate change for the Inuit in Greenland.

More OU News

- Accessibility
- Sustainability
- OU Job Search
- Legal Notices
- Resources and Offices
- OU Report It!

IMAGES
VIDEO
COMMENTS
New cause of diabetes discovered, offering potential target for new classes of drugs to treat the disease. ScienceDaily . Retrieved April 26, 2024 from www.sciencedaily.com / releases / 2023 / 12 ...
The new research, published in the journal Nature Communications, offers a potential strategy for developing new therapies that could restore dysfunctional pancreatic beta-cells or, perhaps, even prevent Type 2 diabetes from developing. The new study shows that the beta-cells of Type 2 diabetes patients are deficient in a cell trafficking ...
This finding encourages further investigation into inceptor as a potential therapeutic target for treating type 2 diabetes. These findings, led by Helmholtz Munich in collaboration with the German Center for Diabetes Research, the Technical University of Munich, and the Ludwig-Maximilians-University Munich, drive advancements in diabetes research.
Type 2 diabetes mellitus, the most frequent subtype of diabetes, is a disease characterized by high levels of blood glucose (hyperglycaemia). It arises from a resistance to and relative deficiency ...
Large-scale study reveals new genetic details of diabetes. In experiments of unprecedented scale, investigators at Weill Cornell Medicine and the National Institutes of Health have revealed new aspects of the complex genetics behind Type 2 diabetes. Through these discoveries, and by providing a template for future studies, this research ...
Amelioration of Both Central and Peripheral Neuropathy in Mouse Models of Type 1 and Type 2 Diabetes by the Neurogenic Molecule NSI-189. Diabetes, 68(11), 2143-2154. Read more. ADA-funded researcher studying link between ageing and type 2 diabetes. One of the most important risk factors for developing type 2 diabetes is age.
Surgery led to diabetes remission in roughly 28% of patients, compared with a remission rate of just 4% among the non-surgery group, according to the study results. More research has found that ...
Both are now adults, and both have Type 1 diabetes. My son was 6 months old when he was diagnosed. And that's when I changed my research plan. And my daughter, who's four years older than my son, became diabetic about 10 years later, when she was 14. When my son was diagnosed, I knew nothing about diabetes and had been working on how frogs ...
The largest genome-wide association study for type 2 diabetes so far, which included several ancestry groups, led to the identification of eight clusters of genetic risk variants.
I. Introduction. Diabetes mellitus, a metabolic disease defined by elevated fasting blood glucose levels due to insufficient insulin production, has reached epidemic proportions worldwide (World Health Organization, 2020).Type 1 and type 2 diabetes (T1D and T2D, respectively) make up the majority of diabetes cases with T1D characterized by autoimmune destruction of the insulin-producing ...
By Andrew Stewart, MD, as told to Hallie Levine. Type 2 diabetes is one of the world's greatest health problems. It affects about 400 million people globally. If it's uncontrolled, it can lead ...
People with obesity and type 2 diabetes lost more weight using daily periods of fasting than by trying to restrict calories over a six-month period. ... In a new clinical trial, an NIH-funded research team led by Dr. Krista Varady from the University of Illinois Chicago compared fasting and calorie restriction for weight loss and blood-sugar ...
There are many known risk factors for type 2 diabetes, including family members having it, being of African or Asian ancestry, high blood pressure, obesitym and polycystic ovary syndrome (PCOS ...
A new study found that tiny biodegradable particles improved insulin sensitivity in the liver cells of humans and in diabetic mice, which could offer a promising new treatment for type 2 diabetes.
Together, the findings suggest that type II diabetes may be driven by an overabundance of NO attaching to proteins like insulin. Any enzymes, like SCAN, that work to attach NO to its receptors could, therefore, be useful targets in future research. Stamler hopes that by blocking the SCAN enzyme, scientists may find new treatments for at least ...
Even if the rate of new diabetes diagnoses among young people remains the same over the decades, type 2 diabetes diagnoses could increase nearly 70% and type 1 diabetes diagnoses could increase 3% by 2060. Type 1 diabetes remains more common in U.S. youth, but type 2 diabetes has substantially increased among young people over the last two decades.
The chronic complications of type 2 diabetes are a major cause of mortality and disability worldwide [ 1, 2 ]. Clinical research is the main way to gain knowledge about long-term diabetic complications and reduce the burden of diabetes. This allows for designing effective programs for screening and follow-up and fine-targeted therapeutic ...
The ADA is committed to continuing progress in the fight against type 2 diabetes by funding research, including support for potential new treatments, a better understating of genetic factors, addressing disparities, and more. For specific examples of projects currently funded by the ADA, see below. Greg J. Morton, PhD.
The FDA approved metformin for the treatment of type 2 diabetes in the U.S. in the 1990s. Since then, researchers have documented several surprises, including a reduced risk of cancer. "That was a ...
Promising research directions for obesity and type 2 diabetes. Study Designs. • Novel designs/methods for evaluating multi-level interventions including mixed methods research. • Study designs other than the traditional RCTs to allow for flexible recruitment approaches and account for dynamic, pragmatic issues.
Type 2 diabetes affects more than 38.4 million Americans, with an estimated 1.4 million new cases diagnosed every year, according to the Centers for Disease Control and Prevention.
depression and type 2 diabetes ... of more than £100m, new research from the University of Exeter has found. According to the World Health Organization (WHO) the most common
Researchers forecasted the number of kids and teens who will be diagnosed with diabetes from 2017 to 2060 based on two scenarios: Constant incidence: If the rate of new cases stays the same, type 1 diabetes cases would remain about the same. Type 2 diabetes cases would increase about 70%. Total diabetes cases would increase about 12%.
Coffee appears to lower pro-inflammatory biomarkers while increasing anti-inflammatory ones. Consuming coffee is linked to a lower risk of type 2 diabetes. The relationship is well-established ...
Develop new habits and address barriers to changing habits. ... Research has shown the following results about popular supplements for type 2 diabetes: Chromium supplements have been shown to have few or no benefits. Large doses can result in kidney damage, muscle problems and skin reactions. ... Type 2 diabetes is a serious disease, and ...
According to a new study published April 19, 2023 in the journal The BMJ, among people diagnosed with type 2 diabetes, those who drink the most sugar-sweetened beverages may be at a 20% higher ...
Research suggests that a medication commonly used to control Type 2 diabetes may help protect against age-related chronic diseases and promote longevity. A series of nationwide test trials will be launched to evaluate whether men and women taking metformin, a popular, low-cost diabetes drug, experience a delay in development or progression of ...
Research increasingly suggests that when a woman with obesity becomes pregnant, a process of "fetal reprogramming" increases the risk that her baby will face problems like obesity, Type 2 diabetes and liver disease earlier in life. To better understand how that reprogramming occurs, University of Oklahoma researchers recently earned a $2.3 million grant from the National Institutes of Health.