- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Buyline Personal Finance
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- March Madness
- AP Top 25 Poll
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media

How common is transgender treatment regret, detransitioning?

FILE - South Dakota Republican Rep. Jon Hansen speaks during a news conference at the state Capitol, Tuesday, Jan. 17, 2023, in Pierre, S.D. Hansen is pushing a bill to outlaw gender-affirming health care for transgender youth. (AP Photo/Stephen Groves, File)
FILE - People gather in support of transgender youth during a rally at the Utah State Capitol Tuesday, Jan. 24, 2023, in Salt Lake City. Utah lawmakers on Friday, Jan. 27, 2023, gave final approval for a measure that would ban most transgender youth from receiving gender-affirming health care like surgery or puberty blockers. (AP Photo/Rick Bowmer, File)
- Copy Link copied

Many states have enacted or contemplated limits or outright bans on transgender medical treatment, with conservative U.S. lawmakers saying they are worried about young people later regretting irreversible body-altering treatment.
But just how common is regret? And how many youth change their appearances with hormones or surgery only to later change their minds and detransition?
Here’s a look at some of the issues involved.
WHAT IS TRANSGENDER MEDICAL TREATMENT?
Guidelines call for thorough psychological assessments to confirm gender dysphoria — distress over gender identity that doesn’t match a person’s assigned sex — before starting any treatment.
That treatment typically begins with puberty-blocking medication to temporarily pause sexual development. The idea is to give youngsters time to mature enough mentally and emotionally to make informed decisions about whether to pursue permanent treatment. Puberty blockers may be used for years and can increase risks for bone density loss, but that reverses when the drugs are stopped.

Sex hormones — estrogen or testosterone — are offered next. Dutch research suggests that most gender-questioning youth on puberty blockers eventually choose to use these medications, which can produce permanent physical changes. So does transgender surgery, including breast removal or augmentation, which sometimes is offered during the mid-teen years but more typically not until age 18 or later.
Reports from doctors and individual U.S. clinics indicate that the number of youth seeking any kind of transgender medical care has increased in recent years.
HOW OFTEN DO TRANSGENDER PEOPLE REGRET TRANSITIONING?
In updated treatment guidelines issued last year, the World Professional Association for Transgender Health said evidence of later regret is scant, but that patients should be told about the possibility during psychological counseling.
Dutch research from several years ago found no evidence of regret in transgender adults who had comprehensive psychological evaluations in childhood before undergoing puberty blockers and hormone treatment.
Some studies suggest that rates of regret have declined over the years as patient selection and treatment methods have improved. In a review of 27 studies involving almost 8,000 teens and adults who had transgender surgeries, mostly in Europe, the U.S and Canada, 1% on average expressed regret. For some, regret was temporary, but a small number went on to have detransitioning or reversal surgeries, the 2021 review said.
Research suggests that comprehensive psychological counseling before starting treatment, along with family support, can reduce chances for regret and detransitioning.
WHAT IS DETRANSITIONING?
Detransitioning means stopping or reversing gender transition, which can include medical treatment or changes in appearance, or both.
Detransitioning does not always include regret. The updated transgender treatment guidelines note that some teens who detransition “do not regret initiating treatment” because they felt it helped them better understand their gender-related care needs.
Research and reports from individual doctors and clinics suggest that detransitioning is rare. The few studies that exist have too many limitations or weaknesses to draw firm conclusions, said Dr. Michael Irwig, director of transgender medicine at Beth Israel Deaconess Medical Center in Boston.
He said it’s difficult to quantify because patients who detransition often see new doctors, not the physicians who prescribed the hormones or performed the surgeries. Some patients may simply stop taking hormones.
“My own personal experience is that it is quite uncommon,” Irwig said. “I’ve taken care of over 350 gender-diverse patients and probably fewer than five have told me that they decided to detransition or changed their minds.”
Recent increases in the number of people seeking transgender medical treatment could lead to more people detransitioning, Irwig noted in a commentary last year in the Journal of Clinical Endocrinology & Metabolism. That’s partly because of a shortage of mental health specialists, meaning gender-questioning people may not receive adequate counseling, he said.
Dr. Oscar Manrique, a plastic surgeon at the University of Rochester Medical Center, has operated on hundreds of transgender people, most of them adults. He said he’s never had a patient return seeking to detransition.
Some may not be satisfied with their new appearance, but that doesn’t mean they regret the transition, he said. Most, he said, “are very happy with the outcomes surgically and socially.”
Follow AP Medical Writer Lindsey Tanner at @LindseyTanner.
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.

UK Edition Change
- UK Politics
- News Videos
- Paris 2024 Olympics
- Rugby Union
- Sport Videos
- John Rentoul
- Mary Dejevsky
- Andrew Grice
- Sean O’Grady
- Photography
- Theatre & Dance
- Culture Videos
- Food & Drink
- Health & Families
- Royal Family
- Electric Vehicles
- Lifestyle Videos
- UK Hotel Reviews
- News & Advice
- Simon Calder
- Australia & New Zealand
- South America
- C. America & Caribbean
- Middle East
- Politics Explained
- News Analysis
- Today’s Edition
- Home & Garden
- Fashion & Beauty
- Travel & Outdoors
- Sports & Fitness
- Sustainable Living
- Climate Videos
- Behind The Headlines
- On The Ground
- Decomplicated
- You Ask The Questions
- Binge Watch
- Travel Smart
- Watch on your TV
- Crosswords & Puzzles
- Most Commented
- Newsletters
- Ask Me Anything
- Virtual Events
- Betting Sites
- Online Casinos
- Wine Offers
Thank you for registering
Please refresh the page or navigate to another page on the site to be automatically logged in Please refresh your browser to be logged in
Gender reversal surgery is more in-demand than ever before
But what are the consequences, article bookmarked.
Find your bookmarks in your Independent Premium section, under my profile

Stay ahead of the trend in fashion and beyond with our free weekly Lifestyle Edit newsletter
Thanks for signing up to the lifestyle edit email.
Gender reassignment surgery has been available on the NHS for more than 17 years.
It’s a treatment for those experiencing gender dysphoria, whereby a person recognises a discrepancy between their biological sex and their gender identity.
Gender identity clinics are in place throughout the UK to provide support to those feeling distressed by the condition - but what happens when a trans person undergoes surgery and later decides to revert back to their original gender?
- John Lewis gender neutral clothing labels faces public backlash
Is it possible? Is it safe? And is it available on the NHS?
These are not questions that are not easily-answered. Five phone calls and endless emails later, the details regarding what circumstances would allow for such a treatment to be carried out on the NHS remain muddled.
It's potentially why some of those seeking “reversal” surgeries are heading to a clinic in Serbia, where Professor Misoslav Djordjevic has been performing them for five years at the Belgrade Center for Genital Reconstructive Surgery.
A specialist in genital reconstruction with 20 years of experience, Prof Djordjevic began conducting the innovative procedures after a transgender patient who had undergone surgery to remove male genitalia requested a reversal.
It's by no means a common practice. He has performed just 14 surgeries to date and is currently in the process of treating two “reversal” patients, reports The Daily Telegraph , explaining that the procedure is extremely complex and can cost up to €18,000 (£15,965).
- Parents hit out at school's 'political agenda' over transgender pupil
However, his services aren't easily-accessed. Djordjevic will only treat patients who have undergone a full one-year-long psychiatric evaluation and he stresses the importance of post-surgery aftercare, revealing that he remains in contact with the majority of his patients.
It's not simply a case of people regretting their decision, explains James Morton, manager at the Scottish Trans Alliance , who told The Independent that a range of factors could catalyse the desire for a gender reversal including unusual surgical complications, being worn down by transphobic harassment, family rejection, or developing religious or political beliefs that being transgender is unacceptable.
"If a person has regret about undergoing gender reassignment, it is especially important that they receive counselling and in-depth assessment before undergoing any surgery to attempt partial reversal as their chance of regretting further surgery could be even higher," he said.
- What the legalisation of gay sex 50 years ago means to LGBT people now
"Any further NHS surgery is determined on an individualised case by case basis because the numbers are so tiny."
So far, Djordjevic has exclusively treated transgender females who have asked to recreate their male genitalia.
Known as phalloplasty, the procedure entails the construction of a penis from skin taken from the groin, abdomen or thigh. Though the surgery produces aesthetic results, many mistakenly assume that it will ultimately render one’s genitalia physically futile.
However, a 2013 study revealed that the introduction of penile stiffeners has allowed some plastic surgeons to create a fully functioning organ.
- We need more clothing sections than 'men's' and 'women's' says tailor
It is a much more risky procedure than its male to female counterpart, vaginoplasty, whereby the testicles are removed and the skin of the penis is used to artificially create a vagina.
Whilst awareness of non-binary issues has increased in recent years, gender reassignment remains a severely under researched topic, so much so that the NHS has produced an online e-learning guide to GPs who might be unfamiliar with gender dysphoria.
The severe lack of understanding surrounding the topic - and its reversal counterpart - became particularly prevalent last week, when a proposed study to explore why transsexual people may want to “detransition” was reportedly shut down by Bath Spa University so as “not to offend people.”
- Trans artist helps break down period stigma with bold post
“The fundamental reason given was that it might cause criticism of the research on social media and criticism of the research would be criticism of the university and they also added it was better not to offend people,” James Caspian, the psychotherapist behind the proposed research, told BBC Radio 4 .
He confessed to being “astonished” at the university’s decision.
As of 30 August, there were 213 patients on the list for gender reassignment surgery at Imperial College Healthcare NHS Trust .
At present, there are no statistics regarding gender reversal surgeries in the UK.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Subscribe to Independent Premium to bookmark this article
Want to bookmark your favourite articles and stories to read or reference later? Start your Independent Premium subscription today.
New to The Independent?
Or if you would prefer:
Want an ad-free experience?
Hi {{indy.fullName}}
- My Independent Premium
- Account details
- Help centre
May 12, 2022
What the Science on Gender-Affirming Care for Transgender Kids Really Shows
Laws that ban gender-affirming treatment ignore the wealth of research demonstrating its benefits for trans people’s health
By Heather Boerner

As attacks against transgender kids increase in the U.S., Minnesotans hold a rally at the state’s capitol in Saint Paul in March 2022 to support trans kids in Minnesota and Texas and around the country.
Michael Siluk/UCG/Universal Images Group via Getty Images
Editor’s Note (3/30/23): This article from May 2022 is being republished to highlight the ways that ongoing anti-trans legislation is harmful and unscientific.
For the first 40 years of their life, Texas resident Kelly Fleming spent a portion of most years in a deep depression. As an adult, Fleming—who uses they/them pronouns and who asked to use a pseudonym to protect their safety—would shave their face in the shower with the lights off so neither they nor their wife would have to confront the reality of their body.
What Fleming was experiencing, although they did not know it at the time, was gender dysphoria : the acute and chronic distress of living in a body that does not reflect one’s gender and the desire to have bodily characteristics of that gender. While in therapy, Fleming discovered research linking access to gender-affirming hormone therapy with reduced depression in transgender people. They started a very low dose of estradiol, and the depression episodes became shorter, less frequent and less intense. Now they look at their body with joy.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
So when Fleming sees what authorities in Texas , Alabama , Florida and other states are doing to bar transgender teens and children from receiving gender-affirming medical care, it infuriates them. And they are worried for their children, ages 12 and 14, both of whom are agender—a identity on the transgender spectrum that is neither masculine nor feminine.
“I’m just so excited to see them being able to present themselves in a way that makes them happy,” Fleming says. “They are living their best life regardless of what others think, and that’s a privilege that I did not get to have as a younger person.”
Laws Based on “Completely Wrong” Information
Currently more than a dozen state legislatures or administrations are considering—or have already passed—laws banning health care for transgender young people. On April 20 the Florida Department of Health issued guidance to withhold such gender-affirming care. This includes social gender transitioning—acknowledging that a young person is trans, using their correct pronouns and name, and supporting their desire to live publicly as the gender of their experience rather than their sex assigned at birth. This comes nearly two months after Texas Governor Greg Abbott issued an order for the Texas Department of Family and Protective Services to investigate for child abuse parents who allow their transgender preteens and teenagers to receive medical care. Alabama recently passed SB 184 , which would make it a felony to provide gender-affirming medical care to transgender minors. In Alabama, a “minor” is defined as anyone 19 or younger.
If such laws go ahead, 58,200 teens in the U.S. could lose access to or never receive gender-affirming care, according to the Williams Institute at the University of California, Los Angeles. A decade of research shows such treatment reduces depression, suicidality and other devastating consequences of trans preteens and teens being forced to undergo puberty in the sex they were assigned at birth).
The bills are based on “information that’s completely wrong,” says Michelle Forcier, a pediatrician and professor of pediatrics at Brown University. Forcier literally helped write the book on how to provide evidence-based gender care to young people. She is also an assistant dean of admissions at the Warren Alpert Medical School of Brown University. Those laws “are absolutely, absolutely incorrect” about the science of gender-affirming care for young people, she says. “[Inaccurate information] is there to create drama. It’s there to make people take a side.”
The truth is that data from more than a dozen studies of more than 30,000 transgender and gender-diverse young people consistently show that access to gender-affirming care is associated with better mental health outcomes—and that lack of access to such care is associated with higher rates of suicidality, depression and self-harming behavior. (Gender diversity refers to the extent to which a person’s gendered behaviors, appearance and identities are culturally incongruent with the sex they were assigned at birth. Gender-diverse people can identify along the transgender spectrum, but not all do.) Major medical organizations, including the American Academy of Pediatrics (AAP) , the American Academy of Child and Adolescent Psychiatry , the Endocrine Society , the American Medical Association , the American Psychological Association and the American Psychiatric Association , have published policy statements and guidelines on how to provide age-appropriate gender-affirming care. All of those medical societies find such care to be evidence-based and medically necessary.
AAP and Endocrine Society guidelines call for developmentally appropriate care, and that means no puberty blockers or hormones until young people are already undergoing puberty for their sex assigned at birth. For one thing, “there are no hormonal differences among prepubertal children,” says Joshua Safer, executive director of the Mount Sinai Center for Transgender Medicine and Surgery in New York City and co-author of the Endocrine Society’s guidelines. Those guidelines provide the option of gonadotropin-releasing hormone analogues (GnRHas), which block the release of sex hormones, once young people are already into the second of five puberty stages—marked by breast budding and pubic hair. These are offered only if a teen is not ready to make decisions about puberty. Access to gender-affirming hormones and potential access to gender-affirming surgery is available at age 16—and then, in the case of transmasculine youth, only mastectomy, also known as top surgery. The Endocrine Society does not recommend genital surgery for minors.
Before puberty, gender-affirming care is about supporting the process of gender development rather than directing children through a specific course of gender transition or maintenance of cisgender presentation, says Jason Rafferty, co-author of AAP’s policy statement on gender-affirming care and a pediatrician and psychiatrist at Hasbro Children’s Hospital in Rhode Island. “The current research suggests that, rather than predicting or preventing who a child might become, it’s better to value them for who they are now—even at a young age,” Rafferty says.
A Safe Environment to Explore Gender
A 2021 systematic review of 44 peer-reviewed studies found that parent connectedness, measured by a six-question scale asking about such things as how safe young people feel confiding in their guardians or how cared for they feel in the family, is associated with greater resilience among teens and young adults who are transgender or gender-diverse. Rafferty says he sees his role with regard to prepubertal children as offering a safe environment for the child to explore their gender and for parents to ask questions. “The gender-affirming approach is not some railroad of people to hormones and surgery,” Safer says. “It is talking and watching and being conservative.”
Only once children are older, and if the incongruence between the sex assigned to them at birth and their experienced gender has persisted, does discussion of medical transition occur. First a gender therapist has to diagnose the young person with gender dysphoria .
After a gender dysphoria diagnosis—and only if earlier conversations suggest that hormones are indicated—guidelines call for discussion of fertility, puberty suppression and hormones. Puberty-suppressing medications have been used for decades for cisgender children who start puberty early, but they are not meant to be used indefinitely. The Endocrine Society guidelines recommend a maximum of two years on GnRHa therapy to allow more time for children to form their gender identity before undergoing puberty for their sex assigned at birth, the effects of which are irreversible.
“[Puberty blockers] are part of the process of ‘do no harm,’” Forcier says, referencing a popular phrase that describes the Hippocratic Oath, which many physicians recite a version of before they begin to practice.
Hormone blocker treatment may have side effects. A 2015 longitudinal observational cohort study of 34 transgender young people found that, by the time the participants were 22 years old, trans women experienced a decrease in bone mineral density. A 2020 study of puberty suppression in gender-diverse and transgender young people found that those who started puberty blockers in early puberty had lower bone mineral density before the start of treatment than the public at large. This suggests, the authors wrote, that GnRHa use may not be the cause of low bone mineral density for these young people. Instead they found that lack of exercise was a primary factor in low bone-mineral density, especially among transgender girls.
Other side effects of GnRHa therapy include weight gain, hot flashes and mood swings. But studies have found that these side effects—and puberty delay itself—are reversible , Safer says.
Gender-affirming hormone therapy often involves taking an androgen blocker (a chemical that blocks the release of testosterone and other androgenic hormones) and estrogen in transfeminine teens, and testosterone supplementation in transmasculine teens. Such hormones may be associated with some physiological changes for adult transgender people. For instance, transfeminine people taking estrogen see their so-called “good” cholesterol increase. By contrast, transmasculine people taking testosterone see their good cholesterol decrease. Some studies have hinted at effects on bone mineral density, but these are complicated and also depend on personal, family history, exercise, and many other factors in addition to hormones.”
And while some critics point to decade-old study and older studies suggesting very few young people persist in transgender identity into late adolescence and adulthood, Forcier says the data are “misleading and not accurate.” A recent review detailed methodological problems with some of these studies . New research in 17,151 people who had ever socially transitioned found that 86.9 percent persisted in their gender identity. Of the 2,242 people who reported that they reverted to living as the gender associated with the sex they were assigned at birth, just 15.9 percent said they did so because of internal factors such as questioning their experienced gender but also because of fear, mental health issues and suicide attempts. The rest reported the cause was social, economic and familial stigma and discrimination. A third reported that they ceased living openly as a trans person because doing so was “just too hard for me.”
The Harms of Denying Care
Data suggest the effects of denying that care are worse than whatever side effects result from delaying sex-assigned-at-birth puberty. And medical society guidelines conclude that the benefits of gender-affirming care outweigh the risks. Without gender-affirming hormone therapy, cisgender hormones take over, forcing body changes that can be permanent and distressing.
A 2020 study of 300 gender-incongruent young people found that mental distress—including self-harm, suicidal thoughts and depression— increased as the children were made to proceed with puberty according to their assigned sex. By the time 184 older teens (with a median age of 16) reached the stage in which transgender boys began their periods and grew breasts and transgender girls’ voice dropped and facial hair began to appear, 46 percent had been diagnosed with depression, 40 percent had self-harmed, 52 percent had considered suicide, and 17 percent had attempted it—rates significantly higher than those of gender-incongruent children who were a median of 13.9 years old or of cisgender kids their own age.
Conversely, access to gender-affirming hormones in adolescence appears to have a protective effect. In one study, researchers followed 104 teens and young adults for a year and asked them about their depression, anxiety and suicidality at the time they started receiving hormones or puberty blockers and again at the three-month, six-month and one-year mark. At the beginning of the study, which was published in JAMA Network Open in February 2022, more than half of the respondents reported moderate to severe depression, half reported moderate to severe anxiety, and 43.3 percent reported thoughts of self-harm or suicide in the past two weeks.
But when the researchers analyzed the results based on the kind of gender-affirming care the teens had received, they found that those who had access to puberty blockers or gender-affirming hormones were 60 percent less likely to experience moderate to severe depression. And those with access to the medical treatments were 73 percent less likely to contemplate self-harm or suicide.
“Delays in prescribing puberty blockers and hormones may in fact worsen mental health symptoms for trans youth,” says Diana Tordoff, an epidemiology graduate student at the University of Washington and co-author of the study.
That effect may be lifelong. A 2022 study of more than 21,000 transgender adults showed that just 41 percent of adults who wanted hormone therapy received it, and just 2.3 percent had access to it in adolescence. When researchers looked at rates of suicidal thinking over the past year in these same adults, they found that access to hormone therapy in early adolescence was associated with a 60 percent reduction in suicidality in the past year and that access in late adolescence was associated with a 50 percent reduction.
For Fleming’s kids in Texas, gender-affirming hormones are not currently part of the discussion; not all trans people desire hormones or surgery to feel affirmed in their gender. But Fleming is already looking at jobs in other states to protect their children’s access to such care, should they change their mind. “Getting your body closer to the gender [you] identify with—that is what helps the dysphoria,” Fleming says. “And not giving people the opportunity to do that, making it harder for them to do that, is what has made the suicide rate among transgender people so high. We just—trans people are just trying to survive.”
IF YOU NEED HELP If you or someone you know is struggling or having thoughts of suicide, help is available. Call the National Suicide Prevention Lifeline at 1-800-273-8255 (TALK), use the online Lifeline Chat or contact the Crisis Text Line by texting TALK to 741741.
- Search the site GO Please fill out this field.
- Newsletters
- Mental Health
- Social and Public Health
What Is Gender Affirmation Surgery?
:max_bytes(150000):strip_icc():format(webp)/KP-Headshot-IMG_1661-0d48c6ea46f14ab19a91e7b121b49f59.jpg)
A gender affirmation surgery allows individuals, such as those who identify as transgender or nonbinary, to change one or more of their sex characteristics. This type of procedure offers a person the opportunity to have features that align with their gender identity.
For example, this type of surgery may be a transgender surgery like a male-to-female or female-to-male surgery. Read on to learn more about what masculinizing, feminizing, and gender-nullification surgeries may involve, including potential risks and complications.
Why Is Gender Affirmation Surgery Performed?
A person may have gender affirmation surgery for different reasons. They may choose to have the surgery so their physical features and functional ability align more closely with their gender identity.
For example, one study found that 48,019 people underwent gender affirmation surgeries between 2016 and 2020. Most procedures were breast- and chest-related, while the remaining procedures concerned genital reconstruction or facial and cosmetic procedures.
In some cases, surgery may be medically necessary to treat dysphoria. Dysphoria refers to the distress that transgender people may experience when their gender identity doesn't match their sex assigned at birth. One study found that people with gender dysphoria who had gender affirmation surgeries experienced:
- Decreased antidepressant use
- Decreased anxiety, depression, and suicidal ideation
- Decreased alcohol and drug abuse
However, these surgeries are only performed if appropriate for a person's case. The appropriateness comes about as a result of consultations with mental health professionals and healthcare providers.
Transgender vs Nonbinary
Transgender and nonbinary people can get gender affirmation surgeries. However, there are some key ways that these gender identities differ.
Transgender is a term that refers to people who have gender identities that aren't the same as their assigned sex at birth. Identifying as nonbinary means that a person doesn't identify only as a man or a woman. A nonbinary individual may consider themselves to be:
- Both a man and a woman
- Neither a man nor a woman
- An identity between or beyond a man or a woman
Hormone Therapy
Gender-affirming hormone therapy uses sex hormones and hormone blockers to help align the person's physical appearance with their gender identity. For example, some people may take masculinizing hormones.
"They start growing hair, their voice deepens, they get more muscle mass," Heidi Wittenberg, MD , medical director of the Gender Institute at Saint Francis Memorial Hospital in San Francisco and director of MoZaic Care Inc., which specializes in gender-related genital, urinary, and pelvic surgeries, told Health .
Types of hormone therapy include:
- Masculinizing hormone therapy uses testosterone. This helps to suppress the menstrual cycle, grow facial and body hair, increase muscle mass, and promote other male secondary sex characteristics.
- Feminizing hormone therapy includes estrogens and testosterone blockers. These medications promote breast growth, slow the growth of body and facial hair, increase body fat, shrink the testicles, and decrease erectile function.
- Non-binary hormone therapy is typically tailored to the individual and may include female or male sex hormones and/or hormone blockers.
It can include oral or topical medications, injections, a patch you wear on your skin, or a drug implant. The therapy is also typically recommended before gender affirmation surgery unless hormone therapy is medically contraindicated or not desired by the individual.
Masculinizing Surgeries
Masculinizing surgeries can include top surgery, bottom surgery, or both. Common trans male surgeries include:
- Chest masculinization (breast tissue removal and areola and nipple repositioning/reshaping)
- Hysterectomy (uterus removal)
- Metoidioplasty (lengthening the clitoris and possibly extending the urethra)
- Oophorectomy (ovary removal)
- Phalloplasty (surgery to create a penis)
- Scrotoplasty (surgery to create a scrotum)
Top Surgery
Chest masculinization surgery, or top surgery, often involves removing breast tissue and reshaping the areola and nipple. There are two main types of chest masculinization surgeries:
- Double-incision approach : Used to remove moderate to large amounts of breast tissue, this surgery involves two horizontal incisions below the breast to remove breast tissue and accentuate the contours of pectoral muscles. The nipples and areolas are removed and, in many cases, resized, reshaped, and replaced.
- Short scar top surgery : For people with smaller breasts and firm skin, the procedure involves a small incision along the lower half of the areola to remove breast tissue. The nipple and areola may be resized before closing the incision.
Metoidioplasty
Some trans men elect to do metoidioplasty, also called a meta, which involves lengthening the clitoris to create a small penis. Both a penis and a clitoris are made of the same type of tissue and experience similar sensations.
Before metoidioplasty, testosterone therapy may be used to enlarge the clitoris. The procedure can be completed in one surgery, which may also include:
- Constructing a glans (head) to look more like a penis
- Extending the urethra (the tube urine passes through), which allows the person to urinate while standing
- Creating a scrotum (scrotoplasty) from labia majora tissue
Phalloplasty
Other trans men opt for phalloplasty to give them a phallic structure (penis) with sensation. Phalloplasty typically requires several procedures but results in a larger penis than metoidioplasty.
The first and most challenging step is to harvest tissue from another part of the body, often the forearm or back, along with an artery and vein or two, to create the phallus, Nicholas Kim, MD, assistant professor in the division of plastic and reconstructive surgery in the department of surgery at the University of Minnesota Medical School in Minneapolis, told Health .
Those structures are reconnected under an operative microscope using very fine sutures—"thinner than our hair," said Dr. Kim. That surgery alone can take six to eight hours, he added.
In a separate operation, called urethral reconstruction, the surgeons connect the urinary system to the new structure so that urine can pass through it, said Dr. Kim. Urethral reconstruction, however, has a high rate of complications, which include fistulas or strictures.
According to Dr. Kim, some trans men prefer to skip that step, especially if standing to urinate is not a priority. People who want to have penetrative sex will also need prosthesis implant surgery.
Hysterectomy and Oophorectomy
Masculinizing surgery often includes the removal of the uterus (hysterectomy) and ovaries (oophorectomy). People may want a hysterectomy to address their dysphoria, said Dr. Wittenberg, and it may be necessary if their gender-affirming surgery involves removing the vagina.
Many also opt for an oophorectomy to remove the ovaries, almond-shaped organs on either side of the uterus that contain eggs and produce female sex hormones. In this case, oocytes (eggs) can be extracted and stored for a future surrogate pregnancy, if desired. However, this is a highly personal decision, and some trans men choose to keep their uterus to preserve fertility.
Feminizing Surgeries
Surgeries are often used to feminize facial features, enhance breast size and shape, reduce the size of an Adam’s apple , and reconstruct genitals. Feminizing surgeries can include:
- Breast augmentation
- Facial feminization surgery
- Penis removal (penectomy)
- Scrotum removal (scrotectomy)
- Testicle removal (orchiectomy)
- Tracheal shave (chondrolaryngoplasty) to reduce an Adam's apple
- Vaginoplasty
- Voice feminization
Breast Augmentation
Top surgery, also known as breast augmentation or breast mammoplasty, is often used to increase breast size for a more feminine appearance. The procedure can involve placing breast implants, tissue expanders, or fat from other parts of the body under the chest tissue.
Breast augmentation can significantly improve gender dysphoria. Studies show most people who undergo top surgery are happier, more satisfied with their chest, and would undergo the surgery again.
Most surgeons recommend 12 months of feminizing hormone therapy before breast augmentation. Since hormone therapy itself can lead to breast tissue development, transgender women may or may not decide to have surgical breast augmentation.
Facial Feminization and Adam's Apple Removal
Facial feminization surgery (FFS) is a series of plastic surgery procedures that reshape the forehead, hairline, eyebrows, nose, cheeks, and jawline. Nonsurgical treatments like cosmetic fillers, botox, fat grafting, and liposuction may also be used to create a more feminine appearance.
Some trans women opt for chondrolaryngoplasty, also known as a tracheal shave. The procedure reduces the size of the Adam's apple, an area of cartilage around the larynx (voice box) that tends to be larger in people assigned male at birth.
Vulvoplasty and Vaginoplasty
As for bottom surgery, there are various feminizing procedures from which to choose. Vulvoplasty (to create external genitalia without a vagina) or vaginoplasty (to create a vulva and vaginal canal) are two of the most common procedures.
Dr. Wittenberg noted that people might undergo six to 12 months of electrolysis or laser hair removal before surgery to remove pubic hair from the skin that will be used for the vaginal lining.
Surgeons have different techniques for creating a vaginal canal. A common one is a penile inversion, where the masculine structures are emptied and inverted into a created cavity, explained Dr. Kim. Vaginoplasty may be done in one or two stages, said Dr. Wittenberg, and the initial recovery is three months—but it will be a full year until people see results.
Surgical removal of the penis or penectomy is sometimes used in feminization treatment. This can be performed along with an orchiectomy and scrotectomy.
However, a total penectomy is not commonly used in feminizing surgeries . Instead, many people opt for penile-inversion surgery, a technique that hollows out the penis and repurposes the tissue to create a vagina during vaginoplasty.
Orchiectomy and Scrotectomy
An orchiectomy is a surgery to remove the testicles —male reproductive organs that produce sperm. Scrotectomy is surgery to remove the scrotum, that sac just below the penis that holds the testicles.
However, some people opt to retain the scrotum. Scrotum skin can be used in vulvoplasty or vaginoplasty, surgeries to construct a vulva or vagina.
Other Surgical Options
Some gender non-conforming people opt for other types of surgeries. This can include:
- Gender nullification procedures
- Penile preservation vaginoplasty
- Vaginal preservation phalloplasty
Gender Nullification
People who are agender or asexual may opt for gender nullification, sometimes called nullo. This involves the removal of all sex organs. The external genitalia is removed, leaving an opening for urine to pass and creating a smooth transition from the abdomen to the groin.
Depending on the person's sex assigned at birth, nullification surgeries can include:
- Breast tissue removal
- Nipple and areola augmentation or removal
Penile Preservation Vaginoplasty
Some gender non-conforming people assigned male at birth want a vagina but also want to preserve their penis, said Dr. Wittenberg. Often, that involves taking skin from the lining of the abdomen to create a vagina with full depth.
Vaginal Preservation Phalloplasty
Alternatively, a patient assigned female at birth can undergo phalloplasty (surgery to create a penis) and retain the vaginal opening. Known as vaginal preservation phalloplasty, it is often used as a way to resolve gender dysphoria while retaining fertility.
The recovery time for a gender affirmation surgery will depend on the type of surgery performed. For example, healing for facial surgeries may last for weeks, while transmasculine bottom surgery healing may take months.
Your recovery process may also include additional treatments or therapies. Mental health support and pelvic floor physiotherapy are a few options that may be needed or desired during recovery.
Risks and Complications
The risk and complications of gender affirmation surgeries will vary depending on which surgeries you have. Common risks across procedures could include:
- Anesthesia risks
- Hematoma, which is bad bruising
- Poor incision healing
Complications from these procedures may be:
- Acute kidney injury
- Blood transfusion
- Deep vein thrombosis, which is blood clot formation
- Pulmonary embolism, blood vessel blockage for vessels going to the lung
- Rectovaginal fistula, which is a connection between two body parts—in this case, the rectum and vagina
- Surgical site infection
- Urethral stricture or stenosis, which is when the urethra narrows
- Urinary tract infection (UTI)
- Wound disruption
What To Consider
It's important to note that an individual does not need surgery to transition. If the person has surgery, it is usually only one part of the transition process.
There's also psychotherapy . People may find it helpful to work through the negative mental health effects of dysphoria. Typically, people seeking gender affirmation surgery must be evaluated by a qualified mental health professional to obtain a referral.
Some people may find that living in their preferred gender is all that's needed to ease their dysphoria. Doing so for one full year prior is a prerequisite for many surgeries.
All in all, the entire transition process—living as your identified gender, obtaining mental health referrals, getting insurance approvals, taking hormones, going through hair removal, and having various surgeries—can take years, healthcare providers explained.
A Quick Review
Whether you're in the process of transitioning or supporting someone who is, it's important to be informed about gender affirmation surgeries. Gender affirmation procedures often involve multiple surgeries, which can be masculinizing, feminizing, or gender-nullifying in nature.
It is a highly personalized process that looks different for each person and can often take several months or years. The procedures also vary regarding risks and complications, so consultations with healthcare providers and mental health professionals are essential before having these procedures.
American Society of Plastic Surgeons. Gender affirmation surgeries .
Wright JD, Chen L, Suzuki Y, Matsuo K, Hershman DL. National estimates of gender-affirming surgery in the US . JAMA Netw Open . 2023;6(8):e2330348-e2330348. doi:10.1001/jamanetworkopen.2023.30348
Coleman E, Radix AE, Bouman WP, et al. Standards of care for the health of transgender and gender diverse people, version 8 . Int J Transgend Health . 2022;23(S1):S1-S260. doi:10.1080/26895269.2022.2100644
Chou J, Kilmer LH, Campbell CA, DeGeorge BR, Stranix JY. Gender-affirming surgery improves mental health outcomes and decreases anti-depressant use in patients with gender dysphoria . Plast Reconstr Surg Glob Open . 2023;11(6 Suppl):1. doi:10.1097/01.GOX.0000944280.62632.8c
Human Rights Campaign. Get the facts on gender-affirming care .
Human Rights Campaign. Transgender and non-binary people FAQ .
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877–84. doi:10.21037/tau.2016.09.04
Richards JE, Hawley RS. Chapter 8: Sex Determination: How Genes Determine a Developmental Choice . In: Richards JE, Hawley RS, eds. The Human Genome . 3rd ed. Academic Press; 2011: 273-298.
Randolph JF Jr. Gender-affirming hormone therapy for transgender females . Clin Obstet Gynecol . 2018;61(4):705-721. doi:10.1097/GRF.0000000000000396
Cocchetti C, Ristori J, Romani A, Maggi M, Fisher AD. Hormonal treatment strategies tailored to non-binary transgender individuals . J Clin Med . 2020;9(6):1609. doi:10.3390/jcm9061609
Van Boerum MS, Salibian AA, Bluebond-Langner R, Agarwal C. Chest and facial surgery for the transgender patient . Transl Androl Urol . 2019;8(3):219-227. doi:10.21037/tau.2019.06.18
Djordjevic ML, Stojanovic B, Bizic M. Metoidioplasty: techniques and outcomes . Transl Androl Urol . 2019;8(3):248–53. doi:10.21037/tau.2019.06.12
Bordas N, Stojanovic B, Bizic M, Szanto A, Djordjevic ML. Metoidioplasty: surgical options and outcomes in 813 cases . Front Endocrinol . 2021;12:760284. doi:10.3389/fendo.2021.760284
Al-Tamimi M, Pigot GL, van der Sluis WB, et al. The surgical techniques and outcomes of secondary phalloplasty after metoidioplasty in transgender men: an international, multi-center case series . The Journal of Sexual Medicine . 2019;16(11):1849-1859. doi:10.1016/j.jsxm.2019.07.027
Waterschoot M, Hoebeke P, Verla W, et al. Urethral complications after metoidioplasty for genital gender affirming surgery . J Sex Med . 2021;18(7):1271–9. doi:10.1016/j.jsxm.2020.06.023
Nikolavsky D, Hughes M, Zhao LC. Urologic complications after phalloplasty or metoidioplasty . Clin Plast Surg . 2018;45(3):425–35. doi:10.1016/j.cps.2018.03.013
Nota NM, den Heijer M, Gooren LJ. Evaluation and treatment of gender-dysphoric/gender incongruent adults . In: Feingold KR, Anawalt B, Boyce A, et al., eds. Endotext . MDText.com, Inc.; 2000.
Carbonnel M, Karpel L, Cordier B, Pirtea P, Ayoubi JM. The uterus in transgender men . Fertil Steril . 2021;116(4):931–5. doi:10.1016/j.fertnstert.2021.07.005
Miller TJ, Wilson SC, Massie JP, Morrison SD, Satterwhite T. Breast augmentation in male-to-female transgender patients: Technical considerations and outcomes . JPRAS Open . 2019;21:63-74. doi:10.1016/j.jpra.2019.03.003
Claes KEY, D'Arpa S, Monstrey SJ. Chest surgery for transgender and gender nonconforming individuals . Clin Plast Surg . 2018;45(3):369–80. doi:10.1016/j.cps.2018.03.010
De Boulle K, Furuyama N, Heydenrych I, et al. Considerations for the use of minimally invasive aesthetic procedures for facial remodeling in transgender individuals . Clin Cosmet Investig Dermatol . 2021;14:513-525. doi:10.2147/CCID.S304032
Asokan A, Sudheendran MK. Gender affirming body contouring and physical transformation in transgender individuals . Indian J Plast Surg . 2022;55(2):179-187. doi:10.1055/s-0042-1749099
Sturm A, Chaiet SR. Chondrolaryngoplasty-thyroid cartilage reduction . Facial Plast Surg Clin North Am . 2019;27(2):267–72. doi:10.1016/j.fsc.2019.01.005
Chen ML, Reyblat P, Poh MM, Chi AC. Overview of surgical techniques in gender-affirming genital surgery . Transl Androl Urol . 2019;8(3):191-208. doi:10.21037/tau.2019.06.19
Wangjiraniran B, Selvaggi G, Chokrungvaranont P, Jindarak S, Khobunsongserm S, Tiewtranon P. Male-to-female vaginoplasty: Preecha's surgical technique . J Plast Surg Hand Surg . 2015;49(3):153-9. doi:10.3109/2000656X.2014.967253
Okoye E, Saikali SW. Orchiectomy . In: StatPearls [Internet] . Treasure Island (FL): StatPearls Publishing; 2022.
Salgado CJ, Yu K, Lalama MJ. Vaginal and reproductive organ preservation in trans men undergoing gender-affirming phalloplasty: technical considerations . J Surg Case Rep . 2021;2021(12):rjab553. doi:10.1093/jscr/rjab553
American Society of Plastic Surgeons. What should I expect during my recovery after facial feminization surgery?
American Society of Plastic Surgeons. What should I expect during my recovery after transmasculine bottom surgery?
de Brouwer IJ, Elaut E, Becker-Hebly I, et al. Aftercare needs following gender-affirming surgeries: findings from the ENIGI multicenter European follow-up study . The Journal of Sexual Medicine . 2021;18(11):1921-1932. doi:10.1016/j.jsxm.2021.08.005
American Society of Plastic Surgeons. What are the risks of transfeminine bottom surgery?
American Society of Plastic Surgeons. What are the risks of transmasculine top surgery?
Khusid E, Sturgis MR, Dorafshar AH, et al. Association between mental health conditions and postoperative complications after gender-affirming surgery . JAMA Surg . 2022;157(12):1159-1162. doi:10.1001/jamasurg.2022.3917
Related Articles
- Patient Care & Health Information
- Tests & Procedures
- Feminizing hormone therapy
Feminizing hormone therapy typically is used by transgender women and nonbinary people to produce physical changes in the body that are caused by female hormones during puberty. Those changes are called secondary sex characteristics. This hormone therapy helps better align the body with a person's gender identity. Feminizing hormone therapy also is called gender-affirming hormone therapy.
Feminizing hormone therapy involves taking medicine to block the action of the hormone testosterone. It also includes taking the hormone estrogen. Estrogen lowers the amount of testosterone the body makes. It also triggers the development of feminine secondary sex characteristics. Feminizing hormone therapy can be done alone or along with feminizing surgery.
Not everybody chooses to have feminizing hormone therapy. It can affect fertility and sexual function, and it might lead to health problems. Talk with your health care provider about the risks and benefits for you.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Feminizing hormone therapy is used to change the body's hormone levels. Those hormone changes trigger physical changes that help better align the body with a person's gender identity.
In some cases, people seeking feminizing hormone therapy experience discomfort or distress because their gender identity differs from their sex assigned at birth or from their sex-related physical characteristics. This condition is called gender dysphoria.
Feminizing hormone therapy can:
- Improve psychological and social well-being.
- Ease psychological and emotional distress related to gender.
- Improve satisfaction with sex.
- Improve quality of life.
Your health care provider might advise against feminizing hormone therapy if you:
- Have a hormone-sensitive cancer, such as prostate cancer.
- Have problems with blood clots, such as when a blood clot forms in a deep vein, a condition called deep vein thrombosis, or a there's a blockage in one of the pulmonary arteries of the lungs, called a pulmonary embolism.
- Have significant medical conditions that haven't been addressed.
- Have behavioral health conditions that haven't been addressed.
- Have a condition that limits your ability to give your informed consent.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Stay Informed with LGBTQ+ health content.
Receive trusted health information and answers to your questions about sexual orientation, gender identity, transition, self-expression, and LGBTQ+ health topics. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing to our LGBTQ+ newsletter.
You will receive the first newsletter in your inbox shortly. This will include exclusive health content about the LGBTQ+ community from Mayo Clinic.
If you don't receive our email within 5 minutes, check your SPAM folder, then contact us at [email protected] .
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Research has found that feminizing hormone therapy can be safe and effective when delivered by a health care provider with expertise in transgender care. Talk to your health care provider about questions or concerns you have regarding the changes that will happen in your body as a result of feminizing hormone therapy.
Complications can include:
- Blood clots in a deep vein or in the lungs
- Heart problems
- High levels of triglycerides, a type of fat, in the blood
- High levels of potassium in the blood
- High levels of the hormone prolactin in the blood
- Nipple discharge
- Weight gain
- Infertility
- High blood pressure
- Type 2 diabetes
Evidence suggests that people who take feminizing hormone therapy may have an increased risk of breast cancer when compared to cisgender men — men whose gender identity aligns with societal norms related to their sex assigned at birth. But the risk is not greater than that of cisgender women.
To minimize risk, the goal for people taking feminizing hormone therapy is to keep hormone levels in the range that's typical for cisgender women.
Feminizing hormone therapy might limit your fertility. If possible, it's best to make decisions about fertility before starting treatment. The risk of permanent infertility increases with long-term use of hormones. That is particularly true for those who start hormone therapy before puberty begins. Even after stopping hormone therapy, your testicles might not recover enough to ensure conception without infertility treatment.
If you want to have biological children, talk to your health care provider about freezing your sperm before you start feminizing hormone therapy. That procedure is called sperm cryopreservation.
How you prepare
Before you start feminizing hormone therapy, your health care provider assesses your health. This helps address any medical conditions that might affect your treatment. The evaluation may include:
- A review of your personal and family medical history.
- A physical exam.
- A review of your vaccinations.
- Screening tests for some conditions and diseases.
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections.
- Discussion about sperm freezing and fertility.
You also might have a behavioral health evaluation by a provider with expertise in transgender health. The evaluation may assess:
- Gender identity.
- Gender dysphoria.
- Mental health concerns.
- Sexual health concerns.
- The impact of gender identity at work, at school, at home and in social settings.
- Risky behaviors, such as substance use or use of unapproved silicone injections, hormone therapy or supplements.
- Support from family, friends and caregivers.
- Your goals and expectations of treatment.
- Care planning and follow-up care.
People younger than age 18, along with a parent or guardian, should see a medical care provider and a behavioral health provider with expertise in pediatric transgender health to discuss the risks and benefits of hormone therapy and gender transitioning in that age group.
What you can expect
You should start feminizing hormone therapy only after you've had a discussion of the risks and benefits as well as treatment alternatives with a health care provider who has expertise in transgender care. Make sure you understand what will happen and get answers to any questions you may have before you begin hormone therapy.
Feminizing hormone therapy typically begins by taking the medicine spironolactone (Aldactone). It blocks male sex hormone receptors — also called androgen receptors. This lowers the amount of testosterone the body makes.
About 4 to 8 weeks after you start taking spironolactone, you begin taking estrogen. This also lowers the amount of testosterone the body makes. And it triggers physical changes in the body that are caused by female hormones during puberty.
Estrogen can be taken several ways. They include a pill and a shot. There also are several forms of estrogen that are applied to the skin, including a cream, gel, spray and patch.
It is best not to take estrogen as a pill if you have a personal or family history of blood clots in a deep vein or in the lungs, a condition called venous thrombosis.
Another choice for feminizing hormone therapy is to take gonadotropin-releasing hormone (Gn-RH) analogs. They lower the amount of testosterone your body makes and might allow you to take lower doses of estrogen without the use of spironolactone. The disadvantage is that Gn-RH analogs usually are more expensive.
After you begin feminizing hormone therapy, you'll notice the following changes in your body over time:
- Fewer erections and a decrease in ejaculation. This will begin 1 to 3 months after treatment starts. The full effect will happen within 3 to 6 months.
- Less interest in sex. This also is called decreased libido. It will begin 1 to 3 months after you start treatment. You'll see the full effect within 1 to 2 years.
- Slower scalp hair loss. This will begin 1 to 3 months after treatment begins. The full effect will happen within 1 to 2 years.
- Breast development. This begins 3 to 6 months after treatment starts. The full effect happens within 2 to 3 years.
- Softer, less oily skin. This will begin 3 to 6 months after treatment starts. That's also when the full effect will happen.
- Smaller testicles. This also is called testicular atrophy. It begins 3 to 6 months after the start of treatment. You'll see the full effect within 2 to 3 years.
- Less muscle mass. This will begin 3 to 6 months after treatment starts. You'll see the full effect within 1 to 2 years.
- More body fat. This will begin 3 to 6 months after treatment starts. The full effect will happen within 2 to 5 years.
- Less facial and body hair growth. This will begin 6 to 12 months after treatment starts. The full effect happens within three years.
Some of the physical changes caused by feminizing hormone therapy can be reversed if you stop taking it. Others, such as breast development, cannot be reversed.
While on feminizing hormone therapy, you meet regularly with your health care provider to:
- Keep track of your physical changes.
- Monitor your hormone levels. Over time, your hormone dose may need to change to ensure you are taking the lowest dose necessary to get the physical effects that you want.
- Have blood tests to check for changes in your cholesterol, blood sugar, blood count, liver enzymes and electrolytes that could be caused by hormone therapy.
- Monitor your behavioral health.
You also need routine preventive care. Depending on your situation, this may include:
- Breast cancer screening. This should be done according to breast cancer screening recommendations for cisgender women your age.
- Prostate cancer screening. This should be done according to prostate cancer screening recommendations for cisgender men your age.
- Monitoring bone health. You should have bone density assessment according to the recommendations for cisgender women your age. You may need to take calcium and vitamin D supplements for bone health.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing hormone therapy care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/contents/search. Accessed Oct. 10, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Oct. 10, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming hormone therapy (adult). Mayo Clinic; 2022.
- Nippoldt TB (expert opinion). Mayo Clinic. Sept. 29, 2022.
- Gender dysphoria
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.
Gender reassignment surgery: an overview
Affiliation.
- 1 Gender Surgery Unit, Charing Cross Hospital, Imperial College NHS Trust, 179-183 Fulham Palace Road, London W6 8QZ, UK.
- PMID: 21487386
- DOI: 10.1038/nrurol.2011.46
Gender reassignment (which includes psychotherapy, hormonal therapy and surgery) has been demonstrated as the most effective treatment for patients affected by gender dysphoria (or gender identity disorder), in which patients do not recognize their gender (sexual identity) as matching their genetic and sexual characteristics. Gender reassignment surgery is a series of complex surgical procedures (genital and nongenital) performed for the treatment of gender dysphoria. Genital procedures performed for gender dysphoria, such as vaginoplasty, clitorolabioplasty, penectomy and orchidectomy in male-to-female transsexuals, and penile and scrotal reconstruction in female-to-male transsexuals, are the core procedures in gender reassignment surgery. Nongenital procedures, such as breast enlargement, mastectomy, facial feminization surgery, voice surgery, and other masculinization and feminization procedures complete the surgical treatment available. The World Professional Association for Transgender Health currently publishes and reviews guidelines and standards of care for patients affected by gender dysphoria, such as eligibility criteria for surgery. This article presents an overview of the genital and nongenital procedures available for both male-to-female and female-to-male gender reassignment.
Publication types
- Plastic Surgery Procedures / methods*
- Plastic Surgery Procedures / psychology
- Postoperative Complications / prevention & control
- Postoperative Complications / psychology
- Sex Reassignment Surgery / methods*
- Sex Reassignment Surgery / psychology
- Transsexualism / diagnosis
- Transsexualism / psychology
- Transsexualism / surgery*
- Open access
- Published: 25 April 2022
Patient reported outcomes in genital gender-affirming surgery: the time is now
- Nnenaya Agochukwu-Mmonu ORCID: orcid.org/0000-0003-4620-8897 1 , 2 ,
- Asa Radix 3 , 4 ,
- Lee Zhao 2 ,
- Danil Makarov 1 , 2 ,
- Rachel Bluebond-Langner 5 ,
- A. Mark Fendrick 6 , 7 ,
- Elijah Castle 1 , 2 &
- Carolyn Berry 2 , 3
Journal of Patient-Reported Outcomes volume 6 , Article number: 39 ( 2022 ) Cite this article
2898 Accesses
6 Citations
2 Altmetric
Metrics details
Transgender and non-binary (TGNB) individuals often experience gender dysphoria. TGNB individuals with gender dysphoria may undergo genital gender-affirming surgery including vaginoplasty, phalloplasty, or metoidioplasty so that their genitourinary anatomy is congruent with their experienced gender. Given decreasing social stigma and increasing coverage from private and public payers, there has been a rapid increase in genital gender-affirming surgery in the past few years. As the incidence of genital gender-affirming surgery increases, a concurrent increase in the development and utilization of patient reported outcome measurement tools is critical. To date, there is no systematic way to assess and measure patients’ perspectives on their surgeries nor is there a validated measure to capture patient reported outcomes for TGNB individuals undergoing genital gender-affirming surgery. Without a systematic way to assess and measure patients’ perspectives on their care, there may be fragmentation of care. This fragmentation may result in challenges to ensure patients’ goals are at the forefront of shared- decision making. As we aim to increase access to surgical care for TGNB individuals, it is important to ensure this care is patient-centered and high-quality. The development of patient-reported outcomes for patients undergoing genital gender-affirming surgery is the first step in ensuring high quality patient-centered care. Herein, we discuss the critical need for development of validated patient reported outcome measures for transgender and non-binary patients undergoing genital reconstruction. We also propose a model of patient-engaged patient reported outcome measure development.
Approximately 1 in every 200 US adults, roughly 1.4 million Americans, identify as transgender [ 1 ]. Some transgender and non-binary (TGNB) individuals experience gender dysphoria, which is discomfort, distress, physical, and psychological impairment that results from an incongruence between an individual’s gender identity and their sex assigned at birth [ 2 ]. TGNB individuals who experience gender dysphoria may seek medical and/or surgical interventions so that their physical features are congruent with their gender identity. In the past decade increased recognition of gender dysphoria, decreasing social stigma towards TGNB individuals, and increasing insurance coverage have led to a three-fold increase in gender-affirming surgeries [ 3 , 4 , 5 , 6 ]. Of gender-affirming surgeries, the incidence of genital gender-affirming surgery—vaginoplasty, phalloplasty and metoidioplasty—has steeply increased and is likely the most common inpatient gender-affirming surgery [ 7 ]. Although increased coverage has undoubtedly had many benefits for the TGNB community, to date, there have been few, if any, attempts to systematically assess patients’ perspectives on genital gender-affirming surgery. Without direct input from patients undergoing gender-affirming surgery, we cannot truly understand patients’ goals and preferences (e.g., sexual and aesthetic goals, quality of life) beyond amelioration of gender dysphoria, nor can we reliably assess the magnitude of benefits of gender-affirming surgery or prepare patients with realistic expectations of genital surgeries. Perhaps the most impactful result of a lack of explicit capture and incorporation of the patient perspective is the lack of shared decision-making and propagation of a paternalistic care model. This is evidenced by single-center studies, which have demonstrated evidence of decision-related regret and depending on an individuals’ goals, revision surgery [ 8 , 9 , 10 ]. There is also evidence that patients’ knowledge about outcomes after gender-affirming surgery is lacking and patients may have unrealistic expectations [ 11 ]. The current system of outcome reporting prioritizes clinical outcomes, which only captures physicians’ reports of outcomes, is subject to bias, does not include the patients’ perspective and, hence, are inadequate. The process of genital reconstruction is intensive and patients undertake significant risk to undergo life-changing genital gender-affirming surgery; there is an urgent need for patient-centered metrics. Patient reported outcome measures (PROMs) are patient-centered metrics and represent a viable solution to these challenges and shortcomings.
PROMs developed by and for TGNB patients undergoing genital gender-affirming surgery are imperative to delivering high-value, high-quality, patient-centered care. There has been an increased recognition of the importance of PROMs generally, with concurrent emphasis on the patient experience as a fundamental component of quality of care. PROMs as defined by the FDA are “measurement[s] based on a report that comes directly from the patient about the status of a patient’s health condition without amendment or interpretation of the patient’s response by a clinician or anyone else.” [ 12 ] PROMs are patient-generated and patient-centered health data, are measures of care delivery, evaluate patients’ symptoms, functional status, health related quality of life, satisfaction with care, and provide a holistic view of the patient experience [ 13 , 14 ]. While PROMs have traditionally been used as research tools, they are now recognized as meaningful clinical data elements, which may in certain instances be more accurate than those assessed by clinicians [ 15 , 16 ]. PROMs have been shown to support clinical improvements and positively impact patients in several fields [ 14 , 17 , 18 , 19 , 20 , 21 ]. In addition, preliminary data has demonstrated that PROMs may have an overwhelmingly positive impact in gender-affirming surgery as well [ 22 ]. Moreover, the TGNB community desires high-quality, long-term outcome data [ 23 ]. PROMs are especially necessary in reconstructive surgery given the challenge in evaluating short and long-term outcomes and quality. Reconstructive surgery is a complex journey for a patient and is purely patient-driven; PROMs will ensure that this journey is patient- centered at each step including the initial consultation, decision-making process, surgery, and perhaps most importantly, outcome reporting and measurement.
While wide agreement for the need for PROMs in gender-affirming care exists [ 24 , 25 ], there are many challenges to their development and implementation [ 26 ]. Questions such as how data should be most effectively collected, visualized, shared, and used to improve quality have limited the routine use of PROMs in clinical care [ 21 ]. Surmounting these challenges begins by considering the benefit of PROMs at the patient, provider, and system levels [ 27 ]. At the patient level, PROMs can help patients undergoing genital gender-affirming surgery develop realistic expectations. In addition, PROMs provide an opportunity to understand patients’ priorities and enable them to become fully informed about benefits, risks, and available options much earlier in the process of seeking genital gender-affirming surgery. The routine collection of PROMs for patients undergoing genital gender-affirming surgery and their utilization in clinical practice can facilitate the provision of a roadmap for patients at each step on this journey. Ultimately, counseling with the use of PROMs can inform patients’ decision regarding whether to have surgery and which surgery to have (e.g., metoidioplasty vs. phalloplasty).
At the provider level, there is evidence that PROMs improve patient and physician satisfaction, increase workflow efficiency, and enable critical discussions [ 28 ]. PROMs help enhance both patient and provider satisfaction by helping physicians set appropriate expectations regarding patients’ outcomes. PROMs can also improve relationships and communication between physicians and patients as surgeons gain better understanding of patients’ priorities and desired outcomes from surgery [ 28 ]. The availability and utilization of PROMs may greatly influence the success of surgery and potentially avoid the need for revision surgery, which is beneficial to the patient and the provider. The success of surgery is highly dependent on an individual patient’s values and preferences; a physicians’ definition of success may be highly divergent from a patients’ definition. PROMs magnify the individuals’ voice and thereby emphasize and facilitate, for the provider, a patient- centered model of care. This patient-centered model of care, facilitated in part by PROMs, portends higher chances of success for the patient. It also gives the surgeon and team an opportunity to understand what is important to their patients. The use of a PROM tool in this context may be a segue to the development and use of tools to measure patient reported experience measures as well, which would further improve patients’ experience of gender-affirming surgery [ 29 ].
Finally, at the system level, one can use PROMs as a quality metric [ 26 ]. Distinct from clinical outcomes, PROMs can be used to measure structures, processes, and outcomes of health care and thereby, can improve quality of care at each step and in several ways [ 30 ]. PROM data can be used to evaluate variation in patient care—specifically, variation in the “best” outcomes from the patient’s perspectives and subsequently, areas for quality improvement. This can thereby lead to modified processes to improve outcomes and quality. PROMs focus on the effectiveness and experience of care, both of which are essential components of quality. Incorporating PROMs facilitates shared decision-making, which also improves quality of care. Additionally, PROMs have the unique ability to capture two additional major components of clinical care provision and quality—provider accountability and performance measurement. The potential of collaborative quality improvement among providers in this setting is vast. At the policy level, PROMs are fundamental for a transition from volume to value-based healthcare reform. Validated PROMs may also contribute to advocacy efforts for wider coverage and policies that serve transgender and non-binary patients. In this context, validation is important and refers to a PROM tool, which measures what it intends to measure in the target population [ 12 ]. PROMs have been and are currently used in genital gender-affirming surgery research, though they are not validated for use in transgender and non-binary populations nor are they specific for genital gender-affirming surgery [ 25 ].
The primary role of PROMs is to capture the patients’ voice; given this, amplification of the patient’s voice at the forefront of PROM development is crucial. Figure 1 demonstrates a conceptual model for patient- engagement in PROM development; it is critical to have a conceptual framework to guide PRO measurement and assessment [ 31 ]. We plan to magnify the patients’ voices at each stage of development of PROMs for genital gender-affirming surgery. We propose early engagement with members of the transgender and non-binary communities in a Community-Based Participatory Research model. Engagement and collaboration with the TGNB community is fundamental in development of PROMs that are meaningful and relevant to the TGNB community and most importantly it will illuminate that which is often invisible—the patient perspective. Through engagement with LGBTQ community health centers, we are conducting focus group sessions for patients who will undergo or who have undergone phalloplasty, vaginoplasty, and metoidioplasty to gain a deep and detailed understanding of goals, experiences, quality of life, expectations, and aspirations. Qualitative analysis will then lead to convergent themes as depicted in Fig. 2 . Members of the transgender and non-binary community are leading or co-leading the focus group sessions. From initial discussions, dialogue, and thematic analysis, we will generate a pool of potential items for a PROM tool. This tool will then be rigorously vetted by the transgender and non-binary community members via a modified Delphi method, an iterative process whereby through data collection, analysis, and interpretation, the item pool is further modified with repeat in the cycle until there is agreement [ 32 ]. This enables and prioritizes PROMs that align with actual patient outcomes; this is divergent from the current outcome measurements, which prioritize surgical opinion. Only once agreement and homogeneity are reached amongst experts including TGNB focus group participants, TGNB community partners, qualitative researchers, and genital gender-affirming surgeons will decisions be made on items for the final tool, which would encompass domains (e.g., sexual, urinary, quality of life). This process will refine and finalize the tool which will then undergo rigorous validation testing. The final component of Figs. 1 and 2 depict the potential outcomes and areas of improvement from utilization of this PROM tool, including quality improvement, satisfaction, value, and shared decision making.
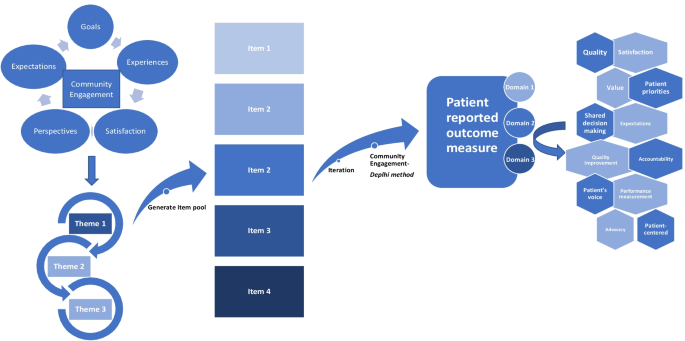
Patient-engaged conceptual model of patient reported outcome measure development
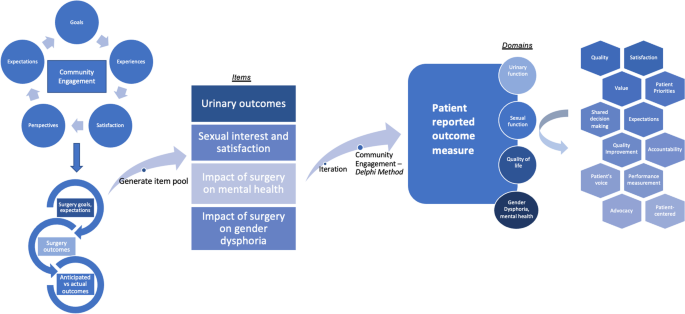
Potential themes, items, and domains resulting from community-based participatory research model of PROM tool development in genital gender-affirming surgery
PROMs for genital gender-affirming surgery are long overdue. Through intensive community engagement, we aim to develop PROMs with the transgender and non-binary community and inform the process of patient-centered care to serve transgender and non-binary patients. If surgeons who provide essential gender-affirming surgical care embrace the opportunity to be early adopters of PROMs, we can transform patient- centered care by making it a reality for transgender and non-binary patients.
Availability of data and materials
Not applicable.
Abbreviations
- Patient reported outcomes
Transgender and non-binary
Flores AR, Herman J, Gates GJ, Brown TNT (2016) How many adults identify as transgender in the United States?
Byne W, Karasic DH, Coleman E et al (2018) Gender dysphoria in adults: an overview and primer for psychiatrists. Transgend Health 3(1):57–70
Article Google Scholar
Dhejne C, Öberg K, Arver S, Landén M (2014) An analysis of all applications for sex reassignment surgery in Sweden, 1960–2010: prevalence, incidence, and regrets. Arch Sex Behav 43(8):1535–1545
Sutcliffe PA, Dixon S, Akehurst RL et al (2009) Evaluation of surgical procedures for sex reassignment: a systematic review. J Plast Reconstr Aesthet Surg 62(3):294–306 ( discussion 306-298 )
Article CAS Google Scholar
Berli JU, Knudson G, Fraser L et al (2017) What surgeons need to know about gender confirmation surgery when providing care for transgender individuals: a review. JAMA Surg 152(4):394–400
Colebunders B, Brondeel S, D’Arpa S, Hoebeke P, Monstrey S (2017) An update on the surgical treatment for transgender patients. Sex Med Rev 5(1):103–109
Canner JK, Harfouch O, Kodadek LM et al (2018) Temporal trends in gender-affirming surgery among transgender patients in the United States. JAMA Surg 153(7):609–616
Djordjevic ML, Bizic MR, Duisin D, Bouman MB, Buncamper M (2016) Reversal surgery in regretful male-to-female transsexuals after sex reassignment surgery. J Sex Med 13(6):1000–1007
Bodlund O, Kullgren G (1996) Transsexualism–general outcome and prognostic factors: a five-year follow-up study of nineteen transsexuals in the process of changing sex. Arch Sex Behav 25(3):303–316
Boas SR, Ascha M, Morrison SD et al (2019) Outcomes and predictors of revision labiaplasty and clitoroplasty after gender-affirming genital surgery. Plast Reconstr Surg 144(6):1451–1461
Frohard-Dourlent H, MacAulay M, Shannon M (2020) Experiences of surgery readiness assessments in British Columbia. Int J Transgend Health 21(2):147–162
(2006) Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes 4:79
Locklear TD, Hudson KE, Mularski RA, Hills MT, Cope EL, Wahba S, Zirkle M, Kripalani S, on behalf of the PCORnet PRO Task Force (2015) Reaching consensus on patient-centered definitions: a report from the patient-reported outcomes PCORnet Task Force
LeBlanc TW, Abernethy AP (2017) Patient-reported outcomes in cancer care—hearing the patient voice at greater volume. Nat Rev Clin Oncol 14(12):763–772
Basch E, Iasonos A, McDonough T et al (2006) Patient versus clinician symptom reporting using the National Cancer Institute common terminology criteria for adverse events: results of a questionnaire-based study. Lancet Oncol 7(11):903–909
Atkinson TM, Li Y, Coffey CW et al (2012) Reliability of adverse symptom event reporting by clinicians. Qual Life Res 21(7):1159–1164
Little P, Everitt H, Williamson I et al (2001) Preferences of patients for patient centred approach to consultation in primary care: observational study. BMJ 322(7284):468–472
Chang SS, Movsas B (2021) How vital are patient reported outcomes? J Natl Cancer Inst 114:347–348
Cappelleri JC, Stecher VJ (2008) An assessment of patient-reported outcomes for men with erectile dysfunction: Pfizer’s perspective. Int J Impot Res 20(4):343–357
Baradaran N, Hampson LA, Edwards TC, Voelzke BB, Breyer BN (2018) Patient-reported outcome measures in urethral reconstruction. Curr Urol Rep 19(7):48
Baumhauer JF (2017) Patient-reported outcomes—Are they living up to their potential? N Engl J Med 377(1):6–9
Massie JP, Morrison SD, Smith JR, Wilson SC, Satterwhite T (2017) Patient-reported outcomes in gender confirming surgery. Plast Reconstr Surg 140(1):236e–237e
Four corners: health research priorities among transgender and nonbinary communities (2021)
Barone M, Cogliandro A, Di Stefano N, Tambone V, Persichetti P (2017) A systematic review of patient-reported outcome measures following transsexual surgery. Aesthetic Plast Surg 41(3):700–713
Dy GW, Nolan IT, Hotaling J, Myers JB (2019) Patient reported outcome measures and quality of life assessment in genital gender confirming surgery. Transl Androl Urol 8(3):228–240
Squitieri L, Bozic KJ, Pusic AL (2017) The role of patient-reported outcome measures in value-based payment reform. Value Health 20(6):834–836
Basch E (2017) Patient-reported outcomes—harnessing patients’ voices to improve clinical care. N Engl J Med 376(2):105–108
Rotenstein LS, Huckman RS, Wagle NW (2017) Making patients and doctors happier—the potential of patient-reported outcomes. N Engl J Med 377(14):1309–1312
Black N, Varaganum M, Hutchings A (2014) Relationship between patient reported experience (PREMs) and patient reported outcomes (PROMs) in elective surgery. BMJ Qual Saf 23(7):534–542
Basch E, Spertus J, Dudley RA et al (2015) Methods for developing patient-reported outcome-based performance measures (PRO-PMs). Value Health 18(4):493–504
Rothman ML, Beltran P, Cappelleri JC, Lipscomb J, Teschendorf B (2007) Patient-reported outcomes: conceptual issues. Value Health 10(Suppl 2):S66-75
Powell C (2003) The Delphi technique: myths and realities. J Adv Nurs 41(4):376–382
Download references
Acknowledgements
We would like to thank members of the transgender and non-binary community for their partnership in this work.
The project described was supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number 2KL2TR001446-06A1 (NAM). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and affiliations.
Department of Urology, NYU School of Medicine, New York University, 221 East 41st Street, New York, NY, 10017, USA
Nnenaya Agochukwu-Mmonu, Danil Makarov & Elijah Castle
Department of Population Health, NYU School of Medicine, New York, NY, USA
Nnenaya Agochukwu-Mmonu, Lee Zhao, Danil Makarov, Elijah Castle & Carolyn Berry
Department of Medicine, NYU School of Medicine, New York, NY, USA
Asa Radix & Carolyn Berry
Callen-Lorde Community Health Center, New York, NY, USA
Department of Plastic and Reconstructive Surgery, NYU School of Medicine, New York, NY, USA
Rachel Bluebond-Langner
Department of Medicine, University of Michigan, Ann Arbor, MI, USA
A. Mark Fendrick
Department of Public Policy, University of Michigan, Ann Arbor, MI, USA
You can also search for this author in PubMed Google Scholar
Contributions
N.A.M., A.R., C.B.—original draft, all authors—editing and revising. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Nnenaya Agochukwu-Mmonu .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Agochukwu-Mmonu, N., Radix, A., Zhao, L. et al. Patient reported outcomes in genital gender-affirming surgery: the time is now. J Patient Rep Outcomes 6 , 39 (2022). https://doi.org/10.1186/s41687-022-00446-x
Download citation
Received : 08 June 2021
Accepted : 02 April 2022
Published : 25 April 2022
DOI : https://doi.org/10.1186/s41687-022-00446-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Gender-affirming surgery
- Vaginoplasty
- Metoidioplasty
- Phalloplasty
Treatment - Gender dysphoria
Treatment for gender dysphoria aims to help people live the way they want to, in their preferred gender identity or as non-binary.
What this means will vary from person to person, and is different for children, young people and adults. Waiting times for referral and treatment are currently long.
Treatment for children and young people
If your child may have gender dysphoria, they'll usually be referred to one of the NHS Children and Young People's Gender Services .
Your child or teenager will be seen by a multidisciplinary team including a:
- clinical psychologist
- child psychotherapist
- child and adolescent psychiatrist
- family therapist
- social worker
The team will carry out a detailed assessment, usually over 3 to 6 appointments over a period of several months.
Depending on the results of the assessment, options for children and teenagers include:
- family therapy
- individual child psychotherapy
- parental support or counselling
- group work for young people and their parents
- regular reviews to monitor gender identity development
- referral to a local Children and Young People's Mental Health Service (CYPMHS) for more serious emotional issues
Most treatments offered at this stage are psychological rather than medical. This is because in many cases gender variant behaviour or feelings disappear as children reach puberty.

Hormone therapy in children and young people
Some young people with lasting signs of gender dysphoria who meet strict criteria may be referred to a hormone specialist (consultant endocrinologist). This is in addition to psychological support.
Puberty blockers and gender-affirming hormones
Puberty blockers (gonadotrophin-releasing hormone analogues) are not available to children and young people for gender incongruence or gender dysphoria because there is not enough evidence of safety and clinical effectiveness.
From around the age of 16, young people with a diagnosis of gender incongruence or gender dysphoria who meet various clinical criteria may be given gender-affirming hormones alongside psychosocial and psychological support.
These hormones cause some irreversible changes, such as:
- breast development (caused by taking oestrogen)
- breaking or deepening of the voice (caused by taking testosterone)
Long-term gender-affirming hormone treatment may cause temporary or even permanent infertility.
However, as gender-affirming hormones affect people differently, they should not be considered a reliable form of contraception.
There is some uncertainty about the risks of long-term gender-affirming hormone treatment.
Children, young people and their families are strongly discouraged from getting puberty blockers or gender-affirming hormones from unregulated sources or online providers that are not regulated by UK regulatory bodies.
Transition to adult gender identity services
Young people aged 17 or older may be seen in an adult gender identity clinic or be referred to one from a children and young people's gender service.
By this age, a teenager and the clinic team may be more confident about confirming a diagnosis of gender dysphoria. If desired, steps can be taken to more permanent treatments that fit with the chosen gender identity or as non-binary.
Treatment for adults
Adults who think they may have gender dysphoria should be referred to a gender dysphoria clinic (GDC).
Find an NHS gender dysphoria clinic in England .
GDCs have a multidisciplinary team of healthcare professionals, who offer ongoing assessments, treatments, support and advice, including:
- psychological support, such as counselling
- cross-sex hormone therapy
- speech and language therapy (voice therapy) to help you sound more typical of your gender identity
For some people, support and advice from the clinic are all they need to feel comfortable with their gender identity. Others will need more extensive treatment.
Hormone therapy for adults
The aim of hormone therapy is to make you more comfortable with yourself, both in terms of physical appearance and how you feel. The hormones usually need to be taken for the rest of your life, even if you have gender surgery.
It's important to remember that hormone therapy is only one of the treatments for gender dysphoria. Others include voice therapy and psychological support. The decision to have hormone therapy will be taken after a discussion between you and your clinic team.
In general, people wanting masculinisation usually take testosterone and people after feminisation usually take oestrogen.
Both usually have the additional effect of suppressing the release of "unwanted" hormones from the testes or ovaries.
Whatever hormone therapy is used, it can take several months for hormone therapy to be effective, which can be frustrating.
It's also important to remember what it cannot change, such as your height or how wide or narrow your shoulders are.
The effectiveness of hormone therapy is also limited by factors unique to the individual (such as genetic factors) that cannot be overcome simply by adjusting the dose.
Find out how to save money on prescriptions for hormone therapy medicines with a prescription prepayment certificate .
Risks of hormone therapy
There is some uncertainty about the risks of long-term cross-sex hormone treatment. The clinic will discuss these with you and the importance of regular monitoring blood tests with your GP.
The most common risks or side effects include:
- blood clots
- weight gain
- dyslipidaemia (abnormal levels of fat in the blood)
- elevated liver enzymes
- polycythaemia (high concentration of red blood cells)
- hair loss or balding (androgenic alopecia)
There are other risks if you're taking hormones bought over the internet or from unregulated sources. It's strongly recommended you avoid these.
Long-term cross-sex hormone treatment may also lead, eventually, to infertility, even if treatment is stopped.
The GP can help you with advice about gamete storage. This is the harvesting and storing of eggs or sperm for your future use.
Gamete storage is sometimes available on the NHS. It cannot be provided by the gender dysphoria clinic.
Read more about fertility preservation on the HFEA website.
Surgery for adults
Some people may decide to have surgery to permanently alter body parts associated with their biological sex.
Based on the recommendations of doctors at the gender dysphoria clinic, you will be referred to a surgeon outside the clinic who is an expert in this type of surgery.
In addition to you having socially transitioned to your preferred gender identity for at least a year before a referral is made for gender surgery, it is also advisable to:
- lose weight if you are overweight (BMI of 25 or over)
- have taken cross-sex hormones for some surgical procedures
It's also important that any long-term conditions, such as diabetes or high blood pressure, are well controlled.
Surgery for trans men
Common chest procedures for trans men (trans-masculine people) include:
- removal of both breasts (bilateral mastectomy) and associated chest reconstruction
- nipple repositioning
- dermal implant and tattoo
Gender surgery for trans men includes:
- construction of a penis (phalloplasty or metoidioplasty)
- construction of a scrotum (scrotoplasty) and testicular implants
- a penile implant
Removal of the womb (hysterectomy) and the ovaries and fallopian tubes (salpingo-oophorectomy) may also be considered.
Surgery for trans women
Gender surgery for trans women includes:
- removal of the testes (orchidectomy)
- removal of the penis (penectomy)
- construction of a vagina (vaginoplasty)
- construction of a vulva (vulvoplasty)
- construction of a clitoris (clitoroplasty)
Breast implants for trans women (trans-feminine people) are not routinely available on the NHS.
Facial feminisation surgery and hair transplants are not routinely available on the NHS.
As with all surgical procedures there can be complications. Your surgeon should discuss the risks and limitations of surgery with you before you consent to the procedure.
Life after transition
Whether you've had hormone therapy alone or combined with surgery, the aim is that you no longer have gender dysphoria and feel at ease with your identity.
Your health needs are the same as anyone else's with a few exceptions:
- you'll need lifelong monitoring of your hormone levels by your GP
- you'll still need contraception if you are sexually active and have not yet had any gender surgery
- you'll need to let your optician and dentist know if you're on hormone therapy as this may affect your treatment
- you may not be called for screening tests as you've changed your name on medical records – ask your GP to notify you for cervical and breast screening if you're a trans man with a cervix or breast tissue
- trans-feminine people with breast tissue (and registered with a GP as female) are routinely invited for breast screening from the ages of 50 up to 71
Find out more about screening for trans and non-binary people on GOV.UK.
NHS guidelines for gender dysphoria
NHS England has published what are known as service specifications that describe how clinical and medical care is offered to people with gender dysphoria:
- Non-surgical interventions for adults
- Surgical interventions for adults
- Interim service specification for specialist gender incongruence services for children and young people
Review of gender identity services
NHS England has commissioned an independent review of gender identity services for children and young people. The review will advise on any changes needed to the service specifications for children and young people.
Page last reviewed: 28 May 2020 Next review due: 28 May 2023
(855) 687-6227
1329 Cherry Way Dr, Suite 700, Gahanna, OH 43230, USA
1080 Beecher Crossing N, Suite A Gahanna, Ohio 43230 Fax: 855–687–6227

Home > Cosmetic Procedures > Body Contouring > Reverse Top Surgery
Reverse Top Surgery
Reverse top surgery: reclaiming your identity with midwest breast.
In the journey of self-discovery and self-acceptance, individuals may find themselves at various crossroads. For those who have previously undergone gender reassignment surgery but now seek to reclaim their original identity, reverse top surgery can provide peace of mind. In this blog post, we will explore the benefits of transgender surgery reversal, the procedure itself, and the support available through Midwest Breast & Aesthetic Surgery .
Understanding Reverse Top Surgery
Reverse top surgery, also known as detransitioning surgery, is a transformative process aimed at restoring physical appearance to align with one’s original gender identity. This procedure involves the reversal of chest-related modifications made during gender reassignment surgery. Reverse top surgery may be an option for those who have undergone male-to-female (MTF) top surgery and female-to-male (FTM) top surgery . Understanding the intricacies of this surgery is crucial for individuals considering detransitioning.
Many who are exploring gender reassignment reversal may wonder if top surgery is reversible, as feeling content with one’s appearance is essential for those who choose to transition or detransition. Reverse top surgery allows individuals to reclaim their authentic selves, offering a sense of congruence between their physical appearance and internal gender identity.
Detransitioning Surgery: What to Expect
Before reverse top surgery.
The choice to pursue detransitioning surgery is a big decision, so individuals will need to undergo thorough pre-operative preparations and consultations beforehand. This involves discussions with the surgical team to understand goals, expectations, and the specific steps involved in the process. This collaborative approach ensures a personalized and tailored experience.
Post-operative Care and Recovery Timeline
Post-surgery, a detailed care plan is essential for a smooth recovery. From managing discomfort to resuming daily activities, understanding the recovery journey is instrumental in preparing individuals for life after detransitioning surgery.
The recovery timeline after reverse top surgery can vary from person to person, and it’s essential to note that individual experiences may differ. However, here is a general overview of what individuals undergoing reverse top surgery can expect during the recovery process:
Immediate Postoperative Period (First Few Days to Weeks):
- In some cases, patients may stay in the hospital for a day or two immediately after the surgery, allowing medical professionals to monitor their initial recovery.
- Discomfort and pain are common during the initial days. Pain medication prescribed by the surgeon will help manage postoperative pain.
- Patients are advised to limit physical activity and movement during the first few days to weeks.
- Patients should carefully monitor their surgical sites for any signs of infection, excessive swelling, or unusual changes and report any concerns to their surgical team.
First Two Weeks:
- Patients typically have a follow-up appointment with the surgical team within the first week or two to assess initial healing and address any concerns.
- Proper wound care is crucial during this period. Patients may need to change dressings and keep the surgical sites clean as per the surgeon’s instructions.
- While some light activities may be permitted, heavy lifting and strenuous exercises are usually restricted during the initial weeks.
- Swelling and bruising gradually subside during this period, improving the overall appearance of the chest.
- Depending on the individual’s progress, they may gradually resume light activities and daily routines as their surgeon recommends.
- Patients are often advised on scar care, which may include the application of ointments or silicone sheets to promote optimal scar healing.
Weeks 6-12:
- With the surgeon’s approval, patients can begin to reintegrate more strenuous activities into their routine during this period.
- As the physical healing progresses, individuals may also experience emotional and psychological adjustments. Support from healthcare professionals, support groups, or therapists can be beneficial during this time.
Beyond 12 Weeks:
- While most physical healing occurs within the first few months, the complete resolution of swelling and the maturation of scars may take several months to a year.
- Patients continue to have follow-up visits with their surgical team to monitor long-term healing and address residual concerns.
- By this stage, patients should be able to resume all normal activities, including exercise and physical activities, in consultation with their surgeon.
Support and Resources: Choosing Midwest Breast for Your Surgery
With 30 years of combined expertise in gender affirmation surgery, Dr. Ergun Kocak, Dr. Pankaj Tiwari, and Dr. Santosh Kale are among Ohio’s most experienced and trusted reverse top surgeons. Our team performs hundreds of successful gender reassignment procedures each year, and we take pride in providing personalized care and achieving results that empower our patients on their transition journey, wherever it takes them.
Choosing Midwest Breast & Aesthetic Surgery means trusting a team who will be there every step of the way to guide you along your journey. We offer extensive patient resources to help prepare for surgery and life after surgery, including educational videos , patient stories , our podcast , and more.
Scheduling a Consultation
If you’re ready to begin your detransitioning surgery journey, contact our Ohio clinics to start the process. We’ll discuss your goals at your initial consultation and help you determine if reverse top surgery is right for you.
Related Procedures:

What to Expect During Tummy Tuck Surgery in Ohio

Bra-line Back Lift

Top Surgery
*The information available on this page was created to educate our patients. It is not an alternative for a formal consultation with a board-certified plastic and reconstructive surgeon. Individual results vary per patient. For more information, we strongly recommend scheduling a consultation with our doctors.
SCHEDULE A CONSULTATION

The Gender Reassignment Controversy
When people opt for surgery, are they satisfied with the outcome.
Posted March 16, 2018 | Reviewed by Ekua Hagan
In an age of increasing gender fluidity, it is surprising that so many find it difficult to accept the gender of their birth and take the drastic step of changing it through surgery. What are their motives? Are they satisfied with the outcome?
Gender may be the most important dimension of human variation, whether that is either desirable, or inevitable. In every society, male and female children are raised differently and acquire different expectations, and aspirations, for their work lives, emotional experiences, and leisure pursuits.
These differences may be shaped by how children are raised but gender reassignment, even early in life, is difficult, and problematic. Reassignment in adulthood is even more difficult.
Such efforts are of interest not just for medical reasons but also for the light they shed on gender differences.
The first effort at reassignment, by John Money, involved David Reimer whose penis was accidentally damaged at eight months due to a botched circumcision.
The Money Perspective
Money believed that while children are mostly born with unambiguous genitalia, their gender identity is neutral. He felt that which gender a child identifies with is determined primarily by how parents treat it and that parental views are shaped by the appearance of the genitals.
Accordingly, Money advised the parents to have the child surgically altered to resemble a female and raise it as “Brenda.” For many years, Money claimed that the reassignment had been a complete success. Such was his influence as a well-known Johns Hopkins gender researcher that his views came to be widely accepted by scholars and the general public.
Unfortunately for Brenda, the outcome was far from happy. When he was 14, Reimer began the process of reassignment to being a male. As an adult, he married a woman but depression and drug abuse ensued, culminating in suicide at the age of 38 (1).
Money's ideas about gender identity were forcefully challenged by Paul McHugh (2), a leading psychiatrist at the same institution as Money. The brunt of this challenge came from an analysis of gender reassignment cases in terms of both motivation and outcomes.
Adult Reassignment Surgery Motivation
Why do people (predominantly men) seek surgical reassignment (as a woman)? In a controversial take, McHugh argued that there are two main motives.
In one category fall homosexual men who are morally uncomfortable about their orientation and see reassignment as a way of solving the problem. If they are actually women, sexual interactions with men get redefined as heterosexual.
McHugh argued that many of the others seeking reassignment are cross-dressers. These are heterosexual men who derive sexual pleasure from wearing women's clothing. According to McHugh, surgery is the logical extreme of identifying with a female identity through cross-dressing.
If his thesis is correct, McHugh denies that reassignment surgery is ever either medically necessary or ethically defensible. He feels that the surgeon is merely cooperating with delusional thinking. It is analogous to providing liposuction treatment for an anorexic who is extremely slender but believes themselves to be overweight.
To bolster his case, McHugh looked at the clinical outcomes for gender reassignment surgeries.
Adult Reassignment Results
Anecdotally, the first hurdle for reassignment is how the result is perceived by others. This problem is familiar to anyone who looked at Dustin Hoffman's depiction of a woman ( Tootsie ). Diligent as the actor was in his preparation, his character looked masculine.
For male-to-female transsexuals, the toughest audience to convince is women. As McHugh reported, one of his female colleagues said: “Gals know gals, and that's a guy.”
According to McHugh, although transsexuals did not regret their surgery, there were little or no psychological benefits:
“They had much the same problems with relationships, work, and emotions, as before. The hope that they would emerge now from their emotional difficulties to flourish psychologically had not been fulfilled (2)”.

Thanks to McHugh's influence, gender reassignment surgeries were halted at Johns Hopkins. The surgeries were resumed, however, and are now carried out in many hospitals here and around the world.
What changed? One likely influence was the rise of the gay rights movement that now includes transgender people under its umbrella and has made many political strides in work and family.
McHugh's views are associated with the religious right-wing that has lost ground in this area.
Transgender surgery is now covered by medical insurance reflecting more positive views of the psychological benefits.
Aspirational Surgery
Why do people who are born as males want to be women? Why do females want to be men? There seems to be no easy biological explanation for the transgender phenomenon (2).
Transgender people commonly report a lifelong sense that they feel different from their biological category and express satisfaction after surgery (now called gender affirmation) that permits them to be who they really are.
The motivation for surgical change is thus aspirational rather than medical, as is true of most cosmetic surgery also. Following surgery, patients report lower gender dysphoria and improved sexual relationships (3).
All surgeries have potential costs, however. According to a Swedish study of 324 patients (3, 41 percent of whom were born female) surgery was associated with “considerably higher risks for mortality, suicidal behavior, and psychiatric morbidity than the general population.”
1 Blumberg, M. S. (2005). Basic instinct: The genesis of behavior. New York: Thunder's Mouth Press.
2 McHugh, P. R. (1995). Witches, multiple personalities, and other psychiatric artifacts. Nature Medicine, 1, 110-114.
3 Dhejne, S., Lichtenstein, P., Boman, M., et al. (2011). Long-term follow-up of transsexual persons undergoing sex reassignment surgery: Cohort study of Sweden . Plos One.

Nigel Barber, Ph.D., is an evolutionary psychologist as well as the author of Why Parents Matter and The Science of Romance , among other books.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience

Sex reassignment in minors may be medical history’s ‘greatest ethical scandal’, French report says

Ron DeSantis just signed a bill barring Florida kids under 14 from using TikTok, SnapChat, and Instagram

Girl, 8, who drowned after being sucked into ‘malfunctioning’ pipe at hotel pool identified

Jon Stewart Breaks Down Why Trump’s Brazen Fraud Is No ‘Victimless’ Crime

Togo adopts new constitution, parliament set to elect president

Meet Simon Harris, Ireland’s first TikTok prime minister

Former Lifelong Democrat Elon Musk: ‘We Need a Red Wave or America Is Toast’

Donald Trump says time for Israel to ‘finish up’ Gaza war

UK Pledges £350 Million For Nuclear Defense and Energy By 2030

Hawks stage 30-point comeback to stun Celtics

There Is No Easy Way to Go Public About Cancer

Garbage AI posts like Shrimp Jesus are destroying Facebook

Hong Kongers Now Only Whisper About Freedom
- Environment

French Senators want to ban gender transition treatments for under-18s, after a report described sex reassignment in minors as potentially “one of the greatest ethical scandals in the history of medicine”.
The report, commissioned by the opposition centre-Right Les Republicains (LR) party, documents various practices by health professionals, which it claims are indoctrinated by a “trans-affirmative” ideology under the sway of experienced trans-activist associations.
The report, which cites a “ tense scientific and medical debate ”, accuses such associations of encouraging gender transition in minors via intense propaganda campaigns on social media.
Jacqueline Eustache-Brinio, an LR senator who led the working group behind the report, concluded that “fashion plays a big role” in the rise of gender reassignment treatments.
If this factor and the risks involved are underestimated, she added, “the sexual transition of young people will be considered as one of the greatest ethical scandals in the history of medicine”.
LR senators now want to table a Bill by the summer that would effectively ban the medical transition of minors in France by halting the prescription or administration of puberty blockers and hormones to people under the age of 18.
Sex reassignment surgery could also be banned for minors.
Reacting to the report, Ypomoni, a French parents’ group, said: “We welcome this return to reason.”
Maud Vasselle, a mother whose daughter underwent gender transition treatment, told Le Figaro: “A child is not old enough to ask to have her body altered.
“My daughter just needed the certificate of a psychiatrist, which she obtained after a one-hour consultation. But doctors don’t explain the consequences of puberty blockers,” she added.
“My daughter didn’t realise that life wasn’t going to be so easy with all these treatments… She was a brilliant little girl but now she’s failing at school. And she is far from having found the solution to her problems.”
Shocking and ideological
Transgender activists and certain health professionals expressed alarm at the report.
Clément Moreau, the clinical psychologist and coordinator of the mental health unit of the association Espace Santé Trans (Trans Health Space), said the report was “shocking” and called the move “ideological”.
“Using blockers if necessary or hormones before coming of age reduces the rate of suicidality, depression and anxiety,” he added.
The French report comes after the NHS banned children from receiving puberty blockers on prescription earlier this month.
France’s health regulation body, the Haute Autorité de Santé, was already examining a similar move.
The LR senators want to accelerate the process following the report.
Citing British, Swedish and American studies, the report said that the number of children identifying themselves as trans has exploded over the past decade.
One hospital in Paris receives around 40 new requests from minors every year, with 16 per cent of those under the age of 12 and the report points out that many suffer from other issues.
A quarter of the children seen at the Pitié-Salpêtrière Hospital for gender dysphoria have dropped out of school, 42 per cent have been victims of harassment, and 61 per cent have experienced an episode of depression. One in five has attempted suicide.
Their conclusions are in line with those of British experts called in to investigate London’s Tavistock clinic over its use of mass gender reassignment surgery on minors.
David Bell. a British psychiatrist and psychoanalyst, found that a third of the children consulted at the Tavistock suffered from autistic disorders, and many were victims of family violence or had difficulty in accepting or expressing homosexuality, yet they were rushed into gender transition regardless.
The post Sex reassignment in minors may be medical history’s ‘greatest ethical scandal’, French report says appeared first on The Telegraph .
Trending Posts

It’s time to hit Amazon where it really hurts: In its pocket

Rachel Maddow Speaks Out on NBC Hiring Ronna McDaniel

GREG GUTFELD: Angry, hyper-liberal women in the Bay Area are scaring off what would be their best partners

‘Safety, safety, safety’: Boeing shakes up leadership in bid to stem crisis

New York City to Give Migrant Families Debit Cards for Food, Baby Supplies
Copyright © 2023.
Site Navigation
- Privacy & Policy
Privacy Overview

This State Just Outlawed Gender Reassignment Surgery on Children

Republican Gov. Mark Gordon (R-WYo.) signed a series of bills banning gender reassignment surgery on minors. However, he rejected a bill that would have elevated significant barriers to abortion,
On Friday, Gordon signed the “Children gender change prohibition," legislation into law, which bans physicians from performing gender-reassignment procedures on children and administering such medications that would alter their body chemistry.
"I signed SF99 because I support the protections this bill includes for children, however, it is my belief that the government is straying into the personal affairs of families," Gordon said in a statement. "Our legislature needs to sort out its intentions with regard to parental rights. While it inserts governmental prerogative in some places, it affirms parental rights in others."
The law will prohibit any “surgery that sterilizes the child, including castration, vasectomy, hysterectomy, oophorectomy, metoidioplasty, orchiectomy, penectomy, phalloplasty and vaginoplasty."
It will also ban related prescription drugs “that induce transient or permanent infertility," or are considered a “puberty suppression or blocking prescription drugs to stop or delay normal puberty."
Recommended

However, Gordon vetoed the “Regulation of abortions” bill, which would have placed further restrictions on abortions in the state.
The legislation would have "properly regulated surgical abortion clinics in Wyoming," however, the governor noted that the "amendments to the bill complicated its purpose, making it vulnerable to legal challenges."
“It is my opinion that HB148, as amended, had the potential to further delay the resolution of this critical issue for the unborn," Gordon said in the statement. "The potential of starting over on a new course of legal arguments would in my mind be derelict, and would have only sacrificed additional unborn lives in Wyoming."
The bill would have classified abortion clinics as a “ambulatory surgical center.”

Trending on Townhall Videos
- America Is Going to Be Targeted for a Massive Terrorist Attack...Will You Be Ready?
- John Kirby Turns to Delusional Responses As Netanyahu Calls Off Talks
- My Wife's Black Anesthesiologist Wasn't an Affirmative Action Hire
- Did Tim Kaine Offer the Worst Answer on the Border Crisis?

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Biomed Res Int

Gender Dysphoria: Bioethical Aspects of Medical Treatment
Marta r. bizic.
1 Belgrade Center for Genital Reconstructive Surgery, Serbia
2 University Children's Hospital, Belgrade, Serbia
Milos Jeftovic
3 School of Medicine, University of Belgrade, Serbia
Slavica Pusica
Borko stojanovic, dragana duisin, svetlana vujovic, vojin rakic.
4 Center for the Study of Bioethics, University of Belgrade, Serbia
Miroslav L. Djordjevic
Gender affirmation surgery remains one of the greatest challenges in transgender medicine. In recent years, there have been continuous discussions on bioethical aspects in the treatment of persons with gender dysphoria. Gender reassignment is a difficult process, including not only hormonal treatment with possible surgery but also social discrimination and stigma. There is a great variety between countries in specified tasks involved in gender reassignment, and a complex combination of medical treatment and legal paperwork is required in most cases. The most frequent bioethical questions in transgender medicine pertain to the optimal treatment of adolescents, sterilization as a requirement for legal recognition, role of fertility and parenthood, and regret after gender reassignment. We review the recent literature with respect to any new information on bioethical aspects related to medical treatment of people with gender dysphoria.
1. Introduction
Gender dysphoria (GD) represents a condition where a person's gender assigned at birth and the gender with which they identify themselves are incongruent. Hence, these individuals can be very uncomfortable with their biological sex, primary and secondary sex characteristics, and social gender roles and they experience various levels of distress. Presence of public figures who are openly transgender, their appearance in mainstream media, and political and social climate lead to more individuals coming out in the open as to their state. Prevalence rate cannot be correctly estimated considering that people are still hesitant to come forward to health centers. According to DSM-5, the prevalence of gender dysphoria is 0.005-0.014% for adult natal males and 0.002-0.003% for adult natal females [ 1 ].
In accordance with their wishes, individuals with this condition can choose the direction in which their transition will proceed. To take the edge off their state, one can choose to go through a social transition. The social transition includes using a different name, pronouns, transformation of physical appearance, use of suitable bathrooms, and taking social roles of the affirmed gender. A more radical approach is the medical transition that includes hormonal and surgical treatment. Medical treatment requires a team of experienced experts, and it usually includes mental health professionals, endocrinologists, and surgeons. Psychiatric assessment is the first step and is very complex because it is necessary to exclude other conditions that might mimic gender dysphoria. The next step is hormonal treatment, under the care of an endocrinologist, which is then followed by “a real-life trial.” Some individuals decide to stop here, while others continue to gender-affirming surgery (GAS). The seventh edition of the Standards of Care of the World Professional Association of Transgender Health (WPATH) offers flexible guidelines for the treatment of people experiencing gender dysphoria and describes the criteria for surgical treatment [ 2 ]. Patients undergoing GAS of their choice are required to provide two recommendation letters from certified psychiatrists and a gender specialist, as well as a confirmation of having been on hormonal therapy prescribed by an endocrinologist for a period of a minimum of one year. Gender affirmation surgery refers to all surgical procedures that a patient wishes to undergo in an attempt to become as similar as possible to the desired gender.
Treatment of gender dysphoria always raised numerous ethical issues, and with rapid acknowledgment and recent achievements, new complex issues in medical management have emerged. With unknown etiology and questionable definition (mental/medical illness, social construct, and variation of sex) who can decide, with 100% certainty, what treatment is in the best interest of a particular patient? The most prominent challenges and ethical questions pertain to the treatment of underage individuals, fertility after GAS, and possibility of regret after GAS. Main ethical principles are autonomy, beneficence, nonmaleficence, and informed consent. The individual must have autonomy of thought and intention when making decisions about medical treatment. This is an especially sensitive field in treatment of gender dysphoria, because sometimes the individual's desires, hopes, and expectations might not correlate with reality. Experts must be very straightforward regarding specific possibilities, risks, and benefits of medical treatment, especially considering that the last step in medical transition, GAS, is irreversible. Beneficence implies doing only good, only what is in the patient's best interest. However, some may consider that surgical alteration of healthy organs, in case of GAS, is not in line with this principle. Nonmaleficence must ensure that the treatment does not harm the individual in an emotional, social, or physical sense. Always keeping these principles in mind, WPATH Standards of Care and criteria for diagnosis might not be enough to be ascertain that we are doing the right thing. Although it may seem that an individual fulfills all these criteria on paper, sometimes we can observe their personal disadvantages, youth, impairment, or desperation. It seems that, even with the reassurance and recommendation from a mental health professional, ethical unease cannot be entirely erased because treatment guidelines have preceded the answers to vitally relevant questions [ 3 , 4 ].
2. Transgender Youth
Children represent a small number of individuals with gender dysphoria and in only 10-20% of the children, gender dysphoria will continue to manifest in adolescence [ 5 ]. However, psychological therapy and support are highly recommended; while such services are now far more widely available, they are still insufficient to provide for complete wellbeing of these patients. Inadequate management of children with persistent gender dysphoria can lead to isolation, feeling of self-hatred, and suicidal ideas and attempts. Also, “passing through the wrong puberty” can have serious consequences for these individuals. Viable treatment options vary from fully reversible treatment, such as puberty-suppressing gonadotropin-releasing hormone analogues (GnRH) to partly reversible treatment, gonadal steroid treatment, as well as irreversible treatment, such as surgical removal of genitalia and reconstruction of new ones according to the desired gender. Surgery includes bilateral mastectomy with chest reconstruction, hysterectomy with oophorectomy followed by either metoidioplasty or phalloplasty for trans-male individuals, and bilateral orchiectomy with penectomy followed by vulvoplasty and vaginoplasty in trans-female individuals [ 6 ].
Pubertal suppression is implemented using GnRH analogues at Tanner 2 or 3 stage of puberty. Hypothalamus produces GnRH at low levels in prepubertal children. Levels become cyclical during puberty, leading to the production of luteinizing hormone (LH) and follicle stimulating hormone (FSH) by the anterior pituitary. LH and FSH stimulate ovaries and testicles to produce sex hormones, estrogen and testosterone, which are responsible for stimulating the growth of genitalia. Also, they lead to the development of breasts, voice deepening, menstrual cycle, and so forth, which transgender youth can find particularly tough to handle [ 7 ].
There are only a few reports related to the use of GnRH analogues in transgender youth. De Vries et al. were the first to introduce the concept and research on the use of puberty blockers for treatment of transgender youth. The main idea behind the suppression of endogenous puberty was to decrease distress by preventing the development of “noncongruent” secondary sexual characteristics. This would give young individuals more time to get accustomed to their situation and to better explore their gender. In the examined group, all of 70 eligible candidates showed improved mental health and general functioning. Authors concluded that the treatment was fully reversible, which was one of its main advantages [ 8 ]. Despite the positive outcomes in puberty suppression, many experts still have concerns and resist the implementation of this treatment in their regular practice. Viner et al. proposed that GnRH therapy can be physically damaging for teenagers and can lead to unfavorable psychological consequences [ 9 ]. Olson-Kennedy et al. also recognized these dilemmas, stating that available data on puberty suppression was limited and many questions remained unanswered [ 10 ]. One of the main reasons against this treatment is that going through puberty may help the individual to become congruent with their biological sex, meaning that their GD would not persist into adolescence. Results from Steensma et al. showed that majority of children developed homosexual orientation after completion of the GnRH treatment [ 11 ]. As for potential consequences, Hembree recently reported no long-term consequences in follow-up studies of GnRH treatment [ 12 ].
Finally, the decision about implementing GnRH treatment is very difficult and cannot be made without ethical dilemmas. Both opponents and advocates of pubertal suppression are guided by the same ethical principles, beneficence, nonmaleficence, and autonomy, but have different views on where these principles lead. A unique and clear overview is necessary, and, to this day, it has not yet been elaborated. Considering that GnRH treatment is relatively new and controversial, additional qualitative research and empirical studies are necessary for appropriate bioethical definitions.
Transgender persons require safe and effective hormonal support to develop the physical characteristics that affirm their gender identity. The main indications for the beginning of hormonal therapy are confirmed persistence of gender dysphoria and adequate mental capacity to give informed consent and accept this partially irreversible treatment. According to the most recent Endocrine Society guidelines, most adolescents develop this capacity by the age of 16 [ 12 ]. Also, Hembree et al. recognized some compelling reasons to initiate sex hormonal therapy before 16, but there is little data published on the experiences with this treatment prior to 14 years of age [ 12 ]. The main goals of cross-sex hormonal therapy are suppression of endogenous sex hormone secretion, determined by the person's genetic/gonadal sex, and maintaining sex hormone levels within the normal range for the person's affirmed gender. This therapy harmonizes the external appearance with affirmed gender, leading to, in transgender men, male-sounding voice, different fat distribution, increase in muscle mass and, in transgender women, breast growth, decreased facial and body hair, more feminine fat redistribution, and decreased muscle mass [ 12 ].
Many studies demonstrated long-term safety and high efficiency of hormonal therapy in transgender adults. For trans-women, Asscheman et al. emphasized a warning to a side effect of particular concern, estrogen-induced hypercoagulability and subsequent venous thromboembolism. Hembree addressed some potential adverse physical effects of testosterone treatment, such as polycythemia vera and dyslipidemia, in transgender men. Generally, a majority of the authors concluded that this therapy was safe, with necessary follow-up for potential complications [ 12 – 14 ]. However, only a few studies looked into the impact of cross-sex hormonal therapy on transgender youth. Jarin et al. performed a retrospective study on 116 adolescents aged 14–25 years with gender dysphoria and have reported minimal impact of hormone treatment. In trans-men, the only findings were an increase in hemoglobin, hematocrit, and body mass index with lowering of high-density lipoprotein levels; in trans-women, only lower testosterone and alanine aminotransferase (ALT) were reported [ 15 ]. Olson-Kennedy et al., in their prospective study, found several statistically significant changes in mean values of physiological parameters over time but of no consequence to clinical safety concerns [ 16 ]. In both studies, the authors indicated that this cross-sex hormonal therapy is safe for transgender youth over a period of approximately two years. However, the strongest argument against cross-sex therapy lies in the lack of knowledge of its long-term effects, which means that more studies and follow-up information are necessary. One of the questions is a possibility for cross-sex hormonal therapy in individuals below 16 years of age. The authors of the latest guidelines of the Endocrine Society recognized this possibility but only on a “case by case” principle, meaning that age does not always accurately reflect one's readiness for medical interventions. Also, some experts noticed that a clear majority of children on GnRH therapy will decide to pursue cross-sex hormonal therapy. Only a few side effects of using GnRH were observed, such as decreased bone density [ 17 ].
Based on bioethical principles, children usually do not have the power to make legal decisions and actions at the initiation of cross-hormonal therapy. Nevertheless, their judgment and opinions should not be disregarded. Cross-sex therapy primarily helps individuals with GD to harmonize their external appearance with their experienced gender. In this case, proper education of the patient and pointing out advantages and shortcomings of such treatment are of crucial importance. Following the principle of beneficence, clinicians are always obliged to help the person and to follow the prescribed hormonal treatment, since there are no better options at this moment. Patients who are denied treatment can develop serious psychological consequences. Generally, the transgender population is at higher risk of self-harm and suicide [ 18 ]. A more individualized approach, as in the “case by case” system, will ensure that a right decision is made in accordance with the patient's maturity, age, and judgment.
Gender affirmation surgery is the last step in the medical transition. It is considered to be irreversible and is technically demanding to perform, even for experienced surgeons. According to WPATH Standards of Care, a criterion for eligibility for GAS is “reached legal age of maturity in a given country.” Presumably, the threshold is 18 years of age in most countries [ 19 ]. The increasing usage of puberty blockers and pushing the limits for the start of the cross-sex hormone therapy lead to further problems and dilemmas. With these developments, it was only a matter of time before the issue of GAS in minors would arise. Viewpoints are different and vary between the beneficence principle embodied in the motto “doing nothing is doing harm” and the nonmaleficence variation of “the treatment plan that involves less extensive surgery or none at all,” reported by Cohen-Kettenis and Holman, respectively [ 20 , 21 ].
Changing the legislation for hormonal therapy without GAS increases the gap between the two medical procedures and postpones the desired outcome of the transition. During this interim period, someone living with atypical genitalia can easily be exposed in public and lose control over something that used to be very private [ 22 ]. Transgender community is more often targeted by bullying and has higher rates of suicide. Leaving these patients to wait for the final stage in their transition can have an impact on their social and psychological state. Goffman's theory of stigma postulates that the transitioning adolescents must prove their affirmed gender to others [ 23 ]. If others question the individual's gender identity, including the presence of gender-congruent genitals, he or she fails to manage the stigma and becomes “discredited.” In addition, postponing romantic relationships and dating until the age of 18 can also lead to psychological struggles and challenges.
On the other hand, the main “technical” issue in case of children treated with puberty blockers lies in their undeveloped genitalia. Thus, the GAS will be more troublesome, especially in case of penile inversion vaginoplasty. Some authors reported autologous skin grafting from donor site or use of bowel segments as viable solutions for this issue [ 24 , 25 ]. However, the main concern is the possibility of regret after the GAS. As already mentioned in Introduction, GD does not persist through adolescence in the vast majority of children. The results of GAS in transgender minors and their possible regret are a great cause of concern and a huge responsibility for medical professionals [ 26 ]. The dilemmas remain: is it better to suffer the consequences of GD or GAS? Are children or teenagers mature enough to make these kinds of decisions? Further research and data are necessary to resolve these crucial dilemmas.
3. Fertility
Treatment of GD enables the individuals to continue their life in their affirmed gender. For some transgender individuals, this implies the same as for cisgender persons, marriage or/and children. Members of the transgender population have the same desire for offspring, for the same reasons as the cisgender population, and fertility presents one of the most delicate issues. Infertility in trans-women is caused by orchiectomy as a part of the GAS. Conversely, hysterectomy and oophorectomy eliminate the chance of pregnancy in trans-men. Cross-sex hormonal therapy also has an impact on fertility, but such treatment is not a definitive cause of infertility, due to the possibility of reversal. Three decades ago, Payer described that estrogen in trans-women leads to the reduction of testicular volume and has a strong suppressive effect on sperm motility and density [ 27 ]. Testosterone therapy for trans-men leads to reversible amenorrhea according to Van Den Broecke's study in 2001 [ 28 ]. Patients are usually at full reproductive age at the initiation of their transition and a clear majority of them express the desire for reproductive potential after transition [ 29 , 30 ]. This is almost impossible, as irreversible transition means losing the option for having children. Dunne reviewed sterilization requirements for transgender people in Europe and found sterilization as the only possible option in 20 European countries; this means that any chance for biological offspring is lost with this transition [ 31 ]. This discrimination deeply undermines the fundamental bioethics law, and societies such as WPATH and the Endocrine Society advocate for counseling and detailed explanation of the consequences of treatment and viable options for fertility preservation. In addition, the possibility of sterility following the use of puberty blockers and cross-sex hormones gives rise to further controversy and ethical dilemmas, as do options of cryopreservation prior to the start of cross-sex hormonal therapy and uterus transplantation for trans-women.
As we have previously mentioned, puberty blockers are considered to be the reversible part of the transition, preventing secondary sex characteristics from developing. However, some authors confirmed that these blockers also have an impact on maturation of germ cells, which could be used for preservation of the biological fertility potential [ 32 ]. Individuals on puberty suppression therapy may show an interest in offspring but, at the same time, may not want to pass through the wrong puberty in the gender assigned at birth. Thus, their options for offspring are very limited, since prepubertal cryopreservation is still in the experimental stages [ 33 ]. There are other questions as well, including their maturity for making these kinds of decisions and the responsibility of their parents as legal guardians. In the literature, a few authors reported the desire of transgender people to have children and found that about half of both trans-men and trans-women wanted offspring after transition [ 29 , 34 ].
Cryopreservation of embryos, oocytes, or ovarian tissue is a viable option for trans-men. Some authors recommend cryopreservation just before initiation of hormonal transition due to the possibility that cross-sex hormone therapy might cause amenorrhea or affect follicle growth. In cases where the hormonal transition has already started, they suggest an interruption of hormone treatment for minimum 3 months with a goal to revert any potential therapy-induced effects [ 35 ]. These could be very aggravating facts, since other doctors reported that majority of transgender individuals did not want to postpone their transition for these procedures. Interestingly, Wallace et al. noticed that transvaginal ultrasound examination, as a necessary part for cryopreservation of embryos and oocytes, is not always in accordance with individuals' male identity and can lead to distress [ 36 ].
Sperm cryopreservation, surgical sperm extraction, and testicular tissue cryopreservation could be offered as possibilities for preserving fertility in trans-women. The issues with hormonal therapy exist in this case, too. De Sutter et al. described additional distress, caused by masturbating in clinical settings or sperm banking as a reminder of their former gender [ 34 ].
In some countries, cryopreservation is not technically available to the transgender population and thus cannot be offered during the transition. Despite the fact that cryopreservation is a routine procedure in case of malignant diseases, it still remains a controversial topic in less economically developed countries.
In some countries, like USA, sterilization is not mandatory and trans-men can keep their ovaries and uterus for later pregnancy. They must discontinue cross-sex therapy in this period. Light et al. described transgender pregnancies and challenges that come with this phenomenon [ 37 ]. Conversely, pregnancy is still not an option for trans-women. There is hope on the horizon from the first successful uterus transplantation, performed by a gynecology team from Sweden [ 38 ]. This is a solution for all women suffering from absolute uterine infertility who want to carry their own children. This procedure brings a new insight for researchers, making the possibility for transplantation in trans-women realistic. The main problems could arise from the different anatomy of the male pelvis, as well as from immunosuppressive therapy.
Fertility, including all the related issues and dilemmas, should be discussed very profoundly and meticulously. Transgender population should be informed about all possibilities, advantages, and drawbacks before any treatment and each option should ultimately be the patient's decision.
4. Regret and Revision Surgery
There are various levels of regret after GAS. Definite regret happens when the patient wants to get back to their gender assigned at birth after the GAS is performed. They come to surgeons with the request for the restitution of congenital anatomical features. Regret manifests with a more or less pronounced expression of dissatisfaction and second thoughts about the GAS. After suicide, regret could be considered one of the worst possible complications.
Reasons for regret vary greatly. Inadequate social adaptation, comorbidity with certain psychiatric disorders, poor psychological and psychiatric evaluation, and dissatisfaction with aesthetic or functional outcome of GAS can lead to regret. Researchers have concluded that the presence of the following factors can be associated with a risk of regret: age above 30 years at first surgery, personality disorders, social instability, dissatisfaction with surgical results, and poor support from partner or family [ 39 – 41 ].
In 2016, we published a retrospective analysis of seven patients who underwent reversal surgery after regretting undergoing male-to-female GAS elsewhere [ 42 ]. Main reasons for regret in these cases were related to inadequate psychiatric assessment. First stages of transition like the “real-life experience” were mostly skipped, cross-sex hormonal therapy was not carried out properly, and letters of recommendation were written by psychiatrists who lacked experience. Also, main diagnostic criteria for gender dysphoria had been neglected. It is therefore important to avoid situations where inadequately trained or inexperienced psychologists or psychiatrists work with transgender patients without supervision or collaboration with more experienced colleagues. Satisfying postoperative results were achieved in all patients. Reversal surgery significantly enhanced their general well-being.
Each regret occurrence represents a major issue for every expert in the field of transgender medicine. Proper diagnosis and listening to and monitoring our patients are of crucial importance for avoiding these kinds of mistakes [ 43 ]. Every physician should be aware that not all individuals suffering from GD want or need all three elements of therapy.
5. Conclusion
All physicians included in gender dysphoria treatment are facing great bioethical challenges and dilemmas. A multidisciplinary approach is necessary, but it does not always guarantee a successful outcome. The most sensitive issues are the treatment of transgender youth, fertility and parenting in transgender individuals, and the risk of regret after the irreversible part of the treatment, the gender affirmation surgery. In order to avoid the complex issue of regret, proper preoperative evaluation by experienced professionals, psychologists, and psychiatrists is necessary. More research and studies are necessary to shed light on these issues.
Acknowledgments
This work is supported by Ministry of Science and Technical Development, Republic of Serbia (Project no. 175048).
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this article.

Wyoming governor signs bill outlawing gender-reassignment procedures on children, vetoes abortion restrictions
Wyoming's Republican Governor Mark Gordon signed into legislation Friday a bill outlawing gender-reassignment procedures on children and vetoed a bill that would have imposed further restrictions on abortion clinics, including required licensure.
SF0099, also titled "Children gender change prohibition," prohibits physicians from performing gender-reassignment procedures on children and administering related medications. The legislation specifically banned "a surgery that sterilizes the child, including castration, vasectomy, hysterectomy, oophorectomy, metoidioplasty, orchiectomy, penectomy, phalloplasty and vaginoplasty."
The legislation continued on to specify that outlawed medications under the legislation included "any of the following prescription drugs that induce transient or permanent infertility," proceeded by a list of medications , including "puberty suppression or blocking prescription drugs to stop or delay normal puberty."
WYOMING JUDGE TO RULE ON ABORTION LAWS, INCLUDING THE FIRST-IN-THE-NATION BAN ON ABORTION PILLS
The bill also outlined various procedures that were exempt from the legislation, such as procedures or treatments performed on a child as a result of "a medically verifiable genetic disorder of sex development." The legislation specified that parental/guardian consent was required.
"I signed SF99 because I support the protections this bill includes for children, however, it is my belief that the government is straying into the personal affairs of families" Gordon said in a statement released. "Our legislature needs to sort out its intentions with regard to parental rights. While it inserts governmental prerogative in some places, it affirms parental rights in others."
READ ON THE FOX NEWS APP
TRUMP SUGGESTS HE WOULD SUPPORT ABORTION BAN AT AROUND 15 WEEKS OF PREGNANCY
Gordon also vetoed HB0148, known as "Regulation of abortions," that would have placed additional restrictions on abortion clinics in the state. The press release noted that the bill would have "properly regulated surgical abortion clinics in Wyoming," but "amendments to the bill complicated its purpose, making it vulnerable to legal challenges."
The legislation would have required a surgical abortion facility in the state to be licensed as "an ambulatory surgical center," and a facility conducting the procedures would need a separate license as well.
NEW STUDY FINDS WOMEN WHO CHOOSE SUPPORTIVE BIRTH SERVICES OVER ABORTION BENEFIT IN TRAGIC FETAL ANOMALY CASES
"It is my opinion that HB148, as amended, had the potential to further delay the resolution of this critical issue for the unborn," Gordon said in the statement. "The potential of starting over on a new course of legal arguments would in my mind be derelict, and would have only sacrificed additional unborn lives in Wyoming."
Abortion is currently legal in Wyoming, pending a court decision challenging the state's abortion laws.
On the national scale, the U.S. Supreme Court is set to hear oral arguments Tuesday about the federal government's approval process of the drug mifepristone, a medication used to terminate pregnancies. A ruling is expected about three months later.
The Supreme Court is currently allowing the FDA to continue regulating the drug while the appeals process plays out. Such regulation includes continued telemedicine prescriptions and retail pharmacy dispensing.
Fox News' Shannon Bream, Bill Mears and The Associated Press contributed to this report.
Original article source: Wyoming governor signs bill outlawing gender-reassignment procedures on children, vetoes abortion restrictions

- #donaldtrump
- #election2024
- #openthread
- #ronnamcdaniel
- #republicans
- #healthcare
- #vladimirputin
- #photography
- #environment
- #mikejohnson
Wyoming 24th State to Ban Gender Reassignment Surgery
What happened to the “preservation of life, and liberty, and the pursuit of happiness” in one-half of our United States? Wyoming just became the 24th state banning physicians from performing gender transitioning and gender reassignment procedures for children.
The law, recently signed by Republican Governor Mark Gordon, also penalizes pharmacists and other healthcare professionals for providing gender-affirming care to minors. These punishments include license revocation.
With SCOTUS overturning Roe vs Wade in 2022, the pernicious proliferation of book banning in America, and this draconian ukase in almost half the country, the US is deteriorating into the dreaded, dystopic Republic of Gilead Canadian Margaret Atwood warned us about decades ago in The Handmaid’s Tale .
Who is free to pursue what happiness with what liberty?
Sources: Wyoming governor signs bill banning gender reassignment surgery, care - UPI.com
www.cnn.com/...
Bias of United Press International
92% of our members expressed interest in funding our mission.
Become an Angel Investor Now

TRUST, restored. NEWS, balanced. DEMOCRACY, strengthened.

- Balanced News
- Story of the Week
- News Curation Principles
- Newsletters
- Balanced Search
Wyoming governor signs bill banning gender reassignment surgery, care

United Press International
Related Coverage

AllSides Picks

March 25th, 2024

Joan Blades
March 22nd, 2024

More News about Politics from the Left , Center and Right
From the left, from the center, from the right.

IMAGES
COMMENTS
Introduction: Sex reassignment surgery (SRS) has proved an effective intervention for patients with gender identity disorder. However, misdiagnosed patients sometimes regret their decision and request reversal surgery. This review is based on our experience with seven patients who regretted their decision to undergo male-to-female SRS.
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
This means that they freely expressed their regret toward the procedure, but some had role reversal to the former gender and others did not. ... Male-to-female sex reassignment surgery using the combined vaginoplasty technique: satisfaction of transgender patients with aesthetic, functional, and sexual outcomes. ...
In a review of 27 studies involving almost 8,000 teens and adults who had transgender surgeries, mostly in Europe, the U.S and Canada, 1% on average expressed regret. For some, regret was temporary, but a small number went on to have detransitioning or reversal surgeries, the 2021 review said. Research suggests that comprehensive psychological ...
As of 30 August, there were 213 patients on the list for gender reassignment surgery at Imperial College Healthcare NHS Trust. At present, there are no statistics regarding gender reversal ...
Overview. Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
If the respondents had experience with patients seeking reversal surgery, the number of such interventions were queried to include: the initial gender-affirming procedure and the patients' reason(s) for requesting reversal procedures. ... Thirty Years of International Follow-up Studies After Sex Reassignment Surgery: A Comprehensive Review ...
The Endocrine Society does not recommend genital surgery for minors. Before puberty, gender-affirming care is about supporting the process of gender development rather than directing children ...
The authors of the March 2021 Gender Affirming Surgery Mini-series article entitled "Regret after Gender-affirmation Surgery: A Systematic Review and Meta-analysis of Prevalence" (Plast Reconstr Surg Glob Open. 2021;9(3):e3477), wish to make the following corrections in the tables and figures.The systematic review was re-conducted, and the meta-analysis was re-run with the updated numbers ...
The effect of hormone therapy on fertility is potentially reversible, but the extent is unclear. Gender-affirming surgery (GAS) that includes hysterectomy and oophorectomy in transmen or orchiectomy in transwomen results in permanent sterility. ... (GD) undergoing sex reassignment surgery (SRS). J Sex Med 2015; 12:2190-200. 10.1111/jsm.13022 ...
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender.The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals.
Facial feminization surgery (FFS) is a series of plastic surgery procedures that reshape the forehead, hairline, eyebrows, nose, cheeks, and jawline. Nonsurgical treatments like cosmetic fillers ...
Reversal surgery in regretful male-to-female transsexuals after sex reassignment surgery. J Sex Med, 13 (2016), ... Adolescents with gender identity disorder who were accepted or rejected for sex reassignment surgery: a prospective follow-up study. J Am Acad Child Psychiatr, 40 (2001), pp. 472-481, 10.1097/00004583-200104000-00017.
Feminizing hormone therapy also is called gender-affirming hormone therapy. Feminizing hormone therapy involves taking medicine to block the action of the hormone testosterone. It also includes taking the hormone estrogen. Estrogen lowers the amount of testosterone the body makes. It also triggers the development of feminine secondary sex ...
Gender reassignment surgery is a series of complex surgical procedures (genital and nongenital) performed for the treatment of gender dysphoria. Genital procedures performed for gender dysphoria, such as vaginoplasty, clitorolabioplasty, penectomy and orchidectomy in male-to-female transsexuals, and penile and scrotal reconstruction in female ...
Researchers surveyed 27,715 TGD adults, including 17,151 people (61.9 percent) who said they had gender-affirming treatment, with 2,242 (13.1 percent) of them reporting a history of ...
Transgender and non-binary (TGNB) individuals often experience gender dysphoria. TGNB individuals with gender dysphoria may undergo genital gender-affirming surgery including vaginoplasty, phalloplasty, or metoidioplasty so that their genitourinary anatomy is congruent with their experienced gender. Given decreasing social stigma and increasing coverage from private and public payers, there ...
Treatment Gender dysphoria. Treatment. Treatment for gender dysphoria aims to help people live the way they want to, in their preferred gender identity or as non-binary. What this means will vary from person to person, and is different for children, young people and adults. Waiting times for referral and treatment are currently long.
With 30 years of combined expertise in gender affirmation surgery, Dr. Ergun Kocak, Dr. Pankaj Tiwari, and Dr. Santosh Kale are among Ohio's most experienced and trusted reverse top surgeons. Our team performs hundreds of successful gender reassignment procedures each year, and we take pride in providing personalized care and achieving ...
Gender dysphoria, earlier known as gender identity disorder, describes a heterogeneous group of individuals having the desire to possess secondary sexual characteristics of the opposite sex and possessing varying degrees of dissatisfaction regarding their anatomical gender . Gender reassignment surgery (GRS) has proven to be a revolutionary ...
When he was 14, Reimer began the process of reassignment to being a male. As an adult, he married a woman but depression and drug abuse ensued, culminating in suicide at the age of 38 (1). Money's ...
Sex reassignment surgery could also be banned for minors. Reacting to the report, Ypomoni, a French parents' group, said: "We welcome this return to reason." Maud Vasselle, a mother whose daughter underwent gender transition treatment, told Le Figaro: "A child is not old enough to ask to have her body altered.
Wyoming's Republican governor has signed a bill into law banning doctors in that state from performing gender transitioning and gender reassignment procedures for children.
French Senators want to ban gender transition treatments for under-18s, after a report described sex reassignment in minors as potentially "one of the greatest ethical scandals in the history of ...
Republican Gov. Mark Gordon (R-WYo.) signed a series of bills banning gender reassignment surgery on minors. However, he rejected a bill that would have elevated significant barriers to abortion ...
Gender reassignment is a difficult process, including not only hormonal treatment with possible surgery but also social discrimination and stigma. There is a great variety between countries in specified tasks involved in gender reassignment, and a complex combination of medical treatment and legal paperwork is required in most cases.
Wyoming's Gov. Mark Gordon passed legislation Friday outlawing gender-reassignment procedures on minors in the state and vetoed a separate bill that would have placed additional restrictions on ...
Wyoming just became the 24th state banning physicians from performing gender transitioning and gender reassignment procedures for... #donaldtrump #community
Wyoming governor signs bill banning gender reassignment surgery, care. Politics. Posted on AllSides March 23rd, 2024. Save for Later . From The Center. Read full story. Politics. United Press International. AllSides Media Bias Rating: Center. agree; disagree; 125387 / 93967.