Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article

Global distribution and coincidence of pollution, climate impacts, and health risk in the Anthropocene
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliations The Joan B. Kroc Institute for International Peace Studies, University of Notre Dame, Notre Dame, Indiana, United States of America, Department of Anthropology, University of Notre Dame, Notre Dame, Indiana, United States of America
Roles Methodology, Writing – original draft, Writing – review & editing
Affiliation Department of Political Science, University of Notre Dame, Notre Dame, Indiana, United States of America
Roles Data curation, Formal analysis, Methodology, Visualization
Affiliation Department of Anthropology, University of Notre Dame, Notre Dame, Indiana, United States of America
Roles Conceptualization, Writing – original draft, Writing – review & editing
Affiliation Department of Anthropology, Princeton University, Princeton, New Jersey, United States of America
- Richard Marcantonio,
- Debra Javeline,
- Sean Field,
- Agustin Fuentes

- Published: July 21, 2021
- https://doi.org/10.1371/journal.pone.0254060
- Reader Comments
Previous research demonstrates that low-income countries face higher risks than high-income countries from toxic pollution and climate change. However, the relationship between these two risks is little explored or tested, and efforts to address the risks are often independent and uncoordinated. We argue that the global risks from toxic pollution and climate change are highly correlated and should be jointly analyzed in order to inform and better target efforts to reduce or mitigate both risks. We provide such analysis for 176 countries and found a strong (r s = -0.798;95%CI -0.852, -0.727) and significant (p<0.0001) relationship between the distribution of climate risk and toxic pollution. We also found that inequities in pollution production, economic status, and institutional readiness are interconnected and exacerbate risk for countries already in the highest risk categories for both toxic and non-toxic (greenhouse gas) pollution. The findings have policy implications, including the use of the proposed Target assessment to decide where best to address toxic and non-toxic pollution simultaneously, based on the need to minimize human suffering and maximize return on effort.
Citation: Marcantonio R, Javeline D, Field S, Fuentes A (2021) Global distribution and coincidence of pollution, climate impacts, and health risk in the Anthropocene. PLoS ONE 16(7): e0254060. https://doi.org/10.1371/journal.pone.0254060
Editor: Shah Md Atiqul Haq, Shahjalal University of Science and Technology, BANGLADESH
Received: April 1, 2021; Accepted: June 18, 2021; Published: July 21, 2021
Copyright: © 2021 Marcantonio et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Human-produced pollution is destabilizing the entire Earth System [ 1 – 3 ]. This pollution poses severe risk to human health and the contemporary human niche [ 4 – 11 ]. Most research assesses the independent risks of toxic emissions (e.g. fine particulate matter or PM2.5) and non-toxic emissions (e.g. greenhouse gases) and people’s vulnerability to them [ 9 , 12 , 13 ]. However, these risks are intricately connected and substantially catalyze each other both in the environment and the human body [ 9 – 11 , 14 – 20 ]. For example, flood events disturb and redistribute toxic materials [ 16 , 21 , 22 ]. Research is lacking on the simultaneous and interactive risk from toxic and non-toxic emissions to human health [ 23 ]. There is a need for “bold and comprehensive strategies that simultaneously address both problems…to overcome the separation between pollution prevention and climate change mitigation” [ 23 ]. Numerous collaborative efforts are underway to rectify this shortfall—e.g., the new Center for Climate Change and the Center for Climate, Health and the Global Environment (C-CHANGE) at the Harvard TH Chan School of Public Health, the latter led until recently by Gina McCarthy, former Administrator of the US Environmental Protection Agency (2013–2017) and now the first White House National Climate Advisor [ 24 ]. However, no studies to date have tested the relationship between toxic pollution risk and climate risk to human health in order to inform these new efforts [ 7 – 11 , 17 , 23 ].
Such a gap in information and analyses restricts broadscale, and local, efforts to characterize specific patterns and processes of interaction accurately and holistically between toxic and non-toxic (climate impact) pollution. The relationships between the two processes, as compared to models that keep the two processes and corresponding risks separate, may be a better representation of the actual overall dynamic of challenges faced. Improved understanding of these interfaces offers institutions, agencies, and practitioners a greater toolkit with which to attempt amelioration of the harms resulting from pollution.
How does the human health risk due to toxic and non-toxic pollution vary by country? How strong is the relationship between the risk from each pollution type, and where specifically is the risk, and the potential to address the risk, greatest? To answer these questions, we join data measuring global climate risk and institutional capacity from the Notre Dame Global Adaptation Index (ND-GAIN) Country Index [ 12 ], environmental quality from the Yale Environmental Performance Index (EPI) [ 13 ], and toxic pollution-caused mortality from the Global Alliance on Health and Pollution (GAHP) [ 9 ], all for the year 2018, to explore the global distribution of human-produced or exacerbated environmental risks in multiple countries (N = 176). We hypothesize that there is a strong relationship between the global distribution of toxic pollution risk and climate impacts risk. Low- and middle-income countries are often unable to afford or enforce strict regulatory regimes against polluting industries or the infrastructure and other costs associated with reducing vulnerability to climate change and hazardous waste. Using a novel, holistic measure of the environmental risk people face globally, we test the spatial relationship between both types of pollution risks at the country level. We present the results of a prioritization assessment wherein the Target score reflects the relationships of Vulnerability , Eco-health , and Readiness for each country (see Methods for variable descriptions). This tool should allow policymakers and other stakeholders to place toxic pollution risk and climate impacts risk in dialogue with core structural aspects of a given country and not only identify where this risk is greatest, but also estimate where targeted actions in reducing this risk, and thus potential human suffering, might produce the highest return and probability of success when accounting for the institutional capacity of each country.
Human-produced pollution causes an array of cascading ecological and social effects [ 3 , 4 , 25 , 26 ]. These risks are pushing the Earth System into a planetary state distinct in human evolutionary history, posing substantial new risks and challenges [ 3 , 27 – 29 ]. Primary components of these changes and corresponding risks are toxic pollution—materials that are directly harmful to human health via emission into the air, water, or land—and non-toxic pollution—materials not directly toxic to humans but indirectly deleterious to human health via their emission as greenhouse gases (GHG) that change the climate and the functioning of the Earth System. Toxic pollution results in the death of more than 8 million people annually [ 7 , 9 , 30 , 31 ] and other harms to humans from cognitive dysfunction [ 32 – 39 ] to chronic respiratory illnesses [ 40 – 45 ]. Non-toxic pollution is driving global environmental changes that endanger human health through global warming [ 11 , 46 – 48 ], land degradation [ 28 , 49 , 50 ], extreme weather events [ 51 , 52 ], and sea-level rise [ 53 , 54 ]. The number of annual global deaths resulting from these changes is yet undetermined, but between 2030–2050 an additional 250,000 people are estimated to perish annually [ 55 ], and likely the actual figures are much higher [ 56 ]. By 2050 an estimated 530,000 additional deaths will occur annually solely due to food production losses caused by climate change [ 57 ]. The biogeophysical effects of human-produced pollution are not equally distributed, with low-income countries undergoing the highest risks and resultant negative human health impacts from toxic pollution and climate change [ 7 – 9 , 46 ]. Importantly, toxic pollution emissions primarily, though not solely, affect the areas more proximal to where they are released, whereas GHGs drive a global process of climatic change that can result in risk far from where they are emitted [ 10 , 11 ]. This difference is critical because lower-income countries are relatively more exposed to climate risk but middle- and high-income countries are responsible for a larger share of historical and contemporary GHG emissions [ 46 , 58 – 64 ].
The social outcomes and costs associated with these risk factors are as far reaching as the biogeophysical outcomes. The estimated current economic output lost due to the human health effects of toxic pollution is $4.6 trillion annually, or 6.2% of global GDP [ 9 ]. The estimated current economic productivity losses from global warming, in just the US and the EU, is $4 trillion. By 2100 world GDP per capita is expected to be reduced by 7.2% due to climate change [ 65 ]. By 2040 global climate change will add at least 20%—or $100 billion a year—to the annual global cost of extreme weather events [ 66 ]; in 2017 extreme weather exacerbated by climate change wrought $300 billion in just infrastructural and material damage alone [ 67 ]. The economic effects of climate change are not distributed equally across countries, with tropical countries at least 5% poorer than they would be in the absence of climate change [ 68 ] and increasing global income inequality within and between countries and classes, respectively, by approximately 25% [ 69 ]. Other indirect social effects from climate change range from the potential for increased rates of violent conflict and warfare [ 70 – 76 ] to increased incidence of mental health issues [ 77 – 80 ].
Low-income countries face relatively higher risks from toxic pollution and climate change than high-income countries [ 16 , 46 ]. However, the relationship between the global distribution of these two risks has not been explored and tested [ 9 , 23 ], resulting in a critical gap in current understandings of human health risk due to human-produced pollution. Further, where and how targeted efforts should be made to reduce or mitigate these risks with the highest rate and probability of return on efforts—i.e., reductions in the loss or risk of loss of human life—also remains unclear.
Materials and methods
The processes and effects of human-produced toxic and non-toxic pollution are differentiable but interrelated. We collate and analyze three broadly utilized datasets (ND-GAIN, EPI, and GAHP) to measure the global distribution of risk from toxic pollution and climate change, to test the spatial relationship between these risks, and to identify how best to target their mitigation. All data utilized can be found in S1 Data and are publicly available from the institutions that curate them. All three datasets are for the year 2018, the most recent available data from all three sources that includes all of the same countries, at the time this article was written.
Notre Dame–Global Adaptation Index (ND-GAIN).
The ND-GAIN Country Index summarizes a country’s vulnerability and exposure to climate impacts risks and its readiness to improve climate resilience [ 12 ]. The full ND-GAIN index is comprised of 45 indicators of climate impacts risk ( Vulnerability ; 36 indicators) and Readiness (9 indicators) for 182 countries. ND-GAIN assesses the Vulnerability of a country by considering six life-supporting sectors: food, water, health, ecosystem services, human habitat and infrastructure. The exposure of each sector to climate-related or climate-exacerbated hazards, the sensitivity of that sector to the impacts of the hazard and the adaptive capacity of the sector to cope or adapt to these impacts, are in turn measured by six indicators each. ND-GAIN assesses Readiness by considering a country’s ability to implement adaptation actions if effectively incentivized. ND-GAIN measures overall Readiness by considering three components: economic readiness, governance readiness, and social readiness. ND-GAIN does not include measures for toxic pollution, nor does it measure GHG emissions rates; it measures only a country’s climate risk—their exposure and vulnerability to climate-driven hazards—and their readiness to deal with that risk.
Environmental Performance Index (EPI).
The EPI ranks 180 countries on 24 performance indicators across ten issue categories covering environmental health ( Eco-health ) and ecosystem vitality [ 16 ]. Eco-health measures environmental degradation and exposure to toxic pollution, while ecosystem vitality focuses on ecological health—such as tree cover loss—and the policies and protections in place to preserve it—e.g. national level biome protections. Ecosystem vitality includes measures that both partially overlap with ND-GAIN measures and measures of GHG emissions and other components not relevant to toxic pollution. As such we only utilize Eco-health from EPI, which represents toxic pollution distributions only. Eco-health measures toxic pollution risk via air quality (52%), water and sanitation (12%), and heavy metals (2%). The air quality measure focuses primarily on PM2.5 exposure and exceedances. While not the only hazardous air pollution, PM2.5 has been demonstrated to pose the greatest risk to human health due to effect and distribution [ 31 , 39 , 43 , 81 – 84 ]. The water and sanitation variable measures drinking water quality and sanitation infrastructure with regards to exposure to toxic pollutants, while the heavy metals measure is comprised solely of estimated lead exposure. Notably, many toxic pollutantsthat directly and pervasively harm humans are not included in Eco-health —e.g., air pollutants such as ground-level Ozone and Sulfur dioxide and heavy metals such as mercury and chromium. This is mostly due to lack of reliable and accessible data on the global distribution of these pollutants and because PM2.5 accounts for the majority of human health harm from air pollution [ 9 , 30 , 31 ].
Global Alliance on Health and Pollution (GAHP).
The GAHP estimates the number of toxic pollution deaths for a country [ 9 ]. They include deaths caused by exposure to toxic air, water, soil, and chemical pollution globally. The GAHP utilizes the Institute for Health Metric’s Global Burden of Disease Study [ 85 ] that measures annual deaths due to all causes. The GAHP results are conservative, as many known toxins are not included in their analysis, yet they assess toxic pollution to be the single largest cause of premature mortality. Their estimates indicate that in 2017 toxic pollution resulted in the premature death of at least 8.3 million premature deaths, or 15% of all deaths globally, and 275 million Disability-Adjusted Life Years. These deaths were caused by toxic air pollution (4.9 million; 59%), water pollution (1.6 million; 19%), occupational exposure (800,000; 9%), or lead exposure (1 million; 12%). As research on the effects of other pollutants becomes more certain—such as growing work on PFAS [ 86 , 87 ] and microplastics [ 88 , 89 ]—the number of premature deaths attributed to pollution is expected to increase substantially [ 7 – 9 ]. We operationalize their data, specifically the estimated proportion of total mortality due to pollution ( Proportion Mortality ) to test the relationship between the EPI assessed toxic pollution distribution ( Eco-health ) and deaths resulting from toxic pollution exposure, and thus validate ecosystem health as an effective measure of toxic pollution risk. We use Proportion Mortality as opposed to total pollution mortality or pollution mortality rate per 100,000 persons to avoid issues of country demographic effects such as total population, access to health care services, and other potentially confounding factors.
We hypothesize that there is a significant positive relationship between the spatial distribution of toxic environments ( Eco-health ) and climate risk ( Vulnerability ). Research strongly suggests that low- and middle-income countries face higher climate risks—though they contribute less than high-income countries to producing the risk—and are on average more impacted by toxic pollution. But, the alignment between the countries most and least at risk of each risk type, and the strength of this potential relationship, remains untested.
Statistical analysis
We specify Vulnerability and Eco-health as additive and Readiness as multiplicative. Together Vulnerability and Eco-health account for where people face the highest pollution risks, while Readiness balances a country’s ability to do something about it if mitigation incentives or policies were targeted there. Target , though it results in a normally distributed measure (Anderson-Darling = 0.563; p = 0.143), is then best interpreted in rank order to compare countries. Research indicates that formal and informal institutional capacity is the most critical component for effective environmental management and regulation [ 90 – 99 ]. Thus, we weight Readiness (making it multiplicative as opposed to additive) to account for the effect of institutional capacity on pollution risk reduction outcomes. Vulnerability and eco-health are weighted equally as there is not a clear consensus as to whether it is toxic or non-toxic pollution that poses the greatest risk to human health. Note that to operationalize Vulnerability and Eco-health in this way, both variables were transformed in the dataset from their raw values to a 100-point scale and such that larger values represent worse health and greater vulnerability and lower values represent better health and lesser vulnerability (see S1 Data ).
Limitations
The data we utilize to account for toxic and non-toxic pollution do not measure all forms of harm or potential risks from these processes. For example, Eco-health only includes PM2.5 to assess air quality, whereas there are numerous hazardous air pollutants. As more and better data on other pollutants becomes available, it will need to be integrated into this assessment and the estimates of highest risk areas may potentially shift. Similar limitations are present in Vulnerability as a measure of climate impacts risk. The total toxic pollution death estimates that comprise Proportion Mortality include only those deaths where pollution-as-cause has high scientific consensus [ 7 ]. The authors estimate that this is only a relatively small portion of the premature mortality that toxic pollution causes or contributes to [ 7 , 9 ]. Also, our measures are static whereas the processes that they measure are dynamic. As such, our estimates provide a critical assessment of the global distribution of the combined risk of toxic pollution and climate impacts risk today, but they are temporally limited. Finally, the data are aggregated to the country level, when toxic and non-toxic pollution risks, as well as the readiness to address these risks, can vary widely within countries, and targeting decisions to reduce pollution may thus require finer intra-country assessments.
A strong (r s = -0.798; 95% CI -0.852, -0.727) and statistically significant (p<0.0001) relationship exists between the spatial distribution of global climate risk ( Vulnerability ) and toxic pollution ( Eco-health ) ( S1 Fig ). Countries that are most at risk of the impacts of climate change are most often also the countries facing the highest risks of toxic pollution. Corroborating this finding, Eco-health and Proportion Mortality are strongly (r s = -.793; 95% CI -0.848, -0.720) and significantly (p<0.0001) correlated; and Proportion Mortality and Vulnerability are strongly (r s = 0.761; 95% CI 0.680, 0.823) and significantly (p<0.0001) correlated. In short, deaths resulting from toxic pollution are highest where the distribution of toxic pollution is greatest and, critically, also where the impacts of climate change pose the greatest risk.
Figs 1 – 3 show the global distribution of Vulnerability , Eco-health , and Proportion Mortality , respectively. Fig 4 shows the combined global distribution of climate risk and toxic pollution risk ( Vulnerability and Eco-health taken together); in alignment with our Spearman rank-order correlation coefficient results, Fig 4 depicts the equally weighted and averaged rank-order of Vulnerability and Eco-health , as opposed to the raw index values. As the correlation test results indicate and the maps visually affirm, the highest climate and toxic pollution risks appear to coincide in the same countries, and they are geographically concentrated across the African continent and Southeast Asia.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
The global distribution of climate impacts risk using by-country rank-order, as measured by the variable Vulnerability from the 2018 ND-GAIN Country Index [ 12 ].
https://doi.org/10.1371/journal.pone.0254060.g001
The global distribution of toxic pollution risk using by-country rank-order, as measured by the variable Eco-health from the 2018 EPI [ 13 ].
https://doi.org/10.1371/journal.pone.0254060.g002
The global distribution of toxic pollution deaths as a percentage of total deaths in 2018, using by-country rank-order, as measured by the variable Proportion Mortality from the GAHP Pollution and Health Metrics Report [ 9 ].
https://doi.org/10.1371/journal.pone.0254060.g003
The global distribution of the combined risk of toxic pollution (low or high ecosystem health) and climate impacts (high or low vulnerability) risk using the average of the by-country rank-order of Vulnerability and Eco-health .
https://doi.org/10.1371/journal.pone.0254060.g004
Our final analysis offers suggestions for how to reduce climate and toxic pollution risks. Directly targeting directly pollution reduction makes sense in countries that are assessed to have high Readiness— a measure of a country’s economic, governance, and social readiness to adapt to environmental risks—scores and will respond effectively to investments or other incentives, such as favorable trade terms. However, in places experiencing governance challenges, such as low state capacity or high corruption, efforts and resources might be better placed in addressing the governance challenges first. We therefore join Vulnerability and Eco-health with Readiness to produce Target . Table 1 lists the top 10 countries most likely to generate a high rate of return on effort in the reduction of toxic pollution and climate change impacts and the bottom 10 countries most likely to require attention to governance issues before pollution could be effectively addressed. Fig 5 depicts the global distribution of the Target variable results.
The global distribution of Target , a measure of a country’s climate impacts risk, toxic pollution risk, and their potential readiness to mitigate these risks.
https://doi.org/10.1371/journal.pone.0254060.g005
https://doi.org/10.1371/journal.pone.0254060.t001
Our tests of the relationship between the distribution of Vulnerability and Eco-health strongly indicate that the countries that face the greatest human health risks from toxic pollution are also those most at risk of the impacts wrought by our changing climate. The potential for these two types of risk to interact and synergize in the environment and in the human body, while understudied [ 9 , 15 , 100 ], is substantial [ 21 , 101 , 102 ]. Compounding these risks is the fact that the countries most at-risk include many of the poorest and least developed in the world, such as the Democratic Republic of the Congo (DRC) (#1), Burundi (#2), and the Central African Republic (#3), which are ranked 179 th , 185 th , and 188 th of 189, respectively, by the United Nations Human Development Index [ 103 ]. The demographic, ecological, and social factors that contribute to these consistently ‘low’ rankings are not independent of each other and are demonstrative of broader patterns of inequality [ 68 , 69 , 104 – 107 ]. Our results affirm the indications from previous research that low-income countries face the highest risks of impacts from climate change and risk from toxic pollution. Our results do not estimate the corresponding impact of the interactions of toxic and climate risk, but evidence from other studies suggests the combined effect is substantial [ 101 , 108 , 109 ]. For example, warming temperatures have been shown to both increase rates of heat-related illness and mortality and to produce and to enhance the toxicity of contaminants in the environment [ 20 , 48 , 110 ]Thus, targeting the improvement of conditions, outcomes, and structures in such countries is globally beneficial and practically and ethically urgent. However, not all countries offer the same basal context for such actions and thus models for assessing structures of risk reduction efforts remain critical.
The incidence of toxic pollution and climate impacts risk in low-income countries is shaped by intersecting local or domestic structural conditions—including reduced capacity for environmental policy regulation and enforcement, especially as applied to industry and transportation standards [ 111 ], as well as physical geography—and by ‘external’ factors such as foreign firms taking advantage of reduced environmental regulation [ 112 ] or shifts in precipitation patterns driven by climate change [ 46 ]. For example, the DRC faces the intersecting risks of PM2.5 transported from the Saharan Desert by predominant wind currents from the northeast (external) but also locally produced PM2.5 from low grade fuels and inefficient vehicles concentrated in city centers, and a landscape littered with foreign commercial (external) and local artisanal (internal) extractive mining operations that alter landscapes and pollute waterways with heavy metals [ 113 – 115 ]. Intersecting with these factors are climate impact risks such as changing rainfall patterns and increased warming that disrupt the farming cycle and concurrently increase risks of malnutrition and incidence of communicable and non-communicable disease [ 116 ]. A similar pattern of intersecting, mutually amplifying environmental risks and endogenous and exogenous factors can be found in all of the countries at the top of our combined Vulnerability - Eco-health list. Notably, our results find that the top one-third of countries at risk of toxic pollution and climate impacts represent more than two-thirds of the world’s population, highlighting the magnitude of the problem and unequal distribution of environmental risk.
Given that a large portion of the world’s population lives in countries at higher toxic pollution and climate impacts risk, understanding where and how to target in pollution risk mitigation is critical to maximizing reductions of potential human harm. Our Target results indicate that the countries facing the highest toxic pollution and climate impacts risk also often lack institutional Readiness to address these problems. This does not mean that efforts to support these countries or to improve their conditions should be abandoned—or that efforts to restrict the external factors acting upon them should be altered—but rather that focusing on and bolstering institutional capacity development is likely the initial, and primary, focus of effort.
However, many other countries could benefit from direct efforts towards pollution risk reduction. Two of the countries in our top 5 highest Target results, China and India, are substantially economically developed and hold prominent geopolitical power. They are the largest countries on the planet, together representing over 2.5 billion people, and both have relatively high Proportion Mortality ranks, ranking 13 th and 5 th (17.9% and 23.5% of annual deaths are associated with toxic pollution, equaling 1.9 and 2.3 million premature deaths annually, respectively) [ 9 ]. Despite these high rates, recently developed national policies and their resultant impacts suggest that the benefits of augmenting facilitation of such changes (via targeted policy efforts and incentives) are large and achievable. For example, as a result of China’s Air Pollution and Prevention and Control Action Plan enacted in 2013 and targeting PM2.5 specifically, Han et al. [ 117 ] find that annual average PM2.5 levels reduced substantially between 2013–2017—from 101.7 μg m -3 to 58.6 μg m -3 , a 40% reduction. The improved air quality resulted in significant corresponding reductions in respiratory disease and cardiovascular disease mortality rates—both of which have been demonstrated to be strongly linked to toxic air pollution [ 30 , 31 , 84 ]. Interestingly, if global annual average PM2.5 emissions could be reduced even half the amount that China achieved—i.e. 20%—the estimated corresponding effect would be 1.4 million fewer premature deaths annually worldwide [ 31 ]. Han et al. caution that air pollution remains severe across China and further regulatory restrictions and mitigation efforts are much needed. Importantly, while our results indicate that targeting these countries will likely produce positive reductions in human suffering domestically, as China is the world’s leading total GHG emitter and India is on track to join it at the top in the future, both emit high rates of toxic pollution ( Eco-health) that also can travel outside of their borders. Thus, there is strong potential for co-benefits from efforts focused on China and India in risk reduction for neighboring countries and other countries at-risk of climate change more broadly.
Importantly, our Target results should be understood as assessing where policy tools can potentially be leveraged with high effects—whether those tools be local, national, and international in nature, scale, and application. A range of measures can be used to promote risk reduction such as trade incentives, be they negative or positive incentives, or other policy and regulatory enforcement mechanisms. Likely a suite of tools will need to be employed and leveraged to achieve the desired risk reduction goals [ 8 , 11 , 17 , 94 ].
Despite the interdependence of risks from toxic and non-toxic pollution, no prior study has analyzed the joint global distribution of these risks nor offered evidence-based arguments for how to address the co-impact of both risks efficiently. We fill components of these knowledge gaps with data on global climate risk, environmental quality, toxic pollution caused mortality, and institutional capacity for 176 countries. Our analysis demonstrates a strong correlation between toxic pollution risk and climate risk, along with varying capacities of countries to manage that risk. We argue that the Target assessment tool can be usefully employed to determine optimal locations for risk reduction, while also drawing attention to high-risk low-income countries that must urgently address governance challenges in order to have a chance at successfully addressing pollution risk.
Some have argued that the challenges presented by human-produced pollution may be nearing tipping points past which returning to the ecological niche representative of most of human history will become unattainable [ 3 , 28 ]. However, recent global events have highlighted that behavioral changes at national levels can have dramatic and rapid effects on pollution levels [ 118 – 120 ]. For example, regulation on movement and activity in response to Covid-19 resulted in dramatic decreases in air pollution rates in some countries [ 120 , 121 ]. Broad and expansive action, akin to that sparked by Covid-19 but more strategic and sustainable is needed to combat the pressures wrought by human-produced pollution on the human niche [ 46 , 50 , 122 ]. It is our hope that the Target measure can be deployed as part of a larger ongoing empirical assessment of human caused pollution to increase political and social will at national levels for drastic policy measures and broad reaching pollution reduction actions.
Supporting information
S1 fig. results of spearman’s rank-order correlation coefficient (r s ) and corresponding scatterplots for the variables vulnerability , eco-health , and proportion mortality ..
https://doi.org/10.1371/journal.pone.0254060.s001
https://doi.org/10.1371/journal.pone.0254060.s002
- View Article
- Google Scholar
- PubMed/NCBI
- 9. Fuller R, Sandilya K, Hanrahan D. Pollution and Health Metrics. New York, NY: Global Alliance on Health and Pollution; 2019 p. 56. Available: https://gahp.net/wp-content/uploads/2019/12/PollutionandHealthMetrics-final-12_18_2019.pdf .
- 12. ND-GAIN. ND-GAIN Country Index rankings | ND-GAIN Index. Notre Dame: Notre Dame Global Adaptation Index; 2019. Available: http://index.gain.org/ranking .
- 13. EPI. Environmental Performance Index 2018. New Haven, CT: Yale Center for Environmental Law and Policy; 2018 p. 200.
- 16. GAHP. Pollution Health Overview and Solutions. Geneva: Global Alliance on Health and Pollution; 2019 p. 5.
- 24. Psaki J. Press Briefing by Press Secretary Jen Psaki, Special Presidential Envoy for Climate John Kerry, and National Climate Advisor Gina McCarthy, January 27, 2021. Washington, D.C.: The White House Press Briefings; 2021 Jan p. 14. Available: https://www.whitehouse.gov/briefing-room/press-briefings/2021/01/27/press-briefing-by-press-secretary-jen-psaki-special-presidential-envoy-for-climate-john-kerry-and-national-climate-advisor-gina-mccarthy-january-27-2021/ .
- 46. IPCC. Summary for Policy Makers. In Global warming of 1.5°C. An IPCC special report on the impacts of global warming of 1.5°C above pre-industrial levels and related global greenhouse gas emission pathways. Geneva, Switzerland: World Meteorological Organization; 2018.
- 50. IPCC. Climate Change and Land: An IPCC Special Report on climate change, desertification, land degradation, sustainable land management, food security, and greenhouse gas fluxes in terrestrial ecosystems. Geneva, Switzerland: International Panel on Climate Change; 2019 p. 43.
- 53. IPCC. IPCC Special Report on the Ocean and Cryosphere in a Changing Climate. New York: International Panel on Climate Change; 2019 p. 1170.
- 55. WHO. Quantitative risk assessment of the effects of climate change on selected causes of death, 2030s and 2050s. Geneva: World Health Organization; 2014. Available: https://apps.who.int/iris/handle/10665/134014 .
- 66. Cambridge Centre for Risk Studies. Global Risk Index 2019. University of Cambridge: Cambridge Centre for Risk Studies; 2019 p. 16. Available: https://www.jbs.cam.ac.uk/fileadmin/user_upload/research/centres/risk/downloads/crs-global-risk-index-exec-summary-2019.pdf .
- 67. Smith A, Lott N, Houston T, Shein K, Crouch J, Enloe J. U.S. Billion-Dollar Weather & Climate Disasters 1980–2018. Silver Springs, Maryland: National Oceanic and Atmospheric Administration; 2018 pp. 1–14.
- 68. Burke M, Tanutama V. Climatic Constraints on Aggregate Economic Output. Cambridge, MA: National Bureau of Economic Research; 2019 Apr p. w25779. Report No.: w25779. https://doi.org/10.3386/w25779
- 76. Fagan B. The Great Warming: Climate Change and the Rise and Fall of Civilizations. Bloomsbury Publishing USA; 2010.
- 98. Kraft ME. Environmental Policy and Politics. Taylor & Francis; 2017.
- 103. UNDP. Human Development Index (HDI) | Human Development Reports. Geneva, Switzerland: United Nations Development Program; 2019 p. 2. Available: http://hdr.undp.org/en/content/human-development-index-hdi .
- 111. World Bank. Natural Hazards, UnNatural Disasters: the economics of effective prevention. Washington, D.C.: World Bank; 2010.
- 116. Hales S, Kovats S, Lloyd S, Campbell-Lendrum D. Quantitative risk assessment of the effects of climate change on selected causes of death, 2030s and 2050s. Geneva, Switzerland: World Health Orgnaization; 2014 p. 128.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Wiley-Blackwell Online Open

Air pollution: Impact and prevention
Martha patricia sierra-vargas.
1 National Institute for Respiratory Diseases ‘Ismael Cosío Villegas’, México
LUIS M TERAN
2 Biomedicine in the Post-Genomic Era, Huitzilac, Morelos, Mexico
Air pollution is becoming a major health problem that affects millions of people worldwide. In support of this observation, the World Health Organization estimates that every year, 2.4 million people die because of the effects of air pollution on health. Mitigation strategies such as changes in diesel engine technology could result in fewer premature mortalities, as suggested by the US Environmental Protection Agency. This review: (i) discusses the impact of air pollution on respiratory disease; (ii) provides evidence that reducing air pollution may have a positive impact on the prevention of disease; and (iii) demonstrates the impact concerted polices may have on population health when governments take actions to reduce air pollution.
INTRODUCTION
Environmental pollution has been a matter of concern for many years. The Mellon Institute of Pittsburgh, PA, USA, sponsored the first broad scientific study of smoke abatement, which resulted in legislation designed to decrease the effects of smoke. 1 It is now well known that environmental contamination impacts on health; the World Health Organization estimates that every year, 2.4 million people die from causes associated with air pollution. It is increasingly recognized that implementation of strategies to reduce pollution can have substantial health benefits. For example, the Environmental Protection Agency proposed that the implementation of measures to reduce emissions from diesel e ngines could result in 12 000 fewer mortalities and prevent 15 000 heart attacks and 8900 hospital admissions in the United States each year. 2 The aim of this review is to provide information on the impact of pollution on respiratory health, as well as to discuss strategies for reducing air pollution, as proposed in a number of clinical reports. Particulate matter (PM) and ozone (O 3 ) pollution are major causes of concern in the community.
PARTICULATE MATTER (PM)
PM is a complex mixture of solid and liquid particles suspended in air that is released into the atmosphere when coal, gasoline, diesel fuels and wood are burned. It is also produced by chemical reactions of nitrogen oxides and organic compounds that occur in the environment. Vegetation and livestock are also sources of PM. In big cities, production of PM is attributed to cars, trucks and coal-fired power plants.
The health effects of PM depend on several factors, including the size and composition of the particles, the level and duration of exposure, and the gender, age and sensitivity of the exposed individual. Symptoms of exposure may include persistent cough, sore throat, burning eyes and chest tightness. PM may also trigger asthma or lead to premature death, particularly in elderly individuals with pre-existing disease. 3,4 In addition, people who are active outdoors are at higher risk, as physical activity increases the amounts of PM penetrating into the airways. People with disease (e.g. diabetes mellitus, malnutrition) are also at increased risk. 5–7 A comprehensive review on diesel PM by Ristovski et al . was published in an earlier issue of this review series on air pollution and lung disease. 8
OZONE (O 3 )
O 3 is mainly formed by the interaction of ultraviolet light with both nitrogen oxides and organic compounds. O 3 exhibits potent anti-oxidant properties and induces alterations in the airways that depend on concentration and the duration of exposure.
EFFECTS ON RESPIRATORY HEALTH
The airways are a point of entry for pollutants, which in turn may cause lung disease. For example, PM may be deposited into any of the three respiratory compartments: the extrathoracic, tracheobronchial and alveolar regions. 9 PM > 10 µm in diameter (coarse particles) is deposited in the extrathoracic region, PM with a diameter between 5 and 10 µm is deposited in the tracheobronchial region and particles <2.5 µm in diameter (fine particles) are deposited in the alveolar region ( Fig. 1 , Table 1 ). 10 For particles between 3 and 5 µm in diameter, the total deposition fraction is greater for women than for men. 11 The potential health effects of greatest concern are associated with particles that penetrate to the tracheobronchial and alveolar regions. 12 The deposition rate may also be increased in individuals with pre-existing respiratory disease, as compared with healthy individuals. 13 It has been suggested that particles ≤0.1 µm in diameter (ultrafine particles) are more toxic than larger particles as they may cover a greater area of the alveolus. One host defence mechanism is phagocytosis of ultrafine particles by alveolar macrophages ( Fig. 2 ). However, due to their small size, ultrafine particles overwhelm macrophage phagocytosis, resulting in increased penetration, which causes deleterious effects in other organs (e.g. brain, heart, bone marrow, etc.). 14,15

Regional deposition of particles in the human respiratory tract.
Environmental Protection Agency (EPA) terminology for particle sizes
d pa , aerodynamic particle diameter.
Data taken from http://www.epa.gov/apti/bces/module3/category/category.htm

Alveolar deposition of particles and cell activation. Particles deposited in the bronchoalveolar region may be trapped and are cleared by the mucus layer (1); particles phagocytosed by alveolar macrophages follow the lymphatic clearance pathway, can impair phagocytosis and trigger the release of inflammatory mediators (2, 3) and neutrophil chemotactic factors, which in turn results in the release of reactive oxygen and nitrogen species (4). Furthermore, soluble particle components (e.g. metals) can cross the epithelial barrier and be distributed to other organs where they can cause adverse effects (5). ICAM, intercellular adhesion molecule; IL, interleukin; MPO, myeloperoxidase; VCAM, vascular cell adhesion molecule (6).
Toxicological studies have demonstrated the translocation of particles from the olfactory mucosa via axons to the olfactory bulb of the brain. 16,17 Indoor activities in the home that result in the generation of particles include cooking (in ovens, toasting, frying, barbecuing), cleaning (dusting, sweeping, vacuuming) and the movement of people. Ozkaynak et al . reported that cooking resulted in the generation of 4.1 ± 1.6 mg/min of PM 10 , with the fine fraction contributing 40% of the total PM. 18 Once PM enters the body, it affects different organ systems.
The source and composition of particles determine their toxicity, 19,20 but size is a major factor determining toxicity in the lungs due to the generation of reactive oxygen and reactive nitrogen species. Particle size may also physically hinder macrophage clearance, 21 thereby increasing toxicity. In general, particles exacerbate acute and pre-existing respiratory diseases, including viral infections, asthma, bronchitis and chronic respiratory disease. 22–24 Many transition metals present on particles serve as catalysts for a Fenton-like reaction that initiates the production of reactive oxygen and reactive nitrogen species, resulting in an inflammatory response. Using electron microscopy, Brauer et al . 25 showed significantly higher particle concentrations in the lungs, at autopsy of Mexican females who had never smoked, as compared with control Vancouver residents. Interestingly, Budinger et al . 26 reported that inhalation of PM 2.5 was sufficient to activate coagulation and inhibit fibrinolysis. Traffic particles appear to be more strongly associated with these effects, 27 as they are rich in elemental carbon, which can cause an increase in respiratory symptoms in children 28,29 and women living in urban areas. 30
It is now well established that exposure to O 3 impairs lung function. In healthy individuals, O 3 causes reductions in vital capacity, forced expiratory volume in 1 s and lung resistance. The effects of O 3 exposure increase with physical exercise. Patients with respiratory diseases are more susceptible to the effects of O 3 . Under conditions of oxidizing air pollution, as in summer, O 3 exposure may lead to asthma exacerbations.
ALLERGIC DISEASES
Allergic diseases such as asthma and allergic rhinitis are very common in children and young adults. In most cases, asthma in these groups of patients is characterized by increased synthesis of immunoglobulin E against common allergens. 31 Exposure of these patients to specific aeroallergens such as pollens leads to a series of immunological changes culminating in the symptoms of asthma. It is now well established that increased air pollution affects pollen production, which in turn impacts negatively on the prevalence and severity of allergic asthma.
Diesel exhaust contains numerous pollutants and polycyclic aromatic hydrocarbons, which enhance allergenicity and asthma symptoms by acting in synergy with allergens. Experimental studies conducted by Muranaka et al . 32 showed that diesel-exhaust particles act as an adjuvant for immunoglobulin E production in response to specific allergens (ovalbumin or Japanese Cedar pollen). Moreover, inhalation of diesel-exhaust particle leads to a typical asthma phenotype, characterized by pulmonary inflammation and airway hyperresponsiveness. 33,34 It has been proposed that when diesel-exhaust particles are engulfed by macrophages, a Th2-type inflammatory response is induced, whereas diesel-exhaust particles that are not engulfed produce a Th1-type inflammatory response. 35–37
High carbon dioxide concentrations in the environment increase both pollen production and the allergenicity of pollen. Indeed, Singer et al . 38 showed that high concentrations of carbon dioxide enhanced the production of Amb a 1, an allergenic protein in ragweed pollen, while Ziska et al . 39 reported that in urban locations where carbon dioxide concentrations are higher, ragweed produces greater amounts of pollen (which contains the Amb allergen) than it does in rural locations. The enhanced allergenicity of pollen may be explained by the synergistic association between allergen-loaded pollen debris and aromatic hydrocarbons contained in fine particles. 40
On the other hand, traffic-related pollutants (nitrogen dioxide, O 3 ) can trigger the release of allergens from pollen granules, leading to an increase in the concentration of airborne pollen allergens. 41 For example, Dutch children attending schools that were within 400 m of a major roadway showed increased sensitization to outdoor allergens; the relationship between symptoms and traffic-related pollution was observed mainly in children who were sensitive to allergens. 42 Similarly, increased levels of O 3 and PM 2.5 in summer were found to be associated with a higher prevalence of respiratory allergy symptoms in US children living in urban areas. 43 D'Amato et al . 44 hypothesize that air pollutants: (i) allow easier penetration of pollen allergens into the airways; (ii) increase the release of antigens from pollen grains, thereby leading to allergic responses; and (iii) absorb pollen grains, leading to prolonged retention of pollen grains in the body. A recent prospective birth cohort study involving over 2000 children showed that exposure to ambient PM increased the risk of atopic diseases. 45
MECHANISMS OF LUNG DAMAGE
Oxidative stress.
Oxidative stress plays a central role in the mechanisms by which air pollutants damage human health. In addition, reactive nitrogen species are generated in the lungs following exposure to particles. Nitric oxide released by inflammatory cells reacts with superoxide anion radicals to form peroxynitrite, which then initiates the nitration of tyrosine residues on proteins. These changes contribute to the progression of disease. 46,47 On the other hand, the endogenous pool of H 2 O 2 reacts with some enzymes such as myeloperoxidase to produce highly reactive metabolites (hypochlorous acid). 47,48 Vujovic et al . reported an increase in malondialdehyde concentrations, whereas there was a reduction in superoxide dismutase activity (anti-oxidant defence) in children exposed to air pollution. 49 Similarly, increased plasma levels of thiobarbituric acid reactive substances have been associated with exposure to black carbon and PM 2.5 . 50 Individuals living in a polluted environment also showed increased plasma levels of thiobarbituric acid reactive substances. 52
In animals, intratracheal instillation of PM causes a significant increase in serum levels of cytokines such as interleukin-6. 53 Human macrophages exposed to particles, release a range of cytokines, including tumour necrosis factor-α, interleukin-6, interleukin-1β, macrophage inflammatory protein-1-α and granulocyte macrophage-colony stimulating factor. 54 These cytokines activate nuclear factor kappa B and/or activator protein 1. 55,56 Ultrafine black carbon is also involved in the activation of nuclear factor kappa B via protein kinase C. 57,58 Metals contained in PM can induce a series of redox reactions causing oxidative DNA damage.
We have shown that exposure to O 3 results in the release of increased levels of growth-related oncogene-α into the airway lining fluid in normal subjects. 59 Interestingly, in a separate study, we demonstrated that neutrophils from asthmatic patients exposed to fine particles (PM 2.5 ) generated reactive oxygen species. 60 There is also a relationship between air pollution and cancer; pollutants may increase the risk of cancer through the formation of reactive oxygen species, especially hydroxyl and superoxide anion radicals, which may induce oxidative damage to cellular membrane lipids, protein enzymes and DNA. 61
PREVENTION OF AIR POLLUTION
Clinical studies.
It is well understood that pollution has a profound effect on health; therefore, reduction of pollution has a positive effect on health, particularly the health of susceptible individuals. The first population-based study that showed significant improvements in life expectancy in relation to reductions in PM 2.5 concentrations was conducted in the United States, 62 and showed a clear relationship between reduction in fine-particle concentrations and life expectancy. This observation was confirmed in a cohort study of Swiss adults, which demonstrated that decreases in ambient PM 10 levels were associated with reductions in respiratory symptoms. 63
Reductions in the levels of air pollution can be achieved in many ways, and governments can play a key role. Figure 3 shows PM 10 levels in some of the most polluted countries. For example, during the 2008 Olympic Games, the Chinese government was able to control air pollution. 64 This resulted in a 41.6% decrease in the average number of outpatient visits for asthma during the Olympics, as compared with before the games started. A separate study of 36 fourth-grade Beijing children, before, during and after the Beijing Olympics, showed that fractional exhaled nitric oxide (FeNO) levels were significantly lower during the period of the Olympics and increased by 16.6% in the first hours after exposure, suggesting that rapid inflammatory changes took place. 65

Pollution in 37 cities selected from 91 countries, as reported by the World Health Organization (WHO). Particulate matter (PM) 10 levels >20 µg/m 3 may pose health risks (data taken from http://apps.who.int/ghodata/?vid=4201 ).
In rural Mexico, a randomized trial of properly vented wood-burning cooking stoves versus open fires showed reductions in the longitudinal decline in forced expiratory volume in 1 s and improvements in respiratory symptoms, when proper cooking stoves were used. 66 The use of improved cooking stoves has also been found to halve the exposure to carbon monoxide and resulted in a lower rate of diagnosis of pneumonia. 67
Evidence is accumulating that polymorphisms in several genes involved in oxidative stress play an important role in susceptibility to O 3 . 68–70 These genes include those coding for phase II enzymes, including glucuronosyl transferases, glutathione S -transferases (GST), NAD(P)H:quinone oxidoreductases and N -acetyltransferases, all of which mediate the detoxification and elimination of toxic products.
GSTM1 and GSTP1 have been the most frequently studied enzymes. A study of Mexican children exposed to high concentrations of O 3 showed an association between polymorphisms in the oxidative stress-related GSTM1 gene and the development of asthma. 68 Interestingly, children with the GSTM1-null genotype were more susceptible to the effects of O 3 . However, taking supplements containing the anti-oxidant vitamins C and E conferred protection against O 3 exposure. 68 Similarly, sulforaphane, a potent inducer of phase II enzymes, was also shown to enhance enzyme expression and downregulate inflammatory responses in human bronchial epithelial cells; 69 sulforaphane increased GSTM1 and NAD(P)H:quinone oxidoreductase 1 expression, as well as GST activity while decreasing cytokine production. More recently, long-term supplementation with D-α-tocopheryl acetate, a natural vitamin E anti-oxidant, was shown to inhibit oxidant stress in the airways of mild atopic asthmatics exposed to segmental allergen challenge; improvements in allergic inflammation and bronchial hyperreactivity were observed. 70 Studies of additional genes involved in the oxidative stress response have been reviewed previously. 71
AIR POLLUTION AND CLIMATE-CHANGE MITIGATION
Climate change can enhance the levels of some environmental pollutants, including O 3 and PM 2.5 . For example, the formation of photochemical smog and O 3 increases with higher temperatures. Doherty et al . quantified the burden of heat and O 3 on mortality in 15 UK conurbations during the 2003, 2005 and 2006 heatwave periods. 72 The results indicated that the number of deaths attributable to O 3 was higher than the number attributable to heat. Furthermore, O 3 concentrations rose significantly during the summer of 2003, reaching a maximum of 100 ppb. 72 Ambient concentrations of particles may increase due to forest fires that are a consequence of a dry environment and other climatological effects such as El Niño. During 1998 in Indonesia, forest fires linked with El Niño resulted in the exposure of some 20 million people across South-East Asia to harmful smoke-borne pollutants. Monthly PM 10 values, which usually fluctuate between 30 and 50 µg/m 3 , increased to between 60 and 110 µg/m 3 during September–October 1997. The incidence of medical complaints rose by about 30% during this period.
Some of the planned climate-change mitigation strategies include more efficient use of fossil fuels for industrial processes and electricity generation, switching to renewable energy (solar/wind/wave power), increasing the fuel efficiency of vehicles, improving the insulation of buildings, growing new forests, nuclear power and carbon sequestration. It is generally accepted that efforts in all these areas will, at best, prevent further warming but not reverse existing warming.
The Mexican Government recently introduced significant measures aimed at reducing climate change, including a law to reduce carbon dioxide emissions by 30% by 2020 and by 50% below 2000 levels by 2050. 73 Furthermore, it aims to generate 35% of the country's energy from renewable sources by 2024. At the beginning of 2001, the authorities in Monterrey, Mexico, built a 7-megawatt plant that converts 214 million m 3 of landfill gas into electricity and powers the light rail transit system and city street lighting at night. Despite these changes, Mexico still faces some hurdles, including enforcement of the new laws; current problems include urban planning, excessive industrialization and traffic jams in large cities. In this regard, the United Kingdom has implemented some measures in London, to take taxis older than 15 years and private hire vehicles older than 10 years off the road, build bicycle superhighways (cycle revolution) and introduce 300 hybrid buses by the end of 2012.
Urban forests and green roofs have also been proposed as strategies for reducing pollution in urban areas. 74 Vegetation removes pollutants in several ways; by absorbing gaseous pollutants, through interception of PM by leaves, and by breaking down organic compounds such as polycyclic aromatic hydrocarbons. 75 Transpirational cooling also reduces temperatures indirectly, which results in a reduction in photochemical reactions that form O 3 and other air pollutants in the atmosphere. It has been estimated that in the United States, trees remove 711 000 metric tonnes of carbon monoxide, nitrogen dioxide, O 3 , PM and sulphur dioxide per year. 76 However, in many urban areas, there is little space for planting trees or cultivating urban forests. For example, in the mid-Manhattan, west section of New York, 94% of the land is covered with concrete, leaving little space for planting trees at ground level. 77 However, rooftops, which often comprise nearly half the impermeable area in a city, provide an opportunity for growing vegetation. 78 Two thousand square metres of uncut grass on a green roof can remove upto 4000 kg of PM. 79
Public policy and individual action are both required to reduce the effects of pollutants on respiratory health. Interventions at the individual level may include the avoidance of exercise or cycling near busy roadways to reduce exposure, and improvements in the ventilation of homes in which biomass fuels are used. Moreover, public policies can encourage or mandate engineering solutions that drastically reduce emissions from cooking stoves and vehicles. Trials such as those performed during the Beijing Olympics have demonstrated how such changes may have implications for human health. Taken together, these observations suggest that reducing the levels of air pollutants will have a substantial impact on health, particularly the health of patients with respiratory diseases.
The main public health responses to the projected health impacts of climate change are mitigation and adaptation. Adaptation is not an effective risk management strategy for poor air quality, because physiological mechanisms for decreasing susceptibility to O 3 and other air pollutants are limited. Therefore, if improved modelling experiments continue to predict higher O 3 concentrations with changing climate, rapid reductions in emissions from the burning of fossil fuels are needed, in order to protect the health of current and future generations. Evidence suggests that reducing current tropospheric O 3 concentrations reduces morbidity and mortality, with significant savings in the costs of medical care. 80
CONCLUSIONS
Air pollution currently affects the health of millions of people. We have presented evidence on the effects of pollutants on patients with limitations in their respiratory capacities. For example, O 3 and PM may trigger asthma symptoms or lead to premature death, particularly in elderly individuals with pre-existing respiratory or cardiovascular disease. In addition, pollutants enhance the release of allergenic pollen grains, which results in an increased prevalence of pollen-induced asthma. Thus, the case for action to reduce air pollution is overwhelming and this action can take many forms. Some of these include urban planning, technological developments (e.g. the design of new vehicles that produce less pollution), and at the government level, the introduction of new laws. It has been estimated that reducing both black carbon and O 3 levels would prevent over 3 million premature deaths and increase crop yields by around 50 million tonnes annually. Improvements to cooking stoves would also decrease demand for firewood and reduce deforestation in the developing world. Similarly, improved brick kilns that are used in parts of Latin America and Asia use 50% of the fuel used by traditional kilns. 81
If air pollution levels in heavy traffic areas were reduced, the incidence of asthma and other respiratory diseases would be significantly reduced. 28 While it is generally accepted that efforts to reduce air pollution will prevent further environmental changes, they will not reverse existing warming. Interestingly, an increasing number of studies show that in individuals with low anti-oxidant levels, dietary supplements could be used as a promising approach to reducing susceptibility to air pollution, and providing an alternative strategy for neutralizing the effects of pollutants on health.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 04 October 2021
Clean air for a sustainable world
Nature Communications volume 12 , Article number: 5824 ( 2021 ) Cite this article
20k Accesses
6 Citations
17 Altmetric
Metrics details
Air pollution is a cause of disease for millions around the world and now more than ever urgent action is required to tackle the burden of its impacts. Doing so will not only improve both life expectancy and quality of life, but will also lead to a more just and sustainable world.
Recently, we announced that we will publish a new series of collections focused on issues related to the Sustainable Development Goals (SDGs). We start this series with a multidisciplinary collection on air pollution. As tackling air pollution is not one of the core SDGs, this may seem like an unusual choice. It is, however, a pressing environmental hazard affecting an ever increasing part of the world’s population. Currently, 91% of the world’s population live in locations where pollution levels exceed WHO guidelines, and in a recent announcement the WHO have further cut the recommended limits. Air pollution kills around 6.7 million people per year mainly through respiratory and cardiovascular diseases 1 , and has significant impacts on mental health. The main pollutants are sourced from fossil fuel combustion for transport, industry, agriculture and cooking stoves and, therefore, air pollution is linked directly with fulfilling many of our basic needs. As the SDGs aim to tackle the issue of how humanity can live sustainably, it is thus no surprise that addressing air pollution is related to the SDGs in many different ways. Promoting specific SDGs will lead to improved air quality as a side-effect, while reducing emissions will also progress a number of SDGs directly.
The high air pollution levels that we live with today is another demonstration of how our unsustainable lifestyles are one of the key challenges that needs to be overcome to create a more just and liveable world, which is the ultimate goal of the SDGs.

Although air pollution is a global issue, exposure is often not distributed equally. Industrial processes related to the production, trade and consumption of goods is a key source of air pollution. Much of this pollution is released in low- and middle-income countries while they manufacture goods that are traded abroad, allowing rich countries to outsource the air pollution and health effects of their consumption. Hence, global implementation of responsible consumption and sustainable production practices—the focus of SDG9 (“Industry, Innovation and Infrastructure”) and SDG12 (“Responsible Consumption and Production”)—will be key to reduce this unequal responsibility and exposure to dangerous environmental conditions.
Inequality in exposure does not only occur at an international level, but also within countries. Systematic and historical forms of discrimination often translate into higher exposure levels and, hence, enhanced health burdens to marginalized groups around the world. This is probably best studied in the US, where people of colour are shown to live under poorer air quality, independent of other factors like income 2 . In a commentary for our collection Viniece Jennings highlights that whilst green infrastructure has the potential to reduce air pollution, unequal access can limit improvements for marginalised communities 3 . While we often think of air pollution as an outdoor issue, much of the exposure to harmful particles actually happens inside houses. Household air pollution is mainly related to cooking, heating or lighting, often through the combustion of solid fuels. This exposure affects women and children disproportionately, especially in the developing world 4 . Consequently, targeting SDG10 (“Reduce inequality within and among countries”) and SDG 7 (“Ensure access to affordable, reliable, sustainable and modern energy for all.”) will be of vital importance to tackle embedded inequalities within and among countries to reduce air pollution exposure.
Air pollution and climate change are closely intertwined as they share the same root cause of human emissions. Even though ambitious climate mitigation policies do not come for free, they will in many cases also lead to improved air quality and lower health costs. The societal costs of air pollution avoided through reduced exposure levels as a result of climate mitigation measures alone are thought to outweigh the initial costs of these policies 5 . Air pollution also physically interacts with the climate system; particles in the atmosphere affect surface temperatures as well as clouds and precipitation. Climate change thus has the potential to “worsen air pollution, even in areas where it has been improving”, as pointed out by Denise Mauzarell in a Q&A for our Clean Air collection 6 . An example of this are the dangerous pollutants released by wildfires that are expected to become ever more frequent and intense in many parts of the world.
Similarly, to climate mitigation, improving air quality depends on strict and ambitious regulatory policies and controls, which must be implemented equitably. In this regard, there are reasons to be optimistic, as strict air quality policies like the Clean Air Act in the US and similar policies in Europe have resulted in reductions in pollution since the 1970s even though levels are still too high and continued efforts are crucial. These efforts show that ambitious policy supported by technological advances like improved filtering and modernization can be successful. These efforts should not only be done at national levels, but also need international collaboration, technology and knowledge transfer in order to acknowledge the shared responsibilities of air pollution. As part of the Clean Air collection we highlight papers Nature Communications has published that look at how policy and technology can be part of the solution to air pollution.
The high air pollution levels that we live with today is another demonstration of how our unsustainable lifestyles are one of the key challenges that needs to be overcome to create a more just and liveable world, which is the ultimate goal of the SDGs. Of course, reducing air pollution on its own will not meet the aims of all the other SDGs. Still, it is an illustrative example of how an interdisciplinary focus on a measurable and technologically approachable issue can help to also achieve other goals. It is in this spirit that our collection brings together research from different disciplines, such as applied scientists, economists, political scientists, health scientists and climate scientists as it is this interdisciplinary collaboration that Nature Communications wants to support will be vital in informing policy and decision makers. We envision that our collection on Clean Air will continue to grow and we welcome submissions across disciplines in this area.
GBD Global Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396 , 1223–1249 (2020).
Tessum, C. W. et al. PM 2.5 polluters disproportionately and systemically affect people of color in the United States. Sci. Adv. 7 , 18 (2021).
Jennings, V., Reid C. E., & Fuller C. H. Green infrastructure can limit but not solve air pollution injustice. Nat. Commun. 12 , 4681 (2021).
Gordon, S. B., et al. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir. Med. 2 , 823–860 (2014).
Vandyck, T. et al. Air quality co-benefits for human health and agriculture counterbalance costs to meet Paris Agreement pledges. Nat. Commun. 9 , 4939 (2018).
Nat. Commun. (2021). https://doi.org/10.1038/s41467-021-25491-w .
Download references
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Clean air for a sustainable world. Nat Commun 12 , 5824 (2021). https://doi.org/10.1038/s41467-021-25885-w
Download citation
Published : 04 October 2021
DOI : https://doi.org/10.1038/s41467-021-25885-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Processing nomex nanofibers by ionic solution blow-spinning for efficient high-temperature exhausts treatment.
- Zekun Cheng
- Haiyang Wang
Advanced Fiber Materials (2023)

Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Reference Manager
- Simple TEXT file
People also looked at
Review article, effects of water pollution on human health and disease heterogeneity: a review.

- 1 Research Center for Economy of Upper Reaches of the Yangtse River/School of Economics, Chongqing Technology and Business University, Chongqing, China
- 2 School of Economics and Management, Huzhou University, Huzhou, China
Background: More than 80% of sewage generated by human activities is discharged into rivers and oceans without any treatment, which results in environmental pollution and more than 50 diseases. 80% of diseases and 50% of child deaths worldwide are related to poor water quality.
Methods: This paper selected 85 relevant papers finally based on the keywords of water pollution, water quality, health, cancer, and so on.
Results: The impact of water pollution on human health is significant, although there may be regional, age, gender, and other differences in degree. The most common disease caused by water pollution is diarrhea, which is mainly transmitted by enteroviruses in the aquatic environment.
Discussion: Governments should strengthen water intervention management and carry out intervention measures to improve water quality and reduce water pollution’s impact on human health.
Introduction
Water is an essential resource for human survival. According to the 2021 World Water Development Report released by UNESCO, the global use of freshwater has increased six-fold in the past 100 years and has been growing by about 1% per year since the 1980s. With the increase of water consumption, water quality is facing severe challenges. Industrialization, agricultural production, and urban life have resulted in the degradation and pollution of the environment, adversely affecting the water bodies (rivers and oceans) necessary for life, ultimately affecting human health and sustainable social development ( Xu et al., 2022a ). Globally, an estimated 80% of industrial and municipal wastewater is discharged into the environment without any prior treatment, with adverse effects on human health and ecosystems. This proportion is higher in the least developed countries, where sanitation and wastewater treatment facilities are severely lacking.
Sources of Water Pollution
Water pollution are mainly concentrated in industrialization, agricultural activities, natural factors, and insufficient water supply and sewage treatment facilities. First, industry is the main cause of water pollution, these industries include distillery industry, tannery industry, pulp and paper industry, textile industry, food industry, iron and steel industry, nuclear industry and so on. Various toxic chemicals, organic and inorganic substances, toxic solvents and volatile organic chemicals may be released in industrial production. If these wastes are released into aquatic ecosystems without adequate treatment, they will cause water pollution ( Chowdhary et al., 2020 ). Arsenic, cadmium, and chromium are vital pollutants discharged in wastewater, and the industrial sector is a significant contributor to harmful pollutants ( Chen et al., 2019 ). With the acceleration of urbanization, wastewater from industrial production has gradually increased. ( Wu et al., 2020 ). In addition, water pollution caused by industrialization is also greatly affected by foreign direct investment. Industrial water pollution in less developed countries is positively correlated with foreign direct investment ( Jorgenson, 2009 ). Second, water pollution is closely related to agriculture. Pesticides, nitrogen fertilizers and organic farm wastes from agriculture are significant causes of water pollution (RCEP, 1979). Agricultural activities will contaminate the water with nitrates, phosphorus, pesticides, soil sediments, salts and pathogens ( Parris, 2011 ). Furthermore, agriculture has severely damaged all freshwater systems in their pristine state ( Moss, 2008 ). Untreated or partially treated wastewater is widely used for irrigation in water-scarce regions of developing countries, including China and India, and the presence of pollutants in sewage poses risks to the environment and health. Taking China as an example, the imbalance in the quantity and quality of surface water resources has led to the long-term use of wastewater irrigation in some areas in developing countries to meet the water demand of agricultural production, resulting in serious agricultural land and food pollution, pesticide residues and heavy metal pollution threatening food safety and Human Health ( Lu et al., 2015 ). Pesticides have an adverse impact on health through drinking water. Comparing pesticide use with health life Expectancy Longitudinal Survey data, it was found that a 10% increase in pesticide use resulted in a 1% increase in the medical disability index over 65 years of age ( Lai, 2017 ). The case of the Musi River in India shows a higher incidence of morbidity in wastewater-irrigated villages than normal-water households. Third, water pollution is related to natural factors. Taking Child Loess Plateau as an example, the concentration of trace elements in water quality is higher than the average world level, and trace elements come from natural weathering and manufacture causes. Poor river water quality is associated with high sodium and salinity hazards ( Xiao et al., 2019 ). The most typical water pollution in the middle part of the loess Plateau is hexavalent chromium pollution, which is caused by the natural environment and human activities. Loess and mudstone are the main sources, and groundwater with high concentrations of hexavalent chromium is also an important factor in surface water pollution (He et al., 2020). Finally, water supply and sewage treatment facilities are also important factors affecting drinking water quality, especially in developing countries. In parallel with China rapid economic growth, industrialization and urbanization, underinvestment in basic water supply and treatment facilities has led to water pollution, increased incidence of infectious and parasitic diseases, and increased exposure to industrial chemicals, heavy metals and algal toxins ( Wu et al., 1999 ). An econometric model predicts the impact of water purification equipment on water quality and therefore human health. When the proportion of household water treated with water purification equipment is reduced from 100% to 90%, the expected health benefits are reduced by up to 96%.. When the risk of pretreatment water quality is high, the decline is even more significant ( Brown and Clasen, 2012 ).
To sum up, water pollution results from both human and natural factors. Various human activities will directly affect water quality, including urbanization, population growth, industrial production, climate change, and other factors ( Halder and Islam, 2015 ) and religious activities ( Dwivedi et al., 2018 ). Improper disposal of solid waste, sand, and gravel is also one reason for decreasing water quality ( Ustaoğlua et al., 2020 ).
Impact of Water Pollution on Human Health
Unsafe water has severe implications for human health. According to UNESCO 2021 World Water Development Report , about 829,000 people die each year from diarrhea caused by unsafe drinking water, sanitation, and hand hygiene, including nearly 300,000 children under the age of five, representing 5.3 percent of all deaths in this age group. Data from Palestine suggest that people who drink municipal water directly are more likely to suffer from diseases such as diarrhea than those who use desalinated and household-filtered drinking water ( Yassin et al., 2006 ). In a comparative study of tap water, purified water, and bottled water, tap water was an essential source of gastrointestinal disease ( Payment et al., 1997 ). Lack of water and sanitation services also increases the incidence of diseases such as cholera, trachoma, schistosomiasis, and helminthiasis. Data from studies in developing countries show a clear relationship between cholera and contaminated water, and household water treatment and storage can reduce cholera ( Gundry et al., 2004 ). In addition to disease, unsafe drinking water, and poor environmental hygiene can lead to gastrointestinal illness, inhibiting nutrient absorption and malnutrition. These effects are especially pronounced for children.
Purpose of This Paper
More than two million people worldwide die each year from diarrhoeal diseases, with poor sanitation and unsafe drinking water being the leading cause of nearly 90% of deaths and affecting children the most (United Nations, 2016). More than 50 kinds of diseases are caused by poor drinking water quality, and 80% of diseases and 50% of child deaths are related to poor drinking water quality in the world. However, water pollution causes diarrhea, skin diseases, malnutrition, and even cancer and other diseases related to water pollution. Therefore, it is necessary to study the impact of water pollution on human health, especially disease heterogeneity, and clarify the importance of clean drinking water, which has important theoretical and practical significance for realizing sustainable development goals. Unfortunately, although many kinds of literature focus on water pollution and a particular disease, there is still a lack of research results that systematically analyze the impact of water pollution on human health and the heterogeneity of diseases. Based on the above background and discussion, this paper focuses on the effect of water pollution on human health and its disease heterogeneity.
Materials and Methods
Search process.
This article uses keywords such as “water,” “water pollution,” “water quality,” “health,” “diarrhea,” “skin disease,” “cancer” and “children” to search Web of Science and Google Scholar include SCI and SSCI indexed papers, research reports, and works from 1990 to 2021.
Inclusion-Exclusion Criteria and Data Extraction Process
The existing literature shows that water pollution and human health are important research topics in health economics, and scholars have conducted in-depth research. As of 30 December 2021, 104 related literatures were searched, including research papers, reviews and conference papers. Then, according to the content relevancy, 19 papers were eliminated, and 85 papers remained. The purpose of this review is to summarize the impact of water pollution on human health and its disease heterogeneity and to explore how to improve human health by improving water pollution control measures.
Information extracted from all included papers included: author, publication date, sample country, study methodology, study purpose, and key findings. All analysis results will be analyzed according to the process in Figure 1 .
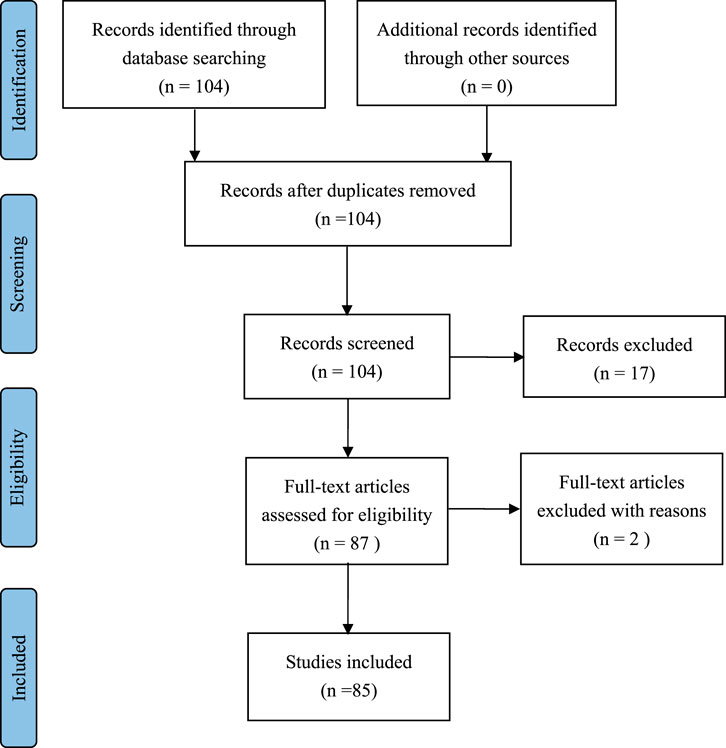
FIGURE 1 . Data extraction process (PRISMA).
The relevant information of the paper is exported to the Excel database through Endnote, and the duplicates are deleted. The results were initially extracted by one researcher and then cross-checked by another researcher to ensure that all data had been filtered and reviewed. If two researchers have different opinions, the two researchers will review together until a final agreement is reached.
Quality Assessment of the Literature
The JBI Critical Appraisal Checklist was used to evaluate the quality of each paper. The JBI (Joanna Briggs Institute) key assessment tool was developed by the JBI Scientific Committee after extensive peer review and is designed for system review. All features of the study that meet the following eight criteria are included in the final summary:1) clear purpose; 2) Complete information of sample variables; 3) Data basis; 4) the validity of data sorting; 5) ethical norms; (6); 7) Effective results; 8) Apply appropriate quantitative methods and state the results clearly. Method quality is evaluated by the Yes/No questions listed in the JBI Key Assessment List. Each analysis paper received 6 out of 8.
The quality of drinking water is an essential factor affecting human health. Poor drinking water quality has led to the occurrence of water-borne diseases. According to the World Health Organization (WHO) survey, 80% of the world’s diseases and 50% of the world’s child deaths are related to poor drinking water quality, and there are more than 50 diseases caused by poor drinking water quality. The quality of drinking water in developing countries is worrying. The negative health effects of water pollution remain the leading cause of morbidity and mortality in developing countries. Different from the existing literature review, this paper mainly studies the impact of water pollution on human health according to the heterogeneity of diseases. We focuses on diarrhea, skin diseases, cancer, child health, etc., and sorts out the main effects of water pollution on human health ( Table 1 ).
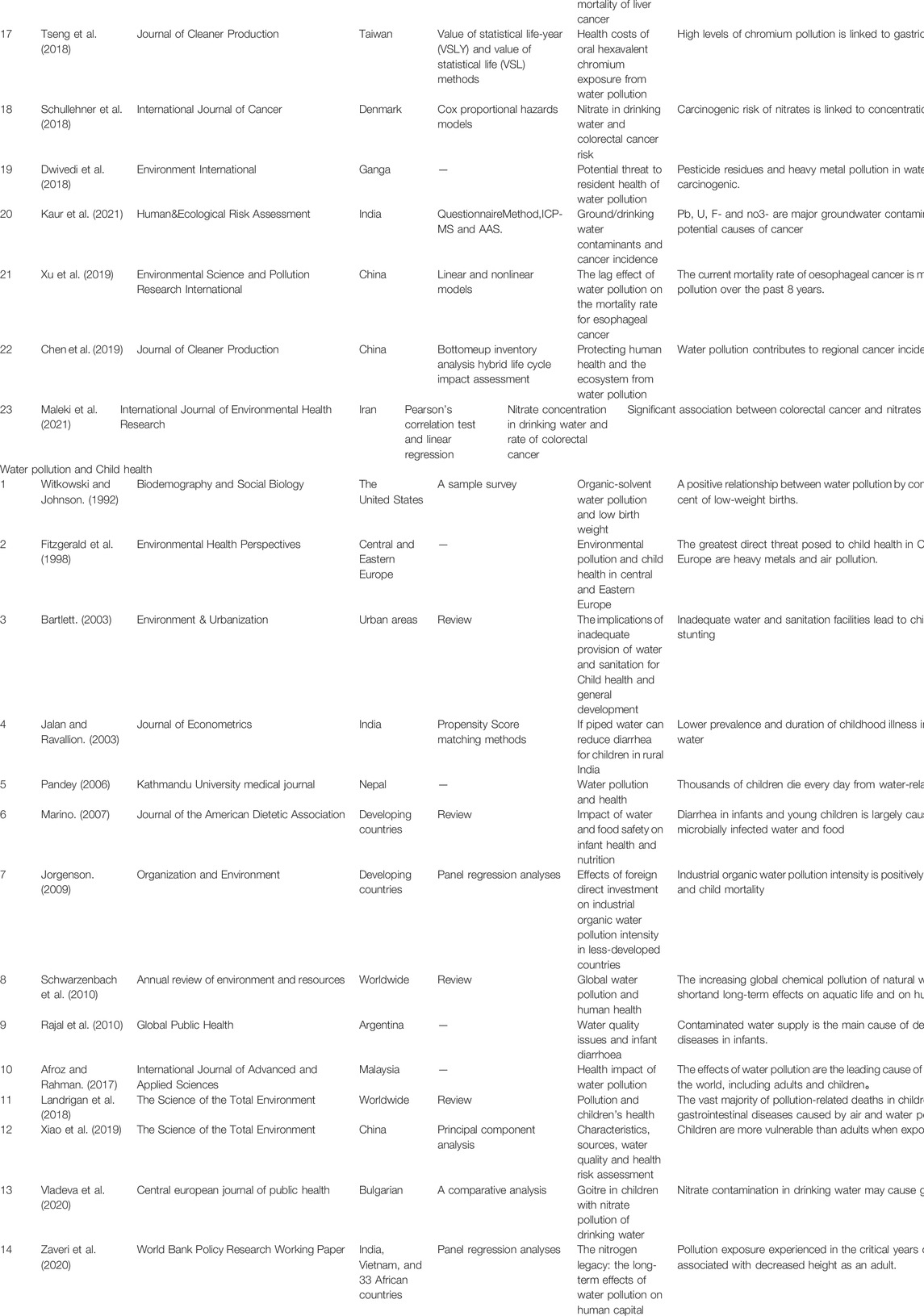
TABLE 1 . Major studies on the relationship between water pollution and health.
Water Pollution and Diarrhea
Diarrhea is a common symptom of gastrointestinal diseases and the most common disease caused by water pollution. Diarrhea is a leading cause of illness and death in young children in low-income countries. Diarrhoeal diseases account for 21% of annual deaths among children under 5 years of age in developing countries ( Waddington et al., 2009 ). Many infectious agents associated with diarrhea are directly related to contaminated water ( Ahmed and Ismail, 2018 ). Parasitic worms present in non-purifying drinking water when is consumed by human beings causes diseases ( Ansari and Akhmatov., 2020 ) . It was found that treated water from water treatment facilities was associated with a lower risk of diarrhea than untreated water for all ages ( Clasen et al., 2015 ). For example, in the southern region of Brazil, a study found that factors significantly associated with an increased risk of mortality from diarrhoea included lack of plumbed water, lack of flush toilets, poor housing conditions, and overcrowded households. Households without access to piped water had a 4.8 times higher risk of infant death from diarrhea than households with access to piped water ( Victora et al., 1988 )
Enteroviruses exist in the aquatic environment. More than 100 pathogenic viruses are excreted in human and animal excreta and spread in the environment through groundwater, estuarine water, seawater, rivers, sewage treatment plants, insufficiently treated water, drinking water, and private wells ( Fong and Lipp., 2005 ). A study in Pakistan showed that coliform contamination was found in some water sources. Improper disposal of sewage and solid waste, excessive use of pesticides and fertilizers, and deteriorating pipeline networks are the main causes of drinking water pollution. The main source of water-borne diseases such as gastroenteritis, dysentery, diarrhea, and viral hepatitis in this area is the water pollution of coliform bacteria ( Khan et al., 2013 ). Therefore, the most important role of water and sanitation health interventions is to hinder the transmission of diarrheal pathogens from the environment to humans ( Waddington et al., 2009 ).
Meta-analyses are the most commonly used method for water quality and diarrhea studies. It was found that improving water supply and sanitation reduced the overall incidence of diarrhea by 26%. Among Malaysian infants, having clean water and sanitation was associated with an 82% reduction in infant mortality, especially among infants who were not breastfed ( Esrey et al., 1991 ). All water quality and sanitation interventions significantly reduced the risk of diarrhoeal disease, and water quality interventions were found to be more effective than previously thought. Multiple interventions (including water, sanitation, and sanitation measures) were not more effective than single-focus interventions ( Fewtrell and Colford., 2005 ). Water quality interventions reduced the risk of diarrhoea in children and reduced the risk of E. coli contamination of stored water ( Arnold and Colford., 2007 ). Interventions to improve water quality are generally effective in preventing diarrhoea in children of all ages and under 5. However, some trials showed significant heterogeneity, which may be due to the research methods and their conditions ( Clasen et al., 2007 ).
Water Pollution and Skin Diseases
Contrary to common sense that swimming is good for health, studies as early as the 1950s found that the overall disease incidence in the swimming group was significantly higher than that in the non-swimming group. The survey shows that the incidence of the disease in people under the age of 10 is about 100% higher than that of people over 10 years old. Skin diseases account for a certain proportion ( Stevenson, 1953 ). A prospective epidemiological study of beach water pollution was conducted in Hong Kong in the summer of 1986–1987. The study found that swimmers on Hong Kong’s coastal beaches were more likely than non-swimmers to complain of systemic ailments such as skin and eyes. And swimming in more polluted beach waters has a much higher risk of contracting skin diseases and other diseases. Swimming-related disease symptom rates correlated with beach cleanliness ( Cheung et al., 1990 ).
A study of arsenic-affected villages in the southern Sindh province of Pakistan emphasized that skin diseases were caused by excessive water quality. By studying the relationship between excessive arsenic in drinking water caused by water pollution and skin diseases (mainly melanosis and keratosis), it was found that compared with people who consumed urban low-arsenic drinking water, the hair of people who consumed high-arsenic drinking water arsenic concentration increased significantly. The level of arsenic in drinking water directly affects the health of local residents, and skin disease is the most common clinical complication of arsenic poisoning. There is a correlation between arsenic concentrations in biological samples (hair and blood) from patients with skin diseases and intake of arsenic-contaminated drinking water ( Kazi et al., 2009 ). Another Bangladesh study showed that many people suffer from scabies due to river pollution ( Hanif et al., 2020 ). Not only that, but water pollution from industry can also cause skin cancer ( Arif et al., 2020 ).
Studies using meta-analysis have shown that exposure to polluted Marine recreational waters can have adverse consequences, including frequent skin discomfort (such as rash or itching). Skin diseases in swimmers may be caused by a variety of pathogenic microorganisms ( Yau et al., 2009 ). People (swimmers and non-swimmers) exposed to waters above threshold levels of bacteria had a higher relative risk of developing skin disease, and levels of bacteria in seawater were highly correlated with skin symptoms.
Studies have also suggested that swimmers are 3.5 times more likely to report skin diseases than non-swimmers. This difference may be a “risk perception bias” at work on swimmers, who are generally aware that such exposure may lead to health effects and are more likely to detect and report skin disorders. It is also possible that swimmers exaggerated their symptoms, reporting conditions that others would not classify as true skin disorders ( Fleisher and Kay. 2006 ).
Water Pollution and Cancer
According to WHO statistics, the number of cancer patients diagnosed in 2020 reached 19.3 million, while the number of deaths from cancer increased to 10 million. Currently, one-fifth of all global fevers will develop cancer during their lifetime. The types and amounts of carcinogens present in drinking water will vary depending on where they enter: contamination of the water source, water treatment processes, or when the water is delivered to users ( Morris, 1995 ).
From the perspective of water sources, arsenic, nitrate, chromium, etc. are highly associated with cancer. Ingestion of arsenic from drinking water can cause skin cancer and kidney and bladder cancer ( Marmot et al., 2007 ). The risk of cancer in the population from arsenic in the United States water supply may be comparable to the risk from tobacco smoke and radon in the home environment. However, individual susceptibility to the carcinogenic effects of arsenic varies ( Smith et al., 1992 ). A high association of arsenic in drinking water with lung cancer was demonstrated in a northern Chilean controlled study involving patients diagnosed with lung cancer and a frequency-matched hospital between 1994 and 1996. Studies have also shown a synergistic effect of smoking and arsenic intake in drinking water in causing lung cancer ( Ferreccio et al., 2000 ). Exposure to high arsenic levels in drinking water was also associated with the development of liver cancer, but this effect was not significant at exposure levels below 0.64 mg/L ( Lin et al., 2013 ).
Nitrates are a broader contaminant that is more closely associated with human cancers, especially colorectal cancer. A study in East Azerbaijan confirmed a significant association between colorectal cancer and nitrate in men, but not in women (Maleki et al., 2021). The carcinogenic risk of nitrates is concentration-dependent. The risk increases significantly when drinking water levels exceed 3.87 mg/L, well below the current drinking water standard of 50 mg/L. Drinking water with nitrate concentrations lower than current drinking water standards also increases the risk of colorectal cancer ( Schullehner et al., 2018 ).
Drinking water with high chromium content will bring high carcinogenicity caused by hexavalent chromium to residents. Drinking water intake of hexavalent chromium experiments showed that hexavalent chromium has the potential to cause human respiratory cancer. ( Zhitkovich, 2011 ). A case from Changhua County, Taiwan also showed that high levels of chromium pollution were associated with gastric cancer incidence ( Tseng et al., 2018 ).
There is a correlation between trihalomethane (THM) levels in drinking water and cancer mortality. Bladder and brain cancers in both men and women and non-Hodgkin’s lymphoma and kidney cancer in men were positively correlated with THM levels, and bladder cancer mortality had the strongest and most consistent association with THM exposure index ( Cantor et al., 1978 ).
From the perspective of water treatment process, carcinogens may be introduced during chlorine treatment, and drinking water is associated with all cancers, urinary cancers and gastrointestinal cancers ( Page et al., 1976 ). Chlorinated byproducts from the use of chlorine in water treatment are associated with an increased risk of bladder and rectal cancer, with perhaps 5,000 cases of bladder and 8,000 cases of rectal cancer occurring each year in the United States (Morris, 1995).
The impact of drinking water pollutants on cancer is complex. Epidemiological studies have shown that drinking water contaminants, such as chlorinated by-products, nitrates, arsenic, and radionuclides, are associated with cancer in humans ( Cantor, 1997 ). Pb, U, F- and no3- are the main groundwater pollutants and one of the potential causes of cancer ( Kaur et al., 2021 ). In addition, many other water pollutants are also considered carcinogenic, including herbicides and pesticides, and fertilizers that contain and release nitrates ( Marmot et al., 2007 ). A case from Hebei, China showed that the contamination of nitrogen compounds in well water was closely related to the use of nitrogen fertilizers in agriculture, and the levels of three nitrogen compounds in well water were significantly positively correlated with esophageal cancer mortality ( Zhang et al., 2003 ).
In addition, due to the time-lag effect, the impact of watershed water pollution on cancer is spatially heterogeneous. The mortality rate of esophageal cancer caused by water pollution is significantly higher downstream than in other regions due to the impact of historical water pollution ( Xu et al., 2019 ). A study based on changes in water quality in the watershed showed that a grade 6 deterioration in water quality resulted in a 9.3% increase in deaths from digestive cancer. ( Ebenstein, 2012 ).
Water Pollution and Child Health
Diarrhea is a common disease in children. Diarrhoeal diseases (including cholera) kill 1.8 million people each year, 90 per cent of them children under the age of five, mostly in developing countries. 88% of diarrhoeal diseases are caused by inadequate water supply, sanitation and hygiene (Team, 2004). A large proportion of these are caused by exposure to microbially infected water and food, and diarrhea in infants and young children can lead to malnutrition and reduced immune resistance, thereby increasing the likelihood of prolonged and recurrent diarrhea ( Marino, 2007 ). Pollution exposure experienced by children during critical periods of development is associated with height loss in adulthood ( Zaveri et al., 2020 ). Diseases directly related to water and sanitation, combined with malnutrition, also lead to other causes of death, such as measles and pneumonia. Child malnutrition and stunting due to inadequate water and sanitation will continue to affect more than one-third of children in the world ( Bartlett, 2003 ). A study from rural India showed that children living in households with tap water had significantly lower disease prevalence and duration ( Jalan and Ravallion, 2003 ).
In conclusion, water pollution is a significant cause of childhood diseases. Air, water, and soil pollution together killed 940,000 children worldwide in 2016, two-thirds of whom were under the age of 5, and the vast majority occurred in low- and middle-income countries ( Landrigan et al., 2018 ). The intensity of industrial organic water pollution is positively correlated with infant mortality and child mortality in less developed countries, and industrial water pollution is an important cause of infant and child mortality in less developed countries ( Jorgenson, 2009 ). In addition, arsenic in drinking water is a potential carcinogenic risk in children (García-Rico et al., 2018). Nitrate contamination in drinking water may cause goiter in children ( Vladeva et al.., 2000 ).
Discussions
This paper reviews the environmental science, health, and medical literature, with a particular focus on epidemiological studies linking water quality, water pollution, and human disease, as well as studies on water-related disease morbidity and mortality. At the same time, special attention is paid to publications from the United Nations and the World Health Organization on water and sanitation health research. The purpose of this paper is to clarify the relationship between water pollution and human health, including: The relationship between water pollution and diarrhea, the mechanism of action, and the research situation of meta-analysis; The relationship between water pollution and skin diseases, pathogenic factors, and meta-analysis research; The relationship between water pollution and cancer, carcinogenic factors, and types of cancer; The relationship between water pollution and Child health, and the major childhood diseases caused.
A study of more than 100 literatures found that although factors such as country, region, age, and gender may have different influences, in general, water pollution has a huge impact on human health. Water pollution is the cause of many human diseases, mainly diarrhoea, skin diseases, cancer and various childhood diseases. The impact of water pollution on different diseases is mainly reflected in the following aspects. Firstly, diarrhea is the most easily caused disease by water pollution, mainly transmitted by enterovirus existing in the aquatic environment. The transmission environment of enterovirus depends on includes groundwater, river, seawater, sewage, drinking water, etc. Therefore, it is necessary to prevent the transmission of enterovirus from the environment to people through drinking water intervention. Secondly, exposure to or use of heavily polluted water is associated with a risk of skin diseases. Excessive bacteria in seawater and heavy metals in drinking water are the main pathogenic factors of skin diseases. Thirdly, water pollution can pose health risks to humans through any of the three links: the source of water, the treatment of water, and the delivery of water. Arsenic, nitrate, chromium, and trihalomethane are major carcinogens in water sources. Carcinogens may be introduced during chlorine treatment from water treatment. The effects of drinking water pollution on cancer are complex, including chlorinated by-products, heavy metals, radionuclides, herbicides and pesticides left in water, etc., Finally, water pollution is an important cause of children’s diseases. Contact with microbiologically infected water can cause diarrhoeal disease in children. Malnutrition and weakened immunity from diarrhoeal diseases can lead to other diseases.
This study systematically analyzed the impact of water pollution on human health and the heterogeneity of diseases from the perspective of different diseases, focusing on a detailed review of the relationship, mechanism and influencing factors of water pollution and diseases. From the point of view of limitations, this paper mainly focuses on the research of environmental science and environmental management, and the research on pathology is less involved. Based on this, future research can strengthen research at medical and pathological levels.
In response to the above research conclusions, countries, especially developing countries, need to adopt corresponding water management policies to reduce the harm caused by water pollution to human health. Firstly, there is a focus on water quality at the point of use, with interventions to improve water quality, including chlorination and safe storage ( Gundry et al., 2004 ), and provision of treated and clean water ( Khan et al., 2013 ). Secondly, in order to reduce the impact of water pollution on skin diseases, countries should conduct epidemiological studies on their own in order to formulate health-friendly bathing water quality standards suitable for their specific conditions ( Cheung et al., 1990 ). Thirdly, in order to reduce the cancer caused by water pollution, the whole-process supervision of water quality should be strengthened, that is, the purity of water sources, the scientific nature of water treatment and the effectiveness of drinking water monitoring. Fourthly, each society should prevent and control source pollution from production, consumption, and transportation ( Landrigan et al., 2018 ). Fifthly, health education is widely carried out. Introduce environmental education, educate residents on sanitary water through newspapers, magazines, television, Internet and other media, and enhance public health awareness. Train farmers to avoid overuse of agricultural chemicals that contaminate drinking water.
Author Contributions
Conceptualization, XX|; methodology, LL; data curation, HY; writing and editing, LL; project administration, XX|.
This article is a phased achievement of The National Social Science Fund of China: Research on the blocking mechanism of the critical poor households returning to poverty due to illness, No: 20BJY057.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Afroz, R., Rahman, A., and Rahman, A. (2017). Health Impact of River Water Pollution in Malaysia. Int. J. Adv. Appl. Sci. 4 (5), 78–85. doi:10.21833/ijaas.2017.05.014
CrossRef Full Text | Google Scholar
Ahmed, S., and Ismail, S. (2018). Water Pollution and its Sources, Effects and Management: a Case Study of Delhi. Int. J. Curr. Adv. Res. 7 (2), 10436–10442. doi:10.24327/ijcar.2018.10442.1768
Ansari, Z. Z., and Akhmatov, S. V. (2020). Impacts of Water Pollution on Human Health: A Case Study of Delhi .
Google Scholar
Arif, A., Malik, M. F., Liaqat, S., Aslam, A., Mumtaz, K., and Afzal, A. (2020). 3. Water Pollution and Industries. Pure Appl. Biol. (PAB) 9 (4), 2214–2224. doi:10.19045/bspab.2020.90237
Arnold, B. F., and Colford, J. M. (2007). Treating Water with Chlorine at Point-Of-Use to Improve Water Quality and Reduce Child Diarrhea in Developing Countries: a Systematic Review and Meta-Analysis. Am. J. Trop. Med. Hyg. 76 (2), 354–364. doi:10.4269/ajtmh.2007.76.354
PubMed Abstract | CrossRef Full Text | Google Scholar
Bartlett, S. (2003). Water, Sanitation and Urban Children: the Need to Go beyond “Improved” Provision. Environ. Urbanization 15 (2), 57–70. doi:10.1177/095624780301500220
Bessong, P. O., Odiyo, J. O., Musekene, J. N., and Tessema, A. (2009). Spatial Distribution of Diarrhoea and Microbial Quality of Domestic Water during an Outbreak of Diarrhoea in the Tshikuwi Community in Venda, South Africa. J. Health Popul. Nutr. 27 (5), 652–659. doi:10.3329/jhpn.v27i5.3642
Boldo, E., MartÍN-Olmedo, P., Medina, S., Pirard, P., Mouly, D., and Beaudeau, P. (2006). Towards the Quantification of Health Impacts Caused by Drinking-Water Pollution in European Countries. Epidemiology 17 (6), S447. doi:10.1097/00001648-200611001-01198
Brown, J., and Clasen, T. (2012). High Adherence Is Necessary to Realize Health Gains from Water Quality Interventions. PLoS ONE 7 (5), e36735–9. doi:10.1371/journal.pone.0036735
Cantor, K. P., Hoover, R., Mason, T. J., and McCabe, L. J. (1978). Associations of Cancer Mortality with Halomethanes in Drinking Water. J. Natl. Cancer Inst. 61 (4), 979
PubMed Abstract | Google Scholar
Cantor, K. P. (1997). Drinking Water and Cancer. Cancer Causes Control CCC 8 (3), 292–308. doi:10.1023/a:1018444902486
Chen, B., Wang, M., Duan, M., Ma, X., Hong, J., Xie, F., et al. (2019). In Search of Key: Protecting Human Health and the Ecosystem from Water Pollution in China. J. Clean. Prod. 228, 101–111. doi:10.1016/j.jclepro.2019.04.228
Cheung, W. H. S., Chang, K. C. K., Hung, R. P. S., and Kleevens, J. W. L. (1990). Health Effects of Beach Water Pollution in Hong Kong. Epidemiol. Infect. 105 (1), 139–162. doi:10.1017/s0950268800047737
Cheung, W. H. S., Hung, R. P. S., Chang, K. C. K., and Kleevens, J. W. L. (1991). Epidemiological Study of Beach Water Pollution and Health-Related Bathing Water Standards in Hong Kong. Water Sci. Technol. 23 (1-3), 243–252. doi:10.2166/wst.1991.0422
Chowdhary, P., Bharagava, R. N., Mishra, S., and Khan, N. (2020). Role of Industries in Water Scarcity and its Adverse Effects on Environment and Human Health. Environ. Concerns Sustain. Dev. , 235–256. doi:10.1007/978-981-13-5889-0_12
Clasen, T. F., Alexander, K. T., Sinclair, D., Boisson, S., Peletz, R., Chang, H. H., et al. (2015). Interventions to Improve Water Quality for Preventing Diarrhoea. Cochrane Database Syst. Rev. 10, CD004794. doi:10.1002/14651858.CD004794.pub3
Clasen, T., Schmidt, W.-P., Rabie, T., Roberts, I., and Cairncross, S. (2007). Interventions to Improve Water Quality for Preventing Diarrhoea: Systematic Review and Meta-Analysis. Bmj 334 (7597), 782. doi:10.1136/bmj.39118.489931.be
Conroy, R. M., Elmore-Meegan, M., Joyce, T., McGuigan, K. G., and Barnes, J. (1996). Solar Disinfection of Drinking Water and Diarrhoea in Maasai Children: a Controlled Field Trial. Lancet 348 (9043), 1695–1697. doi:10.1016/s0140-6736(96)02309-4
Dasgupta, P. (2004). Valuing Health Damages from Water Pollution in Urban Delhi, India: a Health Production Function Approach. Envir. Dev. Econ. 9 (1), 83–106. doi:10.1017/s1355770x03001098
Dwivedi, S., Mishra, S., and Tripathi, R. D. (2018). Ganga Water Pollution: A Potential Health Threat to Inhabitants of Ganga Basin. Environ. Int. 117, 327–338. doi:10.1016/j.envint.2018.05.015
Ebenstein, A. (2012). The Consequences of Industrialization: Evidence from Water Pollution and Digestive Cancers in China. Rev. Econ. Statistics 94 (1), 186–201. doi:10.1162/rest_a_00150
El-Kowrany, S. I., El- Zamarany, E. A., El-Nouby, K. A., El-Mehy, D. A., Abo Ali, E. A., and Othman, A. A. (2016). Water Pollution in the Middle Nile Delta, Egypt: an Environmental Study. J. Adv. Res. 7 (5), 781–794. doi:10.1016/j.jare.2015.11.005
Enrique Biagini, R. (1975). Chronic Arsenic Water Pollution in the Republic of Argentina. Med. Cutan. Ibero Lat. Am. 3 (6), 423
Esrey, S. A., Potash, J. B., Roberts, L., and Shiff, C. (1991). Effects of Improved Water Supply and Sanitation on Ascariasis, Diarrhoea, Dracunculiasis, Hookworm Infection, Schistosomiasis, and Trachoma. Bull. World Health Organ 69 (5), 609
Ferreccio, C., González, C., Milosavjlevic, V., Marshall, G., Sancha, A. M., and Smith, A. H. (2000). Lung Cancer and Arsenic Concentrations in Drinking Water in Chile. Epidemiology 11 (6), 673–679. doi:10.1097/00001648-200011000-00010
Fewtrell, L., and Colford, J. M. (2005). Water, Sanitation and Hygiene in Developing Countries: Interventions and Diarrhoea-A Review. Water Sci. Technol. A J. Int. Assoc. Water Pollut. Res. 52 (8), 133–142. doi:10.2166/wst.2005.0244
Fitzgerald, E. F., Schell, L. M., Marshall, E. G., Carpenter, D. O., Suk, W. A., and Zejda, J. E. (1998). Environmental Pollution and Child Health in Central and Eastern Europe. Environ. Health Perspect. 106 (6), 307–311. doi:10.1289/ehp.98106307
Fleisher, J. M., and Kay, D. (2006). Risk Perception Bias, Self-Reporting of Illness, and the Validity of Reported Results in an Epidemiologic Study of Recreational Water Associated Illnesses. Mar. Pollut. Bull. 52 (3), 264–268. doi:10.1016/j.marpolbul.2005.08.019
Fong, T.-T., and Lipp, E. K. (2005). Enteric Viruses of Humans and Animals in Aquatic Environments: Health Risks, Detection, and Potential Water Quality Assessment Tools. Microbiol. Mol. Biol. Rev. 69 (2), 357–371. doi:10.1128/mmbr.69.2.357-371.2005
Froom, P. (2009). Water Pollution and Cancer in Israeli Navy Divers. Int. J. Occup. Environ. Health 15 (3), 326–328. doi:10.1179/oeh.2009.15.3.326
Gundry, S., Wright, J., and Conroy, R. (2004). A Systematic Review of the Health Outcomes Related to Household Water Quality in Developing Countries. J. water health 2 (1), 1–13. doi:10.2166/wh.2004.0001
Halder, J., Islam, N., and Islam, N. (2015). Water Pollution and its Impact on the Human Health. Eh 2 (1), 36–46. doi:10.15764/eh.2015.01005
Hanif, M., Miah, R., Islam, M., and Marzia, S. (2020). Impact of Kapotaksha River Water Pollution on Human Health and Environment. Prog. Agric. 31 (1), 1–9. doi:10.3329/pa.v31i1.48300
Haseena, M., Malik, M. F., Javed, A., Arshad, S., Asif, N., Zulfiqar, S., et al. (2017). Water Pollution and Human Health. Environ. Risk Assess. Remediat. 1 (3), 20. doi:10.4066/2529-8046.100020
Henry, F. J., Huttly, S. R. A., Patwary, Y., and Aziz, K. M. A. (1990). Environmental Sanitation, Food and Water Contamination and Diarrhoea in Rural Bangladesh. Epidemiol. Infect. 104 (2), 253–259. doi:10.1017/s0950268800059422
Jalan, J., and Ravallion, M. (2003). Does Piped Water Reduce Diarrhea for Children in Rural India? J. Econ. 112 (1), 153–173. doi:10.1016/s0304-4076(02)00158-6
Jensen, P. K., Jayasinghe, G., Hoek, W., Cairncross, S., and Dalsgaard, A. (2004). Is There an Association between Bacteriological Drinking Water Quality and Childhood Diarrhoea in Developing Countries? Trop. Med. Int. Health 9 (11), 1210–1215. doi:10.1111/j.1365-3156.2004.01329.x
Jorgenson, A. K. (2009). Foreign Direct Investment and the Environment, the Mitigating Influence of Institutional and Civil Society Factors, and Relationships between Industrial Pollution and Human Health. Organ. Environ. 22 (2), 135–157. doi:10.1177/1086026609338163
Kaur, G., Kumar, R., Mittal, S., Sahoo, P. K., and Vaid, U. (2021). Ground/drinking Water Contaminants and Cancer Incidence: A Case Study of Rural Areas of South West Punjab, India. Hum. Ecol. Risk Assess. Int. J. 27 (1), 205–226. doi:10.1080/10807039.2019.1705145
Kazi, T. G., Arain, M. B., Baig, J. A., Jamali, M. K., Afridi, H. I., Jalbani, N., et al. (2009). The Correlation of Arsenic Levels in Drinking Water with the Biological Samples of Skin Disorders. Sci. Total Environ. 407 (3), 1019–1026. doi:10.1016/j.scitotenv.2008.10.013
Khan, S., Shahnaz, M., Jehan, N., Rehman, S., Shah, M. T., and Din, I. (2013). Drinking Water Quality and Human Health Risk in Charsadda District, Pakistan. J. Clean. Prod. 60, 93–101. doi:10.1016/j.jclepro.2012.02.016
Kochhar, N., Gill, G. S., Tuli, N., Dadwal, V., and Balaram, V. (2007). Chemical Quality of Ground Water in Relation to Incidence of Cancer in Parts of SW Punjab, India. Asian J. Water, Environ. Pollut. 4 (2), 107 doi:10.1086/114154
Kumar, S., Meena, H. M., and Verma, K. (2017). Water Pollution in India: its Impact on the Human Health: Causes and Remedies. Int. J. Appl. Environ. Sci. 12 (2), 275
Lai, W. (2017). Pesticide Use and Health Outcomes: Evidence from Agricultural Water Pollution in China. J. Environ. Econ. Manag. 86, 93–120. doi:10.1016/j.jeem.2017.05.006
Landrigan, P. J., Fuller, R., Fisher, S., Suk, W. A., Sly, P., Chiles, T. C., et al. (2018). Pollution and Children's Health. Sci. Total Environ. 650 (Pt 2), 2389–2394. doi:10.1016/j.scitotenv.2018.09.375
Lin, H.-J., Sung, T.-I., Chen, C.-Y., and Guo, H.-R. (2013). Arsenic Levels in Drinking Water and Mortality of Liver Cancer in Taiwan. J. Hazard. Mater. 262, 1132–1138. doi:10.1016/j.jhazmat.2012.12.049
Lu, Y., Song, S., Wang, R., Liu, Z., Meng, J., Sweetman, A. J., et al. (2015). Impacts of Soil and Water Pollution on Food Safety and Health Risks in China. Environ. Int. 77, 5–15. doi:10.1016/j.envint.2014.12.010
Marino, D. D. (2007). Water and Food Safety in the Developing World: Global Implications for Health and Nutrition of Infants and Young Children. J. Am. Dietetic Assoc. 107 (11), 1930–1934. doi:10.1016/j.jada.2007.08.013
Marmot, M., Atinmo, T., Byers, T., Chen, J., and Zeisel, S. H. (2007). Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. Nutr. Bull.
Marr, A., and Dasgupta, N. (2009). Industrial Water Pollution in Dhaka, Bangladesh: Strategies and Incentives for Pollution Control in Small and Medium Enterprises. Int. J. Interdiscip. Soc. Sci. Annu. Rev. 3 (11), 97–108. doi:10.18848/1833-1882/cgp/v03i11/52752
Morris, R. D. (1995). Drinking Water and Cancer. Environ. Health Perspect. 103, 225. doi:10.2307/3432315
Moss, B. (2008). Water Pollution by Agriculture. Phil. Trans. R. Soc. B 363 (1491), 659–666. doi:10.1098/rstb.2007.2176
Page, T., Harris, R. H., and Epstein, S. S. (1976). Drinking Water and Cancer Mortality in Louisiana. Science 193 (4247), 55–57. doi:10.1126/science.935854
Pandey, S. (2006). Water Pollution and Health. Kathmandu Univ. Med. J. (KUMJ) 4 (1), 128. doi:10.1016/j.crvi.2013.04.013
Parris, K. (2011). Impact of Agriculture on Water Pollution in OECD Countries: Recent Trends and Future Prospects. Int. J. Water Resour. Dev. 27 (1), 33–52. doi:10.1080/07900627.2010.531898
Payment, P., Siemiatycki, J., Richardson, L., Renaud, G., Franco, E., and Prevost, M. (1997). A Prospective Epidemiological Study of Gastrointestinal Health Effects Due to the Consumption of Drinking Water. Int. J. Environ. Health Res. 7 (1), 5–31. doi:10.1080/09603129773977
Rabbani, M., Chowdhury, M., and Khan, N. A. (2010). Impacts of Industrial Pollution on Human Health: Empirical Evidences from an Industrial Hotspot (Kaliakoir) in Bangladesh. Asian J. Water, Environ. Pollut. 7 (1), 27
Rajal, V. B., Cruz, C., and Last, J. A. (2010). Water Quality Issues and Infant Diarrhoea in a South American Province. Glob. Public Health 5 (4), 348–363. doi:10.1080/17441690802447267
Rampen, F. H. J., Nelemans, P. J., and Verbeek, A. L. (1992). Is Water Pollution a Cause of Cutaneous Melanoma? Epidemiology 3, 263–265. doi:10.1097/00001648-199205000-00013
Royal Commission for Environmental Pollution 1979 Seventh Report. Agriculture and Pollution . London, UK: H.M.S.O .
Rusiñol, M., Fernandez-Cassi, X., Timoneda, N., Carratalà, A., and Abril, J. F. (2015). Evidence of Viral Dissemination and Seasonality in a Mediterranean River Catchment: Implications for Water Pollution Management. J. Environ. Manag. 159, 58–67. doi:10.1016/j.jenvman.2015.05.019
Schullehner, J., Hansen, B., Thygesen, M., Pedersen, C. B., and Sigsgaard, T. (2018). Nitrate in Drinking Water and Colorectal Cancer Risk: A Nationwide Population-Based Cohort Study. Int. J. Cancer 143 (1), 73–79. doi:10.1002/ijc.31306
Schwarzenbach, R. P., Egli, T., Hofstetter, T. B., Von Gunten, U., and Wehrli, B. (2010). Global Water Pollution and Human Health. Annu. Rev. Environ. Resour. 35, 109–136. doi:10.1146/annurev-environ-100809-125342
Sliman, N. A. (1978). Outbreak of Guillain-Barre Syndrome Associated with Water Pollution. Bmj 1 (6115), 751–752. doi:10.1136/bmj.1.6115.751
Smith, A. H., Hopenhayn-Rich, C., Bates, M. N., Goeden, H. M., Hertz-Picciotto, I., Duggan, H. M., et al. (1992). Cancer Risks from Arsenic in Drinking Water. Environ. Health Perspect. 97, 259–267. doi:10.1289/ehp.9297259
Stephens, J. K. (2002). Deterioration of Stored Domestic Water Quality and Diarrhoea in Zenu . University of Ghana .
Stevenson, A. H. (1953). Studies of Bathing Water Quality and Health. Am. J. Public Health Nations Health 43 (5 Pt 1), 529–538. doi:10.2105/ajph.43.5_pt_1.529
Team, S. H. (2004). Water, Sanitation and Hygiene Links to Health: Facts and Figures . World Health Organization .
Tondel, M., Rahman, M., Magnuson, A., Chowdhury, I. A., Faruquee, M. H., and Ahmad, S. A. (1999). The Relationship of Arsenic Levels in Drinking Water and the Prevalence Rate of Skin Lesions in Bangladesh. Environ. health Perspect. 107 (9), 727–729. doi:10.1289/ehp.99107727
Tseng, C.-H., Lei, C., and Chen, Y.-C. (2018). Evaluating the Health Costs of Oral Hexavalent Chromium Exposure from Water Pollution: A Case Study in Taiwan. J. Clean. Prod. 172, 819–826. doi:10.1016/j.jclepro.2017.10.177
Ustaoğlu, F., Tepe, Y., Taş, B., and Pag, N. (2020). Assessment of Stream Quality and Health Risk in a Subtropical Turkey River System: A Combined Approach Using Statistical Analysis and Water Quality Index. Ecol. Indic. , 113. doi:10.1016/j.ecolind.2019.105815
Vartiainen, T., Pukkala, E., Rienoja, T., Strandman, T., and Kaksonen, K. (1993). Population Exposure to Tri- and Tetrachloroethene and Cancer Risk: Two Cases of Drinking Water Pollution. Chemosphere 27 (7), 1171–1181. doi:10.1016/0045-6535(93)90165-2
Victora, C. G., Smith, P. G., Vaughan, J. P., Nobre, L. C., Lombard, C., Teixeira, A. M. B., et al. (1988). Water Supply, Sanitation and Housing in Relation to the Risk of Infant Mortality from Diarrhoea. Int. J. Epidemiol. 17 (3), 651–654. doi:10.1093/ije/17.3.651
Vladeva, S., Gatseva, P., and Gopina, G. (2000). Comparative Analysis of Results from Studies of Goitre in Children from Bulgarian Villages with Nitrate Pollution of Drinking Water in 1995 and 1998. Cent. Eur. J. Public Health 8 (3), 179
Waddington, H., Snilstveit, B., White, H., and Fewtrell, L. (2009). Water, Sanitation and Hygiene Interventions to Combat Childhood Diarrhoea in Developing Countries . New Delhi India Global Development Network International Initiative for Impact Evaluation Aug .
Witkowski, K. M., and Johnson, N. E. (1992). Organic-solvent Water Pollution and Low Birth Weight in Michigan. Soc. Biol. 39 (1-2), 45–54. doi:10.1080/19485565.1992.9988803
Wu, C., Maurer, C., Wang, Y., Xue, S., and Davis, D. L. (1999). Water Pollution and Human Health in China. Environ. Health Perspect. 107 (4), 251–256. doi:10.1289/ehp.99107251
Wu, H., Gai, Z., Guo, Y., Li, Y., Hao, Y., and Lu, Z. N. (2020). Does Environmental Pollution Inhibit Urbanization in China? A New Perspective through Residents' Medical and Health Costs. Environ. Res. 182 (Mar.), 109128–109128.9. doi:10.1016/j.envres.2020.109128
Xiao, J., Wang, L., Deng, L., and Jin, Z. (2019). Characteristics, Sources, Water Quality and Health Risk Assessment of Trace Elements in River Water and Well Water in the Chinese Loess Plateau. Sci. Total Environ. 650 (Pt 2), 2004–2012. doi:10.1016/j.scitotenv.2018.09.322
Xu, C., Xing, D., Wang, J., and Xiao, G. (2019). The Lag Effect of Water Pollution on the Mortality Rate for Esophageal Cancer in a Rapidly Industrialized Region in China. Environ. Sci. Pollut. Res. 26 (32), 32852–32858. doi:10.1007/s11356-019-06408-z
Xu, X., Wang, Q., and Li, C. (2022b). The Impact of Dependency Burden on Urban Household Health Expenditure and its Regional Heterogeneity in China: Based on Quantile Regression Method. Front. Public Health 10, 876088. doi:10.3389/fpubh.2022.876088
Xu, X., Yang, H., and Li, C. (2022a). Theoretical Model and Actual Characteristics of Air Pollution Affecting Health Cost: A Review. Ijerph 19, 3532. doi:10.3390/ijerph19063532
Yassin, M. M., Amr, S. S. A., and Al-Najar, H. M. (2006). Assessment of Microbiological Water Quality and its Relation to Human Health in Gaza Governorate, Gaza Strip. Public Health 120 (12), 1177. doi:10.1016/j.puhe.2006.07.026
Yau, V., Wade, T. J., de Wilde, C. K., and Colford, J. M. (2009). Skin-related Symptoms Following Exposure to Recreational Water: a Systematic Review and Meta-Analysis. Water Expo. Health 1 (2), 79–103. doi:10.1007/s12403-009-0012-9
Zaveri, E. D., Russ, J. D., Desbureaux, S. G., Damania, R., Rodella, A. S., and Ribeiro Paiva De Souza, G. (20203). The Nitrogen Legacy: The Long-Term Effects of Water Pollution on Human Capital . World Bank Policy Research Working Paper .
Zhang, X.-L., Bing, Z., Xing, Z., Chen, Z.-F., Zhang, J.-Z., Liang, S.-Y., et al. (2003). Research and Control of Well Water Pollution in High Esophageal Cancer Areas. Wjg 9 (6), 1187–1190. doi:10.3748/wjg.v9.i6.1187
Zhitkovich, A. (2011). Chromium in Drinking Water: Sources, Metabolism, and Cancer Risks. Chem. Res. Toxicol. 24 (10), 1617–1629. doi:10.1021/tx200251t
Keywords: water pollution, human health, disease heterogeneity, water intervention, health cost
Citation: Lin L, Yang H and Xu X (2022) Effects of Water Pollution on Human Health and Disease Heterogeneity: A Review. Front. Environ. Sci. 10:880246. doi: 10.3389/fenvs.2022.880246
Received: 21 February 2022; Accepted: 09 June 2022; Published: 30 June 2022.
Reviewed by:
Copyright © 2022 Lin, Yang and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaocang Xu, [email protected]
This article is part of the Research Topic
Bioaerosol Emission Characteristics and the Epidemiological, Occupational, and Public Health Risk Assessment of Waste and Wastewater Management

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
JavaScript appears to be disabled on this computer. Please click here to see any active alerts .
Research on Health Effects from Air Pollution
Decades of research have shown that air pollutants such as ozone and particulate matter (PM) increase the amount and seriousness of lung and heart disease and other health problems. More investigation is needed to further understand the role poor air quality plays in causing detrimental effects to health and increased disease, especially in vulnerable populations. Children, the elderly, and people living in areas with high levels of air pollution are especially susceptible.
Results from these investigations are used to support the nation's air quality standards under the Clean Air Act and contribute to improvements in public health.
On this page:
Health Effects of Air Pollutants on Vulnerable Populations
Long-term and short-term effects from exposure to air pollutants.
- Multipollutant Exposures and Changes in Environmental Conditions
- Leveraging Big Data for Innovations in Health Science
Health Effects of Wildfire Smoke
Public health intervention and communications strategies, integrated science assessments for air pollutants.

Research has shown that some people are more susceptible than others to air pollutants. These groups include children, pregnant women, older adults, and individuals with pre-existing heart and lung disease. People in low socioeconomic neighborhoods and communities may be more vulnerable to air pollution because of many factors. Proximity to industrial sources of air pollution, underlying health problems, poor nutrition, stress, and other factors can contribute to increased health impacts in these communities.
There is a need for greater understanding of the factors that may influence whether a population or age group is at increased risk of health effects from air pollution. In addition, advances to analytical approaches used to study the health effects from air pollution will improve exposure estimates for healthy and at-risk groups.
The research by EPA scientists and others inform the required reviews of the primary National Ambient Air Quality Standards (NAAQS), which is done with the development of Integrated Science Assessments (ISAs). These ISAs are mandated by Congress every five years to assess the current state of the science on criteria air pollutants and determine if the standards provide adequate protection to public health.
Research is focused on addressing four areas:
- Identifying and characterizing whether there are key reproductive factors and critical stages of development that are impacted by air pollution exposures;
- Determining the role of acute and chronic sociodemographic factors in air pollution health disparities;
- Understanding how diet modifies responses to air pollution;
- Evaluating long-term lifestyle and chronic disease effects on air pollution-induced respiratory and cardiovascular responses
A multi-disciplinary team of investigators is coordinating epidemiological, human observational, and basic toxicological research to assess the effects of air pollution in at-risk populations and develop strategies to protect these populations, particularly those with pre-existing disease. The results from these products will improve risk assessments by clarifying the role of modifying factors such as psychosocial stress (e.g. noise) and diet, and determining the impact of individual susceptibility on the relationship between air pollutant exposures and health.
Related Links
- Healthy Heart Research
- Integrated Science Assessments
- Criteria Air Pollutants

People can experience exposure to varying concentrations of air pollution. Poor air quality can impact individuals for a short period of time during the day, or more frequently during a given day. Exposure to pollutants can also occur over multiple days, weeks or months due to seasonal air pollution, such as increased ozone during the summer or particulate matter from woodstoves during the winter.
The health impact of air pollution exposure depends on the duration and concentrations, and the health status of the affected populations. Studies are needed to increase knowledge of the exposure duration and the possible cumulative increase in risk.
The research is focused on three main areas:
- Short-term peak exposures, such as wildfires, traffic-related sources, or other episodic events;
- Intermittent and cumulative exposures;
- Mechanisms underlying the exposure risks
Researchers are evaluating the health responses of intermittent multiple days versus one-day air pollution exposure in controlled human exposure, animal, and in vitro models and associated cellular and molecular mechanisms. They are employing population-based models and electronic health records to assess the health effects of short-term and long-term exposures and identifying populations at greatest risk of health effects. The work is improving our understanding of the possible cumulative effects of multiple short-term peak exposures and the relationship of these exposures to longer-term exposures and risks.
Multipollutant Exposures and Changes in Environmental Conditions

EPA research is providing information to understand how individuals may respond to two or more pollutants or mixtures and how environmental conditions may impact air quality. While risk estimates for exposure to individual criteria air pollutants such as PM and ozone are well established, the acute and cumulative effects of combinations of pollutants is not well understood. In addition, research is needed to determine how changes in the environment affect both pollutant formation and subsequent responsiveness to exposures in healthy and susceptible individuals.
The research is focused on three specific questions:
- What is the role of temperature and photochemical aging on the health impact of wildfire smoke and air pollution mixtures?
- What is the effect of changing environmental conditions (i.e., temperature and humidity) on responsiveness to air pollution?
- Does prior pollutant exposure modify responsiveness to subsequent exposures?
The integrated, multi-disciplinary research includes:
- Epidemiologic analyses of environmental influences on morbidity and mortality in populations,
- Simulations of changing environmental conditions in multi-pollutant formation in atmospheric chamber studies coupled with clinical and toxicological assessments in healthy and at-risk populations,
- Evaluation of pre-exposure as a modifying effect on subsequent exposures
The results are revealing how changes in environmental conditions affect pollutant formation and subsequent health impact in at-risk populations. The research findings are informing EPA’s Integrated Science Assessments for criteria air pollutants and assisting with future regulatory decisions on the National Ambient Air Quality Standards (NAAQS).
Leveraging Big Data for Innovations in Health Science

EPA is at the cutting edge of health science, using electronic health records, novel data systems, tissue-like advanced cellular models, molecular approaches, and animal models to evaluate the health impacts of air pollution. Researchers are using these powerful new techniques to identify factors that may increase sensitivity and vulnerability to air pollution effects.
The research is building capacity for future risk assessment and regulatory analyses that go beyond traditional lines of evidence to more clearly define populations and lifestages at increased risk of health effects from air pollution.
To continue to protect public health from poor air quality, researchers must consider new epidemiological, toxicological and clinical approaches to understand the health risks of poor air quality and the biological mechanisms responsible for these risks. At the center of these new research approaches is an explosion of data availability and methodological approaches for handling large clinical and molecular datasets, also known as "big data."
While data of increasing size, depth, and complexity have accelerated research for many industries and scientific fields, big data is sometimes less recognized for the impacts it is having on environmental health studies. Increasingly, researchers are able to examine vulnerable populations with unprecedented precision and detail while also evaluating hundreds of thousands of molecular biomarkers in order to understand biological mechanisms associated with exposure.

Larger and more intense wildfires are creating the potential for greater smoke production and chronic exposures in the United States, particularly in the West. Wildfires increase air pollution in surrounding areas and can affect regional air quality.
The health effects of wildfire smoke can range from eye and respiratory tract irritation to more serious disorders, including reduced lung function, exacerbation of asthma and heart failure, and premature death. Children, pregnant women, and the elderly are especially vulnerable to smoke exposure. Emissions from wildfires are known to cause increased visits to hospitals and clinics by those exposed to smoke.
It is important to more fully understand the human health effects associated with short- and long-term exposures to smoke from wildfires as well as prescribed fires, together referred to as wildland fires. EPA is conducting research to advance understanding of the health effects from different types of fires as well as combustion phases. Researchers want to know:
- What is the full extent of health effects from smoke exposure?
- Who is most at risk?
- Are there differences in health effects from different wildfire fuel types or combustion phases (burning versus flaming)?
- What strategies and approaches are most effective in protecting public health?
- What are the environmental, social and economic impacts of wildfire emissions?
- Wildland Fire Research
- Smoke-Ready Toolbox for Wildfires
- Smoke Sense Project and App

Many communities throughout the United States face challenges in providing advice to residents about how best to protect their health when they are exposed to elevated concentrations of air pollutants from motor vehicle and industrial emissions and other sources of combustion, including wildland fire smoke.
Researchers are studying intervention strategies to reduce the health impacts from exposure to air pollution as well as ways to effectively communicate these health risks. To translate the science for use in public health communication and community empowerment, EPA is collaborating with other federal agencies, such as the Centers for Disease Control and Prevention (CDC) and the National Heart, Lung, and Blood Institute (NHLBI), and state and local agencies and tribes. The objectives are to identify ways to lower air pollution exposure or mitigate the biological responses at individual, community or ecosystem levels, and ultimately evaluate whether such interventions have benefits as measured by indicators of health, well-being or economics.
Studies are evaluating the interactions between behavior and social and economic factors to more thoroughly understand how these factors may influence health and well-being outcomes, which can inform effective and consistent health risk messaging.
- Healthy Heart Initiative and Research

EPA sets National Ambient Air Quality Standards (NAAQS) for six principal criteria air pollutants —nitrogen oxides, sulfur oxides, particulate matter, carbon monoxide, ozone and lead—all of which have been shown to be harmful to public health and the environment.
The Agency’s Integrated Science Assessments (ISAs) form the scientific foundation for the review of the NAAQS standards by providing the primary (human health-based) assessments and secondary (welfare-based, e.g. ecology, visibility, materials) assessments. The ISAs are assessments of the state of the science on the criteria pollutants. They are conducted as mandated under the Clean Air Act.
- Air Research Home
- Air Monitoring & Emissions
- Air Quality Modeling
- Wildland Fires
- Health Effects from Air Pollution
- Air & Energy
- Outreach, Tools & Resources

We apologize for the inconvenience...
To ensure we keep this website safe, please can you confirm you are a human by ticking the box below.
If you are unable to complete the above request please contact us using the below link, providing a screenshot of your experience.
https://ioppublishing.org/contacts/

IMAGES
COMMENTS
Short-term and long-term adverse effects on human health are observed. VOCs are responsible for indoor air smells. Short-term exposure is found to cause irritation of eyes, nose, throat, and mucosal membranes, while those of long duration exposure include toxic reactions ( 92 ).
Integrated Pollution Control (IPC) was a major innovation in environmental law. Introduced as part of the UK Environmental Protection Act 1990 (EPA 1990), the organising idea of IPC is a holistic ...
Air pollution is high on the global agenda and is widely recognised as a threat to both public health and economic progress. The World Health Organization (WHO) estimates that 4.2 million deaths ...
The Lancet Commission on pollution and health reported that pollution was responsible for 9 million premature deaths in 2015, making it the world's largest environmental risk factor for disease and premature death. We have now updated this estimate using data from the Global Burden of Diseases, Injuriaes, and Risk Factors Study 2019. We find that pollution remains responsible for approximately ...
Moreover, air pollution seems to have various malign health effects in early human life, such as respiratory, cardiovascular, mental, and perinatal disorders ( 3 ), leading to infant mortality or chronic disease in adult age ( 6 ). National reports have mentioned the increased risk of morbidity and mortality ( 1 ).
Overall, four in 10 people exposed to unsafe PM2.5 levels live on less than $5.50 a day. Of the 716 million people living in extreme poverty and exposed to unsafe levels of air pollution, almost ...
Most air pollution research has focused on assessing the urban landscape effects of pollutants in megacities, little is known about their associations in small- to mid-sized cities. Considering ...
Air pollution is a grave problem that impacts billions of people across the globe. For example, it is the primary cause of death in India, killing over 1.6 million people a year [1].According to the Environmental Protection Agency (EPA), in 2017 about 111 million Americans (about 35% of the U.S. population) were living in counties with unhealthy air [2].
Introduction. Human-produced pollution is destabilizing the entire Earth System [1-3].This pollution poses severe risk to human health and the contemporary human niche [4-11].Most research assesses the independent risks of toxic emissions (e.g. fine particulate matter or PM2.5) and non-toxic emissions (e.g. greenhouse gases) and people's vulnerability to them [9,12,13].
Plastic pollution is a persistent challenge worldwide with the first reports evidencing its impact on the living and nonliving components of the environment dating back more than half a century. The rising concerns regarding the immediate and long-term consequences of plastic matter entrainment into foods and water cannot be overemphasized in light of our pursuit of sustainability (in terms of ...
Environmental Pollution is an international peer-reviewed journal that publishes high quality research papers and review articles about all aspects of environmental pollution and its effects on ecosystems and human health. The journal welcomes high-quality process-oriented and hypothesis-based submissions that report results from original and novel research and contribute new knowledge to help ...
Palla vi Saxena and V aishali Naik. 1 Anthropogenic Sources of Air Pollution 6. Chinmay Mallik. 2 Biogenic Sources of Air Pollution 26. Harpreet Kaur and Ruchi K umari. 3 Transport of Air P ...
1. Pollution—An Overview. Pollution is a global phenomenon, a persistent challenge that is transnational (i.e., borderless) in nature, transinstitutional in purview, and transdisciplinary in solution scope. 1−3 As indicated in Figure Figure1 1, pollution can arise naturally, for example, by saltwater intrusion into freshwater resources and volcanic eruptions that release dangerous gases ...
1. Introduction. Air pollution is almost a century-old challenge in India. However, the last few decades have been severe, the primary cause of which can be attributed to rapid population growth, unplanned urbanization, and industrialization (Kapoor, 2017; Udara, 2016).India is the second-most populous country in the world, which accounts for 17.7% of the global population (Census, 2011).
This paper comprehensively searched all the literature on the subject of 'land pollution' through the core collection of the Web of Science database, and systematically processed the research literature from 1944 to 2021 using CiteSpace software, and carried out bibliometric analysis and visual presentation, which uncovers the LP research dynamics in detail, and draw the following conclusions ...
INTRODUCTION. Environmental pollution has been a matter of concern for many years. The Mellon Institute of Pittsburgh, PA, USA, sponsored the first broad scientific study of smoke abatement, which resulted in legislation designed to decrease the effects of smoke. 1 It is now well known that environmental contamination impacts on health; the World Health Organization estimates that every year ...
Air pollution is a cause of disease for millions around the world and now more than ever urgent action is required to tackle the burden of its impacts. Doing so will not only improve both life ...
Background: More than 80% of sewage generated by human activities is discharged into rivers and oceans without any treatment, which results in environmental pollution and more than 50 diseases. 80% of diseases and 50% of child deaths worldwide are related to poor water quality.Methods: This paper selected 85 relevant papers finally based on the keywords of water pollution, water quality ...
Research on Health Effects from Air Pollution. Decades of research have shown that air pollutants such as ozone and particulate matter (PM) increase the amount and seriousness of lung and heart disease and other health problems. More investigation is needed to further understand the role poor air quality plays in causing detrimental effects to ...
The. groundwater reserve globally is about 70, 000, 00 Km 3. This surplus amount of water is brought. in to the ground annually by the process of precipitation and percolation. For the last few ...
Atmospheric Pollution Research (APR) is an international journal designed for the publication of articles on air pollution. Papers should present novel experimental results, theory and modeling of air pollution on local, regional, or global scales. Areas covered are research on inorganic, organic, and persistent organic air pollutants, air ...
1. Introduction. Plastic pollution is a global concern in today's world. In almost everywhere large fragments of plastic have been seen even from the most popular beaches to remote lonesome islands (Bucci and Rochman 2020).According to the report of Plastics Europe (2018), worldwide production of plastics has been expanded exponentially which nearly arrived at 350 million tons in 2017.
The iron content of coal ash has been documented in the context of coal quality control and commercial iron sourcing. Although typical values for the iron content in coal ash range 20%, with a variance of several tens of percent (Myers et al. 1973), higher values can be obtained if the ash is magnetically selected (Murtha & Burnet 1978).Spherule size is another source of bias as discussed in ...
Water pollution, according to (Olaniran et al., 1995), is. defined as the presence of excessive concentr ations of a danger (pollutants) in water to. the point where it is no longer appropriate ...